Professional Documents
Culture Documents
WHO - Pregnancy, Childbirth, Postpartum and Newborn Care
WHO - Pregnancy, Childbirth, Postpartum and Newborn Care
Uploaded by
liska ramdanawatiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WHO - Pregnancy, Childbirth, Postpartum and Newborn Care
WHO - Pregnancy, Childbirth, Postpartum and Newborn Care
Uploaded by
liska ramdanawatiCopyright:
Available Formats
Department of Making Pregnancy Safer
2
n
d
E
d
i
t
i
o
n
Integrated Management of Pregnancy and Childbirth
Pregnancy, Childbirth, Postpartum and Newborn Care:
A guide for essential practice
World Health Organization
Geneva
2006
WHO Library Cataloguing-in-Publication Data
Pregnancy, childbirth, postpartum and newborn care : a guide for essential practice.
At head of title: Integrated Management of Pregnancy and Childbirth.
1.Labor, Obstetric 2.Delivery, Obstetric 3.Prenatal care 4.Perinatal care
methods 5.Postnatal care - methods 6.Pregnancy complications - diagnosis
7.Pregnancy complications - therapy 8.Manuals I.World Health Organization.
ISBN 92 4 159084 X (NLM classification: WQ 175)
First edition 2003
Second edition 2006
Reprinted with changes 2009
World Health Organization 2006
All rights reserved. Publications of the World Health Organization can be obtained from
Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27,
Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: bookorders@who.int).
Requests for permission to reproduce or translate WHO publications whether for sale or
for noncommercial distribution should be addressed to Publications, at the above address
(fax: +41 22 791 4806; email: permissions@who.int).
The designations employed and the presentation of the material in this publication
do not imply the expression of any opinion whatsoever on the part of the World Health
Organization concerning the legal status of any country, territory, city or area or of its
authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on
maps represent approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers products does not imply
that they are endorsed or recommended by the World Health Organization in preference
to others of a similar nature that are not mentioned. Errors and omissions excepted, the
names of proprietary products are distinguished by initial capital letters.
The World Health Organization does not warrant that the information contained in this
publication is complete and correct and shall not be liable for any damages incurred as
a result of its use.
Printed in India
Foreword
F
O
R
E
W
O
R
D
In modern times, improvements in knowledge and technological advances have greatly improved the
health of mother and children. However, the past decade was marked by limited progress in reducing
maternal mortality and a slow-down in the steady decline of childhood mortality observed since the
mid 1950s in many countries, the latter being largely due to a failure to reduce neonatal mortality.
Every year, over four million babies less than one month of age die, most of them during the critical
first week of life; and for every newborn who dies, another is stillborn. Most of these deaths are a
consequence of the poor health and nutritional status of the mother coupled with inadequate care
before, during, and after delivery. Unfortunately, the problem remains unrecognized or- worse- accepted
as inevitable in many societies, in large part because it is so common.
Recognizing the large burden of maternal and neonatal ill-health on the development capacity of
individuals, communities and societies, world leaders reaffirmed their commitment to invest in mothers
and children by adopting specific goals and targets to reduce maternal and childhood-infant mortality
as part of the Millennium Declaration.
There is a widely shared but mistaken idea that improvements in newborn health require sophisticated
and expensive technologies and highly specialized staff. The reality is that many conditions that result
in perinatal death can be prevented or treated without sophisticated and expensive technology. What
is required is essential care during pregnancy, the assistance of a person with midwifery skills during
childbirth and the immediate postpartum period, and a few critical interventions for the newborn
during the first days of life.
It is against this background that we are proud to present the document Pregnancy, Childbirth,
Postpartum and Newborn Care: A guide for essential practice, as new additions to the Integrated
Management of Pregnancy and Childbirth tool kit. The guide provides a full range of updated,
evidence-based norms and standards that will enable health care providers to give high quality care
during pregnancy, delivery and in the postpartum period, considering the needs of the mother and her
newborn baby.
We hope that the guide will be helpful for decision-makers, programme managers and health care
providers in charting out their roadmap towards meeting the health needs of all mothers and children.
We have the knowledge, our major challenge now is to translate this into action and to reach those
women and children who are most in need.
Dr. Tomris Trmen
Executive director
Family and Community Health (FCH)
FOREWORD
A
C
K
N
O
W
L
E
D
G
E
M
E
N
T
S
The Guide was prepared by a team of the World Health Organization, Department of Reproductive
Health and Research (RHR), led by Jerker Liljestrand and Jelka Zupan.
The concept and first drafts were developed by Sandra Gove and Patricia Whitesell/ACT International,
Atlanta, Jerker Liljestrand, Denise Roth, Betty Sweet, Anne Thompson, and Jelka Zupan.
Revisions were subsequently carried out by Annie Portela, Luc de Bernis, Ornella Lincetto, Rita Kabra,
Maggie Usher, Agostino Borra, Rick Guidotti, Elisabeth Hoff, Mathews Matthai, Monir Islam,
Felicity Savage, Adepeyu Olukoya, Aafje Rietveld, TinTin Sint, Ekpini Ehounu, Suman Mehta.
Valuable inputs were provided by WHO Regional Offices and WHO departments:
Reproductive Health and Research
Child and Adolescent Health and Development
HIV/AIDS
Communicable Diseases
Nutrition for Health and Development
Essential Drugs and Medicines Policy
Vaccines and Biologicals
Mental Health and Substance Dependence
Gender and Womens Health
Blindness and Deafness
Editing: Nina Mattock, Richard Casna
Layout: rsdesigns.com srl
Cover design: Mare N Mhearin
WHO acknowledges with gratitude the generous contribution of over 100 individuals and organizations
in the field of maternal and newborn health, who took time to review this document at different stages
of its development. They came from over 35 countries and brought their expertise and wide experience
to the final text.
This guide represents a common understanding between WHO, UNFPA, UNICEF, and the World Bank
of key elements of an approach to reducing maternal and perinatal mortality and morbidity. These
agencies co-operate closely in efforts to reduce maternal and perinatal mortality and morbidity.
The principles and policies of each agency are governed by the relevant decisions of each agencys
governing body and each agency implements the interventions described in this document in
accordance with these principles and policies and within the scope of its mandate.
The guide has also been reviewed and endorsed by the International Confederation of Midwives, the
International Federation of Gynecology and Obstetrics and International Pediatric Association.
The financial support towards the preparation and production of this document provided by UNFPA and
the Governments of Australia, Japan and the United States of America is gratefully acknowledged,
as is financial support received from The World Bank. In addition, WHOs Making Pregnancy Safer
initiative is grateful to the programme support received from the Governments of the Netherlands,
Norway, Sweden and the United Kingdom of Great Britain and Northern Ireland.
Acknowledgements
ACKNOWLEDGEMENTS
International
Pediatric Association
International
Confederation of Midwives
International Federation of
Gynecology and Obstetrics
Table of contents
T
A
B
L
E
O
F
C
O
N
T
E
N
T
S
TABLE OF CONTENTS
A
INTRODUCTION
Introduction
How to read the Guide
Acronyms
Content
Structure and presentation
Assumptions underlying the guide
A
PRINCIPLES OF GOOD CARE
A2 Communication
A3 Workplace and administrative procedures
A4 Standard precautions and cleanliness
A5 Organising a visit
B
QUICK CHECK, RAPID ASSESSMENT AND MANAGEMENT OF WOMEN OF CHILDBEARING AGE
B2 Quick check
B3-B7 Rapid assessment and management
B3 Airway and breathing
B3 Circulation (shock)
B4-B5 Vaginal bleeding
B6 Convulsions or unconscious
B6 Severe abdominal pain
B6 Dangerous fever
B7 Labour
B7 Other danger signs or symptoms
B7 If no emergency or priority signs, non urgent
B
EMERGENCY TREATMENTS FOR THE WOMAN
B9 Airway, breathing and circulation
B9 Manage the airway and breathing
B9 Insert IV line and give fluids
B9 If intravenous access not possible
B10-B12 Bleeding
B10 Massage uterus and expel clots
B10 Apply bimanual uterine compression
B10 Apply aortic compression
B10 Give oxytocin
B10 Give ergometrine
B11 Remove placenta and fragments manually
B11 After manual removal of placenta
B12 Repair the tear and empty bladder
B12 Repair the tear or episiotomy
B13-B14 Important considerations in caring for a woman with eclampsia or pre-eclampsia
B13 Give magnesium sulphate
B13 Important considerations in caring for a woman with eclampsia
B14 Give diazepam
B14 Give appropriate antihypertensive drug
B15 Infection
B15 Give appropriate IV/IM antibiotics
B16 Malaria
B16 Give arthemether or quinine IM
B16 Give glucose IV
B17 Refer the woman urgently to the hospital
B17 Essential emergency drugs and supplies for transport and home delivery
B
BLEEDING IN EARLY PREGNANCY AND POST-ABORTION CARE
B19 Examination of the woman with bleeding in early pregnancy and post-abortion care
B20 Give preventive measures
B21 Advise and counsel on post-abortion care
B21 Advise on self-care
B21 Advise and counsel on family planning
B21 Provide information and support after abortion
B21 Advise and counsel during follow-up visits
Table of contents
T
A
B
L
E
O
F
C
O
N
T
E
N
T
S
C
ANTENATAL CARE
C2 Assess the pregnant woman: pregnancy status, birth and emergency plan
C3 Check for pre-eclampsia
C4 Check for anaemia
C5 Check for syphilis
C6 Check for HIV status
C7 Respond to observed signs or volunteered problems
C7 If no fetal movement
C7 If ruptured membranes and no labour
C8 If fever or burning on urination
C9 If vaginal discharge
C10 If signs suggesting HIV infection
C10 If smoking, alcohol or drug abuse, or history of violence
C11 If cough or breathing difficulty
C11 If taking antituberculosis drugs
C12 Give preventive measures
C13 Advise and counsel on nutrition and self-care
C14-C15 Develop a birth and emergency plan
C14 Facility delivery
C14 Home delivery with a skilled attendant
C15 Advise on labour signs
C15 Advise on danger signs
C15 Discuss how to prepare for an emergency in pregnancy
C16 Advise and counsel on family planning
C16 Counsel on the importance of family planning
C16 Special consideration for family planning counselling during pregnancy
C17 Advise on routine and follow-up visits
C18 Home delivery without a skilled attendant
C19 Assess eligibility of ARV for HIV-positive pregnant woman
D
CHILDBIRTH LABOUR, DELIVERY AND IMMEDIATE POSTPARTUM CARE
D2 Examine the woman in labour or with ruptured membranes
D3 Decide stage of labour
D4-D5 Respond to obstetrical problems on admission
D6-D7 Give supportive care throughout labour
D6 Communication
D6 Cleanliness
D6 Mobility
D6 Urination
D6 Eating, drinking
D6 Breathing technique
D6 Pain and discomfort relief
D7 Birth companion
D8-D9 First stage of labour
D8 Not in active labour
D9 In active labour
D10-D11 Second stage of labour: deliver the baby and give immediate newborn care
D12-D13 Third stage of labour: deliver the placenta
D14-D18 Respond to problems during labour and delivery
D14 If fetal heart rate <120 or >160 beats per minute
D15 If prolapsed cord
D16 If breech presentation
D17 If stuck shoulders (Shoulder dystocia)
D18 If multiple births
D19 Care of the mother and newborn within first hour of delivery of placenta
D20 Care of the mother one hour after delivery of placenta
D21 Assess the mother after delivery
D22-D25 Respond to problems immediately postpartum
D22 If vaginal bleeding
D22 If fever (temperature >38C)
D22 If perineal tear or episiotomy (done for lifesaving circumstances)
D23 If elevated diastolic blood pressure
D24 If pallor on screening, check for anaemia
D24 If mother severely ill or separated from the child
D24 If baby stillborn or dead
D25 Give preventive measures
Table of contents
T
A
B
L
E
O
F
C
O
N
T
E
N
T
S
D
CHILDBIRTH LABOUR, DELIVERY AND IMMEDIATE POSTPARTUM CARE (CONTINUED)
D26 Advise on postpartum care
D26 Advise on postpartum care and hygiene
D26 Counsel on nutrition
D27 Counsel on birth spacing and family planning
D27 Counsel on the importance of family planning
D27 Lactation amenorrhea method (LAM)
D28 Advise on when to return
D28 Routine postpartum visits
D28 Follow-up visits for problems
D28 Advise on danger signs
D28 Discuss how to prepare for an emergency in postpartum
D29 Home delivery by skilled attendant
D29 Preparation for home delivery
D29 Delivery care
D29 Immediate postpartum care of mother
D29 Postpartum care of newborn
E
POSTPARTUM CARE
E2 Postpartum examination of the mother (up to 6 weeks)
E3-E10 Respond to observed signs or volunteered problems
E3 If elevated diastolic blood pressure
E4 If pallor, check for anaemia
E5 Check for HIV status
E6 If heavy vaginal bleeding
E6 If fever or foul-smelling lochia
E7 If dribbling urine
E7 If pus or perineal pain
E7 If feeling unhappy or crying easily
E8 If vaginal discharge 4 weeks after delivery
E8 If breast problem
E9 If cough or breathing difficulty
E9 If taking anti-tuberculosis drugs
E10 If signs suggesting HIV infection
F
PREVENTIVE MEASURES AND ADDITIONAL TREATMENTS FOR THE WOMAN
F2F4 Preventive measures
F2 Give tetanus toxoid
F2 Give vitamin A postpartum
F3 Give iron and folic acid
F3 Give mebendazole
F3 Motivate on compliance with iron treatment
F4 Give preventive intermittent treatment for falciparum malaria
F4 Advise to use insecticide-treated bednet
F4 Give appropriate oral antimalarial treatment
F4 Give paracetamol
F5F6 Additional treatments for the woman
F5 Give appropriate oral antibiotics
F6 Give benzathine penicillin IM
F6 Observe for signs of allergy
Table of contents
T
A
B
L
E
O
F
C
O
N
T
E
N
T
S
G
INFORM AND COUNSEL ON HIV
G2 Provide key information on HIV
G2
What is HIV and how is HIV transmitted?
G2 Advantage of knowing the HIV status in pregnancy
G2 Counsel on safer sex including use of condoms
G3 HIV testing and counselling
G3 HIV testing and counselling
G3 Discuss confidentiality of HIV infection
G3 Counsel on implications of the HIV test result
G3 Benefits of disclosure (involving) and testing the male partner(s)
G4 Care and counselling for the HIV -positive woman
G4 Additional care for the HIV -positive woman
G4 Counsel the HIV -positive woman on family planning
G5 Support to the HIV-positive woman
G5 Provide emotional support to the woman
G5 How to provide support
G6 Give antiretroviral (ARV) medicine(s) to treat HIV infection
G6 Support the initiation of ARV
G6 Support adherence to ARV
G7 Counsel on infant feeding options
G7 Explain the risks of HIV transmission through breastfeeding and not breastfeeding
G7 If a woman does not know her HIV status
G7 If a woman knows that she is HIV positive
G8 Support the mothers choice of newborn feeding
G8 If mother chooses replacement feeding : teach her replacement feeding
G8 Explain the risks of replacement feeding
G8 Follow-up for replacement feeding
G8 Give special counselling to the mother who is HIV-positive and chooses breastfeeding
G9 Give appropriate antiretroviral to HIV- positive woman and the newborn
G10 Respond to observed signs and volunteered problems
G10 If a woman is taking Antiretroviral medicines and develop new signs/symptoms, respond to
her problems
G11 Prevent HIV infection in health care workers after accidental exposure with body fluids (post
exposure prophylaxis)
G11 If a health care worker is exposed to body fluids by cuts/pricks/ splashes, give him
appropriate care.
H
THE WOMAN WITH SPECIAL NEEDS
H2 Emotional support for the woman with special needs
H2 Sources of support
H2 Emotional support
H3 Special considerations in managing the pregnant adolescent
H3 When interacting with the adolescent
H3 Help the girl consider her options and to make decisions which best suit her needs
H4 Special considerations for supporting the woman living with violence
H4 Support the woman living with violence
H4 Support the health service response to needs of women living with violence
I
COMMUNITY SUPPORT FOR MATERNAL AND NEWBORN HEALTH
I2 Establish links
I2 Coordinate with other health care providers and community groups
I2 Establish links with traditional birth attendants and traditional healers
I3 Involve the community in quality of services
Table of contents
T
A
B
L
E
O
F
C
O
N
T
E
N
T
S
J
NEWBORN CARE
J2 Examine the newborn
J3 If preterm, birth weight <2500 g or twin
J4 Assess breastfeeding
J5 Check for special treatment needs
J6 Look for signs of jaundice and local infection
J7 If danger signs
J8 If swelling, bruises or malformation
J9 Assess the mothers breasts if complaining of nipple or breast pain
J10 Care of the newborn
J11 Additional care of a small baby (or twin)
J12 Assess replacement feeding
K
BREASTFEEDING, CARE, PREVENTIVE MEASURES AND TREATMENT FOR THE NEWBORN
K2 Counsel on breastfeeding
K2 Counsel on importance of exclusive breastfeeding
K2 Help the mother to initiate breastfeeding
K3 Support exclusive breastfeeding
K3 Teach correct positioning and attachment for breastfeeding
K4 Give special support to breastfeed the small baby (preterm and/or low birth weight)
K4 Give special support to breastfeed twins
K5 Alternative feeding methods
K5 Express breast milk
K5 Hand express breast milk directly into the babys mouth
K6 Cup feeding expressed breast milk
K6 Quantity to feed by cup
K6 Signs that baby is receiving adequate amount of milk
K7 Weigh and assess weight gain
K7 Weigh baby in the first month of life
K7 Assess weight gain
K7 Scale maintenance
K8 Other breastfeeding support
K8 Give special support to the mother who is not yet breastfeeding
K8 If the baby does not have a mother
K8 Advise the mother who is not breastfeeding at all on how to relieve engorgement
K9 Ensure warmth for the baby
K9 Keep the baby warm
K9 Keep a small baby warm
K9 Rewarm the baby skin-to-skin
K10 Other baby care
K10 Cord care
K10 Sleeping
K10 Hygiene
K11 Newborn resuscitation
K11 Keep the baby warm
K11 Open the airway
K11 If still not breathing, ventilate
K11 If breathing less than 30 breaths per minute or severe chest in-drawing, stop ventilating
K11 If not breathing or gasping at all after 20 minutes of ventilation
K12 Treat and immunize the baby
K12 Treat the baby
K12 Give 2 IM antibiotics (first week of life)
K12 Give IM benzathine penicillin to baby (single dose) if mother tested RPR-positive
K12 Give IM antibiotic for possible gonococcal eye infection (single dose)
K13 Teach the mother to give treatment to the baby at home
K13 Treat local infection
K13 Give isoniazid (INH) prophylaxis to newborn
K13 Immunize the newborn
K13 Give antiretroviral (ARV) medicine to newborn
K14 Advise when to return with the baby
K14 Routine visits
K14 Follow-up visits
K14 Advise the mother to seek care for the baby
K14 Refer baby urgently to hospital
Table of contents
T
A
B
L
E
O
F
C
O
N
T
E
N
T
S
L
EQUIPMENT, SUPPLIES, DRUGS AND LABORATORY TESTS
L2 Equipment, supplies, drugs and tests for pregnancy and postpartum care
L3 Equipment, supplies and drugs for childbirth care
L4 Laboratory tests
L4 Check urine for protein
L4 Check haemoglobin
L5 Perform rapid plamareagin (RPR) test for syphilis
L5 Interpreting results
L6 Perform rapid test for HIV
M
INFORMATION AND COUNSELLING SHEETS
M2 Care during pregnancy
M3 Preparing a birth and emergency plan
M4 Care for the mother after birth
M5 Care after an abortion
M6 Care for the baby after birth
M7 Breastfeeding
M8-M9 Clean home delivery
N
RECORDS AND FORMS
N2 Referral record
N3 Feedback record
N4 Labour record
N5 Partograph
N6 Postpartum record
N7 International form of medical certificate of cause of death
O
GLOSSARY AND ACRONYMS
The aim of Pregnancy, childbirth, postpartum and newborn care guide for essential practice (PCPNC) is
to provide evidence-based recommendations to guide health care professionals in the management of
women during pregnancy, childbirth and postpartum, and post abortion, and newborns during their first
week of life, including management of endemic diseases like malaria, HIV/AIDS, TB and anaemia.
All recommendations are for skilled attendants working at the primary level of health care, either at the
facility or in the community. They apply to all women attending antenatal care, in delivery, postpartum
or post abortion care, or who come for emergency care, and to all newborns at birth and during the first
week of life (or later) for routine and emergency care.
The PCPNC is a guide for clinical decision-making. It facilitates the collection, analysis, classification and
use of relevant information by suggesting key questions, essential observations and/or examinations,
and recommending appropriate research-based interventions. It promotes the early detection of
complications and the initiation of early and appropriate treatment, including timely referral, if
necessary.
Correct use of this guide should help reduce the high maternal and perinatal mortality and morbidity
rates prevalent in many parts of the developing world, thereby making pregnancy and childbirth safer.
The guide is not designed for immediate use. It is a generic guide and should first be adapted to
local needs and resources. It should cover the most serious endemic conditions that the skilled birth
attendant must be able to treat, and be made consistent with national treatment guidelines and other
policies. It is accompanied by an adaptation guide to help countries prepare their own national guides
and training and other supporting materials.
The first section, How to use the guide, describes how the guide is organized, the overall content and
presentation. Each chapter begins with a short description of how to read and use it, to help the
reader use the guide correctly.
The Guide has been developed by the Department of Reproductive Health and Research with
contributions from the following WHO programmes:
Child and Adolesscent Health and Development
HIV/AIDS
Nutrition for Health and Development
Essential drugs and Medicines Policy
Vaccines and Biologicals
Communicable Diseases Control, Prevention and Eradication (tuberculosis, malaria, helminthiasis)
Gender and Womens Health
Mental Health and Substance Dependence
Blindness and Deafness
INTRODUCTION
I
N
T
R
O
D
U
C
T
I
O
N
Introduction
How to read the guide
H
O
W
T
O
R
E
A
D
T
H
E
G
U
I
D
E
Content
The Guide includes routine and emergency care
for women and newborns during pregnancy,
labour and delivery, postpartum and post
abortion, as well as key preventive measures
required to reduce the incidence of endemic and
other diseases like malaria, anaemia, HIV/AIDS
and TB, which add to maternal and perinatal
morbidity and mortality.
Most women and newborns using the services
described in the Guide are not ill and/or do not
have complications. They are able to wait in line
when they come for a scheduled visit. However,
the small proportion of women/newborns who
are ill, have complications or are in labour, need
urgent attention and care.
The clinical content is divided into six sections
which are as follows:
Quick check (triage), emergency management
(called Rapid Assessment and Management
or RAM) and referral, followed by a chapter on
emergency treatments for the woman.
Post-abortion care.
Antenatal care.
Labour and delivery.
Postpartum care.
Newborn care.
In each of the six clinical sections listed
above there is a series of flow, treatment and
information charts which include:
Guidance on routine care, including
monitoring the well-being of the mother and/
or baby.
Early detection and management of
complications.
Preventive measures.
Advice and counselling.
In addition to the clinical care outlined above,
other sections in the guide include:
Advice on HIV, prevention and treatment.
Support for women with special needs.
Links with the community.
Drugs, supplies, equipment, universal
precautions and laboratory tests.
Examples of clinical records.
Counselling and key messages for women and
families.
There is an important section at the beginning
of the Guide entitled Principles of good care
A1-A5 . This includes principles of good care
for all women, including those with special
needs. It explains the organization of each
visit to a healthcare facility, which applies to
overall care. The principles are not repeated
for each visit.
Recommendations for the management of
complications at secondary (referral)
health care level can be found in the following
guides for midwives and doctors:
Managing complications of pregnancy and
childbirth (WHO/RHR/00.7)
Managing newborn problems.
Documents referred to in this Guide can be
obtained from the Department of Making
Pregnancy Safer, Family and Community Health,
World Health Organization, Geneva, Switzerland.
E-mail: mpspublications@who.int.
Other related WHO documents can be
downloaded from the following links:
Medical Eligibility Criteria 3rd edition:
http://www.who.int/reproductive-health/
publications/mec/mec.pdf.
Selected Practice Recommendations 2nd
edition: http://www.who.int/reproductive-
health/publications/spr/spr.pdf.
Guidelines for the Management of Sexually
Transmitted Infections: http://www.who.
int/reproductive-health/publications/
rhr_01_10_mngt_stis/guidelines_mngt_stis.
pdf
Sexually Transmitted and other Reproductive
Tract Infections: A Guide to Essential Practice:
http://www.who.int/reproductive-health/
publications/rtis_gep/rtis_gep.pdf
Antiretroviral treatment of HIV infection in
infants and children in resource-limited
settings, towards universal access:
Recommendations for a public health
approach Web-based public review,
312 November 2005
http://www.who.int/hiv/pub/prev_care/en
WHO consultation on technical and
operational recommendations for scale-up
of laboratory services and monitoring HIV
antiretroviral therapy in resource-limited
settings. http://www.who.int/hiv/pub/prev_
care/en ISBN 92 4 159368 7
Malaria and HIV Interactions and their
Implications for Public Health Policy.
http://www.who.int/hiv/pub/prev_care/en:
ISNB 92 4 159335 0
Interim WHO clinical staging of HIV/AIDS and
HIV/AIDS case definitions for surveillance
African Region. http://www.who.int/hiv/pub/
prev_care/en Ref no:: WHO/HIV/2005.02
HIV and Infant Feeding. Guidelines for
decision-makers http://www.who.int/child-
adolescent-health/publications/NUTRITION/
ISBN_92_4_159122_6.htm
HIV and Infant Feeding. A guide for health-care
managers and supervisors http://www.who.
int/child-adolescent-health/publications/
NUTRITION/ISBN_92_4_159123_4.htm
Integrated Management of Adolescent and
adult illness
http://www.who.int/3by5/publications/
documents/imai/en/index.html
HOW TO READ THE GUIDE
Structure and presentation
H
O
W
T
O
R
E
A
D
T
H
E
G
U
I
D
E
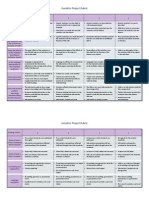
ASK, CHECK RECORD LOOK, LISTEN FEEL SIGNS TREAT AND ADVISE CLASSIFY
1
2
3
4 5
6
7
8
This Guide is a tool for clinical decision-making.
The content is presented in a frame work of
coloured flow charts supported by information
and treatment charts which give further details
of care.
The framework is based on a syndromic
approach whereby the skilled attendant
identifies a limited number of key clinical signs
and symptoms, enabling her/him to classify
the condition according to severity and give
appropriate treatment. Severity is marked in
colour: red for emergencies, yellow for less
urgent conditions which nevertheless need
attention, and green for normal care.
Flow charts
The flow charts include the following information:
1. Key questions to be asked.
2. Important observations and examinations to
be made.
3. Possible findings (signs) based on information
elicited from the questions, observations and,
where appropriate, examinations.
4. Classification of the findings.
5. Treatment and advice related to the signs and
classification.
Treat, advise means giving the treatment indicated
(performing a procedure, prescribing drugs or other
treatments, advising on possible side-effects and how to
overcome them) and giving advice on other important
practices. The treat and advise column is often cross-
referenced to other treatment and/or information charts.
Turn to these charts for more information.
Use of colour
Colour is used in the flow charts to indicate the
severity of a condition.
6. Green usually indicates no abnormal
condition and therefore normal care is given,
as outlined in the guide, with appropriate
advice for home care and follow up.
7. Yellow indicates that there is a problem that
can be treated without referral.
8. Red highlights an emergency which requires
immediate treatment and, in most cases,
urgent referral to a higher level health facility.
Key sequential steps
The charts for normal and abnormal deliveries
are presented in a framework of key sequential
steps for a clean safe delivery. The key sequential
steps for delivery are in a column on the left side
of the page, while the column on the right has
interventions which may be required if problems
arise during delivery. Interventions may be linked
to relevant treatment and/or information pages,
and are cross-referenced to other parts of the
Guide.
Treatment and information pages
The flow charts are linked (cross-referenced) to
relevant treatment and/or information pages in other
parts of the Guide. These pages include information
which is too detailed to include in the flow charts:
Treatments.
Advice and counselling.
Preventive measures.
Relevant procedures.
Information and counselling
sheets
These contain appropriate advice and
counselling messages to provide to the woman,
her partner and family. In addition, a section is
included at the back of the Guide to support the
skilled attendant in this effort. Individual sheets
are provided with simplified versions of the
messages on care during pregnancy (preparing a
birth and emergency plan, clean home delivery,
care for the mother and baby after delivery,
breastfeeding and care after an abortion) to be
given to the mother, her partner and family at the
appropriate stage of pregnancy and childbirth.
These sheets are presented in a generic format.
They will require adaptation to local conditions
and language, and the addition of illustrations
to enhance understanding, acceptability and
attractiveness. Different programmes may prefer
a different format such as a booklet or flip chart.
STRUCTURE AND PRESENTATION
Assumptions underlying the Guide
H
O
W
T
O
R
E
A
D
T
H
E
G
U
I
D
E
Recommendations in the Guide are generic,
made on many assumptions about the health
characteristics of the population and the
health care system (the setting, capacity and
organization of services, resources and staffing).
Population and
endemic conditions
High maternal and perinatal mortality
Many adolescent pregnancies
High prevalence of endemic conditions:
Anaemia
Stable transmission of falciparum malaria
Hookworms (Necator americanus and
Ancylostoma duodenale)
Sexually transmitted infections, including
HIV/AIDS
Vitamin A and iron/folate deficiencies.
Health care system
The Guide assumes that:
Routine and emergency pregnancy, delivery and
postpartum care are provided at the primary
level of the health care, e.g. at the facility near
where the woman lives. This facility could be a
health post, health centre or maternity clinic.
It could also be a hospital with a delivery ward
and outpatient clinic providing routine care to
women from the neighbourhood.
A single skilled attendant is providing care.
She may work at the health care centre, a
maternity unit of a hospital or she may go
to the woman's home, if necessary. However
there may be other health workers who receive
the woman or support the skilled attendant
when emergency complications occur.
Human resources, infrastructure, equipment,
supplies and drugs are limited. However,
essential drugs, IV fluids, supplies, gloves and
essential equipment are available.
If a health worker with higher levels of skill (at
the facility or a referral hospital) is providing
pregnancy, childbirth and postpartum care to
women other than those referred, she follows
the recommendations described in this Guide.
Routine visits and follow-up visits are
scheduled during office hours.
Emergency services (unscheduled visits) for
labour and delivery, complications, or severe
illness or deterioration are provided 24/24
hours, 7 days a week.
Women and babies with complications or
expected complications are referred for further
care to the secondary level of care, a referral
hospital.
Referral and transportation are appropriate for
the distance and other circumstances. They
must be safe for the mother and the baby.
Some deliveries are conducted at home,
attended by traditional birth attendants (TBAs)
or relatives, or the woman delivers alone (but
home delivery without a skilled attendant is
not recommended).
Links with the community and traditional
providers are established. Primary health care
services and the community are involved in
maternal and newborn health issues.
Other programme activities, such as
management of malaria, tuberculosis and
other lung diseases, treatment for HIV, and
infant feeding counselling, that require
specific training, are delivered by a different
provider, at the same facility or at the referral
hospital. Detection, initial treatment and
referral are done by the skilled attendant.
All pregnant woman are routinely offered HIV
testing and counselling at the first contact
with the health worker, which could be during
the antenatal visits, in early labour or in the
postpartum period.
Women who are first seen by the health worker
in late labour are offered the test after the
childbirth.
Health workers are trained to provide HIV
testing and counselling.
HIV testing kits and ARV medicines are
available at the Primary health-care
Knowledge and
skills of care providers
This Guide assumes that professionals using
it have the knowledge and skills in providing
the care it describes. Other training materials
must be used to bring the skills up to the level
assumed by the Guide.
Adaptation of the Guide
It is essential that this generic Guide is adapted
to national and local situations, not only within
the context of existing health priorities and
resources, but also within the context of respect
and sensitivity to the needs of women, newborns
and the communities to which they belong.
An adaptation guide is available to assist
national experts in modifying the Guide
according to national needs, for different
demographic and epidemiological conditions,
resources and settings. The adaptation guide
offers some alternatives. It includes guidance on
developing information and counselling tools so
that each programme manager can develop a
format which is most comfortable for her/him.
ASSUMPTIONS UNDERLYING THE GUIDE
A1
P
R
I
N
C
I
P
L
E
S
O
F
G
O
O
D
C
A
R
E
PRINCIPLES OF GOOD CARE
Communication
PRIN
CIPLES O
F GO
O
D
CARE
A2
Communicating with the w oman
(and her companion)
Makethe w oman (and her companion) feel wel come. Befriendly, respectful and non-judgmental at all times. Use simple and clear languag e. Encourage her to ask questions. Ask and pro vide infor mation related to her needs. Support her in understanding her options and making decisions. Atany examination or before an y procedure: seek her per mission and informher of w hat y ou are doing . Summarize the most impor tant infor mation, including the infor mation on routine laborator y tests and treatments.
Ver ify that she understands emerg ency signs, treatment instr uctions, and w hen and w here to retur n.Check for understanding b y asking her to explain or demonstrate treatment instructions.
Privacy and confidentiality
In all contacts with the w oman and her par tner: Ensure a priv ate place for the examinat ion and counselling . Ensure, whe n discussing sen sitivesubjects, that y ou cannot be o ver heard. Makesure y ou ha vethe w omans consent before discussing with her par tner or family . Neverdi scuss confidential infor mation about clients with other pro viders, or outside the health facility . Or ganize the examination are a so that, during examination, the w oman is protected from the viewof other people (cur tain, screen, wall). Ensure all records are confidential and k ept locked away. Li mit access to logbooks and registers to responsible pro viders only .
Prescribing and recommending
treatments and pre ventive
measures for the w oman
and/or her bab y
When giving a treatment (drug, vaccine, bednet, condom) at the clinic, orpr escribing measures to be follo wedathome: Explain to the w oman w hat the treatment is and w hyit should be gi ven. Explain to her that the t reatment will not har m her or her bab y,and that not taking it ma y be more dang erous. Gi veclear and helpfu l advice on ho w to tak e the dr ug regular ly: for example: tak e 2 tablets 3 times a day, thus e ver y 8 hou rs,in the mor ning, afternoon and e vening with some water and after a meal, for 5 da ys.
Demonstrate the procedure. Explain ho w the treatment is giv en to the bab y. Wat ch her as she does the first treatmen the clinic. Explain the side-effects to her . Explain that theyare not seri ous, and tell her ho w to manage them. Advise her to retur n if she has any problems or concerns about taking the dr ugs. Explore an y bar riers she or her family m ay have,or ha veheard from others, about using the treatment, where possible: Has she or anyone she kno ws used the treatment or pre ventivemeasure before? We re there problems? Reinforce the cor rectinformation that she has, and tr y to cla rify the incor rect information. Di scuss with her the importance of buying and taking the prescribed amount. Help her to think about ho w she will be able to p urchase this.
COMMUNICATION
A3 Wor kplace and administrative procedures
PRIN
CIPLES O
F GO
O
D
CARE
Wor kplace
Servi ce hours should be clear ly posted. Beonti me with appointments or infor m the woman/women if she/the y need to wait. Before beginning the ser vices, check that equipment is clean and functioning and that supplies and dr ugs are in place. Keep the facility clean b y regular cleaning . Atthe end of the ser vice: di scard litter and sharps safely pr epare for disinfection; clean and disinfect equipment and supplies replace linen, pr epare for washing replenish supplies and dr ugs ensure routine cleaning of all areas. Hand overessential infor mation to the colleague w ho follo ws on duty .
Daily and occasional
administrative activities
Keep records of equipment , supplies, drugs and v accines. Check a vai lability and functioning of essential equipment (order stocks of supplies, drugs, vaccines and contraceptiv es before the y r un out). Establish staffing lists and schedules. Complete periodic repor ts on bir ths, deaths and other indicators asrequired, according to instructions.
Record k eeping
Al ways record finding s on a clinical record and home-base d recor d.Record treatments, reasons for refer ral, and follo w-up recommendation s at the ti me the obser vat ion is made. Donot record conf idential information on the home-based record if the woman is unwi lling. Maintain and file appropr iately: al l clinical reco rds al l other docume ntat ion.
International conv entions
The health facility should not allo w distribution of free orlow-cost suplies or products withi n the scope of the Inter national Code of Mark eting of Brea st Milk Substitutes. Itshould also be tobacco free and suppor t a tobacco-free enviro nment.
WOR KPLACE AND ADMINISTRA TIVE PR OCEDURES
Standard precautions and cleanliness
PRIN
CIPLES O
F GO
O
D
CARE
A4
Observe these precautions to protect the woman and her bab y,and you as the health provider , from infections with bacteria and viruses, including HIV .
Was h hands
Wa sh hands with soap and water : Before and after caring for a w oman or ne wborn, and before an y treatment procedure Wh eneverthe hands (or an y other skin area) are contaminated with blood or other bodyfluids Af ter remo ving the glo ves, because the y mayhave holes Af ter changing soiled bedsheets or clothing . Keep nails shor t.
Wea r glo ves
We ar sterile or highly disinfected glo veswhen perfor ming v aginal examination, deliver y,cord cutting, repair of episiotomy or tear , blood drawing . We ar long sterile or highly disinfected glo vesfor manual remo valofpl acenta. We ar clean glo veswhen: Handling and cleaning instr uments Handling contaminated waste Cl eaning blood and bod y fluid spills Dr awi ng blood.
Protect y ourself from blood and
other bod y fluids during deliv eries
We ar glo ves; coverany cuts, abrasions or broken skin with a waterproof bandag e; takecare w hen handling an y sharp instruments (use g ood light); and practic e safe sharps disposal. We ar a long apron made from plasti c or other fluid resistant materia l,and shoes. Ifpossible, protect y our e yesfrom splashes of blood.
Practice safe sharps disposal
Keep a puncture resistant container nearb y. Use each needle and syringe only once. Donot recap, bend or break needles after giving an injection. Dr op all used (disposable ) needles, pl astic syringes and blades directly int o this container, wi thout recapping , and without passing to another person. Empty or send for incinerati on when the container is three-quar ters full.
Practice safe waste disposal
Di spose of placenta o r blood, orbodyfluid contaminated items, inleak-proof container s. Burnor bur y contaminated solid waste. Wa sh hands, gl ovesand conta iners after disposal of infectious wa ste. Pour liquid waste do wn a drain or flushable toilet. Wa sh hands after di sposal of infectious waste.
Deal with contaminated
laundry
Collect clothing or she ets stained with blood or bod y fluids and k eep themseparately from other laundr y,wearing glo vesoruse a plas tic bag. DO NO Ttouch them di rectly. Ri nse off blood or o ther bod y fluids before washing with soap.
Sterilize and clean contaminated
equipment
Makesure that instr uments w hich penet rate the skin (such as ne edles) are adequately sterilized, or that single-use instr uments are disposed of after one use. Thoroughly clean or disi nfect an y equip ment whi ch comes into contact with intact skin (according to instr uctions). Use bleach for clea ning bo wls and buck ets, and for blood or bod y flui d spills.
Clean and
disinfect glo ves
Wa sh the glo vesinsoap and water . Check for damage: Blowglov es full of air , twist the cuff closed, then hold under clean water and look for air le aks. Discard if damag ed. Soak over night in bleach solution with 0.5 available chlorine (made b y adding 90 ml water to 10 ml bleach containing 5% a vai lable chlorine) . Dry awayfrom direct sunlight. Dust inside with talcum po wder or starch.
This produces disinfected gl oves . Theyare not sterile.
Good quality latex glo vescan be dis infected 5 or more time s.
Sterilize glo ves
Sterilize b y autocla ving or highly di sinfect b y steaming or boiling .
UNIVERSAL PRECA UTIONS AND CLEANLINESS
A5 Organizing a visit
PRIN
CIPLES O
F GO
O
D
CARE
Receive and
respond immediately
Receive ever y woman and newbor n bab y seeking care immediately after ar rival(or organize reception b y another pro vider). Perfor mQuick Check on all ne w incoming women and babies and those in the waiting room, especially if no-one is receiving them B2. Atthe first emerg ency sign on Quick Check, begin emerg ency assessment and management (RAM) B1-B7for the w oman, or examine the ne wbornJ1-J11. Ifshe is in labour , accompany her to an appropriate place and follo w the steps as in Childbirth: labour, delivery and immediate postpartum careD1-D29 . Ifshe has priority signs, examine her immediately using Antenatal car e, PostpartumorPost-abortion care char ts C1-C18E1-E10B18-B22 . Ifnoemergency or priority sign on RAM or not in labour , invi te her to wait in the waiting room. Ifbabyis ne wly bor n,looks small, examine immediately. Donot let the mother wait in the queue.
Begin each emerg ency care visit
Introduce y ourself. Ask the name of the w oman. Encourage the companion to sta y with the w oman. Explain all procedures, ask per mission, and k eep the w oman infor med as much as
youcan about w hat y ou are doing . If she is unconscious, talk to the companion. Ensure and respect priv acy during examination and discussion. Ifshe came with a bab y and the bab y is wel l,ask the companion to tak e care of the baby during the mate rnal examination an d treatment.
Care of w oman or bab y refer red for
special care to secondar y le velfacility
Wh en a w oman or bab y is refer red to a secondary level care facility becaus e of a specific probl em or complications, the underlying assumption of the Guide is that, at refer ral le vel , the woman/bab y will be assessed, treated, counselled and ad vised on follo w-up for that par ticular condition/ complication. Follow-up for that specific condi tion will be either: or ganized b y the refer ral facility or wr itten instr uctions will be giv en to the woman/bab y for the skilled attendant at the primar y levelwho refer red the w oman/ baby. the woman/bab y will be ad vised to g o for a follo w-up visit within 2 w eeks according to severity of the condition. Routine care continues at the primar y care level where it was initiated.
Begin each routine visit
(for the w oman and/or the bab y)
Gr eet the w oman and offer her a seat. Introduce y ourself. Ask her name (and the name of the bab y). Ask her : Wh y did y ou come? For y ourself or for y our baby? For a scheduled (routine) visit? For specific complain ts about y ou or y our baby? Fi rst or follo w-up visi t? Doyou want to in clude y our companion or other family membe r (parent if adolescent) in the examinati on and discussion? Ifthe woman is recently deliv ered, assess the baby or ask to see the babyif not wit h the mother . Ifantenatal care, al ways revise the bir th plan at the end of the visit afte r completi ng the char t. For a postpar tum visit, ifshe came w ith the baby,also examine the bab y: Followthe appropr iate char ts according to pregnancy sta tus/age of the bab y and purpose of visit. Followall steps on the char t andinrelevant boxes. Unless the condition ofthe woman or the baby requires urg ent refer ral to hosp ital, give prev entive measures ifdue evenifthe woman has a condition "in y ellow" that requires special treatment.
Iffollow-up visit is within a w eek, and if no other complaints: Assess the w oman for the specific condit requiring follo w-up only Compare with ear lier assessment and re- class ify. Ifa f ollow-up visit is more than a weekafter the initial examination (but not the next scheduled visit): Repeat the w hole assess ment as required for an antenatal, post-abortion, postpartum or ne wborn visit according to the s chedule Ifantenatal visit, revise the bir th plan .
During the visit
Explain all procedures, Ask per missi on before under taking an examination or test. Keep the w oman infor med throughout. Discuss findings with her (and her par tner). Ensure priv acy duri ng the examination and discussion .
At the end of the visi t
Ask the w oman if she has an y questions. Summarize the most impor tant messa geswi th her . Encourag e her to returnfor a routine visit (tell her w hen) and if she has an y concer ns. Fi ll the Home-Base d Mater nal Record (HBMR) and giv e her the approp riate infor mation sheet. Ask her if there are an y points w hich need to be discussed and w ould she lik e suppor t for t his.
ORGANIZING A VISIT
A2 COMMUNICATION
A3 WORKPLACE AND ADMINISTRATIVE
PROCEDURES
A4 STANDARD PRECAUTIONS AND
CLEANLINESS
A5 ORGANIZING A VISIT
These principles of good care apply to all contacts between the skilled attendant and all women and their babies; they are not repeated in
each section. Care-givers should therefore familiarize themselves with the following principles before using the Guide. The principles concern:
Communication A2 .
Workplace and administrative procedures A3 .
Standard precautions and cleanliness A4 .
Organizing a visit A5 .
Communication
P
R
I
N
C
I
P
L
E
S
O
F
G
O
O
D
C
A
R
E
A2
Communicating with the woman
(and her companion)
Make the woman (and her companion) feel
welcome.
Be friendly, respectful and non-judgmental at
all times.
Use simple and clear language.
Encourage her to ask questions.
Ask and provide information related to her
needs.
Support her in understanding her options and
making decisions.
At any examination or before any procedure:
seek her permission and
inform her of what you are doing.
Summarize the most important information,
including the information on routine
laboratory tests and treatments.
Verify that she understands emergency signs,
treatment instructions, and when
and where to return. Check for understanding by
asking her to explain or demonstrate treatment
instructions.
Privacy and confidentiality
In all contacts with the woman and her partner:
Ensure a private place for the examination
and counselling.
Ensure, when discussing sensitive subjects,
that you cannot be overheard.
Make sure you have the womans consent
before discussing with her partner or family.
Never discuss confidential information about
clients with other providers, or outside the
health facility.
Organize the examination area so that, during
examination, the woman is protected from the
view of other people (curtain, screen, wall).
Ensure all records are confidential and kept
locked away.
Limit access to logbooks and registers to
responsible providers only.
Prescribing and recommending
treatments and preventive
measures for the woman
and/or her baby
When giving a treatment (drug, vaccine, bednet,
condom) at the clinic, or prescribing measures to
be followed at home:
Explain to the woman what the treatment is
and why it should be given.
Explain to her that the treatment will not harm
her or her baby, and that not taking it may be
more dangerous.
Give clear and helpful advice on how to take
the drug regularly:
for example: take 2 tablets 3 times a
day, thus every 8 hours, in the morning,
afternoon and evening with some water and
after a meal, for 5 days.
Demonstrate the procedure.
Explain how the treatment is given to the baby.
Watch her as she does the first treatment in
the clinic.
Explain the side-effects to her. Explain that
they are not serious, and tell her how to
manage them.
Advise her to return if she has any problems or
concerns about taking the drugs.
Explore any barriers she or her family may
have, or have heard from others, about using
the treatment, where possible:
Has she or anyone she knows used the
treatment or preventive measure before?
Were there problems?
Reinforce the correct information that
she has, and try to clarify the incorrect
information.
Discuss with her the importance of buying and
taking the prescribed amount. Help her to think
about how she will be able to purchase this.
COMMUNICATION
A3
P
R
I
N
C
I
P
L
E
S
O
F
G
O
O
D
C
A
R
E
Workplace
Service hours should be clearly posted.
Be on time with appointments or inform the
woman/women if she/they need to wait.
Before beginning the services, check that
equipment is clean and functioning and that
supplies and drugs are in place.
Keep the facility clean by regular cleaning.
At the end of the service:
discard litter and sharps safely
prepare for disinfection; clean and disinfect
equipment and supplies
replace linen, prepare for washing
replenish supplies and drugs
ensure routine cleaning of all areas.
Hand over essential information to the
colleague who follows on duty.
Daily and occasional
administrative activities
Keep records of equipment, supplies, drugs
and vaccines.
Check availability and functioning of essential
equipment (order stocks of supplies, drugs,
vaccines and contraceptives before they run out).
Establish staffing lists and schedules.
Complete periodic reports on births, deaths
and other indicators as required, according to
instructions.
Record keeping
Always record findings on a clinical
record and home-based record. Record
treatments, reasons for referral, and follow-up
recommendations at the time the observation
is made.
Do not record confidential information on the
home-based record if the woman is unwilling.
Maintain and file appropriately:
all clinical records
all other documentation.
International conventions
The health facility should not allow distribution
of free or low-cost suplies or products within the
scope of the International Code of Marketing
of Breast Milk Substitutes. It should also be
tobacco free and support a tobacco-free
environment.
WORKPLACE AND ADMINISTRATIVE PROCEDURES
Standard precautions and cleanliness
P
R
I
N
C
I
P
L
E
S
O
F
G
O
O
D
C
A
R
E
A4
Observe these precautions to protect the
woman and her baby, and you as the health
provider, from infections with bacteria and
viruses, including HIV.
Wash hands
Wash hands with soap and water:
Before and after caring for a woman
or newborn, and before any treatment
procedure
Whenever the hands (or any other skin
area) are contaminated with blood or other
body fluids
After removing the gloves, because they
may have holes
After changing soiled bedsheets or clothing.
Keep nails short.
Wear gloves
Wear sterile or highly disinfected gloves when
performing vaginal examination, delivery, cord
cutting, repair of episiotomy or tear, blood
drawing.
Wear long sterile or highly disinfected gloves for
manual removal of placenta.
Wear clean gloves when:
Handling and cleaning instruments
Handling contaminated waste
Cleaning blood and body fluid spills
Drawing blood.
Protect yourself from blood and
other body fluids during deliveries
Wear gloves; cover any cuts, abrasions or
broken skin with a waterproof bandage;
take care when handling any sharp
instruments (use good light); and practice
safe sharps disposal.
Wear a long apron made from plastic or
other fluid resistant material, and shoes.
If possible, protect your eyes from splashes
of blood.
Practice safe sharps disposal
Keep a puncture resistant container nearby.
Use each needle and syringe only once.
Do not recap, bend or break needles after
giving an injection.
Drop all used (disposable) needles, plastic
syringes and blades directly into this
container, without recapping, and without
passing to another person.
Empty or send for incineration when the
container is three-quarters full.
Practice safe waste disposal
Dispose of placenta or blood, or body fluid
contaminated items, in leak-proof containers.
Burn or bury contaminated solid waste.
Wash hands, gloves and containers after
disposal of infectious waste.
Pour liquid waste down a drain or flushable toilet.
Wash hands after disposal of infectious waste.
Deal with contaminated
laundry
Collect clothing or sheets stained with blood
or body fluids and keep them separately from
other laundry, wearing gloves or use a plastic
bag. DO NOT touch them directly.
Rinse off blood or other body fluids before
washing with soap.
Sterilize and clean contaminated
equipment
Make sure that instruments which penetrate
the skin (such as needles) are adequately
sterilized, or that single-use instruments are
disposed of after one use.
Thoroughly clean or disinfect any equipment
which comes into contact with intact skin
(according to instructions).
Use bleach for cleaning bowls and buckets,
and for blood or body fluid spills.
Clean and
disinfect gloves
Wash the gloves in soap and water.
Check for damage: Blow gloves full of air, twist
the cuff closed, then hold under clean water
and look for air leaks. Discard if damaged.
Soak overnight in bleach solution with 0.5%
available chlorine (made by adding 90 ml
water to 10 ml bleach containing 5% available
chlorine).
Dry away from direct sunlight.
Dust inside with talcum powder or starch.
This produces disinfected gloves. They are not
sterile.
Good quality latex gloves can be disinfected 5 or
more times.
Sterilize gloves
Sterilize by autoclaving or highly disinfect by
steaming or boiling.
STANDARD PRECAUTIONS AND CLEANLINESS
A5
P
R
I
N
C
I
P
L
E
S
O
F
G
O
O
D
C
A
R
E
Receive and
respond immediately
Receive every woman and newborn baby
seeking care immediately after arrival (or
organize reception by another provider).
Perform Quick Check on all new incoming
women and babies and those in the waiting
room, especially if no-one is receiving them B2 .
At the first emergency sign on Quick
Check, begin emergency assessment and
management (RAM) B1-B7 for the woman, or
examine the newborn J1-J11 .
If she is in labour, accompany her to an
appropriate place and follow the steps as in
Childbirth: labour, delivery and immediate
postpartum care D1-D29.
If she has priority signs, examine her
immediately using Antenatal care,
Postpartum or Post-abortion care charts
C1-C19 E1-E10 B18-B22.
If no emergency or priority sign on RAM or not
in labour, invite her to wait in the waiting room.
If baby is newly born, looks small, examine
immediately. Do not let the mother wait in the
queue.
Begin each emergency care visit
Introduce yourself.
Ask the name of the woman.
Encourage the companion to stay with the woman.
Explain all procedures, ask permission,
and keep the woman informed as much as
you can about what you are doing. If she is
unconscious, talk to the companion.
Ensure and respect privacy during
examination and discussion.
If she came with a baby and the baby is
well, ask the companion to take care of the
baby during the maternal examination and
treatment.
Care of woman or baby referred for
special care to secondary level facility
When a woman or baby is referred to a
secondary level care facility because of
a specific problem or complications, the
underlying assumption of the Guide is that,
at referral level, the woman/baby will be
assessed, treated, counselled and advised
on follow-up for that particular condition/
complication.
Follow-up for that specific condition will be
either:
organized by the referral facility or
written instructions will be given to the
woman/baby for the skilled attendant at
the primary level who referred the woman/
baby.
the woman/baby will be advised to go for a
follow-up visit within 2 weeks according to
severity of the condition.
Routine care continues at the primary care
level where it was initiated.
Begin each routine visit
(for the woman and/or the baby)
Greet the woman and offer her a seat.
Introduce yourself.
Ask her name (and the name of the baby).
Ask her:
Why did you come? For yourself or for your
baby?
For a scheduled (routine) visit?
For specific complaints about you or your
baby?
First or follow-up visit?
Do you want to include your companion or
other family member (parent if adolescent)
in the examination and discussion?
If the woman is recently delivered, assess the
baby or ask to see the baby if not with the mother.
If antenatal care, always revise the birth plan at
the end of the visit after completing the chart.
For a postpartum visit, if she came with the
baby, also examine the baby:
Follow the appropriate charts according
to pregnancy status/age of the baby and
purpose of visit.
Follow all steps on the chart and in relevant
boxes.
Unless the condition of the woman or the
baby requires urgent referral to hospital, give
preventive measures if due even if the woman
has a condition "in yellow" that requires
special treatment.
If follow-up visit is within a week, and if no
other complaints:
Assess the woman for the specific condition
requiring follow-up only
Compare with earlier assessment and
re-classify.
If a follow-up visit is more than a week after
the initial examination (but not the next
scheduled visit):
Repeat the whole assessment as required
for an antenatal, post-abortion, postpartum
or newborn visit according to the schedule
If antenatal visit, revise the birth plan.
