Professional Documents
Culture Documents
Papular Acrodermatitis of Childhood: An Australia Antigen
Papular Acrodermatitis of Childhood: An Australia Antigen
Uploaded by
ghinsavitOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Papular Acrodermatitis of Childhood: An Australia Antigen
Papular Acrodermatitis of Childhood: An Australia Antigen
Uploaded by
ghinsavitCopyright:
Available Formats
Archives of Disease in Childhood, 1973, 48, 794.
Papular acrodermatitis of childhood
An Australia antigen disease
FERDINANDO GIANOTTI
From the Department of Dermatology, University of Milan, Italy
Gianotti, F. (1973). Archives of Disease in Childhood, 48, 794. Papular acrodermatitis of childhood: an Australia antigen disease. Papular acrodermatitis (PAC) is a fairly widespread, probably slightly infectious, nonrelapsing disease of childhood characterized by (a) papular eruption on the face and limbs lasting 20 days or more, (b) reactive reticulohistiocytic lymphadenitis, and (c) acute hepatitis, usually anicteric, which commonly lasts about 2 months. Australia antigen is always present; it is detectable 10 or more days after the onset of the skin eruption and persists from 2 months to several years. The mother of some children with PAC are found to be carriers of Au antigen, as are some sibs when tested many years later. Whether the causative agent of PAC is the same as that causing serum hepatitis, or is different, remains to be established.
Papular acrodermatitis of childhood (PAC) is an infective disease characterized by a recognizable skin eruption localized to the face and limbs, by enlargement of lymph nodes (mainly inguinal and axillary), and by an acute hepatitis which is usually anicteric, but is always associated with Australia antigenaemia. The present article reviews current knowledge of the condition and its possible relation to serum hepatitis. PAC was first recognized in Milan in 1953 and described by Gianotti (1955). Since then the disease has been reported all over the world (Bernhardt and Szczepanski, 1968; Blagoslovenskii, 1970; Blancher et al., 1962; Boyanov, Boyanov, and Dimitrova, 1963; Braun-Falco and Rupec, 1964; Brown and Rentiers, 1969; Despres et al., 1969; Duperrat and Puissant, 1958; Eiloart, 1966; Jeune, Moulin, and Rosenberg, 1964; Nurse, 1967; Pomposiello and Abulafia, 1968; Reich, 1963; Schirren and Mutter, 1964; Stevanovic and Sofronic, 1962; Terao and Takemura, 1971; Thiers and Moulin, 1964; Vulcan, Wolkonsky, and Nicolescu, 1965; Winkelmann and Bourlond, 1965; Woerderman, 1965).
Clinical and pathological features Cutaneous lesions. The eruption consists of monomorphic, lenticular, flat erythematopapular, nonitching lesions, symmetrically spread over face, buttocks, and limbs (Fig. 1). The trunk is usually spared, but a
Received 19 March 1973.
transient rash may be seen on it in the early eruptive phase; the eruption develops in a few days and lasts for 15 to 20 days or more. The mucous membranes are not affected. This is the eruption usually found in children between 2 and 6 years of age; but in infancy larger lesions 5 to 10 mm in diameter are seen, while in older children the dermatitis is often micropapular, 1 to 2 mm in diameter. In the few cases observed in adults the lesions had the typical lenticular form. Occasionally the lesions have a purpura-like appearance or are infiltrated so as to protrude from the skin surface. During the eruptive phase the Koebner reaction may be used. The skin eruption does not relapse. Histo-
(b) (a) FIG. 1.-Typical case of papular acrodermatitis. The cutaneous eruption remains localized to the (a) face and (b) limbs.
794
Papular acroderrn atitis of childhood
logically, the cutaneous lesion shows a perivascular lympho-monocytic and histiocytic infiltration of the papillary and superficial dermis. In the epidermis Langerhans cells are abundant, as shown by electron
microscopy.
