Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
49 viewsSpring Pat 2
Spring Pat 2
Uploaded by
api-241359111Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- Remote DepossessionDocument168 pagesRemote DepossessionMuhammad Ali100% (9)
- Pat 2 Medsurg1Document20 pagesPat 2 Medsurg1api-300849832No ratings yet
- Deepeners - Everything You Want To Know About HypnosisDocument8 pagesDeepeners - Everything You Want To Know About HypnosisarbetaNo ratings yet
- The Book of KnowledgeDocument113 pagesThe Book of Knowledgefever14345100% (4)
- Workbook 2003 AnxietyDocument64 pagesWorkbook 2003 Anxietysherell220100% (5)
- MPT Inter Test 4 PDFDocument5 pagesMPT Inter Test 4 PDFmalgorzata0% (1)
- Pat FundamentalsDocument14 pagesPat Fundamentalsapi-281676750No ratings yet
- Pat Med Surg 1Document22 pagesPat Med Surg 1api-324658071No ratings yet
- Pat 11052014Document18 pagesPat 11052014api-300362983No ratings yet
- Final PatDocument22 pagesFinal Patapi-259394980No ratings yet
- Pat Revised 2013 1Document19 pagesPat Revised 2013 1api-300362033No ratings yet
- Pat 1 Medsurg 2Document18 pagesPat 1 Medsurg 2api-294300618No ratings yet
- Pat PortfolioDocument20 pagesPat Portfolioapi-300861055No ratings yet
- Pat Revised 9-2014 FundamentalsDocument17 pagesPat Revised 9-2014 Fundamentalsapi-300362033No ratings yet
- Med Surg 1 PatDocument20 pagesMed Surg 1 Patapi-301978768No ratings yet
- Pat Semester 1Document17 pagesPat Semester 1api-300946501No ratings yet
- Pat 2 Med SurgDocument18 pagesPat 2 Med Surgapi-316861395No ratings yet
- Portfolio Pat 3Document19 pagesPortfolio Pat 3api-300861055No ratings yet
- Msii Pat 2Document22 pagesMsii Pat 2api-300946501No ratings yet
- Pat1 Med Surg 1Document19 pagesPat1 Med Surg 1api-339132978No ratings yet
- Ms 1 PatDocument19 pagesMs 1 Patapi-281676750No ratings yet
- Case StudyDocument9 pagesCase StudyJayr MartinNo ratings yet
- Pat FundamentalsDocument16 pagesPat Fundamentalsapi-339980385No ratings yet
- Pat II MedsurgDocument19 pagesPat II Medsurgapi-301881424No ratings yet
- Patient Assessment Tool ms2Document27 pagesPatient Assessment Tool ms2api-280998981No ratings yet
- Ms 2 Pat MaffettDocument20 pagesMs 2 Pat Maffettapi-339784339No ratings yet
- Pat FinalDocument20 pagesPat Finalapi-259267079No ratings yet
- Pat 1 2015Document18 pagesPat 1 2015api-315192697No ratings yet
- Pat 2 - Med SurgDocument21 pagesPat 2 - Med Surgapi-315731045No ratings yet
- Jones PatDocument16 pagesJones Patapi-301978768No ratings yet
- Pat Fall 2014Document21 pagesPat Fall 2014api-288536467No ratings yet
- Pat Semester 2Document27 pagesPat Semester 2api-300946501No ratings yet
- Pat Revised 2013 1Document18 pagesPat Revised 2013 1api-324886317No ratings yet
- Pat 2Document21 pagesPat 2api-270783686No ratings yet
- Pat Fall 2014Document17 pagesPat Fall 2014api-300849832No ratings yet
- Case StudyDocument3 pagesCase StudyAngelica Joyce SinnacoNo ratings yet
- Fundamentals PatDocument20 pagesFundamentals Patapi-340247560No ratings yet
- Case StudyDocument9 pagesCase StudyEko CecogoNo ratings yet
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocument20 pagesUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-300454618No ratings yet
- Pat DHDocument17 pagesPat DHapi-283153247No ratings yet
- Pat 2 Medsurg 2Document22 pagesPat 2 Medsurg 2api-315731045No ratings yet
- Shelf IM Patient NotesDocument6 pagesShelf IM Patient NotesRuth SanmooganNo ratings yet
- Monek Case StudyDocument24 pagesMonek Case StudyashnairafatimamaulanaNo ratings yet
- Fundamentals Pat Part 3 - Dean GradedDocument22 pagesFundamentals Pat Part 3 - Dean Gradedapi-252790184No ratings yet
- Chronic Illness: Group 5Document17 pagesChronic Illness: Group 5SelwynVillamorPatenteNo ratings yet
- Pat ms1Document19 pagesPat ms1api-301120253No ratings yet
- Pat 2014Document20 pagesPat 2014api-324658071No ratings yet
- Pat 2 sd-1Document22 pagesPat 2 sd-1api-283672381No ratings yet
- Fluphenazine Decanoate RBMDocument9 pagesFluphenazine Decanoate RBMMustika OktariniNo ratings yet
- Pat 2Document20 pagesPat 2api-300362983No ratings yet
- SOAP - Case Study FormatsDocument8 pagesSOAP - Case Study FormatsDr-Sanjay SinghaniaNo ratings yet
- Pat Ms IIDocument18 pagesPat Ms IIapi-339980385No ratings yet
- MH Case StudyDocument17 pagesMH Case StudyS. JacobsNo ratings yet
- Pat Spring Ms II 2015Document16 pagesPat Spring Ms II 2015api-315435865No ratings yet
- Pat 2Document18 pagesPat 2api-273138891No ratings yet
- Fibromyalgia A Clinical ReviewDocument9 pagesFibromyalgia A Clinical ReviewastrogliaNo ratings yet
- 3 HPLCDocument9 pages3 HPLClorrainebarandonNo ratings yet
- University of South Florida College of Nursing: Fundamental Patient Assessment ToolDocument18 pagesUniversity of South Florida College of Nursing: Fundamental Patient Assessment Toolapi-315731045No ratings yet
- Patsummersemester2015 Anjouligerez-2Document21 pagesPatsummersemester2015 Anjouligerez-2api-325112936No ratings yet
- 6635 NRNP and PRAC Comprehensive Psychiatric EvaluationDocument5 pages6635 NRNP and PRAC Comprehensive Psychiatric EvaluationMarieamme BinaleNo ratings yet
- Literature Review: Parental Refusal of Childhood Vaccinations TonsillectomyDocument2 pagesLiterature Review: Parental Refusal of Childhood Vaccinations TonsillectomyilldoitNo ratings yet
- Pat FinalDocument24 pagesPat Finalapi-252804976No ratings yet
- Soap Note1 - Gyn ComplaintDocument6 pagesSoap Note1 - Gyn Complaintapi-482726932100% (3)
- The Best Practice Is The Lowest Effective Dose Your Third Psychiatric Consultation: Diet, Exercise, and Sleep Trump Medications Medication is the Last Option Your Fourth Psychiatric ConsultationFrom EverandThe Best Practice Is The Lowest Effective Dose Your Third Psychiatric Consultation: Diet, Exercise, and Sleep Trump Medications Medication is the Last Option Your Fourth Psychiatric ConsultationNo ratings yet
- Acharya Masterclass Work BookDocument9 pagesAcharya Masterclass Work BookAnjaniSwethaAnanthapalliNo ratings yet
- Family Coping Index..Document3 pagesFamily Coping Index..Lharra Cagulada-PostranoNo ratings yet