During the visit
Explain all procedures,
Ask permission before undertaking an
examination or test.
Keep the woman informed throughout.
Discuss findings with her (and her partner).
Ensure privacy during the examination and
discussion.
At the end of the visit
Ask the woman if she has any questions.
Summarize the most important messages with her.
Encourage her to return for a routine visit (tell
her when) and if she has any concerns.
Fill the Home-Based Maternal Record (HBMR)
and give her the appropriate information sheet.
Ask her if there are any points which need to be
discussed and would she like support for this.
ORGANIZING A VISIT
Quick check, rapid assessment and management of women of childbearing age
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
B1
QUICK CHECK, RAPID ASSESSMENT AND MANAGEMENT OF WOMEN OF CHILDBEARING AGE
Quick check
QUICK CHECK,
RAPID ASSESSM
ENT AND
M
ANAGEM
ENT OF
W
OMEN OF CHILDB
EARING AGE
ASK, CHECK RECORD
Wh y did y ou come? for yourself? for the bab y? How old is the bab y? Wh at is the concer n?
LOOK, LISTEN, FEEL
Is the woman being wheeled or carr ied in or : bl eeding v aginally convulsing looking v eryill unconscious insever e pain inlabour deliver y is imminent
Check if bab y is or has: verysmall convulsing breathing difficulty
SIGNS
If the w oman is or has: unconscious (does not ans wer ) convulsing bl eeding sever e abdominal pain orlooks v eryill headache and visual disturbance sever e difficulty bre athing fever sever e vomiting.
Imminent deliv eryor Labour
If the bab y is or has: verysmall convulsions di fficult breathing just bor n any mater nal concer n.
Pr egnant w oman, or after deliv ery , with no dang er signs Anewbor n with no dang er signs or maternal complaints.
TREAT
Tr ansfer woman to a treatment room for Rapid assess ment and manag ement B3-B7. Call for help if needed. Reassure the w oman that she will be tak en care of immediately. Ask her co mpanion to sta y.
Tr ansfer the w oman to the labour ward. Call for immediate assessm ent.
Tr ansfer the bab y to the treatment room for immediate Ne wborn careJ1-J11. Ask the mo ther to sta y.
Keep the w oman and bab y in the waiting room for routine care.
CLASSIFY
EMERGENCY FOR WOMAN
LABOUR
EMERGENCY FOR BABY
ROUTINE CARE
IFemergency for w oman or bab y or labour , go toB3. IFnoemergency , go to rele vant section
QUI CK CHECK
A person responsible for initial reception of women of childbearing ag e and newbor ns seeking care should:
assess the g eneral condition of the careseek er(s) immediately on ar rival
periodically repeat this procedure if the line is long .
If a woman is ver y sick, talk to her companion.
B2
Rapid assessment and management (RAM) Airway and breathing , circulation (shock)
NEXT : Vaginal bleeding QUICK CHECK,
RAPID ASSESSM
ENT AND
M
ANAGEM
ENT OF
W
OMEN OF CHILDBEARING
AGE
B3
This may be pneumonia, severe anaemia with hear t failur e, obstructed breathing , asthma.
This may be haemor rhagic shock, septic shock.
TREATMENT
Manageairwa y and breathing B9. Refer woman urg ently to hospi tal* B17.
Measure blood pressure. Ifsystolic BP < 90 mmHg or pulse >110 per minute: Position the w oman on her lef t side with legs higher than chest. Insertan IV line B9. Gi vefluids rapidly B9. Ifnot able to inser t peripher al IV , use alter nativeB9. Keep her war m (co verher). Refer her urg ently to hospital * B17.
* But if bir th is imminent (bul ging , thin peri neum during contractions, vi sible fetal head), transfer w oman to labour room and proceed as on D1-D28 .
RAPID ASSESSMENT AND MANA GEMENT (RAM)
Use this char t for r apid assessment and manag ement (RAM) of all women of childbearing ag e,and also for women in labour , on firs t arrival and periodically throughout
labour, delivery and the postpar tum period. Assess for all emerg ency and priority signs and give appropriate treatments, then refe r the woman to hospital.-
FIRST ASSESS
EMERGENCY SIGNS
Do all emerg ency steps before refer ral
AIRWA Y ANDBREATHING
Verydifficult breathing or Central cy anosis
CIRCULATION (SHOCK)
Cold moist skin or We ak and fast pulse
MEASURE
Measure blood pressure Count pulse
Rapid assessment and management (RAM) Vaginal bleeding
QUICK CHECK,
RAPID ASSESSM
ENT AND
M
ANAGEM
ENT OF
W
OMEN OF CHILDB
EARING AGE
B4
PREGNANCY ST ATUS
EARLY PREGNANCY not a ware of pregnancy , or not pregnant (uterus NOTabov e umbilicus)
LATEPREGNANCY (uterus abov e umbilicus)
DURING LAB OUR before deliv eryof bab y
BLEEDING
HEAVY BLEEDING Padorcl oth soak ed in < 5 minutes.
LIGHT BLEEDING
ANY BLEEDING IS D ANGEROUS
BLEEDING MORE THAN 100 ML SINCE LAB OUR BEGAN
This may be abor tion, menorr hagia, ectopic pr egnancy.
This may be placenta pr evi a, abruptio placentae, ruptured uterus.
This may be pl acenta pr evi a,abruptio placenta, ruptureduterus.
TREATMENT
Insertan IV line B9. Gi vefluids rapidly B9. Gi ve0.2 mg erg ometrine IM B10. Repeat 0.2 mg erg ometrine IM/IV ifbl eeding continues. Ifsuspect possible complicated abor tion, giveappropria te IM/IV antibiotics B15. Refer woman urg ently to hospit al B17.
Examine w oman as on B19. Ifpr egnancy not lik ely,refer to other clinical guidelines.
DO NO T do v aginal examination, but: Insertan IV line B9. Gi vefluids rapidly if hea vy bleed ing or shock B3. Refer woman urg ently to hospit al* B17.
DO NO T do v aginal examination, but: Insertan IV line B9. Gi vefluids rapidly if hea vy bleed ing or shock B3. Refer woman urg ently to hospit al* B17.
* But if bir th is imminent (bulging , thin perineum during con traction s,visible fetal head), transfer w oman to labour room and proceed as on D1-D28 .
VAGI NAL BLEEDING
Assess pre gnancy status
Assess amount of bleeding
NEXT : Vaginal bleeding in postpar tum
Rapid assessment and management (RAM) Vaginal bleeding : postpar tum
NEXT : Convulsion s or unconscious QUICK CHECK,
RAPID ASSESSM
ENT AND
M
ANAGEM
ENT OF
W
OMEN OF CHILDBEARING
AGE
B5
PREGNANCY ST ATUS
POSTP ARTUM (baby is bor n)
Check and ask if placenta is delivered
Check for perineal and lower vaginal tears
Check if still bleeding
BLEEDING
HEAVY BLEEDING Pad or cloth soa kedin< 5 minutes Constant trickling of blood Bl eeding >250ml or deliv ered outside healthcentre and still bleeding
PLACENT A NOT DELIVERED
PLACENT A DELIVERED
Check placenta B11
IF PRESENT
HEAVY BLEEDING
CONTROLLED BLEEDING
This may be uterine aton y, ret ained placen ta,ruptured uterus, vaginal or cer vical tear .
TREATMENT
Call for extra help. Massageuterus until it is hard and giv e oxytocin 10 IU IM B10. Insertan IV line B9 and giv e IV fluids w ith 20 IU oxytocin at 60 drops/minute. Empty bladder . Catheterize if necessar yB12. Check and record BP and pulse e ver y 15 min utes and treat asonB3.
Wh en uter us is hard, deliver placenta b y controlled cord tracti onD12. Ifunsuccessful and bleeding continues, remov e place nta manually and check placenta B11. Gi veappropriate IM/IV antibiotics B15. Ifunable to remo veplacenta, refer w oman urg ently to hospital B17. During transfer , continue IV fluids with 20 IU of oxytocin at 30 drops/minute.
If placenta is compl ete: Massageuterus to express an y clots B10. Ifut erusremains soft, gi veergometrine 0.2 mg IV B10. DO NO Tgi veergometrine to women with ec lampsia, pre-eclam psia or kno wn h ypertension. Continue IV fluids with 20 IU oxytocin/litr e at 30 drops/minute. Continue massaging uter us till it is hard. If placenta is incom plete (or not a vai lable for inspection) : Remov e placental frag mentsB11. Gi veappropriate IM/IV antibiotics B15. Ifunable to remo ve,refer w oman urg entlyto hospital B17.
Examine the tear and deter mine the deg reeB12. If third deg ree tear (in vol ving rectum or anus), refer w oman urg entlyto hospital B17. For other tears: apply pressure o verthe tear w ith a sterile pad or g auze and put legs tog ether. Donot cross a nkles. Check after 5 minutes, ifbl eeding persists repair the tear B12.
Continue IV fluids with 20 units of oxytocin at 30 drops/minute. Insertsecond IV line. Apply bimanual uterine oraorti c compression B10. Gi veappropriate IM/IV antibiotics B15. Refer woman urg ently to hospital B17.
Continue oxytocin infusion with 20 IU/litre of IV fluids at 20 drops/min for at least one hour after bl eeding stops B10. Observ e closely (e ver y 30 minutes) for 4 hou rs.Keep nearb y for 24 hour s.If se ver e pallor , refer to health cen tre. Examine the w oman using Assess the mother aft er deliver yD12.
Rapid assessment and management (RAM) Emergency signs
QUICK CHECK,
RAPID ASSESSM
ENT AND
M
ANAGEM
ENT OF
W
OMEN OF CHILDB
EARING AGE
B6
EMERGENCY SIGNS
Convulsing (no w or recently), or Unconscious Ifunconscious, ask relativ e has there been a recent con vulsion?
Sever e abdominal pain (not nor mal labour)
Fever (temperature more than 38C) and an y of: Veryfast breathing Stiff neck Lethargy Veryweak/not able to stand
This may be eclampsia.
This may be r uptured uterus, obstructed labour, abruptio placenta, puerper al or post- abortion sepsis, ectopic pregnancy .
This may be malaria, meningitis, pneumonia, septicemia.
CONVULSIONS OR UNCONSCIOUS
SEVERE ABDOMINAL PAI N
DANGEROUS FEVER
TREATMENT
Pr otect w oman from fall and inj ury . Get help. Manageairwa y B9. Af ter con vulsion ends, help woman onto her left side. Insertan IV line and giv e fluid s slowly (30 drops/min) B9. Gi vemagnesium sulphate B13. Ifearlypr egnancy, gi vediazepam IV or rectally B14. Ifdi astolic BP >110mm of Hg , giveantih ypertensiv e B14. Iftemperature >38C, orhi story of fe ver , also giv e treatment for dang erous fever (belo w). Refer woman urg ently to hospit al* B17.
Measure BP and temper ature Ifdi astolic BP >110mm of Hg , giveantih ypertensiv e B14. Iftemperature >38C, orhi story of fe ver , also giv e treatment for dang erous fever (belo w). Refer woman urg ently to hospit al* B17.
Insertan IV line and giv e fluid s B9. Iftemperature more than 38C, gi vefirst dose of appropriate IM/IV antiobiotics B15. Refer woman urg ently to hospit al* B17. Ifsystolic BP <90 mm Hg see B3.
Insertan IV line B9. Gi vefluids slo wlyB9. Gi vefirst dose of appropriate IM/IV anti biotics B15. Gi veartemether IM(if not a vai lable, givequinine IM) and glucose B16. Refer woman urg ently to hospit al* B17.
* But if bir th is imminent (bul ging , thin peri neum during contractions, vi sible fetal head), transfer w oman to labour room and proceed as on D1-D28 .
MEASURE
Measure blood pressure Measure temperature Assess pregnancy status
Measure blood pressure Measure temperature
Measure temperature
NEXT : Priority signs
Rapid assessment and management (RAM) Priority signs
QUICK CHECK,
RAPID ASSESSM
ENT AND
M
ANAGEM
ENT OF
W
OMEN OF CHILDBEARING
AGE
B7
PRIORITY SIGNS
Labour pains or Ruptured membranes
If an y of: Sever e pallor Epigastric or abdominal pain Sever e headache Bl urr ed vision Fever(temperature more than 38C) Breathing difficulty
Noemergency signs or Nopr iority signs
TREATMENT
Manageas for Childbir thD1-D28 .
Ifpr egnant (and not in labour), pr ovi de antenatal care C1-C18. Ifrecently giv en bir th,provide postpartum careD21. andE1-E10. Ifrecent abor tion, provide post-abor tion care B20-B21 . Ifearlypr egnancy, ornot aware of pregnancy , check for ectopic pregnancy B19.
Ifpr egnant (and not in labour), pr ovi de antenatal care C1-C18. Ifrecently giv en bir th,provide postpartum careE1-E10.
LABOUR
OTHER DANGER SIGNS OR SYMPT OMS
IF NO EMERGENCY OR PRIORITY SIGNS , NON URGENT
MEASURE
Measure blood pressure Measure temperature
B2
QUICK CHECK
B3 RAPID ASSESSMENT AND
MANAGEMENT (RAM) (1)
Airway and breathing
Circulation and shock
B4 RAPID ASSESSMENT AND
MANAGEMENT (RAM) (2)
Vaginal bleeding
B5 RAPID ASSESSMENT AND
MANAGEMENT (RAM) (3)
Vaginal bleeding: postpartum
B6 RAPID ASSESSMENT AND
MANAGEMENT (RAM) (4)
Convulsions
Severe abdominal pain
Dangerous fever
B7 RAPID ASSESSMENT AND
MANAGEMENT (RAM) (5)
priority signs
Labour
Other danger signs or symptoms
Non-urgent
Perform Quick check immediately after the woman arrives B2 .
If any danger sign is seen, help the woman and send her quickly to the emergency room.
Always begin a clinical visit with Rapid assessment and management (RAM) B3-B7 :
Check for emergency signs first B3-B6 .
If present, provide emergency treatment and refer the woman urgently to hospital.
Complete the referral form N2 .
Check for priority signs. If present, manage according to charts B7 .
If no emergency or priority signs, allow the woman to wait in line for routine care, according to pregnancy status.
Quick check
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
ASK, CHECK RECORD
Why did you come?
for yourself?
for the baby?
How old is the baby?
What is the concern?
LOOK, LISTEN, FEEL
Is the woman being wheeled or
carried in or:
bleeding vaginally
convulsing
looking very ill
unconscious
in severe pain
in labour
delivery is imminent
Check if baby is or has:
very small
convulsing
breathing difficulty
SIGNS
If the woman is or has:
unconscious (does not answer)
convulsing
bleeding
severe abdominal pain or looks very ill
headache and visual disturbance
severe difficulty breathing
fever
severe vomiting.
Imminent delivery or
Labour
If the baby is or has:
very small
convulsions
difficult breathing
just born
any maternal concern.
Pregnant woman, or after delivery,
with no danger signs
A newborn with no danger signs or
maternal complaints.
TREAT
Transfer woman to a treatment room for Rapid
assessment and management B3-B7 .
Call for help if needed.
Reassure the woman that she will be taken care of
immediately.
Ask her companion to stay.
Transfer the woman to the labour ward.
Call for immediate assessment.
Transfer the baby to the treatment room for
immediate Newborn care J1-J11 .
Ask the mother to stay.
Keep the woman and baby in the waiting room for
routine care.
CLASSIFY
EMERGENCY
FOR WOMAN
LABOUR
EMERGENCY
FOR BABY
ROUTINE CARE
IF emergency for woman or baby or labour, go to B3 .
IF no emergency, go to relevant section
QUICK CHECK
A person responsible for initial reception of women of childbearing age and newborns seeking care should:
assess the general condition of the careseeker(s) immediately on arrival
periodically repeat this procedure if the line is long.
If a woman is very sick, talk to her companion.
B2
Rapid assessment and management (RAM) Airway and breathing, circulation (shock)
NEXT: Vaginal bleeding
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
B3
This may be pneumonia, severe
anaemia with heart failure,
obstructed breathing, asthma.
This may be haemorrhagic shock,
septic shock.
TREATMENT
Manage airway and breathing B9 .
Refer woman urgently to hospital* B17 .
If systolic BP < 90 mmHg or pulse >110 per minute:
Position the woman on her left side with legs higher than chest.
Insert an IV line B9 .
Give fluids rapidly B9 .
If not able to insert peripheral IV, use alternative B9 .
Keep her warm (cover her).
Refer her urgently to hospital* B17 .
* But if birth is imminent (bulging, thin perineum during contractions, visible
fetal head), transfer woman to labour room and proceed as on D1-D28.
RAPID ASSESSMENT AND MANAGEMENT (RAM)
Use this chart for rapid assessment and management (RAM) of all women of childbearing age, and also for women in labour, on first arrival and periodically throughout
labour, delivery and the postpartum period. Assess for all emergency and priority signs and give appropriate treatments, then refer the woman to hospital.-
FIRST ASSESS
EMERGENCY SIGNS
Do all emergency steps before referral
AIRWAY AND BREATHING
Very difficult breathing or
Central cyanosis
CIRCULATION (SHOCK)
Cold moist skin or
Weak and fast pulse
MEASURE
Measure blood pressure
Count pulse
Rapid assessment and management (RAM) Vaginal bleeding
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
B4
PREGNANCY STATUS
EARLY PREGNANCY
not aware of pregnancy, or not pregnant
(uterus NOT above umbilicus)
LATE PREGNANCY
(uterus above umbilicus)
DURING LABOUR
before delivery of baby
BLEEDING
HEAVY BLEEDING
Pad or cloth soaked in < 5 minutes.
LIGHT BLEEDING
ANY BLEEDING IS DANGEROUS
BLEEDING
MORE THAN 100 ML
SINCE LABOUR BEGAN
This may be abortion,
menorrhagia, ectopic pregnancy.
This may be placenta previa,
abruptio placentae, ruptured
uterus.
This may be
placenta previa, abruptio
placenta, ruptured uterus.
TREATMENT
Insert an IV line B9 .
Give fluids rapidly B9 .
Give 0.2 mg ergometrine IM B10 .
Repeat 0.2 mg ergometrine IM/IV if bleeding continues.
If suspect possible complicated abortion, give appropriate IM/IV antibiotics B15 .
Refer woman urgently to hospital B17 .
Examine woman as on B19 .
If pregnancy not likely, refer to other clinical guidelines.
DO NOT do vaginal examination, but:
Insert an IV line B9 .
Give fluids rapidly if heavy bleeding or shock B3 .
Refer woman urgently to hospital* B17 .
DO NOT do vaginal examination, but:
Insert an IV line B9 .
Give fluids rapidly if heavy bleeding or shock B3 .
Refer woman urgently to hospital* B17 .
* But if birth is imminent (bulging, thin perineum during contractions, visible
fetal head), transfer woman to labour room and proceed as on D1-D28.
VAGINAL BLEEDING
Assess pregnancy status
Assess amount of bleeding
NEXT: Vaginal bleeding in postpartum
Rapid assessment and management (RAM) Vaginal bleeding: postpartum
NEXT: Convulsions or unconscious
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
B5
PREGNANCY STATUS
POSTPARTUM
(baby is born)
Check and ask if placenta is delivered
Check for perineal and lower
vaginal tears
Check if still bleeding
BLEEDING
HEAVY BLEEDING
Pad or cloth soaked in < 5 minutes
Constant trickling of blood
Bleeding >250 ml or delivered outside
health centre and still bleeding
PLACENTA NOT DELIVERED
PLACENTA DELIVERED
Check placenta B11
IF PRESENT
HEAVY BLEEDING
CONTROLLED BLEEDING
This may be uterine atony,
retained placenta, ruptured
uterus, vaginal or cervical tear.
TREATMENT
Call for extra help.
Massage uterus until it is hard and give oxytocin 10 IU IM B10 .
Insert an IV line B9 and give IV fluids with 20 IU oxytocin at 60 drops/minute.
Empty bladder. Catheterize if necessary B12 .
Check and record BP and pulse every 15 minutes and treat as on B3 .
When uterus is hard, deliver placenta by controlled cord traction D12 .
If unsuccessful and bleeding continues, remove placenta manually and check placenta B11 .
Give appropriate IM/IV antibiotics B15 .
If unable to remove placenta, refer woman urgently to hospital B17 .
During transfer, continue IV fluids with 20 IU of oxytocin at 30 drops/minute.
If placenta is complete:
Massage uterus to express any clots B10 .
If uterus remains soft, give ergometrine 0.2 mg IV B10 .
DO NOT give ergometrine to women with eclampsia, pre-eclampsia or known hypertension.
Continue IV fluids with 20 IU oxytocin/litre at 30 drops/minute.
Continue massaging uterus till it is hard.
If placenta is incomplete (or not available for inspection):
Remove placental fragments B11 .
Give appropriate IM/IV antibiotics B15 .
If unable to remove, refer woman urgently to hospital B17 .
Examine the tear and determine the degree B12 .
If third degree tear (involving rectum or anus), refer woman urgently to hospital B17 .
For other tears: apply pressure over the tear with a sterile pad or gauze and put legs together. Do not cross ankles.
Check after 5 minutes, if bleeding persists repair the tear B12 .
Continue IV fluids with 20 units of oxytocin at 30 drops/minute. Insert second IV line.
Apply bimanual uterine or aortic compression B10 .
Give appropriate IM/IV antibiotics B15 .
Refer woman urgently to hospital B17 .
Continue oxytocin infusion with 20 IU/litre of IV fluids at 20 drops/min for at least one hour after bleeding stops B10 .
Observe closely (every 30 minutes) for 4 hours. Keep nearby for 24 hours. If severe pallor, refer to health centre.
Examine the woman using Assess the mother after delivery D12 .
Rapid assessment and management (RAM) Emergency signs
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
B6
EMERGENCY SIGNS
Convulsing (now or recently), or
Unconscious
If unconscious, ask relative
has there been a recent convulsion?
Severe abdominal pain (not normal labour)
Fever (temperature more than 38C)
and any of:
Very fast breathing
Stiff neck
Lethargy
Very weak/not able to stand
This may be eclampsia.
This may be ruptured uterus,
obstructed labour, abruptio
placenta, puerperal or post-
abortion sepsis, ectopic
pregnancy.
This may be malaria,
meningitis, pneumonia,
septicemia.
CONVULSIONS OR UNCONSCIOUS
SEVERE ABDOMINAL PAIN
DANGEROUS FEVER
TREATMENT
Protect woman from fall and injury. Get help.
Manage airway B9 .
After convulsion ends, help woman onto her left side.
Insert an IV line and give fluids slowly (30 drops/min) B9 .
Give magnesium sulphate B13 .
If early pregnancy, give diazepam IV or rectally B14 .
If diastolic BP >110mm of Hg, give antihypertensive B14 .
If temperature >38C, or history of fever, also give treatment for dangerous
fever (below).
Refer woman urgently to hospital* B17 .
Measure BP and temperature
If diastolic BP >110mm of Hg, give antihypertensive B14 .
If temperature >38C, or history of fever, also give treatment for dangerous
fever (below).
Refer woman urgently to hospital* B17 .
Insert an IV line and give fluids B9 .
If temperature more than 38C, give first dose of appropriate IM/IV
antiobiotics B15 .
Refer woman urgently to hospital* B17 .
If systolic BP <90 mm Hg see B3 .
Insert an IV line B9 .
Give fluids slowly B9 .
Give first dose of appropriate IM/IV antibiotics B15 .
Give artemether IM (if not available, give quinine IM) and glucose B16 .
Refer woman urgently to hospital* B17 .
* But if birth is imminent (bulging, thin perineum during contractions, visible
fetal head), transfer woman to labour room and proceed as on D1-D28.
MEASURE
Measure blood pressure
Measure temperature
Assess pregnancy status
Measure blood pressure
Measure temperature
Measure temperature
NEXT: Priority signs
Rapid assessment and management (RAM) Priority signs
Q
U
I
C
K
C
H
E
C
K
,
R
A
P
I
D
A
S
S
E
S
S
M
E
N
T
A
N
D
M
A
N
A
G
E
M
E
N
T
O
F
W
O
M
E
N
O
F
C
H
I
L
D
B
E
A
R
I
N
G
A
G
E
B7
PRIORITY SIGNS
Labour pains or
Ruptured membranes
If any of:
Severe pallor
Epigastric or abdominal pain
Severe headache
Blurred vision
Fever (temperature more than 38C)
Breathing difficulty
No emergency signs or
No priority signs
TREATMENT
Manage as for Childbirth D1-D28.
If pregnant (and not in labour), provide antenatal care C1-C19.
If recently given birth, provide postpartum care D21 . and E1-E10 .
If recent abortion, provide post-abortion care B20-B21.
If early pregnancy, or not aware of pregnancy, check for ectopic pregnancy B19 .
If pregnant (and not in labour), provide antenatal care C1-C19.
If recently given birth, provide postpartum care E1-E10 .
LABOUR
OTHER DANGER SIGNS OR SYMPTOMS
IF NO EMERGENCY OR PRIORITY SIGNS, NON URGENT
MEASURE
Measure blood pressure
Measure temperature
Emergency treatments for the woman
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B8
EMERGENCY TREATMENTS FOR THE WOMAN
AIRWA Y,BREATHING AND CIRCULA TION
Airway, breathing and circulation
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B9
Manage the airwa y and breathing
If the w oman has g reat difficulty breathing and:
Ifyou suspect obstr uction:
Tr y to clear the airwa y and dislodg e obstr uction
Help the w oman to find the best position for breathing
Urgently refer the woman to hospital.
Ifthe woman is unconscious:
Keep her on her back, arms at the side
Ti lt her head backwards (unless trauma is suspected)
Li ft her chin to open airwa y
Inspect her mouth for foreign bod y; remo veif found
Cl ear secretions from throat.
Ifthe woman is not breathing:
Ventilate with bag and mask until she star ts breathing spontaneously
Ifwoman still has g reat difficulty breathing , keep her propped up, and
Refer the woman urg ently to hospital.
Insert IV line and giv e fluids
Was h hands with s oap and water and put on glo ves.
Clean w omans skin with spirit at site for IV line.
Insert an intra venous line (IV line) using a 16-18 g augeneedle.
Attach Ring erslactate or nor mal sali ne.Ensure infusion is r unning w ell.
Givefluids at rapid r ateifshock, systolic BP<90 mmHg , pulse>110/minute, orheavyvaginal bleeding:
Infuse 1 litre in 15-20 min utes (as rapid as possible).
Infuse 1 litre in 30 minut es at 30 ml/minute. Repeat if necessar y.
Monitor e ver y 15 minu tes for :
blood pressure (BP) a nd puls e
shortness of breath or puffiness.
Reduce the infusion r ate to 3 ml/mi nute (1 litre in 6-8 hours) w hen pulse slo ws to less than 100/
minute, systolic BP increases to 100 mmHg or higher .
Reduce the infusion r ate to 0.5 ml/ minute if breathing difficulty or puffiness develops.
Monitor urine output.
Record time and amou nt of fluids giv en.
Givefluids at moderate rate ifsever e abdominal pain, obstructed labour, ectopic pregnancy , dangerous
fever or deh ydration:
Infuse 1 litre in 2-3 hou rs.
Givefluids at slow r ateifsever e anaemia/se ver e pre- eclampsia oreclampsia:
Infuse 1 litre in 6-8 hou rs.
If intra venous access not possible
Gi veoral reh ydration solution (ORS) b y mouth if able to drink, orbynasogastric (NG) tube .
Quantity of ORS: 300 to 500 mlin1 hour.
DO NO Tgi veORS to a w oman w ho is unconscious or has con vulsions.
BLEEDING
Bleeding (1)
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B10
Massage uterus and expel clots
If hea vy postpar tum bleeding persists after placenta is deliv ered, or uter us is not w ell contrac ted (is soft):
Pl ace cupped palm on uterine fundus and feel for state of contraction .
Massagefundus in a circular motion with cupped palm until uter us is w ell contracted.
Wh en well contracted, pl ace fing ers behind fundus and push do wn in one s wift action to expel clots.
Collect blood in a container placed close to the vulv a.Measure or estimate blood loss, and record.
Apply bimanual uterine compression
If hea vy postpar tum bleeding persists despite uterine massag e,oxytocin/erg ometrine treatment and
remov al of placenta:
We ar sterile or clean glo ves.
Introduce the right hand into the v agina, clenched fist, wi th the back of the hand directe d posterior ly
and the knuckles in the anterior for nix.
Pl ace the other hand on the abdomen behind the uter us and squeeze the uter us fir mly betw een the
twohands.
Continue compression until bleeding stops (no bleeding if the compres sion is released).
Ifbl eeding persists, apply aor tic compression and transpor t woman to hospital.
Apply aor tic compression
If hea vy postpar tum bleeding persists despite uterine massag e,oxytocin/ergometrine treatment and
remov al of placenta:
Feel for femoral pulse.
Apply pressure abo vethe umbilicus to stop bleeding . Apply sufficient pr essure until femoral pulse is not felt.
After finding cor rect site, showassistant or relativ e how to apply pressure, ifnecessary .
Continue pressure until bleeding stops. Ifbl eeding persists, keep applying pressure w hile transpor ting
woman to hospital.
Giveoxytocin
If hea vy postpar tum bleed ing
Initial dose Continuing dose Maximum dose
IM/IV: 10 IU IM/IV: repeat 10 IU
after 20 minu tes Not more than 3 litres
ifheavybl eeding persists of IV fluids containing
IV infusion: IV infusion: oxytocin
20 IU in 1 litre 10 IU in 1 litre
at 60 drops/min at 30 drops/min
Giveergometrine
If hea vy bleeding in ear ly pregnancy or postpartum bleeding (after oxytocin) but
DO NO T give if eclampsia, pre-eclampsia, orhypertension
Initial dose Continuing dose Maximum dose
IM/IV:0.2 mg IM: repeat 0.2 mg Not more than
slowly IM after 15 minutes if hea vy 5 doses (total 1.0 mg)
bl eeding persists
Bleeding (2)
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B11
Remov e placenta and fragments manually
Ifpl acenta not deliv ered 1 hour after deliv eryof the bab y,OR
Ifheavyvaginal bleeding continues despite massag e and oxytocin and placenta cannot be deliv ered
bycontrolled cord traction, orifpl acenta is incomplete and bleeding c ontinues.
Prepar ation
Explain to the w oman the need for manual remo valofthe placenta and obtain her consent.
Insertan IV line. Ifbl eeding, gi vefluids rapidly . If not bleeding , givefluids slo wlyB9.
Assist w oman to g et onto her back.
Gi vediazepam (10-mg IM/IV).
Cl ean vulv a and perineal area.
Ensure the bladder is empty . Catheterize if necessar yB12.
Wa sh hands and forear ms well and put on long sterile glo ves(and an apron or g ownifavailable).
Technique
Wi th the left hand, hold the umbilical cord with the clamp. Then pull the cord g ently until it is
horizontal.
Insertright hand into the v agina and up into the uter us.
Leavethe cord and hold the fundus with the left hand in order to supp ortthe fundus of the uter us
and to pro vide counter-traction during remo val .
Movethe fing ers of the right hand side ways until edg e of the placenta is located.
Detach the placenta from the implantation site b y keeping the fing ers tightly tog ether and using the
edgeof the hand to g radually mak e a space betw een the placenta and the uterine wall.
Pr oceed g radually all around the placental bed until the w hole placenta is detached fromthe uterine
wall.
Wi thdraw the right hand from the uter us gradually, bringing the placenta w ith it.
Explore the inside of the uterine ca vity to ensure all placental tissue has been remo ved.
Wi th the left hand, pr ovi de counter-traction to the fundus through the abdomen b y pushing it in the
opposite direction of the hand that is being withdra wn. This pre vents in ver sion of the uter us.
Examine the uterine surface of the placenta to ensure that lobes and membranes are complete. If
anyplacental lobe or tissue fragments are missing , explore ag ain the uterine ca vity to remo vethem.
If hours or da ys ha ve passed since deliver y,or if the placenta is retaine d due to constrictio n ring
or closed cer vix, it ma y not be possible to put the hand into the uter us.DO NO T persist. Refer
urgently to hospital B17.
If the placenta does not separ ate from the uterine surface b y gentle sidew aysmovement of the
finger tips at the line of clea vage,suspect placenta accreta. DONOT persist in effor ts to remove
placenta. Refer urg ently to hospital B17.
After manual remo valofthe placenta
Repeat oxytocin 10-I U IM/IV .
Massagethe fundus of the uter us to encourag e a tonic uterine contraction.
Gi veampicillin 2 g IV/IM B15.
Iffever>38.5C, foul-smelling lochia or histor y of r upture of membranes for 18 or more hours al so
givegentamicin 80 mg IM B15.
Ifbl eeding stops:
gi vefluids slo wly for at least 1 hour after remo valofpl acenta.
Ifheavybl eeding continues:
gi veergometrine 0.2 mg IM
gi ve20 IU oxytocin ineach litr e of IV f luids and infuse rapidly
Refer urg ently to ho spitalB17.
During transpor tation, feel continuously w hethe r uter us is w ell contracted (hard and roun d).If not,
massage and repeat oxytocin 10 IU IM/IV .
Pr ovi de bimanual or aor tic compression if se ver e bleeding before and during transpor tationB10.
REPAIR THE TEAR AND EMPTY BLADDER
Bleeding (3)
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B12
Repair the tear or episiotomy
Examine the tear and deter mine the deg ree:
The tear is small and in vol vedonly v aginal mucosa and connectiv e tissues and und erlying
muscles (first or second deg ree tear). Ifthe tear is not bleeding , leave the w ound open.
The tear is long and deep through the perineumand in vol vesthe anal sphincte r and rectal muco sa
(third and four th deg ree tear). Coveritwi th a clean pad and refer the woman urg ently to hospital B17.
If first or second deg ree tear and hea vy bleeding persists after applying pr essure o verthe wound:
Suture the tear or refer for suturing if no one is a vai lable with suturing s kills.
Suture the tear using univ ersal precautions, aseptic technique and sterile equipment.
Use a needle holder and a 21 g auge, 4 cm,curv ed needle.
Use absorbable polyglycon suture material.
Makesure that the apex of the tear is reached before y ou begin suturing .
Ensure that edg es of the tear match up w ell.
DO NO Tsuture if more than 12 hours since deliv ery . Refer woman to hospital.
Empty bladder
If bladder is distended and the w oman is unable to pass urine:
Encourage the w oman to urinate.
If she is unable to ur inate, catheterize the bladder :
Wa sh hands
Cl ean urethral ar ea with antiseptic
Put on clean glo ves
Spread labia. Cl ean area again
Insertcatheter up to 4 cm
Measure urine and r ecordamount
Remov e catheter .
ECLAMPSIA AND PRE-ECLAMPSIA (1)
Eclampsia and pre-eclampsia (1)
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B13
Givemagnesium sulphate
If se ver e pre-eclampsia and eclampsia
IV/IM combined dose (loading dose)
Insert IV line and giv e fluids slo wly (nor mal saline or Ring erslactate)
1 litre in 6-8 hours (3-ml/minute) B9.
Give4-g of magnesium sulphate (20 ml of 20% solution) IV slo wly o ver20mi nutes
(woman mayfeel war m during injection).
AND:
Give10 g of magnesium sulphate IM: giv e 5 g (10 ml of 50% solution) IMdeep in upper outer
quadrant of each buttock with 1 ml of 2% lignocaine in the same syri nge.
If unable to give IV , give IM only (loading dose)
Give10 g of magnesium sulphate IM: giv e 5 g (10 ml of 50% solution) IMdeep in upper outer
quadrant of each buttock with 1 ml of 2% lignocaine in the same syri nge.
If con vulsions recur
After 15 minutes, gi vean additional 2 g of magnesium sulphate (10 m l of 20% solution) IV
over20mi nutes. If con vulsions still continue, gi vediazepamB14.
If refer raldelayedfor long , or the woman is in late labour , continue treatment:
Give5 g of 50% magnesium sulphate solution IM with 1 ml of 2% l ignocaine e ver y 4 hours in
alternate buttocks until 24 hours after bir th or after last con vulsion (w hichev er is later).
Monitor urine output: collect urine and measure the quantity .
Before giving the next dose of magnesium sulphate, ensure:
knee jerk is present
ur ine output >100 ml/4 hrs
respirator y rate >16/min.
DO NO Tgi vethe next dose if an y of these signs:
knee jerk absent
urine output <100 ml/4 hrs
respirator y rate <16/min.
Record findings and dr ugs giv en.
Important considerations incaring for
a woman with eclampsia or pre -eclampsia
Donot lea vethe w oman on her o wn.
Help her into the le ft side position and protec t her fr om fall and injur y
Pl ace padded tong ue blades betw een her teeth to pre vent a tongue bite, and secure it to pre vent
aspiration ( DO NO Tattempt this during a con vulsion).
Gi veIV 20% magnesi um sulphate slo wly o ver20mi nutes. Rapid injection can cause respirator y
failure or death.
Ifrespirator y depre ssion(breathi ng less than 16/minute) occurs after magnesium sulph do
not giv e any more magnesium sulphate. Gi vethe antidote: calcium gluconate 1 g IV (10 ml
10% solution) o ver10mi nutes.
DO NO Tgi veintrav enous flui ds rapidly .
DO NO Tgi veintrav enously 50% magnesium sulphate without dilluting it to 20%.
Refer urg ently to hospit al unless deliv eryis imminent.
Ifdeliver y imminent, manageas in Childbir th D1-D29and accom panythe w oman duri ng
transpor t
Keep her in the lef t sidepositi on
Ifa convulsion occurs during the jour ney , givemagnesiumsulphate and protect her fromf all and
injury .
Formulation of magnesiu m sulphat e
50% solutio n: 20% solutio n: to mak e 10 ml of 20% sol ution, vial contain ing 5 g in 10 ml (1g/2ml) add 4 ml of 50% solution to 6 ml sterile water
IM 5 g 10 ml and 1 ml 2% lignocaine Not applicable
IV 4 g 8 ml 20 ml
2 g 4 ml 10 ml
After receiving magnes ium sulphate a w oman feel flushing , thirst, headache, nauseaormay vomit.
B9
AIRWAY, BREATHING AND
CIRCULATION
Manage the airway and breathing
Insert IV line and give fluids
B10 BLEEDING (1)
Massage uterus and expel clots
Apply bimanual uterine compression
Apply aortic compression
Give oxytocin
Give ergometrine
B11 BLEEDING (2)
Remove placenta and fragments manually
After manual removal of the placenta
B12 BLEEDING (3)
Repair the tear
Empty bladder
B13 ECLAMPSIA AND
PRE-ECLAMPSIA (1)
Important considerations in caring for a
woman with eclampsia and pre-eclampsia
Give magnesium sulphate
ECLAMPSIA AND PRE-ECLAMPSIA (2)
Eclampsia and pre-eclampsia (2)
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B14
Givediazepam
If con vulsions occur in ear ly pregnancy or
If magnesium sulphate toxicity occurs or magnesium sulphate is not a vai lable.
Loading dose IV
Gi vediazepam 10 mg IV slo wly o ver2 minutes.
Ifconvulsions recur , repeat 10 mg .
Maintenance dose
Gi vediazepam 40 mg in 500 ml IV fluids (nor mal saline or Ring erslactate) titrated o ver6-8 hours
to k eep the w oman sedated but rousable.
Stop the maintenance dose if breathing <16 breaths/minute.
Assist v entilation if necessar y with mask and bag .
Donot giv e more than 100 mg in 24 hours.
IfIVaccess is not possible (e.g . during con vulsion), givediazepam rectally .
Loading dose rectally
Gi ve20 mg (4 ml) in a 10 ml syring e (or urinar y catheter):
Remov e the needle, lubricate the bar rel and inser t the syring e into the rectu m to half its lengt h.
Di scharge the contents and lea vethe syring e in place, holding the buttocks tog ether for 10
minutes to pre vent expulsion of the dr ug.
Ifconvulsions recur , repeat 10 mg .
Maintenance dose
Gi veadditional 10 mg (2 ml) e ver y hour during transpor t.
Diazepam : vial containing 10 mg in 2 ml
IV Rectally
Initial dose 10mg= 2ml 20mg= 4ml
Second dose 10 mg = 2 ml 10 mg = 2 ml
Giveappropriate antihyper tensive drug
If diastolic blood pres sure is > 110-mmHg:
Gi vehydralazine 5 mg IV slo wly (3-4 mi nutes). IfIVnot possible giv e IM.
Ifdi astolic blood press ure remains > 90 mmHg , repeat the dos e at 30 minute inter val s until
diastolic BP is around 90 mmHg .
Donot giv e more tha n 20 mg in total.
INFECTION
Infection
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B15
Giveappropriate IV/IM antibiotics
Gi vethe first dose of antibiotic(s) before refer ral. If refer ral is dela yedornot possible, continue
antibiotics IM/IV for 48 hours after w oman is fe verfree.Then giv e amoxicillin ora lly 500 mg 3 times
daily until 7 da ys of treatment completed.
Ifsi gns persist or mother becomes w eak or has abdominal pain postpar tum, refer urg ently to hospital B17.
CONDITION ANTIBIO TICS
Sever e abdominal pain 3 antibiotics
Dangerous fever/ver y sever e febrile disease Ampicillin
Complicated abor tion Gentamicin
Ut erine and fetal infection Metronidazole
Postpartum bleeding 2 antibiotics :
lasting > 24 hours Ampicillin
occurr ing > 24 hours after deliv ery Gentamicin
Upper urinar y tract infection
Pneumonia
Manual remo valofpl acenta/fragments 1 antibiotic :
Ri sk of uterine and fetal infection Ampicillin
Inlabour > 24 hours
Antibiotic Prepar ation Dosag e/route Frequency
Ampicillin Vi al containing 500 mg as po wder: Fi rst 2 g IV/IM then 1 gevery6 hours
tobemi xed with 2.5 ml sterile water
Gentamicin Vi al containing 40 mg/ml in 2 ml 80 mg IM every8 hours
Metronidazole Vi al containing 500 mg in 100 ml 500 mg or 100 ml IV infusion e ver y 8 hours DONOT GIVE IM
Erythr omycin Vi al containing 500 mg as po wder 500 mg IV/IM every6 hours (if allerg y to ampicillin)
MALARIA
Malaria
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B16
Givearthemeter orquinine IM
If dang erous fe verorverysevere febrile disease
Arthemeter Quinine*
1ml vial containing 80 mg/ml 2 ml vial containing 300 mg/ml
Leading dose for 3.2 mg/kg 20 mg/kg
assumed weight 50-60 kg 2ml 4ml
Continue treatment 1.6 mg/kg 10 mg/kg
if unable to refer 1ml once daily for 3 da ys** 2ml/8 hours for a total of 7 da ys**
Gi vethe loading dose of the most effectiv e dr ug,according to the national policy .
Ifquinine:
di vide the required dose equally into 2 injections and giv e 1 in each anteri or thigh
al ways giveglucose with quinine.
Refer urg ently to hospital B17.
Ifdeliver y imminent or unable to refer immediately , continue treatment as abo veand refer after
deliver y.
* These dosages are for quinine dih ydrochloride. If quinine base, gi ve8.2 mg/kg e ver y 8 hours.
** Discontinue parenteral treatment as soon as w oman is conscious and able to s wallow . Begin oral
treatment according to national guidelines.
Giveglucose IV
If dang erous fe verorverysevere febrile disease treated with quinine
50% glucose solution* 25% glucose soluti on 10%glucose solution (5 ml/kg)
25-50 ml 50-10 0 ml 125-250 ml
Makesure IV drip is r unning w ell.Giveglucose byslowIV push.
IfnoIVgl ucose is a vai lable, givesugar water b y mouth ornasogastr ic tube.
Tomakesugar water, di ssolve 4 levelteaspoons of sug ar (20 g) in a 200 ml cup of clean water .
* 50%glucose solution is the same as 50% dextrose solution or D50. This solu tionis ir ritating to
vei ns.Dilute it with an equa l quantity of sterile water or saline to produce 25% glucose
REFER THE W OMAN URGENTL Y TO THE HOSPITAL
Refer the woman urgently to hospital
EM
ER
G
EN
C
Y
T
R
EA
T
M
EN
T
S FO
R
T
H
E WO
M
A
N
B17
Refer the w oman urg ently to hospital
Af ter emerg ency manag ement, discuss decision with w oman and relativ es.
Quickly org anize transpor t and possible financial aid.
Informthe refer ral centre if possible b y radio or phone.
Accompany the w oman if at all possible, orsend:
a health w orker trained in deliv erycare
a relativ e who can donate blood
baby with the mother , if possible
essential emerg ency dr ugs and supplies B17.
refer ral note N2.
During jour ney:
watch IV infusion
if jour neyis long , giveappropriate treatment on the wa y
keeprecord of all IV fluids, medications giv en,time of administratio n and the w omans condition.
Essential emerg ency dr ugs and supplies
for transpor t and ho me deliv ery
Emergency drugs Strength and F orm Quantit y for car ry
Oxytocin 10 IU vial 6
Ergometrine 0.2 mg vial 2
Magnesium sulphate 5 g vials (20 g) 4
Diazepam (parenteral ) 10mg vial 3
Calcium gluconate 1 g vial 1
Ampicillin 500 mg vial 4
Gentamicin 80 mg vial 3
Metronidazole 500 mg vial 2
Ringer s lactate 1 litre bottle 4 (ifdi stant refer ral)
Emergency supplies
IV catheters and tubin g 2sets
Glov es 2pairs, atleast,one pair sterile
Sterile syring es and needles 5 sets
Urinar y catheter 1
Antiseptic solution 1 small bottle
Container for sharps 1
Bag for trash 1
Tor ch and extra batter y 1
If deliver y is anticipated onthe way
Soap, towels 2sets
Disposable deliv erykit (blade, 3 t ies) 2sets
Clean cloths (3) for recei ving, drying and wrapping the bab y 1set
Clean clothes for the bab y 1set
Plastic bag for placenta 1 set
Resuscitation bag and mask for the bab y 1set
B14 ECLAMPSIA AND
PRE-ECLAMPSIA (2)
Give diazepam
Give appropriate antihypertensive
B15 INFECTION
Give appropriate IV/IM antibiotics
B16 MALARIA
Give artemether or quinine IM
Give glucose IV
B17 REFER THE WOMAN URGENTLY
TO THE HOSPITAL
Refer the woman urgently to the hospital
Essential emergency drugs and supplies
for transport and home delivery
This section has details on emergency treatments identified
during Rapid assessment and management (RAM)
B3-B6
to be
given before referral.
Give the treatment and refer the woman urgently to hospital
B17.
If drug treatment, give the first dose of the drugs before referral.
Do not delay referral by giving non-urgent treatments.
AIRWAY, BREATHING AND CIRCULATION
Airway, breathing and circulation
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B9
Manage the airway and breathing
If the woman has great difficulty breathing and:
If you suspect obstruction:
Try to clear the airway and dislodge obstruction
Help the woman to find the best position for breathing
Urgently refer the woman to hospital.
If the woman is unconscious:
Keep her on her back, arms at the side
Tilt her head backwards (unless trauma is suspected)
Lift her chin to open airway
Inspect her mouth for foreign body; remove if found
Clear secretions from throat.
If the woman is not breathing:
Ventilate with bag and mask until she starts breathing spontaneously
If woman still has great difficulty breathing, keep her propped up, and
Refer the woman urgently to hospital.
Insert IV line and give fluids
Wash hands with soap and water and put on gloves.
Clean womans skin with spirit at site for IV line.
Insert an intravenous line (IV line) using a 16-18 gauge needle.
Attach Ringers lactate or normal saline. Ensure infusion is running well.
Give fluids at rapid rate if shock, systolic BP<90 mmHg, pulse>110/minute, or heavy vaginal bleeding:
Infuse 1 litre in 15-20 minutes (as rapid as possible).
Infuse 1 litre in 30 minutes at 30 ml/minute. Repeat if necessary.
Monitor every 15 minutes for:
blood pressure (BP) and pulse
shortness of breath or puffiness.
Reduce the infusion rate to 3 ml/minute (1 litre in 6-8 hours) when pulse slows to less than 100/
minute, systolic BP increases to 100 mmHg or higher.
Reduce the infusion rate to 0.5 ml/minute if breathing difficulty or puffiness develops.
Monitor urine output.
Record time and amount of fluids given.
Give fluids at moderate rate if severe abdominal pain, obstructed labour, ectopic pregnancy, dangerous
fever or dehydration:
Infuse 1 litre in 2-3 hours.
Give fluids at slow rate if severe anaemia/severe pre-eclampsia or eclampsia:
Infuse 1 litre in 6-8 hours.
If intravenous access not possible
Give oral rehydration solution (ORS) by mouth if able to drink, or by nasogastric (NG) tube.
Quantity of ORS: 300 to 500 ml in 1 hour.
DO NOT give ORS to a woman who is unconscious or has convulsions.
BLEEDING
Bleeding (1)
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B10
Massage uterus and expel clots
If heavy postpartum bleeding persists after placenta is delivered, or uterus is not well contracted (is soft):
Place cupped palm on uterine fundus and feel for state of contraction.
Massage fundus in a circular motion with cupped palm until uterus is well contracted.
When well contracted, place fingers behind fundus and push down in one swift action to expel clots.
Collect blood in a container placed close to the vulva. Measure or estimate blood loss, and record.
Apply bimanual uterine compression
If heavy postpartum bleeding persists despite uterine massage, oxytocin/ergometrine treatment and
removal of placenta:
Wear sterile or clean gloves.
Introduce the right hand into the vagina, clenched fist, with the back of the hand directed posteriorly
and the knuckles in the anterior fornix.
Place the other hand on the abdomen behind the uterus and squeeze the uterus firmly between the
two hands.
Continue compression until bleeding stops (no bleeding if the compression is released).
If bleeding persists, apply aortic compression and transport woman to hospital.
Apply aortic compression
If heavy postpartum bleeding persists despite uterine massage, oxytocin/ergometrine treatment and
removal of placenta:
Feel for femoral pulse.
Apply pressure above the umbilicus to stop bleeding. Apply sufficient pressure until femoral pulse is not felt.
After finding correct site, show assistant or relative how to apply pressure, if necessary.
Continue pressure until bleeding stops. If bleeding persists, keep applying pressure while transporting
woman to hospital.
Give oxytocin
If heavy postpartum bleeding
Initial dose Continuing dose Maximum dose
IM/IV: 10 IU IM/IV: repeat 10 IU
after 20 minutes Not more than 3 litres
if heavy bleeding persists of IV fluids containing
IV infusion: IV infusion: oxytocin
20 IU in 1 litre 10 IU in 1 litre
at 60 drops/min at 30 drops/min
Give ergometrine
If heavy bleeding in early pregnancy or postpartum bleeding (after oxytocin) but
DO NOT give if eclampsia, pre-eclampsia, or hypertension
Initial dose Continuing dose Maximum dose
IM/IV:0.2 mg IM: repeat 0.2 mg Not more than
slowly IM after 15 minutes if heavy 5 doses (total 1.0 mg)
bleeding persists
Bleeding (2)
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B11
Remove placenta and fragments manually
If placenta not delivered 1 hour after delivery of the baby, OR
If heavy vaginal bleeding continues despite massage and oxytocin and placenta cannot be delivered
by controlled cord traction, or if placenta is incomplete and bleeding continues.
Preparation
Explain to the woman the need for manual removal of the placenta and obtain her consent.
Insert an IV line. If bleeding, give fluids rapidly. If not bleeding, give fluids slowly B9 .
Assist woman to get onto her back.
Give diazepam (10-mg IM/IV).
Clean vulva and perineal area.
Ensure the bladder is empty. Catheterize if necessary B12 .
Wash hands and forearms well and put on long sterile gloves (and an apron or gown if available).
Technique
With the left hand, hold the umbilical cord with the clamp. Then pull the cord gently until it is
horizontal.
Insert right hand into the vagina and up into the uterus.
Leave the cord and hold the fundus with the left hand in order to support the fundus of the uterus
and to provide counter-traction during removal.
Move the fingers of the right hand sideways until edge of the placenta is located.
Detach the placenta from the implantation site by keeping the fingers tightly together and using the
edge of the hand to gradually make a space between the placenta and the uterine wall.
Proceed gradually all around the placental bed until the whole placenta is detached from the uterine
wall.
Withdraw the right hand from the uterus gradually, bringing the placenta with it.
Explore the inside of the uterine cavity to ensure all placental tissue has been removed.
With the left hand, provide counter-traction to the fundus through the abdomen by pushing it in the
opposite direction of the hand that is being withdrawn. This prevents inversion of the uterus.
Examine the uterine surface of the placenta to ensure that lobes and membranes are complete. If
any placental lobe or tissue fragments are missing, explore again the uterine cavity to remove them.
If hours or days have passed since delivery, or if the placenta is retained due to constriction ring
or closed cervix, it may not be possible to put the hand into the uterus. DO NOT persist. Refer
urgently to hospital B17 .
If the placenta does not separate from the uterine surface by gentle sideways movement of the
fingertips at the line of cleavage, suspect placenta accreta. DO NOT persist in efforts to remove
placenta. Refer urgently to hospital B17 .
After manual removal of the placenta
Repeat oxytocin 10-IU IM/IV.
Massage the fundus of the uterus to encourage a tonic uterine contraction.
Give ampicillin 2 g IV/IM B15 .
If fever >38.5C, foul-smelling lochia or history of rupture of membranes for 18 or more hours, also
give gentamicin 80 mg IM B15 .
If bleeding stops:
give fluids slowly for at least 1 hour after removal of placenta.
If heavy bleeding continues:
give ergometrine 0.2 mg IM
give 20 IU oxytocin in each litre of IV fluids and infuse rapidly
Refer urgently to hospital B17 .
During transportation, feel continuously whether uterus is well contracted (hard and round). If not,
massage and repeat oxytocin 10 IU IM/IV.
Provide bimanual or aortic compression if severe bleeding before and during transportation B10 .
REPAIR THE TEAR AND EMPTY BLADDER
Bleeding (3)
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B12
Repair the tear or episiotomy
Examine the tear and determine the degree:
The tear is small and involved only vaginal mucosa and connective tissues and underlying
muscles (first or second degree tear). If the tear is not bleeding, leave the wound open.
The tear is long and deep through the perineum and involves the anal sphincter and rectal mucosa
(third and fourth degree tear). Cover it with a clean pad and refer the woman urgently to hospital B17 .
If first or second degree tear and heavy bleeding persists after applying pressure over the wound:
Suture the tear or refer for suturing if no one is available with suturing skills.
