Professional Documents
Culture Documents
13hellman - Vasopressors
13hellman - Vasopressors
Uploaded by
Daniel YakubovichCopyright:
Available Formats
You might also like
- Internet Book of Critical Care (IBCC) : Rapid ReferenceDocument1 pageInternet Book of Critical Care (IBCC) : Rapid Referenceian porterNo ratings yet
- PCOL - Chapter 11 - Anti Hypertensive AgentsDocument3 pagesPCOL - Chapter 11 - Anti Hypertensive AgentsCharles BayogNo ratings yet
- Emergency Medications: Hamdan Al HarbiDocument7 pagesEmergency Medications: Hamdan Al Harbijohn72decNo ratings yet
- الادوية الفعالة وعائياDocument78 pagesالادوية الفعالة وعائياosamaNo ratings yet
- Cholinergic System: e CarbamatesDocument26 pagesCholinergic System: e CarbamatesAcai BoncaiNo ratings yet
- Adrenergic Agonists Drug Action Receptor Pharmacologic UseDocument1 pageAdrenergic Agonists Drug Action Receptor Pharmacologic Usesunshine151No ratings yet
- Pharmacology of Inotropes and VasopressorsDocument51 pagesPharmacology of Inotropes and VasopressorsApen Silaban100% (1)
- Antiadrenergic DrugsDocument19 pagesAntiadrenergic DrugsshivanshpandeNo ratings yet
- 6 AntiadrenergicDocument37 pages6 Antiadrenergicaljoury4936No ratings yet
- I No Trpe Sand Hypotensive AgentsDocument100 pagesI No Trpe Sand Hypotensive AgentsMorad SatariNo ratings yet
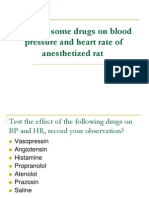
- Effect of Some Drugs On Blood Pressure and - PPT ManalDocument26 pagesEffect of Some Drugs On Blood Pressure and - PPT ManalMoonAIRNo ratings yet
- Drenergic AND Anti Adrenergic Drugs: Shabib AkhtarDocument21 pagesDrenergic AND Anti Adrenergic Drugs: Shabib AkhtarDeepa ShaiekhNo ratings yet
- Application of Drugs Acting On Autonomic Nervous System in HospitalsDocument58 pagesApplication of Drugs Acting On Autonomic Nervous System in HospitalsTama Fara ChiNo ratings yet
- Adrenergic & Antiadrenergic DrugsDocument54 pagesAdrenergic & Antiadrenergic DrugsUzma KhanNo ratings yet
- Adrenergic and Cholinergic (2017 - 11 - 01 22 - 03 - 49 UTC)Document2 pagesAdrenergic and Cholinergic (2017 - 11 - 01 22 - 03 - 49 UTC)Kimberly WhitesideNo ratings yet
- Vaso Pressors and InotropesDocument18 pagesVaso Pressors and InotropesBabu RamakrishnanNo ratings yet
- Drugs Acting On The Autonomic Nervous SystemDocument68 pagesDrugs Acting On The Autonomic Nervous SystemjisooNo ratings yet
- Pharmacology Chapter 42 zp-1-3Document42 pagesPharmacology Chapter 42 zp-1-3sho bartNo ratings yet
- SympathomimeticDocument56 pagesSympathomimeticvarish0% (1)
- Critical Care MedicationsDocument26 pagesCritical Care MedicationsSara HaniNo ratings yet
- CVS DiseasesDocument15 pagesCVS DiseasesNaavaNo ratings yet
- ICU PharmacologyDocument18 pagesICU PharmacologyIrsani FeniliaNo ratings yet
- LAS 4 Drugs For HypertensionDocument28 pagesLAS 4 Drugs For HypertensionMuhammad Haroon RazaNo ratings yet
- Drugs Receptor Therapeutic Effect Toxic Effect Time Durati OnDocument5 pagesDrugs Receptor Therapeutic Effect Toxic Effect Time Durati OnSharneeshriyaNo ratings yet
- Autonomic Nervous SystemDocument35 pagesAutonomic Nervous SystemAyat KhalilNo ratings yet
- Adrenergic and Anti-Adrenergic DrugsDocument54 pagesAdrenergic and Anti-Adrenergic DrugsChittaranjan Padhy100% (1)
- Adrenergic Blocking AgentsDocument3 pagesAdrenergic Blocking AgentsBern NerquitNo ratings yet
- Classdrugtherapyofshock 160310043509Document55 pagesClassdrugtherapyofshock 160310043509febr1sNo ratings yet
- Autonomic Nervous System: Chapter 16, 17, 18, 19, 20 Clinical Drug TherapyDocument84 pagesAutonomic Nervous System: Chapter 16, 17, 18, 19, 20 Clinical Drug TherapyMuhammad Rehan SarfrazNo ratings yet
- Pcol RevalidaDocument3 pagesPcol RevalidaNash IsmaelNo ratings yet
- Cardiac Medications: Mildred YarboroughDocument51 pagesCardiac Medications: Mildred YarboroughQueennitaNo ratings yet