795
Lymphadenitis. The enlargement of lymph nodes, mainly inguinal and axillary, lasts for 2 or 3 months. Biopsy studies show a 'reactive reticulohistiocytic hyperplasia' consisting of (a) conspicuous activation of the endothelial components, with thickening of the endothelium of the capillaries and prominent sinuses, (b) proliferation of pleomorphic reticulohistiocytic elements in small groups, within and outside the follicle centres, sometimes with the presence of binucleate cells. With the electron microscope (Jean, Lambertenghi, and Gianotti, 1968) the main proliferating histiocytes appear to be sinusoid-lining cells, sometimes containing Langerhans granules. Hepatitis. Acute hepatitis always occurs; it is generally anicteric but in some children, usually those over 6 years, jaundice may appear about 20 days after the onset of the skin eruption (Gianotti, 1966; Jean et al., 1967; Bologa, 1966; Cieri, Rezza, and Anibaldi, 1966; De Benedetti, 1969; Ricciardiello, 1969). The liver usually remains clinically enlarged, but not tender, for 1 to 3 months. There are high levels of SGOT and SGPT (sometimes exceeding 2000 units/ml), aldolase, glucose-6-phosphatase, and alkaline phosphatase; bromsulphalein retention is raised (up to 400o), but serum bilirubin is usually not increased. In most cases the hepatitis begins at the same time as, or a week or two after, the skin eruption. After the first month when the eruption is fading the hepatitis is generally in a fully developed stage. The changes in serum enzymes usually persist for 2 to 3 months but levels sometimes remain raised for months or even years. Liver biopsy (in 32 children) has shown that during the dermatitis phase the histological picture is indistinguishable from that of acute viral hepatitis (Jean et al., 1967). 6 months to a year or more after the onset of the dermatitis liver biopsy has shown either a normal histological picture, or that of a persistent chronic hepatitis. Rarely the picture has been that of a chronic aggressive hepatitis with moderate activity, type A (De Groote et al., 1968) and, in these cases, SGOT and SGPT levels often remain slightly increased. The liver eventually returns to normal, though this may take as long as 4 years. 23 biopsies obtained from 16 children at different phases of the anicteric hepatitis have been studied by electron microscopy, with findings similar to those found in acute viral hepatitis (Jean et al., 1967).
monocytic cells (up to 20%) and Turk's cells. The electron microscope shows these monocytes to be identical with those found in infectious mononucleosis (Jean, Ranzi, and Lambertenghi, 1969). In bone marrow there is an increase in the number of histiocytes and eosinophils. The Paul-Bunnell test, the dye test, and complement-fixation for toxoplasmosis are negative. In the acute phase there is an increase in a2- and a-globulins; in the late phase y-globulins may be increased. Epidemiology The infectiousness of the disease appears low, so that more than one case occurs only occasionally in infant communities or in a family. Sporadic cases occur throughout the year, and though there is no marked seasonal incidence, PAC frequently occurs within a period of a few days in some children in distant districts of a city, though it is not known what these children might have in common. The
children have not received injections or blood transfusion. Occasionally, the disease occurs in sibs after 1 or more years; in these families the patient who had originally suffered from PAC has remained an Au antigen carrier. Children with Down's syndrome seem to be predisposed to PAC, and we have seen 5 such cases.
Aetiological findings PAC shows all the characteristic features of a diffuse hyperplasic reactive reticulohistiocytosis of viral orgin, though the virus is still unidentified despite many investigations by us and others.
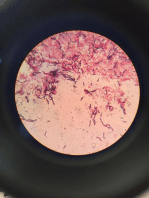
Electron microscopy findings. In lymph nodes of children with PAC, particles 40 to 50 nm in diameter, bounded by a membrane and containing an electron-opaque core, have been observed within the cytoplasm of some sinusoid-lining cells (Jean et al., 1968). These particles have a similar structure to those seen in organ cultures inoculated with serum from hepatitis patients with Au antigenaemia (Jenson et al., 1970), and to those seen in the endoplasmic reticulum of hepatocytes of Au antigen carriers (Stein, Fainaru, and Stein, 1972). These particles resemble the virus-like particles about 42 nm in diameter that have been found in Au antigen positive hepatitis patients by Dane, Cameron, and Briggs (1970). Also, in the cytoplasm of some macrophages and reticular cells of the liver we have Other symptoms and laboratory findings. found (Jean et al., 1967) some spherical particles, Constitutional symptoms at no stage are more than slight, showing an electron-opaque core, surrounded by a with mild fever and lassitude. The blood shows normal with an outer granular layer (Fig. membrane double erythrocyte sedimentation rate (ESR), mild hypochromic anaemia, increased vascular fragility with normal 2); these particles appear to be in close connexion platelets; prothrombin activity 50 to 90/%; leucocytes with cisternae of the endoplasmic reticulum and normal or diminished with a relative abundance of Golgi's apparatus. Indeed, such virus-like particles
796
Ferdinando Gianotti
FIG. 2.-Liver biopsy during the dermatitis phase. Reticulohistiocytic cell in the cytoplasm containing numerous particles (arrows) with electron-opaque core, surrounded by double membrane with an outer granular layer.
Papular acrodermatitis of childhood
show the same structures as those seen in the cytoplasm of hepatocytes and Kupffer's cells of children suffering from infectious icteric hepatitis, after azothioprine administration (Sirtori, 1970).
