Professional Documents
Culture Documents
Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino Women
Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino Women
Uploaded by
otartil_nimanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino Women
Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino Women
Uploaded by
otartil_nimanCopyright:
Available Formats
Transcribers: Angala, M.H., Javier, K.A.
Page 1 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
TOPIC OUTLINE
I. Introduction
II. General Consideration for Vaccination
III. General Contraindication to Vaccination
IV. Recommended Vaccines
a. Tetanus-Diphtheria [td] and Tetanus-
Diphtheria-Pertussis [tdap]
Immunization
b. Human Papilloma Virus [HPV]
c. Varicella Virus
d. Measles, Mumps, and Rubella Viruses
[MMR]
e. Influenza Virus
f. Pneumococcal Virus
g. Hepatitis A Virus [HAV]
h. Hepatitis B Virus [HBV]
V. Appendix
a. Levels of Evidence and Grades of
Recommendation
INTRODUCTION
Recognizing that immunization is one of the most
effective primary health care services, and that there
is a need to fill a gap in such service for adolescent
and adults, the Philippine Obstetrics and Gynecology
Society Foundation, Inc. POGS, through its
immunization for Filipino women IFW task Force,
has embarked in 2006 on an advocacy to incorporate
vaccination on the practice of obstetrics and
gynecology. Thus immunization has been
incorporated in the curriculum of accredited agency
training programs, and subsequently into the
certification examinations of the Philippine Board of
Obstetrics and Gynecology PBOG. The IFW task force
has published three editions 2006, 2009, 2010 of the
recommendation on Immunization for Filipino
Women.
The creation of the clinical Practice Guideline on
Immunization for Filipino Women represents the
continuing efforts of POGS to fulfill its advocacy in
improving the health not only of women, but also the
health of their children and other members of their
families.
GENERAL CONSIDERATIONS FOR VACCINATION
1. Never administer vaccines in the buttock
2. Confirm completion of childhood (or more recent)
primary vaccines series for measles, mumps, rubella
(MMR) and Tetanus-Diphtheria (Td) before
initiating adult recommended vaccine schedules
3. Maintain vaccine administration record in patients
chart, including date, site and route of
administration, manufacturer and lot number of
vaccine.
4. Knowing the route of vaccine administration,
needle size, and vaccine storage and handling are
critical components of a quality, office-based
vaccine program
5. Simultaneous use of any vaccines is not
contraindicated
6. Antibiotic therapy or breastfeeding are not
contraindications to vaccination. Likewise, the
presence of a pregnant woman or
immunosuppressed person in the household is not
a reason to withhold an indicated vaccine to a
family member.
GENERAL CONTRAINDICATION TO VACCINATION
1. Severe allergy to vaccine components
2. Pregnancy (or if planning pregnancy within four
weeks) for live attenuated vaccines
3. Severe immune attenuation (for live attenuated
vaccines only) consultation with an infectious
disease specialist is advised
4. Moderate or severe acute illness
5. If a live attenuated vaccine is given simultaneously
with another vaccine, a four week separation
interval should be used between vaccinations
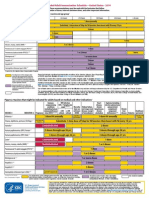
RECOMMENDED VACCINES
A. TETANUS-DIPHTHERIA (Td) AND TETANUS-
DIPHTHERIA-PERTUSSIS (Tdap) IMMUNIZATION
TARGET POPULATION
General Adults
All persons with zero, incomplete or unknown primary
series of tetanus immunization should receive a
primary series of Tetanus-Diphtheria immunization
All persons who have completed the primary series of
tetanus immunization should have booster Td
injections every 10 yrs
One dose of Tdap should substitute one Td booster
Td vaccine preferred over Tetanus Toxoid (TT)
because of additional protection against diphtheria.