- What Is Qigong 2023Document40 pagesWhat Is Qigong 2023JinadNo ratings yet
- Resoucalm Mindrce Cheat SheetDocument5 pagesResoucalm Mindrce Cheat SheetnihadNo ratings yet
- Energy Healing Hand Positions Mudra CourseDocument36 pagesEnergy Healing Hand Positions Mudra Courseraluuuu2No ratings yet
- Implementation and Intervension (English)Document9 pagesImplementation and Intervension (English)Devi SitudewiNo ratings yet
- What Is Swar VigyanDocument28 pagesWhat Is Swar VigyanNarendra BhogalNo ratings yet
- Deep Breathing ExercisesDocument17 pagesDeep Breathing ExercisesPamela Warner100% (1)
- Working With Older AdultsDocument84 pagesWorking With Older AdultsdarketaNo ratings yet
- Stress, Relaxation States, and CreativityDocument8 pagesStress, Relaxation States, and CreativitySoumitra KunduNo ratings yet
- Improving Creativity For EngineersDocument32 pagesImproving Creativity For EngineersVenkatesh100% (1)
- Self Management SkillsDocument7 pagesSelf Management SkillsAnuj HalderNo ratings yet
- Dialogue (Siti Sabrina, Mita Azani)Document2 pagesDialogue (Siti Sabrina, Mita Azani)mita yuliantiNo ratings yet
- LS5 Managing Emotions and Impulses Activity SheetDocument19 pagesLS5 Managing Emotions and Impulses Activity SheetJocelene Zamora Parungao100% (2)
- Fatigue Related To Autoimmune Disease As Evidenced by Patient Inability To Maintain Usual Level of Physical ActivityDocument5 pagesFatigue Related To Autoimmune Disease As Evidenced by Patient Inability To Maintain Usual Level of Physical ActivityJordz PlaciNo ratings yet
- William G. Braud - Human Interconnectedness: Research IndicationsDocument22 pagesWilliam G. Braud - Human Interconnectedness: Research IndicationsFlikk34100% (1)
- Orgone Energy Info PackDocument39 pagesOrgone Energy Info Packimparante100% (2)
- Assignment-Specific Stress Inoculation Training For Highly Specialized IT PersonnelDocument7 pagesAssignment-Specific Stress Inoculation Training For Highly Specialized IT PersonnelbijsshrjournalNo ratings yet
- Top 10 Benefits of Exercising DailyDocument2 pagesTop 10 Benefits of Exercising DailyRicha VermaNo ratings yet
- Journal of Interprofessional Education & Practice: Kristine Wood, Carolanne CariniDocument4 pagesJournal of Interprofessional Education & Practice: Kristine Wood, Carolanne CariniNatalia BettancourtNo ratings yet
- Exercises For The Master Key: by Charles F. HaanelDocument9 pagesExercises For The Master Key: by Charles F. HaanelPradeep Uday K UNo ratings yet
- Plan de Lectie Unit 5 IntermediateDocument2 pagesPlan de Lectie Unit 5 IntermediateRaluca MotreanuNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument19 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaARJUN BNo ratings yet
- The Little Bowen BookDocument80 pagesThe Little Bowen BookJeremy Monroe100% (6)
- BreathhhhhDocument16 pagesBreathhhhhMOULIANNA8949100% (1)
Spring Pat 2
Spring Pat 2
Uploaded by
api-2413591110 ratings0% found this document useful (0 votes)
49 views22 pagesOriginal Title
spring pat 2
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
49 views22 pagesSpring Pat 2
Spring Pat 2
Uploaded by
api-241359111Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 22
1
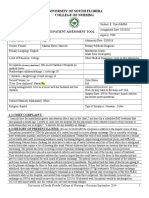
University of South Florida College of Nursing Revision April 2012
UNIVERSITY OF SOUTH FLORIDA
COLLEGE OF NURSING
2 CC:
I came in because the doctor wanted to do an EEG video for my seizures.
3 HPI: (OLD CART)
This is a 59 year old female who arrived in the Emergency Department on 1/28/13 experiencing seizures. Patient stated that the
seizures began about 4 years ago and that she has never been hospitalized for them before. The seizures normally last between 5-10
minutes and tend to happen every morning with occasional ones during the day. Stress could be an aggravating factor and medications
seem to relieve some of the seizures. She is currently on topamax, depacote, and neurontin for her seizures.
Student: Kayla Cormier
PATIENT ASSESSMENT TOOL .
Assignment Date: 2/5/13
Agency: FHT
Patient Initials: EMA Age: 59 Admission Date: 1/28/13
Gender: Female Marital Status: married Primary Medical Diagnosis with ICD-10 code:
Primary Language: English 780.39
Level of Education: High school graduate Other Medical Diagnoses:
Occupation (if retired, what from?): had been a saleswomen and a
beautician
Number/ages children/siblings:
1 sister: 71
2 children: 39 and 37 Code Status: Full code
Living Arrangements: lives at home with her husband Advanced Directives: Living will
Surgery Date: Procedure:
Culture/ Ethnicity /Nationality: American
Religion: Presbyterian Type of Insurance: Medicare
2
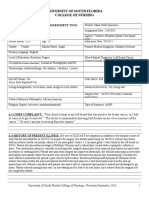
University of South Florida College of Nursing Revision April 2012
3
University of South Florida College of Nursing Revision April 2012
2 PMH/PSH Hospitalizations for any medical illness or operation
Date Operation or Illness Management/Treatment
1973, 1976 Cesarian Section
1982 carpal tunnel release
1982 deviated septum surgery
1984, 1985 ulnar nerve transposition
1987 anterior cervical disc fusion and spurring [C5-6 and 6-
7]
1989 posterior cervical disc fusion and spurring
1991 lumbar bilateral degeneration [L2-3 and 3-4 and 4-5,
fusion L5-S1 herniation]
1993 complete hysterectomy
1994 2nd carpal tunnel release
1996 Lumbar L5-S1 disc protrusion
2005 Torn rotator cuff [right shoulder]
2006 torn rotator cuff [left shoulder]
2007 left and right arthroscopic knee surgery
2008 right total knee
2008 right carpal tunnel release
2009 left total knee
2 FMH
A
g
e
(
i
n
y
e
a
r
s
)
Cause
of
Death
(if applicable)
A
l
c
o
h
o
l
i
s
m
E
n
v
i
r
o
n
m
e
n
t
a
l
A
l
l
e
r
g
i
e
s
A
n
e
m
i
a
A
r
t
h
r
i
t
i
s
A
s
t
h
m
a
B
l
e
e
d
s
E
a
s
i
l
y
C
a
n
c
e
r
D
i
a
b
e
t
e
s
G
l
a
u
c
o
m
a
G
o
u
t
H
e
a
r
t
T
r
o
u
b
l
e
(
a
n
g
i
n
a
,
M
I
,
D
V
T
H
y
p
e
r
t
e
n
s
i
o
n
K
i
d
n
e
y
P
r
o
b
l
e
m
s
M
e
n
t
a
l
H
e
a
l
t
h
P
r
o
b
l
e
m
s
S
e
i
z
u
r
e
s
S
t
o
m
a
c
h
U
l
c
e
r
s
S
t
r
o
k
e
T
u
m
o
r
4
University of South Florida College of Nursing Revision April 2012
e
t
c
.
