Professional Documents
Culture Documents
Ventilator Protocol Card
Ventilator Protocol Card
Uploaded by
Heleninha Marisa Cruz PalasCopyright:
Available Formats
You might also like
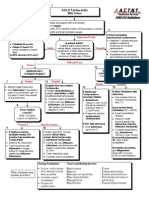
- Algorithm-ACLS Electrical Cardioversion 200612Document1 pageAlgorithm-ACLS Electrical Cardioversion 200612Kavya ShreeNo ratings yet
- Family Case StudyDocument41 pagesFamily Case StudyAcohCChao100% (1)
- Liberation From Mechanical VentilationDocument21 pagesLiberation From Mechanical VentilationRins Chacko50% (2)
- Manual Vortran Go2vent 2Document24 pagesManual Vortran Go2vent 2Carlos Andres Jaimes RicoNo ratings yet
- Coherencia HemodinamicaDocument9 pagesCoherencia HemodinamicaMaritza Alejandra Baeza EricesNo ratings yet
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyNo ratings yet
- Scape Vs FospeDocument5 pagesScape Vs FospeDr. FarhanNo ratings yet
- ACLS NotesDocument3 pagesACLS Notessaxmanwrv0% (1)
- AclsDocument4 pagesAclsAnusha Verghese100% (1)
- CPRDocument4 pagesCPRjeetNo ratings yet
- ACLS PEA Asystole AlgorithmDocument3 pagesACLS PEA Asystole AlgorithmSafira RNo ratings yet
- Swan Ganz CathetersDocument27 pagesSwan Ganz CatheterschadchimaNo ratings yet
- AclsDocument11 pagesAclsdyah rahayu hutamiNo ratings yet
- Defibrillatorppt 131028115457 Phpapp01Document41 pagesDefibrillatorppt 131028115457 Phpapp01Simon JosanNo ratings yet
- ACLS Training - Most Important Points To RememberDocument5 pagesACLS Training - Most Important Points To RememberEman ElzeftawyNo ratings yet
- 2.basic Life SupportDocument7 pages2.basic Life SupportNay ThureinNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- Review of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicDocument105 pagesReview of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicGHALEB A. Almekhlafi100% (1)
- ECG Basics 1Document24 pagesECG Basics 1Dr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- AclsDocument21 pagesAclsMelvin Sierra TejedaNo ratings yet
- Advanced Cardiovascular Life Support (ACLS)Document2 pagesAdvanced Cardiovascular Life Support (ACLS)Vijay MgNo ratings yet
- Post Cardiac ArrestDocument2 pagesPost Cardiac ArrestAlthea AlcalaNo ratings yet
- AHA For PregnancyDocument77 pagesAHA For PregnancyAndrew TimantaNo ratings yet
- Ventilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Document7 pagesVentilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Tarran PhagooNo ratings yet
- Basic Mechanical Ventilation 2014Document62 pagesBasic Mechanical Ventilation 2014dragon66No ratings yet
- ECPRRole CardsDocument17 pagesECPRRole Cardsghg sddNo ratings yet
- Pals Que Estion and Answer FullDocument31 pagesPals Que Estion and Answer FullNeo Latoya MadunaNo ratings yet
- Management of Cardiogenic ShockDocument15 pagesManagement of Cardiogenic ShockcastillojessNo ratings yet
- Heart BlocksDocument6 pagesHeart BlocksMark Hammerschmidt100% (1)
- ACLS TeoriDocument27 pagesACLS TeoriTita Luthfia100% (1)
- ACLS QuizletDocument7 pagesACLS Quizletek.9006001No ratings yet
- DefibrilatorDocument23 pagesDefibrilatorAdank ZonicNo ratings yet
- The Crash CartDocument39 pagesThe Crash Cartpramod kumawat100% (1)
- ACLS Full LectureDocument47 pagesACLS Full LectureAdhydeva Purusanti100% (3)
- Acls TachiDocument1 pageAcls TachiratnawkNo ratings yet
- Abg PrimerDocument22 pagesAbg PrimerAraceli Ecot CalunodNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- Ajnr 7 4 2 PDFDocument8 pagesAjnr 7 4 2 PDFniaNo ratings yet