- Goal 3 ANS - Expt Pharmacology - Dr. NikDocument18 pagesGoal 3 ANS - Expt Pharmacology - Dr. NikalexrishabNo ratings yet
- Farma - Antihipertensi Farmako NewDocument18 pagesFarma - Antihipertensi Farmako NewLucky Arie SandiNo ratings yet
- Adrenergic Drugs: S. Parasuraman, M.Pharm., PH.D.Document25 pagesAdrenergic Drugs: S. Parasuraman, M.Pharm., PH.D.Zakaria salimNo ratings yet
- HypertensionDocument39 pagesHypertensionapi-648595816No ratings yet
- Autonomic Nervous System AgentsDocument120 pagesAutonomic Nervous System Agentscoosa liquors100% (1)
- Cardiovascular Drugs: Dr. April Dawn R. LuceroDocument122 pagesCardiovascular Drugs: Dr. April Dawn R. LuceroRjDNo ratings yet
- Update: Review and Update On Inotropes and VasopressorsDocument9 pagesUpdate: Review and Update On Inotropes and VasopressorsMaryam JamilahNo ratings yet
- A.2 Category B and e Pharma ActDocument7 pagesA.2 Category B and e Pharma ActMichael Angelo CarballoNo ratings yet
- CVSDocument128 pagesCVSearldem1996No ratings yet
- Post Op Care PH Yogya-Ok - SipDocument29 pagesPost Op Care PH Yogya-Ok - SipTaufik KurniawanNo ratings yet
- Drugs Acting On The ANS: Clinical Pharmacist: Dr. Fatima Bani SalamaDocument144 pagesDrugs Acting On The ANS: Clinical Pharmacist: Dr. Fatima Bani SalamaNada AlhaririNo ratings yet
- Adrenergic DrugsDocument26 pagesAdrenergic DrugsManish ChoudharyNo ratings yet
- KHH - Hypertension in Surgical Operation Latest PPT FinalDocument37 pagesKHH - Hypertension in Surgical Operation Latest PPT FinalLearnerNo ratings yet
- 1 ER MedicationDocument89 pages1 ER MedicationAhmed Al-arapyNo ratings yet
- Antihypertensive Drugs: Loretta Walker, PH.DDocument11 pagesAntihypertensive Drugs: Loretta Walker, PH.DAdrian Jake LiuNo ratings yet
- The Use of Vasopressor and Inotropes in The Emergency Departement For The Treatment of ShockDocument36 pagesThe Use of Vasopressor and Inotropes in The Emergency Departement For The Treatment of ShockAndre Eka Putra PrakosaNo ratings yet
- ICU Pharmacology: Sean Forsythe M.D. Assistant Professor of MedicineDocument52 pagesICU Pharmacology: Sean Forsythe M.D. Assistant Professor of Medicinecoolboy1990No ratings yet
- Septic Shock: Francisco, Orlea ADocument13 pagesSeptic Shock: Francisco, Orlea AOrlea Francisco-SisioNo ratings yet
- ICU Pharmacology: Sedatives Analgesics Paralytics PressorsDocument51 pagesICU Pharmacology: Sedatives Analgesics Paralytics Pressorsdevi trismiaNo ratings yet
- Berapa Nilai Parameter Hemodinamik Utk. Diagnosis PH?Document58 pagesBerapa Nilai Parameter Hemodinamik Utk. Diagnosis PH?Anggara DwiputraNo ratings yet
- Pcol Part 2Document207 pagesPcol Part 2PB kate LocsonNo ratings yet
- Emergency Drugs in BriefDocument6 pagesEmergency Drugs in BriefBrian Dreamyeyes KendleyNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Baroreceptors and Therefore The Sympathetic SystemDocument5 pagesBaroreceptors and Therefore The Sympathetic SystemS GNo ratings yet
- Inotropes in PicuDocument2 pagesInotropes in PicuDijattxNo ratings yet
- Farmakologi Obat VasopresorDocument25 pagesFarmakologi Obat VasopresorNudyan BetharinaNo ratings yet
- P Harm Lab NotesDocument3 pagesP Harm Lab NotesaapjennNo ratings yet
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Chemical KineticsDocument69 pagesChemical KineticsDaniel YakubovichNo ratings yet
- Manual Copasi PDFDocument139 pagesManual Copasi PDFcirce5690No ratings yet
- Mukhopadhyay 1999Document6 pagesMukhopadhyay 1999Daniel YakubovichNo ratings yet
- Florio 1985Document7 pagesFlorio 1985Daniel YakubovichNo ratings yet
13hellman - Vasopressors
13hellman - Vasopressors
Uploaded by
Daniel YakubovichOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
13hellman - Vasopressors
13hellman - Vasopressors
Uploaded by
Daniel YakubovichCopyright:
Available Formats
Vasopressors
Vasopressors
Judith Hellman, M.D.