797
Differential diagnosis PAC has characteristic clinical features so that most cases are easily recognized. However, there are some papular eruptions of childhood from which it has to be differentiated. New papular erythema of childhood (Brunner, Rubin, and Dunlap, 1962) is characterized by small conical erythematous papules, sometimes coalescent, generally sited unilaterally near the axilla, on an arm or side of the trunk; itching is moderate. Frictional lichenoid eruption in children (Waisman and Sutton, 1966) presents as pale, flat papules, 1 to 2 mm in diameter, closely aggregated centrally in the plaque; these papules are mainly localized on the elbow, knee, dorsum of and the extensor aspects of the forearms; fingers, TABLE I itching is absent. The cutaneous eruption papuloPersistence of Australia antigen in the blood of 25 vesicular-acrolocated syndrome described by us children after papular acrodermatitis (Crosti and Gianotti, 1964), and then by others (Brown and Rentiers, 1969; Eiloart, 1966; Hjorth, AuAg negative AuAg still positive Kopp, and Osmundsen, 1967; Puissant et al., 1966; Stevanovic and Sofronic, 1962; Terao and Length of time Length of time Takemura, 1971; Winkelmann and Bourlond, 1965), No. cases after skin No. cases since skin eruption eruptions (yr) is more likely to cause confusion, the most important features of the two diseases being summarized in 4 4 mth 7 Within 2 mth 3 1 3 Within 3 mth Table II. 2 2 2 6 Comment 2 8 19 the of The nature hepatitis that occurs in this 11 1 1 disease remains to be established. The hepatitis of PAC is distinguishable from that caused by yellow with PAC. 10 of the 25 became AuAg negative fever, by cytomegalovirus infection, and by Epsteinwithin the first 3 months, while 15 so far remain Barr virus infection (giving rise to infectious positive, either having remained positive throughout mononucleosis), since the hepatitis of these diseases or having shown short intervals of being negative. has distinct clinical and pathological features, and Of 3 sisters who all suffered from PAC 8 years ago, since it is never associated with Au antigenaemia. Short-incubation infectious hepatitis (virus A), only one still remains AuAg positive. AuAg becomes detectable in the serum by the though indistinguishable from PAC in its histotime the hepatitis has developed and SGOT and pathological aspects, can be differentiated both on SGPT have reached high levels. The persistence clinical grounds and from the lack of Au antiof AuAg in the blood during subsequent months is genaemia. It is more difficult to establish the relation, if any, usually accompanied by slightly raised levels of SGOT and SGPT. 1 to 2 years after the eruption, between long-incubation hepatitis (virus B) and the AuAg may still be present with normal SGOT and hepatitis of PAC, now that it is clear that Au antigenaemia is not peculiar to serum hepatitis but SGPT levels. A search for AuAg among other members of the occurs also in PAC. Some of the features of PACfamily of children with PAC revealed that 3 mothers the constant association of hepatitis with skin
Australia antigen (AuAg). We have assayed Australia antigen in the serum of 39 children with PAC by immunodiffusion as described by Prince (1968), or by electro-syneresis, as described by Bedarida, Trinchieri, and Carbonara (1969). AuAg was repeatedly detected in the serum of all 39 children throughout the skin eruptive phase (Gianotti, 1970, 1971). In 4 children AuAg appeared 10 to 15 days after the onset of the eruption, while in the other 35 children AuAg was already present when they came under observation. Other investigators (De Gaspari, Bardare, and Costantino, 1970; Pifnol-Aguade and Mascaro, 1971) have detected AuAg in PAC, whereas the Milan antigen, i.e. the serum antigen associated with infectious epidemic hepatitis, is absent (Costantino et al., 1973). Table I gives the results of following 25 children
of children in the eruptive phase were AuAg positive. 3 mothers whose children had been affected by PAC 11, 6, and 1j years before were also found to be AuAg positive. 2 children whose brothers had suffered from PAC, 6 and 1 years before, were AuAg positive. In these families the child who had originally been affected by PAC usually remained AuAg positive.