- Normal Ranges Vital Signs 2017Document2 pagesNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- 2016 Mechanical Ventilation Course MCCADocument38 pages2016 Mechanical Ventilation Course MCCAsultan mansoubNo ratings yet
- Test 3 OutlineDocument3 pagesTest 3 Outlinemara5140No ratings yet
- INTRODUCTION TO SPIROMETRY and 6MWT EditDocument8 pagesINTRODUCTION TO SPIROMETRY and 6MWT Editsai vasavi bandaruNo ratings yet
- Basic Life Support Study Guide: Critical Care Training CenterDocument12 pagesBasic Life Support Study Guide: Critical Care Training CenterTODNo ratings yet
- Cardiopulmonary BypassDocument62 pagesCardiopulmonary BypassNidya Putri100% (1)
- Care of Patient With TPM Slide PresentationDocument16 pagesCare of Patient With TPM Slide PresentationirzehronNo ratings yet
- Noninvasive VentilationDocument6 pagesNoninvasive VentilationEma MagfirahNo ratings yet
- 2020 Acls Megacode Testing Scenarios - 2Document13 pages2020 Acls Megacode Testing Scenarios - 2Dr. Saqib RazaNo ratings yet
- ACLS DrugDocument7 pagesACLS DrugPhongsatorn Thunin100% (1)
- Questions FinalDocument3 pagesQuestions FinalKeerthi Chowdary AmaraneniNo ratings yet
- Med Surge 3 p2Document5 pagesMed Surge 3 p2Ivy NguyenNo ratings yet
- Prognosis MGDocument7 pagesPrognosis MGPutri Cindy Claudia PandoyoNo ratings yet
- Chest PT in Icu 1996@609.full PDFDocument17 pagesChest PT in Icu 1996@609.full PDFDyah SafitriNo ratings yet
- ACLS Skills ChecklistDocument2 pagesACLS Skills ChecklistabdullahNo ratings yet
- How To Dominate The Ventilator: Spinning DialsDocument5 pagesHow To Dominate The Ventilator: Spinning DialsIgnacia Cid PintoNo ratings yet
- How To Dominate The Ventilator: Spinning DialsDocument5 pagesHow To Dominate The Ventilator: Spinning DialsDaia DaiaNo ratings yet
- Spinning Dials - How To Dominate The Ventilator - Handout (EMCRIT, ARDSnet) PDFDocument5 pagesSpinning Dials - How To Dominate The Ventilator - Handout (EMCRIT, ARDSnet) PDFPkernNo ratings yet
- ArdsDocument2 pagesArdsKakaa KakaNo ratings yet
- ARDSNet VentilatorProtocolDocument3 pagesARDSNet VentilatorProtocolMohammed BadieNo ratings yet
- ARDS Management Protocol: February 2018Document6 pagesARDS Management Protocol: February 2018soulstakers100% (1)
- Aprv ManagementDocument2 pagesAprv ManagementSamNo ratings yet
- Anestesia Consideraciones de Anesthesia en Paciente Geratricos PDFDocument3 pagesAnestesia Consideraciones de Anesthesia en Paciente Geratricos PDFFernanda PérezNo ratings yet
- A Simple and Fast Experimental Model: Laboratory InvestigationDocument4 pagesA Simple and Fast Experimental Model: Laboratory InvestigationAjay PeddiNo ratings yet
- Esc Guidelines For The Management of Heart Failure (Autosaved)Document80 pagesEsc Guidelines For The Management of Heart Failure (Autosaved)Ahmad AlKhataybehNo ratings yet
- Innomed Medical Inc.: Cardio-Aid 360-B Biphasic Defibrillator Service ManualDocument45 pagesInnomed Medical Inc.: Cardio-Aid 360-B Biphasic Defibrillator Service ManualLenin SànchezNo ratings yet
- Summary CVS Davidson 23rdDocument5 pagesSummary CVS Davidson 23rdDeshi SportsNo ratings yet
- Lesson 3 Hemodynamic Monitoring Semi Finals 3Document18 pagesLesson 3 Hemodynamic Monitoring Semi Finals 3Juffer ConconNo ratings yet