)
Father 57 heart X X
Mother 81 lung cancer X X X X X X
Brother
Sister
relationship
relationship
relationship
Comments:
1 IMMUNIZATION HISTORY
YES NO
Routine childhood vaccinations X
Routine adult vaccinations for military or federal service X
Adult Diphtheria (Date) X
Adult Tetanus (Date) X
Influenza (flu) (Date) October 2013 X
Pneumococcal (pneumonia) (Date) within the last 5 years X
Have you had any other vaccines given for international travel or
occupational purposes? Please List
X
1 Allergies or
Adverse Reactions
NAME of
Causative Agent
Type of Reaction (describe explicitly)
Medications
aspirin trouble breathing
bacitracin swelling, red skin
ciprofloxacin unknown
Other (food, tape, dye,
etc.)
5
University of South Florida College of Nursing Revision April 2012
5 PATHOPHYSIOLOGY: (include APA reference) (include any genetic factors impacting the diagnosis,
prognosis or treatment)
Pseudoseizure is a condition in which a person experiences a loss of consciousness and has moments when the muscles contract and
relax, however there are no abnormal firings in the brain. The best way to diagnose a pseudoseizure disorder is through video EEG
monitoring. Electrodes are attached to the patients head and can read the signals the brain sends. Pseudoseizures do not have a
specific treatment, and tend to have an underlying psychological background. Sometimes the pseudoseizures happen as a result of a
traumatic event or something a person unconsciously hides. Patients are normally on anti-seizure medications to try to help control the
seizure activity. There do not seem to be any genetic factors that predispose this condition.
Huether, S., McCance, K. (2012). Understanding Pathophysiology, 1053.
5 MEDICATIONS: (Include both prescription and OTC)
Name: Sodium Chloride Concentration 0.9% Dosage Amount: 10 mL
Route: IV Push Frequency: Q4H
Pharmaceutical class: mineral electrolyte replacement supplements
Home Hospital or Both
Indication: hydration, maintain fluid/electrolyte balance
Name: Conjugated Estrogens Concentration: 0.3 mg Dosage Amount: .45 mg
Route: PO Frequency: daily
Pharmaceutical class: hormone replacement
Home Hospital or Both
Indication: used to treat menopausal symptoms and prevent osteoporosis
Name: cyanocobalamin Concentration: 1000 mcg Dosage Amount: 500 mcg
Route: PO Frequency: daily
Pharmaceutical class: water soluble vitamins
Home Hospital or Both
6
University of South Florida College of Nursing Revision April 2012
Indication: vitamin B12 deficiency, pernicious anemia
Name: dicyclomine Concentration: 10 mg Dosage Amount: 20 mg
Route: PO Frequency: TID
Pharmaceutical class: anticholinergics
Home Hospital or Both
Indication: management of irritable bowel syndrome
Name: ducosate sodium Concentration: 100 mg Dosage Amount: 100 mg
Route: PO Frequency: BID
Pharmaceutical class
Home Hospital or Both
Indication
Name: fexofenadine Concentration: 180 mg Dosage Amount: 180 mg
Route: PO Frequency: daily
Pharmaceutical class: antihistamine
Home Hospital or Both
Indication: relief of symptoms of seasonal allergic rhinitis
Name: fondaparinux Concentration: 2.5 mg/ 0.5 mL Dosage Amount: 2.5 mg
Route: Subcutaneous Frequency: daily
Pharmaceutical class: active factor x inhibitors
Home Hospital or Both
Indication: prevent DVT and PE
Name: Levothyroxine Concentration: 0.112 mg Dosage Amount: 0. 112 mg
Route: PO Frequency: daily
Pharmaceutical class: thyroid preparations
Home Hospital or Both
Indication: thyroid supplementation in hypothyroidism, treatment of euthyroid goiters
Name: lubiprostone Concentration: 24 mcg Dosage Amount:24 mcg
Route: PO Frequency: BID
Pharmaceutical class: chloride channel activators
Home Hospital or Both
Indication: irritable bowel syndrome, chronic constipation
Name: Montelukast Concentration: 10 mg Dosage Amount 10 mg
Route: PO Frequency: QHS
Pharmaceutical class: leukotriene antagonists
Home Hospital or Both
Indication: prevention and chronic treatment of asthma, seasonal allergies
Name: Morphine Sulfate Concentration: 30 mg Dosage Amount: 30 mg
7
University of South Florida College of Nursing Revision April 2012
Route: PO Frequency: BID
Pharmaceutical class: opioid
Home Hospital or Both
Indication: control of acute or chronic pain
Name: Saccharomyces Boulardii Concentration Dosage Amount
Route: PO Frequency: BID
Pharmaceutical class:
Home Hospital or Both
Indication
Name: Sertraline Concentration: 100 mg Dosage Amount: 100 mg
Route: PO Frequency: QHS
Pharmaceutical class: SSRI
Home Hospital or Both
Indication: major depressive disorder, panic disorder, general anxiety disorder
Name: Diphenhydramine Concentration: 25 mg Dosage Amount: 25 mg
Route: PO Frequency: Q6H
Pharmaceutical class: antihistamine
Home Hospital or Both
Indication: relief of allergic symptoms
8
University of South Florida College of Nursing Revision April 2012
4 NUTRITION: (Include: type of diet, 24 HR average home diet, 24 HR diet recall, your nutritional analysis)
Diet ordered in hospital? Analysis of home diet (Compare to food pyramid and
Regular diet Consider co-morbidities and cultural considerations):
Diet pt follows at home?
Breakfast:
Poptarts, breakfast burrito, eggs, sausage, biscuits
Lunch:
sandwich, or has big lunch and small dinner
Dinner:
lasagna, skillet dinners, quick and easy dinners
Snacks:
occasional granola bar
2 COPING ASSESSMENT/SUPPORT SYSTEM: (these are prompts designed to help guide your discussion)
Who helps you when you are ill?