Tetanus Toxoid
o should only be given a booster dose and should
not be part of a primary immunization series
o is preferred to the diphtheria-containing vaccines
only if there is a contraindication to the diphtheria
component
*all of the above - (Level I, Grade A)
Pregnant Women
with no previous tetanus immunization or unknown
tetanus immunization history should receive 3 doses
of Td vaccine to be give 1 month apart, starting 2
nd
trimester. Third dose can be given postpartum as
Tdap
whose last Td/Tdap vaccination was >10 yrs ago
should receive Td booster in the 2
nd
/3
rd
trimester of
pregnancy
*all of the above - (Level I, Grade A)
Persons more than 65 yrs old
Persons 65 yrs of age or older may be vaccinated with
Tdap
Persons 65 yrs of age or older who have close contact
with an infant <12 month old should be vaccinated
with Tdap (Level I, Grade A)
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO
WOMEN
SPECIAL TOPIC
1.05
JUNE 16, 2014
Transcribers: Angala, M.H., Javier, K.A. Page 2 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
DOSE REGIMEN
The primary tetanus immunization series
o consists of 3 Td injections given IM
o first 2 doses : given one month apart
o 3
rd
dose ; given 6-12 months after 2
nd
dose
o 3
rd
dose may be given as Tdap
Tdap dose is 0.5 ml, administered IM, preferably into
deltoid muscle
*all of the above - (Level I, Grade A)
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
Contraindication
Severe allergic reaction (e.g. anaphylaxis) after a
previous dose or to a vaccine component
Precaution
History of arthus-type hypersensitivity reactions
following a previous dose of TT-containing vaccine
Defer vaccination until at least 10 yrs have elapsed
since the last TT-containing vaccine
Adverse Events
Mild problems (noticeable, but did not interfere with
activities)
o Pain (up to about 8 in 10)
o Redness or swelling (up to about 1 in 3)
o Mild fever (up to about 1 in 15)
o Headache or tiredness (uncommon)
Moderate problems (interfered with activities, but did
not require medical attention)
o Fever over 102 F (rare)
o extensive swelling of the arm where the shot was
give (up to about 3 in 100)
Severe problem (unable to perform usual activities;
required medical attention)
o Swelling, severe pain, and redness in the arm
where the shot was given (rare)
AVAILABLE PREPARATIONS
Vaccine Formulation
Tetanus toxoid 0.5 ml/ampule
Tdap absorbed 0.5 ml/syringe
Tetanus-Diphtheria 0.5 ml/syringe
B. HUMAN PAPILLOMA VIRUS (HPV) IMMUNIZATION
TARGET POPULATION
Bivalent human papillomavirus (HPV) vaccination
o protect women aged 15-25 yrs from persistent
HPV infection and cervical intraepithelial
neoplasia (CIN) 2+;
o can be given to patients age 10-14 years and 26-55
years
o can protect target women from developing vulvar
intraepithelial neoplasia (VIN) & vaginal
intraepithelial neoplasia (VAIN);
o can protect target women from CIN 2+
associated with combined nonvaccine oncogenic
HPV types (HPV 33,45)
*all of the above - (Level I, Grade A)
Quadrivalent HPV vaccination
o protect women 16-45 yrs from persistent HPV
infection and cervical intraepithelial neoplasia
(CIN) 2+
o can be given to patients age 9-45 yrs
o protect women aged 9-45 yrs from developing
vulvar intraepithelial neoplasia (VIN) & vaginal
intraepithelial neoplasia (VEIN)
o can protect women aged 16-45 yrs from
developing anogenital warts
*all of the above - (Level I, Grade A)
HPV vaccination can be given in women with the
following special situations:
o Abnormal Papanicolaou (Pap) smear
o History of genital warts
o Breastfeeding
o Immunocompromised
*all of the above - (GPP)
Pap smear and HPV infection status are not a
prerequisite for HPV vaccination (GPP)
DOSE REGIMEN
Bivalent HPV vaccine
o Injected imtramuscularly at 0,1,6 months (Level I,
Grade A)
o Can be given concomitantly with diphtheria-
tetanus-acellular pertussis (dTpa), inactivated
poliovirus vaccine (IPV), Hepatitis A inactivated
caccine (HepA) and Hepatitis B inactivated vaccine
(HepB) (GPP)
Quadrivalent HPV vaccine
o Injected intramuscularly at 0,2,6 months
o Can be given concomitantly with diphtheria,
tetanus, pertussis, and poliomyelitis vaccine in
healthy adolescents 11-17 yrs of age
*all of the above - (Level I, Grade A)
Bivalent and quadrivalent HPV vaccines are not
interchangeable to complete the 3 doses.
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
HPV vaccines
o cannot be given to pregnant women
o can be given to women with minor acute illnesses
o should not be given to patients with a history of
adverse reactions to any vaccine component
Women who receive HPV vaccination should be
observed for syncope in the clinic for 15 min.
*all of the above - (GPP)
AVAILABLE PREPARATIONS
Vaccine Formulation
Bivalent HPV vaccine 0.5 ml/syringe
Quadrivalent HPV vaccine 0.5 ml/syringe
C. VARICELLA ZOSTER VIRUS IMMUNIZATION
TARGET POPULATION
Routine Vaccination
The following population groups with no evidence of
immunity to Varicella (reliable clinical history of
disease, Physician-documented vaccination) should
Transcribers: Angala, M.H., Javier, K.A. Page 3 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
routinely receive the Varicella vaccine (Level I, Grade
A):
o Persons aged > 13 yrs
o School-aged children, college students, and
students in other postsecondary educational
institutions
o Other healthy adults:
Health care professionals (HCP)
Household contacts of immunocompromised
persons
Persons who live or work in environments in
which transmission of Varicella zoster virus is
likely (e.g. teachers, day-care employees,
residents and staff in institutional settings)
Persons who live or work in environments in
which transmission has been reported (e.g.
college students, inmates, and staff members
of correctional institutions, and military
personnel)
Nonpregnant women of childbearing age
Adolescents and adults living in households
with children
International travelers
Postpartum Vaccination
Prenatal assessment of women for evidence of
Varicella immunity is recommended.
