Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
220 viewsAngelam - Database Assessment 2
Angelam - Database Assessment 2
Uploaded by
api-257604563Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Stretchies - Lunch Box Business Plan FinalDocument24 pagesThe Stretchies - Lunch Box Business Plan Finalapi-25760456397% (36)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Pre-NEET Surgery (Khandelwal & Arora) PDFDocument124 pagesPre-NEET Surgery (Khandelwal & Arora) PDFdrng4850% (4)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Cancer Hiv Urine Therapy 44 PDFDocument24 pagesCancer Hiv Urine Therapy 44 PDFAvi G. Ujawane100% (2)
- Angelam-Nutassndiscussion Reviewed-2Document2 pagesAngelam-Nutassndiscussion Reviewed-2api-257604563No ratings yet
- Angelam Chapter4leadershipDocument4 pagesAngelam Chapter4leadershipapi-257604563100% (1)
- Angelam Leadershipch7Document4 pagesAngelam Leadershipch7api-257604563No ratings yet
- Meal Rounds ReportDocument2 pagesMeal Rounds Reportapi-257604563No ratings yet
- Tray AssessmentDocument6 pagesTray Assessmentapi-257604563100% (1)
- Angelam - LTC Case StudiesDocument6 pagesAngelam - LTC Case Studiesapi-257604563No ratings yet
- Angelam - Sodexo Blog PostDocument2 pagesAngelam - Sodexo Blog Postapi-257604563No ratings yet
- Which of The Following Assessment Findings Would Help Confirm A Diagnosis of AsthmaDocument79 pagesWhich of The Following Assessment Findings Would Help Confirm A Diagnosis of Asthmaluiz ManieboNo ratings yet
- Neutrophil To Lymphocyte Ratio (NLR) As An Indicator of Poor Prognosis in Stage IV Non-Small Cell Lung CancerDocument6 pagesNeutrophil To Lymphocyte Ratio (NLR) As An Indicator of Poor Prognosis in Stage IV Non-Small Cell Lung CancerWilliamRayCassidyNo ratings yet
- 2017 PCHRD Completed and Ongoing ProjectsDocument10 pages2017 PCHRD Completed and Ongoing ProjectsInna HusniaNo ratings yet
- 1 s2.0 S0006295223002642 MainDocument15 pages1 s2.0 S0006295223002642 Main吴善统No ratings yet
- Colorectal Cancer: What Is Colorectal Carcinoma?Document4 pagesColorectal Cancer: What Is Colorectal Carcinoma?Ryana Fitriana IINo ratings yet
- Mcqs Mock Exams For General Surgery Board ExamDocument5 pagesMcqs Mock Exams For General Surgery Board ExamMoiz AhmedNo ratings yet
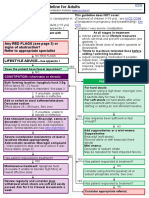
- Laxative Treatment Guideline For AdultsDocument7 pagesLaxative Treatment Guideline For AdultsPurim KTshipNo ratings yet
- GL Principles and Practice of PET-CT Part 1Document101 pagesGL Principles and Practice of PET-CT Part 1Victoria Lopez RodriguezNo ratings yet
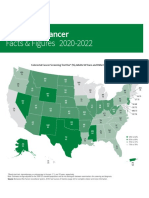
- Colorectal Cancer Facts and Figures 2020 2022 PDFDocument48 pagesColorectal Cancer Facts and Figures 2020 2022 PDFm_manuela2002No ratings yet
- Calprotectin LactoferrinDocument16 pagesCalprotectin LactoferrinCristian LaraNo ratings yet
- Kolorektal & Anus: Dr. Yusmaidi, SP.BDocument104 pagesKolorektal & Anus: Dr. Yusmaidi, SP.BAsmorowatiNo ratings yet
- Group 1 CHN OrlandoDocument56 pagesGroup 1 CHN OrlandocabalidarealynNo ratings yet
- A 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaDocument5 pagesA 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaYUSUF MUSANo ratings yet
- NCM 112 MS CA 3.3 Colorectal CancerDocument4 pagesNCM 112 MS CA 3.3 Colorectal CancerCherry Añonuevo RañesesNo ratings yet
- Sample NCLEX Questions With RationaleDocument26 pagesSample NCLEX Questions With RationaleSalanio JinalineNo ratings yet
- Im Irritable Bowel Syndrome Intestinal Obstruction Acute Appendicitis Lecture TransDocument6 pagesIm Irritable Bowel Syndrome Intestinal Obstruction Acute Appendicitis Lecture TransMelissa LabadorNo ratings yet
- Gastroenterology by Elagouri MohammedDocument31 pagesGastroenterology by Elagouri MohammedStylesh GuRlyNo ratings yet
