Professional Documents
Culture Documents
Uti Case416
Uti Case416
Uploaded by
Ted Cipriano VistaCopyright:
Available Formats
You might also like
- Lab09 Therapy4 IronDeficiencyDocument5 pagesLab09 Therapy4 IronDeficiencyHayna Rose100% (1)
- Kolkata Paces Final-1Document17 pagesKolkata Paces Final-1Dr. Tom100% (1)
- Nbme 18Document49 pagesNbme 18Dilawar Jan95% (38)
- Nursing Informatics in South AmericaDocument3 pagesNursing Informatics in South AmericaTed Cipriano VistaNo ratings yet
- Staff Round: Ward 32 Prof. N. Gupta UnitDocument22 pagesStaff Round: Ward 32 Prof. N. Gupta UnitSaroj SahooNo ratings yet
- Morning Report: Jawaria K. Alam, MD/PGY3Document20 pagesMorning Report: Jawaria K. Alam, MD/PGY3Emily EresumaNo ratings yet
- Timothy P. Moran Patient H&P #14 CC: Bilateral Knee Pain HpiDocument4 pagesTimothy P. Moran Patient H&P #14 CC: Bilateral Knee Pain Hpistarskyhutch0000No ratings yet
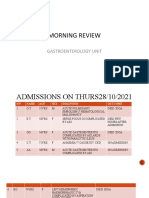
- MR GastroDocument31 pagesMR GastroAdefuye AbiolaNo ratings yet
- More Than A Sore ThroatDocument17 pagesMore Than A Sore ThroatEmily EresumaNo ratings yet
- PCC CaseDocument9 pagesPCC CaseKaila AbeledaNo ratings yet
- Case PresentationDocument42 pagesCase Presentationjose henaoNo ratings yet
- 5 PancreatitisDocument15 pages5 PancreatitisAbdullah As'adNo ratings yet
- Long CaseDocument16 pagesLong CaseGolam Fahad ZahidNo ratings yet
- Esrd FinalDocument26 pagesEsrd FinalCreighton A. BayonganNo ratings yet
- Varicoceles 02.01.2012Document12 pagesVaricoceles 02.01.2012Emily EresumaNo ratings yet
- History of Present IllnessDocument10 pagesHistory of Present IllnessArepalli SanthoshNo ratings yet
- A Patient With Haemoptysis: Professorial Group B Iwc 3 MFC 864 - 873Document31 pagesA Patient With Haemoptysis: Professorial Group B Iwc 3 MFC 864 - 873Tashii TsheringNo ratings yet
- YL3 GI End of Module Activity Complex Task - StudentsDocument1 pageYL3 GI End of Module Activity Complex Task - StudentsAnonymous Xlpj86laNo ratings yet
- Case Presentation On Chronic Liver Disease: Shreyas M Salimath Pharm D 2 Year REG NO. 21Q0172Document18 pagesCase Presentation On Chronic Liver Disease: Shreyas M Salimath Pharm D 2 Year REG NO. 21Q0172AmalinNo ratings yet
- Lab 10Document5 pagesLab 10Mira Mhsen KhaloufNo ratings yet
- Written Case Report HADocument7 pagesWritten Case Report HAJoan junioNo ratings yet
- Respiratory System Diseases Case StudyDocument9 pagesRespiratory System Diseases Case Studykuyetjoy20No ratings yet
- Sickle CellDocument47 pagesSickle CellEmily EresumaNo ratings yet
- Fasciola: A 53-Year-Old Man With Intermittent Colicky Abdominal Pain Due To Incarceration in Common Bile Duct: A CaseDocument5 pagesFasciola: A 53-Year-Old Man With Intermittent Colicky Abdominal Pain Due To Incarceration in Common Bile Duct: A CaseCahyo TriwidiantoroNo ratings yet
- IJSCR 109192 Session ReportDocument11 pagesIJSCR 109192 Session ReportFarhan ShahzadNo ratings yet
- A PT With AnemiaDocument2 pagesA PT With AnemiaCharl UnalNo ratings yet