Upon completion or termination of their pregnancies,
women who do not have evidence of Varicella
immunity should receive the first dose of vaccine
before discharge from the health-care facility
Second dose should be administered 4-8 weeks later
Women should be counseled to avoid conception for
1 month after each dose of Varicella
DOSE REGIMEN
Eligible recipients should receive two 0.5 ml doses of
single-antigen Varicella vaccine administered
subcutaneously, 4-8 weeks apart
If >8 weeks elapsed after the 1
st
dose, the 2
nd
dose
may be administered without restarting the schedule
(Level I, Grade A)
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
Contraindications(Level I, Grade A)
who have a history of anaphylactic reaction to any
component of the vaccine
who have a history of anaphylactic reaction to
neomycin
who have any malignant condition, including blood
dyscrasias, leukemia, lymphomas of any type, or other
malignant neoplasms affecting the bone marrow or
lymphatic systems
who have a family history of congenital or hereditary
immunodeficiency in first-degree relatives (e.g.
parents and siblings) unless the immune competence
of the potential vaccine recipient has been clinically
substantiated or verified by a laboratory
persons receiving high-dose systemic
immunosuppressive therapy, including persons on
oral steroids >2mg/kg of body weight or a total
of >20mg/day of prednisone or equivalent for persons
who weigh >10kg, when administered for >2wks
pregnant women
Precautions
Vaccination of persons who have acute severe illness,
including untreated, active tuberculosis, should be
postponed until recovery. Tuberculin skin testing is
not a prerequisite for vaccination
Because of the potential inhibition of the response to
Varicella vaccination by passively transferred
antibodies, Varicella vaccines should not be
administered for the same intervals as measles
vaccine (3-11 months, depending on the dosage),
after administration of blood (except washed red
blood cells), plasma, or immunoglobulin (Ig).
Persons who received a Varicella vaccine should not
be administered an antibody-containing product for 2
weeks after vaccination unless the benefits exceed
those of vaccination
In such cases, the vaccine recipient should either be
revaccinated or tested for immunity at the
appropriate intervals, depending on the dose received,
and then revaccinated if seronegative
AVAILABLE PREPARATIONS
Vaccine Formulation
Varicella Virus Vaccine,
live-attenuated, freeze-
dried with separate
diluent, to be
reconstituted right before
administration
0.5 ml
D. MEASLES, MUMPS AND RUBELLA VIRUSES (MMR)
TARGET POPULATION
All non-pregnant women of childbearing age must be
offered measles, mumps, and rubella (MMR)
vaccination
Upon completion or termination of pregnancy,
women who do not have serologic evidence or rubella
immunity or documentation of rubella vaccination
should be vaccinated with MMR before discharge
from the hospital or birthing center
Routine prenatal serologic testing for rubella on all
pregnant women who lac acceptable evidence of
rubella immunity
*all of the above - (Level I, Grade A)
DOSE REGIMEN
0.5 ml, administered subcutaneously, 1-2 doses
2
nd
dose of MMR vaccine
o Administered 4 weeks after the first dose is
recommended for adults
o Indicated for individuals who :
Have been recently exposed to
measles/mumps or are in an outbreak setting
Have been vaccinated previously with killed
measles vaccine
Have been vaccinated with an unknown type of
measles vaccine during 1963-1967
Are students in postsecondary educational
institutions
Work in a health-care facility
Plan to travel internationally
Transcribers: Angala, M.H., Javier, K.A. Page 4 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
Contraindications
Severe allergic reaction after a previous dose of the
vaccine
Pregnancy
Severely immunocompromised patients
o Hematologic and solid tumors
o Receipt of chemotherapy
o Congenital immunodeficiency
o Long-term immunosuppressive therapy
o Patients with human immunodeficiency (HIV)
infection who are severely immunocompromised
Precaution
Women administered with MMR vaccine should be
advised not to get pregnant during the next 4 weeks
post-vaccination
Recent (11months) receipt of the antibody-
containing blood product (specific interval depends on
the product)
History of thrombocytopenia or thrombocytopenic
purpura
Need for tuberculin skin testing
Moderate or severe acute illness with or without
fever
STORAGE REQUIREMENTS
Vaccine
o Refrigerate immediately upon arrival
o Store at 35-46F (2-8C)
o Protect from light at all times, since such exposure
may inactivate the vaccine viruses
Diluent
o May be refrigerated or stored at room
temperature (68-77F [20-25C])
o Do not freeze or expose to freezing temperatures
After reconstitution, use immediately or store at 35-
46 F (2-8C) and protect from light. Discard if not
used within 8 hours of reconstitution
AVAILABLE PREPARATIONS
Vaccine Formulation
Measles, Mumps, Rubella
Virus Vaccine, live-
attenuated
0.5 ml
E. INFLUENZA VIRUS
TARGET POPULATION
All pregnant and breastfeeding women should receive
the inactivated flu vaccine. (Level I, Grade A).
Individuals belonging to the ff. high risk groups. (Level
I, Grade A).
o All children: 6-18y.o
o All persons: 50 years
o Other persons at risk for medical complications
from influenza, their household and close contacts.
o All health care professionals (HCP)
DOSE REGIMEN
Infants, children, adolescents: 6-18 years (refer to
Philippine Pediatric Society Guidelines)
Women 19 years old: IM, every year, as soon as the
newest/current WHO-recommended vaccine strains
become available. (Level III, GPP)
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
Contraindication
Severe allergic reactions (e.g anaphylaxis) after a
previous dose or to a vaccine component, including
egg protein.
Precaution
Guillan Barre Syndrome within 6 weeks of previous
dose of influenza vaccine.
Moderate or severe acute illness with or without
fever.