- 2021 - Skrlec - Sex Differences in Circadian Clock Genes and MI - jcdd-08-00053Document12 pages2021 - Skrlec - Sex Differences in Circadian Clock Genes and MI - jcdd-08-00053Ivana V SkrlecNo ratings yet
- Plactis Datasheet Eastar - Copolyester - MN211 - NaturalDocument3 pagesPlactis Datasheet Eastar - Copolyester - MN211 - NaturalThanh Vũ NguyễnNo ratings yet
- Magensium SulfateDocument2 pagesMagensium SulfateAndrea ANo ratings yet
- Peripheral Vascular SystemDocument3 pagesPeripheral Vascular SystemCzayanne Belle AdreceNo ratings yet
- Level 1-2 Lesson 5 Reading TextDocument1 pageLevel 1-2 Lesson 5 Reading TextJohan ZamoraNo ratings yet
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
- Newborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegeDocument59 pagesNewborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegemgerzonNo ratings yet
- Chest PainDocument5 pagesChest PainAndrei MurariuNo ratings yet
- IFU Ed 2.0 - DFM100 - English-453564403811Document240 pagesIFU Ed 2.0 - DFM100 - English-453564403811technicalservice.pnpNo ratings yet
- PDFDocument19 pagesPDFMYMANo ratings yet
- Case Based Discussion: Sindy Helda PutriDocument30 pagesCase Based Discussion: Sindy Helda PutriSindyputri HeldaNo ratings yet
- M-Mode Echocardiography in DogsDocument10 pagesM-Mode Echocardiography in DogsTactvisNo ratings yet
- MATCVS2023 SouvenirProgrammeDocument57 pagesMATCVS2023 SouvenirProgrammeSim Hann LiangNo ratings yet
- Chapter 22 Assessment of Cardiovascualr SysteamDocument36 pagesChapter 22 Assessment of Cardiovascualr Systeamسلطان محمد فوزي سلمانNo ratings yet
- I. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationDocument2 pagesI. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationBryan Andrew GonzalesNo ratings yet
- 2 - SR Tables On Death 2020 (4) - Rev - JRV - CRDDocument17 pages2 - SR Tables On Death 2020 (4) - Rev - JRV - CRDJosh San PedroNo ratings yet
- BLS Skills Session Checklist and Test CompleteDocument14 pagesBLS Skills Session Checklist and Test Completeicups baptisbatuNo ratings yet
- Defib ATI TemplateDocument1 pageDefib ATI Templatejoshua stapleNo ratings yet
- Adrenergic DrugsDocument6 pagesAdrenergic DrugsbezaleeljonelNo ratings yet
- Jurding DR SaugiDocument44 pagesJurding DR SaugiDian FitriNo ratings yet
- Myocardial Infarction: Basic InformationDocument11 pagesMyocardial Infarction: Basic InformationAnonymous cdLyeXKBNo ratings yet
- Abark PDFDocument73 pagesAbark PDFkeshavNo ratings yet
- LACANGAN Unit 8 Assignment Part 1 - ISBARDocument3 pagesLACANGAN Unit 8 Assignment Part 1 - ISBARLacangan, Thea YvonneNo ratings yet
Ventilator Protocol Card
Ventilator Protocol Card
Uploaded by
Heleninha Marisa Cruz PalasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ventilator Protocol Card
Ventilator Protocol Card
Uploaded by
Heleninha Marisa Cruz PalasCopyright:
Available Formats
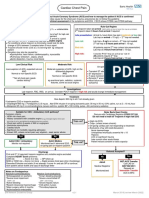
I NCLUSI ON CRI TERI A: Acute onset of
1. PaO
2
/FiO
2
300 (corrected for altitude)
2. Bilateral (patchy, diffuse, or homogeneous) infiltrates consistent with
pulmonary edema
3. No clinical evidence of left atrial hypertension
PART I: VENTI LATOR SETUP AND ADJ USTMENT
1. Calculate predicted body weight (PBW)
Males = 50 + 2.3 [height (inches) - 60]
Females = 45.5 + 2.3 [height (inches) -60]
2. Select any ventilator mode
3. Set ventilator settings to achieve initial V
T
= 8 ml/kg PBW
4. Reduce V
T
by 1 ml/kg at intervals 2 hours until V
T
= 6ml/kg PBW.