Husband helps when he is able.
How do you generally cope with stress? or What do you do when you are upset?
She just moves on; sometimes she walks the dog if she needs to take a walk.
Recent difficulties (Feelings of depression, anxiety, being overwhelmed, relationships, friends, social life)
The health of her and her husband; she wants to be back with her kids in Maryland; she is also having trouble dealing with recent
independence changes [becoming more dependent]
9
University of South Florida College of Nursing Revision April 2012
+2 DOMESTIC VIOLENCE ASSESSMENT
Consider beginning with: Unfortunately many, children, as well as adult women and men have been or currently are
unsafe in their relationships in their homes. I am going to ask some questions that help me to make sure that you are
safe.
Have you ever felt unsafe in a close relationship? ____NO___________________________________________________
Have you ever been talked down to?_NOT REALLY____ Have you ever been hit punched or slapped? ___NO________
Have you been emotionally or physically harmed in other ways by a person in a close relationship with you?
__NO________________________________________ If yes, have you sought help for this? ______________________
Are you currently in a safe relationship?
Yes
5 DEVELOPMENTAL CONSIDERATIONS:
Eriksons stage of psychosocial development: Trust vs. Mistrust Autonomy vs. Doubt & Shame Initiative vs. Guilt Industry vs. Inferiority
Identity vs. Role Confusion/Diffusion Intimacy vs. Isolation Generativity vs. Self absorption/Stagnation Ego Integrity vs. Despair
Give the textbook definition of both parts of Ericksons developmental stage for your patients age group:
Erikson theorized that a person wants to gain the capacity to produce something that outlives the individual.
This time in a persons life they tend to be caring, mentoring, and self-aware.
Rider, E., Sigelman, C. (2009). Life-Span Human Development, 332.
Describe the characteristics that the patient exhibits that led you to your determination:
The patient is a 59 year old female who lives with her husband. She takes care of her husband and his mother. Her children live in
Maryland and she doesnt see them very often. I can tell from talking to her that she worries much more about her children and
grandchildren than she does herself. I think the stagnant part also shines through because of the disease interrupting her life and her
inability to be with her family in her time of need.
Describe what impact of disease/condition or hospitalization has had on your patients developmental stage of life:
The disease has interrupted the generativity of her life and put her in a stagnant pattern of focusing on the distance of family in her
life.
+3 Cultural Assessment:
What do you think is the causes of your illness?
She wishes she knew.
What does your illness mean to you?
This illness is interrupting her life and is stressful.
10
University of South Florida College of Nursing Revision April 2012
+3 Sexuality Assessment: (the following prompts may help to guide your discussion)
Consider beginning with: I am asking about your sexual history in order to obtain information that will screen for
possible sexual health problems, these are usually related to either infection, changes with aging and/or quality of
life. All of these questions are confidential and protected in your medical record
Have you ever been sexually active?__YES_______________________________________________________________
Do you prefer women, men or both genders? ___MEN_____________________________________________________
Are you aware of ever having a sexually transmitted infection? ___NO________________________________________
Have you or a partner ever had an abnormal pap smear?___NO_______________________________________________
Have you or your partner received the Gardasil (HPV) vaccination? ___NO_____________________________________
Are you currently sexually active? __YES_____________________When sexually active, what measures do you take to
prevent acquiring a sexually transmitted disease or an unintended
pregnancy? ___LOYALTY_______________________
How long have you been with your current partner?___17 YEARS___________________________________________
Have any medical or surgical conditions changed your ability to have sexual activity? _NO________________________
Do you have any concerns about sexual health or how to prevent sexually transmitted disease or unintended pregnancy?
NO
11
University of South Florida College of Nursing Revision April 2012
+3 SMOKING, CHEMICAL USE, OCCUPATIONAL/ENVIRONMENTAL EXPOSURES:
1. Does the patient currently, or has he/she ever smoked or used chewing tobacco? Yes No
If so, what? How much? For how many years?
cigarettes 1/2 - 1 pack daily (age 12 thru 44 )
If applicable, when did the patient
quit?
1998
Does anyone in the patients household smoke tobacco? If so,
what, and how much?
Has the patient ever tried to quit? Yes.
NO
2. Does the patient drink alcohol or has he/she ever drank alcohol? Yes No
What? How much? For how many years?
(age thru )
If applicable, when did the patient quit?
3. Has the patient ever used street drugs such as marijuana, cocaine, heroin, or other? Yes No
If so, what?
How much? For how many years?
(age thru )
Is the patient currently using these drugs?
Yes No
If not, when did he/she quit?
4. Have you ever, or are you currently exposed to any occupational or environmental Hazards/Risks
None known
12
University of South Florida College of Nursing Revision April 2012
10 REVIEW OF SYSTEMS
General Constitution Gastrointestinal Immunologic
X Recent weight loss or gain X Nausea, vomiting, or diarrhea Chills with severe shaking
Integumentary X Constipation X Irritable Bowel Night sweats
Changes in appearance of skin X GERD Cholecystitis Fever
Problems with nails XIndigestion Gastritis / Ulcers HIV or AIDS
Dandruff XHemorrhoids Blood in the stool Lupus
Psoriasis Yellow jaundice Hepatitis Rheumatoid Arthritis
Hives or rashes Pancreatitis Sarcoidosis
Skin infections Colitis Tumor
X Use of sunscreen SPF: Diverticulitis Life threatening allergic reaction
Bathing routine: every other day Appendicitis Enlarged lymph nodes
Other: Abdominal Abscess Other:
X Last colonoscopy?