- Practice Guidelines For Tumor Marker Use in The Clinic: Catharine SturgeonDocument9 pagesPractice Guidelines For Tumor Marker Use in The Clinic: Catharine SturgeonYder AtrupNo ratings yet
- Clinicopathological Staging For Colorectal CancerDocument20 pagesClinicopathological Staging For Colorectal Cancertr0xanNo ratings yet
- Selected-Handbook-Case ArimgsasDocument62 pagesSelected-Handbook-Case ArimgsasGabriela ChristianNo ratings yet
- Diabetes and Cancer: A Consensus ReportDocument12 pagesDiabetes and Cancer: A Consensus ReportDeekay06No ratings yet
- Article. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Document8 pagesArticle. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Trí Cương NguyễnNo ratings yet
- 2011 SLE 1st BankDocument222 pages2011 SLE 1st BankEmad Hajali100% (1)
- Colonoscopy Categorisation Guidelines 2017Document2 pagesColonoscopy Categorisation Guidelines 2017ScribboddNo ratings yet
- Eras GynDocument6 pagesEras GynFirah Triple'sNo ratings yet
- DYHFS10 Cancer Prevention Mar 2005Document2 pagesDYHFS10 Cancer Prevention Mar 2005Ngaire TaylorNo ratings yet
- Faktor-Faktor Yang Berhubungan Dengan Terjadinya Maserasi Stoma Pada Pasien Yang Terpasang Kolostomi Di Rsup DR Wahidin Sudirohusodo MakassarDocument8 pagesFaktor-Faktor Yang Berhubungan Dengan Terjadinya Maserasi Stoma Pada Pasien Yang Terpasang Kolostomi Di Rsup DR Wahidin Sudirohusodo MakassarNovia Swanda SinagaNo ratings yet
- Cancer Plan After 1 YrDocument46 pagesCancer Plan After 1 YrShirley SpenceNo ratings yet
Angelam - Database Assessment 2
Angelam - Database Assessment 2
Uploaded by
api-2576045630 ratings0% found this document useful (0 votes)
220 views9 pagesOriginal Title
angelam - database assessment 2
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
220 views9 pagesAngelam - Database Assessment 2
Angelam - Database Assessment 2
Uploaded by
api-257604563Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 9
Nutrition Database
Intern Name Angela Misko
Patient Initials H, P DOB 10/18/40 Age 73 Sex F Unit/Room# 1029
Admit Date 11/09/13 Admitting Diagnosis Vomiting X 4hrs, Gassy
Prior Medical History Colon caner with colon resection, HTN
Diet Order Low Fat Supplements None
If applicable, describe food intake since admission or past 5 days Poor PO intake. Not having any protein foods.
Any Food Allergies / Intolerances? None.
Height (in inches and cm) 56 Weight (in pounds and kg) 151lbs. (68kg) Weight History Loss
Gain
if weight , how much in what time frame? Was loss/gain intentional or unintentional? Unintentional
Usual Body Weight (UBW) Ideal Body Weight (IBW) 130 % IBW 116 % BMI 24.3
Social History (occupation, marital status, support system at home, alcohol use, who prepares meal, food secure / insecure, etc.)
Retired, Buddhist.
Pertinent Medications (list medications, state what they are used for, and if applicable nutritional implications)
Drug name(s) Indication Nutritional Implication
Morphine Sulfate
(Pain meds)
Pain. Take with food. May cause taste
changes and constipation.
Famotidine
(Pepcid)
Stomach ulcers, GERD, over-
production of stomach acid
Bland diet may be
recommended. Limit caffeine.
Loperamide + Simethicone
(Maalox)
Diarrhea +
Gas
Diarrhea may increase fluid and
electrolyte needs. +
Avoid carbonated beverages
and gas-forming foods to
prevent flatulence.
IVFs Dehydration Fluid requirements may be
slightly decreased since they are
receiving IV fluids on top of diet.
Fe Sucrose
Ondansetron
(Zofran)
Prevent nausea and vomiting
Nutrition Database
Nutrition related laboratory values
Lab Test
Lab value indicate if
abnormal
high or low ( or )
Nutritional significance if abnormal
Can a nutrition intervention help to correct this abnormal lab value? How?
Na
138
K
3.6
BUN
106
CREAT
0.81
Albumin
2.7 low
Additional protein supplement to aid in wound healing.