Suture the tear using universal precautions, aseptic technique and sterile equipment.
Use a needle holder and a 21 gauge, 4 cm, curved needle.
Use absorbable polyglycon suture material.
Make sure that the apex of the tear is reached before you begin suturing.
Ensure that edges of the tear match up well.
DO NOT suture if more than 12 hours since delivery. Refer woman to hospital.
Empty bladder
If bladder is distended and the woman is unable to pass urine:
Encourage the woman to urinate.
If she is unable to urinate, catheterize the bladder:
Wash hands
Clean urethral area with antiseptic
Put on clean gloves
Spread labia. Clean area again
Insert catheter up to 4 cm
Measure urine and record amount
Remove catheter.
ECLAMPSIA AND PRE-ECLAMPSIA (1)
Eclampsia and pre-eclampsia (1)
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B13
Give magnesium sulphate
If severe pre-eclampsia and eclampsia
IV/IM combined dose (loading dose)
Insert IV line and give fluids slowly (normal saline or Ringers lactate)
1 litre in 6-8 hours (3-ml/minute) B9 .
Give 4-g of magnesium sulphate (20 ml of 20% solution) IV slowly over 20 minutes
(woman may feel warm during injection).
AND:
Give 10 g of magnesium sulphate IM: give 5 g (10 ml of 50% solution) IM deep in upper outer
quadrant of each buttock with 1 ml of 2% lignocaine in the same syringe.
If unable to give IV, give IM only (loading dose)
Give 10 g of magnesium sulphate IM: give 5 g (10 ml of 50% solution) IM deep in upper outer
quadrant of each buttock with 1 ml of 2% lignocaine in the same syringe.
If convulsions recur
After 15 minutes, give an additional 2 g of magnesium sulphate (10 ml of 20% solution) IV
over 20 minutes. If convulsions still continue, give diazepam B14 .
If referral delayed for long, or the woman is in late labour, continue treatment:
Give 5 g of 50% magnesium sulphate solution IM with 1 ml of 2% lignocaine every 4 hours in
alternate buttocks until 24 hours after birth or after last convulsion (whichever is later).
Monitor urine output: collect urine and measure the quantity.
Before giving the next dose of magnesium sulphate, ensure:
knee jerk is present
urine output >100 ml/4 hrs
respiratory rate >16/min.
DO NOT give the next dose if any of these signs:
knee jerk absent
urine output <100 ml/4 hrs
respiratory rate <16/min.
Record findings and drugs given.
Important considerations in caring for
a woman with eclampsia or pre-eclampsia
Do not leave the woman on her own.
Help her into the left side position and protect her from fall and injury
Place padded tongue blades between her teeth to prevent a tongue bite, and secure it to prevent
aspiration (DO NOT attempt this during a convulsion).
Give IV 20% magnesium sulphate slowly over 20 minutes. Rapid injection can cause respiratory
failure or death.
If respiratory depression (breathing less than 16/minute) occurs after magnesium sulphate, do
not give any more magnesium sulphate. Give the antidote: calcium gluconate 1 g IV (10 ml of
10% solution) over 10 minutes.
DO NOT give intravenous fluids rapidly.
DO NOT give intravenously 50% magnesium sulphate without dilluting it to 20%.
Refer urgently to hospital unless delivery is imminent.
If delivery imminent, manage as in Childbirth D1-D29 and accompany the woman during
transport
Keep her in the left side position
If a convulsion occurs during the journey, give magnesium sulphate and protect her from fall and
injury.
Formulation of magnesium sulphate
50% solution: 20% solution: to make 10 ml of 20% solution,
vial containing 5 g in 10 ml (1g/2ml) add 4 ml of 50% solution to 6 ml sterile water
IM 5 g 10 ml and 1 ml 2% lignocaine Not applicable
IV 4 g 8 ml 20 ml
2 g 4 ml 10 ml
After receiving magnesium sulphate a woman feel flushing, thirst, headache, nausea or may vomit.
ECLAMPSIA AND PRE-ECLAMPSIA (2)
Eclampsia and pre-eclampsia (2)
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B14
Give diazepam
If convulsions occur in early pregnancy or
If magnesium sulphate toxicity occurs or magnesium sulphate is not available.
Loading dose IV
Give diazepam 10 mg IV slowly over 2 minutes.
If convulsions recur, repeat 10 mg.
Maintenance dose
Give diazepam 40 mg in 500 ml IV fluids (normal saline or Ringers lactate) titrated over 6-8 hours
to keep the woman sedated but rousable.
Stop the maintenance dose if breathing <16 breaths/minute.
Assist ventilation if necessary with mask and bag.
Do not give more than 100 mg in 24 hours.
If IV access is not possible (e.g. during convulsion), give diazepam rectally.
Loading dose rectally
Give 20 mg (4 ml) in a 10 ml syringe (or urinary catheter):
Remove the needle, lubricate the barrel and insert the syringe into the rectum to half its length.
Discharge the contents and leave the syringe in place, holding the buttocks together for 10
minutes to prevent expulsion of the drug.
If convulsions recur, repeat 10 mg.
Maintenance dose
Give additional 10 mg (2 ml) every hour during transport.
Diazepam: vial containing 10 mg in 2 ml
IV Rectally
Initial dose 10 mg = 2 ml 20 mg = 4 ml
Second dose 10 mg = 2 ml 10 mg = 2 ml
Give appropriate antihypertensive drug
If diastolic blood pressure is > 110-mmHg:
Give hydralazine 5 mg IV slowly (3-4 minutes). If IV not possible give IM.
If diastolic blood pressure remains > 90 mmHg, repeat the dose at 30 minute intervals until
diastolic BP is around 90 mmHg.
Do not give more than 20 mg in total.
INFECTION
Infection
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B15
Give appropriate IV/IM antibiotics
Give the first dose of antibiotic(s) before referral. If referral is delayed or not possible, continue
antibiotics IM/IV for 48 hours after woman is fever free. Then give amoxicillin orally 500 mg 3 times
daily until 7 days of treatment completed.
If signs persist or mother becomes weak or has abdominal pain postpartum, refer urgently to hospital B17 .
CONDITION ANTIBIOTICS
Severe abdominal pain 3 antibiotics
Dangerous fever/very severe febrile disease Ampicillin
Complicated abortion Gentamicin
Uterine and fetal infection Metronidazole
Postpartum bleeding 2 antibiotics:
lasting > 24 hours Ampicillin
occurring > 24 hours after delivery Gentamicin
Upper urinary tract infection
Pneumonia
Manual removal of placenta/fragments 1 antibiotic:
Risk of uterine and fetal infection Ampicillin
In labour > 24 hours
Antibiotic Preparation Dosage/route Frequency
Ampicillin Vial containing 500 mg as powder: First 2 g IV/IM then 1 g every 6 hours
to be mixed with 2.5 ml sterile water
Gentamicin Vial containing 40 mg/ml in 2 ml 80 mg IM every 8 hours
Metronidazole Vial containing 500 mg in 100 ml 500 mg or 100 ml IV infusion every 8 hours
DO NOT GIVE IM
Erythromycin Vial containing 500 mg as powder 500 mg IV/IM every 6 hours
(if allergy to ampicillin)
MALARIA
Malaria
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B16
Give arthemeter or quinine IM
If dangerous fever or very severe febrile disease
Arthemeter Quinine*
1ml vial containing 80 mg/ml 2 ml vial containing 300 mg/ml
Leading dose for 3.2 mg/kg 20 mg/kg
assumed weight 50-60 kg 2 ml 4 ml
Continue treatment 1.6 mg/kg 10 mg/kg
if unable to refer 1 ml once daily for 3 days** 2 ml/8 hours for a total of 7 days**
Give the loading dose of the most effective drug, according to the national policy.
If quinine:
divide the required dose equally into 2 injections and give 1 in each anterior thigh
always give glucose with quinine.
Refer urgently to hospital B17 .
If delivery imminent or unable to refer immediately, continue treatment as above and refer after
delivery.
* These dosages are for quinine dihydrochloride. If quinine base, give 8.2 mg/kg every 8 hours.
** Discontinue parenteral treatment as soon as woman is conscious and able to swallow. Begin oral
treatment according to national guidelines.
Give glucose IV
If dangerous fever or very severe febrile disease treated with quinine
50% glucose solution* 25% glucose solution 10% glucose solution (5 ml/kg)
25-50 ml 50-100 ml 125-250 ml
Make sure IV drip is running well. Give glucose by slow IV push.
If no IV glucose is available, give sugar water by mouth or nasogastric tube.
To make sugar water, dissolve 4 level teaspoons of sugar (20 g) in a 200 ml cup of clean water.
* 50% glucose solution is the same as 50% dextrose solution or D50. This solution is irritating to
veins. Dilute it with an equal quantity of sterile water or saline to produce 25% glucose solution.
REFER THE WOMAN URGENTLY TO THE HOSPITAL
Refer the woman urgently to hospital
E
M
E
R
G
E
N
C
Y
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
B17
Refer the woman urgently to hospital
After emergency management, discuss decision with woman and relatives.
Quickly organize transport and possible financial aid.
Inform the referral centre if possible by radio or phone.
Accompany the woman if at all possible, or send:
a health worker trained in delivery care
a relative who can donate blood
baby with the mother, if possible
essential emergency drugs and supplies B17 .
referral note N2 .
During journey:
watch IV infusion
if journey is long, give appropriate treatment on the way
keep record of all IV fluids, medications given, time of administration and the womans condition.
Essential emergency drugs and supplies
for transport and home delivery
Emergency drugs Strength and Form Quantity for carry
Oxytocin 10 IU vial 6
Ergometrine 0.2 mg vial 2
Magnesium sulphate 5 g vials (20 g) 4
Diazepam (parenteral) 10 mg vial 3
Calcium gluconate 1 g vial 1
Ampicillin 500 mg vial 4
Gentamicin 80 mg vial 3
Metronidazole 500 mg vial 2
Ringers lactate 1 litre bottle 4 (if distant referral)
Emergency supplies
IV catheters and tubing 2 sets
Gloves 2 pairs, at least, one pair sterile
Sterile syringes and needles 5 sets
Urinary catheter 1
Antiseptic solution 1 small bottle
Container for sharps 1
Bag for trash 1
Torch and extra battery 1
If delivery is anticipated on the way
Soap, towels 2 sets
Disposable delivery kit (blade, 3 ties) 2 sets
Clean cloths (3) for receiving, drying and wrapping the baby 1 set
Clean clothes for the baby 1 set
Plastic bag for placenta 1 set
Resuscitation bag and mask for the baby 1set
Antenatal care
A
N
T
E
N
A
T
A
L
C
A
R
E
Always begin with Rapid assessment and management (RAM) B3-B7 . If the woman has no
emergency or priority signs and has come for antenatal care, use this section for further care.
Next use the Pregnancy status and birth plan chart C2 to ask the woman about her present
pregnancy status, history of previous pregancies, and check her for general danger signs. Decide on
an appropriate place of birth for the woman using this chart and prepare the birth and emergency
plan. The birth plan should be reviewed during every follow-up visit.
Check all women for pre-eclampsia, anaemia, syphilis and HIV status according to the charts C3-C6 .
In cases where an abnormal sign is identified (volunteered or observed), use the charts Respond to
observed signs or volunteered problems C7-C11 to classify the condition and identify appropriate
treatment(s).
Give preventive measures due C12 .
Develop a birth and emergency plan C14-C15 .
Advise and counsel on nutrition C13 , family planning C16 , labour signs, danger signs C15 , routine
and follow-up visits C17 using Information and Counselling sheets M1-M19.
Record all positive findings, birth plan, treatments given and the next scheduled visit in the home-
based maternal card/clinic recording form.
Assess eligibility of ARV for HIV-positive woman C19 .
If the woman is HIV positive, adolescent or has special needs, see G1-G11 H1-H4 .
ANTENATAL CARE
Antenatal care
A
N
T
E
N
A
T
A
L
C
A
R
E
C1
Assess the pregnant woman Pregancy status, bi rthand emergenc y plan
AN
TEN
ATAL CARE
ASK, CHECK, RECORD
ALL VISITS Check duration of pregnancy . Wh ere do y ou plan to deliv er? Any vaginal bleeding since last visit? Isthe bab y mo ving? (after 4 months) Check record for pre vious complications and treatments receiv ed during this pregnancy . Doyou ha veanyconcerns?
FIRST VISIT How man y months pregnant are y ou? Wh en was y our last period? Wh en do y ou expect to deliv er? How old are y ou? Haveyouhad a bab y before? If y es: Check record for prior pregnancies or if there is no record ask about: Number of prior pregnancies/deliv eries Pr ior caesarean section, forceps, or v acuum Pr ior third deg ree tear Heavybl eeding during or after deliv ery Convulsions Stillbirth or death in first da y. Doyou smok e,drink alcohol or use an y dr ugs?
THIRD TRIMESTER Has she been counselled on family planning? If y es,does she want tubal lig ation or IUD A15.
LOOK, LISTEN, FEEL
Feel for trimester of pr egnancy.
Look for caesarean scar
Feel for ob vious multiple pregnancy. Feel for transv erse lie. Li sten to fetal hear t.
INDICATIONS
Pr ior deliv erybycaesarean. Age less than 14 y ears. Tr ansverse lie or other ob vious malpresentation within one month of expected deliv ery . Obvious multiple pregnancy . Tubal lig ation or IUD desired immediately after deliv ery . Documented third deg ree tear . Hi story of or cur rent v aginal bleeding or other complication during this pregnancy .
Fi rst bir th. Last bab y bor n dead or died in f irst day . Age less than 16 y ears. More than six pre vious bir ths. Pr ior deliv erywith hea vy bleeding . Pr ior deliv erywith con vulsions. Pr ior deliv erybyforceps or v acuum. HI V-positive woman.
None of the abo ve.
ADVISE
Explain w hydeliver y needs to be at referr al levelC14. Devel op the bir th andemergency planC14.
Explain w hydeliv eryneeds to be at primar y health care le velC14. Devel op the bir th andemergency planC14.
Explain w hydeliv eryneeds to be with a skilled bi rth attendant , prefe rablyat a facil ity. Devel op the bir th andemergency planC14.
PLACE OF DELIVERY
REFERRAL LEVEL
PRIMAR Y HEALTH CARE LEVEL
ACCORDING T O WOMANS PREFERENC E
NEXT : Check for pre-eclampsia
ASSESS THE PREGNANT W OMAN: PREGNANCY ST ATUS, BIRTH AND EMERGENCY PLAN
Use this char t to assess the pre gnant woman at each of the four antenatal care visits. During first antenatal visit, prepare a bir th and emerg ency plan using this char t
and review them during following visits. Modify the bir th plan if an y complications arise.
C2
Assess the pregnant woman Check for pre-eclampsia
ASK, CHECK RECORD
Blood pressure at the last visit?
LOOK, LISTEN, FEEL
Measure blood pressure in sitting position. Ifdi astolic blood pressure is90 mmHg, repeat after 1 hour rest. Ifdi astolic blood pressure is still 90 mmHg, ask the w oman if she has: sever e headache bl urr ed vision epigastric pain and check protein in urine.
SIGNS
Di astolic blood pressure 110 mmHg and 3+ proteinuria, or Di astolic blood pressure 90-mmHg on tw o readings and 2+ proteinuria, and an y of: sever e headache bl urr ed vision epigastric pain.
Di astolic blood pressure 90-110-mmHg on tw o readings and 2+ proteinuria.
Di astolic blood pressure 90 mmHg on 2 readings.
None of the abo ve.
TREAT AND AD VISE
Gi vemagnesium sulphate B13. Gi veappropria te anti-h ypertensiv esB14. Revise the bir th planC2. Refer urg ently to hospita l B17.
Revise the bir th planC2. Refer to hospital.
Advise to reduce w orkload and to rest. Advise on dang er sign s C15. Reassessatthe next antenatal visit or in 1 w eek if >8 month s pregnant. Ifhypertension persists after 1 week or at next visit, refer to hospital or discuss case with the doct midwif e,if avai lable.
No treatment required.
CLASSIFY
SEVERE PRE-ECLAMPSIA
PRE-ECLAMPSIA
HYPERTENSION
NO HYPERTENS ION
NEXT : Check for anaemia
CHECK FOR PRE-ECLAMPSIA
Screen all pre gnant women at ever y visit.
AN
TEN
ATAL CARE
C3
Assess the pregnant woman Check for anaemia
AN
TEN
ATAL CARE
ASK, CHECK RECORD
Doyou tire easily? Ar e you breathless (shor t of breath) during routine household w ork?
LOOK, LISTEN, FEEL
On first visit: Measure haemoglobin
On subsequent visits: Look for conjunctiv al pallor . Look for palmar pallor . If pallor : Isitsever e pallor? Some pallor? Count number of breat hs in 1 minute.
SIGNS
Haemoglobin <7-g/dl. AND/OR Sever e palmar and conj unctival pallor or
Any pallor with an y of >30 breaths per min ute ti res easily breathlessness at rest
Haemoglobin 7-11-g/dl. OR Palmar or conjunctiv al pallor .
Haemoglobin >11-g/dl. Nopallor.
TREAT AND AD VISE
Revise bir th plan so as to deliv er in a faci lity with bloodtransfus ion ser vicesC2. Gi vedouble dose of iron (1 tablet twice daily) for 3 months F3. Counsel on compliance with treatment F3. Gi veappropria te oral antimalarial F4. Followup in 2 w eeks to check cli nical prog ress, test results, and compliance with treatment. Refer urg ently to hospita l B17.
Gi vedouble dose of iron (1 tablet twice daily) for 3 months F3. Counsel on compliance with treatment F3. Gi veappropria te oral antimalarial if not giv en in the past month F4. Reassessatnext antenatal visit (4-6 w eeks). If anaemia persists, refer to hospital.
Gi veiron 1 tablet once daily for 3 month s F3. Counsel on compliance with treatment F4.
CLASSIFY
SEVERE ANAEMIA
MODERATE ANAEMIA
NO CLINIC AL ANAEMIA
NEXT : Check for syphilis
CHECK FOR ANAEMIA
Screen all pre gnant women at ever y visit.
C4
Assess the pregnant woman Check for syphilis
ASK, CHECK RECORD
Haveyoubeen tested for syphilis during this pregnancy? Ifnot,perfor m the rapid plasma reagin (RPR) test L5. Iftest was positiv e,have you and your par tner been treated for syphilis? Ifnot,and test is positiv e,ask Ar e you allergic to penicillin?
LOOK, LISTEN, FEEL TEST RESUL T
RPR test positiv e.
RPR test neg ative.
TREAT AND AD VISE
Givebenzathine benzylpenicillin IM. Ifal lergy , give erythr omycinF6. Pl an to treat the ne wbornK12. Encourag e woman to bring her sexual par tnerfor treatment. Counsel on safer sex including use of condoms t prev ent ne w infection G2.
Counsel on safer sex including use of condoms t prev ent infection G2.
CLASSIFY
POSSIBLE SYPHILIS
NO SYPHILIS
NEXT : Check for HIV status
CHECK FOR SYPHILIS
Test all pre gnant women at first visit. Check status at ever y visit.
AN
TEN
ATAL CARE
C5
Assess the pregnant woman Check for HIV status
AN
TEN
ATAL CARE
ASK, CHECK RECORD
Provide k ey infor mation on HIV G2. Wh at is HIV and ho w is HIV transmit- tedG2? Advantageof kno wing the HIV status in pregnancy G2. Explain about HIV testing and counselling including confidentiality of the result G3.
Ask the woman: Haveyoubeen tested for HIV? If not: tell her that she will be tested for HIV , unless she refuses. If y es: Check result. (Explain to her that she has a right not to disclose the result.) Ar e you taking an y AR V? Check AR V treatment plan. Has the par tner been tested?
LOOK, LISTEN, FEEL
Per formthe Rapid HIV test ifnot perfor med in this pregnanc y L6.
SIGNS
PositiveHIV-positive.
Negat iveHIV test.
She refuses the tes t or is not willin g to disclose the result of pre vious test or no test results a vai lable.
TREAT AND AD VISE
Counsel on implications ofa positi vetestG3. If HIV ser vices a vai lable: Refer the w oman to HIV ser vices for fur ther assess ment. Ask her to returnin 2 w eeks with her documents. If HIV ser vices are not a vai lable: Determine the se ver ity of the disease and assess eligibil ity for ARVsC19. Gi veher appro priate AR V G6, G9. Forall women: Support adherence to ARVG6. Counsel on infant feeding options G7. Pr ovi de additional care for HIV- positive woman G4. Counsel on family planning G4. Counsel on safer sex including use of condoms G2. Counsel on benefits of disclosure (in vol ving) and testing her par tnerG3. Pr ovi de suppor t to the HIV-positiv e womanG5.
Counsel on implication s of a ne gative testG3. Counsel on the impor tance of sta ying neg ative by practising safer sex, including use of condoms G2. Counsel on benefits of in vol ving and testing the partner G3.
Counsel on safer sex including use of condoms G2. Counsel on benefits of in vol ving and testi ng the partner G3.
CLASSIFY
HIV-POSITI VE
HIV-NEGATIVE
UNKNOWN HIV ST ATUS
NEXT : Respond to obser vedsigns or v olunteered problems
If no problem, gotopageC12.
CHECK FOR HIV ST ATUS
Test and counsel all pre gnant women for HIV at the first antenatal visit. Check status at ever y visit.
Inform the w omen that HIV test will be done routinely and t hat she may refuse the HI V test.
C6
IF RUPTURED MEMBRANES AND NO LAB OUR
Respond to obser ved signs or volunteered problems (1)
ASK, CHECK RECORD
Wh en did the bab y last mo ve? Ifnomovement felt, ask woman to mo vearound for some time, reassess fetal mo vement.
Wh en did the membranes r upture? Wh en is y our bab y due?
LOOK, LISTEN, FEEL
Feel for fetal mo vements. Li sten for fetal hear t after 6 months of pregnancy D2. Ifnoheartbeat, repeat after 1 hour .
Look at pad or underw ear for evi dence of: amniotic fluid foul-smelling v aginal discharg e Ifnoevidence, ask her to w ear a pad. Check ag ain in 1 hour . Measure temperature.
SIGNS
Nofetal mo vement. Nofetal hear t beat.
Nofetal mo vement but fetal hear t beat present.
Fever38C. Foul-smelling v aginal discharg e.
Rupture of membranes at <8 months of pregnancy .
Rupture of membranes at >8 months of pregnancy .
TREAT AND AD VISE
Informthe w oman and par tner about the possibility of dead bab y. Refer to hospital.
Informthe w oman that babyis fine and lik ely to be wel l but to retur n if pr oblem persists.
Gi veappropria te IM/IV antibiotics B15. Refer urg ently to hospita l B17.
Gi veappropria te IM/IV antibiotic B15. Refer urg ently to hospita l B17.
Manageas Woman in childbir thD1-D28 .
CLASSIFY
PROBABL Y DEAD BABY
WELL BABY
UTERINE AND FETAL INFECTION
RISK OF UTERINE AND FET AL INFECTI ON
RUPTURE OF MEMBRANES
NEXT : If fe verorburni ng on urination
RESPOND T O OBSER VED SIGNS OR VOL UNTEERED PR OBLEMS
AN
TEN
ATAL CARE
C7
IF NO FET AL MO VEMENT
C2 ASSESS THE PREGNANT WOMAN:
PREGNANCY STATUS, BIRTH AND
EMERGENCY PLAN
C3 CHECK FOR PRE-ECLAMPSIA
C4 CHECK FOR ANAEMIA
C5 CHECK FOR SYPHILIS
C6 CHECK FOR HIV STATUS
C7 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (1)
If no fetal movement
If ruptured membrane and no labour
Respond to obser ved signs or volunteered problems (2)
AN
TEN
ATAL CARE
ASK, CHECK RECORD
Haveyouhad fever ? Doyou ha veburning on urination?
LOOK, LISTEN, FEEL
Ifhi story of fe verorfeels hot: Measure axillar y temperature. Look or feel for stiff ne ck. Look for letharg y. Percuss flanks for tenderness.
SIGNS
Fever>38C and an y of: veryfast breathing or stiff neck lethargy veryweak/not able to stand.
Fever>38C and an y of: Fl ank pain Burni ng on urination.
Fever>38C or histor y of fe ver (in last 48 hours).
Burni ng on urination.
TREAT AND AD VISE
InsertIV line and giv e fluids slo wlyB9. Gi veappropria te IM/IV antibiotics B15. Gi veartemet her/quinine IM B16. Gi veglucose B16. Refer urg ently to hospita l B17.
Gi veappropria te IM/IV antibiotics B15. Gi veappropria te oral antimalarial F4. Refer urg ently to hospita l B17.
Gi veappropria te oral antimalarial F4. Ifnoimprov ement in 2 da ys or condition is w orse, refer to hospital.
Gi veappropria te oral antibiotics F5. Encourag e her to drink more fluids. Ifnoimprov ement in 2 da ys or condition is w orse, refer to hospital.
CLASSIFY
VERYSEVERE FEBRILE DISEASE
UPPER URINAR Y TRA CT INFECTION
MALARIA
LOWER URINAR Y TRA CT INFECTION
NEXT : If v aginal discharg e
IF FEVER OR BURNING ON URINA TION
C8
Respond to obser ved signs or volunteered problems (3)
ASK, CHECK RECORD
Haveyounoticed chang es in y our vaginal discharg e? Doyou ha veitching at the vulv a? Has your par tner had a urinar y problem?
If par tner is present in the clinic, ask the w oman if she feels comfor table if youask him similar questions. If y es,ask him if he has: ur ethral discharg e or pus. burni ng on passing urine.
If par tner could not be approached, explain impor tance of par tner assessment and treatment to a voi d reinfection. Schedule follo w-up appointment for woman and par tner (if possible).
LOOK, LISTEN, FEEL
Separate the labia and loo k for abnormal vaginal discharg e: amount colour odour/smell. Ifnodi scharge is seen, examine with a glo vedfi nger and look at the discharge on the glo ve.
SIGNS
Abnormal vaginal discharg e. Partner has urethral dischar geor burning on passing urine.
Curd lik e vaginal discharg e. Intense vulv al itching .
Abnormal vaginal discharg e
TREAT AND AD VISE
Gi veappropria te oral antibiotics to w omanF5. Tr eat par tner with appropriate oral antibiotics F5. Counsel on safer sex including use of condoms G2.
Gi veclotrima zoleF5. Counsel on safer sex including use of condoms G2.
Gi vemetronida zole to w omanF5. Counsel on safer sex including use of condoms G2.
CLASSIFY
POSSIBLE GONORRHOEA OR CHLAMYDIA INFECTION
POSSIBLE CANDID A INFECTIO N
POSSIBLE BACTERIA L OR TRICHOMO NAS INFECTION
NEXT : If signs sugg esting HIV infection
IF VAGI NAL DISCHARGE
AN
TEN
ATAL CARE
C9
Respond to obser ved signs or volunteered problems (4)
AN
TEN
ATAL CARE
ASK, CHECK RECORD
Haveyoulost weight? Doyou ha vefever? Howlong (>1 month)? Haveyougot diar rhoea (continuous or inter mittent)? Howlong, >1month? Haveyouhad cough? Howlong, >1month?
Assess if in high risk g roup: Occupational exposure? Multiple sexual par tner? Intrav enous dr ug abuse? Hi story of blood transfusion? Il lness or death from AIDS in a sexual par tner? Hi story of forced sex?
LOOK, LISTEN, FEEL
Look for visible wasting . Look for ulcers and w hite patches in the mouth (thr ush). Look at the skin: Isthere a rash? Ar e there blisters along the ribs on one side of the bod y?
SIGNS
Two of these signs: weight loss fever>1month di arr hoea >1month. OR One of the abo vesigns and one or more other si gns or from a risk g roup.
TREAT AND AD VISE
Reinforce the need to kno w HIV status and ad vise on HIV testing and counselling G2-G3. Counsel on the benefits of testing the par tnerG3. Counsel on safer sex including use of condoms G2. Refer to TB centre if cough.
Counsel on stopping smoking For alcohol/dr ug abuse, refer to specialized care provide rs. For counselling on violence, see H4.
CLASSIFY
STRONG LIKELIHOOD OF HIV INFECTIO N
NEXT : If cough or breathing difficulty
IF SIGNS SUGGESTING HIV INFECTION
(HIV status unknown)
C10
IF SMOKING, ALCOHOL OR DR UG ABUSE, ORHI STOR Y OFVIOLENCE
IF TAKING ANTI- TUBERCULOSIS DR UGS
Respond to obser ved signs or volunteered problems (5)
ASK, CHECK RECORD
How long ha veyoubeen coughing? How long ha veyouhad difficulty in breathing? Doyou ha vechest pain? Doyou ha veanyblood in sputum? Doyou smok e?
Ar e you taking anti-tuberculosis drugs? If y es,since w hen? Does the treatment include injection (streptomycin)?
LOOK, LISTEN, FEEL
Look for breathlessness. Li sten for w heezing. Measure temperature.
SIGNS
At least 2 of the follow ing signs: Fever>38C. Breathlessness. Chest pain.
At least 1 of the follow ing signs: Cough or breathing diffic ulty for >3 w eeks Bl ood in sputum Wh eezing
Fever<38C,and Cough <3 w eeks.
Taking anti-tuberculo sis dr ugs. Receiving injectable anti- tuberculosis dr ugs.
TREAT AND AD VISE
Gi vefirst dose of appropriate I M/IVantibiotics B15. Refer urg ently to hospita l B17.
Refer to hospital for assessment. Ifsever e wheezing, refer urg ently to hospital.
Advise safe, soothing remed y. Ifsmoking, counsel to stop smoking.
Ifanti-tubercular treatment includes streptomy (injection), refer the w oman to district hospital for revision of trea tment as streptomycin is ototoxic t the fetus. Iftreatment does not include streptomycin, assure the w oman that the dr ugs are not har mful to her baby,and urg e her to continue treatment for a succes sful outcome of pregna ncy. Ifher sputu misTB positiv e within 2 months of deliv ery , plan to giv e INH proph ylaxis to the ne wborn K13. Reinforce ad vice on HIV testing and counselling G2-G3. Ifsmoking, counsel to stop smoking. Advise to screen immed iate family members and closecontacts for tuberculosis.
CLASSIFY
POSSIBLE PNEUMON IA
POSSIBLE CHR ONIC LUNG DISEASE
UPPER RESPIRAT ORYTRACT INFECTION
TUBERCULOSIS
NEXT : Giveprev entive measures
IF COUGH OR BREA THING DIFFICUL TY
AN
TEN
ATAL CARE
C11
Antenatal care
AN
TEN
ATAL CARE
C12 Give pre ventive measures
AN
TEN
ATAL CARE
C12
GIVE PREVENTIVE MEASURES
Advise and counsel all pre gnant women at ever y antenatal care visit.
ASSESS , CHECK RECORD
Check tetanus toxoid (TT) immunization status.
Check w omans supply of the prescribed dose of iron/folate
Check w hen last dose of mebendazole giv en.
Check w hen last dose of an antimalarial giv en. Ask if she (and children) are sleeping under insecticide treated bednets .
Record all visits and treatments giv en.
TREAT AND AD VISE
Gi vetetanus toxoid if due F2. IfTT1 , plan to giv e TT2 at next visit.
Gi ve3 month s supply of iron and counsel on compliance and safety F3.
Gi vemebendazole once in secon d or third trimester F3.
Gi veintermittent prev entiv e treatment in second and third trimesters F4. Encourage sleeping under insecticide treated bednets.
First visit Devel op a bir th and emerg ency plan C14. Counsel on nutrition C13. Counsel on impor tance of exclus ivebreastfeeding K2. Counsel on stopping sm oking and alcohol and dr ug abuse. Counsel on safer sex i ncluding use of condoms.
All visits Reviewand update t he bir th andemergency plan according to ne w findings C14-C15 . Advise on w hen to seek care: C17 routine visits follow-up visits danger signs.
Third trimester Counsel on family pla nningC16.
Advise and counsel on nutrition and self-care
AN
TEN
ATAL CARE
C13
ADVISE AND COUNSEL ON NUTRITION AND SELF-CARE
Use the infor mation and counselling sheet to suppor t your inter action with the woman, her par tner and family .
Counsel on nutrition
Advise the w oman to eat a g reater amount and v ariety of health y foods, such as meat, fi sh,oils, nuts, seeds, cereals, beans, vegetables, cheese, milk, to help her feel w ell and strong (giv e examples of types of food and ho w much to eat). Spend more time on nutrition counselling with v erythin, adolescent and HIV-positiv e woman. Determine if there are impor tant taboos about foods w hich are nutritiona lly impor tant for g ood health. Advise the w oman ag ainst these taboos. Talk to family members such as the par tner and mother-in-la w,to encourag e them to help ensure the woman eats enough and a voi ds hard ph ysical w ork.
Advise on self-care during pregnancy
Advise the woman to: Takeiron tablets (p.T3). Rest and a voi d lifting hea vy objects. Sleep under an insecticide impregnated bednet. Counsel on safer sex including use of condoms, ifatri sk for STI or H IVG2. Avoid alcohol and smoking during pregnancy . NOT to tak e medication unless prescribed at the health centre/hospital.
C8 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (2)
If fever or burning on urination
C9 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (3)
If vaginal discharge
C10 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (4)
If signs suggesting HIV infection
If smoking, alcohol or drug abuse,
or history of violence
C11 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (5)
If cough or breathing difficulty
If taking anti-tuberculosis drugs
C12 GIVE PREVENTIVE MEASURES
C13 ADVISE AND COUNSEL ON
NUTRITION AND SELF-CARE
Counsel on nutrition
Advise on self-care during pregnancy
Deve lop a bir th and emergency plan (1)
AN
TEN
ATAL CARE
C14
DEVELOP A BIRTH AND EMERGENCY PLAN
Use the infor mation and counselling sheet to suppor t your inter action with the woman, her par tner and family .
Facility deliv ery
Explain wh y bir th in a facility is recommended Any complication can de vel op during deliv ery- the y are not alwa ys predictable. Afacility has staff, equipment, supplies and dr ugs a vai lable to pro vide best care if needed, and a refer ral system. AI f HIV-positiv e she will need appropriate ARVtreatment for herself a nd her bab y during childbir th. Complications are more common in HIV-positiv e women and her ne wborns. Wo men should deliv er in a facility .
Advise how to prepare Revie w the ar rangements for deliv ery: How will she g et there? Wil l she ha veto pa y for transpor t? How much will it cost to deliv er at the facility? Ho w will she pa y? Can she star t saving straight a way? Wh o will g o with her for suppor t during labour and deliv ery? Wh o will help w hile she is a wayto care for her home and other childre n?
Advise when to g o Ifthe woman liv es near the facility , she should g o at the first signs of labour. Ifliving far from the facility , she should g o 2-3 w eeks before bab y due date and sta y either at the maternity waiting home or with family or friends near the facility . Advise to ask for help from the community , if neededI2 .
Advise what to bring Home-based mater nal record. Cl ean cloths for washing , dryi ng and wrapping the bab y. Additional clean cloths to use as sanitar y pads after bir th. Cl othes for mother and bab y. Food and water for w oman and suppor t person.
Home deliv erywith a skilled attendant
Advise how to prepare Revie w the follo wing with her: Wh o will be the co mpanion during labour and deliv ery? Wh o will be close b y for at least 24 hou rs afte r deliv ery? Wh o will help to ca re for her home and other children? Advise to call the skill ed attendant at the first signs of labour . Advise to ha veher home- based mater nal record read y. Advise to ask for help fr om the community , if neededI2 .
Explain supplies needed for home deliver y Wa rmspot for the bir th with a clean surface or a clean cloth. Cl ean cloths of diffe rent sizes: for the bed, for dr ying and wrapping the bab y,for clea ning the bab ys eyes,for the bir th atte ndant to wash and dr y her hands, for use as sanitar y pads. Bl ankets. Bucketsof clean water and some wa y to heat this water . Soap. Bowls: 2 for washing and 1 f or the placenta. Pl astic for wrapping th e placenta.
Advise on labour signs
Advise to g o to the facility or contact the skilled bir th attendant if an y of the follo wing signs: abloody sticky discharg e. painful contractions e ver y 20 minutes or less. waters ha vebroken.
Advise on dang er signs
Advise to g o to the hospital/health centre immediately, day or night, WI THOUT w aiting if an y of the follo wing signs: vaginal bleeding . convulsions. sever e headaches with blur red vision. feverand too w eak to g et out of bed. sever e abdominal pain. fast or difficult breathing .
She should g o to the health centre as soon as possible ifany of the follo wing signs: fever . abdominal pain. feels ill. swelling of fing ers, face, legs.
Discuss ho w to prep are for an emerg ency in pregnan cy
Di scuss emerg ency issue s with the w oman and her par tner/family: where will she g o? how will the y get there? how much it will cost for ser vices and transpor t? can she star t saving straight a way? who will g o with her for suppor t duri ng labour and deliv ery? who will care for her home and other children? Advise the w oman to ask for help from the community , if neededI1I3. Advise her to bring her hom e-based maternal record to the health centre, even for an emer gency visit .
Deve lop a bir th and emergency plan (2)
AN
TEN
ATAL CARE
C15
Advise and counsel on family planning
AN
TEN
ATAL CARE
C16
ADVISE AND COUNSEL ON F AMILY PLANNING
Counsel on the impor tance of family plannin g
Ifappropriate, ask the w oman if she w ould lik e her par tner or another fam ily member to be included in the counselling session. Explain that after bir th,if she has sex and is not exclusiv ely breastfeeding , she can become pregnant as soon as four w eeks after deliv ery . Therefore it is impor tant to star t thinking ear ly on about w hat family planning method the y will use. Ask about plans for ha ving more children. Ifshe (and her par tner) want more children, advise that waiting at least 2-3 y ears betw een pregnancies is healthier for th e mother and chil d. Information on when to star t a method after deliv erywill v arydepending w hether a w oman is breastfeeding or not. Makearr angements for the w oman to see a family planning counsel lor,orcounsel her directly (see the Decision-making tool for family planning pro viders and clients for infor mation on methods and on the counselling process). Counsel on safer sex including use of condoms for dual protection fro m sexually transmit ted infections (STI) or HIV and pregnancy . Promote especially if at risk f or STI or HIV G4. For HIV-positiv e women, see G5 for family planning considerations Her par tner can decide to ha vea vasectomy (male sterilization) at an y time.
Method options for the non-breastfeeding woman Can be used immediately postpar tum Condoms Pr ogestogen-only oral contraceptiv es Pr ogestogen-only injectables Implant Spermicide Female sterilization (w ithin 7 da ys or dela y 6 w eeks) Copper IUD (immediat ely follo wing expulsion of placenta or within 48 hours) Delay3 weeks Combined oral contrac eptives Combined injectables Di aphragm Ferti lity a wareness methods
Special considera tions for
family planning counsel ling during pr egnancy
Counselling should be given during the third trimeste r of pre gnancy. Ifthe woman chooses female sterilization: can be perfor med immediately postpar tum if no sign of infection (ideally within 7 da ys,or dela y for 6 w eeks). pl an for deliv eryin hos pital or health centre w here the y are trained to car ryout the procedure. ensure counsellin g and infor med consent prior to labour and deliv ery . Ifthe woman chooses anintrauterin e device (IUD): can be inser ted imme diately postpar tum if no sign ofinfection (up to 48 hours, ordelay4 weeks) pl an for deliv eryin hos pital or health centre w here the y are trained to inser t the IUD .
Method options for the breastf eeding woman Can be used immediately postpartum Lactational amenor rhoea method (LAM) Condoms Spermicide Female sterilization (within 7 da ys or delay6 weeks) Copper IUD (within 48 hours or dela y 4 w eeks) Delay6 weeks Pr ogestogen-only oral contraceptiv es Pr ogesto gen-only injectables Implants Di aphragm Delay6 months Combined oral contraceptiv es Combined injectables Ferti lity a wareness methods
ADVISE ON R OUTINE AND FOLLO W-UP VISITS
Encourag e the woman to bring her par tner or family member to at least 1 visit.
Antenatal care
AN
TEN
ATAL CARE
C17 Advise on routine and follow-up visits
AN
TEN
ATAL CARE
C17
Routine antenatal care visits
1st visit Before 4 months 12-16 w eeks 2nd visit 6months 24-28 week s 3rd visit 8months 30-32 week s 4th visit 9months 36-38 week s
Al l pregnant w omen should ha ve4 routine antenatal visits. Fi rst antenatal contact should be as ear ly in pregnancy as possible. During the last visit, informthe w oman to retur n if she does not deliv er within 2 w eeks after the expected date of deliv ery . More frequent visits or different schedules ma y be required according to national malaria orHI V policies. Ifwomen are HIV-positiv e ensure a visit betw een 26-28 w eeks.
Follo w-up visits
If the problem w as: Retur n in: Hypertension 1 week if >8 months pre gnant Severe anaemia 2 weeks HIV-positive 2 weeks after HIV testin g
Antenatal care
AN
TEN
ATAL CARE
C18
HOME DELIVER Y WITHOUT A SKILLED A TTENDANT
Reinforce the impor tance of deliver y with a skilled bir th attendant
Instruct mother and family on
clean and safer deliv eryat home
If the w oman has chosen to deliv er at home without a skilled attendant, reviewthese simple instructions with the w oman and family members. Gi vethem a disposable deliv erykit and explain ho w to use it.
Tel l her/them: Toensure a clean deliv erysurface for the bir th. Toensure that the attendant should wash her hands with clean water and soap before/afte r touching mother/bab y.She should also k eep her nails clean. To, after deliv ery , place the bab y on the mother s chest with skin-to-ski n contact and wipe the bab ys eyes using a clean cloth for each e ye. Tocoverthe mother and the bab y. Touse the ties and razor blade from the disposable deliv erykit to tie and cut the cord. The cord is cut whe n it stops pulsating . Todry the bab y after cutting the cord. Towi pe clean but not bathe the baby until after 6 hours. Towait for the placenta to deliv er on its o wn. Tostartbreastfeeding w hen the bab y sho ws signs of readiness, wi thin the first hour after bir th. ToNOT lea vethe mother alone for the first 24 hours. Tokeep the mother and bab y war m.Todress or wrap the bab y,including the bab yshead. Todispose of the placenta in a cor rect, safe and culturally appropriate manner (bur n or bur ry) .
Advise to avoi d har mful practices
For example: NOTtouse local medi cations to hasten labour . NOTtowait for waters t o stop before g oing to health facility . NOTtoinsertanysubstances into the vagina dur ing lab our or after deliv ery . NOTtopush on the abdom en during labour or deliv ery . NOTtopull on the cord t o deli verthe placenta. NOTtoput ashes, cow dung or other su bstance on umbilical cord/stump.
Encourage helpful traditional practices:
____________________________________________________________________
____________________________________________________________________
Advise on dang er signs
If the mother or bab y has an y of the se signs, she/the y must g o to the health centre immediately, day or night, WI THOUT w aiting
Mother Wa ters break and not i n labou r after 6 hours. Labour pains/contr actions continue for more than 12 hours. Heavybl eeding after deliv ery(pad/cloth soak ed in less than 5 minutes). Bl eeding increases. Pl acenta not expelled 1 hour afte r bir th of the bab y.
Baby Verysmall. Di fficulty in breathing . Fi ts. Fever . Feels cold. Bl eeding. Not able to feed.
Assesses eligibility of ARV for HIV-positive pregnant woman
AN
TEN
ATAL CARE
C19
ASK, CHECK RECORD
Haveyoulost weight? Haveyougot diar rhoea (continuous or inter mittent)? Do y ou ha vefever? Howlong (>1 month)? Hav e you had cough? Howlong (> 1 month)? Hav e you an y difficulty in breathing? Howlong (> 1 month)? Have younoticed an y chang e in vaginal discharg e?
LOOK, LISTEN, FEEL
Look for ulcers and w hite patches in the mouth (thr ush). Look at the skin: Isthere a rash? Are there blisters along the ribs on one side of the bod y? Look for visible wasting . Feel the head, neck,and underar m for enlarg ed lymph nodes. Look for an y abnor mal v aginal discharge C9.
SIGNS
HIV-positive and an y of the follo wing: We ight loss or no w eight g ain Vi sible wasting Di arr hoea > 1 month Fever> 1month Cough > 1 month or difficult breathing Cr acks/ulcers around lips/mouth Itching rash Bl isters along the ribs on one side of the bod y Enlarged lymph nodes Abnormal vaginal discharg e
HIV-positive and none of the abo ve signs
TREAT AND AD VISE
Refer to hospital for fur ther assessme nt.
Gi veappropriate AR Vs G9. Support initiation of ARVG6. Revise ANC visit accordingly .
CLASSIFY
HIV-POSITI VE WITH HIV-RELATED SIGNS AND SYMPT OMS
HIV-POSITI VE WITHOU T HIV-RELATED SIGNS AND SYMPT OMS
ASSESS ELIGIBILITY OF ARVFOR HIV-POSITIVE PRE GNANT W OMAN
Use this char t to assess HIV-related signs and symptoms and to deter mine AR V needs for HIV-positive woman and her bab y when appropriate HIV ser vices and CD4 count
are not a vai lable.
C14 DEVELOP A BIRTH AND
EMERGENCY PLAN
Facility delivery
Home delivery with a skilled attendant
C15 Advise on labour signs
Advise on danger signs
Discuss how to prepare for an emergency in
pregnancy
C16 ADVISE AND COUNSEL ON
FAMILY PLANNING
Counsel on the importance of family planning
Special considerations for family planning
counselling during pregnancy
C17 ADVISE ON ROUTINE AND
FOLLOW-UP VISITS
C18 HOME DELIVERY WITHOUT A
SKILLED ATTENDANT
Instruct mother and family on clean and safer
delivery at home
Advise to avoid harmful practices
Advise on danger signs
C19 ASSESS ELIGIBILITY OF ARV FOR
HIV-POSITIVE WOMAN
Assess the pregnant woman Pregnancy status, birth and emergency plan
A
N
T
E
N
A
T
A
L
C
A
R
E
ASK, CHECK RECORD
ALL VISITS
Check duration of pregnancy.
Where do you plan to deliver?
Any vaginal bleeding since last visit?
Is the baby moving? (after 4 months)
Check record for previous complications and
treatments received during this pregnancy.
Do you have any concerns?
FIRST VISIT
How many months pregnant are you?
When was your last period?
When do you expect to deliver?
How old are you?
Have you had a baby before? If yes:
Check record for prior pregnancies or if
there is no record ask about:
Number of prior pregnancies/deliveries
Prior caesarean section, forceps, or vacuum
Prior third degree tear
Heavy bleeding during or after delivery
Convulsions
Stillbirth or death in first day.
Do you smoke, drink alcohol or
use any drugs?
HIV status and ARV treatment
THIRD TRIMESTER
Has she been counselled on family
planning? If yes, does she want
tubal ligation or IUD A15 .
LOOK, LISTEN, FEEL
Feel for trimester of pregnancy.
Look for caesarean scar
Feel for obvious multiple
pregnancy.
Feel for transverse lie.
Listen to fetal heart.
INDICATIONS
Prior delivery by caesarean.
Age less than 14 years.
Transverse lie or other obvious
malpresentation within one month
of expected delivery.
Obvious multiple pregnancy.
Tubal ligation or IUD desired
immediately after delivery.
Documented third degree tear.
History of or current vaginal
bleeding or other complication
during this pregnancy.
First birth.
Last baby born dead or died in first
day.
Age less than 16 years.
More than six previous births.
Prior delivery with heavy bleeding.
Prior delivery with convulsions.
Prior delivery by forceps or vacuum.
HIV-positive woman.
None of the above.
ADVISE
Explain why delivery needs to be at referral level C14 .
Develop the birth and emergency plan C14 .
Explain why delivery needs to be at primary health
care level C14 .
Develop the birth and emergency plan C14 .
Explain why delivery needs to be with a skilled birth
attendant, preferably at a facility.
Develop the birth and emergency plan C14 .
PLACE OF DELIVERY
REFERRAL LEVEL
PRIMARY
HEALTH CARE LEVEL
ACCORDING TO
WOMANS PREFERENCE
NEXT: Check for pre-eclampsia
ASSESS THE PREGNANT WOMAN: PREGNANCY STATUS, BIRTH AND EMERGENCY PLAN
Use this chart to assess the pregnant woman at each of the four antenatal care visits. During first antenatal visit, prepare a birth and emergency plan using this chart
and review them during following visits. Modify the birth plan if any complications arise.
C2
Assess the pregnant woman Check for pre-eclampsia
ASK, CHECK RECORD
Blood pressure at the last visit?
LOOK, LISTEN, FEEL
Measure blood pressure in sitting
position.
If diastolic blood pressure is 90
mmHg, repeat after 1 hour rest.
If diastolic blood pressure is still 90
mmHg, ask the woman if she has:
severe headache
blurred vision
epigastric pain and
check protein in urine.
SIGNS
Diastolic blood pressure
110 mmHg and 3+ proteinuria, or
Diastolic blood pressure 90-mmHg
on two readings and 2+ proteinuria,
and any of:
severe headache
blurred vision
epigastric pain.
Diastolic blood pressure
90-110-mmHg on two readings and
2+ proteinuria.
Diastolic blood pressure
90 mmHg on 2 readings.
None of the above.
TREAT AND ADVISE
Give magnesium sulphate B13 .
Give appropriate anti-hypertensives B14 .
Revise the birth plan C2 .
Refer urgently to hospital B17 .
Revise the birth plan C2 .
Refer to hospital.
Advise to reduce workload and to rest.
Advise on danger signs C15 .
Reassess at the next antenatal visit or in 1 week if
>8 months pregnant.
If hypertension persists after 1 week or at next visit,
refer to hospital or discuss case with the doctor or
midwife, if available.
No treatment required.
CLASSIFY
SEVERE
PRE-ECLAMPSIA
PRE-ECLAMPSIA
HYPERTENSION
NO HYPERTENSION
NEXT: Check for anaemia
CHECK FOR PRE-ECLAMPSIA
Screen all pregnant women at every visit.
A
N
T
E
N
A
T
A
L
C
A
R
E
C3
Assess the pregnant woman Check for anaemia
A
N
T
E
N
A
T
A
L
C
A
R
E
ASK, CHECK RECORD
Do you tire easily?
Are you breathless (short of breath)
during routine household work?
LOOK, LISTEN, FEEL
On first visit:
Measure haemoglobin
On subsequent visits:
Look for conjunctival pallor.
Look for palmar pallor. If pallor:
Is it severe pallor?
Some pallor?
Count number of breaths in 1
minute.
SIGNS
Haemoglobin <7-g/dl.
AND/OR
Severe palmar and conjunctival
pallor or
Any pallor with any of
>30 breaths per minute
tires easily
breathlessness at rest
Haemoglobin 7-11-g/dl.
OR
Palmar or conjunctival pallor.
Haemoglobin >11-g/dl.
No pallor.
TREAT AND ADVISE
Revise birth plan so as to deliver in a facility with
blood transfusion services C2 .
Give double dose of iron (1 tablet twice daily)
for 3 months F3 .
Counsel on compliance with treatment F3 .
Give appropriate oral antimalarial F4 .
Follow up in 2 weeks to check clinical progress, test
results, and compliance with treatment.
Refer urgently to hospital B17 .
Give double dose of iron (1 tablet twice daily)
for 3 months F3 .
Counsel on compliance with treatment F3 .
Give appropriate oral antimalarial if not given in the
past month F4 .
Reassess at next antenatal visit (4-6 weeks). If
anaemia persists, refer to hospital.
Give iron 1 tablet once daily for 3 months F3 .
Counsel on compliance with treatment F4 .
CLASSIFY
SEVERE
ANAEMIA
MODERATE ANAEMIA
NO CLINICAL
ANAEMIA
NEXT: Check for syphilis
CHECK FOR ANAEMIA
Screen all pregnant women at every visit.
C4
Assess the pregnant woman Check for syphilis
ASK, CHECK RECORD
Have you been tested for syphilis
during this pregnancy?
If not, perform the rapid plasma
reagin (RPR) test L5 .
If test was positive, have you and
your partner been treated for
syphilis?
If not, and test is positive, ask
Are you allergic to penicillin?
LOOK, LISTEN, FEEL TEST RESULT
RPR test positive.
RPR test negative.
TREAT AND ADVISE
Give benzathine benzylpenicillin IM. If allergy, give
erythromycin F6 .
Plan to treat the newborn K12 .
Encourage woman to bring her sexual partner for
treatment.
Counsel on safer sex including use of condoms to
prevent new infection G2 .
Counsel on safer sex including use of condoms to
prevent infection G2 .
CLASSIFY
POSSIBLE SYPHILIS
NO SYPHILIS
NEXT: Check for HIV status
CHECK FOR SYPHILIS
Test all pregnant women at first visit. Check status at every visit.
A
N
T
E
N
A
T
A
L
C
A
R
E
C5
Assess the pregnant woman Check for HIV status
A
N
T
E
N
A
T
A
L
C
A
R
E
ASK, CHECK RECORD
Provide key information on HIV G2 .
What is HIV and how is HIV transmit-
ted G2 ?
Advantage of knowing the HIV status
in pregnancy G2 .
Explain about HIV testing and
counselling including confidentiality
of the result G3 .
Ask the woman:
Have you been tested for HIV?
If not: tell her that she will be
tested for HIV, unless she refuses.
If yes: Check result. (Explain to
her that she has a right not to
disclose the result.)
Are you taking any ARV?
Check ARV treatment plan.
Has the partner been tested?
LOOK, LISTEN, FEEL
Perform the Rapid HIV test if not
performed in this pregnancy L6 .
SIGNS
Positive HIV test.
Negative HIV test.
She refuses the test or is not willing
to disclose the result of previous
test or no test results available.
TREAT AND ADVISE
Counsel on implications of a positive test G3 .
If HIV services available:
Refer the woman to HIV services for further asses-
sment.
Ask her to return in 2 weeks with her documents.
If HIV services are not available:
Determine the severity of the disease and assess
eligibility for ARVs C19 .
Give her appropriate ARV G6 , G9 .
For all women:
Support adherence to ARV G6 .
Counsel on infant feeding options G7 .
Provide additional care for HIV-positive woman G4 .
Counsel on family planning G4 .
Counsel on safer sex including use of condoms G2 .
Counsel on benefits of disclosure (involving) and
testing her partner G3 .
Provide support to the HIV-positive woman G5 .
Counsel on implications of a negative test G3 .