HEENT Other: Hematologic/Oncologic
X Difficulty seeing Genitourinary Anemia
Cataracts or Glaucoma nocturia Bleeds easily
X Difficulty hearing dysuria X Bruises easily
X Ear infections hematuria Cancer
X Sinus pain or infections polyuria X Blood Transfusions
X Nose bleeds kidney stones Blood type if known: A+
X Post-nasal drip Normal frequency of urination: 8 x/day Other:
Oral/pharyngeal infection X Bladder or kidney infections
Dental problems Metabolic/Endocrine
Routine brushing of teeth 1-2 x/day Diabetes Type:
Routine dentist visits 2 x/year X Hypothyroid /Hyperthyroid
X Vision screening Intolerance to hot or cold
Other: Osteoporosis
Other:
Pulmonary
X Difficulty Breathing Central Nervous System
Cough - dry or productive WOMEN ONLY CVA
X Asthma Infection of the female genitalia X Dizziness
X Bronchitis X Monthly self breast exam X Severe Headaches
Emphysema Frequency of pap/pelvic exam X Migraines
Pneumonia Date of last gyn exam? X Seizures
Tuberculosis menstrual cycle regular irregular Ticks or Tremors
Environmental allergies menarche age? Encephalitis
X last CXR? menopause age? Meningitis
Other: Date of last Mammogram &Result: Other:
Date of DEXA Bone Density & Result:
Cardiovascular MEN ONLY Mental Illness
Hypertension Infection of male genitalia/prostate? X Depression
X Hyperlipidemia Frequency of prostate exam? Schizophrenia
X Chest pain / Angina Date of last prostate exam? Anxiety
Myocardial Infarction BPH Bipolar
CAD/PVD Urinary Retention Other:
CHF Musculoskeletal
X Murmur Injuries or Fractures Childhood Diseases
Thrombus X Weakness X Measles
Rheumatic Fever X Pain X Mumps
Myocarditis Gout Polio
13
University of South Florida College of Nursing Revision April 2012
Arrhythmias Osteomyelitis Scarlet Fever
X Last EKG screening, when? 5 YEARS X Arthritis X Chicken Pox
Other: Other: Other:
REVIEW OF SYSTEMS NARRATIVE
General Constitution
Pts perception of health:
The patient perceives her health as declining. She is afraid of losing her independence. Her husband has MS
and she is his care taker. However, while she is in the hospital dealing with her own illness she has to rely on
other people for transportation and to care for her and her husband. The seizures are interrupting her life and the
lack of close family in the area also adds stress and anxiety to her life. She hopes that finding the cause of her
seizures will lead to a way to deal with them and hopefully allow her to return to her life.
Is there any problem that is not mentioned that your patient sought medical attention for with anyone?
None that she stated.
Any other questions or comments that your patient would like you to know?
Not that she stated.
14
University of South Florida College of Nursing Revision April 2012
10 PHYSICAL EXAMINATION:
Orientation and level of Consciousness: ALERT TO PERSON, PLACE, AND TIME
General Survey: Height: 152.4 CM Weight: 71.6 KG BMI: 30.8 Pain: (include rating & location)
NO PAIN AT TIME OF ASSESSMENT
Pulse: 77 Blood
Pressure: 123/57 RIGHT
(include location) ARM
Temperature: (route taken?) Respirations: 18
SpO
2 99
Is the patient on Room Air or O
2
: ROOM AIR
Overall Appearance: [Dress/grooming/physical handicaps/eye contact]
clean, hair combed, dress appropriate for setting and temperature, maintains eye contact, no obvious handicaps
Overall Behavior: [e.g.: appropriate/restless/odd mannerisms/agitated/lethargic/other]
awake, calm, relaxed, interacts well with others, judgment intact
Speech: [e.g.: clear/mumbles /rapid /slurred/silent/other]
clear, crisp diction
Mood and Affect: pleasant cooperative cheerful talkative quiet boisterous flat
apathetic bizarre agitated anxious tearful withdrawn aggressive hostile loud
Other:
Integumentary
X Skin is warm, dry, and intact
X Skin turgor elastic
X No rashes, lesions, or deformities
X Nails without clubbing
X Capillary refill < 3 seconds
X Hair evenly distributed, clean, without vermin
Peripheral IV site Type: 22 GAUGE Location: RIGHT FOREARM Date inserted: 1/28/13
no redness, edema, or discharge
Fluids infusing? no yes - what?
Peripheral IV site Type: Location: Date inserted:
no redness, edema, or discharge
Fluids infusing? no yes - what?
Central access device Type: Location: Date inserted:
Fluids infusing? no yes - what?
HEENT: X Facial features symmetric X No pain in sinus region X No pain, clicking of TMJ X Trachea midline
15
University of South Florida College of Nursing Revision April 2012
X Thyroid not enlarged X No palpable lymph nodes X sclera white and conjunctiva clear; without
discharge
X Eyebrows, eyelids, orbital area, eyelashes, and lacrimal glands symmetric without edema or tenderness
Functional vision: right eye - left eye - without corrective lenses
right eye - left eye - with corrective lenses
Functional vision both eyes together: with corrective lenses or NA
PERRLA pupil size / mm Peripheral vision intact EOM intact through 6 cardinal fields without nystagmus
X Ears symmetric without lesions or discharge Whisper test heard: right ear- inches & left ear- inches
Weber test, heard equally both ears Rinne test, air time(s) longer than bone
X Nose without lesions or discharge X Lips, buccal mucosa, floor of mouth, & tongue pink & moist without lesions
Dentition:
Comments: THE VISION AND HEARING TESTS WERE NOT PERFORMED
16
University of South Florida College of Nursing Revision April 2012
Pulmonary/Thorax: Respirations regular and unlabored Transverse to AP ratio 2:1 Chest expansion
symmetric
Lungs clear to auscultation in all fields without adventitious sounds
CL Clear
Percussion resonant throughout all lung fields, dull towards posterior bases
WH Wheezes
Tactile fremitus bilaterally equal without overt vibration
CR - Crackles
Sputum production: thick thin Amount: scant small moderate large
RH Rhonchi
Color: white pale yellow yellow dark yellow green gray light tan brown red
D Diminished
S Stridor
Ab - Absent
Cardiovascular: No lifts, heaves, or thrills PMI felt at: 5TH ICS MCL
Heart sounds: S
1
S
2
Regular Irregular X No murmurs, clicks, or adventitious heart sounds X No JVD
Rhythm (for patients with ECG tracing tape 6 second strip below and analyze)
X Calf pain bilaterally negative Pulses bilaterally equal [rating scale: 0-absent, 1-barely palpable, 2-weak, 3-normal, 4-bounding]
Apical pulse: Carotid: Brachial: Radial: 2 Femoral: Popliteal: DP: PT: 2
X No temporal or carotid bruits Edema: [rating scale: 0-none, +1 (1-2mm), +2 (3-4mm), +3 (5-6mm), +4(7-8mm) ]
Location of edema: pitting non-pitting
X Extremities warm with capillary refill less than 3 seconds
GI/GU: X Bowel sounds active x 4 quadrants; no bruits auscultated No organomegaly Liver span cm
Percussion dull over liver and spleen and tympanic over stomach and intestine X Abdomen non-tender to palpation
17
University of South Florida College of Nursing Revision April 2012
Urine output: Clear Cloudy Color: Previous 24 hour output: mLs N/A
Foley Catheter Urinal or Bedpan Bathroom Privileges without assistance or X with assistance
CVA punch without rebound tenderness
Last BM: (date 1 / 24 / 2013 ) Formed Semi-formed Unformed Soft Hard Liquid Watery
Color: Light brown Medium Brown Dark Brown Yellow Green White Coffee Ground Maroon Bright Red
Hemoccult positive / negative
Genitalia: Clean, moist, without discharge, lesions or odor Not assessed, patient alert, oriented, denies problems
Other Describe:
Musculoskeletal: X Full ROM intact in all extremities without crepitus
Strength bilaterally equal at __4_____ in UE & __4_____ in LE
[rating scale: 0-absent, 1-trace, 2-not against gravity, 3-against gravity but not against resistance, 4-against some resistance, 5-against full resistance]
vertebral column without kyphosis or scoliosis
Neurovascular status intact: peripheral pulses palpable, no pain, pallor, paralysis or parathesias
Neurological: X Patient awake, alert, oriented to person, place, time, and date Confused; if confused attach mini mental exam
CN 2-12 grossly intact Sensation intact to touch, pain, and vibration Rombergs Negative
Stereognosis, graphesthesia, and proprioception intact Gait smooth, regular with symmetric length of the stride
DTR: [rating scale: 0-absent, +1 sluggish/diminished, +2 active/expected, +3 slightly hyperactive, +4 Hyperactive, with intermittent or transient clonus]
Triceps: Biceps: Brachioradial: Patellar: Achilles: Ankle clonus: positive negative Babinski: positive negative
10 PERTINENT LAB VALUES AND DIAGNOSTIC TEST RESULTS (include pertinent normals as well
as abnormals, include rationale and analysis. List dates with all labs and diagnostic tests):
For this patient, a CBC and PT/PTT/INR were ordered on admission. The HMG at 11.8 and HCT at 38.9 are low. I am not sure the
reason for this because she had not had not had surgery recently.