Judith Hellman, M.D.
Associate Professor
Associate Professor
Anesthesia and Perioperative Care
Anesthesia and Perioperative Care
University of California, San Francisco
University of California, San Francisco
Overview
Overview
Define shock states
Define shock states
Review drugs commonly used to treat hypotension
Review drugs commonly used to treat hypotension
Overview of drug management of shock states
Overview of drug management of shock states
Describe recent studies on pharmacologic management
Describe recent studies on pharmacologic management
of hypotension in septic shock
of hypotension in septic shock
VASST VASST - - Vasopressin versus Vasopressin versus Norepinephrine Norepinephrine for septic for septic
shock shock
European study European study - - Epinephrine Epinephrine vs Norepinephrine vs Norepinephrine + +
dobutamine dobutamine
Portuguese Study Portuguese Study - - Dopamine versus Dopamine versus Norepinephrine Norepinephrine
Shock States
Shock States
Cardiogenic
Cardiogenic
Hypovolemic
Hypovolemic
Obstructive
Obstructive
-
-
Impairment of normal
Impairment of normal
flow of blood
flow of blood
Obstruction of outflow Obstruction of outflow - - PE, pulmonary HTN, severe AS PE, pulmonary HTN, severe AS
Obstruction of inflow Obstruction of inflow - - Cardiac Cardiac tamponade tamponade, , pneumothorax pneumothorax
Medication effects
Medication effects
Neuraxial Neuraxial local anesthetics local anesthetics
Systemically active drugs Systemically active drugs
Distributive
Distributive
-
-
Low vascular tone, increased vascular
Low vascular tone, increased vascular
capacitance
capacitance
Sepsis and other systemic inflammatory processes Sepsis and other systemic inflammatory processes
Acute adrenal insufficiency Acute adrenal insufficiency
Neurogenic Neurogenic shock shock
Drugs Commonly Used to Treat
Drugs Commonly Used to Treat
Shock in ICUs
Shock in ICUs
Adrenergic Agents
Adrenergic Agents
Phenylephrine
Phenylephrine
Norepinephrine
Norepinephrine
Epinephrine
Epinephrine
Dopamine
Dopamine
Dobutamine
Dobutamine
Isoproterenol
Isoproterenol
Vasopressin
Vasopressin
1 2
+++
+++ ++ +
+++ +++ ++
++ ++ +
+ +++ +
+++ +++
Phenylephrine
Phenylephrine
Receptors:
Receptors:
Vascular effects:
Vascular effects:
Potent vasoconstrictor
Potent vasoconstrictor
Cardiac effects
Cardiac effects
-
-
Reflex
Reflex
Bradycardia Bradycardia
Decreased cardiac output Decreased cardiac output
Uses
Uses
Epidural and spinal anesthesia/analgesia Epidural and spinal anesthesia/analgesia
Vasodilation Vasodilation (autonomic instability, (autonomic instability, vasodilators) vasodilators)
To temporize while awaiting access for To temporize while awaiting access for other agents other agents
When agents with When agents with - -adrenergic activity cause tachycardia adrenergic activity cause tachycardia
Norepinephrine
Norepinephrine
Receptors:
Receptors:
and
and
1,
1,
minimal
minimal
2
2
-
-
>
>
Vascular effects:
Vascular effects:
Potent vasoconstrictor
Potent vasoconstrictor
Cardiac effects
Cardiac effects
Increased contractility
Increased contractility
Increased heart rate/tachycardia (variable)
Increased heart rate/tachycardia (variable)
Uses
Uses
Combined
Combined
vasodilation
vasodilation
and myocardial dysfunction
and myocardial dysfunction
Sepsis/SIRS
Sepsis/SIRS
Epinephrine
Epinephrine
Receptors:
Receptors:
and
and
-
-
=
=
Vascular effects:
Vascular effects:
Potent vasoconstrictor
Potent vasoconstrictor