AVAILABLE PREPARATIONS
Vaccine Formulation
Inactivated Split-Influenza
Virus
0.5ml prefilled syringe
Inactivated Influenza Virus
Vaccine
0.25ml and 0.5ml prefilled
syringe
F. PNEUMOCOCCAL BACTERIA IMMUNIZATION
TARGET POPULATION
High-risk patients who have not received prior
immunization or whose prior vaccination status is
unknown.
o All persons >50 years old, particularly those living
in institutions
o Persons with certain underlying chronic medical
conditions
Chronic cardiovascular disease (e.g congestive
heart failure [CHF], cardiomyopathies)
Chronic pulmonary disease (e.g asthma,
chronic obstructive pulmonary disease [COPD],
bronchiectasis, pulmonary tuberculosis [PTB])
Sickle-cell disease
Diabetes mellitus
Alcoholism
Chronic liver disease
Cerebrospinal fluid or cochlear implants
Functional or anatomic asplenia
Immunocompromised persons 2yo:
o HIV infection or AIDS
o Leukemia, Hodgkins disease, lymphoma, multiple
myeloma, generalized malignancy
o Chronic renal failure
o Nephrotic syndrome
o Immunosuppressive chemotherapy, radiation
therapy
o Functional or anatomic asplenia
o Organ or bone marrow transplant recipients
Any adult 19-49 years old who is a smoker and has
asthma (Grade B)
Revaccination with pneumococcal polysaccharide
vaccine (PPSV) is recommended, at least 5 years after
the first dose particularly with ff population: (Grade A)
o 50-64 years old should be revaccinated if their
prior PPSV dose was given at least 5years prior
Transcribers: Angala, M.H., Javier, K.A. Page 5 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
o >65years who had a prior dose with a lapse of at
least 5years
o 2-49 years old with/ on: (Grade B)
Damaged spleen or asplenia
Sickle-cell disease
HIV infections or AIDS
Generalized malignancy, leukemia, lymphoma,
multiple myeloma
Nephritic syndrome
Organ or bone marrow transplant
Long-term steroid therapy, chemotherapy and
radiation therapy
Pregnant and breastfeeding women who are at high-
risk for invasive pneumococcal disease.
Preferably administered during the 2
nd
or 3
rd
trimester
of pregnancy as a general safety precaution.
Women at high-risk should be offered vaccination
before becoming pregnant.
o High-risk women include those with: (Grade B)
Chronic cardiovascular disease (e.g congestive
heart failure [CHF], cardiomyopathies)
Chronic pulmonary disease (e.g asthma,
chronic obstructive pulmonary disease [COPD],
bronchiectasis, pulmonary tuberculosis [PTB])
Sickle-cell disease
Diabetes mellitus/ gestational DM
Chronic liver disease
Cerebrospinal fluid leaks or cochlear implants
Functional or anatomic asplenia
Immunocompromised persons:
HIV infections or AIDS
Leukemia, Hodgkins disease, lymphoma,
multiple myeloma, generalized malignancy
Chronic renal failure, Nephrotic syndrome
Organ or bone marrow transplant recipients
DOSE REGIMEN
Single 0.5ml dose, IM or SQ injection
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
Contraindications/Precautions
Hypersensitivity to any component of the vaccine.
Epinephrine injection (1:1000) must be available
immediately in case of anaphylaxis
Severely compromised cardiovascular and/ or
pulmonary function (since a system reaction incurs
significant risks)
Children < 2years as safety and efficacy have not been
established for this group
Adverse Events
PPSV and pneumococcal conjugate vaccine (PCV) are
relatively safe vaccines. About 30-50% of patients who
received the PPSV had mild side effect such as local
erythema.
Serious allergic reactions with the PPSV are
uncommon. Among children who received the PCV,
10-20% developed local erythema, tenderness or
swelling and 11% had low-grade fever
AVAILABLE PREPARATIONS
PPSV is licensed for persons aged 2 years and
recommended for persons with certain underlying
medical conditions (including immunocompromised
individuals) and for all persons aged 60 years.
Vaccine Formulation
Pneumococcal 23-Valent
Polysaccharide Vaccine,
PPSV23
0.5 ml prefilled syringe
G. HEPATITIS A VIRUS (HAV)
TARGET POPULATION
Women
o >18yo with close contact with persons with
Hepatitis A, must be vaccinated. (Level I, Grade A)
o Travelling to working in countries with high or
intermediate prevalence of hepatitis a should be
vaccinated. (Level I, Grade A)
o Use street drugs are candidates for vaccination.
(Level I, Grade A)
o With chronic liver disease (including Hepatitis B
and C) should receive Hepatitis A vaccination.
(Level I, Grade A)
o Previously treated with clotting factor
concentrated should avail of hepatitis A
vaccination. (Level I, Grade A)
o With occupational risk including laboratory staff
should be vaccinated. (Level I, Grade A)
Post-exposure Prophylaxis
For susceptible healthy women up to age 40yrs,
single-antigen hepatitis A vaccine should be
administered as soon as possible for exposure.
Beyond age 40yrs, immune globulin (Ig) is preferred.
Vaccine can be used if Ig cannot be obtained.
DOSE REGIMEN
IM for 2 doses, 6-12mos apart, for lasting protection
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
Severe or life-threatening allergic reaction to a
previous dose of hepatitis A vaccine is an absolute
contraindication.
Severe or life-threatening allergic reaction to any
vaccine component contraindicates the
administration of hepatitis A vaccine.
Moderate or severe illness at the time of vaccination
may defer the scheduled administration.
Safety of the hepatitis A vaccine for pregnant has not
been determined.