Cl is 108 and slightly elevated. An elevated chlorine can present as Kussmauls breathing, weakness, and intense thirst. For this
patient, she was weak but did not experience any excessive thirst or abnormal breathing.
PT is 13 elevated and PTT is 28 low. This symbolizes that the time it takes for blood to clot is longer than it should be. This is
important to know because she should be on bleeding precautions.
Also, patients EEG during seizures, showed no abnormal electrical activity which brought about the pseudoseizure diagnosis.
+2 CURRENT HEALTHCARE TREATMENTS AND PROCEDURES:
The patient is talking to a hospital psychologist.
The patient is also undergoing video EEG monitoring to help diagnose and analyze her seizures.
18
University of South Florida College of Nursing Revision April 2012
19
University of South Florida College of Nursing Revision April 2012
2 Medical Diagnoses
(as listed on the chart)
8 Nursing Diagnoses
(actual and potential - listed in order of priority)
1. unspecified epilepsy 1. Moderate anxiety r/t unknown cause of seizures aeb
patients appearance and statement of anxiety
2. 2. Compromised family coping r/t situational crisis the
significant person may be facing aeb husband suffering his
own illness
3. 3. Stress overload r/t illness, coping, and helpless feelings
aeb patient appearing and stating that stress is a problem.
4. 4. risk for ineffective breathing pattern r/t seizure activity
aeb patients interrupted breathing while experiencing a
seizure.
5. 5. Risk for loneliness r/t social isolation from children aeb
patient complaints of not seeing her children and feeling
lonely in Tampa.
20
University of South Florida College of Nursing Revision April 2012
15 for Care Plan
Nursing Diagnosis: Moderate anxiety r/t unknown cause of seizures aeb patients appearance and statement of
anxiety from illness
Patient
Goals/Outcomes
Nursing Interventions
to Achieve Goal
Rationale for
Interventions
Provide References
Evaluation of
Interventions on Day
care is Provided
1. Patient is will begin to
recognize signs of her anxiety by
the end of the shift.
1.a. Talk to patient about
stressors in her life and how
anxiety affects her life
1.b. Have patient state possible
signs of incoming anxiety
Talking to patient will help her
be able to think through possible
boundaries and help realized
potential triggers to prevent
them.
Patient stated that she was
anxious but during my time was
not able to discuss signs and
symptoms of her anxiety.
2. Patient will verbalize and
demonstrate positive coping
skills throughout shift.
2.a. Discuss how patient copes
with stress
2.b. Give patient some additional
options for coping mechanisms
Allowing the patient to think
about how they cope will help
them open up. It is also
important to provide additional
information to help them
improve their coping ability and
minimize anxiety.
Patient stated that she coped by
walking away when she needed.
I did not get to talk about other
coping skills during my time on
the floor.
3. Patient will state a reduced
level of anxiety by the end of the
shift
3.a. Establish a beginning
numerical rating of anxiety [0-
10] and find a comfortable level
of anxiety to be a goal.
3.b. Provide a quiet and
welcoming atmosphere
If the patient is feeling
comfortable hopefully the
anxiety level will go down.
Patient went from a 7 level to a 4
level while I was on the floor.
Discharge Planning: (put a * in front of any pt education in above care plan that you would include for
discharge teaching)
Upon discharge I would make sure follow up appointments have been arrange and patient has transportation to
physician's offices. I would discuss the patients living arrangement, making sure there arent stairs and throw
rugs to minimize fall risk, and to know who lives with the patient to see if I need to include teaching with
family members. Next I would discuss the medications the patient will be going home with. I will ask about her
access to the prescriptions like cost and transportation for pick-up. I would teach her when to take medications,
what side effects to look for, when to notify her physician or come to the ER. I would ask the patient about her
questions/concerns. Throughout the teaching I would assess the patients level of anxiety. I would talk about
positive coping skills and how to try to work those in to her life to prevent the anxiety from building up.
Consider the following needs:
SS Consult
Dietary Consult
PT/ OT
*Pastoral Care: could also be able to help heal patient as a whole person
Durable Medical Needs
*F/U appts for a psychologist and maybe a weekly counseling session
Med Instruction/Prescription
are any of the patients medications available at a discount pharmacy? Yes No
Rehab/ HH
Palliative Care
21
University of South Florida College of Nursing Revision April 2012
15 for Care Plan
Nursing Diagnosis: Compromised family coping r/t situational crisis the significant person may be facing aeb
husband suffering his own illness
Patient
Goals/Outcomes
Nursing Interventions
to Achieve Goal
Rationale for
Interventions
Provide References
Evaluation of
Interventions on Day
care is Provided
1. Have patient discuss her
family and support system
1.a. Determine current familial
roles.
1.b. Discuss where and when
patient feels the support is
lacking
Determining the role of the
family members can help see
where the patients support
system is.
The patient did talk about her
family with me during the shift
2. Have patient state importance
of maintaining independence in
her life.
2.a. Identify ways of
demonstrating support while
maintaining clients
independence.
2.b. Talk about areas that can
help maintain independence
(counseling, group meetings, bus
systems, etc)
It is important for the patient to
come to terms with her
independence and understand
that there are options to help
maintain the independence
Patient stated that her
independence felt threatened by
this hospitalization and her
family was not around to help
make a transition
3. Describe communication
among the family.
3.a. Find strengths and
weaknesses in family
communication.
3.b. Empower patient to not be
afraid to reach out to her family
when needed
This patient felt distanced from
her family and I believed that
focusing on familial
communication would benefit
her and maybe relieve some
anxiety.