- Nbme 18 AnswersDocument27 pagesNbme 18 AnswersUsmle Usmle100% (1)
- Nbme 18 AnswersDocument27 pagesNbme 18 AnswersUsmle Usmle100% (1)
- NCM 103 (RLE) : Bangued, AbraDocument26 pagesNCM 103 (RLE) : Bangued, AbraJess L PayagNo ratings yet
- AnasarcaDocument54 pagesAnasarcaSulaiman TahsinNo ratings yet
- Nbme 18Document49 pagesNbme 18Romina GomezNo ratings yet
- Renal Cell Carcinoma Tuberous SclerosisDocument48 pagesRenal Cell Carcinoma Tuberous SclerosisPiyushNo ratings yet
- Grand Round Final DraftDocument80 pagesGrand Round Final DraftBol Dhalbeny MalualNo ratings yet
- NDocument35 pagesNNitish SinghNo ratings yet
- Imm and Inf Case Infected WoundDocument7 pagesImm and Inf Case Infected WoundRafaela Dela CruzNo ratings yet
- Case History: Personal DataDocument5 pagesCase History: Personal DataMohammed AhmedNo ratings yet
- Breast and Endocrine Case Report - Mohammed AlrubaiaanDocument8 pagesBreast and Endocrine Case Report - Mohammed Alrubaiaantwgp6pg5ghNo ratings yet
- Rury PomrDocument11 pagesRury Pomrabng1278No ratings yet
- Practice Based Learning (Grand Round)Document48 pagesPractice Based Learning (Grand Round)AnnumNo ratings yet
- Renal Disorders Case 5Document2 pagesRenal Disorders Case 5Geriz Daniella VigoNo ratings yet
- Infective Endocarditis CaseDocument3 pagesInfective Endocarditis CaseMershen GaniaNo ratings yet
- Case 167: MD Pediatrics PHD Ped Study Children Special NeedDocument49 pagesCase 167: MD Pediatrics PHD Ped Study Children Special NeedMona MostafaNo ratings yet
- General Data EdwinDocument3 pagesGeneral Data EdwinEdwin AngelesNo ratings yet
- NBM18Q&ADocument11 pagesNBM18Q&AIlse Pol TRuizNo ratings yet
- EMQsDocument30 pagesEMQsnob2011nob100% (1)
- Acute AppendicitisDocument6 pagesAcute Appendicitiscuka suka jerpNo ratings yet
- Peds Case 3Document5 pagesPeds Case 3Mohammed AhmedNo ratings yet
- PIDC Grand Round FinalDocument32 pagesPIDC Grand Round Finalhailu henockNo ratings yet
- Hashim Major LogDocument26 pagesHashim Major LogHashim AlsammawiNo ratings yet
- All Recalls of MDDocument517 pagesAll Recalls of MDaliakbar178No ratings yet
- MR SulaemanDocument14 pagesMR Sulaemanfikriatul fadhilahNo ratings yet
- A Case Study For Patient X: Saint Louis University College of Nursing Baguio CityDocument24 pagesA Case Study For Patient X: Saint Louis University College of Nursing Baguio CityJemima AtigaNo ratings yet
- Liver Cirrhosis: DR - Aryadevi A SDocument89 pagesLiver Cirrhosis: DR - Aryadevi A SMahesh PethkarNo ratings yet
- Incase 21102016 Lung TumorDocument39 pagesIncase 21102016 Lung TumorwenyinriantoNo ratings yet
- Pancytopenia Secondary To Bacterial SepsisDocument16 pagesPancytopenia Secondary To Bacterial Sepsisiamralph89No ratings yet
- Case ReportDocument12 pagesCase Reportmohammad khinagirNo ratings yet
- Dr. Farin's Grand Round Presentation 31.09.23Document75 pagesDr. Farin's Grand Round Presentation 31.09.23Anika TasnimNo ratings yet