798
Ferdinando Gianotti
TABLE II
Differentiation of papular acrodermatitis from papulo-vesicular-acrolocated syndrome
Papular acrodermatitis of childhood
Papulo-vesicular-acrolocated syndrome
2-6 yr
Age Cutaneous lesions Location
Eruption Pruritus Capillary fragility Koebner reaction Pathology Lymph node enlargement Splenomegaly Liver Australia antigen Course Infectiousness Relapse
6 mth-12 yr Lentilform erythematous papules Symmetrical on face, buttocks, limbs (antecubital and popliteal surfaces spared); no coalescence lesions Not recurrent Absent Common Present Lympho-mono-histiocytic infiltrate in superficial dermis, predominantly perivascular
Inguinal and axillary Slight and transient Acute hepatitis Present 15-25 dy Slight Never
Pink pinhead-sized vesicular-like papules Symmetrical on cheeks, ears, buttocks, and limbs; lesions may coalesce in patches on limbs Sometimes recurrent Common Rare Absent Spongiosis and sometimes vesiculation; lymphomonocytic exocitosis and infiltration in perivascular papillary dermis Inguinal and axillary Absent Normal
Absent 20-50 dy None Very rare
eruption and lymphadenitis, the lack of Au antigenaemia in the earliest phase, its occurrence without contact with human blood-might suggest that PAC and serum hepatitis are two different diseases due to different viruses. However, the fact that both are constantly associated with Au antigenaemia, and have similar microscopical and ultramicroscopical pathology, and that their contagiousness is low, suggests that the two conditions may be linked. If the two diseases are due to a single infectious agent, then PAC would represent the naturally occurring form of primary infection of the serum hepatitis disease. In keeping with this view, the primary infection of PAC occurs almost exclusively in children who are intially AuAnegative. If this view is correct, it is not clear why cases of serum hepatitis from inoculation of blood carrying Au are not associated with the cutaneous and lymph node manifestationzs of PAC. Possibly these manifestations appear only when the infection is acquired by cutaneous or mucous membrane routes, or when some particular genetic or immunological situation exists, as in the apparently high incidence of PAC in children with Down's syndrome.
REFERENCES
Belarida, G., Trinchieri, G., and Carbonara, A. (1969). The detection cf Australia antigen and anti-Au antibodies by a rapid procedure combining electrophoresis and immunoprecipitation.
Haematologica, 54, 591. Bernhardt, E., and Szczepanski, A. (1968). Zespol GianottiegoCrostiego. Przeglad Dermatologiczny, 55, 513. Blagoslovenskii, G. S. (1970). The Gianotti-Crosti syndrome in children. VoprosY? Okhrany Materinstvai Detstva, 15, 84. Blancher, G., Sugier, J., Pringuet, G., Bach, C., and Rossier, A. (1962). Acrodermatite erythemato-papuleuse infantile (syndrome de Gianotti-Crosti). Contribution a la discussion de l'etiologie. Annales de Pediatrie. 9, 609.
Bologa, E. I. (1966). Sur la participation hepatique dans l'acrodermatite papuleuse infantile. Syndrome de Gianotti-Crosti. Giornale Italiano di Dermatologia, 107, 1385. Boyanov, L., Boyanov, B., and Dimitrova, I. (1963). The clinical picture and pathogenesis of the Gianotti-Crosti syndrome. Vestnik Dermatologit i Venerologii, 37, No. 2, 14. Braun-Falco, O., and Rupec, M. (1964). Ober das GianottiCrosti-Syndrom. Medizinische Klinik, 59, 210. Brown, J., and Rentiers, P. (1969). The Gianotti-Crosti syndrome: a distinctive exanthem. Canadian Medical Association J'ournal, 100, 773. Brunner, M. J., Rubin, L., and Dunlap, F. (1962). A new papular erythema of childhood. Archives of Dermatology, 85, 539. Cieri, E., Rezza, E., and Anibaldi, A. (1966). Studio clinico di 8 casi di dermatite maculo-papulosa acroposta. Rivista di Clinica Pediatrica, 78, 361. Costantino, D., Doglia, M., Bardare, M., and De Gaspari, G. (1973). Acrodermatite papulcsa infantile e antigeni associati all'epatite virale. Minerva Medica. (In the press.) Crosti, A., and Gianotti, F. (1964). Ulteriore contributo alla conoscenza dell'acrodermatite papulosa infantile. Giornale Italianio de Dermatologia, 105, 477. Dane, D. S., Cameron, C. H., and Briggs, M. (1970). Virus-like particles in serum of patients with Australia-antigen-associated hepatitis. Lancet, 1, 695. De Benedetti, L. (1969). Un caso di e)atite anitterica con acrodermatite papulosa di Crosti Gianotti. Minerva Pediatrica, 21, 1401. De Gaspari, G., Bardare, M., and Costantino, D. (1970). Au antigen in Crosti-Gianotti acrodermatitis. Lancet, 1, 1116. De Groote, J., Desmet, V. J., Gedigk, P., Korb, G., Popper, H., Poulsen, H., Scheuer, P. J., Schmid, M., Thaler, H., Uehlinger, E., and Welper, W. (1968). A classification of chronic hepatitis. Lancet, 2, 626. Despres, P., Pringuet, R., and Larregue, M., Basset, Mme., Watchi, J. M., and Seringe, P. (1969). Syndrome de Gianotti-Crosti: a propos d'un cas, contribution a l'etude etiopathogenique. Annales de Pediatrie, 16, 735. Duperrat, B., and Puissant, A. (1958). La dermatite eruptive ees extremites chez les enfants (syndrome de Gianotti-Crosti). Presse Medicale, 66, 1862. Eiloart, M. (1966). The Gianotti-Crosti syndrome. Report of forty-four cases. British Journal of Dermatology, 78, 488. Gianotti, F. (1955). Rilievi di una particolare casistica tossinfettiva caratterizzata da una eruzione eritemato-infiltrativa desquamativa a rocolai lenticolari, a sede elettiva acroesposta. Giornale Italiano di Dermatologia, 96, 678. Gianotti, F. (1966). L'epatite anitterica virale nell'acrodermatite papulosa infantile. Epatologia, 12, 171.