Counsel on the importance of staying negative by
practising safer sex, including use of condoms G2 .
Counsel on benefits of involving and testing the
partner G3 .
Counsel on safer sex including use of condoms G2 .
Counsel on benefits of involving and testing the
partner G3 .
CLASSIFY
HIV-POSITIVE
HIV-NEGATIVE
UNKNOWN HIV STATUS
NEXT: Respond to observed signs or volunteered problems
If no problem, go to page C12 .
CHECK FOR HIV STATUS
Test and counsel all pregnant women for HIV at the first antenatal visit. Check status at every visit.
Inform the women that HIV test will be done routinely and that she may refuse the HIV test.
C6
IF RUPTURED MEMBRANES AND NO LABOUR
Respond to observed signs or volunteered problems (1)
ASK, CHECK RECORD
When did the baby last move?
If no movement felt, ask woman
to move around for some time,
reassess fetal movement.
When did the membranes rupture?
When is your baby due?
LOOK, LISTEN, FEEL
Feel for fetal movements.
Listen for fetal heart after 6 months
of pregnancy D2 .
If no heart beat, repeat after 1 hour.
Look at pad or underwear for
evidence of:
amniotic fluid
foul-smelling vaginal discharge
If no evidence, ask her to wear a
pad. Check again in 1 hour.
Measure temperature.
SIGNS
No fetal movement.
No fetal heart beat.
No fetal movement but fetal heart
beat present.
Fever 38C.
Foul-smelling vaginal discharge.
Rupture of membranes at <=8
months of pregnancy.
Rupture of membranes at >8
months of pregnancy.
TREAT AND ADVISE
Inform the woman and partner about the possibility
of dead baby.
Refer to hospital.
Inform the woman that baby is fine and likely to be
well but to return if problem persists.
Give appropriate IM/IV antibiotics B15 .
Refer urgently to hospital B17 .
Give appropriate IM/IV antibiotic B15 .
Refer urgently to hospital B17 .
Manage as Woman in childbirth D1-D28.
CLASSIFY
PROBABLY DEAD BABY
WELL BABY
UTERINE AND FETAL
INFECTION
RISK OF UTERINE
AND FETAL INFECTION
RUPTURE OF
MEMBRANES
NEXT: If fever or burning on urination
RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
A
N
T
E
N
A
T
A
L
C
A
R
E
C7
IF NO FETAL MOVEMENT
Respond to observed signs or volunteered problems (2)
A
N
T
E
N
A
T
A
L
C
A
R
E
ASK, CHECK RECORD
Have you had fever?
Do you have burning on urination?
LOOK, LISTEN, FEEL
If history of fever or feels hot:
Measure axillary
temperature.
Look or feel for stiff neck.
Look for lethargy.
Percuss flanks for
tenderness.
SIGNS
Fever >38C and any of:
very fast breathing or
stiff neck
lethargy
very weak/not able to stand.
Fever >38C and any of:
Flank pain
Burning on urination.
Fever >38C or history of fever
(in last 48 hours).
Burning on urination.
TREAT AND ADVISE
Insert IV line and give fluids slowly B9 .
Give appropriate IM/IV antibiotics B15 .
Give artemether/quinine IM B16 .
Give glucose B16 .
Refer urgently to hospital B17 .
Give appropriate IM/IV antibiotics B15 .
Give appropriate oral antimalarial F4 .
Refer urgently to hospital B17 .
Give appropriate oral antimalarial F4 .
If no improvement in 2 days or condition is worse,
refer to hospital.
Give appropriate oral antibiotics F5 .
Encourage her to drink more fluids.
If no improvement in 2 days or condition is worse,
refer to hospital.
CLASSIFY
VERY SEVERE FEBRILE
DISEASE
UPPER URINARY TRACT
INFECTION
MALARIA
LOWER URINARY TRACT
INFECTION
NEXT: If vaginal discharge
IF FEVER OR BURNING ON URINATION
C8
Respond to observed signs or volunteered problems (3)
ASK, CHECK RECORD
Have you noticed changes in your
vaginal discharge?
Do you have itching at the vulva?
Has your partner had a urinary
problem?
If partner is present in the clinic, ask
the woman if she feels comfortable if
you ask him similar questions.
If yes, ask him if he has:
urethral discharge or pus.
burning on passing urine.
If partner could not be approached,
explain importance of partner
assessment and treatment to avoid
reinfection.
Schedule follow-up appointment for
woman and partner (if possible).
LOOK, LISTEN, FEEL
Separate the labia and look for
abnormal vaginal discharge:
amount
colour
odour/smell.
If no discharge is seen, examine
with a gloved finger and look at the
discharge on the glove.
SIGNS
Abnormal vaginal discharge.
Partner has urethral discharge or
burning on passing urine.
Curd like vaginal discharge.
Intense vulval itching.
Abnormal vaginal discharge
TREAT AND ADVISE
Give appropriate oral antibiotics to woman F5 .
Treat partner with appropriate oral antibiotics F5 .
Counsel on safer sex including use of condoms G2 .
Give clotrimazole F5 .
Counsel on safer sex including use of condoms G2 .
Give metronidazole to woman F5 .
Counsel on safer sex including use of condoms G2 .
CLASSIFY
POSSIBLE
GONORRHOEA OR
CHLAMYDIA
INFECTION
POSSIBLE
CANDIDA INFECTION
POSSIBLE
BACTERIAL OR
TRICHOMONAS
INFECTION
NEXT: If signs suggesting HIV infection
IF VAGINAL DISCHARGE
A
N
T
E
N
A
T
A
L
C
A
R
E
C9
Respond to observed signs or volunteered problems (4)
A
N
T
E
N
A
T
A
L
C
A
R
E
ASK, CHECK RECORD
Have you lost weight?
Do you have fever?
How long (>1 month)?
Have you got diarrhoea (continuous
or intermittent)?
How long, >1 month?
Have you had cough?
How long, >1 month?
Assess if in high risk group:
Occupational exposure?
Multiple sexual partner?
Intravenous drug use?
History of blood transfusion?
Illness or death from AIDS in a
sexual partner?
History of forced sex?
LOOK, LISTEN, FEEL
Look for visible wasting.
Look for ulcers and white patches in
the mouth (thrush).
Look at the skin:
Is there a rash?
Are there blisters along the ribs
on one side of the body?
SIGNS
Two of these signs:
weight loss
fever >1 month
diarrhoea >1month.
OR
One of the above signs and
one or more other signs or
from a risk group.
TREAT AND ADVISE
Reinforce the need to know HIV status and advise on
HIV testing and counselling G2-G3 .
Counsel on the benefits of testing the partner G3 .
Counsel on safer sex including use of condoms G2 .
Refer to TB centre if cough.
Counsel on stopping smoking
For alcohol/drug abuse, refer to specialized care
providers.
For counselling on violence, see H4 .
CLASSIFY
STRONG LIKELIHOOD OF
HIV INFECTION
NEXT: If cough or breathing difficulty
IF SIGNS SUGGESTING HIV INFECTION
(HIV status unknown)
C10
IF SMOKING, ALCOHOL OR DRUG ABUSE, OR HISTORY OF VIOLENCE
IF TAKING ANTI-TUBERCULOSIS DRUGS
Respond to observed signs or volunteered problems (5)
ASK, CHECK RECORD
How long have you been coughing?
How long have you had difficulty in
breathing?
Do you have chest pain?
Do you have any blood in sputum?
Do you smoke?
Are you taking anti-tuberculosis
drugs? If yes, since when?
Does the treatment include injection
(streptomycin)?
LOOK, LISTEN, FEEL
Look for breathlessness.
Listen for wheezing.
Measure temperature.
SIGNS
At least 2 of the following signs:
Fever >38C.
Breathlessness.
Chest pain.
At least 1 of the following signs:
Cough or breathing difficulty
for >3 weeks
Blood in sputum
Wheezing
Fever <38C, and
Cough <3 weeks.
Taking anti-tuberculosis drugs.
Receiving injectable anti-
tuberculosis drugs.
TREAT AND ADVISE
Give first dose of appropriate IM/IV antibiotics B15 .
Refer urgently to hospital B17 .
Refer to hospital for assessment.
If severe wheezing, refer urgently to hospital.
Advise safe, soothing remedy.
If smoking, counsel to stop smoking.
If anti-tubercular treatment includes streptomycin
(injection), refer the woman to district hospital for
revision of treatment as streptomycin is ototoxic to
the fetus.
If treatment does not include streptomycin, assure
the woman that the drugs are not harmful to her
baby, and urge her to continue treatment for a
successful outcome of pregnancy.
If her sputum is TB positive within 2 months of delivery,
plan to give INH prophylaxis to the newborn K13 .
Reinforce advice on HIV testing and counselling
G2-G3 .
If smoking, counsel to stop smoking.
Advise to screen immediate family members and
close contacts for tuberculosis.
CLASSIFY
POSSIBLE PNEUMONIA
POSSIBLE CHRONIC
LUNG DISEASE
UPPER
RESPIRATORY TRACT
INFECTION
TUBERCULOSIS
NEXT: Give preventive measures
IF COUGH OR BREATHING DIFFICULTY
A
N
T
E
N
A
T
A
L
C
A
R
E
C11
Antenatal care
A
N
T
E
N
A
T
A
L
C
A
R
E
C12
Give preventive measures
A
N
T
E
N
A
T
A
L
C
A
R
E
C12
GIVE PREVENTIVE MEASURES
Advise and counsel all pregnant women at every antenatal care visit.
ASSESS, CHECK RECORD
Check tetanus toxoid (TT) immunization status.
Check womans supply of the prescribed dose of iron/folate
Check when last dose of mebendazole given.
Check when last dose of an antimalarial given.
Ask if she (and children) are sleeping under insecticide treated bednets.
Record all visits and treatments given.
TREAT AND ADVISE
Give tetanus toxoid if due F2 .
If TT1, plan to give TT2 at next visit.
Give 3 months supply of iron and counsel on compliance and safety F3 .
Give mebendazole once in second or third trimester F3 .
Give intermittent preventive treatment in second and third trimesters F4 .
Encourage sleeping under insecticide treated bednets.
First visit
Develop a birth and emergency plan C14 .
Counsel on nutrition C13 .
Counsel on importance of exclusive breastfeeding K2 .
Counsel on stopping smoking and alcohol and drug abuse.
Counsel on safer sex including use of condoms.
All visits
Review and update the birth and emergency plan according to new findings C14-C15.
Advise on when to seek care: C17
routine visits
follow-up visits
danger signs.
Third trimester
Counsel on family planning C16 .
NEXT: Go to
C2
and review the birth and emergency plan.
Advise and counsel on nutrition and self-care
A
N
T
E
N
A
T
A
L
C
A
R
E
C13
ADVISE AND COUNSEL ON NUTRITION AND SELF-CARE
Use the information and counselling sheet to support your interaction with the woman, her partner and family.
Counsel on nutrition
Advise the woman to eat a greater amount and variety of healthy foods, such as meat, fish, oils, nuts,
seeds, cereals, beans, vegetables, cheese, milk, to help her feel well and strong (give examples of
types of food and how much to eat).
Spend more time on nutrition counselling with very thin, adolescent and HIV-positive woman.
Determine if there are important taboos about foods which are nutritionally important for good
health. Advise the woman against these taboos.
Talk to family members such as the partner and mother-in-law, to encourage them to help ensure the
woman eats enough and avoids hard physical work.
Advise on self-care during pregnancy
Advise the woman to:
Take iron tablets (p.T3).
Rest and avoid lifting heavy objects.
Sleep under an insecticide impregnated bednet.
Counsel on safer sex including use of condoms, if at risk for STI or HIV G2 .
Avoid alcohol and smoking during pregnancy.
NOT to take medication unless prescribed at the health centre/hospital.
Develop a birth and emergency plan (1)
A
N
T
E
N
A
T
A
L
C
A
R
E
C14
DEVELOP A BIRTH AND EMERGENCY PLAN
Use the information and counselling sheet to support your interaction with the woman, her partner and family.
Facility delivery
Explain why birth in a facility is recommended
Any complication can develop during delivery - they are not always predictable.
A facility has staff, equipment, supplies and drugs available to provide best care if needed, and a
referral system.
If HIV-positive she will need appropriate ARV treatment for herself and her baby during childbirth.
Complications are more common in HIV-positive women and her newborns. HIV-positive women
should deliver in a facility.
Advise how to prepare
Review the arrangements for delivery:
How will she get there? Will she have to pay for transport?
How much will it cost to deliver at the facility? How will she pay?
Can she start saving straight away?
Who will go with her for support during labour and delivery?
Who will help while she is away to care for her home and other children?
Advise when to go
If the woman lives near the facility, she should go at the first signs of labour.
If living far from the facility, she should go 2-3 weeks before baby due date and stay either at the
maternity waiting home or with family or friends near the facility.
Advise to ask for help from the community, if needed I2 .
Advise what to bring
Home-based maternal record.
Clean cloths for washing, drying and wrapping the baby.
Additional clean cloths to use as sanitary pads after birth.
Clothes for mother and baby.
Food and water for woman and support person.
Home delivery with a skilled attendant
Advise how to prepare
Review the following with her:
Who will be the companion during labour and delivery?
Who will be close by for at least 24 hours after delivery?
Who will help to care for her home and other children?
Advise to call the skilled attendant at the first signs of labour.
Advise to have her home-based maternal record ready.
Advise to ask for help from the community, if needed I2 .
Explain supplies needed for home delivery
Warm spot for the birth with a clean surface or a clean cloth.
Clean cloths of different sizes: for the bed, for drying and wrapping the baby, for cleaning the babys
eyes, for the birth attendant to wash and dry her hands, for use as sanitary pads.
Blankets.
Buckets of clean water and some way to heat this water.
Soap.
Bowls: 2 for washing and 1 for the placenta.
Plastic for wrapping the placenta.
Advise on labour signs
Advise to go to the facility or contact the skilled birth attendant if any of the following signs:
a bloody sticky discharge.
painful contractions every 20 minutes or less.
waters have broken.
Advise on danger signs
Advise to go to the hospital/health centre immediately, day or night, WITHOUT waiting
if any of the following signs:
vaginal bleeding.
convulsions.
severe headaches with blurred vision.
fever and too weak to get out of bed.
severe abdominal pain.
fast or difficult breathing.
She should go to the health centre as soon as possible if any of the following signs:
fever.
abdominal pain.
feels ill.
swelling of fingers, face, legs.
Discuss how to prepare for an emergency in pregnancy
Discuss emergency issues with the woman and her partner/family:
where will she go?
how will they get there?
how much it will cost for services and transport?
can she start saving straight away?
who will go with her for support during labour and delivery?
who will care for her home and other children?
Advise the woman to ask for help from the community, if needed I1I3 .
Advise her to bring her home-based maternal record to the health centre, even for an emergency visit.
Develop a birth and emergency plan (2)
A
N
T
E
N
A
T
A
L
C
A
R
E
C15
Advise and counsel on family planning
A
N
T
E
N
A
T
A
L
C
A
R
E
C16
ADVISE AND COUNSEL ON FAMILY PLANNING
Counsel on the importance of family planning
If appropriate, ask the woman if she would like her partner or another family member to be included
in the counselling session.
Explain that after birth, if she has sex and is not exclusively breastfeeding, she can become pregnant
as soon as four weeks after delivery. Therefore it is important to start thinking early on about what
family planning method they will use.
Ask about plans for having more children. If she (and her partner) want more children, advise that
waiting at least 2 years before trying to become pregnant again is good for the mother and for the
baby's health.
Information on when to start a method after delivery will vary depending whether a woman is
breastfeeding or not.
Make arrangements for the woman to see a family planning counsellor, or counsel her directly
(see the Decision-making tool for family planning providers and clients for information on
methods and on the counselling process).
Counsel on safer sex including use of condoms for dual protection from sexually transmitted
infections (STI) or HIV and pregnancy. Promote especially if at risk for STI or HIV G4 .
For HIV-positive women, see G4 for family planning considerations
Her partner can decide to have a vasectomy (male sterilization) at any time.
Method options for the non-breastfeeding woman
Can be used immediately postpartum Condoms
Progestogen-only oral contraceptives
Progestogen-only injectables
Implant
Spermicide
Female sterilization (within 7 days or delay 6 weeks)
Copper IUD (immediately following expulsion of
placenta or within 48 hours)
Delay 3 weeks Combined oral contraceptives
Combined injectables
Diaphragm
Fertility awareness methods
Special considerations for
family planning counselling during pregnancy
Counselling should be given during the third trimester of pregnancy.
If the woman chooses female sterilization:
can be performed immediately postpartum if no sign of infection
(ideally within 7 days, or delay for 6 weeks).
plan for delivery in hospital or health centre where they are trained to carry out the procedure.
ensure counselling and informed consent prior to labour and delivery.
If the woman chooses an intrauterine device (IUD):
can be inserted immediately postpartum if no sign of infection (up to 48 hours, or delay 4 weeks)
plan for delivery in hospital or health centre where they are trained to insert the IUD.
Method options for the breastfeeding woman
Can be used immediately postpartum Lactational amenorrhoea method (LAM)
Condoms
Spermicide
Female sterilization (within 7 days or
delay 6 weeks)
Copper IUD (within 48 hours or delay 4 weeks)
Delay 6 weeks Progestogen-only oral contraceptives
Progestogen-only injectables
Implants
Diaphragm
Delay 6 months Combined oral contraceptives
Combined injectables
Fertility awareness methods
ADVISE ON ROUTINE AND FOLLOW-UP VISITS
Encourage the woman to bring her partner or family member to at least 1 visit.
Antenatal care
A
N
T
E
N
A
T
A
L
C
A
R
E
C17
Advise on routine and follow-up visits
A
N
T
E
N
A
T
A
L
C
A
R
E
C17
Routine antenatal care visits
1st visit Before 4 months Before 16 weeks
2nd visit 6 months 24-28 weeks
3rd visit 8 months 30-32 weeks
4th visit 9 months 36-38 weeks
All pregnant women should have 4 routine antenatal visits.
First antenatal contact should be as early in pregnancy as possible.
During the last visit, inform the woman to return if she does not deliver within 2 weeks after the
expected date of delivery.
More frequent visits or different schedules may be required according to national malaria or HIV
policies.
If women is HIV-positive ensure a visit between 26-28 weeks.
Follow-up visits
If the problem was: Return in:
Hypertension 1 week if >8 months pregnant
Severe anaemia 2 weeks
HIV-positive 2 weeks after HIV testing
Antenatal care
A
N
T
E
N
A
T
A
L
C
A
R
E
C18
HOME DELIVERY WITHOUT A SKILLED ATTENDANT
Reinforce the importance of delivery with a skilled birth attendant
Instruct mother and family on
clean and safer delivery at home
If the woman has chosen to deliver at home without a skilled attendant, review these simple
instructions with the woman and family members.
Give them a disposable delivery kit and explain how to use it.
Tell her/them:
To ensure a clean delivery surface for the birth.
To ensure that the attendant should wash her hands with clean water and soap before/after
touching mother/baby. She should also keep her nails clean.
To, after birth, dry and place the baby on the mothers chest with skin-to-skin contact and wipe the
babys eyes using a clean cloth for each eye.
To cover the mother and the baby.
To use the ties and razor blade from the disposable delivery kit to tie and cut the cord. The cord is cut
when it stops pulsating.
To wipe baby clean but not bathe the baby until after 6 hours.
To wait for the placenta to deliver on its own.
To start breastfeeding when the baby shows signs of readiness, within the first hour after birth.
To NOT leave the mother alone for the first 24 hours.
To keep the mother and baby warm. To dress or wrap the baby, including the babys head.
To dispose of the placenta in a correct, safe and culturally appropriate manner (burn or burry).
Advise to avoid harmful practices
For example:
NOT to use local medications to hasten labour.
NOT to wait for waters to stop before going to health facility.
NOT to insert any substances into the vagina during labour or after delivery.
NOT to push on the abdomen during labour or delivery.
NOT to pull on the cord to deliver the placenta.
NOT to put ashes, cow dung or other substance on umbilical cord/stump.
Encourage helpful traditional practices:
____________________________________________________________________
____________________________________________________________________
Advise on danger signs
If the mother or baby has any of these signs, she/they must go to the health centre
immediately, day or night, WITHOUT waiting
Mother
Waters break and not in labour after 6 hours.
Labour pains/contractions continue for more than 12 hours.
Heavy bleeding after delivery (pad/cloth soaked in less than 5 minutes).
Bleeding increases.
Placenta not expelled 1 hour after birth of the baby.
Baby
Very small.
Difficulty in breathing.
Fits.
Fever.
Feels cold.
Bleeding.
Not able to feed.
Advise her/them on danger signs for the mother and the baby and where to go.
Assesses eligibility of ARV for HIV-positive pregnant woman
A
N
T
E
N
A
T
A
L
C
A
R
E
C19
ASK, CHECK RECORD
Have you lost weight?
Have you got diarrhoea
(continuous or intermittent)?
Do you have fever?
How long (>1 month)?
Have you had cough?
How long (> 1 month)?
Have you any difficulty in breathing?
How long (> 1 month)?
Have you noticed any change in
vaginal discharge?
LOOK, LISTEN, FEEL
Look for ulcers and white patches in
the mouth (thrush).
Look at the skin:
Is there a rash?
Are there blisters along the ribs
on one side of the body?
Look for visible wasting.
Feel the head, neck, and underarm
for enlarged lymph nodes.
Look for any abnormal vaginal
discharge C9 .
SIGNS
HIV-positive and any of the following:
Weight loss or no weight gain
Visible wasting
Diarrhoea > 1 month
Fever > 1 month
Cough > 1 month or difficult
breathing
Cracks/ulcers around lips/mouth
Itching rash
Blisters along the ribs on one side
of the body
Enlarged lymph nodes
Abnormal vaginal discharge
HIV-positive and none of the above
signs
TREAT AND ADVISE
Refer to hospital for further assessment.
Give appropriate ARVs G9 .
Support initiation of ARV G6 .
Revise ANC visit accordingly C17 .
CLASSIFY
HIV-POSITIVE WITH
HIV-RELATED SIGNS
AND SYMPTOMS
HIV-POSITIVE WITHOUT
HIV-RELATED SIGNS
AND SYMPTOMS
ASSESS ELIGIBILITY OF ARV FOR HIV-POSITIVE PREGNANT WOMAN
Use this chart to determine ARV needs for HIV-positive woman and her baby when appropriate HIV services and CD4 count are not available.
Childbirth: labour, delivery and immediate postpartum care
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
CHILDBIRTH: LABOUR, DELIVERY AND IMMEDIATE POSTPARTUM CARE
Examine the woman in labour or with r uptured membranes
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
ASK, CHECK RECORD
History of this labour : Wh en did contractions begin? How frequent are contractions? Howstrong? Haveyour waters brok en? If y es, whe n? Were the y clear or g reen? Haveyouhad any bleeding? If y es,whe n? Ho w much? Isthe bab y mo ving? Doyou ha veanyconcern? Check record, orifnorecord: Ask when the deliv eryis expected. Determine if preter m (less than 8 months pregnant). Reviewthe bir th plan. If prior pre gnancies: Number of prior pregnancies/ deliveries. Any prior caesarean section, forceps, or v acuum, or other complication such as postpar tum haemorhage? Any prior third deg ree tear? Curr ent pre gnancy: RPR statusC5. HbresultsC4. Tetanus immunization status F2. HI V status C6. Infant feeding plan G7-G8.
LOOK , LI STEN, FEEL
Observ e the w omans response to contractions: Isshe coping w ell or is she distressed? Isshe pushing or g runting? Check abdomen for : caesarean section scar . horizontal ridg e across lo wer abdomen (if present, empty bladder B12and obser veagain). Feel abdomen for : contractions frequency , duration, anycontinuous contractions? fetal lielongitudinal or transverse? fetal presentationhead, breech, other? more than one fetus? fetal mo vement. Li sten to the fetal hear t beat: Count number of beats in1 minute. Ifless than 100 beats pe r minute, or more than 180 , turn woman on her left side and count again. Measure blood pressure. Measure temperature. Look for pallor . Look for sunk en eyes, drymouth. Pi nch the skin of the forea rm:does it go back quickly?
NEXT : Per formvaginal examination and decide stag e of labour
EXAMINE THE W OMAN IN LAB OUR OR WITH R UPTURED MEMBRANES
First do Rapid assessment and manag ementB3-B7. Then use this char t to assess the woman s and fetal status and decide stag e of labour .
D2
Decide stage of labour
ASK, CHECK RECORD
Explain to the w oman that youwi ll giv e her a v aginal examination and ask for her consent.
LOOK, LISTEN, FEEL
Look at vulv a for : bulging perineum any visible fetal par ts vaginal bleeding leaking amniotic fluid; if yes, is it meconium stained, foul-smelling? warts, keloid tissue or scars that ma y interfere with deliv ery .
Performvaginal examination DO NO Tshavethe perineal area. Pr epare: cl ean glo ves swabs,pads. Wa sh hands with soap before and after each examination. Wa sh vulv a and perineal areas. Put on glo ves. Position the w oman with legs flex ed and apar t.
DO NO Tperfor m vaginal examination i f bleeding nowor at an y time after 7 months of pr egnancy.
Perfor m gentle v aginal examination ( do not star t during a contraction): Determine cervical dilatation in centimetres. Feel for presenting par t.Is it hard, round and smooth (the head)? If not, identify the presenting par t. Feel for membranes are theyintact? Feel for cord is it felt? I s it pulsating? I f so,act immediately as on D15.
NEXT : Respond to obstetrical problems on admission . CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D3
DECIDE ST AGEOFLABOUR
SIGNS
Bulging thin perineum, vagina gaping and head visible, full cervical dilatation.
Cervi cal dilatation: multigra vida5 cm pr imigra vida6 cm
Cervi cal dilatation 4 cm.
Cervi cal dilatation: 0-3 cm; contractions w eak and <2 in 10 minutes.
MANA GE
See secon d stag e of labour D10-D11 . Record in par tographN5.
See fir st stag e of lab our activ e labour D9. Startplotting par tographN5. Record in labour recordN5.
See fir st stag e of lab our not activ e labour D8. Record in labour recordN4.
CLASSIFY
IMMINENT DELIVER Y
LATE ACTIVE LAB OUR
EARLY ACTIVE LAB OUR
NOTYET IN ACTIVE LABOUR
Respond to obstetrical problems on admission
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
SIGNS
Tr ansverse lie. Continuous contractions. Constant pain betw een contractions. Sudden and se ver e abdominal pain . Horizontal ridg e across lo wer abdomen. Labour >24 hours.
Rupture of membranes and an y of: Fever>38C Foul-smelling v aginal discharg e.
Rupture of membranes at <8-months of pregnancy .
Di astolic blood pressure >90 mmHg .
Sever e palmar and conj unctival pallor and/or haemoglobin <7-g/dl.
Br eech or other malpresentation D16. Multiple pregnancy D18. Fetal distress D14. Pr olapsed cord D15.
TREAT AND AD VISE
Ifdi stressed, insertan IV line and giv e fluidsB9. Ifinlabour >24 hours, gi veappropriate IM/IV antibiotics B15. Refer urg ently to hospita l B17.
Gi veappropria te IM/IV antibiotics B15. Iflate labour , deliver and ref er to hosp ital after deliver yB17. Pl an to treat ne wbornJ5.
Gi veappropria te IM/IV antibiotics B15. Iflate labour , deliver D10-D28 . Di scontinue antibiotic for mother after deliv eryif no signsofinfection. Pl an to treat ne wbornJ5.
Assess fur therand manag e as onD23.
Manageas onD24.
Followspecific instructions (see pag e numbers in left column).
CLASSIFY
OBSTRUCTED LABOUR
UTERINE AND FETAL INFECTION
RISK OF UTERINE AND FETAL INFECTION
PRE-ECLAMPSIA
SEVERE ANAEMIA
OBSTETRICAL COMPLICATION
RESPOND T O OBSTETRICAL PR OBLEMS ON ADMISSION
Use this char t if abnor mal findings on assessing pre gnancy and fetal status D2-D3.
FORALL SITUA TIONS IN RED BELO W, REFER URGENTL YT O HOSPIT AL IF IN EARL Y LAB OUR, MANAGEONLY IF IN LA TE LAB OUR
D4
Respond to obstetrical problems on admission
SIGNS
War ts,kel oid tissue that ma y interfere with deliv ery . Pr ior third deg ree tear .
Bleeding an y time in third tr imester. Pr ior deliv eryby: caesarean section forceps or v acuum deliv ery . Age less than 14 y ears .
Labour before 8 completed months of pregnancy (more than one month before estimated date of deliv ery).
Fetal hear t rate <120 or >160 beats per minute.
Rupture of membranes at ter m and before labour .
If two or more of the fo llowing signs: thirsty sunkeneyes dry mouth skin pinch g oes back slo wly.
HIV test positiv e. Tak ing AR V treatment or pr ophylaxis and infant feeding .
No fetal mo vement, and No fetal hear t beat on repeated examination
TREAT AND AD VISE
Doa generous episiotomy and carefully control deliv eryof the hea d D10-D11 .
Iflate labour , deliverD10-D28 . Havehelp a vai lable during deliv ery .
Reassessfetal presentation (breech more commo Ifwoman is lying , encourag e her to li e on her left si de. Call for help during deliv ery . Conduct deliv eryver y carefully as small bab y ma y pop out suddenly . In par ticular, control deliv eryof the head. Pr epare equipm ent for resus citat ion of ne wbornK11.
Manageas onD14.
Gi veappropria te IM/IV antibiotics if r upture of membrane >18 hour s B15. Pl an to treat the ne wbornJ5.
Gi veoral fluids. Ifnot able to drink, gi ve1 litre IV fluids o ver3 hoursB9.
Ensure that the woman tak es AR V dr ugs pres cribed G9. Support her choice of infant feeding G7-G8.
Explain to the parents that the bab y is not doing wel l.
CLASSIFY
RISK OF OBSTETRI CAL COMPLICATION
PRETERM LABOUR
POSSIBLE FET AL DISTRESS
RUPTURE OF MEMBRANES
DEHYDRATION
HIV-POSITI VE
POSSIBLE FET AL DEA TH
NEXT : Givesupportiv e care throughout labour CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D5
D6
Communication
Explain all procedures, seek per mission, and discuss findings with th e woman. Keep her infor med about the prog ress of labour . Pr aise her , encourage and reassure her that things are g oing w ell. Ensure and respect priv acy during examinations and discussions. IfknownHI V positiv e,find out w hat she has told the companion. Respect her wishes.
Cleanliness
Encourage the w oman to bathe or sho werorwash herself and g enitals at the onset of labour . Wa sh the vulv a and perineal areas before each examination. Wa sh y our hands with soap before and after each examination. Use clean glo vesfor vaginal examination. Ensure cleanliness of labour and bir thing area(s). Cl ean up spills immediately . DO NO Tgi veenema.
Mobility
Encourage the w oman to walk around freely during the first stag e of labour . Support the w omans choice of position (left lateral, squating, kneeling, standing suppor ted b y the companion) for each stag e of labour and deliv ery .
Urination
Encourage the w oman to empty her bladder frequently . Remind her e ver y 2 hours.
Eating, drinking
Encourage the w oman to eat and drink as she wishes throughout labour . Nutritious liquid drinks are impor tant, even in lat e labou r. Ifthe woman has visib le se ver e wasting or tires during labour , makesure she eats and drinks.
Breathing technique
Teach her to notice he r nor mal breat hing. Encourage her to breathe out more slo wly, making a sighing noise, and to relax with each breath. Ifshe feels dizzy , unwell, isfeeling pins-and-needles (tingling) in her face, hands and feet, encourage her to breathe more slo wly. Topr event pushing at the end of first stag e of labour , teach her to pant, tobreathe with an open mouth, to tak e in 2 shor t brea ths follo wedbya l ong breath out. During deliv eryof the he ad,ask her not to push but to breathe steadily or to pant.
Pai n and discomfor t relief
Suggest chang e of pos ition. Encourage mobility, ascomfortable for her . Encourage companion to: massagethe w omans back if she fi nds thi s helpf ul. hold the w omans hand and spong e her face betw een cont ractions. Encourage her to use the breathing technique. Encourage warmbath or sho wer , if avai lable.
Ifwoman is distressed or anxious, investig ate the cause D2-D3. Ifpain is constant (persi sting between contr actions) and ver y severe or sudde n in onset D4.
GIVE SUPPORTIVE CARE THROUGHOUT LABOUR
Use this char t to provide a suppor tive, encouraging atmosphere for bir th,respectful of the woman s wishes.
Give suppor tive care throughout labour
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
Birthcompanion
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D7
Birthcompanion
Encourage support from the chosen bir th companion throughout labou r. Describe to the bir th companion w hat she or he should do: Al ways be with the w oman. Encourage her. Help her to breathe and relax. Rub her back, wi pe her bro w with a w et cloth, doot her suppor tiveactions. Gi vesupport using local practices w hich do not disturb labour or d eliver y. Encourage woman to mo vearound freely as she wishes and to ad opt the position of her choi ce. Encourage her to drink fluids and eat as she wishes. Assist her to the toilet w hen needed.
Ask the bir th companion to call for help if: The woman is bearing do wn with contractions. There is v aginal bleeding . She is suddenly in much more pain. She loses consciousness or has fits. There is an y other concer n.
Tell the bir th companion w hat she or he SHOULD NOTDOand explain w hy: DO NO Tencourage woman to push. DO NO Tgi veadvice other than that giv en by the health w orker . DONOTkeep woman in bed if she wants to mo vearound.
D2 EXAMINE THE WOMAN IN LABOUR OR
WITH RUPTURED MEMBRES
D3 DECIDE STAGE OF LABOUR
D4 RESPOND TO OBSTETRICAL
PROBLEMS ON ADMISSION (1)
D5 RESPOND TO OBSTETRICAL
PROBLEMS ON ADMISSION (2)
D6 GIVE SUPPORTIVE CARE
THROUGHOUT LABOUR
D7 BIRTH COMPANION
D8
MONITOR EVERY HOUR:
For emerg ency signs, using rapid assessment (RAM) B3-B7. Fr equency, intensity and duration of contractions. Fetal hear t rateD14. Mood and beha viour (distressed, anxious)D6.
Record findings regular ly in Labour record and P artog raphN4-N6. Record time of r upture of membranes and colour of amniotic fluid. Gi veSupportiv e careD6-D7. Never lea ve the woman alone.
ASSESS PR OGRESS OF LAB OUR
Af ter 8 hours if: Contractions strong er and more frequent but Nopr ogress in cer vical dilatation with or without membranes r uptured.
Af ter 8 hours if: noincrease in contractions, and membranes are not r uptured, and nopr ogress in cer vical dilatation.
Cervi cal dilatation 4 cm or g reater .
MONITOR EVERY 4 HOURS:
Cervi cal dilatation D3 D15. Unless indicated, DO NO Tdovaginal examination more frequently than e ver y 4 hours. Temperature. Pulse B3. Bl ood pressure D23.
TREAT AND AD VISE, IF REQUIR ED
Refer the woman urg ently to hospita l B17.
Di scharge the w oman and ad vise her to retur n if: pain/discomfort increases vaginal bleeding membranes r upture.
Begin plotting the p artog raphN5 and manag e the w oman as in Active labourD9.
FIRST ST AGEOFLABOUR: NOT INACTIVE LAB OUR
Use this char t for care of the woman when NO T INACTIVE LAB OUR, when cer vix dilated 0-3 cm and contr actions are weak, less than 2 in 10 minutes.
First stage of labour (1): when the woman is not in active labo ur
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D9
MONITOR EVERY 30 MINUTES:
For emerg ency signs, using rapid assessment (RAM) B3-B7. Fr equency, intensity and duration of contractions. Fetal hear t rateD14. Mood and beha viour (distressed, anxious)D6.
Record findings regular ly in Labour record and P artog raphN4-N6. Record time of r upture of membranes and colour of amniotic fluid. Gi veSupportiv e careD6-D7. Never lea ve the woman alone.
ASSESS PR OGRESS OF LAB OUR
Partograph passes to the right of ALERT LINE.
Partograph passes to the right of ACT ION LINE.
Cervi x dilated 10 cm or bulging perineum.
MONITOR EVERY 4 HOURS:
Cervi cal dilatation D3 D15. Unless indicated, do not do v aginal examination more frequently than e ver y 4 hour s. Temperature. Pulse B3. Bl ood pressure D23.
TREAT AND AD VISE, IF REQUIR ED
Reassess w oman and consider criteria for refer ral. Call senior person i f avai lable. Alert emergency transpor t ser vices. Encourage woman to empt y bladd er. Ensure adequate h ydration but omit solid foods. Encourage upright position and walking if woman wishes. Monitor intensiv ely.Reassess in 2 hours and refer if no prog ress. If refer ral tak es a long tim e,refer immediately (DO NO T wait to cross action line).
Refer urg ently to hospit al B17unless bir th is imminent.
Manageas inSecond stag e of labour D10-D11 .
FIRST ST AGEOFLABOUR: INACTIVE LAB OUR
Use this char t when the woman is IN ACTIVE LAB OUR, when cer vix dilated 4 cm or more.
First stage of labour (2): when the woman is in active labour
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D10
MONITOR EVERY 5 MINUTES:
For emerg ency signs, using rapid assessment (RAM) B3-B7. Fr equency, intensity and duration of contractions. Fetal hear t rateD14. Perineum thinning and bulging . Vi sible descent of fetal head or during contraction. Mood and beha viour (distressed, anxious)D6. Record findings regular ly in Labour record and P artog raph (pp.N4-N6). Gi veSupportiv e careD6-D7. Neverleavethe woman alone.
DELIVER THE BABY
Ensure all deliv eryequipment and supplies, including ne wborn resuscitation equipment, are available, and place of deliv eryis clean and war m (25C)L3.
Ensure bladder is empty . Assist the w oman into a comfor table position of her choice, asupright as possible. Staywith her and offer her emotional and ph ysical suppor t D10-D11 .
Al lowher to push as she wishes with contractions.
Wa it until head visible and perineum distending . Wa sh hands with clean water and soap. Put on glo vesjust before deliv ery . See Univ ersal precautions during labour and deliv eryA4.
TREAT AND AD VISE IF REQUIRED
Ifunable to pass urine and bladder is full, empty bladder B12. DO NO Tlet her lie fl at (horizontally) on her back. Ifthe woman is distre ssed, encourage pain discomfor t relie f D6.
DO NO Turgeher to push. If, after 30 minutes of s pontaneous expulsive efforts, the perineum does not begin to thin and stretch with contracti ons, do a v agina l examination to confir m full dilatation of cer vix. Ifcervi x is not fully dilated, await second stag e.Place w oman on her left side and discourag e pushing. Encourage breathing technique D6.
Ifsecond stag e lastsfor 2 hours or more without visible stead y desce nt of the hea d,callfor staff trained to use v acuum extractor or refer urg ently to hospita l B17. Ifobvious obstr uction to prog ress (war ts/scarr ing/keloid tissue/pre vious third deg ree tear), doa generous episiotomy . DO NO Tperfor m episiotomy routinely . Ifbreech or other malpr esentation, manageas onD16.
SECOND ST AGEOFLABOUR: DELIVER THE BABY AND GIVE IMMEDIA TE NEWB ORN CARE
Use this char t when cer vix dilated 10 cm or bulging thin perineum and head visible.
Second stage of labour : deliver the baby and give immediate newbor n care (1)
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
Second stage of labour : deliver the baby and give immediate newbor n care (2)
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D11
DELIVER THE BABY
Ensure controlled deliv eryof the head: Keep one hand g ently on the head as it ad vances with contractions. Support perineumwith other hand and co veranus with pad held in pos ition b y side of hand during deliv ery . Leavethe perineum visible (betw een thumb and first fing er). Ask the mother to breathe steadily and not to push during deliv eryof the head. Encourage rapid breathing with mouth open.
Feel gently around bab ysneck for the cord. Check if the face is clear of mucus and membranes.
Await spontaneous rotation of shoulders and deliv ery(within 1-2 minutes). Apply g entle do wnward pressure to deliv er top shoulder . Then lift bab y up, towards the mother s abdomen to deliv er lo wershoulder. Pl ace bab y on abdomen or in mother s ar ms. Note time of deliv ery .
Thoroughly dr y the bab y immediately . Wipe e yes. Discard w et cloth. Assess bab ysbreathing w hile dr ying. Ifthe bab y is not cr ying, observ e breathing: breathing w ell (chest rising)? not breathing or g asping?
Exclude second bab y. Palpate mother s abdomen. Gi ve10 IU oxytocin IM to the mother . Wa tch for v aginal bleeding .
Changeglov es.If not possible, wash glo vedhands. Cl amp and cut the cord. put ties tightly around the cord at 2 cm and 5 cm from bab ysabdomen. cut betw een ties with sterile instr ument. observ e for oozing blood.
Leavebabyon the mother s chest in skin-to-skin contact. Pl ace identification label. Coverthe bab y,cover the head with a hat.
Encourage initiation of breastfeeding K2.
TREAT AND AD VISE, IF REQUIR ED
If potentially damagi ng expulsiv e effor ts,exert more pressure on perineum. Discard soiled pad to p revent infec tion.
If cord present and lo ose, deliver the bab y thr ough the loop of cord or slip the cord o verthe bab yshead; if cord is tight, cl amp and cu t cord, then unwind. Gently wipe face clean w ith g auze or cloth, ifnecessary .
If dela y in deliv eryof shoulders: DO NO Tpanic but ca ll for help and ask companion to assist Manage as inStuck shoulde rsD17. If placing ne wborn on abdo men is not acceptable, orthe moth er cannot hold the bab y,place the bab y in a clean, warm,safe plac e close to the mother .
DO NO Tleavethe bab y wet - she/he will become cold. If the bab y is not breat hing or g asping (unless bab y is dead, macerated, severely malfo rme d): Cut cord quickly: transfer to a fir m,warmsurface; star t Ne wborn resuscitation K11. CALL FOR HELP - one per son should care for the mother.
If second bab y,DO NO Tgi veoxytocin no w.GET HELP . Deliver the second bab y.Manage as inMultiple pr egnancy D18. If hea vy bleeding , repeat oxytocin 10-IU-IM.
If blood oozing , place a second tie betw een the skin and the first tie.
DO NO Tapply an y substa nce to the stump. DO NO Tbandageor bind the stump.
If room cool (less tha n 25C), use additional blank et to co verthe moth er and bab y.
If HIV-positiv e mother h as chosen replacement feeding , feed acco rdingly. Check AR V treatment n eededG9.
D12
MONITOR MOTHER EVERY 5 MINUTES:
For emerg ency signs, using rapid assessment (RAM) B3-B7. Feel if uter us is w ell contracted. Mood and beha viour (distressed, anxious)D6. Ti me since third stag e beg an (time since bir th).
Record findings, treatments and procedures in Labour r ecordandPartograph (pp.N4-N6). Gi veSupportive careD6-D7. Never lea ve the woman alone.
DELIVER THE PLACENT A
Ensure 10-IU oxytocin IM is giv enD11. Await strong uterine contraction (2-3 minutes) and deliv er placenta bycontrolled cord traction : Pl ace side of one hand (usually left) abo vesymphysis pubis with palm facing to wards the mothers umbilicus. This applies counter traction to the uter us during controlled cor d traction. At the same time, apply stead y,sustained controlled cord traction. Ifpl acenta does not descend during 30-40 seconds of controlled co rd traction, release both cord traction and counter traction on the abdomen and wait until the u terus is well contracted ag ain. Then repeat controlled cord traction with counter traction. Asthe placenta is coming out, catch in both hands to pre vent tearing of the me mbranes. Ifthe membranes do not slip out spontaneously , gently twist them i nto a rope and mo vethem up and do wn to assist separation without tearing them.
Check that placenta and membranes are complete.
MONITOR BABY EVERY 15 MINU TES:
Breathing: listen for g runting, look for chest in-dra wing and fast breathing J2. Wa rmt h: check to see if feet are cold to touch J2.
TREAT AND AD VISE IF REQUIRED
If, after 30 minutes of g iving oxytocin, the placenta is not deliv ered and the w oman is NO T blee ding: Empty bladder B12 Encourage breastfeeding Repeat controlled cord traction. Ifwoman is bleeding , manageas onB5 Ifpl acenta is not deliv ered in another 30mi nutes (1 hour after deliv ery): Remov e placenta manually B11 Gi veappropriate IM/IV antibiotic B15. Ifin1 hour unable t o remo veplacenta: Refer the w oman to hospital B17 Insertan IV line and givefluids with 20 IU of oxytocin at 30 drops per minute during transfer B9. DO NO Texertexcessive traction on the cord. DO NO Tsqueeze or push t he uter us to deli verthe placenta.
Ifpl acenta is incomple te: Remov e placental fragments manually B11. Gi veappropriate IM/IV antibiotic B15.
THIRD ST AGEOFLABOUR: DELIVER THE PLA CENTA
Use this char t for care of the woman between bir th of the bab y and deliver y of placenta.
Third stage of labour : deliver the placenta
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
Third stage of labour : deliver the placenta
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D13
DELIVER THE PLACENT A
Check that uter us is w ell contracted and there is no hea vy bleeding . Repeat check e ver y 5 minutes.
Examine perineum, lowervagina and vulv a for tears.
Collect, estimate and record blood loss throughout third stag e and immediately afterwards.
Cl ean the w oman and the area beneath her . Put sanitar y pad or fold ed clean cloth under her buttocks to collect blood. Help her to chang e clothes if necessar y.
Keep the mother and bab y in deliv eryroom for a minimum of one ho ur after deliv eryof placenta.
Di spose of placenta in the cor rect, safe and culturally appropriate mann er.
TREAT AND AD VISE, IF REQUIR ED
Ifheavybl eeding: Massageuterus to expel clots if an y,until it is hard B10. Gi veoxytocin 10 IU IMB10. Call for help. Startan IV line B9, add 20 IU of oxytocin to IV fluids and giv e at 60 dr ops per minute N9. Empty the bladder B12. Ifbl eeding persists and ut erusis soft : Continue massaging uter us until it is hard. Apply bimanual or aor tic com pression B10. Continue IV fluids with 20 IU of oxytocin at 30 drops per minute. Refer woman urg ently to hospital B17.
Ifthird deg ree tear ( involving rectum or anus), refer urg ently to hospita l B17. For other tears: ap ply press ure o verthe tear with a sterile pad or gauze and put legs tog ether. DO NO Tcross ankles. Check after 5 minute s.If bleeding persists, repairthe tear B12.
Ifbl ood loss 250-ml, but bleeding has stopped: Pl an to k eep the w oman in the facility for 24 hours. Monitor intensiv ely (e ver y 30 minutes) for 4 hours: BP, pulse vaginal bleedin g ut erus, tomakesure it is w ell contracted. Assist the w oman w hen she first walks after resting and reco ver ing. Ifnot possible to o bserv e at the facility , refer to hospital B17.
Ifdi sposing placenta : Use glo veswhen handling placenta. Put placenta int o a bag and pl ace it int o a leak -proof container . Al ways carr y placen ta in a leak-proof container . Incinerate the placent a or bur y it at least 10 m a wayfroma water source, ina 2m deep pit.
D8 FIRST STAGE OF LABOUR (1): WHEN
THE WOMAN IS NOT IN ACTIVE
LABOUR
D9 FIRST STAGE OF LABOUR (2):
IN ACTIVE LABOUR
D10 SECOND STAGE OF LABOUR: DELIVER
THE BABY AND GIVE IMMEDIATE
NEWBORN CARE (1)
D11 SECOND STAGE OF LABOUR: DELIVER
THE BABY AND GIVE IMMEDIATE
NEWBORN CARE (2)
D12 THIRD STAGE OF LABOUR:
DELIVER THE PLACENTA (1)
D13 THIRD STAGE OF LABOUR:
DELIVER THE PLACENTA (2)
NEXT : If prolapsed cord
RESPOND T O PROBLEMS DURING LAB OUR AND DELIVERY
D14 Respond to problems during labour and deliver y (1) If FHR <120 or >1 60 bpm
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
ASK, CHECK RECORD LOOK, LISTEN, FEEL
Position the w oman on her left side. Ifmembranes ha veruptured, look at vulv a for prolapsed cord. See if liquor was meconium stained. Repeat FHR count after 15 minutes.
SIGNS
Cord seen at vulv a.
FHR remains >160 or <120 after 30 minutes obser vat ion.
FHR retur ns to nor mal.
TREAT AND AD VISE
Manage urgently as onD15.
If ear ly labour : Refer the woman urg ently to hospital B17 Keep her lying on her left side. Iflate labour : Call for help during deliv ery Monitor after e ver y contr action. IfFHR does not retur n to nor mal in 15 minutes explain to the woman (and her companion) that the bab y ma y not be w ell. Pr eparefor ne wborn resuscitation K11.
Monitor FHR e ver y 15 minutes.
CLASSIFY
PROLAPSE D CORD
BABY NO T WELL
BABY WELL
IF FET AL HEART RA TE (FHR) <120 OR >160 BEA TS PER MINUTE
IF PROLAPSED CORD
The cord is visible outside the v agina or can be felt in the v agina below the presenting par t.
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D15 Respond to problems during labour and deliver y (2) If prolapse d cord
ASK, CHECK RECORD LOOK, LISTEN, FEEL
Look at or feel the cord g ently for pulsations. Feel for transv erse lie. Dovaginal examination to determine status of labour .
SIGNS
Tr ansverse lie
Cord is pulsating
Cord is not pulsating
TREAT
Refer urg ently to hospita l B17.
If ear ly labour : Push the head orpr esenting par t out of the pelvis and hold itabovethe brim/pelvis with y our hand on the abdomen until caesarean section is perfor med. Instruct assistant (family , staff) to position the womansbuttocks higher than the shoulder . Refer urg ently to hospita l B17. Iftransfer not possible, al lowlabour to continue.
If late labour : Call for ad ditional help if possible (for mother and b y). Pr epare for Ne wborn resuscitation K11. Ask the w oman to assume an upright or squattin position to help prog ress. Expedite deliv erybyencouraging w oman to push with contraction.
Explain to the parents that bab y ma y not be w ell.
CLASSIFY
OBSTRUCTED LABOUR
FETUS ALIVE
FETUS PROBABL Y DEAD
NEXT : If breech presentation
Respond to problems during labour and deliver y (3) If breech pre sentation
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
SIGN
Ifearlylabour
Iflate labour
Ifthe head does not de liver after se ver al contractions
Iftrapped ar ms or shoulders
Iftrapped head (and bab y is dead)
NEXT : If stuck shoulders
IF BREECH PRESENT ATI ON
D16
TREAT
Refer urg ently to hospital B17.
Call for additional help. Confirmfull dilatation of the cer vix b y vaginal examination D3. Ensure bladder is empty . If unable to empty bladder see Empty bladder B12. Pr epare for ne wborn resuscitation K11. Deliver the bab y: Assist the w oman into a posi tion that will allo w the b abyto hang do wn duri ng deliv ery , for exam ple, propped up with buttocks at e dgeof bed or onto her hands and knees (all fours position). Wh en buttocks are disten ding, makean episi otomy. Al lowbuttocks, trunk and shoulders to deliv er spont aneously during contractions. Af ter deliv eryof the shoulders allo w the b abyto hang until next contraction.
Pl ace the bab y astride y our left forear m with limbs hanging on each side. Pl ace the middle and index fi ngers of the left hand o verthe malar cheek bones on eith er side to apply gentle do wnwards pressure t o aid flexion of head. Keeping the left hand as descri bed, placethe ind ex and ring fing ers of the right hand o verthe bab ys shoulders and the middle fing er on the bab yshead to g ently aid flexion until the hair lineis visible. Wh en the hair line is visible, raise the bab y in upward and forward direct ion to wards the mother s abdomen until the nose and mouth are free. The assistant giv es supra pubic pressure during the period t o maintain fl exion.
Feel the bab yschest for ar ms.If not fel t: Hold the bab y gently with hands around each thi gh and thumbs on sacr um. Gently guiding the bab y do wn, turnthe bab y,keeping the back upper most until the shoulder w hich was posterior (belo w) is no w ante rior (at the top) and the armis released. Then tur n the bab y back, again k eeping the back uppermost to deliv er the other ar m. Then proceed with deliv eryof head as desc ribedabov e.
Ti e a 1 kg w eight to the bab ysfeet and a wait full dilatation. Then proceed with deliv eryof head as desc ribedabov e. NEVERpull on the breech DO NO Tal lowthe w oman to push until the cer vix is full y dilated. Pushingtoo soo n ma y cause the head to be trapped.
LOOK, LISTEN, FEEL
Onexternal examination fetal head felt in fundus. Soft bod y par t (leg or buttocks) felt on v aginal examination. Legs or buttocks presenting at perineum.
Respond to problems during labour and deliver y (4) If stuck shou lders
SIGN
Fetal head is deliv ered, but shoulders are stuck and cannot be delivered.
Ifthe shoulders are s till not delivered and surgical help is not available immediately .
TREAT
Call for addit ional help. Pr epare for ne wborn resuscit ation. Explain the problem to the w oman and her companion. Ask the w oman to lie on her back w hile g ripp ing her legs tightly flexed ag ainst her chest, wi th knees wide apar t.Ask the companion or other helper to k eep the legs in that posi tion. Perfor m an adequate episiotomy . Ask an assi stant to apply continuous pr essure do wnwards, with the palm ofthe hand on the abdome n directly abo vethe pubic area, while y ou maint ain continuous downwa rd traction on the fetal hea d.
Remain calm and explai n to the w oman that you need her cooperation to tr y another position. Assisther to adopt a kneeling on all four sposition and ask her companion to hold her stead y - this simple chang e of position is sometimes suffici ent to dislodg e the impac ted shoulder and achie vedeliver y. Introduce the right hand into the v agina along the posterior cur veof the sacr um. At tempt to deliv er the pos terior shoulder or ar m using pr essure from the fing er of the righ t hand to hook the posterior shoulder and ar m do wnwards and forwards through the v agina. Complete the rest of deliv eryas nor mal. Ifnot successful, refer urg ently to hospita l B17.
DO NO Tpullexcessively on the head.
NEXT : If multiple bir ths
IF STUCK SHOULDERS (SHOULDER D YSTOCIA)
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D17
Respond to problems during labour and deliver y (5) If multiple bi rths
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
SIGN
Pr epare for deliv ery
Second stag e of labour
Third stag e of labour
Immediate postpar tum care
TREAT
Pr epare deliv eryroom and equipment for bir th of 2 or more babies. Include: more war m cloths two sets of cord ties and razor blades resuscitation equipment for 2 babies . Ar range for a helper to assist y ou with the bir ths and care of the babies.