- HematocheziaDocument27 pagesHematocheziaEmily EresumaNo ratings yet
- Syok Hipovolemik PerbaikanDocument24 pagesSyok Hipovolemik Perbaikanyoelpurnama1991No ratings yet
- Thoracic SurgeryDocument33 pagesThoracic SurgeryTed Cipriano VistaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Chief Complaint: IndependentDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Chief Complaint: IndependentTed Cipriano VistaNo ratings yet
- Bela BartokDocument7 pagesBela BartokTed Cipriano VistaNo ratings yet
- PIHDocument2 pagesPIHTed Cipriano VistaNo ratings yet
- Pih Grup 2Document1 pagePih Grup 2Ted Cipriano VistaNo ratings yet
Uti Case416
Uti Case416
Uploaded by
Ted Cipriano VistaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Uti Case416
Uti Case416
Uploaded by
Ted Cipriano VistaCopyright:
Available Formats
Urinary Tract Infection Case Study SP is a 21 year old male who is S/P MVA with subsequent paraplegia one
year ago. He has been straight catheterizing himself 4 times a day since that time. He presents to the ER with complaints of malaise, fevers, occasional chills, hematuria and anorexia. PMH: 1. Paraplegia secondary to C4-5 fracture one year ago. 2. L4 and L3 fractures. 3. Basal skull fracture. 4. Rib fractures. 5. S/P inferior vena cava filter for DVT and PE. 6. Depression. 7. Nonhealing leg wounds with osteomyelitis of the right leg. 8. History of VRE and Pseudomonas in his urine two months ago. FH: Noncontributory
SH: Patients lives with his parents. He denies tobacco use. He intermittently binge drinks. MEDS: Neurontin 300 mg 5x/day, Ditropan 10 mg bid, Prevacid 15 mg qd, MVI, Effexor XR qd, Colace, Baclofen 10 mg qd, Warfarin 8 mg qd, and Ampicillin which was discontinued several days ago. ALL: PE: Tape and possibly milk Flushed white male who is quite warm to the touch with a temp of 102.2, BP 120/70, P 96, R 23. HEENT: Anicteric, no conjunctival lesions, no nasal discharge. There is a well-healed former tracheostomy site. Lungs: clear to A/P. COR: mild tachycardia but regular, without murmur. ABD: Slight fullness in the RLQ, bowel sounds present. Back is without skin breakdown. CVA tenderness could not be assessed. EXT: left lower extremity has a 10 cm ulcer over the posterior calf with good granulation tissue surrounding a rim of maceraton. A right heel ulcer is clean and without discharge. Wt. 65 kg.
LABS: WBCs 18,900 with 13% bands, H/H 12.4/36.6, Plts 132,000, PT 22.6, INR 3.9, Na 135, Cl 101, K 4.1, C02 28, BUN 25 mg/dL, SrCr 1.6 mg/dL, glucose 125 mg/dL, Urine R and M bloody, nitrite positive, Leukocyte esterase large, WBCs 15-30, RBCs 15-30.
1. What signs and symptoms are consistent with pyelonephritis?
2. What is the most likely pathogen? 3. What would be your initial empiric antibiotic therapy?
4. At 24 hours the blood culture is positive for gm-negative rods, lactose negative, oxidase positive (2/2 bottles). Would this cause you to modify your initial empiric therapy? If you would change therapy, what would be the new regimen?