Prealb
--
Glucose
97
HgbA1C
H/H
MCV
MCH
Iron (Fe)
Transferrin Sat (%)
Ferritin
Vitamin B
12
Folate
Ca
Phos
Mg
Is Patients Skin Intact? Yes No
If no, Surgical Wound Decubitus Ulcer
If decubitus ulcer, list stage (I-IV) and site(s)
Is decubitus ulcer Improving? Getting worse?
Nutrition Database
Is any of the following present? Nausea Vomiting Diarrhea Constipation
Difficulty Chewing Difficulty Swallowing
Unable to feed self Malabsorption Early Satiety Taste Changes
Reminder.for calculations, what was the patients height (cm) and weight (kg) again? 168 cm 68 kg
Male Female Age 73
Any stress factors, activity factors to consider? Colon Cancer and Colon Resection
Calculate Energy Needs using
1) Harris-Benedict ------------------------------------ 2100-2300 kcal
2) Mifflin St. Jeor -------------------------------------- 1200-1400 kcal
3) kcal/kg ----------------------------------------------- 1700-2000 kcal
4) Ireton Jones (only use in critically ill) ------- kcal
5) Penn State 2010 equation ---------------------- kcal
What formula did you ultimately use for the Pt & why? Kcal/kg per hospital protocol
Show your work for three of the five methods above used:
1) Harris-Benedict
BMR= 655.1 + 9.56(68kg) + 1.7(168cm) 4.7(73y.o)
BMR= 655.1 + 650 + 285.6 343.1
BMR= 1247.6
Activity Factor= 1.2 (ambulatory)
Stress Factor= 1.5 (s/p surgery)
BMR= 1247.6 x 1.2 x 1.5
BMR= 2244 Range: 2100-2300 kcal
2) Mifflin St. Jeor
RMR= (9.99 x 68kg) + (6.25 x 168cm) (4.92 x 73) 161
RMR= (679) + (1050) (359) (161)
RMR= 1209 Range: 1200-1400 kcal
Nutrition Database
3) Kcal/kg
68kg x (25kcal) = 1700kcal
68kg x (30kcal) = 2040kcal
Range: 1700-2000kcal
Calculate Protein Needs
How many g/kg would you use & why? 1.3-1.7 is a good range due to the increased needs from the patients colon
resection.
Show your work:
68kg x 1.3g = 88.4g
68kg x 1.7g = 115.6g
88-115 g/day
Calculate Fluid Needs using
1) ml/kg depending on age ----------------- 1700 ml/day
2) Holliday-Segar method ------------------- ml/day
3) RDA method --------------------------------- 1700-2000 ml/day
4) urine output (urine out +500ml/day)- ml/day
What formula did you ultimately use for the Pt & why?? RDA gives an appropriate range. Both values very similar
Show your work for two of the four methods above used:
Nutrition Database
1) mL/Kg Depending on age:
25mL/kg 25ml(68kg) = 1700ml H2O
2) RDA Method
Choose 1700-2000kcal needs 1700-2000ml H2O
Parenteral Calculations: What is the macronutrient composition of the TPN recommended by the physician?
Rate? ________mL/hr for how long? 24hr 12hr/day ______hr/day
Any PO intake? No Yes , explain ______________________________________________________________
Total volume/24hr __________ mL 2-in-1 Solution 3-in-1 Solution
Carbohydrate Concentration? D________ Amount of Dextrose (in grams) in 1000mL________ g
kcal from Dextrose in 1000mL (grams * 3.4 kcal/g) ________ kcal
Total kcal from Dextrose provided / 24hr? ________ kcal (did you check total volume/24hr?)
Protein Concentration? ________ % Solution Amount of AA (in grams) in 1000mL________ g
kcal from AA in 1000mL (grams * 4 kcal/g) ________ kcal
Total kcal from AA provided / 24hr? ________ kcal (did you check total volume/24hr?)
Lipids 10% (1.1kcal/mL) 20% (2kcal/mL)
mL of lipid solution provided in 24 hr (if hung separately) ________ mL
Amount of lipids infused in g/day ________ g
kcal from lipids infused per day ________ kcal (did you check total volume/24hr?)
Nutrition Database
Does the prescription meet the calculated nutrition needs?
PN provides: ________ Kcal ________ g Pro ________ mL Fluid per day. Compare to
Est. Needs: ________ Kcal ________ g Pro ________ mL Fluid
PN meets how much of calculated needs in %? ________% kcal ________ % Pro ________ % Fluid
Do you have any recommendations?
Enteral Calculations: What is the macronutrient composition of the Enteral Feedings recommended by the physician?
Formula____________________ Bolus? How frequent? ____________ Continuous?