Deliver the first bab y follo wing the usual procedure. Resuscitate if necessar y.Label her/h imT win 1. Ask helper to attend to the first bab y. Palpate uter us immediately to determine the lie of the second bab y.If transv erse or oblique li e,gently tur n the bab y by abdominal manipulation to head or breech prese Check the presentation b y vaginal examination. Check the fetal hear t rate. Await the retur n of strong contr actions and spontaneous r upture of the second bag of membranes, usually within 1 hour of bir th of first bab y,but ma y be long er. Staywith the w oman and continue monitoring her and the fetal hear t rate intensiv ely. Remov e wet cloths from underneath her. Iffeeling chilled, coverher. Wh en the membranes r upture, perfor m vaginal examination D3 to check for prolapse d cord. Ifpr esent, see Prolapsed cord D15. Wh en strong contractions restart, ask the mother to be ar do wn w hen she feels read y. Deliver the second bab y.Resuscitate if necessar y.Label her/him Twi n 2. Af ter cutting the cord, ask the helper to at tend to the second bab y. Palpate the uter us for a third bab y.If a third bab y is felt, pr oceed as described abo ve.Ifnothird bab y is felt, gotothird stag e of labour . DO NO Tattempt to deliv er the placenta until all the babies are bor n. DO NO Tgi vethe mother oxytoci n until after the bi rthofal l babies.
Gi veoxytocin 10 IU IM after making sure there isnot another bab y. Wh en the uter us is w ell contracted, deliver the placenta and membra nes b y controlled cord traction, applying traction to all cords tog ether D12-D23 . Before and after deliv eryof the placenta and membra nes, observ e closely for v aginal bleeding because this w oman is at g reater risk of postpar tum haemor rhage. If bleeding, see B5. Examine the placenta and membranes for completeness. There ma y be one larg e placenta w ith 2 umbilical cords, ora separate placenta with an umbilical cord for each y.
Monitor intensiv ely as risk of bleeding is incre ased. Pr ovi de immediate P ostpartum careD19-D20 . Inaddition: Keep mother in heal th centre for long er obser vat ion Pl an to measure haemo globin postpar tum if possible Gi vespecial suppor t for care and fee ding of babies J11 and K4.
NEXT : Care of the mother and ne wborn within first hour of deliv eryof placenta
IF MUL TIPLE BIRTHS
D18
D19
MONITOR MOTHER EVERY 15 MINUTES:
For emerg ency signs, using rapid assessment (RAM) B3-B7. Feel if uter us is hard and round.
Record findings, treatments and procedures in Labour r ecordandPartograph N4-N6. Keep mother and bab y in deliv eryroom - do not separ ate them . Never lea ve the woman and newbor n alone.
CARE OF MO THER AND NEWBORN
WOMAN Assess the amount of v aginal bleeding . Encourage the w oman to eat and drink. Ask the companion to sta y with the mother . Encourage the w oman to pass urine.
NEWBORN Wip e the e yes. Apply an antimicrobial within 1 hour of bir th. ei ther 1% silv er nitrate drops or 2.5% po vidone iodine drops or 1% tetracycline oint ment. DO NO T wash a waythe e yeantimicrobial. If blood or meconium, wi pe off with w et cloth and dr y. DO NO T remo vever nix or bathe the bab y. Continue k eeping the bab y war m and in skin-to-skin contact with the mother. Encourage the mother to initiate breastfeeding w hen bab y sho ws signs of readiness. Of fer her help. DO NO T giv e ar tificial teats or pre-lacteal feeds to the ne wborn: no water , sugar water, orlocal feeds. Examine the mother and ne wborn one hour after deliv eryof placenta. UseAssess the mother after deliver yD21and Examine the ne wbornJ2-J8.
MONITOR BABY EVERY 15 MINU TES:
Breathing: listen for g runting, look for chest in-dra wing and fast breathing J2. Wa rmt h: check to see if feet are cold to touch J2.
INTERVENTIONS , IF REQUIRED
Ifpad soak ed in less than 5 minutes, orconstant trickle of blood, manageas onD22.. If uter us soft, manageas onB10. If bleeding from a pe rineal tear , repair if required B12orrefer to hospital B17.
If breathing with difficulty g runting, chest in-dra wing or fast breath ing, examine the bab y as onJ2-J8. If feet are cold to tou ch or moth er and bab y are separated: Ensure the room is wa rm.Covermother and bab y with a blank et Reassess in 1 hour . If still cold,measure temperature. If less than 36.5 0C,manage as onK9. If unable to initiate breastfeeding (mother has complications): Pl an for alter native feeding method K5-K6. Ifmother HIV-po sitive: givetreatment to the ne wbornG9. Support the mother's choice of ne wborn feedingG8. If bab y is stillbor n or dea d,givesupportiv e care to mother and her fami lyD24.
Refer to hospital now if w oman had seri ous complications at admission or during deliv erybut was in late labour .
CARE OF THE MO THER AND NEWBORN WITHIN FIRST HOUR OF DELIVER Y OF PLA CENTA
Use this char t for woman and newbor n during the first hour after complete deliver y of placenta.
Care of the mother within first hour ofdelivery of placenta
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D14 RESPOND TO PROBLEMS DURING
LABOUR AND DELIVERY (1)
If fetal heart rate <120 or >160 bpm
D15 RESPOND TO PROBLEMS DURING
LABOUR AND DELIVERY (2)
If prolapsed cord
D16 RESPOND TO PROBLEMS DURING
LABOUR AND DELIVERY (3)
If breech presentation
D17 RESPOND TO PROBLEMS DURING
LABOUR AND DELIVERY (4)
If stuck shoulders
D18 RESPOND TO PROBLEMS DURING
LABOUR AND DELIVERY (5)
If multiple births
D19 CARE OF THE MOTHER AND
NEWBORN WITHIN FIRST HOUR OF
DELIVERY OF PLACENTA
Childbirth: labour, delivery and immediate postpartum care
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D1
D20
MONITOR MOTHER AT2,3 AND4 HOURS ,
THEN EVERY 4 HOURS:
For emerg ency signs, using rapid assessment (RAM). Feel uter us if hard and round.
Record findings, treatments and procedures in Labour r ecordandPartograph N4-N6. Keep the mother and bab y tog ether. Never lea ve the woman and newbor n alone. DO NO Tdischarge before 12 hours.
CARE OF MO THER
Accompany the mother and bab y to ward. Advise onPostpartumcareand hygiene D26. Ensure the mother has sanitar y napkins or clean material to collect v aginal blood. Encourage the mother to eat, drink and rest. Ensure the room is war m (25C).
Ask the mother s companion to watch her and call for help if bleedin g or pain increa ses,if mother feels dizzy or has se ver e headaches, vi sual disturbance or epig astric distress.
Encourage the mother to empty her bladder and ensure that she has passed urine.
Check record and giv e any treatment or proph ylaxis w hich is due. Advise the mother on postpar tum care and nutrition D26. Advise whe n to seek care D28. Counsel on bir th spacing and other family planning methods D27. Repeat examination of the mother before discharg e using Assess the mother after deliver y D21. For baby,see J2-J8.
INTERVENTIONS , IF REQUIRED
Makesure the w oman has someo ne with her and the y kno w when to call for help. IfHI V-positive: giveher appropriate treatment G6, G9.
Ifheavyvaginal bleeding , palpate the uter us. If uter us not fir m,massage the fun dus to mak e it contract and expel an y clotsB6. If pad is soak ed in less than 5 minutes, manageas onB5. If bleeding is from perineal tear, repair or refer to hospital B17.
Ifthe mother canno t pass urine or the bladder is full (s wel lingoverlowerabdomen) and she is uncomfortable, help her b y gently pouring water on vulv a. DONOTcatheterize unles s you ha veto.
Iftubal lig ation or IUD de sired, makeplans before discharg e. If mother is on antib iotics because of r upture of membranes >18 hours but sho ws no signs of infection no w,discontinue antibiotics.
CARE OF THE MO THER ONE HOUR AFTER DELIVER Y OF PLA CENTA
Use this char t for continuous care of the mother until discharg e.SeeJ10 for care of the bab y.
Care of the mother one hour after delivery of placenta
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
ASSESS THE MOTHER AFTER DELIVER Y
Use this char t to examine the mother the first time after deliver y (at 1 hour after deliver y or later) and for discharg e.
Forexamining the newbor n use the char t onJ2-J8.
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D21 Assess the mother after deliver y
ASK, CHECK RECORD
Check record: bl eeding more than 250 ml? completeness of placenta and membranes? complications during deliv eryor postpartum? special treatment needs? needs tubal lig ation or IUD? How are y ou feeling? Doyou ha veanypains? Doyou ha veanyconcerns? How is y our bab y? How do y our breasts feel?
LOOK, LISTEN, FEEL
Measure temperature. Feel the uter us.Is it hard and round? Look for v aginal bleeding Look at perineum. Isthere a tear or cut? Isitred,swol len or draining pus? Look for conjunctiv al pallor . Look for palmar pallor .
SIGNS
Ut erushard. Li ttle bleeding . Noperineal problem. Nopallor. Nofever . Bl ood pressure nor mal. Pulse nor mal.
TREAT AND AD VISE
Keep the mot her at the faci lity for 12 hours after deliv ery . Ensure pre ventivemeasures D25. Advise on postpar tum care and h ygiene D26. Counsel on nutrition D26. Counsel on bir th spacing and family planning D27. Advise on w hen to seek care and next routine postp artumvisitD28. Reassessfor discharg e D21. Continue an y treatments initiated ear lier. Iftubal lig ation desired, refer to hosp ital within 7 daysof deliv ery . If IUD desired, refer to appropriate service s within 48 hours.
CLASSIFY
MOTHER WELL
NEXT : Respond to problems immediately postpar tum If no problems, gotopageD25.
Respond to problems immediately postpar tum (1)
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
ASK, CHECK RECORD
Ti me since r upture of membranes Abdominal pain Chills
LOOK, LISTEN, FEEL
Apad is soak ed in less than 5 minutes.
Repeat temperature measure ment after 2 hours Iftemperature is still >38 C Look for abnor mal v aginal discharge. Li sten to fetal hear t rate feel lowerabdomen for tenderness
Isthere bleeding from the tear or episiotomy Does it extend to anus or rectum?
SIGNS
More than 1 pad soak ed in 5 minutes Ut erusnot hard and not round
Temperature still >38 0C and an y of: Chills Foul-smelling v aginal discharg e Low abdomen tender ness FHR remains >160 af ter 30 minutes of obser vat ion rupture of membranes >18 hours
Temperature still >38 0C
Tear extending to anus or rectu m.
Perineal tear Episiotomy
TREAT AND AD VISE
See B5 for treatment. Refer urg ently to hospita l B17.
Insertan IV line and giv e flui ds rapidly B9. Gi veappropriate IM/IV antibiotics B15. Ifbabyand plac enta deliv ered: Gi veoxytocin 10 IU IMB10. Refer woman urg ently to hospital B17. Assess the ne wbornJ2-J8. Tre at if an y sign of infection.
Encourage woman to drink plenty of fluids. Measuretemperat ure e ver y 4 hour s. Iftemperature persists for >12 hours, isveryhigh or rises rapidly , giveappropriate antibiotic and refer to hospital B15.
Refer woman urg ently to hospital B15.
Ifbl eeding persists, repair the tear or episiotomy B12 .
CLASSIFY
HEAVY BLEEDING
UTERINE AND FETAL INFECTION
RISK OF UTERINE AND FETAL INFECTION
THIRD DEGREE TEAR
SMALL PERINEAL TEAR
NEXT : If ele vat ed diastolic blood pressure
IF VAGI NAL BLEEDING
IF FEVER (TEMPERA TURE >38C)
IF PERINEAL TEAR OR EPISIO TOMY (DONE FOR LIFESA VING CIRCUMST ANCES)
D22
IF ELEV ATE D DIAST OLIC BLOOD PRESSURE
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D23 Respond to problems immediately postpar tum (2)
ASK, CHECK RECORD LOOK, LISTEN, FEEL
If diastolic blood pressure is 90 mmHg , repeat after 1 hour rest. Ifdi astolic blood pressure is still 90-mmHg, ask the w oman if she has: sever e headache bl urr ed vision epigastric pain and check protein in urine.
SIGNS
Diastolic blood pressure 110 mmHg OR Di astolic blood pressure 90 mmHg and 2+ proteinuria and anyof: sever e headache bl urr ed vision epigastric pain.
Diastolic blood pressure 90-110 mmHg on tw o readings. 2+pr oteinuria (on admission).
Diastolic blood pressure 90 mmHg on 2 readings.
TREAT AND AD VISE
Givemagnesium sulphate B13. Ifinearlylabour or postpar tum, refer urg ently to hospita l B17. If late labour : continue magnesium sulphate treatment B13 monitor blood pressure e ver y hour . DO NO Tgi veergometrine after deliv ery . Refer urg ently to hospita l after de liveryB17.
If ear ly labour , refer urg ently to hospital E17. Iflate labour : monitor blood pressure e ver y hour DO NO Tgiveergomet rine after deliv ery . IfBPremains elevat ed after deliv ery , refer to hospital E17.
Monitor blood pressure e ver y hour . DO NO Tgiveergomet rine after deliv ery . Ifbl ood pressure remains ele vat ed afte r deliv ery , refer woman to hospital E17.
CLASSIFY
SEVERE PRE-ECLAMPSIA
PRE-ECLAMPSIA
HYPERTENSION
NEXT : If pallor on screening , check for anaemia
Respond to problems immediately postpar tum (3)
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
ASK, CHECK RECORD
Bleeding during labour , deliver y or postpartum.
LOOK, LISTEN, FEEL
Measure haemoglobin, ifpossible. Look for conjunctiv al pallor . Look for palmar pallor . If pallor : Isitsever e pallor? Some pallor? Count number of breat hs in 1-minute
SIGNS
Haemoglobin <7 g/dl. AND/OR Severe palmar and conjunctiv al pallor or Anypallor with >30 breaths per minute.
Anybleeding. Haemoglobin 7-11-g/dl. Pal mar or conjunctiv al pallor .
Haemoglobin >11-g/dl No pallor .
CLASSIFY
SEVERE ANAEMIA
MODERATE ANAEMIA
NO ANAEMIA
NEXT : Giveprev entive measures
IF PALLOR ON SCREENING, CHECK FOR ANAEMIA
IF MO THER SEVEREL Y ILL OR SEP ARATED FR OMTHE BABY
IF BABY STILLB ORN OR DEAD
D24
TREAT AND AD VISE
If ear ly labour or postpar tum, refer urg ently to hospital B17.
If late labour : monitor intensiv ely mi nimi ze blood loss refer urg ently to hospita l after de liveryB17.
DO NO Tdi scharge before 24 hours. Check haemo globin after 3 da ys. Givedouble dose of iron for 3 months F3. Followup in 4 w eeks.
Giveiron/folate for 3 months F3.
Teach mother to express breast milk e ver y 3 hour s K5. Help her to express breast milk if necessar y.Ensure bab y receives mothers milkK8. Help her to establish or re-establish breastfeeding as s possible. See K2-K3.
Givesupportiv e care: Informthe parents as soon as possible after the bab ys death. Showthe bab y to the mother , givethe bab y to the mother to hold, whe re culturally appropriate. Of fer the parents and fam ily to be with the dead bab y in privacy as long as the y need. Di scuss with them t he events before the death and the possible causes of death. Advise the mother on breast care K8. Counsel on appropriate family planning method D27.
D25
ASSESS , CHECK RECORDS
Check RPR status in records. IfnoRPR during this pregnancy , do the RPR test L5.
Check tetanus toxoid (TT) immunization status. Check w hen last dose of mebendazole was giv en.
Check w omans supply of prescribed dose of iron/folate. Check if vitamin A giv en.
Ask w hether w oman and bab y are sleeping under insecticide treated bednet. Counsel and ad vise all w omen.
Record all treatments giv en N6.
Check HIV status in records.
TREAT AND AD VISE
IfRPR positiv e: Tre at woman and the partner with benzathine penicillin F6. Tre at the ne wbornK12.
Givetetanus toxoid if due F2. Gi vemebendazole once in 6 monthsF3.
Give3 month s supply of iron and counsel on compliance F3. Gi vevitamin A if dueF2.
Encourage sleeping under insecticide treated bednet F4. Advise on postpar tum care D26. Counsel on nutrition D26. Counsel on bir th spaci ng and family planning D27. Counsel on breastfeed ingK2. Counsel on safer sex i ncluding use of condoms G2. Advise on routine and fo llow-up postpartum visitsD28. Advise on dang er signs D28. Di scuss ho w to prepare for an emerg ency in postpar tumD28.
IfHI V-positive: Support adherence to ARVG6. Tre at the ne wbornG9. IfHI V test not done , offer her the test E5.
GIVE PREVENTIVE MEASURES
Ensure that all are given before discharg e.
Give pre ventive measures
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D20 CARE OF THE MOTHER ONE HOUR
AFTER DELIVERY OF PLACENTA
D21 ASSESS THE MOTHER AFTER DELIVERY
D22 RESPOND TO PROBLEMS
IMMEDIATELY POSTPARTUM (1)
If vaginal bleeding
If fever
If perineal tear or episiotomy
D23 RESPOND TO PROBLEMS
IMMEDIATELY POSTPARTUM (2)
If elevated diastolic blood pressure
D24 RESPOND TO PROBLEMS
IMMEDIATELY POSTPARTUM (3)
If pallor on screening, check for anaemia
If mother severely ill or separated from baby
If baby stillborn or dead
D25 GIVE PREVENTIVE MEASURES
D26
Advise on postpar tum care and h ygiene
Advise and explain to the w oman: Toal ways have someone near her for the first 24 hours to respond to a nychange in her condition. Not to inser t anything into the v agina. Tohaveenough rest and sleep. The impor tance of washing to pre vent infection of the mother and her baby: wash hands before handling bab y wash perineum daily and after faecal excretion changeperineal pads e ver y 4 to 6 hours, ormore frequently if hea vy lochia wash used pads or dispose of them safely wash the bod y daily . Toavoid sexual intercourse until the perineal w ound heals.
Counsel on nutriti on
Advise the w oman to eat a greater amount and v ariety of health y foods, such as meat, fi sh,oils, nuts, seeds, cereals, beans, vegetables, cheese, milk, to help her feel w ell and strong (giv e examples of types of food and h owmuch to eat). Reassure the mother that she can eat an y nor mal foods these wil l not har m the breas tfeeding bab y. Spend more time on n utrition counselling with v erythinwomen and adol escents. Determine if there are impor tant taboos about food s which are nutritionally health y. Advise the w oman ag ainst these taboos. Talk to family membe rs such as par tner and mother-in-la w,to encourag e them to help ensure the woman eats enough and a voi ds hard ph ysical w ork.
ADVISE ON POSTP ARTUM CARE
Advise on postpar tum care
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D27
Counsel on the impor tance of family plannin g
Ifappropriate, ask the w oman if she w ould lik e her par tner or another fami ly member to be included in the counselling session. Explain that after bir th,if she has sex and is not exclusiv ely breastfeeding , she can become pregnant as soon as 4 w eeks after deliv ery . Therefore it is impor tant to star t thinking ear ly about w hat family planning method the y will use. Ask about plans for ha ving more children. Ifshe (and her par tner) want more children, advise that waiting at least 2-3 y ears betw een pregnancies is healthier for th e mother and chil d. Information on when to star t a method after deliv erywill v arydepending on w hether a w oman is breastfeeding or not. Makearr angements for the w oman to see a family planning counsel lor,orcounsel her directly (see the Decision-making tool for family planning provider s and clients for infor mation on methods and on the counselling process). Councel on safer sex including use of condoms for dual protection fromsexually transmitted infection (STI) or HIV and pregnancy . Promote their use, especially if at risk for sexually transmitted infection (STI) or HIV G2. For HIV-positiv e women, see G4 for family planning considerations Her par tner can decide to ha vea vasectomy (male sterilization) at an y time.
Method options for the non-breastfeeding woman Can be used immediately postpar tum Condoms Progestogen-only oral contraceptiv es Progestogen-only injectables Implant Spermicide Female sterilization ( within 7 da ys or dela y 6 w eeks) copper IUD (immediate ly follo wing expulsion of placenta or within 48 hours) Delay3 weeks Combined oral contracept ives Combined injectables Fertility awareness methods
Lactational amenor rhoea method (LAM)
Abreastfeeding w oman is protected from pregnancy only if: she is no more th an 6 months postpar tum, and she is breastfeed ing exclusiv ely (8 or more time s a da y,includin g at least once at night: no daytime feedings more than 4 hours apart and no night feedings more than 6 hours apar t; no complementary foods or fluids), and her menstr ual cycle has not retur ned.
Abreastfeeding w oman can also choose an y other family planning method, ei ther to use alone or together with LAM.
Method options for the breastf eeding woman Can be used immediatel y postpar tum Lactational amenor rhoea method (LAM) Condoms Spermicide Female sterilisation (within 7 da ys or dela y 6 w eeks) copper IUD (within 48 hours or dela y 4 w eeks) Delay6 weeks Pr ogesto gen-only oral contraceptiv es Progestogen-only injectab les Implants Diaphragm Delay6 months Combined oral contraceptiv es Combined injectables Fertility awareness methods
COUNSEL ON BIRTH SP ACI NG AND FAMILYPLANNING
Counsel on bir th spacing and family planning
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D28
Routine postpar tum care visits
FIRST VISIT D19 Wit hin the first w eek, preferably within 2-3 da ys
SECOND VISIT E2 4-6 weeks
Follo w-up visits for problems
If the problem w as: Retur n in: Fever 2days Lower urinar y tract infection 2days Per ineal infection or pain 2 da ys Hypertension 1 week Urinar y incontinence 1week Severe anaemia 2 weeks Postpartum blues 2 week s HIV-positive 2 weeks Moderate anaemia 4 weeks If treated in hospital According to hospital instr uctions or according to national for any complication guidelines, but no later than in 2 weeks.
Advise on dang er signs
Advise to g o to a hospital or health centre imme diately, day or nigh t,WITHOUT WAITING , if any of the following signs: vaginal bleeding: more than 2 or 3 pad s soak ed in 20-30 minutes after deliv eryOR bl eeding increases ratherthan decreases after deliv ery . convulsions. fast or difficult breat hing. feverand too w eak to g et out of bed . sever e abdominal pain.
Go to health centre as soon as possibl e ifany of the following signs: fever abdominal pain feels ill breasts s wol len, red or tender breasts, orsore nipple ur ine dribbling or pa in on micturition pain in the perineum o r draining pus foul-smelling lochia
Discuss ho w to prep are for an emerg ency in postpar tum
Advise to alwa ys ha vesomeone near for at least 24 hours after deliv eryto respond to an y chang e in condition. Di scuss with w oman and her par tnerand family about emerg ency issues: where to g o if dang er signs how to reach the h ospital costs in vol ved family and communi ty suppor t. Advise the w oman to ask for help from the community , if needed I1-I3. Advise the w oman to brin g her home-based mater nal record to the health centre, even for an emergency visit.
ADVISE ON WHEN T O RETURN
Use this char t for advising on postpar tum care on D21or E2. For newbor n babies see the schedule on K14.
Encourag e woman to bring her par tner or family member to at least one visit.
Advise on when to retur n
CH
ILD
BIRTH
: LABO
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D29
Preparation for home deliv ery
Check emerg ency ar rangements. Keep emerg ency transpor t ar rangements up-to-date. Carry with y ou all essential dr ugsB17, records, and the deliv erykit. Ensure that the family prepares, asonC18.
Deliver y care
Followthe labour and deliv eryprocedures D2-D28K11. Observ e univ ersal precautions A4. Gi veSupportive care. Involvethe companion in care and suppor t D6-D7. Maintain the par tograph and labour record N4-N6. Pr ovi de ne wborn careJ2-J8. Refer to facility as soon as possible if an y abnor mal finding in mothe r or bab yB17 K14.
Immediate postpar tum care of mother
Staywith the w oman for fi rst tw o hours after deliv eryof placenta C2 C13-C14 . Examine the mother be fore lea ving her D21. Advise on postpar tum care, nutrition and family planning D26-D27 . Ensure that someone w ill sta y with the mother for the first 24 hours.
Postpartum care of ne wborn
Stayuntil bab y has had the f irst breastfeed and help the mother g ood positioning and attachment B2. Advise on breastfeed ing and breast care B3. Examine the bab y before lea vingN2-N8. Immunize the bab y if possible B13. Advise on ne wborn careB9-B10. Advise the family about danger signsand when and w here to seek care B14. Ifpossible, retur n with in a da y to check the mother and bab y. Advise a postpar tum visi t for the mother and baby wit hin the fir st weekB14.
HOME DELIVER Y BY SKILLED ATTE NDANT
Use these instr uctions if you are attending deliver y at home.
Home deliver y by skilled attendant
CH
ILD
BIRTH
: LAB
O
U
R, D
ELIV
ERY
AN
D
IM
M
ED
IA
TE PO
STP
ARTU
M
CARE
D26 ADVISE ON POSTPARTUM CARE
Advise on postpartum care and hygiene
Counsel on nutrition
D27 COUNSEL ON BIRTH SPACING AND
FAMILY PLANNING
Counsel on importance of family planning
Lactation and amenorrhoea method (LAM)
D28 ADVISE ON WHEN TO RETURN
Routine postpartum visits
Advise on danger signs
Discuss how to prepare for an emergency
postpartum
D29 HOME DELIVERY BY SKILLED
ATTENDANT
Preparation for home delivery
Delivery care
Immediate postpartum care of the mother
Postpartum care of the newborn
Always begin with Rapid assessment and management (RAM) B3-B7 .
Next, use the chart on Examine the woman in labour or with
ruptured membranes D2-D3 to assess the clinical situation and
obstetrical history, and decide the stage of labour.
If an abnormal sign is identified, use the charts on Respond to
obstetrical problems on admission D4-D5 .
Care for the woman according to the stage of labour D8-D13 and
respond to problems during labour and delivery as on D14-D18.
Use Give supportive care throughout labour D6-D7
to provide
support and care throughout labour and delivery.
Record findings continually on labour record and partograph N4-N6 .
Keep mother and baby in labour room for one hour after delivery
and use charts Care of the mother and newborn within first
hour of delivery placenta on D19 .
Next use Care of the mother after the first hour following
delivery of placenta D20 to provide care until discharge. Use
chart on D25 to provide Preventive measures and Advise on
postpartum care D26-D28 to advise on care, danger signs, when
to seek routine or emergency care, and family planning.
Examine the mother for discharge using chart on D21 .
Do not discharge mother from the facility before 12 hours.
If the mother is HIV-positive or adolescent, or has special needs,
see G1-G11 H1-H4 .
If attending a delivery at the womans home, see D29 .
Examine the woman in labour or with ruptured membranes
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
ASK, CHECK RECORD
History of this labour:
When did contractions begin?
How frequent are contractions?
How strong?
Have your waters broken? If yes,
when? Were they clear or green?
Have you had any bleeding?
If yes, when? How much?
Is the baby moving?
Do you have any concern?
Check record, or if no record:
Ask when the delivery is expected.
Determine if preterm
(less than 8 months pregnant).
Review the birth plan.
If prior pregnancies:
Number of prior pregnancies/
deliveries.
Any prior caesarean section,
forceps, or vacuum, or other
complication such as postpartum
haemorhage?
Any prior third degree tear?
Current pregnancy:
RPR status C5 .
Hb results C4 .
Tetanus immunization status F2 .
HIV status C6 .
Infant feeding plan G7-G8 .
Receiving any medicine.
LOOK , LISTEN, FEEL
Observe the womans response to
contractions:
Is she coping well or is she
distressed?
Is she pushing or grunting?
Check abdomen for:
caesarean section scar.
horizontal ridge across lower
abdomen (if present, empty bladder
B12 and observe again).
Feel abdomen for:
contractions frequency, duration,
any continuous contractions?
fetal lielongitudinal or
transverse?
fetal presentationhead, breech,
other?
more than one fetus?
fetal movement.
Listen to the fetal heart beat:
Count number of beats in 1 minute.
If less than 100 beats per
minute, or more than 180, turn
woman on her left side and count
again.
Measure blood pressure.
Measure temperature.
Look for pallor.
Look for sunken eyes, dry mouth.
Pinch the skin of the forearm: does
it go back quickly?
NEXT: Perform vaginal examination and decide stage of labour
EXAMINE THE WOMAN IN LABOUR OR WITH RUPTURED MEMBRANES
First do Rapid assessment and management B3-B7 . Then use this chart to assess the womans and fetal status and decide stage of labour.
D2
Decide stage of labour
ASK, CHECK RECORD
Explain to the woman that
you will give her a vaginal
examination and ask for her
consent.
LOOK, LISTEN, FEEL
Look at vulva for:
bulging perineum
any visible fetal parts
vaginal bleeding
leaking amniotic fluid; if yes, is it
meconium stained, foul-smelling?
warts, keloid tissue or scars that may
interfere with delivery.
Perform vaginal examination
DO NOT shave the perineal area.
Prepare:
clean gloves
swabs, pads.
Wash hands with soap before and after each
examination.
Wash vulva and perineal areas.
Put on gloves.
Position the woman with legs flexed and apart.
DO NOT perform vaginal examination if bleeding
now or at any time after 7 months of pregnancy.
Perform gentle vaginal examination (do not start
during a contraction):
Determine cervical dilatation in
centimetres.
Feel for presenting part. Is it hard, round
and smooth (the head)? If not, identify the
presenting part.
Feel for membranes are they intact?
Feel for cord is it felt? Is it pulsating? If
so, act immediately as on D15 .
NEXT: Respond to obstetrical problems on admission.
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D3
DECIDE STAGE OF LABOUR
SIGNS
Bulging thin perineum, vagina
gaping and head visible, full
cervical dilatation.
Cervical dilatation:
multigravida 5 cm
primigravida 6 cm
Cervical dilatation 4 cm.
Cervical dilatation: 0-3 cm;
contractions weak and
<2 in 10 minutes.
MANAGE
See second stage of labour D10-D11.
Record in partograph N5 .
See first stage of labour active labour D9 .
Start plotting partograph N5 .
Record in labour record N5 .
See first stage of labour not active labour D8 .
Record in labour record N4 .
CLASSIFY
IMMINENT DELIVERY
LATE ACTIVE LABOUR
EARLY ACTIVE LABOUR
NOT YET IN ACTIVE
LABOUR
Respond to obstetrical problems on admission
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
SIGNS
Transverse lie.
Continuous contractions.
Constant pain between contractions.
Sudden and severe abdominal pain.
Horizontal ridge across lower
abdomen.
Labour >24 hours.
Rupture of membranes and any of:
Fever >38C
Foul-smelling vaginal discharge.
Rupture of membranes at
<8-months of pregnancy.
Diastolic blood pressure >90 mmHg.
Severe palmar and conjunctival
pallor and/or haemoglobin <7-g/dl.
Breech or other malpresentation D16 .
Multiple pregnancy D18 .
Fetal distress D14 .
Prolapsed cord D15 .
TREAT AND ADVISE
If distressed, insert an IV line and give fluids B9 .
If in labour >24 hours, give appropriate IM/IV
antibiotics B15 .
Refer urgently to hospital B17 .
Give appropriate IM/IV antibiotics B15 .
If late labour, deliver and refer to hospital
after delivery B17 .
Plan to treat newborn J5 .
Give appropriate IM/IV antibiotics B15 .
If late labour, deliver D10-D28.
Discontinue antibiotic for mother after delivery if no
signs of infection.
Plan to treat newborn J5 .
Assess further and manage as on D23 .
Manage as on D24 .
Follow specific instructions
(see page numbers in left column).
CLASSIFY
OBSTRUCTED LABOUR
UTERINE AND
FETAL INFECTION
RISK OF UTERINE AND
FETAL INFECTION
PRE-ECLAMPSIA
SEVERE ANAEMIA
OBSTETRICAL
COMPLICATION
RESPOND TO OBSTETRICAL PROBLEMS ON ADMISSION
Use this chart if abnormal findings on assessing pregnancy and fetal status D2-D3 .
FOR ALL SITUATIONS IN RED BELOW, REFER URGENTLY TO HOSPITAL IF IN EARLY LABOUR, MANAGE ONLY IF IN LATE LABOUR
D4
Respond to obstetrical problems on admission
SIGNS
Warts, keloid tissue that may
interfere with delivery.
Prior third degree tear.
Bleeding any time in third trimester.
Prior delivery by:
caesarean section
forceps or vacuum delivery.
Age less than 14 years .
Labour before 8 completed months
of pregnancy (more than one month
before estimated date of delivery).
Fetal heart rate
<120 or >160 beats per minute.
Rupture of membranes at term and
before labour.
If two or more of the following signs:
thirsty
sunken eyes
dry mouth
skin pinch goes back slowly.
HIV test positive.
Taking ARV treatment or prophylaxis.
No fetal movement, and
No fetal heart beat on
repeated examination
TREAT AND ADVISE
Do a generous episiotomy and carefully control
delivery of the head D10-D11 .
If late labour, deliver D10-D28 .
Have help available during delivery.
Reassess fetal presentation (breech more common).
If woman is lying, encourage her to lie on her left side.
Call for help during delivery.
Conduct delivery very carefully as small baby may pop
out suddenly. In particular, control delivery of the head.
Prepare equipment for resuscitation of newborn K11 .
Manage as on D14 .
Give appropriate IM/IV antibiotics if rupture of
membrane >18 hours B15 .
Plan to treat the newborn J5 .
Give oral fluids.
If not able to drink, give 1 litre IV fluids over 3 hours B9 .
Ensure that the woman takes ARV drugs as
prescribed G6
, G9 .
Support her choice of infant feeding G7-G8 .
Explain to the parents that the baby is not doing
well.
CLASSIFY
RISK OF OBSTETRICAL
COMPLICATION
PRETERM
LABOUR
POSSIBLE FETAL
DISTRESS
RUPTURE OF
MEMBRANES
DEHYDRATION
HIV-POSITIVE
POSSIBLE FETAL DEATH
NEXT: Give supportive care throughout labour
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D5
D6
Communication
Explain all procedures, seek permission, and discuss findings with the woman.
Keep her informed about the progress of labour.
Praise her, encourage and reassure her that things are going well.
Ensure and respect privacy during examinations and discussions.
If known HIV positive, find out what she has told the companion. Respect her wishes.
Cleanliness
Encourage the woman to bathe or shower or wash herself and genitals at the onset of labour.
Wash the vulva and perineal areas before each examination.
Wash your hands with soap before and after each examination. Use clean gloves for vaginal
examination.
Ensure cleanliness of labour and birthing area(s).
Clean up spills immediately.
DO NOT give enema.
Mobility
Encourage the woman to walk around freely during the first stage of labour.
Support the womans choice of position (left lateral, squating, kneeling, standing supported by the
companion) for each stage of labour and delivery.
Urination
Encourage the woman to empty her bladder frequently. Remind her every 2 hours.
Eating, drinking
Encourage the woman to eat and drink as she wishes throughout labour.
Nutritious liquid drinks are important, even in late labour.
If the woman has visible severe wasting or tires during labour, make sure she eats and drinks.
Breathing technique
Teach her to notice her normal breathing.
Encourage her to breathe out more slowly, making a sighing noise, and to relax with each breath.
If she feels dizzy, unwell, is feeling pins-and-needles (tingling) in her face, hands and feet,
encourage her to breathe more slowly.
To prevent pushing at the end of first stage of labour, teach her to pant, to breathe with an open
mouth, to take in 2 short breaths followed by a long breath out.
During delivery of the head, ask her not to push but to breathe steadily or to pant.
Pain and discomfort relief
Suggest change of position.
Encourage mobility, as comfortable for her.
Encourage companion to:
massage the womans back if she finds this helpful.
hold the womans hand and sponge her face between contractions.
Encourage her to use the breathing technique.
Encourage warm bath or shower, if available.
If woman is distressed or anxious, investigate the cause D2-D3 .
If pain is constant (persisting between contractions) and very severe or sudden in onset D4 .
GIVE SUPPORTIVE CARE THROUGHOUT LABOUR
Use this chart to provide a supportive, encouraging atmosphere for birth, respectful of the womans wishes.
Give supportive care throughout labour
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
Birth companion
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D7
Birth companion
Encourage support from the chosen birth companion throughout labour.
Describe to the birth companion what she or he should do:
Always be with the woman.
Encourage her.
Help her to breathe and relax.
Rub her back, wipe her brow with a wet cloth, do other supportive actions.
Give support using local practices which do not disturb labour or delivery.
Encourage woman to move around freely as she wishes and to adopt the position of her choice.
Encourage her to drink fluids and eat as she wishes.
Assist her to the toilet when needed.
Ask the birth companion to call for help if:
The woman is bearing down with contractions.
There is vaginal bleeding.
She is suddenly in much more pain.
She loses consciousness or has fits.
There is any other concern.
Tell the birth companion what she or he SHOULD NOT DO and explain why:
DO NOT encourage woman to push.
DO NOT give advice other than that given by the health worker.
DO NOT keep woman in bed if she wants to move around.
D8
MONITOR EVERY HOUR:
For emergency signs, using rapid assessment (RAM) B3-B7 .
Frequency, intensity and duration of contractions.
Fetal heart rate D14.
Mood and behaviour (distressed, anxious) D6 .
Record findings regularly in Labour record and Partograph N4-N6 .
Record time of rupture of membranes and colour of amniotic fluid.
Give Supportive care D6-D7 .
Never leave the woman alone.
ASSESS PROGRESS OF LABOUR
After 8 hours if:
Contractions stronger and more frequent but
No progress in cervical dilatation with or without membranes ruptured.
After 8 hours if:
no increase in contractions, and
membranes are not ruptured, and
no progress in cervical dilatation.
Cervical dilatation 4 cm or greater.
MONITOR EVERY 4 HOURS:
Cervical dilatation D3
D15.
Unless indicated, DO NOT do vaginal examination more frequently than every 4 hours.
Temperature.
Pulse B3 .
Blood pressure
D23.
TREAT AND ADVISE, IF REQUIRED
Refer the woman urgently to hospital B17.
Discharge the woman and advise her to return if:
pain/discomfort increases
vaginal bleeding
membranes rupture.
Begin plotting the partograph N5 and manage the woman as in Active labour D9 .
FIRST STAGE OF LABOUR: NOT IN ACTIVE LABOUR
Use this chart for care of the woman when NOT IN ACTIVE LABOUR, when cervix dilated 0-3 cm and contractions are weak, less than 2 in 10 minutes.
First stage of labour (1): when the woman is not in active labour
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D9
MONITOR EVERY 30 MINUTES:
For emergency signs, using rapid assessment (RAM) B3-B7 .
Frequency, intensity and duration of contractions.
Fetal heart rate D14.
Mood and behaviour (distressed, anxious) D6 .
Record findings regularly in Labour record and Partograph N4-N6 .
Record time of rupture of membranes and colour of amniotic fluid.
Give Supportive care D6-D7 .
Never leave the woman alone.
ASSESS PROGRESS OF LABOUR
Partograph passes to the right of ALERT LINE.
Partograph passes to the right of ACTION LINE.
Cervix dilated 10 cm or bulging perineum.
MONITOR EVERY 4 HOURS:
Cervical dilatation D3
D15.
Unless indicated, do not do vaginal examination more frequently than every 4 hours.
Temperature.
Pulse B3 .
Blood pressure
D23.
TREAT AND ADVISE, IF REQUIRED
Reassess woman and consider criteria for referral.
Call senior person if available. Alert emergency transport services.
Encourage woman to empty bladder.
Ensure adequate hydration but omit solid foods.
Encourage upright position and walking if woman wishes.
Monitor intensively. Reassess in 2 hours and refer if no progress. If referral takes a long time, refer
immediately (DO NOT wait to cross action line).
Refer urgently to hospital B17 unless birth is imminent.
Manage as in Second stage of labour D10-D11.
FIRST STAGE OF LABOUR: IN ACTIVE LABOUR
Use this chart when the woman is IN ACTIVE LABOUR, when cervix dilated 4 cm or more.
First stage of labour (2): when the woman is in active labour
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D10
MONITOR EVERY 5 MINUTES:
For emergency signs, using rapid assessment (RAM) B3-B7 .
Frequency, intensity and duration of contractions.
Fetal heart rate D14.
Perineum thinning and bulging.
Visible descent of fetal head or during contraction.
Mood and behaviour (distressed, anxious) D6 .
Record findings regularly in Labour record and Partograph N4-N6 .
Give Supportive care D6-D7 .
Never leave the woman alone.
DELIVER THE BABY
Ensure all delivery equipment and supplies, including newborn resuscitation equipment, are
available, and place of delivery is clean and warm (25C) L3 .
Ensure bladder is empty.
Assist the woman into a comfortable position of her choice, as upright as possible.
Stay with her and offer her emotional and physical support D10-D11.
Allow her to push as she wishes with contractions.
Wait until head visible and perineum distending.
Wash hands with clean water and soap. Put on gloves just before delivery.
See Universal precautions during labour and delivery A4 .
TREAT AND ADVISE IF REQUIRED
If unable to pass urine and bladder is full, empty bladder B12 .
DO NOT let her lie flat (horizontally) on her back.
If the woman is distressed, encourage pain discomfort relief D6 .
DO NOT urge her to push.
If, after 30 minutes of spontaneous expulsive efforts, the perineum does not begin to thin and
stretch with contractions, do a vaginal examination to confirm full dilatation of cervix.
If cervix is not fully dilated, await second stage. Place woman on her left side and discourage
pushing. Encourage breathing technique D6 .
If second stage lasts for 2 hours or more without visible steady descent of the head, call for staff
trained to use vacuum extractor or refer urgently to hospital B17 .
If obvious obstruction to progress (warts/scarring/keloid tissue/previous third degree tear), do a
generous episiotomy. DO NOT perform episiotomy routinely.
If breech or other malpresentation, manage as on D16 .
SECOND STAGE OF LABOUR: DELIVER THE BABY AND GIVE IMMEDIATE NEWBORN CARE
Use this chart when cervix dilated 10 cm or bulging thin perineum and head visible.
Second stage of labour: deliver the baby and give immediate newborn care (1)
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
Second stage of labour: deliver the baby and give immediate newborn care (2)
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D11
DELIVER THE BABY
Ensure controlled delivery of the head:
Keep one hand gently on the head as it advances with contractions.
Support perineum with other hand and cover anus with pad held in position by side of hand during delivery.
Leave the perineum visible (between thumb and first finger).
Ask the mother to breathe steadily and not to push during delivery of the head.
Encourage rapid breathing with mouth open.
Feel gently around babys neck for the cord.
Check if the face is clear of mucus and membranes.
Await spontaneous rotation of shoulders and delivery (within 1-2 minutes).
Apply gentle downward pressure to deliver top shoulder.
Then lift baby up, towards the mothers abdomen to deliver lower shoulder.
Place baby on abdomen or in mothers arms.
Note time of delivery.
Thoroughly dry the baby immediately. Wipe eyes. Discard wet cloth.
Assess babys breathing while drying.
If the baby is not crying, observe breathing:
breathing well (chest rising)?
not breathing or gasping?
Exclude second baby.
Palpate mothers abdomen.
Give 10 IU oxytocin IM to the mother.
Watch for vaginal bleeding.
Change gloves. If not possible, wash gloved hands.
Clamp and cut the cord.
put ties tightly around the cord at 2 cm and 5 cm from babys abdomen.
cut between ties with sterile instrument.
observe for oozing blood.
Leave baby on the mothers chest in skin-to-skin contact. Place identification label.
Cover the baby, cover the head with a hat.
Encourage initiation of breastfeeding K2 .
TREAT AND ADVISE, IF REQUIRED
If potentially damaging expulsive efforts, exert more pressure on perineum.
Discard soiled pad to prevent infection.
If cord present and loose, deliver the baby through the loop of cord or slip the cord over the babys head;
if cord is tight, clamp and cut cord, then unwind.
Gently wipe face clean with gauze or cloth, if necessary.
If delay in delivery of shoulders:
DO NOT panic but call for help and ask companion to assist
Manage as in Stuck shoulders D17 .
If placing newborn on abdomen is not acceptable, or the mother cannot hold the baby, place the baby in
a clean, warm, safe place close to the mother.
DO NOT leave the baby wet - she/he will become cold.
If the baby is not breathing or gasping (unless baby is dead, macerated, severely malformed):
Cut cord quickly: transfer to a firm, warm surface; start Newborn resuscitation K11 .
CALL FOR HELP - one person should care for the mother.
If second baby, DO NOT give oxytocin now. GET HELP.
Deliver the second baby. Manage as in Multiple pregnancy D18 .
If heavy bleeding, repeat oxytocin 10-IU-IM.
If blood oozing, place a second tie between the skin and the first tie.
DO NOT apply any substance to the stump.
DO NOT bandage or bind the stump.
If room cool (less than 25C), use additional blanket to cover the mother and baby.
If HIV-positive mother has chosen replacement feeding, feed accordingly.
Check ARV treatment needed G6
, G9 .
D12
MONITOR MOTHER EVERY 5 MINUTES:
For emergency signs, using rapid assessment (RAM) B3-B7 .
Feel if uterus is well contracted.
Mood and behaviour (distressed, anxious) D6
.
Time since third stage began (time since birth).
Record findings, treatments and procedures in Labour record and Partograph (pp.N4-N6).
Give Supportive care D6-D7 .
Never leave the woman alone.
DELIVER THE PLACENTA
Ensure 10-IU oxytocin IM is given D11 .
Await strong uterine contraction (2-3 minutes) and deliver placenta by controlled cord
traction:
Place side of one hand (usually left) above symphysis pubis with palm facing towards the
mothers umbilicus. This applies counter traction to the uterus during controlled cord traction. At
the same time, apply steady, sustained controlled cord traction.
If placenta does not descend during 30-40 seconds of controlled cord traction, release both cord
traction and counter traction on the abdomen and wait until the uterus is well contracted again.
Then repeat controlled cord traction with counter traction.
As the placenta is coming out, catch in both hands to prevent tearing of the membranes.
If the membranes do not slip out spontaneously, gently twist them into a rope and move them up
and down to assist separation without tearing them.
Check that placenta and membranes are complete.
MONITOR BABY EVERY 15 MINUTES:
Breathing: listen for grunting, look for chest in-drawing and fast breathing
J2 .
Warmth: check to see if feet are cold to touch
J2 .
TREAT AND ADVISE IF REQUIRED
If, after 30 minutes of giving oxytocin, the placenta is not delivered and the woman is NOT bleeding:
Empty bladder B12
Encourage breastfeeding
Repeat controlled cord traction.
If woman is bleeding, manage as on B5
If placenta is not delivered in another 30 minutes (1 hour after delivery):
Remove placenta manually B11
Give appropriate IM/IV antibiotic B15 .
If in 1 hour unable to remove placenta:
Refer the woman to hospital B17
Insert an IV line and give fluids with 20 IU of oxytocin at 30 drops per minute
during transfer B9 .
DO NOT exert excessive traction on the cord.
DO NOT squeeze or push the uterus to deliver the placenta.
If placenta is incomplete:
Remove placental fragments manually B11 .
Give appropriate IM/IV antibiotic B15 .
THIRD STAGE OF LABOUR: DELIVER THE PLACENTA
Use this chart for care of the woman between birth of the baby and delivery of placenta.
Third stage of labour: deliver the placenta
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
Third stage of labour: deliver the placenta
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D13
DELIVER THE PLACENTA
Check that uterus is well contracted and there is no heavy bleeding.
Repeat check every 5 minutes.
Examine perineum, lower vagina and vulva for tears.
Collect, estimate and record blood loss throughout third stage and immediately afterwards.
Clean the woman and the area beneath her. Put sanitary pad or folded clean cloth under her
buttocks to collect blood. Help her to change clothes if necessary.
Keep the mother and baby in delivery room for a minimum of one hour after delivery of placenta.
Dispose of placenta in the correct, safe and culturally appropriate manner.
TREAT AND ADVISE, IF REQUIRED
If heavy bleeding:
Massage uterus to expel clots if any, until it is hard B10 .
Give oxytocin 10 IU IM B10 .
Call for help.
Start an IV line B9 , add 20 IU of oxytocin to IV fluids and give at 60 drops per minute N9 .
Empty the bladder B12 .
If bleeding persists and uterus is soft:
Continue massaging uterus until it is hard.
Apply bimanual or aortic compression B10 .
Continue IV fluids with 20 IU of oxytocin at 30 drops per minute.
Refer woman urgently to hospital B17 .
If third degree tear (involving rectum or anus), refer urgently to hospital B17 .
For other tears: apply pressure over the tear with a sterile pad or gauze and put legs together.
Check after 5 minutes. If bleeding persists, repair the tear B12 .
If blood loss 250-ml, but bleeding has stopped:
Plan to keep the woman in the facility for 24 hours.
Monitor intensively (every 30 minutes) for 4 hours:
BP, pulse
vaginal bleeding
uterus, to make sure it is well contracted.
Assist the woman when she first walks after resting and recovering.
If not possible to observe at the facility, refer to hospital B17 .
If disposing placenta:
Use gloves when handling placenta.
Put placenta into a bag and place it into a leak-proof container.
Always carry placenta in a leak-proof container.
Incinerate the placenta or bury it at least 10 m away from a water source, in a 2 m deep pit.
NEXT: If prolapsed cord
RESPOND TO PROBLEMS DURING LABOUR AND DELIVERY
D14
Respond to problems during labour and delivery (1) If FHR <120 or >160 bpm
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
ASK, CHECK RECORD LOOK, LISTEN, FEEL
Position the woman on her left side.
If membranes have ruptured, look at
vulva for prolapsed cord.
See if liquor was meconium stained.
Repeat FHR count after
15 minutes.
SIGNS
Cord seen at vulva.
FHR remains >160 or <120 after 30
minutes observation.
FHR returns to normal.
TREAT AND ADVISE
Manage urgently as on D15 .
If early labour:
Refer the woman urgently to hospital B17
Keep her lying on her left side.
If late labour:
Call for help during delivery
Monitor after every contraction. If FHR does not
return to normal in 15 minutes explain to the
woman (and her companion) that the baby may
not be well.
Prepare for newborn resuscitation K11 .
Monitor FHR every 15 minutes.
CLASSIFY
PROLAPSED CORD
BABY NOT WELL
BABY WELL
IF FETAL HEART RATE (FHR) <120 OR >160 BEATS PER MINUTE
IF PROLAPSED CORD
The cord is visible outside the vagina or can be felt in the vagina below the presenting part.
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D15
Respond to problems during labour and delivery (2) If prolapsed cord
ASK, CHECK RECORD LOOK, LISTEN, FEEL
Look at or feel the cord gently for
pulsations.
Feel for transverse lie.
Do vaginal examination to
determine status of labour.
SIGNS
Transverse lie
Cord is pulsating
Cord is not pulsating
TREAT
Refer urgently to hospital B17 .
If early labour:
Push the head or presenting part out of the pelvis
and hold it above the brim/pelvis with your hand on
the abdomen until caesarean section is performed.
Instruct assistant (family, staff) to position the
womans buttocks higher than the shoulder.
Refer urgently to hospital B17 .
If transfer not possible, allow labour to continue.
If late labour:
Call for additional help if possible (for mother and baby).
Prepare for Newborn resuscitation K11 .
Ask the woman to assume an upright or squatting
position to help progress.
Expedite delivery by encouraging woman to push
with contraction.
Explain to the parents that baby may not be well.
CLASSIFY
OBSTRUCTED LABOUR
FETUS ALIVE
FETUS
PROBABLY DEAD
NEXT: If breech presentation
Respond to problems during labour and delivery (3) If breech presentation
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
SIGN
If early labour
If late labour
If the head does not deliver
after several contractions
If trapped arms or shoulders
If trapped head (and baby is dead)
NEXT: If stuck shoulders
IF BREECH PRESENTATION
D16
TREAT
Refer urgently to hospital B17 .
Call for additional help.
Confirm full dilatation of the cervix by vaginal examination D3 .
Ensure bladder is empty. If unable to empty bladder see Empty bladder B12 .
Prepare for newborn resuscitation K11 .
Deliver the baby:
Assist the woman into a position that will allow the baby to hang down during delivery, for example,
propped up with buttocks at edge of bed or onto her hands and knees (all fours position).
When buttocks are distending, make an episiotomy.
Allow buttocks, trunk and shoulders to deliver spontaneously during contractions.
After delivery of the shoulders allow the baby to hang until next contraction.
Place the baby astride your left forearm with limbs hanging on each side.
Place the middle and index fingers of the left hand over the malar cheek bones on either side to apply
gentle downwards pressure to aid flexion of head.
Keeping the left hand as described, place the index and ring fingers of the right hand over the babys
shoulders and the middle finger on the babys head to gently aid flexion until the hairline is visible.
When the hairline is visible, raise the baby in upward and forward direction towards the mothers abdomen until
the nose and mouth are free. The assistant gives supra pubic pressure during the period to maintain flexion.
Feel the babys chest for arms. If not felt:
Hold the baby gently with hands around each thigh and thumbs on sacrum.
Gently guiding the baby down, turn the baby, keeping the back uppermost until the shoulder which was
posterior (below) is now anterior (at the top) and the arm is released.
Then turn the baby back, again keeping the back uppermost to deliver the other arm.
Then proceed with delivery of head as described above.
Tie a 1 kg weight to the babys feet and await full dilatation.
Then proceed with delivery of head as described above.
NEVER pull on the breech
DO NOT allow the woman to push until the cervix is fully dilated. Pushing too soon may cause the head to be
trapped.
LOOK, LISTEN, FEEL
On external examination fetal head felt
in fundus.
Soft body part (leg or buttocks)
felt on vaginal examination.
Legs or buttocks presenting at
perineum.
Respond to problems during labour and delivery (4) If stuck shoulders
SIGN
Fetal head is delivered, but
shoulders are stuck and cannot be
delivered.
If the shoulders are still not
delivered and surgical help is not
available immediately.
TREAT
Call for additional help.
Prepare for newborn resuscitation.
Explain the problem to the woman and her companion.
Ask the woman to lie on her back while gripping her legs tightly flexed against her
chest, with knees wide apart. Ask the companion or other helper to keep the legs in
that position.
Perform an adequate episiotomy.