You might also like
- Lab09 Therapy4 IronDeficiencyDocument5 pagesLab09 Therapy4 IronDeficiencyHayna Rose100% (1)
- Kolkata Paces Final-1Document17 pagesKolkata Paces Final-1Dr. Tom100% (1)
- Nbme 18Document49 pagesNbme 18Dilawar Jan95% (38)
- Nursing Informatics in South AmericaDocument3 pagesNursing Informatics in South AmericaTed Cipriano VistaNo ratings yet
- Staff Round: Ward 32 Prof. N. Gupta UnitDocument22 pagesStaff Round: Ward 32 Prof. N. Gupta UnitSaroj SahooNo ratings yet
- Morning Report: Jawaria K. Alam, MD/PGY3Document20 pagesMorning Report: Jawaria K. Alam, MD/PGY3Emily EresumaNo ratings yet
- Timothy P. Moran Patient H&P #14 CC: Bilateral Knee Pain HpiDocument4 pagesTimothy P. Moran Patient H&P #14 CC: Bilateral Knee Pain Hpistarskyhutch0000No ratings yet
- MR GastroDocument31 pagesMR GastroAdefuye AbiolaNo ratings yet
- More Than A Sore ThroatDocument17 pagesMore Than A Sore ThroatEmily EresumaNo ratings yet
- PCC CaseDocument9 pagesPCC CaseKaila AbeledaNo ratings yet
- Case PresentationDocument42 pagesCase Presentationjose henaoNo ratings yet
- 5 PancreatitisDocument15 pages5 PancreatitisAbdullah As'adNo ratings yet
- Long CaseDocument16 pagesLong CaseGolam Fahad ZahidNo ratings yet
- Esrd FinalDocument26 pagesEsrd FinalCreighton A. BayonganNo ratings yet
- Varicoceles 02.01.2012Document12 pagesVaricoceles 02.01.2012Emily EresumaNo ratings yet
- History of Present IllnessDocument10 pagesHistory of Present IllnessArepalli SanthoshNo ratings yet
- A Patient With Haemoptysis: Professorial Group B Iwc 3 MFC 864 - 873Document31 pagesA Patient With Haemoptysis: Professorial Group B Iwc 3 MFC 864 - 873Tashii TsheringNo ratings yet
- YL3 GI End of Module Activity Complex Task - StudentsDocument1 pageYL3 GI End of Module Activity Complex Task - StudentsAnonymous Xlpj86laNo ratings yet
- Case Presentation On Chronic Liver Disease: Shreyas M Salimath Pharm D 2 Year REG NO. 21Q0172Document18 pagesCase Presentation On Chronic Liver Disease: Shreyas M Salimath Pharm D 2 Year REG NO. 21Q0172AmalinNo ratings yet
- Lab 10Document5 pagesLab 10Mira Mhsen KhaloufNo ratings yet
- Written Case Report HADocument7 pagesWritten Case Report HAJoan junioNo ratings yet
- Respiratory System Diseases Case StudyDocument9 pagesRespiratory System Diseases Case Studykuyetjoy20No ratings yet
- Sickle CellDocument47 pagesSickle CellEmily EresumaNo ratings yet
- Fasciola: A 53-Year-Old Man With Intermittent Colicky Abdominal Pain Due To Incarceration in Common Bile Duct: A CaseDocument5 pagesFasciola: A 53-Year-Old Man With Intermittent Colicky Abdominal Pain Due To Incarceration in Common Bile Duct: A CaseCahyo TriwidiantoroNo ratings yet
- IJSCR 109192 Session ReportDocument11 pagesIJSCR 109192 Session ReportFarhan ShahzadNo ratings yet
- A PT With AnemiaDocument2 pagesA PT With AnemiaCharl UnalNo ratings yet
- Nbme 18 AnswersDocument27 pagesNbme 18 AnswersUsmle Usmle100% (1)
- Nbme 18 AnswersDocument27 pagesNbme 18 AnswersUsmle Usmle100% (1)
- NCM 103 (RLE) : Bangued, AbraDocument26 pagesNCM 103 (RLE) : Bangued, AbraJess L PayagNo ratings yet
- AnasarcaDocument54 pagesAnasarcaSulaiman TahsinNo ratings yet
- Nbme 18Document49 pagesNbme 18Romina GomezNo ratings yet