Cardiac effects
Cardiac effects
More potent effect on contractility than More potent effect on contractility than norepinephrine norepinephrine
Increased heart rate/tachycardia Increased heart rate/tachycardia
Uses
Uses
When severe myocardial dysfunction is contributing to shock When severe myocardial dysfunction is contributing to shock
Cardiac arrest Cardiac arrest - - Can be given Can be given intra intra- -tracheally tracheally
Anaphylaxis Anaphylaxis
Potential Problems
Potential Problems
Reduced Reduced splanchnic splanchnic blood flow blood flow
Increased myocardial work load Increased myocardial work load ischemia, heart failure ischemia, heart failure
Dopamine
Dopamine
Receptors:
Receptors:
,
,
1>2,
1>2,
dopaminergic
dopaminergic
Vascular effects:
Vascular effects:
Vasoconstricts
Vasoconstricts
at higher doses
at higher doses
Cardiac effects
Cardiac effects
-
-
Lower doses
Lower doses
Increased cardiac output Increased cardiac output
Increased heart rate Increased heart rate
Uses
Uses
Shock from sepsis or other systemic inflammatory processes Shock from sepsis or other systemic inflammatory processes
To increase urine output (low dose, To increase urine output (low dose, dopaminergic dopaminergic effect) effect)
Potential problems
Potential problems
Dysrhythmias Dysrhythmias - - Atrial Atrial fibrillation, fibrillation, ST ST
Not a potent vasoconstrictor Not a potent vasoconstrictor - - often often need need additional additional pressors pressors
Dobutamine
Dobutamine
Receptors:
Receptors:
1>
1>
2
2
Cardiac
Cardiac
effects:
effects:
1
1
Increased cardiac output Increased cardiac output - - Strong Strong inotrope inotrope
Increased heart rate Increased heart rate
Vascular effects:
Vascular effects:
2,
2,
Vasodilation
Vasodilation
Effect on BP variable
Effect on BP variable
Uses
Uses
Cardiogenic Cardiogenic shock shock
Refractory shock from sepsis or other systemic inflammatory Refractory shock from sepsis or other systemic inflammatory
process process
Potential problems
Potential problems
Tachydysrhythmias Tachydysrhythmias
Hypotension can occur 2 Hypotension can occur 2 to to 2 effects 2 effects
Vasopressin
Vasopressin
Hormone with many effects: vascular, renal, endocrine
Hormone with many effects: vascular, renal, endocrine
Vascular
Vascular
Important role in BP regulation Important role in BP regulation
Variable vasoconstriction and Variable vasoconstriction and vasodilation vasodilation of vascular beds of vascular beds
Vasopressin levels are decreased in sepsis
Vasopressin levels are decreased in sepsis
Uses
Uses
Shock from sepsis and other inflammatory processes Shock from sepsis and other inflammatory processes - - Low dose Low dose
Peri Peri- -cardiopulmonary cardiopulmonary bypass bypass
Instead of Instead of epinephrine during epinephrine during cardiorespiratory cardiorespiratory arrest arrest
Hypotension due to ACE inhibitor Hypotension due to ACE inhibitor
Potential problems
Potential problems
Reduced GI blood flow, even at Reduced GI blood flow, even at low dose low dose
Cardiac ischemia Cardiac ischemia
Vasoactive
Vasoactive
Drug Management
Drug Management
of Shock States
of Shock States
Cardiogenic
Cardiogenic
Shock
Shock
Dobutamine
Dobutamine
Norephinephrine
Norephinephrine
Epinephrine
Epinephrine
Phosphdiesterase
Phosphdiesterase
inhibitors
inhibitors
-
-
Amrinone/milrinone
Amrinone/milrinone
Hypovolemic
Hypovolemic
Shock
Shock
Fluid resuscitation!!
Fluid resuscitation!!