5. Set initial rate to approximate baseline minute ventilation (not > 35
bpm).
6. Adjust V
T
and RR to achieve pH and plateau pressure goals below.
A
A
R
R
D
D
S
S
n
n
e
e
t
t
OXYGENATION GOAL: PaO
2
55-80 mmHg or SpO
2
88-95%
Use a minimum PEEP of 5 cm H
2
O. Consider use of incremental FiO
2
/PEEP
combinations such as shown below (not required) to achieve goal.
Lower PEEP/ higher FiO2
FiO
2
0.3 0.4 0.4 0.5 0.5 0.6 0.7 0.7
PEEP 5 5 8 8 10 10 10 12
NIH NHLBI ARDS Clinical Network FiO
2
0.7 0.8 0.9 0.9 0.9 1.0
PEEP 14 14 14 16 18 18-24
Mechanical Ventilation Protocol Summary
Higher PEEP/ lower FiO2
FiO
2
0.3 0.3 0.3 0.3 0.3 0.4 0.4 0.5
PEEP 5 8 10 12 14 14 16 16
FiO
2
0.5 0.5-0.8 0.8 0.9 1.0 1.0
PEEP 18 20 22 22 22 24
__________________________________________________________
PLATEAU PRESSURE GOAL: 30 cm H
2
O
Check Pplat (0.5 second inspiratory pause), at least q 4h and after each
change in PEEP or V
T
.
I f Pplat > 30 cm H
2
O: decrease V
T
by 1ml/kg steps (minimum = 4
ml/kg).
I f Pplat < 25 cm H
2
O and V
T
< 6 ml/ kg, increase V
T
by 1 ml/kg until
Pplat > 25 cm H
2
O or V
T
= 6 ml/kg.
If Pplat < 30 and breath stacking or dys-synchrony occurs: may
increase V
T
in 1ml/kg increments to 7 or 8 ml/kg if Pplat remains < 30 cm
H
2
O.
_____________________________________________________________
pH GOAL: 7.30-7.45
Acidosis Management: (pH < 7.30)
I f pH 7.15-7.30: Increase RR until pH > 7.30 or PaCO
2
< 25
(Maximum set RR = 35).
.
I f pH < 7.15: Increase RR to 35.
If pH remains < 7.15, V
T
may be increased in 1 ml/kg steps until pH >
7.15 (Pplat target of 30 may be exceeded).
May give NaHCO
3
Alkalosis Management: (pH > 7.45) Decrease vent rate if possible.
______________________________________________________
I: E RATI O GOAL: Recommend that duration of inspiration be <
duration of expiration.
PART II : WEANI NG
A. Conduct a SPONTANEOUS BREATHI NG TRI AL daily when:
1. FiO
2
0.40 and PEEP 8.
2. PEEP and FiO
2
values of previous day.
3. Patient has acceptable spontaneous breathing efforts. (May
decrease vent rate by 50% for 5 minutes to detect effort.)