The most commonly reported adverse following
hepatitis A vaccination is local reaction at the site of
injection.
AVAILABLE PREPARATIONS
Several preparations of Hepatitis A vaccine that
contain inactivated whole-viruses are currently
available.
Vaccine Formulation
Inactivated Hepatitis A
Vaccine
1 ml / vial
Combined inactivated
Hepatitis A & B Vaccine
1 ml prefilled syringe
Transcribers: Angala, M.H., Javier, K.A. Page 6 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
H. HEPATITIS B VIRUS (HBV) IMMUNIZATION
TARGET POPULATION
Given to the following target population. (Level I,
Grade A)
o Healthcare and public safety and security workers
who may have exposure to blood in the workplace
o Persons in training for allied health professions
o Hemodialysis patients and those receiving blood and
blood products including transplant candidates.
o Patients in early course of chronic liver diseases
o Sexually transmitted disease (STD) clinic clients
o Multiple sexual partners or prior STD
o Inmates in correctional facilities
o Clients and staff of institutions for developmental
disability
o Travelers to high endemic areas
o Overseas foreign workers
o Injection drug users
o Household contacts and sexual partners of Hepatitis
B virus carriers
Pregnant women who is otherwise eligible for it.
(Level III, Grade B)
All HBs-Ag negative pregnant women seeking STD
treatment who have not been previously vaccinated
should receive hepatitis B vaccination (Level III, Grade
B).
DOSE REGIMEN
IM in 3 doses at 0, 1, 6-12 months.
Accelerated schedule: 4 doses at 0, 1, 2, 12 months
Rapid schedule: 4 doses at 0, 7, 21 days and 12
months
CONTRAINDICATIONS/PRECAUTIONS/ADVERSE
EVENTS
severe allergic reaction to vaccine component or to a
prior dose of Hepatitis B vaccine is a contraindication
to further doses of the vaccine.
Persons with severe or moderate acute illness should
not be vaccinated until their condition improves.
Minor illnesses like upper respiratory tract infection
are not a contraindication to vaccination.
AVAILABLE PREPARATIONS
Vaccine Formulation
Recombinant Hepatitis B
Virus Vaccine
20 mcg / ml
5ml
APPENDIX
LEVELS OF EVIDENCE AND GRADES OF
RECOMMENDATION
LEVEL DEFINITION
I
Evidence obtained from at least one properly
randomized controlled trial
II-1
Evidence obtained from well-designated
controlled trials without randomization
II-2
Evidence obtained from well-designed cohort
or case-control analytic studies, preferably
from more than one center or research group.
II-3
Evidence obtained from multiple time series
with or without the intervention
III
Opinions of respected authorities, based on
clinical experience, descriptive studies and
case reports or reports of exter committees.
GRADE DEFINITION
A
There is good evidence to support the
recommendation of the practice in
immunization for Filipino women
B
There is a fair evidence to support the
recommendation of the practice in
immunization for Filipino women
C
There is insufficient evidence to recommend
for or against the inclusion of the practice in
immunization for Filipino women
D
There is a fair to support the
recommendation that the practice be
excluded in immunization for Filipino women.
E
There is a good office the recommendation
that the practice be excluded in immunization
for Filipino women
GPP
A good practice point (GPP) is a
recommendation for best practice based on
the experience of the Technical Working
Group.
Review Questions:
1. Vaccine administration record includes the
following except:
a. Date of purchase
b. site and route of administration,
c. manufacturer
d. Lot number of vaccine.
2. True regarding contraindications to Vaccines
includes the following except:
a. Pregnancy [for live attenuated vaccines]
b. Severe immune attenuation (for live
attenuated vaccines only)
c. Moderate acute illness
d. If a live attenuated vaccine is given
simultaneously with another vaccine, a five
week separation interval should be used
between vaccinations
3. Target population of pneumococcal vaccination
except:
a. adult smokers with asthma
b. All persons older than 50 yo.
c. Persons with sickle cell disease
d. Diabetic patients
4. Which of the following available preparations is
TRUE?
a. Inactivated influenza virus: 0.25ml and 0.5
ml prefilled syringe
b. Hepatitis A virus: 20mcg/ml, 5ml
c. Inactivated Split-influenza: 0.5ml prefilled
syringe
d. Inactivated Hepatitis B: 1ml/ vial
5. Given the following:
i. Bivalent HPV vaccination protects women aged
16-45 yrs from persistent HPV infection
j. HPV vaccination can be given to breastfeeding
women
k. Quadrivalent HPV vaccine can be given
intramuscularly at 0, 2, and 6 months
l. Bivalent HPV vaccine can be given with
Hepatitis A vaccine
m. HPV vaccines can be given to pregnant women
Transcribers: Angala, M.H., Javier, K.A. Page 7 of 7
CLINICAL PRACTICE GUIDELINES ON IMMUNIZATION FOR FILIPINO WOMEN
a. All of the statements are correct
b. Majority [3 out of 5] of the statements are
correct
c. All of the statements are incorrect
d. Majority [3 out of 5] of the statements are
incorrect
6. All of the following are injected intramuscularly
except:
a. MMR
b. Tdap
c. HAV
d. HBV
7. Level II-3 is defined as:
a. Evidence obtained from well-designated
controlled trials without randomization
b. Evidence obtained from at least one
properly randomized controlled trial
c. Evidence obtained from well-designed
cohort or case-control analytic studies
d. Evidence obtained from multiple time
series with the intervention
8. A grade given if there is good evidence to support
the recommendation of practice in immunization
for Filipino Women:
a. D
b. C
c. A
d. B
9. Women who received this vaccination should be
observed for syncope for 15 minutes:
a. HPV
b. HAV
c. HBV
d. MMR
10. Which of the following is TRUE?
a. Women administered with MMR vaccine
should be advised not to get pregnant
during the next 4 weeks pre-vaccination
b. Women administered with Influenza
vaccine should be advised not to get
pregnant during the next 4 weeks pre-
vaccination
c. Women administered with MMR should be
advised not to get pregnant during the
next 4 weeks post-vaccination
d. Women administered with Influenza
vaccine should be advised not to get
pregnant during the next 4 weeks post-
vaccination
Answers:
1. A
2. D
3. B
4. C
5. B [J, k and L are correct]
6. A
7. D
8. C
9. A
10. C
You might also like
- CPG Preterm Labor PDFDocument90 pagesCPG Preterm Labor PDFJeffrey Arboleda100% (3)
- CPG AbortionDocument40 pagesCPG AbortionKatharine Nerva75% (12)
- Tuberculosis in Infancy and Childhood 4th Ed (PPS)Document268 pagesTuberculosis in Infancy and Childhood 4th Ed (PPS)Jessica MarianoNo ratings yet
- CPG Prom 2019Document134 pagesCPG Prom 2019Tintalle100% (3)
- Hypertension in Pregnancy (Pogs-Cpg)Document55 pagesHypertension in Pregnancy (Pogs-Cpg)Philip Piolo Fuego67% (3)
- POGS CPG Abnormal Uterine BleedineDocument36 pagesPOGS CPG Abnormal Uterine Bleedinejandale57% (7)
- CPG POGS Cesarean SectionDocument65 pagesCPG POGS Cesarean SectionAngela Caguitla100% (4)
- PayslipDocument1 pagePayslipAshish Agarwal67% (3)
- Leptospirosis CPG 2019Document68 pagesLeptospirosis CPG 2019Batch 2024 Internal Medicine0% (1)
- PCOG CPG - Normal Labor and DeliveryDocument51 pagesPCOG CPG - Normal Labor and Deliveryquixoticdreamer90% (10)
- PROLOG: Patient Management in the Office, Eighth EditionFrom EverandPROLOG: Patient Management in the Office, Eighth EditionNo ratings yet
- POGS PB Dystocia Sept 2022Document6 pagesPOGS PB Dystocia Sept 2022John Piox Badiang100% (1)
- CPG Gestational Trophoblastic DiseasesDocument31 pagesCPG Gestational Trophoblastic DiseasesSMR50% (2)
- CPG-3rd Trimester Bleeding and Postpartum Hemorrage 2009Document107 pagesCPG-3rd Trimester Bleeding and Postpartum Hemorrage 2009lovelots1234100% (9)
- CPG-Abnormal Labor and Delivery 2009Document29 pagesCPG-Abnormal Labor and Delivery 2009lovelots123488% (8)
- Mcsi Description 1Document2 pagesMcsi Description 1esbat07100% (1)
- Clinical Practice Guidelines For The Obstetrician - GynecologistDocument79 pagesClinical Practice Guidelines For The Obstetrician - GynecologistAngela Caguitla67% (3)
- Sgop CPGDocument93 pagesSgop CPGjojolilimomo100% (2)
- CPG UrogynecologyDocument71 pagesCPG UrogynecologyDjurizzaBustamanteGadin100% (2)
- Sample Case ProtocolDocument6 pagesSample Case ProtocoljheyfteeNo ratings yet
- PSCM Guidelines For Clinical Practice PhilippinesDocument10 pagesPSCM Guidelines For Clinical Practice PhilippinesanthonyNo ratings yet
- Benign Prostatic Hyperplasia: Philippine Urological Association, IncDocument7 pagesBenign Prostatic Hyperplasia: Philippine Urological Association, Incsam_llamzon100% (2)
- GTDDocument56 pagesGTDRendy Adhitya PratamaNo ratings yet
- OB - Normal Labor and DeliveryDocument51 pagesOB - Normal Labor and DeliveryJosh Matthew Rosales33% (3)
- CPG On Dengue in Children 2017Document108 pagesCPG On Dengue in Children 2017Hannah LeiNo ratings yet
- 12 Friedmans Curve v2Document4 pages12 Friedmans Curve v2Jowi Sal100% (1)
- PEDIA Case 4.1. Dengue FeverDocument10 pagesPEDIA Case 4.1. Dengue Feverotartil_nimanNo ratings yet
- Tiny Tweaks James WedmoreDocument31 pagesTiny Tweaks James WedmoreErise Global100% (1)
- Hydrolysis of Nucleic AcidsDocument7 pagesHydrolysis of Nucleic Acidskeepersake81% (16)
- CPG On Immunization For WomenDocument28 pagesCPG On Immunization For WomenYnoli DiosomitoNo ratings yet
- Clinical Practice Guidelines Einc 2014Document52 pagesClinical Practice Guidelines Einc 2014dennisreveni100% (1)
- CPG Labor and Delivery 2015Document78 pagesCPG Labor and Delivery 2015TintalleNo ratings yet
- Sgop CPG 2008 FinalDocument105 pagesSgop CPG 2008 FinalVia Alip100% (2)
- Aub Pogs CPGDocument39 pagesAub Pogs CPGVenz Timothy Wesley LandichoNo ratings yet