Papular acrodermatitis of childhood
Gianotti, F. (1970). The Australia antigen in infantile papular acrodermatitis. Proceedings of the 6th Meeting of the European Association for the Study of the Liver, 2-4 September, London, Communication 16. Gianotti, F. (1971). El antigeno Australia en la acrodermati'is papulosa infantil. Actas Dermo-sifiliogrdficas, 62, 227. Hjorth, N., Kopp, H., and Osmundsen, P. E. (1967). GianottiCrosti syndrome; papular eruption of infancy. Transactions of the St. john's Hospital Dermatological Society, 53, 46. Jean, G., Lambertenghi, G., and Gianotti, F. (1968). Ultrastructural aspects of lymph-nodes in infantile papular acrodermatitis. Observation of virus-like particles. Dermatologica, 136, 350. Jean, G., Lambertenghi, G., Gianotti, F., Travaglini, P., and Ranzi, T. (1967). L'Epatite Anitterica Nell'Acrodermatite Papulosa Infantile. Ganassini, Milano. Jean, G., Ranzi, T., and Lambertenghi, G. (1969). Phagocytic activity of peripheral mononuclear blood cells in lymphoreticular disease. Ultrastructural study. Haematologica Latina, 12, 1. Jenson, A. B., McCombs, R. M., Sakurada, N., and Melnick, J. L. (1970). Organ cultures inoculated with serum from a hepatitis patient with Au antigenemia. Experimental and Molecular Pathology, 13, 217. Jeune, M., Moulin, G., and Rosenberg, D. (1964). A propos d'un cas d'acrodermatite papuleuse infantile. Pediatrie, 19, 987. Nurse, D. S. (1967). Infantile lichenoid acrodermatitis. Medical J3ournal of Australia, 2, 1195. Pitsol-Aguade, J., and Mascaro, J. M. (1971). Dos casos de sindrome de Gianotti-Crosti con antigeno Australia positivo. Actas Dermo-sifiliogrdficas, 62, 93. Pomposiello, I. M., and Abulafia, J. (1968). Gianotti-Crosti syndrome. Archivos Argentinos de Dermatologia, 18, 113. Prince, A. M. (1968). Au antigen detected in the blood during an incubation period of serum hepatitis. Proceedings of the National Academy of Sciences of the U.S.A., 60, 814. Puissant, A., Mascaro, J. M., Fauchier, A., and Canet, J. (1966). Syndrome eruptif erythemato-vesiculo-papuleux simple localis6 aux extremites de Gianotti-Crosti. Annales de Dermatologie et de Syphiligraphie, 93, 279.
315.
799
Reich, H. (1963). Das Gianotti-Crosti Syndrom. Hautarzt, 14, Ricciardiello, P. T. (1969). Acrodermatite papulosa infantile accompagnata da epatite ed ittero. Giornale di Malattie Infettive e Parassitarie, 21, 213. Schirren, C. G., and Mutter, M. (1964). Die Akrodermatitis papulosa infantum (Gianotti-Crosti Syndrom) im differentialdiagnostischen Grenzgebiet von Dermatologie und Padiatrie. Monatsschrift furKinderheilkunde, 112, 65. Sirtori, C. (1970). Virus-like particles in infectious hepatitis.