4. Systolic BP 90 mmHg without vasopressor support.
5. No neuromuscular blocking agents or blockade.
B. SPONTANEOUS BREATHING TRIAL (SBT):
If all above criteria are met and subject has been in the study for
at least 12 hours, initiate a trial of UP TO 120 minutes of
spontaneous breathing with FiO2 < 0.5 and PEEP < 5:
1. Place on T-piece, trach collar, or CPAP 5 cm H
2
O with PS < 5
2. Assess for tolerance as below for up to two hours.
a. SpO
2
90: and/or PaO
2
60 mmHg
b. Spontaneous V
T
4 ml/kg PBW
c. RR 35/min
d. pH 7.3
e. No respiratory distress (distress= 2 or more)
HR > 120% of baseline
Marked accessory muscle use
Abdominal paradox
Diaphoresis
Marked dyspnea
3. If tolerated for at least 30 minutes, consider extubation.
4. If not tolerated resume pre-weaning settings.
Definition of UNASSISTED BREATHING
(Different from the spontaneous breathing
criteria as PS is not allowed)
1. Extubated with face mask, nasal prong oxygen, or
room air, OR
2. T-tube breathing, OR
3. Tracheostomy mask breathing, OR
4. CPAP less than or equal to 5 cm H
2
0 without
pressure support or IMV assistance.
You might also like
- Algorithm-ACLS Electrical Cardioversion 200612Document1 pageAlgorithm-ACLS Electrical Cardioversion 200612Kavya ShreeNo ratings yet
- Family Case StudyDocument41 pagesFamily Case StudyAcohCChao100% (1)
- Liberation From Mechanical VentilationDocument21 pagesLiberation From Mechanical VentilationRins Chacko50% (2)
- Manual Vortran Go2vent 2Document24 pagesManual Vortran Go2vent 2Carlos Andres Jaimes RicoNo ratings yet
- Coherencia HemodinamicaDocument9 pagesCoherencia HemodinamicaMaritza Alejandra Baeza EricesNo ratings yet
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyNo ratings yet
- Scape Vs FospeDocument5 pagesScape Vs FospeDr. FarhanNo ratings yet
- ACLS NotesDocument3 pagesACLS Notessaxmanwrv0% (1)
- AclsDocument4 pagesAclsAnusha Verghese100% (1)
- CPRDocument4 pagesCPRjeetNo ratings yet
- ACLS PEA Asystole AlgorithmDocument3 pagesACLS PEA Asystole AlgorithmSafira RNo ratings yet
- Swan Ganz CathetersDocument27 pagesSwan Ganz CatheterschadchimaNo ratings yet
- AclsDocument11 pagesAclsdyah rahayu hutamiNo ratings yet
- Defibrillatorppt 131028115457 Phpapp01Document41 pagesDefibrillatorppt 131028115457 Phpapp01Simon JosanNo ratings yet
- ACLS Training - Most Important Points To RememberDocument5 pagesACLS Training - Most Important Points To RememberEman ElzeftawyNo ratings yet
- 2.basic Life SupportDocument7 pages2.basic Life SupportNay ThureinNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- Review of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicDocument105 pagesReview of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicGHALEB A. Almekhlafi100% (1)
- ECG Basics 1Document24 pagesECG Basics 1Dr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- AclsDocument21 pagesAclsMelvin Sierra TejedaNo ratings yet
- Advanced Cardiovascular Life Support (ACLS)Document2 pagesAdvanced Cardiovascular Life Support (ACLS)Vijay MgNo ratings yet
- Post Cardiac ArrestDocument2 pagesPost Cardiac ArrestAlthea AlcalaNo ratings yet
- AHA For PregnancyDocument77 pagesAHA For PregnancyAndrew TimantaNo ratings yet
- Ventilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Document7 pagesVentilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Tarran PhagooNo ratings yet
- Basic Mechanical Ventilation 2014Document62 pagesBasic Mechanical Ventilation 2014dragon66No ratings yet