- Philippine Obstetrical and Philippine Obstetrical and Gynecological Society (POGS), Foundation, Inc. Gynecological Society (POGS), Foundation, IncDocument51 pagesPhilippine Obstetrical and Philippine Obstetrical and Gynecological Society (POGS), Foundation, Inc. Gynecological Society (POGS), Foundation, IncJanna Janoras ŰNo ratings yet
- Do Cervical Cancer Screening Recommendations Differ Among Women at Different Age Groups?Document8 pagesDo Cervical Cancer Screening Recommendations Differ Among Women at Different Age Groups?Nico Angelo CopoNo ratings yet
- Two Up Cont CPG Intrapartum PDFDocument98 pagesTwo Up Cont CPG Intrapartum PDFjojolilimomoNo ratings yet
- SGOP 2008 (Guidelines On Management)Document87 pagesSGOP 2008 (Guidelines On Management)Via Alip100% (1)
- CPG DM PDFDocument110 pagesCPG DM PDFLisa KriestantoNo ratings yet
- 2022 Pogs Annual Convention SP Rev3 Final - CompressedDocument292 pages2022 Pogs Annual Convention SP Rev3 Final - CompressedKaye HernandezNo ratings yet
- CPG PSSTDDocument40 pagesCPG PSSTDotartil_niman100% (2)
- CPG Anemia Pogs 2009Document38 pagesCPG Anemia Pogs 2009Mark Cristopher JoaquinNo ratings yet
- CPG On Hypertension in PregnancyDocument91 pagesCPG On Hypertension in PregnancyRumelle Reyes100% (3)
- Planes and Diameters of The PelvisDocument32 pagesPlanes and Diameters of The PelvisRumelle ReyesNo ratings yet
- CPG Abnormal Labor and Delivery PDFDocument29 pagesCPG Abnormal Labor and Delivery PDFKarl Jimenez Separa100% (2)
- CPG PcapDocument25 pagesCPG PcapIreen PahangNo ratings yet
- PM PFC MatrixDocument4 pagesPM PFC MatrixFamed residentsNo ratings yet
- CC Silva - Rationalization 2022: # Rationale Answer: C. Contained in The Vestibule RationaleDocument34 pagesCC Silva - Rationalization 2022: # Rationale Answer: C. Contained in The Vestibule RationaleNicole Xyza JunsayNo ratings yet
- 8 Neonatal Sepsis 2019Document45 pages8 Neonatal Sepsis 2019Yan Zhen YuanNo ratings yet
- OBGYN Revalida Review 2019Document74 pagesOBGYN Revalida Review 2019anonymous100% (1)
- OB Gyne ReviewerDocument52 pagesOB Gyne ReviewerRaffy Lucmans100% (1)
- PDFDocument70 pagesPDFPaul Benjomin AgregadoNo ratings yet
- CPG Abortion PDFDocument35 pagesCPG Abortion PDFAlyssaJaneRabayaNo ratings yet
- Medical School Companion Obstetrics and Gynecology Practice Question BookFrom EverandMedical School Companion Obstetrics and Gynecology Practice Question BookNo ratings yet
- Stay Healthy, Stay On Top of Vaccinations: CDC Click Here For The CDC's Full Vaccination ChartDocument4 pagesStay Healthy, Stay On Top of Vaccinations: CDC Click Here For The CDC's Full Vaccination ChartcircularreasoningNo ratings yet
- Adult ScheduleDocument3 pagesAdult ScheduleerilarchiNo ratings yet
- Vaccination WomenDocument6 pagesVaccination WomenVaishakh ShyamNo ratings yet
- Immunization Review GPDocument46 pagesImmunization Review GPKishore ChandkiNo ratings yet
- Recent Advances in ImmunizationDocument50 pagesRecent Advances in ImmunizationHassaan E MuhammadNo ratings yet
- Adult ScheduleDocument3 pagesAdult SchedulelcmurilloNo ratings yet
- Immunizations in PregnancyDocument47 pagesImmunizations in Pregnancymiss_izzniNo ratings yet
- Adult Schedule 11x17Document2 pagesAdult Schedule 11x17lcmurilloNo ratings yet
- Module 1 - Diseases and VaccinesDocument102 pagesModule 1 - Diseases and VaccinesElvin Ryan PlantillaNo ratings yet
- HPV Sbi 2023Document22 pagesHPV Sbi 2023Rose Andrea BergonioNo ratings yet
- Assessment Checklist - CASE PRESENTATIONSDocument7 pagesAssessment Checklist - CASE PRESENTATIONSotartil_nimanNo ratings yet
- Enable-Disable InternetDocument1 pageEnable-Disable Internetotartil_nimanNo ratings yet
- CPG PSSTDDocument40 pagesCPG PSSTDotartil_niman100% (2)
- Placenta PreviaDocument36 pagesPlacenta Previaotartil_nimanNo ratings yet
- Clinical Practice Guidelines. 224.00. in The Approach and Treatment of Urinary Tract Infection in Children in TheDocument1 pageClinical Practice Guidelines. 224.00. in The Approach and Treatment of Urinary Tract Infection in Children in Theotartil_nimanNo ratings yet