Obstructive Forms of Shock
Obstructive Forms of Shock
Outflow problems
Outflow problems
-
-
PE,
PE,
Aortic
Aortic
coarctation
coarctation
, Aortic
, Aortic
stenosis
stenosis
, pulmonary HTN
, pulmonary HTN
Judicious fluids Judicious fluids
Inotropes Inotropes or mixed or mixed inotrope/vasoconstrictor inotrope/vasoconstrictor - - dobutamine dobutamine, ,
norepinephrine norepinephrine
Inflow problems
Inflow problems
-
-
Cardiac
Cardiac
tamponade
tamponade
,
,
pneumothorax
pneumothorax
Fluids Fluids
Relieve source Relieve source ( (pericardiocentesis pericardiocentesis, chest tube) , chest tube)
Medication
Medication
-
-
Induced Shock
Induced Shock
Pathophysiology
Pathophysiology
Vasodilation Vasodilation
Cardiac dysfunction Cardiac dysfunction
Neuraxial
Neuraxial
blockade
blockade
-
-
Phenylephrine
Phenylephrine
Systemic vasodilators
Systemic vasodilators
-
-
Phenylephrine
Phenylephrine
or
or
norepinephrine
norepinephrine
(depending on additional factors)
(depending on additional factors)
Cardiac depressants
Cardiac depressants
Inotrope Inotrope such as such as dobutamine dobutamine
Consider Consider norepinephrine norepinephrine if suspect concomitant if suspect concomitant vasodilation vasodilation
Shock Associated with Systemic
Shock Associated with Systemic
Inflammatory Process
Inflammatory Process
Shock Associated with Inflammation
Shock Associated with Inflammation
Agents used routinely to treat hypotension due to sepsis
Agents used routinely to treat hypotension due to sepsis
and other systemic inflammatory processes:
and other systemic inflammatory processes:
Norephinephrine Norephinephrine
Dopamine Dopamine
Vasopressin Vasopressin
Phenylephrine Phenylephrine
Dobutamine Dobutamine
Epinephrine Epinephrine
Physiology of
Physiology of
hypotension in systemic inflammatory
hypotension in systemic inflammatory
processes
processes
Decreased vascular tone Decreased vascular tone increased vascular capacitance increased vascular capacitance
Decreased myocardial contractility Decreased myocardial contractility
VASST Trial:
VASST Trial:
Vasopressin versus
Vasopressin versus
Norepinephrine
Norepinephrine
Hypothesis: Low dose vasopressin
Hypothesis: Low dose vasopressin
decrease mortality
decrease mortality
vs norepinephrine
vs norepinephrine
(NE) in septic shock
(NE) in septic shock
Inclusion criteria
Inclusion criteria
SIRS SIRS w/documented w/documented or suspected infection or suspected infection
NE at NE at 5 5 g/min g/min
New organ dysfunction New organ dysfunction
Interventions
Interventions
Vasopressin 0.01
Vasopressin 0.01
-
-
0.03U/min
0.03U/min
vs
vs
NE at 5
NE at 5
-
-
15
15 g/min g/min
Titrate other
Titrate other
pressor
pressor
(s) to
(s) to
achieve BP goals
achieve BP goals
Primary Endpoint: 28 day mortality
Primary Endpoint: 28 day mortality
NEJM 2008; 28;358(9):877 NEJM 2008; 28;358(9):877- -87 87
VASST: Results
VASST: Results
Subjects
Subjects
-
-
778 patients randomized
778 patients randomized
Vasopressin Vasopressin 396 396
NE 382 NE 382
Outcome
Outcome
Overall no reduction in 28d (Primary endpoint, P0.26) or 90d Overall no reduction in 28d (Primary endpoint, P0.26) or 90d
mortality (P 0.11) mortality (P 0.11)
No No significant differences in serious adverse events significant differences in serious adverse events
Subgroups Subgroups
More severe More severe NE > 15mcg/min NE > 15mcg/min Higher mortality in Higher mortality in
vasopressin group vasopressin group
Less severe Less severe NE 5 NE 5- -15 mcg/min 15 mcg/min - - Lower mortality at 28d Lower mortality at 28d
(P 0.05) (P 0.05)
Recommendations about Vasopressin
Recommendations about Vasopressin
Based on Available Data
Based on Available Data
Consider using vasopressin in:
Consider using vasopressin in:
Patients with septic shock that are on a mid Patients with septic shock that are on a mid- -range dose of range dose of