- ECPRRole CardsDocument17 pagesECPRRole Cardsghg sddNo ratings yet
- Pals Que Estion and Answer FullDocument31 pagesPals Que Estion and Answer FullNeo Latoya MadunaNo ratings yet
- Management of Cardiogenic ShockDocument15 pagesManagement of Cardiogenic ShockcastillojessNo ratings yet
- Heart BlocksDocument6 pagesHeart BlocksMark Hammerschmidt100% (1)
- ACLS TeoriDocument27 pagesACLS TeoriTita Luthfia100% (1)
- ACLS QuizletDocument7 pagesACLS Quizletek.9006001No ratings yet
- DefibrilatorDocument23 pagesDefibrilatorAdank ZonicNo ratings yet
- The Crash CartDocument39 pagesThe Crash Cartpramod kumawat100% (1)
- ACLS Full LectureDocument47 pagesACLS Full LectureAdhydeva Purusanti100% (3)
- Acls TachiDocument1 pageAcls TachiratnawkNo ratings yet
- Abg PrimerDocument22 pagesAbg PrimerAraceli Ecot CalunodNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- Ajnr 7 4 2 PDFDocument8 pagesAjnr 7 4 2 PDFniaNo ratings yet
- Normal Ranges Vital Signs 2017Document2 pagesNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- 2016 Mechanical Ventilation Course MCCADocument38 pages2016 Mechanical Ventilation Course MCCAsultan mansoubNo ratings yet
- Test 3 OutlineDocument3 pagesTest 3 Outlinemara5140No ratings yet
- INTRODUCTION TO SPIROMETRY and 6MWT EditDocument8 pagesINTRODUCTION TO SPIROMETRY and 6MWT Editsai vasavi bandaruNo ratings yet
- Basic Life Support Study Guide: Critical Care Training CenterDocument12 pagesBasic Life Support Study Guide: Critical Care Training CenterTODNo ratings yet
- Cardiopulmonary BypassDocument62 pagesCardiopulmonary BypassNidya Putri100% (1)
- Care of Patient With TPM Slide PresentationDocument16 pagesCare of Patient With TPM Slide PresentationirzehronNo ratings yet
- Noninvasive VentilationDocument6 pagesNoninvasive VentilationEma MagfirahNo ratings yet
- 2020 Acls Megacode Testing Scenarios - 2Document13 pages2020 Acls Megacode Testing Scenarios - 2Dr. Saqib RazaNo ratings yet
- ACLS DrugDocument7 pagesACLS DrugPhongsatorn Thunin100% (1)
- Questions FinalDocument3 pagesQuestions FinalKeerthi Chowdary AmaraneniNo ratings yet
- Med Surge 3 p2Document5 pagesMed Surge 3 p2Ivy NguyenNo ratings yet
- Prognosis MGDocument7 pagesPrognosis MGPutri Cindy Claudia PandoyoNo ratings yet
- Chest PT in Icu 1996@609.full PDFDocument17 pagesChest PT in Icu 1996@609.full PDFDyah SafitriNo ratings yet
- ACLS Skills ChecklistDocument2 pagesACLS Skills ChecklistabdullahNo ratings yet
- How To Dominate The Ventilator: Spinning DialsDocument5 pagesHow To Dominate The Ventilator: Spinning DialsIgnacia Cid PintoNo ratings yet
- How To Dominate The Ventilator: Spinning DialsDocument5 pagesHow To Dominate The Ventilator: Spinning DialsDaia DaiaNo ratings yet
- Spinning Dials - How To Dominate The Ventilator - Handout (EMCRIT, ARDSnet) PDFDocument5 pagesSpinning Dials - How To Dominate The Ventilator - Handout (EMCRIT, ARDSnet) PDFPkernNo ratings yet
- ArdsDocument2 pagesArdsKakaa KakaNo ratings yet
- ARDSNet VentilatorProtocolDocument3 pagesARDSNet VentilatorProtocolMohammed BadieNo ratings yet
- ARDS Management Protocol: February 2018Document6 pagesARDS Management Protocol: February 2018soulstakers100% (1)
- Aprv ManagementDocument2 pagesAprv ManagementSamNo ratings yet
- Anestesia Consideraciones de Anesthesia en Paciente Geratricos PDFDocument3 pagesAnestesia Consideraciones de Anesthesia en Paciente Geratricos PDFFernanda PérezNo ratings yet