Ask an assistant to apply continuous pressure downwards, with the palm of the
hand on the abdomen directly above the pubic area, while you maintain continuous
downward traction on the fetal head.
Remain calm and explain to the woman that you need her cooperation to try
another position.
Assist her to adopt a kneeling on all fours position and ask her companion to
hold her steady - this simple change of position is sometimes sufficient to dislodge
the impacted shoulder and achieve delivery.
Introduce the right hand into the vagina along the posterior curve of the sacrum.
Attempt to deliver the posterior shoulder or arm using pressure from the finger of
the right hand to hook the posterior shoulder and arm downwards and forwards
through the vagina.
Complete the rest of delivery as normal.
If not successful, refer urgently to hospital B17 .
DO NOT pull excessively on the head.
NEXT: If multiple births
IF STUCK SHOULDERS (SHOULDER DYSTOCIA)
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D17
Respond to problems during labour and delivery (5) If multiple births
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
SIGN
Prepare for delivery
Second stage of labour
Third stage of labour
Immediate postpartum care
TREAT
Prepare delivery room and equipment for birth of 2 or more babies. Include:
more warm cloths
two sets of cord ties and razor blades
resuscitation equipment for 2 babies.
Arrange for a helper to assist you with the births and care of the babies.
Deliver the first baby following the usual procedure. Resuscitate if necessary. Label her/him Twin 1.
Ask helper to attend to the first baby.
Palpate uterus immediately to determine the lie of the second baby. If transverse or oblique lie, gently turn the baby by abdominal manipulation to head or breech presentation.
Check the presentation by vaginal examination. Check the fetal heart rate.
Await the return of strong contractions and spontaneous rupture of the second bag of membranes, usually within 1 hour of birth of first baby, but may be longer.
Stay with the woman and continue monitoring her and the fetal heart rate intensively.
Remove wet cloths from underneath her. If feeling chilled, cover her.
When the membranes rupture, perform vaginal examination D3
to check for prolapsed cord. If present, see Prolapsed cord D15 .
When strong contractions restart, ask the mother to bear down when she feels ready.
Deliver the second baby. Resuscitate if necessary. Label her/him Twin 2.
After cutting the cord, ask the helper to attend to the second baby.
Palpate the uterus for a third baby. If a third baby is felt, proceed as described above. If no third baby is felt, go to third stage of labour.
DO NOT attempt to deliver the placenta until all the babies are born.
DO NOT give the mother oxytocin until after the birth of all babies.
Give oxytocin 10 IU IM after making sure there is not another baby.
When the uterus is well contracted, deliver the placenta and membranes by controlled cord traction, applying traction to all cords together D12-D23.
Before and after delivery of the placenta and membranes, observe closely for vaginal bleeding because this woman is at greater risk of postpartum haemorrhage. If
bleeding, see B5 .
Examine the placenta and membranes for completeness. There may be one large placenta with 2 umbilical cords, or a separate placenta with an umbilical cord for each baby.
Monitor intensively as risk of bleeding is increased.
Provide immediate Postpartum care D19-D20.
In addition:
Keep mother in health centre for longer observation
Plan to measure haemoglobin postpartum if possible
Give special support for care and feeding of babies J11 and K4 .
NEXT: Care of the mother and newborn within first hour of delivery of placenta
IF MULTIPLE BIRTHS
D18
D19
MONITOR MOTHER EVERY 15 MINUTES:
For emergency signs, using rapid assessment (RAM) B3-B7 .
Feel if uterus is hard and round.
Record findings, treatments and procedures in Labour record and Partograph N4-N6 .
Keep mother and baby in delivery room - do not separate them.
Never leave the woman and newborn alone.
CARE OF MOTHER AND NEWBORN
WOMAN
Assess the amount of vaginal bleeding.
Encourage the woman to eat and drink.
Ask the companion to stay with the mother.
Encourage the woman to pass urine.
NEWBORN
Wipe the eyes.
Apply an antimicrobial within 1 hour of birth.
either 1% silver nitrate drops or 2.5% povidone iodine drops or 1% tetracycline ointment.
DO NOT wash away the eye antimicrobial.
If blood or meconium, wipe off with wet cloth and dry.
DO NOT remove vernix or bathe the baby.
Continue keeping the baby warm and in skin-to-skin contact with the mother.
Encourage the mother to initiate breastfeeding when baby shows signs of readiness. Offer her help.
DO NOT give artificial teats or pre-lacteal feeds to the newborn: no water, sugar water, or local feeds.
Examine the mother and newborn one hour after delivery of placenta.
Use Assess the mother after delivery D21 and Examine the newborn J2-J8 .
MONITOR BABY EVERY 15 MINUTES:
Breathing: listen for grunting, look for chest in-drawing and fast breathing
J2 .
Warmth: check to see if feet are cold to touch
J2 .
INTERVENTIONS, IF REQUIRED
If pad soaked in less than 5 minutes, or constant trickle of blood, manage as on D22 ..
If uterus soft, manage as on B10 .
If bleeding from a perineal tear, repair if required B12 or refer to hospital B17 .
If breathing with difficulty grunting, chest in-drawing or fast breathing, examine the baby as on J2-J8 .
If feet are cold to touch or mother and baby are separated:
Ensure the room is warm. Cover mother and baby with a blanket
Reassess in 1 hour. If still cold, measure temperature. If less than 36.5
0
C, manage as on K9 .
If unable to initiate breastfeeding (mother has complications):
Plan for alternative feeding method K5-K6 .
If mother HIV-positive: give treatment to the newborn G9 .
Support the mother's choice of newborn feeding G8 .
If baby is stillborn or dead, give supportive care to mother and her family D24 .
Refer to hospital now if woman had serious complications at admission or during delivery but was
in late labour.
CARE OF THE MOTHER AND NEWBORN WITHIN FIRST HOUR OF DELIVERY OF PLACENTA
Use this chart for woman and newborn during the first hour after complete delivery of placenta.
Care of the mother and newborn within first hour of delivery of placenta
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D20
MONITOR MOTHER AT 2, 3 AND 4 HOURS,
THEN EVERY 4 HOURS:
For emergency signs, using rapid assessment (RAM).
Feel uterus if hard and round.
Record findings, treatments and procedures in Labour record and Partograph N4-N6 .
Keep the mother and baby together.
Never leave the woman and newborn alone.
DO NOT discharge before 12 hours.
CARE OF MOTHER
Accompany the mother and baby to ward.
Advise on Postpartum care and hygiene D26 .
Ensure the mother has sanitary napkins or clean material to collect vaginal blood.
Encourage the mother to eat, drink and rest.
Ensure the room is warm (25C).
Ask the mothers companion to watch her and call for help if bleeding or pain increases, if mother
feels dizzy or has severe headaches, visual disturbance or epigastric distress.
Encourage the mother to empty her bladder and ensure that she has
passed urine.
Check record and give any treatment or prophylaxis which is due.
Advise the mother on postpartum care and nutrition D26 .
Advise when to seek care D28 .
Counsel on birth spacing and other family planning methods D27 .
Repeat examination of the mother before discharge using Assess the mother after delivery D21 . For
baby, see J2-J8 .
INTERVENTIONS, IF REQUIRED
Make sure the woman has someone with her and they know when to call for help.
If HIV-positive: give her appropriate treatment G6
, G9 .
If heavy vaginal bleeding, palpate the uterus.
If uterus not firm, massage the fundus to make it contract and expel any clots B6 .
If pad is soaked in less than 5 minutes, manage as on B5 .
If bleeding is from perineal tear, repair or refer to hospital B17 .
If the mother cannot pass urine or the bladder is full (swelling over lower abdomen) and she is
uncomfortable, help her by gently pouring water on vulva.
DO NOT catheterize unless you have to.
If tubal ligation or IUD desired, make plans before discharge.
If mother is on antibiotics because of rupture of membranes >18 hours but shows no signs of
infection now, discontinue antibiotics.
CARE OF THE MOTHER ONE HOUR AFTER DELIVERY OF PLACENTA
Use this chart for continuous care of the mother until discharge. See J10 for care of the baby.
Care of the mother one hour after delivery of placenta
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
ASSESS THE MOTHER AFTER DELIVERY
Use this chart to examine the mother the first time after delivery (at 1 hour after delivery or later) and for discharge.
For examining the newborn use the chart on J2-J8 .
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D21
Assess the mother after delivery
ASK, CHECK RECORD
Check record:
bleeding more than 250 ml?
completeness of placenta and
membranes?
complications during delivery or
postpartum?
special treatment needs?
needs tubal ligation or IUD?
How are you feeling?
Do you have any pains?
Do you have any concerns?
How is your baby?
How do your breasts feel?
LOOK, LISTEN, FEEL
Measure temperature.
Feel the uterus. Is it hard and
round?
Look for vaginal bleeding
Look at perineum.
Is there a tear or cut?
Is it red, swollen or draining pus?
Look for conjunctival pallor.
Look for palmar pallor.
SIGNS
Uterus hard.
Little bleeding.
No perineal problem.
No pallor.
No fever.
Blood pressure normal.
Pulse normal.
TREAT AND ADVISE
Keep the mother at the facility for 12 hours after
delivery.
Ensure preventive measures D25 .
Advise on postpartum care and hygiene D26 .
Counsel on nutrition D26 .
Counsel on birth spacing and family planning D27 .
Advise on when to seek care and next routine
postpartum visit D28 .
Reassess for discharge D21 .
Continue any treatments initiated earlier.
If tubal ligation desired, refer to hospital within 7
days of delivery. If IUD desired, refer to appropriate
services within 48 hours.
CLASSIFY
MOTHER WELL
NEXT: Respond to problems immediately postpartum
If no problems, go to page D25 .
Respond to problems immediately postpartum (1)
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
ASK, CHECK RECORD
Time since rupture of membranes
Abdominal pain
Chills
LOOK, LISTEN, FEEL
A pad is soaked in less than 5
minutes.
Repeat temperature measurement
after 2 hours
If temperature is still >38C
Look for abnormal vaginal
discharge.
Listen to fetal heart rate
feel lower abdomen for
tenderness
Is there bleeding from the tear or
episiotomy
Does it extend to anus or rectum?
SIGNS
More than 1 pad soaked in
5 minutes
Uterus not hard and not round
Temperature still >38
0
C and any of:
Chills
Foul-smelling vaginal discharge
Low abdomen tenderness
FHR remains >160 after 30
minutes of observation
rupture of membranes >18 hours
Temperature still >38
0
C
Tear extending to anus or rectum.
Perineal tear
Episiotomy
TREAT AND ADVISE
See B5 for treatment.
Refer urgently to hospital B17 .
Insert an IV line and give fluids rapidly B9 .
Give appropriate IM/IV antibiotics B15 .
If baby and placenta delivered:
Give oxytocin 10 IU IM B10 .
Refer woman urgently to hospital B17 .
Assess the newborn J2-J8 .
Treat if any sign of infection.
Encourage woman to drink plenty of fluids.
Measure temperature every 4 hours.
If temperature persists for >12 hours, is very high or
rises rapidly, give appropriate antibiotic and
refer to hospital B15 .
Refer woman urgently to hospital B15 .
If bleeding persists, repair the tear or episiotomy B12
.
CLASSIFY
HEAVY
BLEEDING
UTERINE AND
FETAL INFECTION
RISK OF UTERINE AND
FETAL INFECTION
THIRD DEGREE TEAR
SMALL PERINEAL TEAR
NEXT: If elevated diastolic blood pressure
IF VAGINAL BLEEDING
IF FEVER (TEMPERATURE >38C)
IF PERINEAL TEAR OR EPISIOTOMY (DONE FOR LIFESAVING CIRCUMSTANCES)
D22
IF ELEVATED DIASTOLIC BLOOD PRESSURE
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D23
Respond to problems immediately postpartum (2)
ASK, CHECK RECORD LOOK, LISTEN, FEEL
If diastolic blood pressure is
90 mmHg, repeat after 1 hour rest.
If diastolic blood pressure is still
90-mmHg, ask the woman if she
has:
severe headache
blurred vision
epigastric pain and
check protein in urine.
SIGNS
Diastolic blood pressure
110 mmHg OR
Diastolic blood pressure 90 mmHg
and 2+ proteinuria and any of:
severe headache
blurred vision
epigastric pain.
Diastolic blood pressure 90-110
mmHg on two readings.
2+ proteinuria (on admission).
Diastolic blood pressure
90 mmHg on 2 readings.
TREAT AND ADVISE
Give magnesium sulphate B13 .
If in early labour or postpartum,
refer urgently to hospital B17 .
If late labour:
continue magnesium sulphate treatment B13
monitor blood pressure every hour.
DO NOT give ergometrine after delivery.
Refer urgently to hospital after delivery B17 .
If early labour, refer urgently to hospital E17 .
If late labour:
monitor blood pressure every hour
DO NOT give ergometrine after delivery.
If BP remains elevated after delivery,
refer to hospital E17 .
Monitor blood pressure every hour.
DO NOT give ergometrine after delivery.
If blood pressure remains elevated after delivery,
refer woman to hospital E17 .
CLASSIFY
SEVERE
PRE-ECLAMPSIA
PRE-ECLAMPSIA
HYPERTENSION
NEXT: If pallor on screening, check for anaemia
Respond to problems immediately postpartum (3)
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
ASK, CHECK RECORD
Bleeding during labour, delivery or
postpartum.
LOOK, LISTEN, FEEL
Measure haemoglobin, if possible.
Look for conjunctival pallor.
Look for palmar pallor. If pallor:
Is it severe pallor?
Some pallor?
Count number of breaths in
1-minute
SIGNS
Haemoglobin <7 g/dl.
AND/OR
Severe palmar and conjunctival pallor or
Any pallor with >30 breaths per minute.
Any bleeding.
Haemoglobin 7-11-g/dl.
Palmar or conjunctival pallor.
Haemoglobin >11-g/dl
No pallor.
CLASSIFY
SEVERE
ANAEMIA
MODERATE
ANAEMIA
NO ANAEMIA
NEXT: Give preventive measures
IF PALLOR ON SCREENING, CHECK FOR ANAEMIA
IF MOTHER SEVERELY ILL OR SEPARATED FROM THE BABY
IF BABY STILLBORN OR DEAD
D24
TREAT AND ADVISE
If early labour or postpartum, refer urgently to hospital B17 .
If late labour:
monitor intensively
minimize blood loss
refer urgently to hospital after delivery B17 .
DO NOT discharge before 24 hours.
Check haemoglobin after 3 days.
Give double dose of iron for 3 months F3 .
Follow up in 4 weeks.
Give iron/folate for 3 months F3 .
Teach mother to express breast milk every 3 hours K5 .
Help her to express breast milk if necessary. Ensure baby
receives mothers milk K8 .
Help her to establish or re-establish breastfeeding as soon as
possible. See K2-K3 .
Give supportive care:
Inform the parents as soon as possible after the babys
death.
Show the baby to the mother, give the baby to the mother to
hold, where culturally appropriate.
Offer the parents and family to be with the dead baby in
privacy as long as they need.
Discuss with them the events before the death and the
possible causes of death.
Advise the mother on breast care K8 .
Counsel on appropriate family planning method D27 .
D25
ASSESS, CHECK RECORDS
Check RPR status in records.
If no RPR during this pregnancy, do the RPR test L5 .
Check tetanus toxoid (TT) immunization status.
Check when last dose of mebendazole was given.
Check womans supply of prescribed dose of iron/folate.
Check if vitamin A given.
Ask whether woman and baby are sleeping under insecticide treated bednet.
Counsel and advise all women.
Record all treatments given N6 .
Check HIV status in records.
TREAT AND ADVISE
If RPR positive:
Treat woman and the partner with benzathine penicillin F6 .
Treat the newborn K12 .
Give tetanus toxoid if due F2 .
Give mebendazole once in 6 months F3 .
Give 3 months supply of iron and counsel on compliance F3 .
Give vitamin A if due F2 .
Encourage sleeping under insecticide treated bednet F4 .
Advise on postpartum care D26 .
Counsel on nutrition D26 .
Counsel on birth spacing and family planning D27 .
Counsel on breastfeeding K2 .
Counsel on safer sex including use of condoms G2 .
Advise on routine and follow-up postpartum visits D28 .
Advise on danger signs D28 .
Discuss how to prepare for an emergency in postpartum D28 .
If HIV-positive:
Support adherence to ARV G6 .
Treat the newborn G9 .
If HIV test not done, offer her the test E5 .
GIVE PREVENTIVE MEASURES
Ensure that all are given before discharge.
Give preventive measures
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D26
Advise on postpartum care and hygiene
Advise and explain to the woman:
To always have someone near her for the first 24 hours to respond to any change in her condition.
Not to insert anything into the vagina.
To have enough rest and sleep.
The importance of washing to prevent infection of the mother and her baby:
wash hands before handling baby
wash perineum daily and after faecal excretion
change perineal pads every 4 to 6 hours, or more frequently if heavy lochia
wash used pads or dispose of them safely
wash the body daily.
To avoid sexual intercourse until the perineal wound heals.
Counsel on nutrition
Advise the woman to eat a greater amount and variety of healthy foods, such as meat, fish, oils,
nuts, seeds, cereals, beans, vegetables, cheese, milk, to help her feel well and strong (give examples
of types of food and how much to eat).
Reassure the mother that she can eat any normal foods these will not harm the breastfeeding baby.
Spend more time on nutrition counselling with very thin women and adolescents.
Determine if there are important taboos about foods which are nutritionally healthy.
Advise the woman against these taboos.
Talk to family members such as partner and mother-in-law, to encourage them to help ensure the
woman eats enough and avoids hard physical work.
ADVISE ON POSTPARTUM CARE
Advise on postpartum care
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D27
Counsel on the importance of family planning
If appropriate, ask the woman if she would like her partner or another family member to be included
in the counselling session.
Explain that after birth, if she has sex and is not exclusively breastfeeding, she can become pregnant
as soon as 4 weeks after delivery. Therefore it is important to start thinking early about what family
planning method they will use.
Ask about plans for having more children. If she (and her partner) want more children, advise that
waiting at least 2 years before trying to become pregnant again is good for the mother and for the
baby's health.
Information on when to start a method after delivery will vary depending on whether a woman is
breastfeeding or not.
Make arrangements for the woman to see a family planning counsellor, or counsel her directly
(see the Decision-making tool for family planning providers and clients for information on
methods and on the counselling process).
Councel on safer sex including use of condoms for dual protection from sexually transmitted infection (STI) or
HIV and pregnancy. Promote their use, especially if at risk for sexually transmitted infection (STI) or HIV G2 .
For HIV-positive women, see G4 for family planning considerations
Her partner can decide to have a vasectomy (male sterilization) at any time.
Method options for the non-breastfeeding woman
Can be used immediately postpartum Condoms
Progestogen-only oral contraceptives
Progestogen-only injectables
Implant
Spermicide
Female sterilization (within 7 days or delay 6 weeks)
Copper IUD (immediately following expulsion of
placenta or within 48 hours)
Delay 3 weeks Combined oral contraceptives
Combined injectables
Fertility awareness methods
Lactational amenorrhoea method (LAM)
A breastfeeding woman is protected from pregnancy only if:
she is no more than 6 months postpartum, and
she is breastfeeding exclusively (8 or more times a day, including at least once at night: no
daytime feedings more than 4 hours apart and no night feedings more than 6 hours apart; no
complementary foods or fluids), and
her menstrual cycle has not returned.
A breastfeeding woman can also choose any other family planning method, either to use alone or
together with LAM.
Method options for the breastfeeding woman
Can be used immediately postpartum Lactational amenorrhoea method (LAM)
Condoms
Spermicide
Female sterilisation (within 7 days or delay 6 weeks)
Copper IUD (within 48 hours or delay 4 weeks)
Delay 6 weeks Progestogen-only oral contraceptives
Progestogen-only injectables
Implants
Diaphragm
Delay 6 months Combined oral contraceptives
Combined injectables
Fertility awareness methods
COUNSEL ON BIRTH SPACING AND FAMILY PLANNING
Counsel on birth spacing and family planning
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D28
Routine postpartum care visits
FIRST VISIT D19 Within the first week, preferably within 2-3 days
SECOND VISIT E2
4-6 weeks
Follow-up visits for problems
If the problem was: Return in:
Fever 2 days
Lower urinary tract infection 2 days
Perineal infection or pain 2 days
Hypertension 1 week
Urinary incontinence 1 week
Severe anaemia 2 weeks
Postpartum blues 2 weeks
HIV-positive 2 weeks
Moderate anaemia 4 weeks
If treated in hospital According to hospital instructions or according to national
for any complication guidelines, but no later than in 2 weeks.
Advise on danger signs
Advise to go to a hospital or health centre immediately, day or night, WITHOUT WAITING, if any of
the following signs:
vaginal bleeding:
more than 2 or 3 pads soaked in 20-30 minutes after delivery OR
bleeding increases rather than decreases after delivery.
convulsions.
fast or difficult breathing.
fever and too weak to get out of bed.
severe abdominal pain.
Go to health centre as soon as possible if any of the following signs:
fever
abdominal pain
feels ill
breasts swollen, red or tender breasts, or sore nipple
urine dribbling or pain on micturition
pain in the perineum or draining pus
foul-smelling lochia
Discuss how to prepare for an emergency in postpartum
Advise to always have someone near for at least 24 hours after delivery to respond to any change in
condition.
Discuss with woman and her partner and family about emergency issues:
where to go if danger signs
how to reach the hospital
costs involved
family and community support.
Advise the woman to ask for help from the community, if needed I1-I3.
Advise the woman to bring her home-based maternal record to the health centre, even for an
emergency visit.
ADVISE ON WHEN TO RETURN
Use this chart for advising on postpartum care on D21 or E2 . For newborn babies see the schedule on K14 .
Encourage woman to bring her partner or family member to at least one visit.
Advise on when to return
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
D29
Preparation for home delivery
Check emergency arrangements.
Keep emergency transport arrangements up-to-date.
Carry with you all essential drugs B17 , records, and the delivery kit.
Ensure that the family prepares, as on C18 .
Delivery care
Follow the labour and delivery procedures D2-D28 K11 .
Observe universal precautions A4 .
Give Supportive care. Involve the companion in care and support D6-D7
.
Maintain the partograph and labour record N4-N6 .
Provide newborn care J2-J8 .
Refer to facility as soon as possible if any abnormal finding in mother or baby B17 K14 .
Immediate postpartum care of mother
Stay with the woman for first two hours after delivery of placenta C2 C13-C14.
Examine the mother before leaving her D21 .
Advise on postpartum care, nutrition and family planning D26-D27.
Ensure that someone will stay with the mother for the first 24 hours.
Postpartum care of newborn
Stay until baby has had the first breastfeed and help the mother good positioning and attachment K3 .
Advise on breastfeeding and breast care K2-K3 .
Examine the baby before leaving N2-N8 .
Immunize the baby if possible K13 .
Advise on newborn care K10 .
Advise the family about danger signs and when and where to seek care K14 .
If possible, return within a day to check the mother and baby.
Advise a postpartum visit for the mother and baby within the first week K14 .
HOME DELIVERY BY SKILLED ATTENDANT
Use these instructions if you are attending delivery at home.
Home delivery by skilled attendant
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
I
M
M
E
D
I
A
T
E
P
O
S
T
P
A
R
T
U
M
C
A
R
E
Postpartum care
C
H
I
L
D
B
I
R
T
H
:
L
A
B
O
U
R
,
D
E
L
I
V
E
R
Y
A
N
D
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E1
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E1
POSTPARTUM CARE
PO
STPARTU
M
CAREE2 Postpartumcare
ASK, CHECK RECORD
Wh en and w here did y ou deliv er? How are y ou feeling? Haveyouhad any pain or fe veror bleeding since deliv ery? Doyou ha veanyproblem with passing urine? Haveyoudecided on an y contraception? How do y our breasts feel? Doyou ha veanyother concer ns? Check records: Any complications during deliver y? Receiving an y treatments? HI V status.
LOOK, LISTEN, FEEL
Measure blood pressure an d temperature. Feel uter us.Is it hard and round? Look at vulv a and perineum for: tear swelling pus. Look at pad for bleeding an d lochia. Does it smell? Isitpr ofuse? Look for pallor .
SIGNS
Mother feeling w ell. Di d not bleed >250 ml. Ut eruswel l contracted and hard. Noperineal s wel ling. Bl ood pressure, pulse and temperature nor mal. Nopallor. Nobreast problem, is breastfeeding w ell. Nofeverorpain or concer n. Nopr oblem with urination.
TREAT AND AD VISE
Makesure w oman and family kno w what to watch for and w hen to seek care D28. Advise on P ostpartum care and h ygiene, and couns el on nutrition D26. Counsel on the impor tanceof bir th spacing and family planning D27. Refer for family planning couns elling. Di spense3 months ironsupply and counsel on compliance F3. Gi veanytreatmen t or proph ylaxis due: tetanus immunization if she has not had full course F2. Pr omote use of impregnated bednet for the mother and bab y. Record on the mother s home-b ased mater nal record. Advise to retur n to health centre within 4-6 week s.
CLASSIFY
NORMAL POSTP ARTUM
NEXT : Respond to obser vedsigns or v olunteered problems
POSTP ARTUM EXAMINA TION OF THE MO THER (UP TO6 WEEKS)
Use this char t for examining the mother after discharg e from a facility or after home deliver y
If she delivered less than a week ag o without a skilled attendant, use the char t Assess the mother after deliver yD21.
Toexamine the bab y seeJ2-J8.
If breast problem see J9 .
NEXT : If pallor , check for anaemia
Respond to obser ved signs or volunteered pr oblems (1) Ifel evated diastolic blood pressure
PO
STPARTU
M
CARE
E3
ASK, CHECK RECORD
Hi story of pre-eclampsia or eclampsia in pregnancy , deliver y or after deliv ery?
LOOK, LISTEN, FEEL
Ifdi astolic blood pressure is 90 mmHg , repeat after a 1 hour rest.
SIGNS
Di astolic blood pressure 110 mmHg .
Di astolic blood pressure 90 mmHg on 2 readings.
Di astolic blood pressure <90 mmHg after 2 readings.
TREAT AND AD VISE
Gi veappropria te antih ypertensiv e B14. Refer urg ently to hospita l B17.
Reassessin1 week. If hypertension persists, refe r to ho spital.
Noadditional treatment.
CLASSIFY
SEVERE HYPERTENSION
MODERATE HYPERTENSION
BLOOD PRESSURE NORMAL
RESPOND T O OBSER VED SIGNS OR VOL UNTEERED PR OBLEMS
IF ELEV ATE D DIAST OLIC BLOOD PRESSURE
PO
STPARTU
M
CAREE4 Respond to obser ved signs or volunteered problems (2) Ifpallor, check for anaemia
ASK, CHECK RECORD
Check record for bleeding in pregnancy, deliver y or postpar tum. Haveyouhad hea vy bleeding since deliver y? Doyou tire easily? Ar e you breathless (shor t of breath) during routine house wor k?
LOOK, LISTEN, FEEL
Measure haemoglobin if history of bleeding. Look for conjunctiv al pallor . Look for palmar pallor . Ifpallor: isitsever e pallor? some pallor? Count number of breaths in 1 minute.
SIGNS
Haemoglobin <7-g/dl AND/OR Sever e palmar and conj unctival pallor or Any pallor and an y of: >30 breaths per min ute ti res easily breathlessness at rest.
Haemoglobin 7-11-g/dl OR Palmar or conjunctiv al pallor .
Haemoglobin >11-g/dl. Nopallor.
TREAT AND AD VISE
Gi vedouble dose of iron (1tablet60 mg twice daily for 3 months) F3. Refer urg ently to hospita l B17. Followup in 2 w eeks to check cli nical prog ress and compliance wi th treatment.
Gi vedouble dose of iron for 3 months F3. Reassessatnext postnatal visit (in 4 w eeks). If anaem ia persists, refer to hospital.
Continue trea tment with iron for 3 months altog etherF3.
CLASSIFY
SEVERE ANAEMIA
MODERATE ANAEMIA
NO ANAEMIA
NEXT : Check for HIV status
IF PALLOR, CHECK FOR ANAEMIA
Respond to obser ved signs or volunteered problems (3) Check for HIV status
PO
STPARTU
M
CARE
E5
ASK, CHECK RECORD
Provide k ey infor mation on HIV G2. Wh at is HIV and ho w is HIV transmitted G2?
Advantageof kno wing the HIV status G2. Explain about HIV testing and counselling including confidentiality of the result G3. Ask the woman: Haveyoubeen tested for HIV? If not: tell her that she will be tested for HIV , unless she refuses. If y es: check result. (Explain to her that she has a right not to disclose the result.) Are y ou taking an y AR V treatment? Check treatment plan. Has the par tner been tested?
LOOK, LISTEN, FEEL
Perfor m the Rapid HIV test ifnot perfor med in this pregnanc y L6.
SIGNS
PositiveHIV test
Negat iveHIV test
She refuses the tes t or is not willin g to disclose the result of pre vious test or no test results a vai lable
TREAT AND AD VISE
Counsel on implications of a positiv e testG3. Refer the w oman to HIV ser vices for fur ther assess ment. Counsel on infant feeding options G7. Provide additional care for HIV-positiv e womanG4. Counsel on family planning G4. Counsel on safer sex including use of condoms G2. Counsel on benefits of disclosure (in vol ving) and testing her par tneG3. Provide support to the HIV-positiv e womanG5. Followup in 2 w eeks.
Counsel on implications of a neg ativetestG3. Counsel on the impor tanceof sta ying neg ativeby practisi ng safer sex,includin g use of condoms G2. Counsel on benefits of in vol ving and testi ng the partner G3.
Counsel on safer sex including use of condoms G2. Counsel on benefits of in vol ving and testi ng the partner G3.
CLASSIFY
HIV-POSITI VE
HIV-NEGATIVE
UNKNOWN HIV ST ATUS
NEXT : If hea vy v aginal bleeding
CHECK FOR HIV ST ATUS
Use this char t for HIV testing and counselling during postpar tum visit if the woman is not previously tested. Ifthe women has tak en AR V during pregnancy or childbir th refer her to HI V ser vices for fur ther assessment.
IF HEA VY V AGI NAL BLEEDING
Respond to obser ved signs or volunteered problems (4)
PO
STPARTU
M
CAREE6
ASK, CHECK RECORD
Haveyouhad: heavybl eeding? foul-smelling lochia? burni ng on urination?
LOOK, LISTEN, FEEL
Feel lowerabdomen and flanks for tenderness. Look for abnor mal lochia. Measure temperature. Look or feel for stiff neck . Look for letharg y.
SIGNS
More than 1 pad soak ed in 5 minutes.
Temperature >38C and an y of: veryweak abdominal tender ness foul-smelling lochia pr ofuse lochia ut erusnot w ell contracted lowerabdominal pain hi story of hea vy v aginal bleeding .
Fever>38C and an y of: burni ng on urination fl ank pain.
Burni ng on urination.
Temperature >38C and an y of: stiff neck lethargy .
Fever>38C.
TREAT AND AD VISE
Gi ve0.2 mg erg ometrine IMB10. Gi veappropria te IM/IV antibiotics B15. Manageas in Rapid assessment and manag ementB3-B7. Refer urg ently to hospita l B17.
Insertan IV line and giv e fluids rapidly B9. Gi veappropria te IM/IV antibiotics B15. Refer urg ently to hospita l B17.
Gi veappropria te IM/IV antibiotics B15. Refer urg ently to hospita l B17.
Gi veappropria te oral antibiotic F5. Encourag e her to drink more fluids. Followup in 2 da ys. If no impr ovement, refer to hospital.
Insertan IV line B9. Gi veappropria te IM/IV antibiotics B15. Gi veartemet her IM (or quinine IM if ar temether not available) and glucose B16. Refer urg ently to hospita l B17.
Gi veoral antimalarial F4. Followup in 2 da ys. If no impr ovement, refer to hospital.
CLASSIFY
POSTP ARTUM BLEEDING
UTERINE INFECTION
UPPER URINAR Y TRA CT INFECTION
LOWER URINAR Y TRA CT INFECTION
VERYSEVERE FEBRILE DISEASE
MALARIA
NEXT : If dribbling urine
IF FEVER OR FOUL-SMELLING LOCHIA
Respond to obser ved signs or volunteered problems (5)
PO
STPARTU
M
CARE
E7
ASK, CHECK RECORD
How ha veyoubeen feeling recently? Haveyoubeen in lo w spirits? Haveyoubeen able to enjo y the things y ou usually enjo y? Haveyouhad your usual le velof energy , or ha veyoubeen feeling tired? How has y our sleep been? Haveyoubeen able to concentrate (for example on ne wspaper articles or y our fa vourite radio programmes)?
LOOK, LISTEN, FEEL SIGNS
Dr ibbling or leaking urine.
Excessive swelling of vulv a or perineum.
Pus in perineum. Pain in perineum.
Twoormore of the follo wing symptoms during the same 2 w eek period representing a chang e from nor mal: Inappropriate guilt or neg ative feeling to wards self. Cr ies easily . Decreased interest or pleasure. Feels tired, agitated all the time. Di sturbed sleep (sleeping too much or too little, waking ear ly). Di minished ability to think or concentrate. Markedloss of appetite.
Any of the abo ve, for less than 2 w eeks.
TREAT
Check peri neal trauma. Gi veappropria te oral antibiotics for lo werur inary tract infection F5. Ifconditions persists more than 1 w eek, refer the woman to hospital.
Refer the w oman to hospital.
Remov e sutures, ifpr esent. Cl ean wound. Counsel on care and h ygiene D26. Gi veparacetamo l for pain F4. Followup in 2 da ys.If no impro vement, refe r to ho spital.
Pr ovi de emotional suppor t. Refer urg ently the woman to hosp ital B7.
Assure the w oman that this is v erycommon. Li sten to her concer ns.Giveemotional encourag ement and suppor t. Counsel partner and family to pro vide assistance to the w oman. Followup in 2 w eeks, and refer if no impro vement.
CLASSIFY
URINAR Y INCONTINEN CE
PERINEAL TRAUMA
PERINEAL INFECTION ORPAIN
POSTP ARTUM DEPRESSION (USUALL Y AFTER FIRST WEEK)
POSTP ARTUM BLUES (USUALL Y IN FIRST WEEK)
NEXT : If v aginal discharg e 4 weeks after deliv ery
IF DRIBBLING URINE
IF PUS OR PERINEAL P AIN
IF FEELING UNHAPPY OR CR YING EASIL Y
E2 POSTPARTUM EXAMINATION OF
THE MOTHER (UP TO 6 WEEKS)
E3 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (1)
If elevated diastolic pressure
E4 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (2)
If pallor, check for anaemia
E5 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (3)
Check for HIV status
E6 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (4)
If heavy vaginal bleeding
If fever or foul-smelling lochia
E7 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (5)
If dribbling urine
If puss or perineal pain
If feeling unhappy or crying easily
Respond to obser ved signs or volunteered problems (6)
PO
STPARTU
M
CAREE8
NEXT : If cough or breathing difficulty
ASK, CHECK RECORD
Doyou ha veitching at the vulv a? Has your par tner had a urinar y problem?
If par tner is present in the clinic, ask the w oman if she feels comfor table if youask him similar questions. If y es,ask him if he has: ur ethral discharg e or pus burni ng on passing urine.
If par tner could not be approached, explain impor tance of par tner assessment and treatment to a voi d reinfection.
LOOK, LISTEN, FEEL
Separate the labia and loo k for abnormal vaginal discharg e: amount colour odour/smell. Ifnodi scharge is seen, examine with a glo vedfi nger and look at the discharge on the glo ve.
SIGNS
Abnormal vaginal discharg e,and partner has urethral disch argeor burning on passing urine.
Curd-like vaginal discharg e and/or Intense vulv al itching .
Abnormal vaginal discharg e.
TREAT AND AD VISE
Gi veappropria te oral antibiotics to w omanF5. Tr eat par tner with appropriate oral antibiotics F5. Counsel on safer sex including use of condoms G2.
Gi veclotrima zoleF5. Counsel on safer sex including use of condoms F4. Ifnoimprov ement, refer the w oman to hospital.
Gi vemetronida zole to w omanF5. Counsel on safer sex including use of condoms G2.
CLASSIFY
POSSIBLE GONORRHOEA OR CHLAMYDIA INFECTION
POSSIBLE CANDID A INFECTION
POSSIBLE BACTERIA L OR TRICHOMO NAS INFECTION
IF VAGI NAL DISCHARGE 4 WEEKS AFTER DELIVERY
IF BREAST PR OBLEM
See J9 .
Respond to obser ved signs or volunteere d problems (7)
PO
STPARTU
M
CARE
E9
NEXT : If signs sugg esting HIV infection
ASK, CHECK RECORD
How long ha veyoubeen coughing? How long ha veyouhad difficulty in breathing? Doyou ha vechest pain? Doyou ha veanyblood in sputum? Doyou smok e?
Ar e you taking anti-tuberculosis drugs? If y es,since w hen?
LOOK, LISTEN, FEEL
Look for breathlessness. Li sten for w heezing. Measure temperature.
SIGNS
At least 2 of the follo wing: Temperature >38C. Breathlessness. Chest pain.
At least 1 of the follo wing: Cough or breathing diffic ulty for >3 weeks. Bl ood in sputum. Wh eezing.
Temperature <38C. Cough for <3 w eeks.
Taking anti-tuberculo sis dr ugs.
TREAT AND AD VISE
Gi vefirst dose of appropriate I M/IVantibiotics B15. Refer urg ently to hospita l B17.
Refer to hospital for assessment. Ifsever e wheezing, refer urg ently to hospital. UsePractical Approach to Lung healthguidelines (PAL) for fur ther manag ement.
Advise safe, soothing remed y. Ifsmoking, counsel to stop smoking.
Assure the w oman that the dr ugs are not har mful to her bab y,and of the need to cont inue treatment. Ifher sput umis TB-positiv e within 2 months of deliv ery , plan to giv e INH proph ylaxis to the ne wbornK13. Reinforce ad vice for HIV testing G3. Ifsmoking, counsel to stop smoking. Advise to screen immed iate family members and closecontacts for tuberculosis.
CLASSIFY
POSSIBLE PNEUMON IA
POSSIBLE CHR ONIC LUNG DISEASE
UPPER RESPIRA TORY TRACT INFECTION
TUBERCULOSIS
IF COUGH OR BREA THING DIFFICUL TY
IF TAKING ANTI- TUBERCULOSIS DR UGS
Respond to obser ved signs or volunteered problems (8) Ifsi gns suggesting HIV inf ection
PO
STPARTU
M
CAREE10
ASK, CHECK RECORD
Haveyoulost weight? Doyou ha vefever? Howlong (>1 month)? Haveyougot diar rhoea (continuous or inter mittent)? Howlong (>1 month)? Haveyouhad cough? Howlong (>1 month)?
LOOK, LISTEN, FEEL
Look for visible wasting . Look for ulcers and w hite patches in the mouth (thr ush). Look at the skin: Isthere a rash? Ar e there blisters along the ribs on one side of the bod y?
SIGNS
Two of the follo wing: weight loss fever>1month di arr hoea >1 month. OR One of the abo vesigns and one or more other si gn or from a high-risk g roup.
TREAT AND AD VISE
Reinforce the need to kno w HIV s tatus and c ounsel for HIV testing G3. Counsel on the benefits of testing her par tnerG3. Counsel on safer sex including use of condoms G2. Examine fur ther and manag e according to national HIV guidelines or refer to appropriate HIV ser vices. Refer to TB centre if cough.
CLASSIFY
STRONG LIKELIHOO D OF HIV INFECTION
IF SIGNS SUGGESTING HIV INFECTION
HIV status unknown or known HIV-positive.
E8 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (6)
If vaginal discharge 4 weeks after delivery
If breast problem
J9
E9 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (7)
If cough or breathing difficulty
If taking anti-tuberculosis drugs
E10 RESPOND TO OBSERVED SIGNS OR
VOLUNTEERED PROBLEMS (8)
If signs suggesting HIV infection
Always begin with Rapid assessment and management (RAM)
B2-B7 .
Next use the Postpartum examination of the mother
E2 .
If an abnormal sign is identified (volunteered or observed), use the charts Respond to observed signs or volunteered problems
E3-E10 .
Record all treatment given, positive findings, and the scheduled next visit in the home-based and clinic recording form.
For the first or second postpartum visit during the first week after delivery, use the Postpartum examination chart
D21 and Advise and
counselling section
D26 to examine and advise the mother.
If the woman is HIV positive, adolescent or has special needs, use
G1-G11 H1-H4 .
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E2
Postpartum care
ASK, CHECK RECORD
When and where did you deliver?
How are you feeling?
Have you had any pain or fever or
bleeding since delivery?
Do you have any problem with
passing urine?
Have you decided on any
contraception?
How do your breasts feel?
Do you have any other concerns?
Check records:
Any complications during
delivery?
Receiving any treatments?
HIV status.
LOOK, LISTEN, FEEL
Measure blood pressure and
temperature.
Feel uterus. Is it hard and round?
Look at vulva and perineum for:
tear
swelling
pus.
Look at pad for bleeding and lochia.
Does it smell?
Is it profuse?
Look for pallor.
SIGNS
Mother feeling well.
Did not bleed >250 ml.
Uterus well contracted and hard.
No perineal swelling.
Blood pressure, pulse and
temperature normal.
No pallor.
No breast problem,
is breastfeeding well.
No fever or pain or concern.
No problem with urination.
TREAT AND ADVISE
Make sure woman and family know what to watch
for and when to seek care D28 .
Advise on Postpartum care and hygiene,
and counsel on nutrition D26 .
Counsel on the importance of birth spacing and
family planning D27 .
Refer for family planning counselling.
Dispense 3 months iron supply and
counsel on compliance F3 .
Give any treatment or prophylaxis due:
tetanus immunization if she has not had
full course F2 .
Promote use of impregnated
bednet for the mother and baby.
Record on the mothers home-based maternal
record.
Advise to return to health centre within 4-6 weeks.
CLASSIFY
NORMAL POSTPARTUM
NEXT: Respond to observed signs or volunteered problems
POSTPARTUM EXAMINATION OF THE MOTHER (UP TO 6 WEEKS)
Use this chart for examining the mother after discharge from a facility or after home delivery
If she delivered less than a week ago without a skilled attendant, use the chart Assess the mother after delivery D21 .
To examine the baby see J2-J8 .
If breast problem see J9 .
NEXT: If pallor, check for anaemia
Respond to observed signs or volunteered problems (1) If elevated diastolic blood pressure
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E3
ASK, CHECK RECORD
History of pre-eclampsia or
eclampsia in pregnancy, delivery or
after delivery?
LOOK, LISTEN, FEEL
If diastolic blood pressure is
90 mmHg , repeat after
a 1 hour rest.
SIGNS
Diastolic blood pressure
110 mmHg.
Diastolic blood pressure
90 mmHg on 2 readings.
Diastolic blood pressure
<90 mmHg after 2 readings.
TREAT AND ADVISE
Give appropriate antihypertensive B14 .
Refer urgently to hospital B17 .
Reassess in 1 week.
If hypertension persists, refer to hospital.
No additional treatment.
CLASSIFY
SEVERE
HYPERTENSION
MODERATE
HYPERTENSION
BLOOD PRESSURE
NORMAL
RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
IF ELEVATED DIASTOLIC BLOOD PRESSURE
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E4
Respond to observed signs or volunteered problems (2) If pallor, check for anaemia
ASK, CHECK RECORD
Check record for bleeding in
pregnancy, delivery or postpartum.
Have you had heavy bleeding since
delivery?
Do you tire easily?
Are you breathless (short of breath)
during routine housework?
LOOK, LISTEN, FEEL
Measure haemoglobin if history of
bleeding.
Look for conjunctival pallor.
Look for palmar pallor.
If pallor:
is it severe pallor?
some pallor?
Count number of breaths in 1
minute.
SIGNS
Haemoglobin <7-g/dl
AND/OR
Severe palmar and conjunctival
pallor or
Any pallor and any of:
>30 breaths per minute
tires easily
breathlessness at rest.
Haemoglobin 7-11-g/dl
OR
Palmar or conjunctival pallor.
Haemoglobin >11-g/dl.
No pallor.
TREAT AND ADVISE
Give double dose of iron
(1 tablet 60 mg twice daily for 3 months) F3 .
Refer urgently to hospital B17 .
Follow up in 2 weeks to check clinical progress and
compliance with treatment.
Give double dose of iron for 3 months F3 .
Reassess at next postnatal visit (in 4 weeks).
If anaemia persists, refer to hospital.
Continue treatment with iron for 3 months
altogether F3 .
CLASSIFY
SEVERE
ANAEMIA
MODERATE ANAEMIA
NO ANAEMIA
NEXT: Check for HIV status
IF PALLOR, CHECK FOR ANAEMIA
Respond to observed signs or volunteered problems (3) Check for HIV status
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E5
ASK, CHECK RECORD
Provide key information on HIV G2 .
What is HIV and how is HIV
transmitted G2 ?
Advantage of knowing the HIV status
G2 .
Explain about HIV testing and
counselling including confidentiality
of the result G3 .
Ask the woman:
Have you been tested for HIV?
If not: tell her that she will be
tested for HIV, unless she refuses.
If yes: check result. (Explain to
her that she has a right not to
disclose the result.)
Are you taking any ARV
treatment?
Check treatment plan.
Has the partner been tested?
LOOK, LISTEN, FEEL
Perform the Rapid HIV test if not
performed in this pregnancy L6 .
SIGNS
Positive HIV test
Negative HIV test
She refuses the test or is not willing
to disclose the result of previous
test or no test results available
TREAT AND ADVISE
Counsel on implications of a positive test G3 .
Refer the woman to HIV services for further
assessment.
Counsel on infant feeding options G7 .
Provide additional care for HIV-positive woman G4 .
Counsel on family planning G4 .
Counsel on safer sex including use of condoms G2 .
Counsel on benefits of disclosure (involving) and
testing her partner G3 .
Provide support to the HIV-positive woman G5 .
Follow up in 2 weeks.
Counsel on implications of a negative test G3 .
Counsel on the importance of staying negative by
practising safer sex, including use of condoms G2 .
Counsel on benefits of involving and testing the
partner G3 .
Counsel on safer sex including use of condoms G2 .
Counsel on benefits of involving and testing the
partner G3 .
CLASSIFY
HIV-POSITIVE
HIV-NEGATIVE
UNKNOWN
HIV STATUS
NEXT: If heavy vaginal bleeding
CHECK FOR HIV STATUS
Use this chart for HIV testing and counselling during postpartum visit if the woman is not previously tested.
If the women has taken ARV during pregnancy or childbirth refer her to HIV services for further assessment.
IF HEAVY VAGINAL BLEEDING
Respond to observed signs or volunteered problems (4)
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E6
ASK, CHECK RECORD
Have you had:
heavy bleeding?
foul-smelling lochia?
burning on urination?
LOOK, LISTEN, FEEL
Feel lower abdomen and flanks for
tenderness.
Look for abnormal lochia.
Measure temperature.
Look or feel for stiff neck.
Look for lethargy.
SIGNS
More than 1 pad soaked in 5
minutes.
Temperature >38C and any of:
very weak
abdominal tenderness
foul-smelling lochia
profuse lochia
uterus not well contracted
lower abdominal pain
history of heavy vaginal bleeding.
Fever >38C and any of:
burning on urination
flank pain.
Burning on urination.
Temperature >38C and any of:
stiff neck
lethargy.
Fever >38C.
TREAT AND ADVISE
Give 0.2 mg ergometrine IM B10 .
Give appropriate IM/IV antibiotics B15 .
Manage as in
Rapid assessment and management B3-B7 .
Refer urgently to hospital B17 .
Insert an IV line and give fluids rapidly B9 .
Give appropriate IM/IV antibiotics B15 .
Refer urgently to hospital B17 .
Give appropriate IM/IV antibiotics B15 .
Refer urgently to hospital B17 .
Give appropriate oral antibiotic F5 .
Encourage her to drink more fluids.
Follow up in 2 days.
If no improvement, refer to hospital.
Insert an IV line B9 .
Give appropriate IM/IV antibiotics B15 .
Give artemether IM (or quinine IM if artemether not
available) and glucose B16 .
Refer urgently to hospital B17 .
Give oral antimalarial F4 .
Follow up in 2 days.
If no improvement, refer to hospital.
CLASSIFY
POSTPARTUM
BLEEDING
UTERINE
INFECTION
UPPER URINARY TRACT
INFECTION
LOWER
URINARY TRACT
INFECTION
VERY SEVERE FEBRILE
DISEASE
MALARIA
NEXT: If dribbling urine
IF FEVER OR FOUL-SMELLING LOCHIA
Respond to observed signs or volunteered problems (5)
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E7
ASK, CHECK RECORD
How have you been feeling recently?
Have you been in low spirits?
Have you been able to enjoy the
things you usually enjoy?
Have you had your usual level of
energy, or have you been feeling tired?
How has your sleep been?
Have you been able to concentrate
(for example on newspaper
articles or your favourite radio
programmes)?
LOOK, LISTEN, FEEL SIGNS
Dribbling or leaking urine.
Excessive swelling of vulva or
perineum.
Pus in perineum.
Pain in perineum.
Two or more of the following symptoms
during the same 2 week period
representing a change from normal:
Inappropriate guilt or negative
feeling towards self.
Cries easily.
Decreased interest or pleasure.
Feels tired, agitated all the time.
Disturbed sleep (sleeping too much
or too little, waking early).
Diminished ability to think or
concentrate.
Marked loss of appetite.
Any of the above,
for less than 2 weeks.
TREAT
Check perineal trauma.
Give appropriate oral antibiotics for lower urinary
tract infection F5 .
If conditions persists more than 1 week, refer the
woman to hospital.
Refer the woman to hospital.
Remove sutures, if present.
Clean wound. Counsel on care and hygiene D26 .
Give paracetamol for pain F4 .
Follow up in 2 days. If no improvement, refer to hospital.
Provide emotional support.
Refer urgently the woman to hospital B7 .
Assure the woman that this is very common.
Listen to her concerns. Give emotional
encouragement and support.
Counsel partner and family to provide assistance to
the woman.
Follow up in 2 weeks, and refer if no improvement.
CLASSIFY
URINARY
INCONTINENCE
PERINEAL
TRAUMA
PERINEAL
INFECTION OR PAIN
POSTPARTUM
DEPRESSION
(USUALLY AFTER
FIRST WEEK)
POSTPARTUM BLUES
(USUALLY IN FIRST WEEK)
NEXT: If vaginal discharge 4 weeks after delivery
IF DRIBBLING URINE
IF PUS OR PERINEAL PAIN
IF FEELING UNHAPPY OR CRYING EASILY
Respond to observed signs or volunteered problems (6)
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E8
NEXT: If cough or breathing difficulty
ASK, CHECK RECORD
Do you have itching at the vulva?
Has your partner had a urinary
problem?
If partner is present in the clinic, ask
the woman if she feels comfortable if
you ask him similar questions.
If yes, ask him if he has:
urethral discharge or pus
burning on passing urine.
If partner could not be approached,
explain importance of partner
assessment and treatment to avoid
reinfection.
LOOK, LISTEN, FEEL
Separate the labia and look for
abnormal vaginal discharge:
amount
colour
odour/smell.
If no discharge is seen, examine
with a gloved finger and look at the
discharge on the glove.
SIGNS
Abnormal vaginal discharge, and
partner has urethral discharge or
burning on passing urine.
Curd-like vaginal discharge and/or
Intense vulval itching.
Abnormal vaginal discharge.
TREAT AND ADVISE
Give appropriate oral antibiotics to woman F5 .
Treat partner with appropriate oral antibiotics F5 .
Counsel on safer sex including use of condoms G2 .
Give clotrimazole F5 .
Counsel on safer sex including use of condoms G2 .
If no improvement, refer the woman to hospital.
Give metronidazole to woman F5 .
Counsel on safer sex including use of condoms G2 .
CLASSIFY
POSSIBLE
GONORRHOEA OR
CHLAMYDIA
INFECTION
POSSIBLE CANDIDA
INFECTION
POSSIBLE
BACTERIAL OR
TRICHOMONAS
INFECTION
IF VAGINAL DISCHARGE 4 WEEKS AFTER DELIVERY
IF BREAST PROBLEM
See J9 .
Respond to observed signs or volunteered problems (7)
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E9
NEXT: If signs suggesting HIV infection
ASK, CHECK RECORD
How long have you been coughing?
How long have you had difficulty in
breathing?
Do you have chest pain?
Do you have any blood in sputum?
Do you smoke?
Are you taking anti-tuberculosis
drugs? If yes, since when?
LOOK, LISTEN, FEEL
Look for breathlessness.
Listen for wheezing.
Measure temperature.
SIGNS
At least 2 of the following:
Temperature >38C.
Breathlessness.
Chest pain.
At least 1 of the following:
Cough or breathing difficulty for
>3 weeks.
Blood in sputum.
Wheezing.
Temperature <38C.
Cough for <3 weeks.
Taking anti-tuberculosis drugs.
TREAT AND ADVISE
Give first dose of appropriate IM/IV antibiotics B15 .
Refer urgently to hospital B17 .
Refer to hospital for assessment.
If severe wheezing, refer urgently to hospital.
Advise safe, soothing remedy.
If smoking, counsel to stop smoking.
Assure the woman that the drugs are not harmful to
her baby, and of the need to continue treatment.
If her sputum is TB-positive within 2 months of delivery,
plan to give INH prophylaxis to the newborn K13 .
Reinforce advice for HIV testing G3 .
If smoking, counsel to stop smoking.
Advise to screen immediate family members and
close contacts for tuberculosis.
CLASSIFY
POSSIBLE PNEUMONIA
POSSIBLE CHRONIC
LUNG DISEASE
UPPER RESPIRATORY
TRACT INFECTION
TUBERCULOSIS
IF COUGH OR BREATHING DIFFICULTY
IF TAKING ANTI-TUBERCULOSIS DRUGS
Respond to observed signs or volunteered problems (8) If signs suggesting HIV infection
P
O
S
T
P
A
R
T
U
M
C
A
R
E
E10
ASK, CHECK RECORD
Have you lost weight?
Do you have fever?
How long (>1 month)?
Have you got diarrhoea
(continuous or intermittent)?
How long (>1 month)?
Have you had cough?
How long (>1 month)?
LOOK, LISTEN, FEEL
Look for visible wasting.
Look for ulcers and white patches in
the mouth (thrush).