NE (5 NE (5- -15 mcg/min) 15 mcg/min)
Patients that develop Patients that develop tachydysrhythmias tachydysrhythmias on NE on NE
Patients that are extremely Patients that are extremely acidemic acidemic so won so won t respond as well t respond as well
to NE (vasopressin not inactivated by low pH) to NE (vasopressin not inactivated by low pH)
Patients on extremely high doses of NE Patients on extremely high doses of NE
ACLS ACLS as an alternative to epinephrine as an alternative to epinephrine
Peri Peri- -CPB CPB
European Trial: Epinephrine versus
European Trial: Epinephrine versus
Norepinephrine
Norepinephrine
+
+
Dobutamine
Dobutamine
Hypothesis:
Hypothesis: Epi Epi may be better than NE + may be better than NE + Dobutamine Dobutamine based based
on more on more activity activity
Study Design:
Study Design: Randomized Randomized trial of patients with septic shock trial of patients with septic shock
Subjects:
Subjects: 330 patients randomized 330 patients randomized
Epinephrine 161 Epinephrine 161
NE + NE + Dobutamine Dobutamine 169 169
Outcome
Outcome
Overall no reduction in 28d mortality (Primary endpoint, P Overall no reduction in 28d mortality (Primary endpoint, P
0.31) or other secondary endpoints 0.31) or other secondary endpoints
No No significant differences in serious adverse events significant differences in serious adverse events
Conclusions
Conclusions
No significant difference No significant difference
Lancet. 2007 Aug 25;370(9588):676-84
Dopamine:
Dopamine: Sepsis Occurrence in
Acutely Ill Patients (SOAP) Study
Hypothesis:
Hypothesis: DA worsens outcome in shock
Study Design: Observational study in 198 ICUs
Study Design: Observational study in 198 ICUs
Subjects: 1058 patients with shock; 462 patients with
Subjects: 1058 patients with shock; 462 patients with
septic shock
septic shock
NE: 80.2%; 31.8% received only NE NE: 80.2%; 31.8% received only NE
DA: 35.4%; 8.8% %; 8.8% received only DA received only DA
Epi: 23.3%; 4.5% only Epi: 23.3%; 4.5% only epi epi
Dobutamine Dobutamine + + catecholamines catecholamines 33.9% 33.9%
Outcome
Outcome
DA and epinephrine used more in non DA and epinephrine used more in non- -survivors survivors
DA DA an independent risk factor for mortality in patients with an independent risk factor for mortality in patients with
shock, and in the subcategory of patients with septic shock shock, and in the subcategory of patients with septic shock
Crit Care Med. 2006;34(3):589-97
Portuguese
Portuguese Community Acquired
Sepsis Study
:
:
Dopamine (DA)
Dopamine (DA)
vs
vs
NE
NE
Hypothesis:
Hypothesis:
Study Design:
Study Design: Multicenter Multicenter, observational study of patients with , observational study of patients with
community community- -acquired sepsis in 17 ICUs acquired sepsis in 17 ICUs
Subjects:
Subjects: 458 patients with septic shock 458 patients with septic shock
73% received NE 73% received NE
50.5% received DA 50.5% received DA
Outcome
Outcome
NE associated with worse outcome NE associated with worse outcome
NE independent risk factor for ICU mortality in septic shock NE independent risk factor for ICU mortality in septic shock
Crit Care Med. 2009;37(2):410-6
Surviving Sepsis Campaign:
Surviving Sepsis Campaign:
2008 Guidelines
2008 Guidelines
Vasopressors
NE and DA are the initial vasopressors of choice
Epinephrine, phenylephrine, or vasopressin should not be
administered as the initial vasopressor in septic shock
Vasopressin 0.03 units/min may be subsequently added to
NE
Use epinephrine as the first alternative agent in septic shock
when blood pressure is poorly responsive to NE or DA.
Do not use low-dose dopamine for renal protection
Inotropic therapy
Use dobutamine in patients with myocardial dysfunction
Crit Care Med. 2008 J an;36(1):296-327
Thank You!!