NG PEG Other _________________
Any PO intake? No Yes , explain ______________________________________________________________
Rate? ________mL/hr for how long? 24hr 12hr/day ______hr/day
Total volume (per day) of formula as ordered __________ mL/day
Per 1000mL this formula provides: __________ kcal
__________ g Pro
__________ mL free water
As per total volume (per day) this formula provides: __________ kcal ( ________ kcal/kg)
__________ g Pro (________ g Pro/kg)
__________ mL free water
Any stoppage time to the feedings? yes why? / how long? _________________________ no
If you answered yes above, for how long did the TF run, and what percentage of formula was infused versus
what was ordered for the day? ________________________ %
Additional water flushes per day - __________ mL / day
(also ask nursing how much water is given with medication and try to add to get an idea of fluid given)
Nutrition Database
Total fluid provided (total free water plus additional flushes) __________ mL/day (_______ mL/kcal)
Does the prescription meet the calculated nutrition needs?
TF provides: ________ Kcal ________ g Pro ________ mL Fluid per day. Compare to
Est. Needs: ________ Kcal ________ g Pro ________ mL Fluid
TF meets how much of calculated needs in %? ________% kcal ________ % Pro ________ % Fluid
Do you have any recommendations?
Interaction with the IDT (Interdisciplinary Team)
Indicate if you had interactions with
any of these other health care team
members while providing nutrition
care / patient care
Describe interactions with or referrals made to any of these
health care team professionals:
Nursing (RN)
Spoke to RN about pts plan of care from a nutrition standpoint.
Physician (MD)
Reviewed MDs progress note for any nutrition related issues and
recommendations.
Social Worker (SW)
Speech Therapist (ST/SLP)
Physical Therapist (PT)
Occupational Therapist (OT)
Respiratory Therapist (RRT)
Woundcare / Ostomy Nurse
No noted wounds per chart.
Physicians Assistant (PA)
Other
Nutrition Diagnosis (P-E-S) Statement (write 2)
Problem: Inadequate oral intake
Nutrition Database
related to (Etiology): poor appetite and altered GI functions
as evidenced by Signs and Symptoms: patient report.
Problem: Increased nutrient needs (pro/kcal)
related to (Etiology): increased demands
as evidenced by Signs and Symptoms: colon cancer and colon resection.
Interventions (your recommendation as a dietetic intern)
Encouraged PO intake and hydration
Recommend ensure clear QID
Recommend prostat x 1 packet BID
Consider probiotics (if diarrhea continues)
Provided patient with outpatient referral (per patient request)
Monitoring and Evaluation (how do you monitor this patient, how do you measure progress?)
PO intake goal >75% at most meals
Labs wnl as able
Maintain skin integrity
Avoid further wt. loss
GI fxns wnl as able
Anything else interesting about this patient (e.g. any lab tests or surgical procedures/tests that you were not
familiar with)?
Nutrition Database
Colon resection- bland low residue diet was appropriate. Patients with colon resections do not absorb adequate
amounts of fluid. Hydration encouraged. Because of her colon CA, this patient has increased calorie and protein
needs. This patient mentioned she had three hernias in the abdominal area that could be the cause of her nausea
and vomiting.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Stretchies - Lunch Box Business Plan FinalDocument24 pagesThe Stretchies - Lunch Box Business Plan Finalapi-25760456397% (36)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Pre-NEET Surgery (Khandelwal & Arora) PDFDocument124 pagesPre-NEET Surgery (Khandelwal & Arora) PDFdrng4850% (4)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Cancer Hiv Urine Therapy 44 PDFDocument24 pagesCancer Hiv Urine Therapy 44 PDFAvi G. Ujawane100% (2)
- Angelam-Nutassndiscussion Reviewed-2Document2 pagesAngelam-Nutassndiscussion Reviewed-2api-257604563No ratings yet
- Angelam Chapter4leadershipDocument4 pagesAngelam Chapter4leadershipapi-257604563100% (1)
- Angelam Leadershipch7Document4 pagesAngelam Leadershipch7api-257604563No ratings yet
- Meal Rounds ReportDocument2 pagesMeal Rounds Reportapi-257604563No ratings yet