During my time on the floor I
was not able to talk about
communication with the patient
Discharge Planning: (put a * in front of any pt education in above care plan that you would include for
discharge teaching)
Upon discharge I would make sure follow up appointments have been arrange and patient has transportation to
physician's offices. I would discuss the patients living arrangement, making sure there arent stairs and throw
rugs to minimize fall risk, and to know who lives with the patient to see if I need to include teaching with
family members. Next I would discuss the medications the patient will be going home with. I will ask about her
access to the prescriptions like cost and transportation for pick-up. I would teach her when to take medications,
what side effects to look for, when to notify her physician or come to the ER. I would ask the patient about her
questions/concerns. I would talk to patient about her ways of coping and provide some alternative coping skills
to try.
Consider the following needs:
SS Consult
Dietary Consult
PT/ OT
*Pastoral Care: could also be able to help heal patient as a whole person
Durable Medical Needs
*F/U appts for a psychologist and maybe a weekly counseling session
Med Instruction/Prescription
are any of the patients medications available at a discount pharmacy? Yes No
Rehab/ HH
Palliative Care
22
University of South Florida College of Nursing Revision April 2012
15 for Care Plan
Nursing Diagnosis: Stress overload r/t illness, coping, and helpless feelings aeb patient appearing and stating that
stress is a problem.
Patient
Goals/Outcomes
Nursing Interventions
to Achieve Goal
Rationale for
Interventions
Provide References
Evaluation of
Interventions on Day
care is Provided
1. Patient will point out daily
stressors and new stressors
1.a. Actively listen to what
stresses patient
1.b. Assist patient in minimizing
possible stressors in the hospital
setting
By acknowledging stressors, it is
easier to try to deal with them
Patient started talking about her
recurrent and new stressors
during the shift.
2. Use relaxation techniques to
cope with stress
1.a. Teach patient about certain
relaxation techniques
1.b. Learn what works for
patient.
Relaxation can help with stress,
anxiety, and other problems.
Patient relaxed with sleep,
distraction, and listening to
music during the shift
3. Patient will report feeling less
stressed during the shift.
3.a. Using relaxation techniques
and or coping skills
3.b.
I was not able to quantify this
during my shift
Discharge Planning: (put a * in front of any pt education in above care plan that you would include for
discharge teaching)
Upon discharge I would make sure follow up appointments have been arrange and patient has transportation to
physician's offices. I would discuss the patients living arrangement, making sure there arent stairs and throw
rugs to minimize fall risk, and to know who lives with the patient to see if I need to include teaching with
family members. Next I would discuss the medications the patient will be going home with. I will ask about her
access to the prescriptions like cost and transportation for pick-up. I would teach her when to take medications,
what side effects to look for, when to notify her physician or come to the ER. I would ask the patient about her
questions/concerns. I would discuss stress relieving techniques like deep breathing, relaxation, and music
therapy. I would also talk about coping skills and how to use these skills to minimize stress overload.
Consider the following needs:
SS Consult
Dietary Consult
PT/ OT
*Pastoral Care: could also be able to help heal patient as a whole person
Durable Medical Needs
*F/U appts for a psychologist and maybe a weekly counseling session
Med Instruction/Prescription
are any of the patients medications available at a discount pharmacy? Yes No
Rehab/ HH
Palliative Care
You might also like
- Remote DepossessionDocument168 pagesRemote DepossessionMuhammad Ali100% (9)
- Pat 2 Medsurg1Document20 pagesPat 2 Medsurg1api-300849832No ratings yet
- Deepeners - Everything You Want To Know About HypnosisDocument8 pagesDeepeners - Everything You Want To Know About HypnosisarbetaNo ratings yet
- The Book of KnowledgeDocument113 pagesThe Book of Knowledgefever14345100% (4)
- Workbook 2003 AnxietyDocument64 pagesWorkbook 2003 Anxietysherell220100% (5)
- MPT Inter Test 4 PDFDocument5 pagesMPT Inter Test 4 PDFmalgorzata0% (1)
- Pat FundamentalsDocument14 pagesPat Fundamentalsapi-281676750No ratings yet
- Pat Med Surg 1Document22 pagesPat Med Surg 1api-324658071No ratings yet
- Pat 11052014Document18 pagesPat 11052014api-300362983No ratings yet
- Final PatDocument22 pagesFinal Patapi-259394980No ratings yet
- Pat Revised 2013 1Document19 pagesPat Revised 2013 1api-300362033No ratings yet
- Pat 1 Medsurg 2Document18 pagesPat 1 Medsurg 2api-294300618No ratings yet
- Pat PortfolioDocument20 pagesPat Portfolioapi-300861055No ratings yet
- Pat Revised 9-2014 FundamentalsDocument17 pagesPat Revised 9-2014 Fundamentalsapi-300362033No ratings yet
- Med Surg 1 PatDocument20 pagesMed Surg 1 Patapi-301978768No ratings yet
- Pat Semester 1Document17 pagesPat Semester 1api-300946501No ratings yet
- Pat 2 Med SurgDocument18 pagesPat 2 Med Surgapi-316861395No ratings yet
- Portfolio Pat 3Document19 pagesPortfolio Pat 3api-300861055No ratings yet
- Msii Pat 2Document22 pagesMsii Pat 2api-300946501No ratings yet
- Pat1 Med Surg 1Document19 pagesPat1 Med Surg 1api-339132978No ratings yet
- Ms 1 PatDocument19 pagesMs 1 Patapi-281676750No ratings yet
- Case StudyDocument9 pagesCase StudyJayr MartinNo ratings yet
- Pat FundamentalsDocument16 pagesPat Fundamentalsapi-339980385No ratings yet
- Pat II MedsurgDocument19 pagesPat II Medsurgapi-301881424No ratings yet
- Patient Assessment Tool ms2Document27 pagesPatient Assessment Tool ms2api-280998981No ratings yet
- Ms 2 Pat MaffettDocument20 pagesMs 2 Pat Maffettapi-339784339No ratings yet
- Pat FinalDocument20 pagesPat Finalapi-259267079No ratings yet
- Pat 1 2015Document18 pagesPat 1 2015api-315192697No ratings yet
- Pat 2 - Med SurgDocument21 pagesPat 2 - Med Surgapi-315731045No ratings yet
- Jones PatDocument16 pagesJones Patapi-301978768No ratings yet
- Pat Fall 2014Document21 pagesPat Fall 2014api-288536467No ratings yet
- Pat Semester 2Document27 pagesPat Semester 2api-300946501No ratings yet