- Renal Cell Carcinoma Tuberous SclerosisDocument48 pagesRenal Cell Carcinoma Tuberous SclerosisPiyushNo ratings yet
- Grand Round Final DraftDocument80 pagesGrand Round Final DraftBol Dhalbeny MalualNo ratings yet
- NDocument35 pagesNNitish SinghNo ratings yet
- Imm and Inf Case Infected WoundDocument7 pagesImm and Inf Case Infected WoundRafaela Dela CruzNo ratings yet
- Case History: Personal DataDocument5 pagesCase History: Personal DataMohammed AhmedNo ratings yet
- Breast and Endocrine Case Report - Mohammed AlrubaiaanDocument8 pagesBreast and Endocrine Case Report - Mohammed Alrubaiaantwgp6pg5ghNo ratings yet
- Rury PomrDocument11 pagesRury Pomrabng1278No ratings yet
- Practice Based Learning (Grand Round)Document48 pagesPractice Based Learning (Grand Round)AnnumNo ratings yet
- Renal Disorders Case 5Document2 pagesRenal Disorders Case 5Geriz Daniella VigoNo ratings yet
- Infective Endocarditis CaseDocument3 pagesInfective Endocarditis CaseMershen GaniaNo ratings yet
- Case 167: MD Pediatrics PHD Ped Study Children Special NeedDocument49 pagesCase 167: MD Pediatrics PHD Ped Study Children Special NeedMona MostafaNo ratings yet
- General Data EdwinDocument3 pagesGeneral Data EdwinEdwin AngelesNo ratings yet
- NBM18Q&ADocument11 pagesNBM18Q&AIlse Pol TRuizNo ratings yet
- EMQsDocument30 pagesEMQsnob2011nob100% (1)
- Acute AppendicitisDocument6 pagesAcute Appendicitiscuka suka jerpNo ratings yet
- Peds Case 3Document5 pagesPeds Case 3Mohammed AhmedNo ratings yet
- PIDC Grand Round FinalDocument32 pagesPIDC Grand Round Finalhailu henockNo ratings yet
- Hashim Major LogDocument26 pagesHashim Major LogHashim AlsammawiNo ratings yet
- All Recalls of MDDocument517 pagesAll Recalls of MDaliakbar178No ratings yet
- MR SulaemanDocument14 pagesMR Sulaemanfikriatul fadhilahNo ratings yet
- A Case Study For Patient X: Saint Louis University College of Nursing Baguio CityDocument24 pagesA Case Study For Patient X: Saint Louis University College of Nursing Baguio CityJemima AtigaNo ratings yet
- Liver Cirrhosis: DR - Aryadevi A SDocument89 pagesLiver Cirrhosis: DR - Aryadevi A SMahesh PethkarNo ratings yet
- Incase 21102016 Lung TumorDocument39 pagesIncase 21102016 Lung TumorwenyinriantoNo ratings yet
- Pancytopenia Secondary To Bacterial SepsisDocument16 pagesPancytopenia Secondary To Bacterial Sepsisiamralph89No ratings yet
- Case ReportDocument12 pagesCase Reportmohammad khinagirNo ratings yet
- Dr. Farin's Grand Round Presentation 31.09.23Document75 pagesDr. Farin's Grand Round Presentation 31.09.23Anika TasnimNo ratings yet
- HematocheziaDocument27 pagesHematocheziaEmily EresumaNo ratings yet
- Syok Hipovolemik PerbaikanDocument24 pagesSyok Hipovolemik Perbaikanyoelpurnama1991No ratings yet
- Thoracic SurgeryDocument33 pagesThoracic SurgeryTed Cipriano VistaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Chief Complaint: IndependentDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Chief Complaint: IndependentTed Cipriano VistaNo ratings yet
- Bela BartokDocument7 pagesBela BartokTed Cipriano VistaNo ratings yet
- PIHDocument2 pagesPIHTed Cipriano VistaNo ratings yet
- Pih Grup 2Document1 pagePih Grup 2Ted Cipriano VistaNo ratings yet