- Tray AssessmentDocument6 pagesTray Assessmentapi-257604563100% (1)
- Angelam - LTC Case StudiesDocument6 pagesAngelam - LTC Case Studiesapi-257604563No ratings yet
- Angelam - Sodexo Blog PostDocument2 pagesAngelam - Sodexo Blog Postapi-257604563No ratings yet
- Which of The Following Assessment Findings Would Help Confirm A Diagnosis of AsthmaDocument79 pagesWhich of The Following Assessment Findings Would Help Confirm A Diagnosis of Asthmaluiz ManieboNo ratings yet
- Neutrophil To Lymphocyte Ratio (NLR) As An Indicator of Poor Prognosis in Stage IV Non-Small Cell Lung CancerDocument6 pagesNeutrophil To Lymphocyte Ratio (NLR) As An Indicator of Poor Prognosis in Stage IV Non-Small Cell Lung CancerWilliamRayCassidyNo ratings yet
- 2017 PCHRD Completed and Ongoing ProjectsDocument10 pages2017 PCHRD Completed and Ongoing ProjectsInna HusniaNo ratings yet
- 1 s2.0 S0006295223002642 MainDocument15 pages1 s2.0 S0006295223002642 Main吴善统No ratings yet
- Colorectal Cancer: What Is Colorectal Carcinoma?Document4 pagesColorectal Cancer: What Is Colorectal Carcinoma?Ryana Fitriana IINo ratings yet
- Mcqs Mock Exams For General Surgery Board ExamDocument5 pagesMcqs Mock Exams For General Surgery Board ExamMoiz AhmedNo ratings yet
- Laxative Treatment Guideline For AdultsDocument7 pagesLaxative Treatment Guideline For AdultsPurim KTshipNo ratings yet
- GL Principles and Practice of PET-CT Part 1Document101 pagesGL Principles and Practice of PET-CT Part 1Victoria Lopez RodriguezNo ratings yet
- Colorectal Cancer Facts and Figures 2020 2022 PDFDocument48 pagesColorectal Cancer Facts and Figures 2020 2022 PDFm_manuela2002No ratings yet
- Calprotectin LactoferrinDocument16 pagesCalprotectin LactoferrinCristian LaraNo ratings yet
- Kolorektal & Anus: Dr. Yusmaidi, SP.BDocument104 pagesKolorektal & Anus: Dr. Yusmaidi, SP.BAsmorowatiNo ratings yet
- Group 1 CHN OrlandoDocument56 pagesGroup 1 CHN OrlandocabalidarealynNo ratings yet
- A 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaDocument5 pagesA 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaYUSUF MUSANo ratings yet
- NCM 112 MS CA 3.3 Colorectal CancerDocument4 pagesNCM 112 MS CA 3.3 Colorectal CancerCherry Añonuevo RañesesNo ratings yet
- Sample NCLEX Questions With RationaleDocument26 pagesSample NCLEX Questions With RationaleSalanio JinalineNo ratings yet
- Im Irritable Bowel Syndrome Intestinal Obstruction Acute Appendicitis Lecture TransDocument6 pagesIm Irritable Bowel Syndrome Intestinal Obstruction Acute Appendicitis Lecture TransMelissa LabadorNo ratings yet
- Gastroenterology by Elagouri MohammedDocument31 pagesGastroenterology by Elagouri MohammedStylesh GuRlyNo ratings yet
- Practice Guidelines For Tumor Marker Use in The Clinic: Catharine SturgeonDocument9 pagesPractice Guidelines For Tumor Marker Use in The Clinic: Catharine SturgeonYder AtrupNo ratings yet
- Clinicopathological Staging For Colorectal CancerDocument20 pagesClinicopathological Staging For Colorectal Cancertr0xanNo ratings yet
- Selected-Handbook-Case ArimgsasDocument62 pagesSelected-Handbook-Case ArimgsasGabriela ChristianNo ratings yet
- Diabetes and Cancer: A Consensus ReportDocument12 pagesDiabetes and Cancer: A Consensus ReportDeekay06No ratings yet
- Article. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Document8 pagesArticle. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Trí Cương NguyễnNo ratings yet
- 2011 SLE 1st BankDocument222 pages2011 SLE 1st BankEmad Hajali100% (1)
- Colonoscopy Categorisation Guidelines 2017Document2 pagesColonoscopy Categorisation Guidelines 2017ScribboddNo ratings yet
- Eras GynDocument6 pagesEras GynFirah Triple'sNo ratings yet
- DYHFS10 Cancer Prevention Mar 2005Document2 pagesDYHFS10 Cancer Prevention Mar 2005Ngaire TaylorNo ratings yet
- Faktor-Faktor Yang Berhubungan Dengan Terjadinya Maserasi Stoma Pada Pasien Yang Terpasang Kolostomi Di Rsup DR Wahidin Sudirohusodo MakassarDocument8 pagesFaktor-Faktor Yang Berhubungan Dengan Terjadinya Maserasi Stoma Pada Pasien Yang Terpasang Kolostomi Di Rsup DR Wahidin Sudirohusodo MakassarNovia Swanda SinagaNo ratings yet
- Cancer Plan After 1 YrDocument46 pagesCancer Plan After 1 YrShirley SpenceNo ratings yet