Gram-negative
Bacteria
Terlipressin
Terlipressin
Vasopressin analogue
Vasopressin analogue
Longer acting than vasopressin (half Longer acting than vasopressin (half- -life ~ 6 hours versus 6 life ~ 6 hours versus 6
minutes) minutes)
Widely used in
Widely used in
Europe
Europe
Undergoing Undergoing trials in US trials in US
Uses
Uses
Shock associated with sepsis and other systemic inflammatory Shock associated with sepsis and other systemic inflammatory
processes processes
Potential problems
Potential problems
Decreased cardiac output Decreased cardiac output
You might also like
- Internet Book of Critical Care (IBCC) : Rapid ReferenceDocument1 pageInternet Book of Critical Care (IBCC) : Rapid Referenceian porterNo ratings yet
- PCOL - Chapter 11 - Anti Hypertensive AgentsDocument3 pagesPCOL - Chapter 11 - Anti Hypertensive AgentsCharles BayogNo ratings yet
- Emergency Medications: Hamdan Al HarbiDocument7 pagesEmergency Medications: Hamdan Al Harbijohn72decNo ratings yet
- الادوية الفعالة وعائياDocument78 pagesالادوية الفعالة وعائياosamaNo ratings yet
- Cholinergic System: e CarbamatesDocument26 pagesCholinergic System: e CarbamatesAcai BoncaiNo ratings yet
- Adrenergic Agonists Drug Action Receptor Pharmacologic UseDocument1 pageAdrenergic Agonists Drug Action Receptor Pharmacologic Usesunshine151No ratings yet
- Pharmacology of Inotropes and VasopressorsDocument51 pagesPharmacology of Inotropes and VasopressorsApen Silaban100% (1)
- Antiadrenergic DrugsDocument19 pagesAntiadrenergic DrugsshivanshpandeNo ratings yet
- 6 AntiadrenergicDocument37 pages6 Antiadrenergicaljoury4936No ratings yet
- I No Trpe Sand Hypotensive AgentsDocument100 pagesI No Trpe Sand Hypotensive AgentsMorad SatariNo ratings yet
- Effect of Some Drugs On Blood Pressure and - PPT ManalDocument26 pagesEffect of Some Drugs On Blood Pressure and - PPT ManalMoonAIRNo ratings yet
- Drenergic AND Anti Adrenergic Drugs: Shabib AkhtarDocument21 pagesDrenergic AND Anti Adrenergic Drugs: Shabib AkhtarDeepa ShaiekhNo ratings yet
- Application of Drugs Acting On Autonomic Nervous System in HospitalsDocument58 pagesApplication of Drugs Acting On Autonomic Nervous System in HospitalsTama Fara ChiNo ratings yet
- Adrenergic & Antiadrenergic DrugsDocument54 pagesAdrenergic & Antiadrenergic DrugsUzma KhanNo ratings yet
- Adrenergic and Cholinergic (2017 - 11 - 01 22 - 03 - 49 UTC)Document2 pagesAdrenergic and Cholinergic (2017 - 11 - 01 22 - 03 - 49 UTC)Kimberly WhitesideNo ratings yet
- Vaso Pressors and InotropesDocument18 pagesVaso Pressors and InotropesBabu RamakrishnanNo ratings yet
- Drugs Acting On The Autonomic Nervous SystemDocument68 pagesDrugs Acting On The Autonomic Nervous SystemjisooNo ratings yet
- Pharmacology Chapter 42 zp-1-3Document42 pagesPharmacology Chapter 42 zp-1-3sho bartNo ratings yet
- SympathomimeticDocument56 pagesSympathomimeticvarish0% (1)
- Critical Care MedicationsDocument26 pagesCritical Care MedicationsSara HaniNo ratings yet
- CVS DiseasesDocument15 pagesCVS DiseasesNaavaNo ratings yet
- ICU PharmacologyDocument18 pagesICU PharmacologyIrsani FeniliaNo ratings yet
- LAS 4 Drugs For HypertensionDocument28 pagesLAS 4 Drugs For HypertensionMuhammad Haroon RazaNo ratings yet
- Drugs Receptor Therapeutic Effect Toxic Effect Time Durati OnDocument5 pagesDrugs Receptor Therapeutic Effect Toxic Effect Time Durati OnSharneeshriyaNo ratings yet
- Autonomic Nervous SystemDocument35 pagesAutonomic Nervous SystemAyat KhalilNo ratings yet
- Adrenergic and Anti-Adrenergic DrugsDocument54 pagesAdrenergic and Anti-Adrenergic DrugsChittaranjan Padhy100% (1)
- Adrenergic Blocking AgentsDocument3 pagesAdrenergic Blocking AgentsBern NerquitNo ratings yet
- Classdrugtherapyofshock 160310043509Document55 pagesClassdrugtherapyofshock 160310043509febr1sNo ratings yet