- Pat Revised 2013 1Document18 pagesPat Revised 2013 1api-324886317No ratings yet
- Pat 2Document21 pagesPat 2api-270783686No ratings yet
- Pat Fall 2014Document17 pagesPat Fall 2014api-300849832No ratings yet
- Case StudyDocument3 pagesCase StudyAngelica Joyce SinnacoNo ratings yet
- Fundamentals PatDocument20 pagesFundamentals Patapi-340247560No ratings yet
- Case StudyDocument9 pagesCase StudyEko CecogoNo ratings yet
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocument20 pagesUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-300454618No ratings yet
- Pat DHDocument17 pagesPat DHapi-283153247No ratings yet
- Pat 2 Medsurg 2Document22 pagesPat 2 Medsurg 2api-315731045No ratings yet
- Shelf IM Patient NotesDocument6 pagesShelf IM Patient NotesRuth SanmooganNo ratings yet
- Monek Case StudyDocument24 pagesMonek Case StudyashnairafatimamaulanaNo ratings yet
- Fundamentals Pat Part 3 - Dean GradedDocument22 pagesFundamentals Pat Part 3 - Dean Gradedapi-252790184No ratings yet
- Chronic Illness: Group 5Document17 pagesChronic Illness: Group 5SelwynVillamorPatenteNo ratings yet
- Pat ms1Document19 pagesPat ms1api-301120253No ratings yet
- Pat 2014Document20 pagesPat 2014api-324658071No ratings yet
- Pat 2 sd-1Document22 pagesPat 2 sd-1api-283672381No ratings yet
- Fluphenazine Decanoate RBMDocument9 pagesFluphenazine Decanoate RBMMustika OktariniNo ratings yet
- Pat 2Document20 pagesPat 2api-300362983No ratings yet
- SOAP - Case Study FormatsDocument8 pagesSOAP - Case Study FormatsDr-Sanjay SinghaniaNo ratings yet
- Pat Ms IIDocument18 pagesPat Ms IIapi-339980385No ratings yet
- MH Case StudyDocument17 pagesMH Case StudyS. JacobsNo ratings yet
- Pat Spring Ms II 2015Document16 pagesPat Spring Ms II 2015api-315435865No ratings yet
- Pat 2Document18 pagesPat 2api-273138891No ratings yet
- Fibromyalgia A Clinical ReviewDocument9 pagesFibromyalgia A Clinical ReviewastrogliaNo ratings yet
- 3 HPLCDocument9 pages3 HPLClorrainebarandonNo ratings yet
- University of South Florida College of Nursing: Fundamental Patient Assessment ToolDocument18 pagesUniversity of South Florida College of Nursing: Fundamental Patient Assessment Toolapi-315731045No ratings yet
- Patsummersemester2015 Anjouligerez-2Document21 pagesPatsummersemester2015 Anjouligerez-2api-325112936No ratings yet
- 6635 NRNP and PRAC Comprehensive Psychiatric EvaluationDocument5 pages6635 NRNP and PRAC Comprehensive Psychiatric EvaluationMarieamme BinaleNo ratings yet
- Literature Review: Parental Refusal of Childhood Vaccinations TonsillectomyDocument2 pagesLiterature Review: Parental Refusal of Childhood Vaccinations TonsillectomyilldoitNo ratings yet
- Pat FinalDocument24 pagesPat Finalapi-252804976No ratings yet
- Soap Note1 - Gyn ComplaintDocument6 pagesSoap Note1 - Gyn Complaintapi-482726932100% (3)
- The Best Practice Is The Lowest Effective Dose Your Third Psychiatric Consultation: Diet, Exercise, and Sleep Trump Medications Medication is the Last Option Your Fourth Psychiatric ConsultationFrom EverandThe Best Practice Is The Lowest Effective Dose Your Third Psychiatric Consultation: Diet, Exercise, and Sleep Trump Medications Medication is the Last Option Your Fourth Psychiatric ConsultationNo ratings yet
- Acharya Masterclass Work BookDocument9 pagesAcharya Masterclass Work BookAnjaniSwethaAnanthapalliNo ratings yet
- Family Coping Index..Document3 pagesFamily Coping Index..Lharra Cagulada-PostranoNo ratings yet
- What Is Qigong 2023Document40 pagesWhat Is Qigong 2023JinadNo ratings yet
- Resoucalm Mindrce Cheat SheetDocument5 pagesResoucalm Mindrce Cheat SheetnihadNo ratings yet
- Energy Healing Hand Positions Mudra CourseDocument36 pagesEnergy Healing Hand Positions Mudra Courseraluuuu2No ratings yet
- Implementation and Intervension (English)Document9 pagesImplementation and Intervension (English)Devi SitudewiNo ratings yet
- What Is Swar VigyanDocument28 pagesWhat Is Swar VigyanNarendra BhogalNo ratings yet
- Deep Breathing ExercisesDocument17 pagesDeep Breathing ExercisesPamela Warner100% (1)
- Working With Older AdultsDocument84 pagesWorking With Older AdultsdarketaNo ratings yet
- Stress, Relaxation States, and CreativityDocument8 pagesStress, Relaxation States, and CreativitySoumitra KunduNo ratings yet
- Improving Creativity For EngineersDocument32 pagesImproving Creativity For EngineersVenkatesh100% (1)
- Self Management SkillsDocument7 pagesSelf Management SkillsAnuj HalderNo ratings yet
- Dialogue (Siti Sabrina, Mita Azani)Document2 pagesDialogue (Siti Sabrina, Mita Azani)mita yuliantiNo ratings yet
- LS5 Managing Emotions and Impulses Activity SheetDocument19 pagesLS5 Managing Emotions and Impulses Activity SheetJocelene Zamora Parungao100% (2)
- Fatigue Related To Autoimmune Disease As Evidenced by Patient Inability To Maintain Usual Level of Physical ActivityDocument5 pagesFatigue Related To Autoimmune Disease As Evidenced by Patient Inability To Maintain Usual Level of Physical ActivityJordz PlaciNo ratings yet
- William G. Braud - Human Interconnectedness: Research IndicationsDocument22 pagesWilliam G. Braud - Human Interconnectedness: Research IndicationsFlikk34100% (1)
- Orgone Energy Info PackDocument39 pagesOrgone Energy Info Packimparante100% (2)
- Assignment-Specific Stress Inoculation Training For Highly Specialized IT PersonnelDocument7 pagesAssignment-Specific Stress Inoculation Training For Highly Specialized IT PersonnelbijsshrjournalNo ratings yet
- Top 10 Benefits of Exercising DailyDocument2 pagesTop 10 Benefits of Exercising DailyRicha VermaNo ratings yet
- Journal of Interprofessional Education & Practice: Kristine Wood, Carolanne CariniDocument4 pagesJournal of Interprofessional Education & Practice: Kristine Wood, Carolanne CariniNatalia BettancourtNo ratings yet
- Exercises For The Master Key: by Charles F. HaanelDocument9 pagesExercises For The Master Key: by Charles F. HaanelPradeep Uday K UNo ratings yet
- Plan de Lectie Unit 5 IntermediateDocument2 pagesPlan de Lectie Unit 5 IntermediateRaluca MotreanuNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument19 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaARJUN BNo ratings yet
- The Little Bowen BookDocument80 pagesThe Little Bowen BookJeremy Monroe100% (6)
- BreathhhhhDocument16 pagesBreathhhhhMOULIANNA8949100% (1)