- Clinical Practice Guidelines. 224.00. in The Approach and Treatment of Urinary Tract Infection in Children in TheDocument1 pageClinical Practice Guidelines. 224.00. in The Approach and Treatment of Urinary Tract Infection in Children in Theotartil_nimanNo ratings yet
- CPG For UTIDocument1 pageCPG For UTIotartil_nimanNo ratings yet
- PEDIA Case 3.1. Acute BronchiolitisDocument75 pagesPEDIA Case 3.1. Acute Bronchiolitisotartil_nimanNo ratings yet
- Kulang 2Document1 pageKulang 2otartil_nimanNo ratings yet
- API BasicsDocument6 pagesAPI BasicsSrinivas BathulaNo ratings yet
- Z19 Tnoo 000517 PDFDocument1 pageZ19 Tnoo 000517 PDFGuna RajNo ratings yet
- World's No.1 LCD/LED Solution Designer World's Leading Interactive & Collaboration Solution BrandDocument3 pagesWorld's No.1 LCD/LED Solution Designer World's Leading Interactive & Collaboration Solution BrandINTELL WAVESNo ratings yet
- Tic EbookDocument215 pagesTic EbookTaju Deen100% (1)
- Cell Theory Refers To The Idea That: MicrographiaDocument5 pagesCell Theory Refers To The Idea That: MicrographiadeltasixNo ratings yet
- (Human Behavior and Environment 8) Carol M. Werner, Irwin Altman, Diana Oxley (Auth.), Irwin Altman, Carol M. Werner (Eds.) - Home Environments-Springer US (1985)Document355 pages(Human Behavior and Environment 8) Carol M. Werner, Irwin Altman, Diana Oxley (Auth.), Irwin Altman, Carol M. Werner (Eds.) - Home Environments-Springer US (1985)Carlos Roberto JúniorNo ratings yet
- Soc TB 25 May 2017Document37 pagesSoc TB 25 May 2017Ipie BsaNo ratings yet
- Jamboree GRE StudyPlan PDFDocument3 pagesJamboree GRE StudyPlan PDFMd Minhaj Ahmed AhmedNo ratings yet
- Front Office Section-ReceptionDocument33 pagesFront Office Section-ReceptionRishina CabilloNo ratings yet
- Western Mindanao State University College of Engineering-College Student Council Acknowledgement Form and Waiver of Fees For 1 SemesterDocument4 pagesWestern Mindanao State University College of Engineering-College Student Council Acknowledgement Form and Waiver of Fees For 1 SemesterMaria Julia DenustaNo ratings yet
- Moxa PT g7728 Series Manual v1.4Document128 pagesMoxa PT g7728 Series Manual v1.4Walter Oluoch OtienoNo ratings yet
- J.the Reproduction and Husbandry of The Water Monitor Varanus Salvator at The Gladys Porter Zoo, BrownsvilleDocument7 pagesJ.the Reproduction and Husbandry of The Water Monitor Varanus Salvator at The Gladys Porter Zoo, BrownsvilleAhmad MigifatoniNo ratings yet
- Uji Chi SquareDocument5 pagesUji Chi Squareeldiya yuliSNo ratings yet
- The First Vertebrates, Jawless Fishes, The Agnathans: 2.1 OstracodermsDocument22 pagesThe First Vertebrates, Jawless Fishes, The Agnathans: 2.1 OstracodermsAlejandro Tepoz TelloNo ratings yet
- Christmas Vigil MassDocument106 pagesChristmas Vigil MassMary JosephNo ratings yet
- Bamboo Annals RevisitedDocument14 pagesBamboo Annals RevisitedsreelidNo ratings yet
- Philippine Air Force CAS Aircraft Bidding DocumentsDocument151 pagesPhilippine Air Force CAS Aircraft Bidding DocumentsfuccioniNo ratings yet
- Ozone Therapy Is Safest Known TherapyDocument35 pagesOzone Therapy Is Safest Known Therapyherdin2008100% (1)
- Chapter 6Document18 pagesChapter 6Lydelle Mae CabaltejaNo ratings yet
- Ai PresentationDocument13 pagesAi Presentationapi-534191655No ratings yet
- Statement of PurposeDocument3 pagesStatement of PurposeehsanNo ratings yet
- The Little Book of Breaks 1840241519 PDFDocument61 pagesThe Little Book of Breaks 1840241519 PDFksrbhaskarNo ratings yet
- Japanese Quality Tools and TechniquesDocument36 pagesJapanese Quality Tools and TechniquesNab JiNo ratings yet
- Flexural Test of Concrete Beam SpecimenDocument6 pagesFlexural Test of Concrete Beam SpecimenJenevive TumacderNo ratings yet
- Gen Studs and Engg AptiDocument1 pageGen Studs and Engg AptiasishNo ratings yet
- Gcrouch@wsu - Edu Rmancini@wsu - Edu Andreakl@wsu - Edu: Groups/chem.345Document5 pagesGcrouch@wsu - Edu Rmancini@wsu - Edu Andreakl@wsu - Edu: Groups/chem.345Daniel McDermottNo ratings yet
- Shareholder Value Analysis FrameworkDocument9 pagesShareholder Value Analysis Frameworkashish.the7353No ratings yet