Lancet, 2, 824. Stein, O., Fainaru, M., and Stein, Y. (1972). Visualization of virus-like particles in endoplasmic reticulum of hepatocytes of Australia antigen carriers. Laboratory Investigation, 26, 262. Stevanovic, D. V., and Sofronic, A. D. (1962). Gianotti-Crosti syndrome (subacute infective reticulo-endothelitis). Transactions of the St. J3ohn's Hospital Dermatological Society, 48, 83. Terao, T., and Takemura, T. (1971). Le syndrome de GianottiCrosti au Japon. Bulletin de la Societe Francaise de Dermatologie et de Syphiligraphie, 78, 116. Thiers, H., and Moulin, G. (1964). L'acrodermatite erythematopapuleuse infantile (syndrome de Gianotti-Crosti). A propos de deux observations. Journal de Medecine de Lyon, 45, 2173. Vulcan, P., Wolkonsky, A., and Nicolescu, F. (1965). Acrodermatita eritemapapuloasa infantila (sindromul GianottiCrosti). Consideratii privind doua cazuri clinice. DermatoVenerologia, 10, 309. Waisman, M., and Sutton, R. L. (1966). Frictional lichenoid eruption in children. Archives of Dermatology, 94, 592. Winkelmann, R. K., and Bourlond, A. (1965). Infantile lichenoid acrodermatitis. Report of a case of Gianotti-Crosti syndrome. Archives of Dermatology, 92, 398. Woerdeman, M. J. (1965). Acrodermatitis papulosa infantilis. Syndroom van Gianotti-Crosti. Nederlands Tijdschrift voor Geneeskunde, 109, 1472.
Correspondence to Professor F. Gianotti, Clinica Dermatologica, Universita di Milano, Via Pace 9, 20122 Milano, Italy.
You might also like
- Republic of The Philippines Tarlac State University College of Nursing Graduate Studies ProgramDocument9 pagesRepublic of The Philippines Tarlac State University College of Nursing Graduate Studies ProgramCorinthiaMaeMarceloNo ratings yet
- Erythema NodosumDocument42 pagesErythema Nodosummedpedshospitalist100% (1)
- J Clin Pathol 1980 Brook 1099 101Document4 pagesJ Clin Pathol 1980 Brook 1099 101ysh_girlNo ratings yet
- Thesis Jessica KattanDocument45 pagesThesis Jessica Kattanaztigan100% (2)
- Senin 20 Oktober 2014 - Parasit 1 - Parasitologi - Toxoplasma - 12Document32 pagesSenin 20 Oktober 2014 - Parasit 1 - Parasitologi - Toxoplasma - 12Zahra AstriantaniNo ratings yet
- An Unusual Case of Transient Neonatal Pustular Melanosis: A Diagnostic PuzzleDocument4 pagesAn Unusual Case of Transient Neonatal Pustular Melanosis: A Diagnostic PuzzlecebadawitNo ratings yet
- Q2 GPA Infectious Diseases IIDocument9 pagesQ2 GPA Infectious Diseases IIAdrian CaballesNo ratings yet
- FliktenDocument7 pagesFliktenAngga Maulana IbrahimNo ratings yet
- EN + EosinofiliaDocument3 pagesEN + EosinofiliaAna Flavia BaptistaNo ratings yet
- Practice: Kikuchi-Fujimoto Disease: Lymphadenopathy in SiblingsDocument4 pagesPractice: Kikuchi-Fujimoto Disease: Lymphadenopathy in SiblingsBobby Faisyal RakhmanNo ratings yet
- Auto Psi ADocument13 pagesAuto Psi AoscuracarlyNo ratings yet
- Estenosis Esofagica en LlaDocument3 pagesEstenosis Esofagica en LlaResidencia PediatriaNo ratings yet
- 2006 Gosche Vick SemPedSurgeryDocument8 pages2006 Gosche Vick SemPedSurgeryResya I. NoerNo ratings yet
- Cap Polyposis in Children: Case Report and Literature ReviewDocument6 pagesCap Polyposis in Children: Case Report and Literature ReviewLuis ArrietaNo ratings yet
- Immunological: Section of LaryngologyDocument3 pagesImmunological: Section of LaryngologymfhfhfNo ratings yet
- Elife 79397 v2Document21 pagesElife 79397 v2lata.pauccaraNo ratings yet
- A New Case Report of Severe MucopolysaccharidosisDocument7 pagesA New Case Report of Severe MucopolysaccharidosisKevin JebarajNo ratings yet
- UC Davis: Dermatology Online JournalDocument6 pagesUC Davis: Dermatology Online JournalSuryadi ProtokolcyinNo ratings yet
- Early - Stage Hodgkins Lymphoma in A Child A CaseDocument6 pagesEarly - Stage Hodgkins Lymphoma in A Child A CaseХарш Навнітбхаі НімаватNo ratings yet