- Autonomic Nervous System: Chapter 16, 17, 18, 19, 20 Clinical Drug TherapyDocument84 pagesAutonomic Nervous System: Chapter 16, 17, 18, 19, 20 Clinical Drug TherapyMuhammad Rehan SarfrazNo ratings yet
- Pcol RevalidaDocument3 pagesPcol RevalidaNash IsmaelNo ratings yet
- Cardiac Medications: Mildred YarboroughDocument51 pagesCardiac Medications: Mildred YarboroughQueennitaNo ratings yet
- Goal 3 ANS - Expt Pharmacology - Dr. NikDocument18 pagesGoal 3 ANS - Expt Pharmacology - Dr. NikalexrishabNo ratings yet
- Farma - Antihipertensi Farmako NewDocument18 pagesFarma - Antihipertensi Farmako NewLucky Arie SandiNo ratings yet
- Adrenergic Drugs: S. Parasuraman, M.Pharm., PH.D.Document25 pagesAdrenergic Drugs: S. Parasuraman, M.Pharm., PH.D.Zakaria salimNo ratings yet
- HypertensionDocument39 pagesHypertensionapi-648595816No ratings yet
- Autonomic Nervous System AgentsDocument120 pagesAutonomic Nervous System Agentscoosa liquors100% (1)
- Cardiovascular Drugs: Dr. April Dawn R. LuceroDocument122 pagesCardiovascular Drugs: Dr. April Dawn R. LuceroRjDNo ratings yet
- Update: Review and Update On Inotropes and VasopressorsDocument9 pagesUpdate: Review and Update On Inotropes and VasopressorsMaryam JamilahNo ratings yet
- A.2 Category B and e Pharma ActDocument7 pagesA.2 Category B and e Pharma ActMichael Angelo CarballoNo ratings yet
- CVSDocument128 pagesCVSearldem1996No ratings yet
- Post Op Care PH Yogya-Ok - SipDocument29 pagesPost Op Care PH Yogya-Ok - SipTaufik KurniawanNo ratings yet
- Drugs Acting On The ANS: Clinical Pharmacist: Dr. Fatima Bani SalamaDocument144 pagesDrugs Acting On The ANS: Clinical Pharmacist: Dr. Fatima Bani SalamaNada AlhaririNo ratings yet
- Adrenergic DrugsDocument26 pagesAdrenergic DrugsManish ChoudharyNo ratings yet
- KHH - Hypertension in Surgical Operation Latest PPT FinalDocument37 pagesKHH - Hypertension in Surgical Operation Latest PPT FinalLearnerNo ratings yet
- 1 ER MedicationDocument89 pages1 ER MedicationAhmed Al-arapyNo ratings yet
- Antihypertensive Drugs: Loretta Walker, PH.DDocument11 pagesAntihypertensive Drugs: Loretta Walker, PH.DAdrian Jake LiuNo ratings yet
- The Use of Vasopressor and Inotropes in The Emergency Departement For The Treatment of ShockDocument36 pagesThe Use of Vasopressor and Inotropes in The Emergency Departement For The Treatment of ShockAndre Eka Putra PrakosaNo ratings yet
- ICU Pharmacology: Sean Forsythe M.D. Assistant Professor of MedicineDocument52 pagesICU Pharmacology: Sean Forsythe M.D. Assistant Professor of Medicinecoolboy1990No ratings yet
- Septic Shock: Francisco, Orlea ADocument13 pagesSeptic Shock: Francisco, Orlea AOrlea Francisco-SisioNo ratings yet
- ICU Pharmacology: Sedatives Analgesics Paralytics PressorsDocument51 pagesICU Pharmacology: Sedatives Analgesics Paralytics Pressorsdevi trismiaNo ratings yet
- Berapa Nilai Parameter Hemodinamik Utk. Diagnosis PH?Document58 pagesBerapa Nilai Parameter Hemodinamik Utk. Diagnosis PH?Anggara DwiputraNo ratings yet
- Pcol Part 2Document207 pagesPcol Part 2PB kate LocsonNo ratings yet
- Emergency Drugs in BriefDocument6 pagesEmergency Drugs in BriefBrian Dreamyeyes KendleyNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Baroreceptors and Therefore The Sympathetic SystemDocument5 pagesBaroreceptors and Therefore The Sympathetic SystemS GNo ratings yet
- Inotropes in PicuDocument2 pagesInotropes in PicuDijattxNo ratings yet
- Farmakologi Obat VasopresorDocument25 pagesFarmakologi Obat VasopresorNudyan BetharinaNo ratings yet
- P Harm Lab NotesDocument3 pagesP Harm Lab NotesaapjennNo ratings yet
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Chemical KineticsDocument69 pagesChemical KineticsDaniel YakubovichNo ratings yet
- Manual Copasi PDFDocument139 pagesManual Copasi PDFcirce5690No ratings yet
- Mukhopadhyay 1999Document6 pagesMukhopadhyay 1999Daniel YakubovichNo ratings yet
- Florio 1985Document7 pagesFlorio 1985Daniel YakubovichNo ratings yet