Look at the skin:
Is there a rash?
Are there blisters along the ribs
on one side of the body?
SIGNS
Two of the following:
weight loss
fever >1 month
diarrhoea >1 month.
OR
One of the above signs and
one or more other sign or
from a high-risk group.
TREAT AND ADVISE
Reinforce the need to know HIV status and counsel
for HIV testing G3 .
Counsel on the benefits of testing her partner G3 .
Counsel on safer sex including use of condoms G2 .
Examine further and manage according to national
HIV guidelines or refer to appropriate HIV services.
Refer to TB centre if cough.
CLASSIFY
STRONG
LIKELIHOOD OF HIV
INFECTION
IF SIGNS SUGGESTING HIV INFECTION
HIV status unknown or known HIV-positive.
Preventive measures and additional treatments for the woman
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
A
D
D
I
T
I
O
N
A
L
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
F1
PREVENTIVE MEASURES AND ADDITIONAL TREATMENTS FOR THE WOMAN
F2
Givetetanus toxoid
Immunize all w omen Check the w omans tetanus toxoid (TT) immunization status: Wh en was TT last giv en? Wh ich dose of TT was this? Ifimmunization status unkno wn, giveTT1. Plan to giv e TT2 in 4 w eeks.
If due: Explain to the w oman that the v accine is safe to be giv en in pregnancy; itwi ll not har m the bab y. The injection site ma y become a little s wol len, red and painful, but this will g o awayin a fe w da ys. Ifshe has heard that the injection has contraceptiv e effects, assure her it does not, that it only protects her from disease. Gi ve0.5 ml TT IM, upper ar m. Advise w oman w hen next dose is due. Record on mother s card.
Tet anus toxoid schedule At first contact with w oman of childbearing ag e or at first antenatal care visit, asearlyaspossible. TT1 At least 4 w eeks after TT1 (at next antenatal care visit). TT2 At least 6 months after TT2. TT3 At least 1 y ear after TT3. TT4 At least 1 y ear after TT4. TT5
Givevitamin A postpartum
Gi ve200-000-IU vita min Acapsules after deliver y or within 6 w eeks of deliv ery: Explain to the w oman that the capsule with vitamin A will help her to reco verbetter, and that the baby will receiv e the vi tamin through her breast milk. ask her to s wallowthe capsule in y our prese nce. explain to her that if she feel s nauseated or has a headache, itshould pass in a couple of da ys.
DO NO Tgi vecapsules wi th high dose of v itamin A during pregnancy .
Vit amin A 1 capsule 200-000 1 capsule after deliv eryor within 6 w eeks of deliv ery
PREVENTIVE MEASURES
Preve ntive measures (1)
PREV
EN
TIV
E
M
EASU
RES AN
D
AD
D
ITIO
N
AL TREA
TM
EN
TS FO
R
TH
E WO
M
AN
Preve ntive measures (2) Iron and mebendazole F3
Giveiron and folic acid
Toal l pregnant, postpartum and post-abor tion w omen: Routinely once daily in pregnancy and until 3 months after deliv eryor abor tion. Twice daily as treatment for anaemia (double dose). Check w omans supply of iron and folic acid at each visit and dispense 3 months supply . Advise to store iron safely: Wh ere children cannot g et it Ina dryplace.
Iron and folate 1 tablet = 60-mg , folic acid = 400-g All women Women with anaemia 1 tablet 2 tablets In pre gnancy Throughout the pregnancy 3 months Postpartumand 3 months 3 months post-abortion
Givemebendazole
Gi ve500 mg to e ver y woman once in 6 months. DO NO Tgi veit in the first trimester .
Mebendazole 500 mg tablet 100 mg tablet 1 tablet 5 tablets
Motivate on compliance wi th iron treatm ent
Explore local percepti ons about iron trea tment (examples of incor rect perceptions: making more blo will mak e bleeding w orse, iron will cause too larg e a bab y). Explain to mother and her family: Iron is essential f or her health during preg nancy and after deliv ery The dang er of anaemia and need for supplementation. Di scuss an y incor rect perceptions. Explore the mother s concer ns about the medication: Has she used the tablets before? We re there proble ms? Any other concer ns? Advise on ho w to tak e the tablets Wi th meals or , if once daily , at night Iron tablets ma y help the patient feel les s tired. Donot stop treatment if this occurs Donot worr y about black stools.This is nor mal. Gi veadvice on ho w to manag e side- effects: Ifconstipated, drink more water Taketablets after f ood or at night to a voi d nausea Explain that these si de effects are not serious Advise her to retur n if she has problems taking the iron tablets. Ifnecessary , discuss with family member , TBA,ot her community-based health w orkers or other women,howto help in promoting the use of iron and folate tablets. Counsel on eating iro n-richfoods see C16 D26.
PREV
EN
TIV
E M
EASU
RES
AN
D
AD
D
ITIO
N
AL TREA
TM
EN
TS FO
R
TH
E WO
M
AN
F4
Giveprev entive intermittent treatment for
falciparum malaria
Gi vesulfadoxine-pyrimethamine at the beginning of the second and t hird trimester to all w omen according to national policy . Check w hen last dose of sulfadoxine-p yrimethamine giv en: Ifnodose in last month, gi vesulfadoxine-pyrimethamine, 3 t ablets in clinic. Advise w oman w hen next dose is due. Monitor the bab y for jaundice if giv en just before deliv ery . Record on home-based record.
Sulfadoxine p yrimethamine 1 tablet = 500 mg + 25 mg p yrimethamine sulfadoxine Second trimester Third trimester 3tablets 3 tablets
Advise to use insecticide-treated bednet
Ask whether w oman and ne wborn will be sleeping under a bednet. If y es, Has it been dipped in insecticide? Wh en? Advise to dip e ver y 6 months. Ifnot,advise to use insecticide-treated bednet, and pro vide infor mation to help her do this.
Giveappropriate oral antimalarial treatment
A highly effectiv e antimalarial (e venifsecond-line) is prefer red during pregnancy
Chloroquine Sulfadoxine + Pyrimethamine Givedaily for 3 da ys Givesingle dose in clinic Tablet Tablet Tablet (150 mg base) (100 mg base) 500 mg sulfadoxine + 25 mg p yrimethamine Pregnant w oman Da y 1 Day2 Da y 3 Day1 Day 2 Day3 (for w eight around 50 kg) 4 4 2 6 6 3 3
Giveparacetamol
If se ver e pain
Paracetamol Dose Frequency 1 tablet = 500 mg 1-2 tablets every4-6 hours
ANTIMALARIAL TREA TMENT AND PARACETAMOL
Additional treatments for the woman (1) Antimalarial treatme nt and parac etamol
PREV
EN
TIV
E
M
EASU
RES AN
D
AD
D
ITIO
N
AL TREA
TM
EN
TS FO
R
TH
E WO
M
AN
Additional treatments for the woman (2) Give appropriate ora l antibiot ics
COMMENT
Avoid in latepr egnancy and tw o weeks after deliv ery whe n breastfeeding .
Not safe for pregnant or lactating w omen.
Not safe for pregnant or lactating w oman.
Do not use in the first trimester of pregnancy .
Teach the w oman ho w to inser t a pessar y into v agina and to was h hands before and after each application.
GIVE APPR OPRIATE ORAL ANTIBIO TICS
PREV
EN
TIV
E M
EASU
RES
AN
D
AD
D
ITIO
N
AL TREA
TM
EN
TS FO
R
TH
E WO
M
AN
F5
ANTIBIOTIC
CLOXA CILLIN 1 capsule (500 mg)
AMOXY CILLIN 1 tablet (500 mg) OR TRIMETHOPRIM+ SULPHAMETHOXAZO LE 1 tablet (80 mg + 400 mg)
CEFTRIAXONE (Vial=250 mg)
CIPROFLO XACIN (1 tablet=250 mg)
ERYTHR OMYCIN (1 tablet=250 mg)
TETRACY CLINE (1 tablet=250 mg) OR DOXY CYCLINE (1 tablet=100 mg)
METRONID AZOLE (1 tablet=500 mg)
CLOTRIMAZO LE 1 pessar y 200 mg or 500 mg
INDICATION
Mastitis
Lower urinar y tr act infection
Gonorr hoea Wo man
Partner only
Chlamydia Wo man
Partner only
Tri chomonas or bacterial vaginal infection
Vaginal candida infection
DOSE
500 mg
500 mg
80 mg trimethoprim + 400 mg sulphamethoxa zole
250 mg IM injection
500 mg (2 tablets)
500 mg (2 tablets)
500 mg (2 tablets)
100 mg
2 g or 500 mg
200 mg
500 mg
FREQUENCY
every6 hours
every8 hours
twotablets every12 hours
once only
once only
every6 hours
every6 hours
every12 hours
once only every12 hours
everynight
once only
DURATION
10 da ys
3 da ys
3 da ys
once only
once only
7 da ys
7 da ys
7 da ys
once only 7 da ys
3 da ys
once only
Additional treatments for the woman (3) Give benzathine peni cillin IM
PREV
EN
TIV
E
M
EASU
RES AN
D
AD
D
ITIO
N
AL TREA
TM
EN
TS FO
R
TH
E WO
M
AN
F6
COMMENT
Giveas two IM inj ections at separate sites. Plan to treat ne wbornK12. Counsel on cor rect and consistent use of condoms G2.
Not safe for pregnant or lactating w oman.
ANTIBIOTIC
BENZATHINE PENICILLIN IM (2.4 million units in 5 ml)
ERYTHR OMYCIN (1 tablet = 250 mg)
TETRACY CLINE (1 tablet = 250 mg) OR DOXY CYCLINE (1 tablet = 100 mg)
INDICATION
Syphilis RPR test positive
If woman has allerg y to penicillin
If par tner has allerg y to penicillin
DOSE
2.4 million units IM injection
500 mg (2 tablets)
500 mg (2 tablets)
100 mg
FREQUENCY
once only
every6 hours
every6 hours
every12 hours
DURATION
once only
15 da ys
15 da ys
15 da ys
GIVE BENZA THINE PENICILLIN IM
Treat the par tner. Rule out histor y of allerg y to antibiotics.
OBSERVE FOR SIGNS OF ALLERGY
After giving penicillin injection, keep the woman for a few minutes and obser ve for signs of allerg y.
ASK, CHECK RECORD
How are y ou feeling? Doyou feel tightness in the chest and throat? Doyou feel dizzy and confused?
LOOK, LISTEN, FEEL
Look at the face, neck and tongue for s wel ling. Look at the skin for rash or hiv es. Look at the injection site f or s wel ling and redness. Look for difficult breathing . Li sten for w heezing.
SIGNS
Anyof these signs: Ti ghtness in the chest and throat. Feeling dizzy and confused. Swelling of the face, neck and tongue. Injection site s wol len and red. Rash or hiv es. Di fficult breathing or w heezing.
TREAT
Open the airwa y B9. InsertIV line and giv e fluidsB9. Gi ve0.5 ml adren aline1:1000 in 10 ml saline solution IV slo wly. Repeat in 5-15 minutes, ifrequired. DONOT lea vethe w oman on her o wn. Refer urg ently to hospita l B17.
CLASSIFY
ALLERGY T O PENICILLI N
F2 PREVENTIVE MEASURES (1)
Give tetanus toxoid
Give vitamin A postpartum
F3 PREVENTIVE MEASURES (2)
Give iron and folic acid
Motivate on compliance with iron treatment
Give mebendazole
F4 ADDITIONAL TREATMENTS
FOR THE WOMAN (1)
Give preventive intermittent treatment for
falciparum malaria
Advise to use insecticide-treated bednet
Give paracetamol
F5 ADDITIONAL TREATMENTS
FOR THE WOMAN (2)
Give appropriate oral antibiotics
F6 ADDITIONAL TREATMENTS
FOR THE WOMAN (3)
Give benzathine penicillin IM
Observe for signs of allergy
This section has details on preventive measures and treatments
prescribed in pregnancy and postpartum.
General principles are found in the section on good practice A2 .
For emergency treatment for the woman see B8-B17.
For treatment for the newborn see K9-K13 .
F2
Give tetanus toxoid
Immunize all women
Check the womans tetanus toxoid (TT) immunization status:
When was TT last given?
Which dose of TT was this?
If immunization status unknown, give TT1.
Plan to give TT2 in 4 weeks.
If due:
Explain to the woman that the vaccine is safe to be given in pregnancy; it will not harm the baby.
The injection site may become a little swollen, red and painful, but this will go away in a few days.
If she has heard that the injection has contraceptive effects, assure her it does not, that it only
protects her from disease.
Give 0.5 ml TT IM, upper arm.
Advise woman when next dose is due.
Record on mothers card.
Tetanus toxoid schedule
At first contact with woman of childbearing age or
at first antenatal care visit, as early as possible. TT1
At least 4 weeks after TT1 (at next antenatal care visit). TT2
At least 6 months after TT2. TT3
At least 1 year after TT3. TT4
At least 1 year after TT4. TT5
Give vitamin A postpartum
Give 200-000-IU vitamin A capsules after delivery or within 6 weeks of delivery:
Explain to the woman that the capsule with vitamin A will help her to recover better, and that the
baby will receive the vitamin through her breast milk.
ask her to swallow the capsule in your presence.
explain to her that if she feels nauseated or has a headache, it should pass in a couple of days.
DO NOT give capsules with high dose of vitamin A during pregnancy.
Vitamin A
1 capsule 200-000 IU 1 capsule after delivery or within 6 weeks of delivery
PREVENTIVE MEASURES
Preventive measures (1)
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
A
D
D
I
T
I
O
N
A
L
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
Preventive measures (2) Iron and mebendazole
F3
Give iron and folic acid
To all pregnant, postpartum and post-abortion women:
Routinely once daily in pregnancy and until 3 months after delivery or abortion.
Twice daily as treatment for anaemia (double dose).
Check womans supply of iron and folic acid at each visit and dispense 3 months supply.
Advise to store iron safely:
Where children cannot get it
In a dry place.
Iron and folate
1 tablet = 60-mg, folic acid = 400-g
All women Women with anaemia
1 tablet 2 tablets
In pregnancy Throughout the pregnancy 3 months
Postpartum and 3 months 3 months
post-abortion
Give mebendazole
Give 500 mg to every woman once in 6 months.
DO NOT give it in the first trimester.
Mebendazole
500 mg tablet 100 mg tablet
1 tablet 5 tablets
Motivate on compliance with iron treatment
Explore local perceptions about iron treatment (examples of incorrect perceptions: making more blood
will make bleeding worse, iron will cause too large a baby).
Explain to mother and her family:
Iron is essential for her health during pregnancy and after delivery
The danger of anaemia and need for supplementation.
Discuss any incorrect perceptions.
Explore the mothers concerns about the medication:
Has she used the tablets before?
Were there problems?
Any other concerns?
Advise on how to take the tablets
With meals or, if once daily, at night
Iron tablets may help the patient feel less tired. Do not stop treatment if this occurs
Do not worry about black stools.This is normal.
Give advice on how to manage side-effects:
If constipated, drink more water
Take tablets after food or at night to avoid nausea
Explain that these side effects are not serious
Advise her to return if she has problems taking the iron tablets.
If necessary, discuss with family member, TBA, other community-based health workers or other
women, how to help in promoting the use of iron and folate tablets.
Counsel on eating iron-rich foods see C16 D26 .
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
A
D
D
I
T
I
O
N
A
L
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
F4
Give preventive intermittent treatment for
falciparum malaria
Give sulfadoxine-pyrimethamine at the beginning of the second and third trimester to all women
according to national policy.
Check when last dose of sulfadoxine-pyrimethamine given:
If no dose in last month, give sulfadoxine-pyrimethamine, 3 tablets in clinic.
Advise woman when next dose is due.
Monitor the baby for jaundice if given just before delivery.
Record on home-based record.
Sulfadoxine pyrimethamine
1 tablet = 500 mg + 25 mg pyrimethamine sulfadoxine
Second trimester Third trimester
3 tablets 3 tablets
Advise to use insecticide-treated bednet
Ask whether woman and newborn will be sleeping under a bednet.
If yes,
Has it been dipped in insecticide?
When?
Advise to dip every 6 months.
If not, advise to use insecticide-treated bednet, and provide information to help her do this.
Give appropriate oral antimalarial treatment
A highly effective antimalarial (even if second-line) is preferred during pregnancy
Chloroquine Sulfadoxine +
Pyrimethamine
Give daily for 3 days Give single dose in clinic
Tablet Tablet Tablet
(150 mg base) (100 mg base) 500 mg sulfadoxine +
25 mg pyrimethamine
Pregnant woman Day 1 Day 2 Day 3 Day 1 Day 2 Day 3
(for weight around 50 kg) 4 4 2 6 6 3 3
Give paracetamol
If severe pain
Paracetamol Dose Frequency
1 tablet = 500 mg 1-2 tablets every 4-6 hours
ANTIMALARIAL TREATMENT AND PARACETAMOL
Additional treatments for the woman (1) Antimalarial treatment and paracetamol
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
A
D
D
I
T
I
O
N
A
L
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
Additional treatments for the woman (2) Give appropriate oral antibiotics
COMMENT
Avoid in late pregnancy and two weeks after delivery
when breastfeeding.
Not safe for pregnant or lactating women.
Not safe for pregnant or lactating woman.
Do not use in the first trimester of pregnancy.
Teach the woman how to insert a pessary into vagina
and to wash hands before and after each application.
GIVE APPROPRIATE ORAL ANTIBIOTICS
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
A
D
D
I
T
I
O
N
A
L
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
F5
ANTIBIOTIC
CLOXACILLIN
1 capsule (500 mg)
AMOXYCILLIN
1 tablet (500 mg)
OR
TRIMETHOPRIM+
SULPHAMETHOXAZOLE
1 tablet (80 mg + 400 mg)
CEFTRIAXONE
(Vial=250 mg)
CIPROFLOXACIN
(1 tablet=250 mg)
ERYTHROMYCIN
(1 tablet=250 mg)
TETRACYCLINE
(1 tablet=250 mg)
OR
DOXYCYCLINE
(1 tablet=100 mg)
METRONIDAZOLE
(1 tablet=500 mg)
CLOTRIMAZOLE
1 pessary 200 mg
or
500 mg
INDICATION
Mastitis
Lower urinary tract
infection
Gonorrhoea
Woman
Partner only
Chlamydia
Woman
Partner only
Trichomonas or bacterial
vaginal infection
Vaginal candida infection
DOSE
500 mg
500 mg
80 mg
trimethoprim +
400 mg sulphamethoxazole
250 mg
IM injection
500 mg
(2 tablets)
500 mg
(2 tablets)
500 mg
(2 tablets)
100 mg
2 g
or 500 mg
200 mg
500 mg
FREQUENCY
every 6 hours
every 8 hours
two tablets
every 12 hours
once only
once only
every 6 hours
every 6 hours
every 12 hours
once only
every 12 hours
every night
once only
DURATION
10 days
3 days
3 days
once only
once only
7 days
7 days
7 days
once only
7 days
3 days
once only
Additional treatments for the woman (3) Give benzathine penicillin IM
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
A
D
D
I
T
I
O
N
A
L
T
R
E
A
T
M
E
N
T
S
F
O
R
T
H
E
W
O
M
A
N
F6
COMMENT
Give as two IM injections at separate sites.
Plan to treat newborn K12 .
Counsel on correct and consistent use of condoms G2 .
Not safe for pregnant or lactating woman.
ANTIBIOTIC
BENZATHINE
PENICILLIN IM
(2.4 million units in 5 ml)
ERYTHROMYCIN
(1 tablet = 250 mg)
TETRACYCLINE
(1 tablet = 250 mg)
OR
DOXYCYCLINE
(1 tablet = 100 mg)
INDICATION
Syphilis RPR test positive
If woman has allergy to
penicillin
If partner has allergy to
penicillin
DOSE
2.4 million units
IM injection
500 mg
(2 tablets)
500 mg
(2 tablets)
100 mg
FREQUENCY
once only
every 6 hours
every 6 hours
every 12 hours
DURATION
once only
15 days
15 days
15 days
GIVE BENZATHINE PENICILLIN IM
Treat the partner. Rule out history of allergy to antibiotics.
OBSERVE FOR SIGNS OF ALLERGY
After giving penicillin injection, keep the woman for a few minutes and observe for signs of allergy.
ASK, CHECK RECORD
How are you feeling?
Do you feel tightness in the chest
and throat?
Do you feel dizzy and confused?
LOOK, LISTEN, FEEL
Look at the face, neck and tongue
for swelling.
Look at the skin for rash or hives.
Look at the injection site for swelling
and redness.
Look for difficult breathing.
Listen for wheezing.
SIGNS
Any of these signs:
Tightness in the chest and throat.
Feeling dizzy and confused.
Swelling of the face, neck and
tongue.
Injection site swollen and red.
Rash or hives.
Difficult breathing or wheezing.
TREAT
Open the airway B9 .
Insert IV line and give fluids B9 .
Give 0.5 ml adrenaline 1:1000 in 10 ml saline
solution IV slowly.
Repeat in 5-15 minutes, if required.
DO NOT leave the woman on her own.
Refer urgently to hospital B17 .
CLASSIFY
ALLERGY TO
PENICILLIN
Inform and counsel on HIV
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G1
INFORM AND COUNSEL ON HIV
PROVIDE KEY INFORMA TION ON HIV
Provide key infor mation on HIV
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IVG2
What is HIV (human immunodeficiency vir us)
and ho w is HIV transmitted?
HI V is a vir us that destro ys par ts of the bod ysimmune system. Aperson infected with HIV ma y not feel sick at first, but slo wly the bod ysimmune system is destro yed. The person becomes ill and unable to fight infection. Once a person is infected with HIV , she or he can giv e the vir us to others. HI V can be transmitted through: Exchange of HIV-infected bod y fluids such as semen, vaginal fluid or blood during unprotected sexual intercourse. HI V-infected blood transfusions or contaminated needles. Fr om an infected mother to her child (MTCT) during: pr egnancy labour and deliv ery postpartum through breastfeeding . Al most four out of 20 babies bor n to HIV positiv e women ma y be infected wit hout an y inter vention. HI V cannot be transmitted through hugging or mosquito bites. Ablood test is done to find out if the person is infected with HIV . Al l pregnant w omen are offered this test. Theycan refuse the test.
Adv antage of kno wing the HIV status in pre gnancy
Knowing the HIV status during pre gnancy is impor tant so that the wo man can: the woman kno ws her HIV status can share infor mation with her par tner encourage her par tner to be tested If the w oman is HIV-positiv e she can: get appropriate medical care to treat and/or pre vent HIV-associated i llnesses. reduce the risk of transmission of infection to the bab y: bytaking antiretro viral dr ugs in pregnancy , and during labour G6, G9 bypr acticing safer infant feeding options G9 byadapting bir th and emerg ency plan and deliv erypractices G4. pr otect herself and her sexual par tner(s) from infection or reinfection . makea choice about future pregnancies. If the w oman is HIV- neg ativeshe can: learnhowto remain neg ative.
Counsel on safer sex includi ng use of condoms
SAFER SEX IS ANY SEXU AL PRA CTICE THA T REDUCE S THERISK OF TRANSMITT ING HIV AND SEXUALL Y TRANSMITTED INFECTIONS (STI s) FROM ONE PERSON TOANOTHER
THE BEST PR OTE CTION IS OBT AINED BY: Corr ect and consist ent use of condoms during e ver y sexua l act. Choosing sexual activi ties that do not allo w semen, fl uid from the vagina, or bloo d to ent er the mouth, anus or v agina of the par tner. Reducing the number of par tners. If the w oman is HIV- negativ e explain to her that she is at risk of H IV infe ction and that it is important to remain neg ativeduring pregnancy and breastfeeding . The risk of infecting the bab y is higher if the mot her is ne wly infe cted. If the w oman is HIV -positive explain to her that condom use during e ver y sexual act during pregnancy and bre ast feedin g will pr otect her and her bab y from sex uallytransmitted infections, or reinfection with anot her HIV strain and will pre vent the transmiss ion of HIV infection toher par tner. Makesure the w oman kno ws ho w to us e condoms and w here to g et them.
HIV TESTING AND COUNSELLING
HIV testing and counselling
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IV
G3
Vol untary counselling and testing (VCT) ser vices
Explain about HIV testing: HI V test is used to deter mine if the w oman is infected with HIV . Itincludes blood testing and counselling . Result is a vai lable on the same da y or at the next visit. The test is offered routinely to e ver y woman at e ver y pregnancy to hel p protect her and her bab ys health. She ma y decline the test.
If HIV testing is not a vai lable in your setting , informthe woman about: Pr e-test counselling . Post-test counselling . Infant feeding counselling .
If VCT is not a vai lable in your setting , informthe woman about: Wh ere to g o. How the test is perfor med. How confidentiality is maintained ( see belo w). Wh en and ho w results are giv en. Wh en she should come back to the clinic with the test result Costs in vol ved. Pr ovi de the address of HIV testing in y our area s nearest site :
____________________________________________________________________
____________________________________________________________________
Discuss confidentiality of HIV infection
Assure the w oman that her test result is confidential and will be shar ed only with herself and an y person chosen b y her . Ensure confidentiality w hen discussing HIV results, status, treatment and care related to HIV, opportunistic infections, additional visits and infant feeding options. A2 Ensure all records are confidential and k ept lock ed awayand only health care w orkers taking care of her ha veaccess to the records. DO NO Tlabel records as HIV-positiv e.
Counsel on implicati ons of the HIV test resul t
Di scuss the HIV result s when the w oman is alone or with the person of her choice. State test results in a neutr al tone . Gi vethe w oman time to ex pressany emotions.
IF TEST RESULT IS NEGA TIVE: Explain to the w oman that a neg ativeresult can mean either thatshe is not infected with HIV o r that she is infected with HIV but has not y et made antibodies a gai nst the vir us (this is sometimes called the windo wperiod). Counsel on the impor tanceof sta ying neg ativebysafer sex including use of condoms G2.
IF TEST RESULT IS POSITIVE: Explain to the w oman that a positiv e test result means that she is car ryi ng the inf ection and has the possibility of transmitt ing the infection to her unbor n child without an y inter vention. Let her talk about h er feel ings. Respond to her immediate concerns. Informher that she w ill need fur ther assessment to deter mine the se ver ity of the infection, appropriate care and treat ment needed for herself and her bab y.Tre atment will slo w do wn the progression of her HIV infection and will reduce the risk of infection to the bab y. Provide information on ho w to pre vent HIV re-infection. Informher that suppo rtand couns elling is a vai lable if needed, tocope on living with HIV infection. Discuss disclosure an d par tner testing . Ask the w oman if she has an y concer ns.
Benefits of disclosure (in vol ving) and testing the male
partner (s)
Encourage the w omen to disclose the HIV results to her par tner or another person she tr usts. By disclosing her HIV statustoher par tner and family , the woman ma y be in a better position to: Encourage partner tobetested for HIV . Prev ent the transmis sion of HIV to her par tner(s). Prev ent transmissio n of HIV toher bab y. Protect herself from HI V rein fection. Access HIV treatment , care and suppor t ser vices. Receive support from her par tner(s) and family w hen accessing antenatal care and HIV treatm care and suppor t ser vices. Help to decrease the r isk of suspicion and violence.
CARE AND COUNSELLING FOR THE HIV-POSITIVE WOMAN
Care and counselling for the HIV-positive woman
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IVG4
Additional care for the HIV- positiv e woman
Determine howmuch the w oman has told her par tner, labour companion and family , then respect this confidentiality . Be sensitiv e to her special concer ns and fears. Gi veher additional sup portG5. Advise on the impor tance of g ood nutrition C13D26. Use standard precautions as for all w omenA4. Advise her that she is more prone to infections and should seek medi cal help as soon as possible if she has: fever persistent diar rhoea cold and cough respirator y infections burning urination vaginal itching/foul-smelling discharg e no weight g ain skin infections foul-smelling lochia.
DURING PREGNANCY: Revisethe bir th planC2 C13. Advise her to deliv er in a facility . Advise her to g o to a facility as soon as her membranes r upture or labour star ts. Tel l her to tak e ARV medicine at the onset of labour as instr uctedG6. Discuss the infant feeding options G8-G9. Modify pre ventivetreatment for malaria, according to national strateg y F4.
DURING CHILDBIRTH: Check if ne virapine is tak en at onset of labour . GiveARVmedicines as prescribed G6, G9. Adhere to standard practice for labour and deliv ery . Respect confidentiality w hen giving ARVto the mother and bab y. Record all ARVmedicines giv en on labour record, postpartum record and on refer ral record, if woman is refer red.
DURING THE POSTP ARTUM PERIOD: Tel l her that lochia can cause infection in other people and therefore she should dispose of blood stained sanitar y pads safely (list local options). Counsel her on family planning G4. If not breastfeeding , advi se her on breast care K8. Visit HIV ser vices 2 w eeks after deliv eryfor fur ther assessment.
Counsel the HIV-posi tivewoman on famil y planning
Use the ad vice and coun selling sections on C15during antenatal care and D27 during postp artum visits. The follo wing ad vice should be highlighted: Explain to the w oman that future pregnancies can ha vesignificant health risks for her and her bab y.These incl ude: transmission of HIV to the bab y (dur ing pregnancy , deliver y or breastfeeding), mi scarr iage, pr etermlabour, stillbirth, low bir th weight, ectopic pregnancy and other complicati ons. Ifshe wants more children, advise her that wait ing at least 2-3 y ears betw een pregnancies is healthier for her and the bab y. Di scuss her options for pre venting both pregnancy and infection with other sexually tr infections or HIV reinfec tion. Condoms ma y be the best option for the w oman with HIV . Counsel the w oman on safer sex including the use of condoms G2. Ifthe woman think tha t her par tnerwill not use condoms, she ma y wish touse an addi tional method for pregnancy pr otect ion. Howev er,not all meth ods are appropriate for the HIV-positiv e woman: Gi venthe womans HIV status, she ma y not choose to breastfeed and lactational amenor rhoea method (LAM) ma y not be a suitable method. Spermicides are not rec ommended for HIV-positiv e women. Intrauterine de vice (IUD) use is not recommended for w omen with AIDS w ho are not onARV therapy . Due to chang es in the menstr ual cycle and ele vat ed temperatures fer tility a wareness methods maybe difficult if the w oman has AIDS or is on treatment for HIV infections. Ifthe woman is taking pills for tuberculosis (rifampin), she usually cannot use contraceptiv e pills, monthly injectabl es or implants.
The family planning c ounsell or will pro vide more info rmation.
SUPPORT T O THE HIV-POSITIVE W OMAN
Pregnant women who are HIV- positive benefit g reatly from the following suppor t after the first impact of the test result has been over come.
Support to the HIV-positive woman
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IV
G5
Provide emotional suppor t to the w oman
Empathize with her concer ns and fears. Use g ood counselling skills A2. Help her to assess her situation and decide w hich is the best option for her , her (unbor n) child and her sexual par tner. Support her choice. Connect her with other existing suppor t ser vices including suppor t groups, income- generatingactivities, religious suppor t groups, orphan care, home care. Help her to find wa ys to in vol veher par tner and/or extended family me mbers in sharing responsibility, toidentify a figure from the community w ho will suppor t and care for her . Discuss ho w to pro vide for the other children and help her identify a figure from the extended family or community w ho will suppor t her children. Confirm and suppor t infor mation giv en during HIV testing and counsell ing,the possibility of ARV treatment, safe sex, infant feeding and family planning ad vice (help her to absorb the infor mation and apply it in her o wn case). If the w oman has signs of AIDS and/or of other illness, refer her to appropriate ser vices.
Howto pro vide suppor t
Conduct peer suppor t groups for w omen w ho ha veHIV-infection and couples affected b y HIV/AIDS: Led b y a social w orker and/or w oman w ho has come to termswi th her o wn HIV infection. Establish and maintain constant linkag es with ot her healt h,social and community w orkers support services: To exchange informati on for the coordination of inter ventions To makea plan fo r each family in vol ved. Refer individuals or couples for counselling b y commu nitycounsellors.
Give antiretro viral (ARV) medicine(s) to treat HIV inf ection
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IVG6
GIVE ANTIRETR OVI RAL (AR V) MEDICINE(S) TOTREAT HIV INFECTION
Use these char ts when star ting AR V medicine(s) and to suppor t adherence to ARV
Support the initiation of ARV
Ifthe woman is alread y onARVtreatment continue the treatment durin g pregnancy , as prescribed. If she is in the first trimester of pregnancy and treatment includes efa virenz, replace it with ne virapine. Ifthe woman is not on ARVtreatment and is tested HIV-positiv e,choose appropriate ARVregimens C9, G10according to the stag e of the disease. Iftreatment with Zido vudine (AZT) is planned: measure haemoglobin; i f less than 8 g/dl, refer to hospital C4. Wr ite the treatment plan in the Home Based Mater nal Record. Gi vewritten instr uctions to the w oman on ho w to tak e the medicines. Gi veprophylaxis for oppor tunistic infections according to national guid elines. Modify pre ventivetreatment for malaria according to national guidelin es F4.
Explore local perceptions about ARVs
Explain to the woman and family that: ARV treatment will impro vethe w omans health and will g reatly reduce the risk of infection to her baby.The treatment will not cure the disease. The choice of regimen depends on the stag e of the disease C19. If she is in ear ly stag e of HIV infection, she will need to tak e medicines duri ng pregnancy , childbirth and only for a shor t period after deliv eryto pre vent mother-to-chil d transmission of HIV infection (PMTCT). Pr ogress of disease will be monitored to deter mine if she needs additional treatment. If she has mild-se ver e HIV disease she will need to continue the treatment e venafter childbir th and postpar tum period. She ma y ha vesome side effects but not all w omen ha vethem. Common side effects lik e nausea, diarr ohea, headache or fe verof ten occur in the beginning but the y usually disappe ar within 23 week s.Other side effects lik e yelloweyes,pallor, sever e abdominal pain , shortness of breath, skin rash, painful feet, legs or hands ma y appear at an y time. Ifthese signs persist, she should come to the clinic. Gi veher enough ARVtablets for 2 w eeks or till her next ANC visit. Ask the w oman if she has an y concer ns.Discuss an y incor rect perceptions.
Support adherence to ARV
For AR V medicine to be effectiv e: Advise w oman on: Explain to her that to rec eiveARVprophylact ic treatment, she must: which tablets she needs to tak e during pregnancy , when labo ur begins (painful abdominal contractions and/or membranes r upture) and after childbir th. taking the medicine regular ly,everyday, at the right time. Ifshe choos es to stop taking medicines during pregnancy , her HIV disease could getworse and she ma y pass t he infe ction to her child. ifshe forg ets to tak e a dose, she should not doub le the ne xt dose. continue the treatment during and after the childbir th (if prescribed), even if she is breastfeeding . taking the medicine(s) with meals in order tomi nimize side effects. For ne wborn: Gi vethe first dose of medicine to the ne wborn 812 hours after bir th. Teach the mother ho w to giv e treatment to the ne wborn. Tell the mother that the bab y must c omplete the full course of treatment and will need regula visits throughout the infa ncy. Ifthe mother receiv ed less th an 4 w eeks of Zido vudine (AZT) during pregnancy , givethe treatment to the ne wborn for 4 w eeks. Record all treatment gi ven. If the m other or bab y is refer red, write the treatment giv en and the regimen prescribed o n the re ferr al card .
DO NO Tlabel records asHI V-Posit ive DO NO Tshare dr ugs with family or friends.
Counsel on infant f eeding options
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IV
G7
COUNSEL ON INF ANT FEEDING OPTIONS
Explain the risks of HIV transmission through
breastfeeding and not breastfeeding
Four out of 20 babies bor n to kno wn HIV-positiv e mothers will be i nfected during pregnancy and deliver y without ARVmedication. Three more ma y be infected b y breastfeedin g. The risk ma y be reduced if the bab y is breastfed exclusiv ely using g ood technique, sothat the breasts sta y health y. Mastitis and nipple fissures increase the risk that the bab y will be infecte d. The risk of not breastfeeding ma y be much higher because replacemen t feeding car ries risks too: di arr hoea because of contamination from unclean water , unclean utensils or because the milk is left out too long . malnutrition because of insufficient quantity giv en to the bab y,the milk is too water y,or because of recur rent episodes of diar rhoea. Mi xed feeding increases the risk of diar rhoea. It ma y also increase the ri sk of HIV transmission.
If a w oman does not kno w her HIV status
Counsel on the impor tance of exclusiv e breastfeeding K2. Encourage exclusive breastfeeding. Counsel on the need to kno w the HIV status and w here to g o for HIV testing and counselling G3. Explain to her the risks of HIV transmission: even in areas w here man y women ha veHIV, most women are neg ative the risk of infecting the bab y is higher if the mother is ne wly infected explain that it is v eryimportant to avoi d infection during pregnancy and the breastfeedi ng period.
If a w oman kno ws that she is HIV -positive
Informher about the o ptions for feeding , the ad vantagesand ris ks: If acceptable, feasible, safe and sustai nable (affordable), she might choose replacement feedin with home-prepar ed for mula or commerc ial for mula. Exclusive breastfeeding, stopping as soon as replacement feeding is possible. Ifreplacement feeding is introduced early , she must st op breas tfeeding. Exclusive breastfeeding for 6 months, then continued breastfeeding plus complementar y feedi ng after 6 months of ag e,as recom mended for HIV-neg ativewomen and w omen w ho do not kno w their status. In some situations additiona l possibilities are: expressing and heat- treating her breast milk wetnursing b y an HIV-neg ativewoman. Help her to assess her si tuation and decide w hich is the best option for her , and suppor t her choice. If the mother choos es breas tfeeding, gi veher special ad vice. Makesure the mother understands that if she choos es replacement feeding this includes enric complementary feeding up to 2 years. If this cannot be e nsured, exclusiv e breastfeeding , stopping ear ly when replacement feeding is feasible, is an alter nativ e. All babies receivi ng repl acement feeding need regular follo w-up, and their mothers need suppor t to pro vide cor rect repl acement feeding .
G2
PROVIDE KEY INFORMATION ON HIV
What is HIV and how is HIV transmitted?
Advantage of knowing the HIV status in
pregnancy
Counsel on safer sex including use of condoms
G3 HIV TESTING AND COUNSELLING
HIV testing and counselling
Discuss confidentiality of HIV infection
Counsel on implications of the HIV test result
Benefits of disclosure (involving) and testing the
male partner(s)
G4 CARE AND COUNSELLING FOR
THE HIV-POSTITIVE WOMAN
Additional care for the HIV-positive woman
Counsel the HIV-positive woman on family
planning
G5 SUPPORT TO THE
HIV-POSITIVE WOMAN
Provide emotional support to the woman
How to provide support
G6 GIVE ANTIRETROVIRAL (ARV)
MEDICINE(S) TO TREAT HIV
INFECTION
Support the initiation of ARV
Support adherence to ARV
G7 COUNSEL ON INFANT FEEDING
OPTIONS
Explain the risks of HIV transmission through
breastfeeding and not breastfeeding
If a woman does not know her HIV status
If a woman knows that she is HIV-positive
Support the mother s choice of infant f eeding
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IVG8
SUPPORT THE MOTHERS CHOICE OF INF ANT FEEDING
If the mother chooses replacement feeding ,
teach her replacement feeding
Ask the mother w hat kind of replacement feeding she chose. For the first fe w feeds after deliv ery , prepare the for mula for the mothe r,then teach her ho w to prepare the for mula and feed the bab y by cupK9: Wa sh hands with water and soap Boil the water for fe w minutes Cl ean the cup thoroughly with water , soap and, ifpossible, boil or pour boiled water in it Decide ho w much milk the bab y needs from the instr uctions Measure the milk and water and mix them Teach the mother ho w to feed the bab y by cup Let the mother feed the bab y 8 times a da y (in the first month). Teach her to be flexible and respond to the bab ysdemands Ifthe bab y does not finish the feed within 1 hour of preparation, gi veit to an older child or add to cooking. DONOT giv e the milk to the bab y for the next feed Wa sh the utensils with water and soap soon after feeding the bab y Makea new feed e ver y time. Gi veher written instr uctions on safe preparation of for mula. Explain the risks of replacement feeding and ho w to a voi d them. Advise w hen to seek care. Advise about the follo w-up visit.
Explain the risks of replacement feeding
Her bab y ma y get diar rhoea if: hands, water, orut ensils are not clean the milk stands out too long . Her bab y ma y not g rowwel l if: she/he receiv es too little for mula each feed or too fe w feeds the milk is too water y she/he has diar rhoea.
Follo w-up for re placement feeding
Ensure regular follo w-up visits for g rowth monitoring. Ensure the suppor t to pro vide safe replacement feeding . Advise the mother to r eturnif: the bab y is feeding less than 6 times, oristaking smaller quantities K6 the bab y has diar rhoea there are other dang er signs.
Givespecial counselli ng to the mother
whoisHI V-positive and choos es breast feeding
Support the mother in her choice of breastfeeding . Ensure g ood attachment and suckling to pre vent mas titisand nipp le damag e K3. Advise the mother to r eturnimmediately if: she has an y breast symptoms or signs the bab y has an y difficulty feeding . Ensure a visit in the fir st week to assess attachment and positioning and the condition o mothers breasts. Ar range for fur ther counselling to prepare for the possibility of stopping breastfeeding ear ly. Gi vepsychosocial suppo rt G6.
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IV
G9
ANTIRETR OVI RALS FOR HIV-POSITIVE WOMAN AND HER INF ANT
Below are examples of ARVregime ns.Use national guidelines for local protocols.
Forlongerregime ns to fur ther reduce the risk of tr ansmission follow national guidelines.
Record the ARVmedicine prescribed and given in the appropriate records facility and home-based. DONOT write HIV-positive.
Antiretrovirals for HIV-positive woman and her infant
Woman Newborn infant
Pregnancy Labour, delivery Postpartum**
ARVs Before 28 weeks Starting at 28 weeks At onset of labour* Until bir th of the bab y After bir th of the bab y ARVs Dose (syrup) Give first dose Then give Duration
HIV-positive with HIV-AIDS related signs and symptoms
Tri ple therap y Continue the ARVtreatment prescribed before pregnancy . In the first trim ester replace Efavirenz with Ne virapine (200 mg once daily for 2 w eeks, then e ver y 12 hours) Zidovudi ne 4 mg/kg 812 hour s after birth every 12 hours 7 da ys***
HIV-positive without HIV- related signs and symptoms
3TC 150 mg every12 hours 7 da ys
Zidovudine 300 mg e ver y 12 hours 300 mg every 3 hours every 12 hours 7 da ys Zidovudi ne 4 mg/kg 812 hour s after birth every 12 hours 7 da ys***
Nevirapine 200 mg once Nevirapine 2 mg/kg within 72 hours once
ARVs during labourZidovudine 300 mg every 3 hours Zidovudi ne 4 mg/kg 812 hour s after birth every 12 hours 4 weeks
Or 600 mg
Nevirapine 200 mg once Nevirapine 2 mg/kg within 72 hours once
Only minimal rang e of AR V treatment Nevirapine 200 mg once Nevirapine 2 mg/kg within 72 hours once
* Atonset of contractions or r upture of membranes, regar dless of the pre vious schedule **Arr angefollo w-up for fur ther assessment and treatment within 2 w eeks after deliv ery *** Treat the ne wborn infant with Zido vudine for 4 w eeks if mother recei vedZi dovudine for less than 4 w eeks during pregnancy ,
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IVG10 Respond to obser ved signs or volunteered problems
RESPOND T O OBSER VED SIGNS OR VOL UNTEERED PR OBLEMS
Use this char t to manag e the woman who has a problem while taking ARVmedicines. These problems ma y be side effects of ARVmedicines or of an under lying disease.
Rule out serious pre gnancy-related diseases before assuming that these are side effects of the dr ugs.Fol low up in 2 weeks or ear lier if condition worsens. Innoimprove-
ment, refer the woman to hospital for fur ther manag ement.
SIGNS
Headache
Nausea or vomiting
Fever
Diarr hoea
Rash or blisters/ulcer s
Yel low eyes or mucus membr ane
ADVISE AND TREA T
Measure blood pr essure and manag e as inC2 and E3. IfDBP90mm giv e paracetamol for headache F4.
Measure blood pr essure and manag e as inC2 and E3. Advise to tak e medicines with food. Ifinthe first 3 m onths of pregnancy , reassure that the mor ning nausea and v omiting will disappear afte r a fe w weeks. Refer to hospit al if not passing urine.
Measure temper ature. Manageaccording toC7-C8, C10-C11ifduring pregnancy , andE6-E8ifinpostpartum period.
Advise to drink on e cup of fluid after e ver y stool. Refer to hospit al if blood in stool, not passing urine or fe ver>38C.
Ifrash is limit ed to skin, followup in 2 w eeks. Ifsever e rash, bl isters and ulcers on skin, and mouth and fe ver>38C refer to hospital for further assessment and treatment.
Refer to hospit al for fur therassessment and treatment.
IF WOMAN HAS ANY PR OBLEM
IN
FO
RM
AN
D
CO
U
N
SEL O
N
H
IV
G11 Preve nt HIV inf ection in health-care wor kersafter accidental exposure with body flu ids (P ost exposure prophyl axis)
PREVENT HIV INFECTION IN HEAL TH-CARE W ORKERS AFTER A CCIDENTAL EXPOSURE WITH BODY FLUIDS
(POST EXPOSURE PR OPHYLAXIS)
If y ou are accidentally exposed to blood or bodyfluids b y cuts
or pricks or splashes on face/e yesdothe follo wing steps:
Ifbl ood or blood y fluid splashes on intact skin, immediately wash the area with soap and water . Ifthe glo veis damag ed,wash the area with soap and water and chan gethe glo ve. Ifsplashed in the face (e ye,nose,mouth) wash with water only . Ifa f inger prick or a cut occur red during procedures such as suturing , allowthe w ound to bleed for a fe w seconds, do not squeeze out the blood. Wa sh with soap and water . Use regular w ound care. Topical antiseptics ma y be used. Check records for the HIV status of the pregnant w oman.* Ifwoman is HIV-neg ativeno fur ther action is required. Ifwoman is HIV-positiv e tak e ARV medicines within 2 hours (see na tional guidelines for choice and duration of medicine). Ifthe HIV status of the pregnant w oman is unkno wn: Startthe AR V medicine within 2 hours (see national guidelines for choice and duration ofmedicine). Explain to the w oman w hat has happened and seek her consent for rapid HIV test. DONOT test the w oman without her consent. Maintain confidentiality A2. Per formthe HIV test L6. If the w omans HIV test is neg ative, di scontinue the ARVmedicines. If the w omans HIV test is positiv e,manage the w oman as in C2/ E3 and health w orker (yourself ) should complete the ARVand be tested after 6 w eeks. Informthe super visor of the exposure type and the action tak en for the health-care w orker (yourself). Retest the health-care w orker 6 weeks after the exposure.
* If the health-care w orker (yourself) is HIV-positiv e no PEP is required. DO NO Ttest the w oman.
G8 SUPPORT THE MOTHERS CHOICE
OF INFANT FEEDING
If mother chooses replacement feeding:
Teach her replacement feeding.
Explain the risks of replacement feeding
Follow-up for replacement feeding
Give special counselling to the mother who is
HIV-positive and chooses breastfeeding
G9 GIVE APPROPRIATE
ANTIRETROVIRAL TO HIV-POSITIVE
WOMAN AND THE NEWBORN
G10 RESPOND TO OBSERVED SIGNS
AND VOLUNTEERED PROBLEMS
If a woman is taking antiretroviral medicines
and develops new signs/symptoms, respond
to her problems
G11 PREVENT HIV INFECTION IN
HEALTH-CARE WORKERS AFTER
ACCIDENTAL EXPOSURE WITH BODY
FLUIDS (POST EXPOSURE
PROPHYLAXIS)
If a health-care worker is exposed to body
fluids by cuts/pricks/splashes, give him/her
appropriate care
Use this section when accurate information on HIV must be given
to the woman and her family.
Provide key information on HIV to all women and explain at the
first antenatal care visit how HIV transmitted and the advantages
of knowing the HIV status in pregnancy G2 .
Explain about HIV testing and counselling, the implications of
the test result and benefits of involving and testing the male
partner(s). Discuss confidentiality of HIV infection G3 .
If the woman is HIV-positive:
provide additional care during pregnancy, childbirth and
postpartum G4 .
give any particular support that she may require G5 .
If antiretroviral treatment is indicated give appropriate
treatment G6
,
G9 .
Counsel the woman on infant feeding options G7 .
Support the mothers choice of infant feeding G8 .
Counsel all women on safer sex including use of condoms during
and after pregnancy G2 .
If the woman taking antiretroviral treatment is having complaints,
respond to her problems G10.
If the health-care worker is accidentally exposed to HIV infection,
give her/him appropriate care G11.
PROVIDE KEY INFORMATION ON HIV
Provide key information on HIV
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G2
What is HIV (human immunodeficiency virus)
and how is HIV transmitted?
HIV is a virus that destroys parts of the bodys immune system. A person infected with HIV may not
feel sick at first, but slowly the bodys immune system is destroyed. The person becomes ill and
unable to fight infection. Once a person is infected with HIV, she or he can give the virus to others.
HIV can be transmitted through:
Exchange of HIV-infected body fluids such as semen, vaginal fluid or blood during unprotected
sexual intercourse.
HIV-infected blood transfusions or contaminated needles.
From an infected mother to her child (MTCT) during:
pregnancy
labour and delivery
postpartum through breastfeeding.
Almost four out of 20 babies born to HIV positive women may be infected without any intervention.
HIV cannot be transmitted through hugging or mosquito bites.
A blood test is done to find out if the person is infected with HIV.
All pregnant women are offered this test. They can refuse the test.
Advantage of knowing the HIV status in pregnancy
Knowing the HIV status during pregnancy is important so that:
the woman knows her HIV status
can share information with her partner
encourage her partner to be tested
If the woman is HIV-positive she can:
get appropriate medical care to treat and/or prevent HIV-associated illnesses.
reduce the risk of transmission of infection to the baby:
by taking antiretroviral drugs in pregnancy, and during labour G6
,
G9
by practicing safer infant feeding options G9
by adapting birth and emergency plan and delivery practices G4 .
protect herself and her sexual partner(s) from infection or reinfection.
make a choice about future pregnancies.
If the woman is HIV- negative she can:
learn how to remain negative.
Counsel on safer sex including use of condoms
SAFER SEX IS ANY SEXUAL PRACTICE THAT REDUCES THE RISK OF TRANSMITTING HIV AND
SEXUALLY TRANSMITTED INFECTIONS (STIs) FROM ONE PERSON TO ANOTHER
THE BEST PROTECTION IS OBTAINED BY:
Correct and consistent use of condoms during every sexual act.
Choosing sexual activities that do not allow semen, fluid from the vagina, or blood to enter the
mouth, anus or vagina of the partner.
Reducing the number of partners.
If the woman is HIV-negative explain to her that she is at risk of HIV infection and that it is
important to remain negative during pregnancy and breastfeeding. The risk of infecting the baby
is higher if the mother is newly infected.
If the woman is HIV-positive explain to her that condom use during every sexual act during
pregnancy and breast feeding will protect her and her baby from sexually transmitted infections, or
reinfection with another HIV strain and will prevent the transmission of HIV infection to her partner.
Make sure the woman knows how to use condoms and where to get them.
HIV TESTING AND COUNSELLING
HIV testing and counselling
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G3
HIV testing and Counselling services
Explain about HIV testing:
HIV test is used to determine if the woman is infected with HIV.
It includes blood testing and counselling .
Result is available on the same day or at the next visit.
The test is offered routinely to every woman at every pregnancy to help protect her and her babys
health. She may decline the test.
If HIV testing is not available in your setting, inform the woman about:
Where to go.
How the test is performed.
How confidentiality is maintained ( see below).
When and how results are given.
When she should come back to the clinic with the test result
Costs involved.
Provide the address of HIV testing in your areas nearest site :
____________________________________________________________________
____________________________________________________________________
Ask her if she has any questions or concerns.
Discuss confidentiality of HIV infection
Assure the woman that her test result is confidential and will be shared only with herself and any
person chosen by her.
Ensure confidentiality when discussing HIV results, status, treatment and care related to HIV,
opportunistic infections, additional visits and infant feeding options A2
.
Ensure all records are confidential and kept locked away and only health care workers taking care of
her have access to the records.
DO NOT label records as HIV-positive.
Counsel on implications of the HIV test result
Discuss the HIV results when the woman is alone or with the person of her choice.
State test results in a neutral tone.
Give the woman time to express any emotions.
IF TEST RESULT IS NEGATIVE:
Explain to the woman that a negative result can mean either that she is not infected with HIV or that
she is infected with HIV but has not yet made antibodies against the virus (this is sometimes called
the window period).
Counsel on the importance of staying negative by safer sex including use of condoms G2 .
IF TEST RESULT IS POSITIVE:
Explain to the woman that a positive test result means that she is carrying the infection and has the
possibility of transmitting the infection to her unborn child without any intervention.
Let her talk about her feelings. Respond to her immediate concerns.
Inform her that she will need further assessment to determine the severity of the infection,
appropriate care and treatment needed for herself and her baby. Treatment will slow down the
progression of her HIV infection and will reduce the risk of infection to the baby.
Provide information on how to prevent HIV re-infection.
Inform her that support and counselling is available if needed, to cope on living with HIV infection.
Discuss disclosure and partner testing.
Ask the woman if she has any concerns.
Benefits of disclosure (involving) and testing the male
partner(s)
Encourage the women to disclose the HIV results to her partner or another person she trusts. By
disclosing her HIV status to her partner and family, the woman may be in a better position to:
Encourage partner to be tested for HIV.
Prevent the transmission of HIV to her partner(s).
Prevent transmission of HIV to her baby.
Protect herself from HIV reinfection.
Access HIV treatment, care and support services.
Receive support from her partner(s) and family when accessing antenatal care and HIV treatment,
care and support services.
Help to decrease the risk of suspicion and violence.
CARE AND COUNSELLING FOR THE HIV-POSITIVE WOMAN
Care and counselling for the HIV-positive woman
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G4
Additional care for the HIV- positive woman
Determine how much the woman has told her partner, labour companion and family, then
respect this confidentiality.
Be sensitive to her special concerns and fears. Give her additional support G5 .
Advise on the importance of good nutrition C13 D26.
Use standard precautions as for all women A4 .