- A Rare Localization of Tuberculosis of The Wrist: The Scapholunate JointDocument4 pagesA Rare Localization of Tuberculosis of The Wrist: The Scapholunate JointtaufikolingNo ratings yet
- Parakeratosis Variegata: A Possible Role of Environmental Hazards?Document4 pagesParakeratosis Variegata: A Possible Role of Environmental Hazards?Ega AihenaNo ratings yet
- 2 PBDocument4 pages2 PBPororo KewrenNo ratings yet
- Leptospira: Clinical ManifestationsDocument5 pagesLeptospira: Clinical ManifestationsTania Chintya Dewi KarimaNo ratings yet
- Hydatid Disease of Central Nervous System, A Clinicopathological Study of 33 CasesDocument5 pagesHydatid Disease of Central Nervous System, A Clinicopathological Study of 33 CasesIvory Arévalo ManríquezNo ratings yet
- Childhood PsioriasisDocument6 pagesChildhood PsioriasisYuliana DaisongNo ratings yet
- Kikuchi's Disease: Malathi Sathiyasekaran R. Varadharajan So. ShivbalanDocument3 pagesKikuchi's Disease: Malathi Sathiyasekaran R. Varadharajan So. Shivbalanzulfikar adiNo ratings yet
- Acute and Chronic InflammationDocument3 pagesAcute and Chronic InflammationNicole DumriqueNo ratings yet
- CMV - Cazuri CliniceDocument5 pagesCMV - Cazuri CliniceMinerva StanciuNo ratings yet
- Cutaneous Tuberculosis in China - A Multicentre Retrospective Study of Cases Diagnosed Between 1957 and 2013Document7 pagesCutaneous Tuberculosis in China - A Multicentre Retrospective Study of Cases Diagnosed Between 1957 and 2013NadaaFahmiShofiNo ratings yet
- Somorin SsDocument8 pagesSomorin SsChikezie OnwukweNo ratings yet
- Cytophagic Histiocytic Panniculitis, Hemophagocytic Lymphohistiocytosis and Undetermined Autoimmune Disorder: Reconciling The PuzzleDocument5 pagesCytophagic Histiocytic Panniculitis, Hemophagocytic Lymphohistiocytosis and Undetermined Autoimmune Disorder: Reconciling The PuzzleLe DungNo ratings yet
- Manouvrier Hanu1998Document5 pagesManouvrier Hanu1998wiamelfazikiNo ratings yet
- Arch Dis Child 1998 Ladhani 85 8Document5 pagesArch Dis Child 1998 Ladhani 85 8Dian Ayu Permata SandiNo ratings yet
- Seq Exercise: By: Dr. Mohammad Saad Abdul-MajidDocument27 pagesSeq Exercise: By: Dr. Mohammad Saad Abdul-MajidKalichandren ArumugamNo ratings yet
- Adult Still's Disease and Respiratory Failure in A 74 Year Old WomanDocument3 pagesAdult Still's Disease and Respiratory Failure in A 74 Year Old WomanEduardo Romero StéfaniNo ratings yet
- Microbiology - Inicet Nov 2022Document19 pagesMicrobiology - Inicet Nov 2022Kuldeep SinghNo ratings yet
- Toxoplasmosis Revisited: Sheela Mathew, MD, Infectious Diseases Department, GovernmentDocument11 pagesToxoplasmosis Revisited: Sheela Mathew, MD, Infectious Diseases Department, GovernmentMuhammad Afiq HusinNo ratings yet
- Primary Subacute Hematogenous Osteomyelitis in Children: A Clearer Bacteriological EtiologyDocument6 pagesPrimary Subacute Hematogenous Osteomyelitis in Children: A Clearer Bacteriological EtiologymiNo ratings yet
- Guillain-Barré Syndrome: History, Pathogenesis, Treatment, and Future DirectionsDocument7 pagesGuillain-Barré Syndrome: History, Pathogenesis, Treatment, and Future Directionslakshminivas PingaliNo ratings yet
- LeprosyDocument56 pagesLeprosyAnkit KumarNo ratings yet
- Infectious Mononucleosis: A Case ReportDocument3 pagesInfectious Mononucleosis: A Case ReportSerghei CojocariNo ratings yet
- Case Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureDocument6 pagesCase Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureIrsalinaHusnaAzwirNo ratings yet
- Diagnosis and Treatment Protocol For COVID-19 Patients: (Trial Version 8)Document32 pagesDiagnosis and Treatment Protocol For COVID-19 Patients: (Trial Version 8)Fernando Ruben Rivera CastilloNo ratings yet
- Primary Conjunctival Tuberculosis-2Document3 pagesPrimary Conjunctival Tuberculosis-2puutieNo ratings yet
- Nejmcpc 2201236Document11 pagesNejmcpc 2201236AbinashmishraNo ratings yet