- A Simple and Fast Experimental Model: Laboratory InvestigationDocument4 pagesA Simple and Fast Experimental Model: Laboratory InvestigationAjay PeddiNo ratings yet
- Esc Guidelines For The Management of Heart Failure (Autosaved)Document80 pagesEsc Guidelines For The Management of Heart Failure (Autosaved)Ahmad AlKhataybehNo ratings yet
- Innomed Medical Inc.: Cardio-Aid 360-B Biphasic Defibrillator Service ManualDocument45 pagesInnomed Medical Inc.: Cardio-Aid 360-B Biphasic Defibrillator Service ManualLenin SànchezNo ratings yet
- Summary CVS Davidson 23rdDocument5 pagesSummary CVS Davidson 23rdDeshi SportsNo ratings yet
- Lesson 3 Hemodynamic Monitoring Semi Finals 3Document18 pagesLesson 3 Hemodynamic Monitoring Semi Finals 3Juffer ConconNo ratings yet
- 2021 - Skrlec - Sex Differences in Circadian Clock Genes and MI - jcdd-08-00053Document12 pages2021 - Skrlec - Sex Differences in Circadian Clock Genes and MI - jcdd-08-00053Ivana V SkrlecNo ratings yet
- Plactis Datasheet Eastar - Copolyester - MN211 - NaturalDocument3 pagesPlactis Datasheet Eastar - Copolyester - MN211 - NaturalThanh Vũ NguyễnNo ratings yet
- Magensium SulfateDocument2 pagesMagensium SulfateAndrea ANo ratings yet
- Peripheral Vascular SystemDocument3 pagesPeripheral Vascular SystemCzayanne Belle AdreceNo ratings yet
- Level 1-2 Lesson 5 Reading TextDocument1 pageLevel 1-2 Lesson 5 Reading TextJohan ZamoraNo ratings yet
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
- Newborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegeDocument59 pagesNewborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegemgerzonNo ratings yet
- Chest PainDocument5 pagesChest PainAndrei MurariuNo ratings yet
- IFU Ed 2.0 - DFM100 - English-453564403811Document240 pagesIFU Ed 2.0 - DFM100 - English-453564403811technicalservice.pnpNo ratings yet
- PDFDocument19 pagesPDFMYMANo ratings yet
- Case Based Discussion: Sindy Helda PutriDocument30 pagesCase Based Discussion: Sindy Helda PutriSindyputri HeldaNo ratings yet
- M-Mode Echocardiography in DogsDocument10 pagesM-Mode Echocardiography in DogsTactvisNo ratings yet
- MATCVS2023 SouvenirProgrammeDocument57 pagesMATCVS2023 SouvenirProgrammeSim Hann LiangNo ratings yet
- Chapter 22 Assessment of Cardiovascualr SysteamDocument36 pagesChapter 22 Assessment of Cardiovascualr Systeamسلطان محمد فوزي سلمانNo ratings yet
- I. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationDocument2 pagesI. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationBryan Andrew GonzalesNo ratings yet
- 2 - SR Tables On Death 2020 (4) - Rev - JRV - CRDDocument17 pages2 - SR Tables On Death 2020 (4) - Rev - JRV - CRDJosh San PedroNo ratings yet
- BLS Skills Session Checklist and Test CompleteDocument14 pagesBLS Skills Session Checklist and Test Completeicups baptisbatuNo ratings yet
- Defib ATI TemplateDocument1 pageDefib ATI Templatejoshua stapleNo ratings yet
- Adrenergic DrugsDocument6 pagesAdrenergic DrugsbezaleeljonelNo ratings yet
- Jurding DR SaugiDocument44 pagesJurding DR SaugiDian FitriNo ratings yet
- Myocardial Infarction: Basic InformationDocument11 pagesMyocardial Infarction: Basic InformationAnonymous cdLyeXKBNo ratings yet
- Abark PDFDocument73 pagesAbark PDFkeshavNo ratings yet
- LACANGAN Unit 8 Assignment Part 1 - ISBARDocument3 pagesLACANGAN Unit 8 Assignment Part 1 - ISBARLacangan, Thea YvonneNo ratings yet