- Zoon's Plasma Cell Balanitis Associated With Male Genital Lichen SclerosusDocument4 pagesZoon's Plasma Cell Balanitis Associated With Male Genital Lichen SclerosusMircea-Dan Apopei-RusuNo ratings yet
- Histoid Leprosy: A Case ReportDocument5 pagesHistoid Leprosy: A Case Reportsri karuniaNo ratings yet
- 1 s2.0 S003962571630090X MainDocument14 pages1 s2.0 S003962571630090X MainBenjamin NgNo ratings yet
- Neurological and Ocular FIP v3.pdf Versiunea 1Document11 pagesNeurological and Ocular FIP v3.pdf Versiunea 1monika.olvedi86No ratings yet
- Repeated Furunculosis in Adult Male With Abnormal Neutrophil ActivityDocument4 pagesRepeated Furunculosis in Adult Male With Abnormal Neutrophil ActivityAdrien RochaNo ratings yet
- Confirmed CoExistenceDocument5 pagesConfirmed CoExistencemytriciallorinNo ratings yet
- Lecture 13 - Medical Mycology - HistoplasmosisDocument18 pagesLecture 13 - Medical Mycology - Histoplasmosissinghak203akNo ratings yet
- Hashimoto-Pritzker Disease: Case ReportDocument3 pagesHashimoto-Pritzker Disease: Case ReportMaria MichielinNo ratings yet
- Prepared By: Ken Robin A. Canada, RMT, Mls AscpiDocument35 pagesPrepared By: Ken Robin A. Canada, RMT, Mls AscpiKen Robin CanadaNo ratings yet
- Kikuchi' S Disease of The Mesenteric Lymph Nodes Presenting As Acute AppendicitisDocument3 pagesKikuchi' S Disease of The Mesenteric Lymph Nodes Presenting As Acute AppendicitisZulfikar Adi GumawangNo ratings yet
- Li Ulin LBM 1 IPEDocument16 pagesLi Ulin LBM 1 IPEUlin NuhaNo ratings yet
- Atypical Hemolytic Uremic Syndrome in A Post-COVID-19 Child: Its Differential Diagnosis With COVID-19, Multisystemic Inflammatory Syndrome and OutcomeDocument8 pagesAtypical Hemolytic Uremic Syndrome in A Post-COVID-19 Child: Its Differential Diagnosis With COVID-19, Multisystemic Inflammatory Syndrome and OutcomeSandra77777777No ratings yet
- The Differential Diagnosis of Colitis in Endoscopic Biopsy SpecimensDocument11 pagesThe Differential Diagnosis of Colitis in Endoscopic Biopsy SpecimensDilan SNo ratings yet
- Lecture7 Medical Mycology - YeastsDocument32 pagesLecture7 Medical Mycology - YeastsKarthick AnbuNo ratings yet
- News - EN Radar Opus UpdateDocument2 pagesNews - EN Radar Opus UpdateghinsavitNo ratings yet
- Gianotti-Crosti Syndrome and Allergic Background: Clinical ReportDocument4 pagesGianotti-Crosti Syndrome and Allergic Background: Clinical ReportghinsavitNo ratings yet
- Non-Thyroid Thyroid: Drug and Induced Changes in Function TestsDocument3 pagesNon-Thyroid Thyroid: Drug and Induced Changes in Function TestsghinsavitNo ratings yet
- Vaccin AriDocument1 pageVaccin ArighinsavitNo ratings yet
- Respiratory ExaminationDocument2 pagesRespiratory ExaminationghinsavitNo ratings yet
- Inspection: James WightDocument2 pagesInspection: James WightghinsavitNo ratings yet
- Inspection: James WightDocument2 pagesInspection: James WightghinsavitNo ratings yet
- PART III: LEARNING OF KRIYA YOGA - PRACTICAL ASPECTS Author: Ennio NimisDocument86 pagesPART III: LEARNING OF KRIYA YOGA - PRACTICAL ASPECTS Author: Ennio NimisghinsavitNo ratings yet
- Inspection: Examination of The Cardiovascular SystemDocument2 pagesInspection: Examination of The Cardiovascular SystemghinsavitNo ratings yet
- Vaginismus BrochureDocument2 pagesVaginismus BrochureghinsavitNo ratings yet
- Oxytocin PDFDocument25 pagesOxytocin PDFghinsavitNo ratings yet
- Lecture 1-Mitosis & Meiosis Mitosis: Mitosis Cells Reproduce by Duplicating Their Contents and Dividing in TwoDocument6 pagesLecture 1-Mitosis & Meiosis Mitosis: Mitosis Cells Reproduce by Duplicating Their Contents and Dividing in TwoghinsavitNo ratings yet
- Cell DivisionDocument22 pagesCell DivisionghinsavitNo ratings yet
- SerotoninDocument6 pagesSerotoninghinsavitNo ratings yet
- PART II: SHARING THE KRIYA YOGA TECHNIQUES Author: Ennio NimisDocument65 pagesPART II: SHARING THE KRIYA YOGA TECHNIQUES Author: Ennio NimisghinsavitNo ratings yet