Advise her that she is more prone to infections and should seek medical help
as soon as possible if she has:
fever
persistent diarrhoea
cold and cough respiratory infections
burning urination
vaginal itching/foul-smelling discharge
no weight gain
skin infections
foul-smelling lochia.
DURING PREGNANCY:
Revise the birth plan C2 C13.
Advise her to deliver in a facility.
Advise her to go to a facility as soon as her membranes rupture or labour starts.
Tell her to take ARV medicine at the onset of labour as instructed G6 .
Discuss the infant feeding options G8-G9 .
Modify preventive treatment for malaria, according to national strategy F4 .
DURING CHILDBIRTH:
Check if ARV is taken at onset of labour.
Give ARV medicines as prescribed G6 G9 .
Adhere to standard practice for labour and delivery.
Respect confidentiality when giving ARV to the mother and baby.
Record all ARV medicines given on labour record, postpartum record and on referral record, if
woman is referred.
DURING THE POSTPARTUM PERIOD:
Tell her that lochia can cause infection in other people and therefore she should dispose of blood
stained sanitary pads safely (list local options).
Counsel her on family planning G4 .
If not breastfeeding, advise her on breast care K8 .
Visit HIV services 2 weeks after delivery for further assessment.
Counsel the HIV-positive woman on family planning
Use the advice and counselling sections on C16 during antenatal care and D27
during postpartum
visits. The following advice should be highlighted:
Explain to the woman that future pregnancies can have significant health risks for her and
her baby. These include: transmission of HIV to the baby (during pregnancy, delivery or
breastfeeding), miscarriage, preterm labour, stillbirth, low birth weight, ectopic pregnancy and
other complications.
If she wants more children, advise that waiting at least 2 years before trying to become pregnant
again is good for the mother and for the baby's health.
Discuss her options for preventing both pregnancy and infection with other sexually transmitted
infections or HIV reinfection.
Condoms may be the best option for the woman with HIV. Counsel the woman on safer sex including
the use of condoms G2 .
If the woman think that her partner will not use condoms, she may wish to use an additional
method for pregnancy protection. However, not all methods are appropriate for the HIV-positive
woman:
Given the womans HIV status, she may not choose to breastfeed and lactational amenorrhoea
method (LAM) may not be a suitable method.
Spermicides are not recommended for HIV-positive women.
Intrauterine device (IUD) use is not recommended for women with AIDS who are not on ARV
therapy.
Due to changes in the menstrual cycle and elevated temperatures fertility awareness methods
may be difficult if the woman has AIDS or is on treatment for HIV infections.
If the woman is taking pills for tuberculosis (rifampin), she usually cannot use contraceptive pills,
monthly injectables or implants.
The family planning counsellor will provide more information.
SUPPORT TO THE HIV-POSITIVE WOMAN
Pregnant women who are HIV- positive benefit greatly from the following support after the first impact of the test result has been overcome.
Support to the HIV-positive woman
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G5
Provide emotional support to the woman
Empathize with her concerns and fears.
Use good counselling skills A2 .
Help her to assess her situation and decide which is the best option for her, her (unborn) child and
her sexual partner. Support her choice.
Connect her with other existing support services including support groups, income-
generatingactivities, religious support groups, orphan care, home care.
Help her to find ways to involve her partner and/or extended family members in sharing
responsibility, to identify a figure from the community who will support and care for her.
Discuss how to provide for the other children and help her identify a figure from the extended family
or community who will support her children.
Confirm and support information given during HIV testing and counselling, the possibility of ARV
treatment, safe sex, infant feeding and family planning advice (help her to absorb the information
and apply it in her own case).
If the woman has signs of AIDS and/or of other illness, refer her to appropriate services.
How to provide support
Conduct peer support groups for women who have HIV-infection and couples affected by HIV/AIDS:
Led by a social worker and/or woman who has come to terms with her own HIVinfection.
Establish and maintain constant linkages with other health, social and community workers support
services:
To exchange information for the coordination of interventions
To make a plan for each family involved.
Refer individuals or couples for counselling by community counsellors.
Give antiretroviral (ARV) medicine(s) to treat HIV infection
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G6
GIVE ANTIRETROVIRAL (ARV) MEDICINE(S) TO TREAT HIV INFECTION
Use these charts when starting ARV medicine(s) and to support adherence to ARV
Support the initiation of ARV
If the woman is already on ARV treatment continue the treatment during pregnancy, as prescribed. If
she is in the first trimester of pregnancy and treatment includes efavirenz, replace it with nevirapine.
If the woman is not on ARV treatment and is tested HIV-positive, choose appropriate ARV regimens
C19, G9 according to the stage of the disease.
If treatment with Zidovudine (AZT) is planned: measure haemoglobin; if less than 8 g/dl, refer to
hospital C4 .
Write the treatment plan in the Home Based Maternal Record.
Give written instructions to the woman on how to take the medicines.
Give prophylaxis for opportunistic infections according to national guidelines.
Modify preventive treatment for malaria according to national guidelines F4 .
Explore local perceptions about ARVs
Explain to the woman and family that:
ARV treatment will improve the womans health and will greatly reduce the risk of infection to her
baby. The treatment will not cure the disease.
The choice of regimen depends on the stage of the disease C19
.
If she is in early stage of HIV infection, she will need to take medicines during pregnancy,
childbirth and only for a short period after delivery to prevent mother-to-child transmission of HIV
infection (PMTCT). Progress of disease will be monitored to determine if she needs additional
treatment.
If she has mild-severe HIV disease she will need to continue the treatment even after childbirth
and postpartum period.
She may have some side effects but not all women have them. Common side effects like nausea,
diarrohea, headache or fever often occur in the beginning but they usually disappear within 23
weeks. Other side effects like yellow eyes, pallor, severe abdominal pain, shortness of breath, skin
rash, painful feet, legs or hands may appear at any time. If these signs persist, she should come to
the clinic.
Give her enough ARV tablets for 2 weeks or till her next ANC visit.
Ask the woman if she has any concerns. Discuss any incorrect perceptions.
Support adherence to ARV
For ARV medicine to be effective:
Advise woman on:
which tablets she needs to take during pregnancy, when labour begins (painful abdominal
contractions and/or membranes rupture) and after childbirth.
taking the medicine regularly, every day, at the right time. If she chooses to stop taking medicines
during pregnancy, her HIV disease could get worse and she may pass the infection to her child.
if she forgets to take a dose, she should not double the next dose.
continue the treatment during and after the childbirth (if prescribed), even if she is breastfeeding.
taking the medicine(s) with meals in order to minimize side effects.
For newborn:
Give the first dose of medicine to the newborn 812 hours after birth.
Teach the mother how to give treatment to the newborn.
Tell the mother that the baby must complete the full course of treatment and will need regular
visits throughout the infancy.
If the mother received less than 4 weeks of Zidovudine (AZT) during pregnancy, give the treatment
to the newborn for 4 weeks.
Record all treatment given. If the mother or baby is referred, write the treatment given and the
regimen prescribed on the referral card.
DO NOT label records as HIV-Positive
DO NOT share drugs with family or friends.
Counsel on infant feeding options
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G7
COUNSEL ON INFANT FEEDING OPTIONS
Explain the risks of HIV transmission through
breastfeeding and not breastfeeding
Four out of 20 babies born to known HIV-positive mothers will be infected during pregnancy and
delivery without ARV medication. Three more may be infected by breastfeeding.
The risk may be reduced if the baby is breastfed exclusively using good technique, so that the
breasts stay healthy.
Mastitis and nipple fissures increase the risk that the baby will be infected.
The risk of not breastfeeding may be much higher because replacement feeding carries risks too:
diarrhoea because of contamination from unclean water, unclean utensils or because the milk is
left out too long.
malnutrition because of insufficient quantity given to the baby, the milk is too watery, or because
of recurrent episodes of diarrhoea.
Mixed feeding increases the risk of diarrhoea. It may also increase the risk of HIV transmission.
If a woman does not know her HIV status
Counsel on the importance of exclusive breastfeeding K2 .
Encourage exclusive breastfeeding.
Counsel on the need to know the HIV status and where to go for HIV testing and counselling G3 .
Explain to her the risks of HIV transmission:
even in areas where many women have HIV, most women are negative
the risk of infecting the baby is higher if the mother is newly infected
explain that it is very important to avoid infection during pregnancy and the breastfeeding
period.
If a woman knows that she is HIV-positive
Inform her about the most appropriate infant feeding option. It will depend on her individual
circumstances, her disease status and the local situation:
Exclusive breastfeeding for 6 months, she can stop as soon as replacement feeding becomes
acceptable, feasible, affordable, sustainable and safe.
If acceptable, feasible, affordable, sustainable and safe, she might choose replacement feeding
with commercial formula.
If replacement feeding is not acceptable, feasible, affordable, sustainable and safe, she
can continue breastfeeding after 6 months and give in addition complementary foods, as
recommended for HIV-negative women and women who do not know their status.
In some situations additional possibilities are:
expressing and heat-treating her breast milk
wet nursing by an HIV-negative woman, if culturally acceptable.
Help her to assess her situation and decide which is the best option for her, and support her choice.
If the mother chooses breastfeeding, give her special counselling
G8
.
All babies receiving replacement feeding need regular follow-up, and their mothers need support to
provide correct replacement feeding.
If this cannot be ensured, exclusive breastfeeding, stopping early when replacement feeding is
feasible, is an alternative.
All babies receiving replacement feeding need regular follow-up, and their mothers need support
to provide correct replacement feeding.
Support the mothers choice of infant feeding
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G8
SUPPORT THE MOTHERS CHOICE OF INFANT FEEDING
If the mother chooses replacement feeding,
teach her replacement feeding
Ask the mother what kind of replacement feeding she chose.
For the first few feeds after delivery, prepare the formula for the mother, then teach her how to
prepare the formula and feed the baby by cup K9 :
Wash hands with water and soap
Boil the water for few minutes
Clean the cup thoroughly with water, soap and, if possible, boil or pour boiled water in it
Decide how much milk the baby needs from the instructions
Measure the milk and water and mix them
Teach the mother how to feed the baby by cup
Let the mother feed the baby 8 times a day (in the first month). Teach her to be flexible and
respond to the babys demands
If the baby does not finish the feed within 1 hour of preparation, give it to an older child or add to
cooking. DO NOT give the milk to the baby for the next feed
Wash the utensils with water and soap soon after feeding the baby
Make a new feed every time.
Give her written instructions on safe preparation of formula.
Explain the risks of replacement feeding and how to avoid them.
Advise when to seek care.
Advise about the follow-up visit.
Explain the risks of replacement feeding
Her baby may get diarrhoea if:
hands, water, or utensils are not clean
the milk stands out too long.
Her baby may not grow well if:
she/he receives too little formula each feed or too few feeds
the milk is too watery
she/he has diarrhoea.
Follow-up for replacement feeding
Ensure regular follow-up visits for growth monitoring.
Ensure the support to provide safe replacement feeding.
Advise the mother to return if:
the baby is feeding less than 6 times, or is taking smaller quantities K6
the baby has diarrhoea
there are other danger signs.
Give special counselling to the mother
who is HIV-positive and chooses breastfeeding
Support the mother in her choice of breastfeeding.
Ensure good attachment and suckling to prevent mastitis and nipple damage K3 .
Advise the mother to return immediately if:
she has any breast symptoms or signs
the baby has any difficulty feeding.
Ensure a visit in the first week to assess attachment and positioning and the condition of the
mothers breasts.
Arrange for further counselling to prepare for the possibility of stopping breastfeeding early.
Give psychosocial support G5 .
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G9
ANTIRETROVIRALS FOR HIV-POSITIVE WOMAN AND HER INFANT
Below are examples of ARV regimens. Use national guidelines for local protocols.
For longer regimens to further reduce the risk of transmission follow national guidelines.
Record the ARV medicine prescribed and given in the appropriate records facility and home-based. DO NOT write HIV-positive.
Antiretrovirals for HIV-positive woman and her infant
Woman Newborn infant
Pregnancy Labour, delivery Postpartum**
ARVs
Before
28 weeks
Starting at
28 weeks
At onset of
labour*
Until birth
of the baby
After birth
of the baby
ARVs
Dose
(syrup)
Give first
dose
Then give Duration
HIV-positive
with HIV-AIDS
related signs and
symptoms
Triple therapy Continue the ARV treatment prescribed before pregnancy. In the first trimester replace
Efavirenz with Nevirapine (200 mg once daily for 2 weeks, then every 12 hours)
Zidovudine 4 mg/kg 812 hours
after birth
every
12 hours
7 days***
HIV-positive without
HIV- related signs
and symptoms
3TC 150 mg every 12 hours 7 days
Zidovudine 300 mg every
12 hours
300 mg every
3 hours
every
12 hours
7 days Zidovudine 4 mg/kg 812 hours
after birth
every
12 hours
7 days***
Nevirapine 200 mg once Nevirapine 2 mg/kg within
72 hours
once
ARVs during labour Zidovudine 300 mg every
3 hours
Zidovudine 4 mg/kg 812 hours
after birth
every
12 hours
4 weeks
Or 600 mg
Nevirapine 200 mg once Nevirapine 2 mg/kg within
72 hours
once
Only minimal range
of ARV treatment
Nevirapine 200 mg once Nevirapine 2 mg/kg within
72 hours
once
* At onset of contractions or rupture of membranes, regardless of the previous schedule
**Arrange follow-up for further assessment and treatment within 2 weeks after delivery
*** Treat the newborn infant with Zidovudine for 4 weeks if mother received Zidovudine for less than 4 weeks during pregnancy,
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G10
Respond to observed signs or volunteered problems
RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
Use this chart to manage the woman who has a problem while taking ARV medicines. These problems may be side effects of ARV medicines or of an underlying disease.
Rule out serious pregnancy-related diseases before assuming that these are side effects of the drugs. Follow up in 2 weeks or earlier if condition worsens. In no improve-
ment, refer the woman to hospital for further management.
SIGNS
Headache
Nausea or vomiting
Fever
Diarrhoea
Rash or blisters/ulcers
Yellow eyes or mucus membrane
ADVISE AND TREAT
Measure blood pressure and manage as in C2 and E3 .
If DBP 90mm give paracetamol for headache F4 .
Measure blood pressure and manage as in C2 and E3 .
Advise to take medicines with food.
If in the first 3 months of pregnancy, reassure that the morning nausea and vomiting will
disappear after a few weeks.
Refer to hospital if not passing urine.
Measure temperature.
Manage according to C7-C8 , C10-C11 if during pregnancy, and E6-E8 if in postpartum period.
Advise to drink one cup of fluid after every stool.
Refer to hospital if blood in stool, not passing urine or fever >38C.
If rash is limited to skin, follow up in 2 weeks.
If severe rash, blisters and ulcers on skin, and mouth and fever >38C refer to hospital for
further assessment and treatment.
Refer to hospital for further assessment and treatment.
IF WOMAN HAS ANY PROBLEM
I
N
F
O
R
M
A
N
D
C
O
U
N
S
E
L
O
N
H
I
V
G11
Prevent HIV infection in health-care workers after accidental exposure with body fluids (Post exposure prophylaxis)
PREVENT HIV INFECTION IN HEALTH-CARE WORKERS AFTER ACCIDENTAL EXPOSURE WITH BODY FLUIDS
(POST EXPOSURE PROPHYLAXIS)
If you are accidentally exposed to blood or body fluids by cuts
or pricks or splashes on face/eyes do the following steps:
If blood or bloody fluid splashes on intact skin, immediately wash the area with soap and water.
If the glove is damaged, wash the area with soap and water and change the glove.
If splashed in the face (eye, nose, mouth) wash with water only.
If a finger prick or a cut occurred during procedures such as suturing, allow the wound to bleed for a few seconds,
do not squeeze out the blood. Wash with soap and water. Use regular wound care. Topical antiseptics may be used.
Check records for the HIV status of the pregnant woman.*
If woman is HIV-negative no further action is required.
If woman is HIV-positive take ARV medicines within 2 hours (see national guidelines for choice and duration of
medicine).
If the HIV status of the pregnant woman is unknown:
Start the ARV medicine within 2 hours (see national guidelines for choice and duration of medicine).
Explain to the woman what has happened and seek her consent for rapid HIV test. DO NOT test the woman
without her consent. Maintain confidentiality A2
.
Perform the HIV test L6 .
If the womans HIV test is negative, discontinue the ARV medicines.
If the womans HIV test is positive, manage the woman as in
C2
and
E3 . The health worker (yourself)
should complete the ARV treatment and be tested after 6 weeks.
Inform the supervisor of the exposure type and the action taken for the health-care worker (yourself). Retest the
health-care worker 6 weeks after the exposure.
* If the health-care worker (yourself) is HIV-positive no PEP is required. DO NOT test the woman.
The woman with special needs
T
H
E
W
O
M
A
N
W
I
T
H
S
P
E
C
I
A
L
N
E
E
D
S
H1
THE WOMAN WITH SPECIAL NEEDS
EMOTIO NAL SUPPORT FOR THE W OMAN WITH SPECIAL NEEDS
Youmay need to refer man y women to another level of care or to a suppor t group. However, ifsuch suppor t is not a vai lable, or if the woman will not seek help, counsel
her as follows. Your suppor t and willingness to listen will help her to heal.
Emotional suppor t for the woman with special needs
TH
E WO
M
AN
W
ITH
SPECIAL N
EED
SH2
Sources of suppor t
A key role of the health work er includes linking the health ser vices with the community and other suppor t ser vices a vai lable. Maintain existing links and, when possible, explore needs and alternatives for suppor t through the following: Community g roups, womensgroups, leaders. Peer suppor t groups. Ot her health ser vice pro viders. Community counsellors. Tr aditional pro viders.
Emotional suppor t
Principles of g ood care, including sugg estions on communication with the w oman and her family , are provided on A2. When giving emotional suppor t to the w oman with special needs it is par ticularly important to remember the follo wing: Cr eate a comfor table en vironment : Beaware of y our atti tude Beopen and appro achable Use a g entle, reassuring tone of v oice. Guarantee confident iality and priv acy: Communicate clea rlyabout confidentiality . Tell the w oman that y ou will not tell an yone else about the visit, di scussion or plan. Ifbrought b y a par tner, parent or other family member , makesure y ou ha vetime and space to talk priv ately. Ask the w oman if she w ould lik e to inc lude her family members in the examinat and discussion. Makesure y ou seek her consent first. Makesure the ph ysical area allo ws priv acy. Convey respect: Donot be judgmen tal Beunderstanding of her situat ion Overcome y our o wn discomfor t with her situation. Gi vesimple, direct ans wer s in clear languag e: Verify that she under stands the most impor tant points. Pr ovi de infor mation accor ding to her situation w hich she can use to mak e decisions. Bea good listener : Bepatient. Women with special needs ma y need time to tell y ou their problem or mak e a decision Pay attention to her as she speaks. Follow-up visits ma y be necessar y.
Special considerations in managing the pregnant adolescent
TH
E WO
M
AN
W
ITH
SPECIAL N
EED
S
H3
When interacting with the adolescent
Donot be judg emental. Youshould be a ware of, and over come, your own discomfor t with adolescent sexuality. Encourage the gir l to ask questions and tell her that all topics can be di scussed. Use simple and clear languag e. Repeat guarantee of confidentiality A2 G3. Understand adolescent difficulties in communicating about topics re lated to sexuality (fears of parental disco ver y,adult disappro val , social stigma, etc).
Support her w hen discussing her situation and ask if she has an y par ticular concer ns: Does she liv e with her parents, can she confide in them? Does she liv e as a couple? Is she in a long- termrelationship? Has she been subject to violence or coercion? Determine whoknowsabout this pregnancy she ma y not ha verevealed it openly . Support her concer ns related to puber ty,social acceptance, peer pressure, formi ng relationships , social stigmas and violence.
Help the gir l consider h er options and to mak e
decisions w hich best suit her needs.
Bi rthpl anning: deliv eryin a hospital or he alth centre is highly recommen ded. She needs to understand w hythis is impo rtant,she needs to decide ifshe will do it and and ho w she will a rrangeit. Pr evention of STI or HIV/AIDS is important for her and her bab y.If she or her par tner are at risk of STI or HIV/AIDS , theyshould use a condom in all sexual relations. She ma y need ad vice on ho w to discuss condom use wi th her par tner. Spacing of the next pr egnancy for bo th the w oman and bab yshealth, it is recommended thatany next pregnancy be spa ced b y at lea st 2 or 3 y ears. The gir l,with her par tner if applicable, needs to decide if and w hen a second pr egnancy is desired, based on their plans. Healthyadolescents can safely use an y contraceptiv e method. The gir l needs suppor t in kno wing her options and in deciding whi ch is best for her . Be activ e in pro viding family planning counselling and ad vice.
SPECIAL CONSIDERA TIONS IN MANA GING THE PREGNANT ADOLESCENT
Special tr aining is required to work with adolescent gir ls and this guide does not substitute for spec ial tr aining.
However, when working with an adolescent, whether mar ried or unmar ried, it is par ticularly important to remember the following.
SPECIAL CONSIDERA TIONS FOR SUPPORTING THE W OMAN LIVING WITH VIOLENCE
Violence ag ainst women b y their intimate par tners affects women s physical and mental health, including their reproductive health. While you ma y not ha ve been tr ained
to deal with this problem, women ma y disclose violence to you or you ma y see unexplained br uises and other injuries which mak e you su spectshe ma y be suffering
abuse. The following are some recommendations on how to respond and suppor t her .
The woman living with violence
TH
E WO
M
AN
W
ITH
SPECIAL N
EED
SH4
Support the w oman living with violence
Pr ovi de a space w here the w oman can speak to y ou in priv acy w here her par tner or others cannot hear.Doal l you can to guarantee confidentiality , and reassure her of this. Gently encourag e her to tell y ou what is happening to her . You ma y ask indirect qu estions to help her tell her stor y. Li sten to her in a sympathetic manner . Listening can often be of g reat suppor t. Donot blame her or makea jok e of the situation. She ma y defend her par tners action. Reassure her that she does not deserv e to be abused in an y wa y. Help her to assess her present situation. Ifshe thinks she or her ch ildren are in dang er,explore together the options to ensure her immediate safety (e.g . can she sta y with her parent s or friends? Does she ha ve,orcould she bor row, money?) Explore her options with her . Help her identify local sources of suppor t,either within her family , friends, and local community or through NGOs, shelters or social ser vices, if avai lable.Remind her that she has leg al recourse, ifrelevant. Of fer her an oppor tunity to see y ou ag ain. Violence b y par tners is complex, and she ma y be unable to resolve her situation quickly . Document an y for ms of abuse identified or concer ns y ou ma y ha vein the file.
Support the health ser vice respon se to needs of women
living with violence
Help raise a wareness among heal th care staff about violence ag ainst w omen and its pre val ence in the community the c linic ser ves. Fi nd out w hat if traini ng is a vai labl e to impro vethe suppor t that health care staff can provide to those w omen w ho ma y need it. Di splayposters, leaflets and other infor mation that condemn violence, and infor mation on g roups that can pro vide suppor t. Makecontact with org anizatio ns working to address violence in y our area. Identify those that can provide support for w omen in abusiv e relationships. Ifspecific ser vices are not a vai lable, contact other g roups such as chu rches, womensgroups, elders, orot her local g roups and discuss with them support theycan pro vide or other w hat roles the y can pla y,likeresolving disputes. Ensure y ou ha ve a list of these re sources available.
H2
EMOTIONAL SUPPORT FOR THE
WOMAN WITH SPECIAL NEEDS
Sources of support
Emotional support
H3 SPECIAL CONSIDERATIONS IN
MANAGING THE PREGNANT
ADOLESCENT
When interacting with the adolescent
Help the girl consider her options and to make
decisions which best suit her needs
H4 SPECIAL CONSIDERATIONS FOR
SUPPORTING THE WOMAN LIVING
WITH VIOLENCE
Support the woman living with violence
Support the health service response to the
needs of women living with violence
If a woman is an adolescent or living with violence, she needs
special consideration. During interaction with such women, use
this section to support them.
EMOTIONAL SUPPORT FOR THE WOMAN WITH SPECIAL NEEDS
You may need to refer many women to another level of care or to a support group. However, if such support is not available, or if the woman will not seek help, counsel
her as follows. Your support and willingness to listen will help her to heal.
Emotional support for the woman with special needs
T
H
E
W
O
M
A
N
W
I
T
H
S
P
E
C
I
A
L
N
E
E
D
S
H2
Sources of support
A key role of the health worker includes linking the health services with the community and
other support services available. Maintain existing links and, when possible, explore needs and
alternatives for support through the following:
Community groups, womens groups, leaders.
Peer support groups.
Other health service providers.
Community counsellors.
Traditional providers.
Emotional support
Principles of good care, including suggestions on communication with the woman and her family, are
provided on A2 . When giving emotional support to the woman with special needs it is particularly
important to remember the following:
Create a comfortable environment:
Be aware of your attitude
Be open and approachable
Use a gentle, reassuring tone of voice.
Guarantee confidentiality and privacy:
Communicate clearly about confidentiality. Tell the woman that you will not tell anyone else about
the visit, discussion or plan.
If brought by a partner, parent or other family member, make sure you have time and space to
talk privately. Ask the woman if she would like to include her family members in the examination
and discussion. Make sure you seek her consent first.
Make sure the physical area allows privacy.
Convey respect:
Do not be judgmental
Be understanding of her situation
Overcome your own discomfort with her situation.
Give simple, direct answers in clear language:
Verify that she understands the most important points.
Provide information according to her situation which she can use to make decisions.
Be a good listener:
Be patient. Women with special needs may need time to tell you their problem or make a
decision
Pay attention to her as she speaks.
Follow-up visits may be necessary.
Special considerations in managing the pregnant adolescent
T
H
E
W
O
M
A
N
W
I
T
H
S
P
E
C
I
A
L
N
E
E
D
S
H3
When interacting with the adolescent
Do not be judgemental. You should be aware of, and overcome, your own discomfort with adolescent
sexuality.
Encourage the girl to ask questions and tell her that all topics can be discussed.
Use simple and clear language.
Repeat guarantee of confidentiality A2
G3 .
Understand adolescent difficulties in communicating about topics related to sexuality (fears of
parental discovery, adult disapproval, social stigma, etc).
Support her when discussing her situation and ask if she has any particular concerns:
Does she live with her parents, can she confide in them? Does she live as a couple? Is she in a long-
term relationship? Has she been subject to violence or coercion?
Determine who knows about this pregnancy she may not have revealed it openly.
Support her concerns related to puberty, social acceptance, peer pressure, forming relationships,
social stigmas and violence.
Help the girl consider her options and to make
decisions which best suit her needs.
Birth planning: delivery in a hospital or health centre is highly recommended. She needs to
understand why this is important, she needs to decide if she will do it and and how she will arrange it.
Prevention of STI or HIV/AIDS is important for her and her baby. If she or her partner are at risk of
STI or HIV/AIDS, they should use a condom in all sexual relations. She may need advice on how to
discuss condom use with her partner.
Spacing of the next pregnancy for both the woman and babys health, it is recommended that any
next pregnancy be spaced by at least 2 or 3 years. The girl, with her partner if applicable, needs to
decide if and when a second pregnancy is desired, based on their plans. Healthy adolescents can
safely use any contraceptive method. The girl needs support in knowing her options and in deciding
which is best for her. Be active in providing family planning counselling and advice.
SPECIAL CONSIDERATIONS IN MANAGING THE PREGNANT ADOLESCENT
Special training is required to work with adolescent girls and this guide does not substitute for special training.
However, when working with an adolescent, whether married or unmarried, it is particularly important to remember the following.
SPECIAL CONSIDERATIONS FOR SUPPORTING THE WOMAN LIVING WITH VIOLENCE
Violence against women by their intimate partners affects womens physical and mental health, including their reproductive health. While you may not have been trained
to deal with this problem, women may disclose violence to you or you may see unexplained bruises and other injuries which make you suspect she may be suffering
abuse. The following are some recommendations on how to respond and support her.
The woman living with violence
T
H
E
W
O
M
A
N
W
I
T
H
S
P
E
C
I
A
L
N
E
E
D
S
H4
Support the woman living with violence
Provide a space where the woman can speak to you in privacy where her partner or others cannot
hear. Do all you can to guarantee confidentiality, and reassure her of this.
Gently encourage her to tell you what is happening to her. You may ask indirect questions to help her
tell her story.
Listen to her in a sympathetic manner. Listening can often be of great support. Do not blame her or
make a joke of the situation. She may defend her partners action. Reassure her that she does not
deserve to be abused in any way.
Help her to assess her present situation. If she thinks she or her children are in danger, explore
together the options to ensure her immediate safety (e.g. can she stay with her parents or friends?
Does she have, or could she borrow, money?)
Explore her options with her. Help her identify local sources of support, either within her family,
friends, and local community or through NGOs, shelters or social services, if available. Remind her
that she has legal recourse, if relevant.
Offer her an opportunity to see you again. Violence by partners is complex, and she may be unable to
resolve her situation quickly.
Document any forms of abuse identified or concerns you may have in the file.
Support the health service response to needs of women
living with violence
Help raise awareness among health care staff about violence against women and its prevalence in
the community the clinic serves.
Find out what if training is available to improve the support that health care staff can provide to
those women who may need it.
Display posters, leaflets and other information that condemn violence, and information on groups
that can provide support.
Make contact with organizations working to address violence in your area. Identify those that can
provide support for women in abusive relationships. If specific services are not available, contact
other groups such as churches, womens groups, elders, or other local groups and discuss with them
support they can provide or other what roles they can play, like resolving disputes. Ensure you have
a list of these resources available.
Community support for maternal and newborn health
C
O
M
M
U
N
I
T
Y
S
U
P
P
O
R
T
F
O
R
M
A
T
E
R
N
A
L
A
N
D
N
E
W
B
O
R
N
H
E
A
L
T
H
I1
COMMUNITY SUPPORT FOR MATERNAL AND NEWBORN HEALTH
ESTABLISH LINKS
Establish links
CO
M
M
U
N
ITY SU
PPO
RT FO
R M
A
TERN
AL AN
D
N
EW
BO
RN
H
EALTH
I2
Coordinate with other health care pro viders
and community g roups
Meet with others in the community to discuss and ag ree messag es related to pregnancy , deliver y, postpartum and post-abor tion care of w omen and ne wborns. Wo rk tog ether with leaders and community g roups to discuss the mos t common health pr oblems and find solutions. Groups to contact and establish relations w hich include: ot her health care pro viders traditional bir th attendants and healers maternity waiting homes adolescent health ser vices schools nongover nmental org anizations breastfeeding suppor t groups di strict health committees womens groups agricultural associations neighbourhood committees youth g roups church g roups. Establish links with peer suppor t groups and refer ral sites for w omen with special needs, including women living with HIV , adolescents and w omen living with violence. Ha veavailable the names and contact infor mation for these g roups and refer ral sites, and encourag e the w oman to seek their support.
Establish links with tradit ional
birthattendants and tradi tional healer s
Contact traditional bi rthattendants and healers w ho are w orking in the health facility s catchment area. Discuss ho w y ou can suppo rteach other . Respect their kno wledge, experience and influence in the community . Share with them the i nformation youhaveand lis ten to their opinions on this. Pr ovi de copies of health education mat erials that y ou distribute to community members and discuss the co them. Hav e them exp lain kno wledg e that the y share wi th the community . Together youcan create newknowledg e which is more locally appropriate. Reviewhowtogether youcan pro vide suppor t to w omen, families and g roups for mater nal and newbor n health. Invol veTBAs and healers in counselling sessions in which ad vice is giv en to families and other community members . Include TB As in meetings with community leaders and g roups. Di scuss the recommen dation that all deliv eries shoul d be perfor med b y a skilled bir th attendant. When not possible or n ot pref err ed by the w oman and her family , discuss the requirements for safe deliver y at home, postpartum care, and w hen to seek emergency care. Invite TB As to act as l abour companions for w omen the y ha vefollo wedduring pregnancy , if this is the w omans wish. Makesure TB As are in cluded in the refer ral sys tem. Cl arify ho w and w hen to refer , and pro vide TB As with feedback on w omen the y ha verefer red.
INVOL VE THE COMMUNITY IN Q UALITY OF SER VICES
Involve the community in quality of ser vices
CO
M
M
U
N
ITY SU
PPO
RT FO
R M
A
TERN
AL AN
D
N
EW
BO
RN
H
EALTH
I3
All in the community should be infor med and in volved in the process of improving the health of their members. Ask the different g roups to provide feedback and sugg estions on how to improve the ser vices the health facility provides. Fi nd out w hat people kno w about mater nal and ne wborn mortality and morbidity in their loca lity. Share data y ou ma y ha veand reflect tog ether on w hythese deaths and illnesses may occur . Discuss with them w hat families and communities can do to pre vent these deaths an d illnesses. Toget her prepare an action plan, defining responsibilities. Di scuss the different health messag es that y ou pro vide. Hav e the community m embers talk about their kno wledge in relation to these messag es.Tog ether deter mine w hat families and communities can do to suppor t mater nal and ne wborn health. Di scuss some practical wa ys in w hich families and others in the commu nity can suppor t women during pregnancy , post-abortion, deliver y and postpar tum periods: Recognition of and rapid response to emerg ency/danger signs during pregnancy , deliver y and postpartum periods Pr ovi sion of food and care for children and other family members w hen the w oman needs to be away from home during deliv ery , or when she needs to rest Accompanyin g the w oman after deliv ery Support for pa yment of fees and supplies Motivation of male par tners to help with the w orkload, accompany the w oman to the clinic, al low her to rest and ensure she eats proper ly.Motivate communication betw een males and their partner s,including discussing postpar tum family planning needs. Support the community in preparing an action plan to respond to eme rgencies. Di scuss the follo wing with them: Emergency/danger signs - kno wing w hen to seek care Importance of rapid response to emerg encies to reduce mother and newbor n death, di sability and illness Tr ansport options a vai lable, giving examples of ho w transpor t can be org anized Reasons for dela ys in seeking care and possible difficulties, including hea vy rains Wh at ser vices are a vai lable and w here Wh at options are a vai lable Costs and options for pa yment Aplan of action for responding in emerg encies, including roles and respo nsibilities.
I2
ESTABLISH LINKS
Coordinate with other health care providers
and community groups
Establish links with traditional birth attendants
and traditional healers
I3 INVOLVE THE COMMUNITY IN
QUALITY OF SERVICES
Everyone in the community should be informed and involved in the process of improving the health of their community members. This section
provides guidance on how their involvement can help improve the health of women and newborns.
Different groups should be asked to give feedback and suggestions on how to improve the services the health facilities provide.
Use the following suggestions when working with families and communities to support the care of women and newborns during pregnancy,
delivery, post-abortion and postpartum periods.
ESTABLISH LINKS
Establish links
C
O
M
M
U
N
I
T
Y
S
U
P
P
O
R
T
F
O
R
M
A
T
E
R
N
A
L
A
N
D
N
E
W
B
O
R
N
H
E
A
L
T
H
I2
Coordinate with other health care providers
and community groups
Meet with others in the community to discuss and agree messages related to pregnancy, delivery,
postpartum and post-abortion care of women and newborns.
Work together with leaders and community groups to discuss the most common health problems
and find solutions. Groups to contact and establish relations which include:
other health care providers
traditional birth attendants and healers
maternity waiting homes
adolescent health services
schools
nongovernmental organizations
breastfeeding support groups
district health committees
womens groups
agricultural associations
neighbourhood committees
youth groups
church groups.
Establish links with peer support groups and referral sites for women with special needs, including
women living with HIV, adolescents and women living with violence. Have available the names and
contact information for these groups and referral sites, and encourage the woman to seek their
support.
Establish links with traditional
birth attendants and traditional healers
Contact traditional birth attendants and healers who are working in the health facilitys catchment
area. Discuss how you can support each other.
Respect their knowledge, experience and influence in the community.
Share with them the information you have and listen to their opinions on this. Provide copies of
health education materials that you distribute to community members and discuss the content with
them. Have them explain knowledge that they share with the community. Together you can create
new knowledge which is more locally appropriate.
Review how together you can provide support to women, families and groups for maternal and
newborn health.
Involve TBAs and healers in counselling sessions in which advice is given to families and other
community members. Include TBAs in meetings with community leaders and groups.
Discuss the recommendation that all deliveries should be performed by a skilled birth attendant.
When not possible or not preferred by the woman and her family, discuss the requirements for safer
delivery at home, postpartum care, and when to seek emergency care.
Invite TBAs to act as labour companions for women they have followed during pregnancy, if this is
the womans wish.
Make sure TBAs are included in the referral system.
Clarify how and when to refer, and provide TBAs with feedback on women they have referred.
INVOLVE THE COMMUNITY IN QUALITY OF SERVICES
Involve the community in quality of services
C
O
M
M
U
N
I
T
Y
S
U
P
P
O
R
T
F
O
R
M
A
T
E
R
N
A
L
A
N
D
N
E
W
B
O
R
N
H
E
A
L
T
H
I3
All in the community should be informed and involved in the process of improving the health of
their members. Ask the different groups to provide feedback and suggestions on how to improve
the services the health facility provides.
Find out what people know about maternal and newborn mortality and morbidity in their locality.
Share data you may have and reflect together on why these deaths and illnesses may occur. Discuss
with them what families and communities can do to prevent these deaths and illnesses. Together
prepare an action plan, defining responsibilities.
Discuss the different health messages that you provide. Have the community members talk about
their knowledge in relation to these messages. Together determine what families and communities
can do to support maternal and newborn health.
Discuss some practical ways in which families and others in the community can support women
during pregnancy, post-abortion, delivery and postpartum periods:
Recognition of and rapid response to emergency/danger signs during pregnancy, delivery and
postpartum periods
Provision of food and care for children and other family members when the woman needs to be
away from home during delivery, or when she needs to rest
Accompanying the woman after delivery
Support for payment of fees and supplies
Motivation of male partners to help with the workload, accompany the woman to the clinic, allow
her to rest and ensure she eats properly. Motivate communication between males and their
partners, including discussing postpartum family planning needs.
Support the community in preparing an action plan to respond to emergencies. Discuss the following
with them:
Emergency/danger signs - knowing when to seek care
Importance of rapid response to emergencies to reduce mother and newborn death, disability and
illness
Transport options available, giving examples of how transport can be organized
Reasons for delays in seeking care and possible difficulties, including heavy rains
What services are available and where
What options are available
Costs and options for payment
A plan of action for responding in emergencies, including roles and responsibilities.
Newborn care
N
E
W
B
O
R
N
C
A
R
E
J1
NEWBORN CARE
Examine the ne wborn
N
EW
BO
RN
CARE
ASK, CHECK RECORD
Check mater nal and newborn record or ask the mother : How old is the bab y? Pr eterm(less than 37 w eeks or 1 month or more ear ly)? Breech bir th? Di fficult bir th? Resuscitated at bir th? Has bab y had con vulsions?
Ask the mother : Doyou ha veconcerns? How is the bab y feeding?
Is the mother ver y ill or tr ansferr ed?
LOOK, LISTEN, FEEL
Assess breathing (bab y must be calm) listen for g runting count breaths: are the y 60 or less per minute? Repeat the count if ele vat ed look at the chest for in- drawing . Look at the mo vements: are theynormal and symmetrical? Look at the presenting par t isthere s wel ling and br uises? Look at abdomen for pall or. Look for malfor mations. Feel the tone: is it nor mal? Feel for war mth. If cold, or verywarm, measure temperature. We igh the bab y.
SIGNS
Normal weight bab y (2500-g or more). Feeding w ell suckling effectiv ely 8 times in 24 hour s,dayand night. Nodanger signs. Nospecial treatment needs or treatment completed. Small bab y,feeding w ell and g aining wei ght adequately .
Bodytemperature 35-36.4C.
Mother not able to breastfeed due to receiving specia l treatment. Mother transfer red.
TREAT AND AD VISE
If first exami nation: Ensure care for the ne wbornJ10. Examine ag ain for discharg e.
If pre-disch argeexaminati on: Immunize if dueK13. Advise on bab y careK2 K9-K10. Advise on routin e visi t at ag e 3-7 da ysK14. Advise on w hen to retur n if dang er signsK14. Record in home-ba sed record. Iffurther visits, repeat ad vices.
Re-warmthe bab y skin-to-skin K9. Iftemperature not risi ng after 2 hours, reassess the bab y.
Help the mother express b reast milkK5. Consider alter native feeding methods until mother i wel l K5-K6. Pr ovi de care for the bab y,ensure warmth K9. Ensure mothe r can see the baby regul arly . Tr ansfer the bab y with the mother if possible. Ensure care for the bab y at home.
CLASSIFY
WELL BABY
MILD HYPOTHERMIA
MOTHER NOTABLE TOTAKE CARE FOR B ABY
NEXT : If preter m,birthwei ght <2500 g or twin
EXAMINE THE NEWBORN
Use this char t to assess the newbor n after bir th,classify and treat, possibly around an hour ; for discharg e (not before 12 hours); and during the firs t week of life at rou-
tine, follow-up, or sick newbor n visit. Record the findings on the postpar tum record N6.
Alwa ys examine the bab y in the presence of the mother .
J2
If preter m,birthweight <2500 g or twin
ASK, CHECK RECORD
Babyjust bor n. Bi rthweight <1500-g 1500-g to <2500-g . Pr eterm <32 weeks 33-36 w eeks. Twin.
LOOK, LISTEN, FEEL
Ifthis is repeated visit, assess w eight g ain
SIGNS
Bi rthweight <1500-g . Verypreter m <32 w eeks or >2 months ear ly).
Bi rthweight 1500-g-2500-g . Pr etermbaby (32-36 w eeks or 1-2 months ear ly). Sever al da ys old and wei ght g ain inadequate. Feeding difficulty .
Twin
TREAT AND AD VISE
Refer bab y urg ently to hospital K14. Ensure extr a war mth duri ng refer ral.
Gi vespecial support to breastfeed the small babyK4. Ensure addit ional care for a small bab yJ11. ReassessdailyJ11. Donot discha rgebefore feedin g well,gai ning w eight and bod y temperat ure stable. Iffeedingdifficulties persist for 3 da ys and otherwis e well,refer for breastfeeding counse lling.
Gi vespecial support to the mother to breastfeed twinsK4. Donot discharg e until both twins can g o home.
CLASSIFY
VERYSMALL BABY
SMALL BABY
TWIN
IF PRETERM, BIRTH WEIGHT <2500-G OR TWIN
N
EW
BO
RN
CARE
J3
NEXT : Assess breastfeeding
Assess breastf eeding
N
EW
BO
RN
CARE
ASK,CHECK RECORD
Ask the mother How is the breastfeeding g oing? Has your bab y fed in the pre vious hour? Isthere an y difficulty? Isyour bab y satisfied with the feed? Haveyoufed your bab y any other foods or drinks? How do y our breasts feel? Doyou ha veanyconcerns?
If bab y more than one da y old: How man y times has y our bab y fed in 24 hours?
Toassess replacement feeding see J12.
LOOK, LISTEN, FEEL
Observea breastfeed. If the bab y has not fed in th e pre vious hour, ask the mother to put the baby on her breasts and obs erve breastfeeding for about 5 minu tes.
Look Isthe bab y able to attach corr ectly? Isthe bab y well-positioned? Isthe bab y suckling effecti vel y?
If mother has fed in the last hour, ask her to tell y ou when her bab y is willing to feed ag ain.
SIGNS
Suckling effectiv ely. Breastfeeding 8 times in 24 hours on demand da y and night
Not yet breastfed (first hou rs of life). Not well attached. Not suckling effec tively . Breastfeeding less than 8 times per 24 hours. Receiving other foods or drinks. Sever al da ys old and inadequate wei ght g ain.
Not suckling (afte r 6 hours of ag e). Stopped feeding .
TREAT AND AD VISE
Encourag e the mo ther to continue breastfeeding o demandK3.
Support exclusive breastfee dingK2-K3. Help the mother to initiate breastfeed ingK3. Teach cor rect positioning and attachment K3. Advise to feed more freque ntly, day and night. Reassure her that she has enough milk. Advise the mother tostop feeding the bab y other foods or drinks. Reassess at the next feed or follo w-up visit in2 days.
Refer bab y urg ently to hospital K14.
CLASSIFY
FEEDING WELL
FEEDING DIFFIC ULTY
NOTABLE T O FEED
NEXT : Check for special treatment needs
ASSESS BREASTFEEDING
Assess breastfeeding in ever y bab y as par t of the examination.
If mother is complaining of nipple or breast pain, also assess the mother s breastsJ9.
J4
Check for special treatment needs
ASK, CHECK RECORD
Check record for special treatment needs Has the mother had within 2 da ys of deliv ery: fever >38C? infection treated with antibiotics? Membranes r uptured >18 hours before deliv ery? Mother tested RPR-positiv e? Mother tested HIV-positiv e? isorhas been on ARV has she receiv ed infant feeding counselling? Isthe mother receiving TB treatment whi ch beg an <2 months ag o?
LOOK, LISTEN, FEEL SIGNS
Baby<1 da y old and membran es ruptured >18 hours before deliv ery , or Mother being treated with antibiotics for infection, or Mother has fe ver>38C.
Mother tested RPR-positiv e.
Mother kno wn to be HIV-positiv e. Mother has not been counselled on infant feeding . Mother chose breastfeeding . Mother chose replacement feedin g.
Mother star ted TB treatment <2 months before deliv ery .
TREAT AND AD VISE
Gi vebaby 2 IM antibiotics for 5 da ysK12. Assess bab y dailyJ2-J7.
Gi vebaby single dose of benzathine penicillin K12. Ensure mothe r and par tner are treated F6. Followup in 2 w eeks.
Gi veARVto the ne wbornG9. Informon infant feeding options G7. Gi vespecial counselling to mother w ho is breast feedingG8. Teach the mother replacement feeding . Followup in 2 w eeksG8.
Gi vebaby isoniazid prop ylaxis for 6 months K13. Gi veBCG v accination to the bab y only w hen bab ys treatment completed. Followup in 2 w eeks.
CLASSIFY
RISK OF BACTERIA L INFECTIO N
RISK OF CONGENITAL SYPHILIS
RISK OF HIV TRANSMIS SION
RISK OF TUBERCULOSIS
NEXT : Look for signs of jaundice and local infection
CHECK FOR SPECIAL TREATMENT NEEDS
N
EW
BO
RN
CARE
J5
Look for signs of jaundice and local inf ection
N
EW
BO
RN
CARE
ASK, CHECK RECORD
Wh at has been applied to the umbilicus?
LOOK, LISTEN, FEEL
Look at the skin, isityellow? if bab y is less than 24 hours old, look at skin on the face if bab y is 24 hours old or more, look at palms and soles. Look at the e yes. Are the y swol len and draining pus? Look at the skin, especially around the neck, armpits, inguinal area: Are there skin pustules? Is there s wel ling, hardness or largebullae? Look at the umbilicus: Is it red? Draining pus? Does redness extend to the skin?
SIGNS
Yellowskin on face and only24 hours old. Yellowpalms and soles and >24 hours old.
Eyes swol len and draining pus.
Red umbilicus or sk in around it.
Less than 10 pustules
TREAT AND AD VISE
Refer bab y urg ently to hospital K14. Encourag e breas tfeeding on the wa y. Iffeeding difficu lty, gi veexpressed breast milk b y cupK6.
Gi vesingle dose of appro priate antibiotic for e ye infection K12. Teach mother to treat e yesK13. Followup in 2 da ys.If no impro vement or w orse, refer urg ently to hospital. Assess and treat motherand her par tner for possible gonorr heaE8.
Teach mother to treat umbilical infection K13. Ifnoimprov ement in 2 da ys,or if w orse, refe r urgentl y to hospital.
Teach mother to treat skin infection K13. Followup in 2 da ys. Ifnoimprov ement of pustules in 2 da ys or more, refer urg ently to hospital.
CLASSIFY
JAUNDICE
GONOCOC CAL EYE INFECTI ON
LOCAL UMBILICAL INFECTION
LOCAL SKIN INFECTION
NEXT : If dang er signs
LOOK FOR SIGNS OF J AUNDICE AND LOCAL INFECTION
J6
If danger signs
SIGNS
Anyof the following sig ns: Fast breathing (more than 60 breaths per minute). Slowbreathing (less than 30 breaths per minute). Sever e chest in-dra wing Grunting Convulsions. Fl oppy or stiff. Fever(temperature >38C). Temperature <35C or not rising after re warming . Umbilicus draining pus or umbilical redness extending to skin. More than 10 skin pustules or bullae, orswelling, redness, hardness of skin. Bl eeding from stump or cut.
TREAT AND AD VISE
Gi vefirst dose of 2 IM a ntibiotics K12. Refer bab y urg ently to hospital K14.
In additio n: Re-warmand k eep war m during refer ralK9.
Tr eat local umbili cal infection before refer ralK13.
Tr eat skin inf ection before refer ralK13.
Stop the bleeding .
CLASSIFY
POSSIBLE SERIOUS ILLNESS
NEXT : If swel ling, bruises or malfor mation
IF DANGER SIGNS
N
EW
BO
RN
CARE
J7
J2
EXAMINE THE NEWBORN
J3
IF PRETERM,
BIRTH WEIGHT <2500 G OR TWIN
J4 ASSESS BREASTFEEDING
J5 CHECK FOR SPECIAL
TREATMENT NEEDS
J6 LOOK FOR SIGNS OF JAUNDICE AND
LOCAL INFECTION
J7 IF DANGER SIGNS
If swelling , brui ses or malfor mation
N
EW
BO
RN
CARE
SIGNS
Bruises, swelling on buttocks. Swollen head bump on one or both sides. Abnormal position of legs (after breech presentation). Asymmetrical ar m mo vement, armdoes not mo ve.
Cl ub foot
Cl eft palate or lip
Odd looking , unusual appearance
Open tissue on head, abdomen or back
Ot her abnor mal appearance.
TREAT AND AD VISE
Explain to parents that it does not hur t the bab y, it will disappear in a w eek or tw o and no special treatment is needed. DONOT force legs into a different position. Gently handle the limb that is not mo ving, do not pul l.
Refer for special treatment if a vai lable.
Help mother to breastfeed. Ifnot successful, teach her alter native feeding methods K5-K6. Plan to follo w up. Advise on surgical cor rection at ag e of se ver al months.
Refer for special e val uation.
Coverwi th ster ile tissues soak ed with sterile saline solution before refer ral. Refer for special treatment if a vai lable.
Manageaccording to national guidelines.
CLASSIFY
BIRTH INJUR Y
MALFORMA TION
SEVERE MALFORMA TION
NEXT : Assess the mother s breasts if complaining of nipple or breast pain
IF SWELLING, BRUISES OR MALFORMA TION
J8
NEXT : Care of the ne wborn
Assess the mother s breasts if complaining of nipple or breast pain
ASK, CHECK RECORD
How do y our breasts feel?
LOOK, LISTEN, FEEL
Look at the nipple for fiss ure Look at the breasts for : swelling shininess redness. Feel gently for painful par t of the breast. Measure temperature. Observ e a breastfeed if not y et doneJ4.
SIGNS
Noswelling, redness or tender ness. Normal bod y temperature. Ni pple not sore and no fissure visible. Babywel l attached.
Ni pple sore or fissured. Babynot w ell attached.
Both breasts are s wol len, shinyand patch y red. Temperature <38C. Babynot w ell attached. Not yet breastfeeding .
Partof breast is painful, swol len and red. Temperature >38C Feels ill.
TREAT AND AD VISE
Reassure the mother .
Encourag e the mo ther to continue breastfeeding . Teach cor rect positioning and attachment K3. Reassessafter 2 feeds (or 1 da y).If not bet ter, teach the mother ho w to express breast milk from the affected breast and feed bab y by cup, and continue breastfeeding on the health y side.
Encourag e the mo ther to continue breastfeeding . Teach cor rect positioning and attachment K3. Advise to feed more freque ntly. Reassessafter 2 feeds (1 da y).If not better , teach mother howto express enough breast milk before the feed to relie vediscomfor t K5.
Encourag e mothe r to continue breastfeeding . Teach cor rect positioning and attachment K3. Gi vecloxacil lin for 10 da ys F5. Reassessin2 days. If no impro vement or w orse, refer to hospital. Ifmother is HIV+ let her breas tfeed on the health y breast. Express milk from the affected breast and discard until no fe verK5. Ifsever e pain, gi veparacetamol F4.
CLASSIFY
BREASTS HEALTHY
NIPPLE SORENESS OR FISSURE
BREAST ENGORGEMEN T
MASTITIS
ASSESS THE MOTHERS BREASTS IF COMPLAINING OF NI PPLE OR BREAST P AIN
N
EW
BO
RN
CARE
J9
CARE OF THE NEWB ORN
Use this char t for care of all babies until discharg e.
Care of the ne wborn
N
EW
BO
RN
CARE
J10
CARE AND MONITORING
Ensure the room is war m (not less than 25C and no draught). Keep the bab y in the room with the mother , in her bed or within easy reach. Let the mother and bab y sleep under a bednet.
Support exclusive breastfeeding on demand da y and night. Ask the mother to aler t you if breastfeeding difficulty . Assess breastfeeding in e ver y bab y before planning for discharg e. DO NO Tdi scharge if bab y is not y et feeding w ell.
Teach the mother ho w to care for the bab y. Keep the bab y war mK9 Givecord care K10 Ensure h ygiene K10. DO NO Texpose the bab y in direct sun. DO NO Tput the bab y on an y cold surface. DO NO Tbath the bab y before 6 hours.
Ask the mother and companion to watch the bab y and aler t you if Feet cold Breathing difficulty: g runting, fast or slo w breathing , chest in-dra wing Anybleeding.
Gi veprescribed treatments according to the schedule K12.
Examine e ver y bab y before planning to discharg e mother and bab y J2-J9. DO NO Tdi scharge before bab y is 12 hours old.
RESPOND T O ABNORM AL FINDING S
Ifthe bab y is in a cot , ensure bab y is dressed or wrapped and co ver ed by a blank et. Cov er the head with a hat.
Ifmother repor ts breastfeeding difficulty , assess breastfeeding and help the mother with positioning and attachment J3
Ifthe mother is una ble to tak e care o f the bab y,provide care or teach the companion K9-K10 Wa sh hands before a nd after handling the bab y.
Iffeet are cold: Teach the mother to put the bab y skin-to-skin K13. Reassess in 1 hour; if feet still cold, measuretemperat ure and re-war m the bab y K9. Ifbl eeding from cord, check if tie is loose and retie the cord. Ifot her bleeding , assess the bab y immediately J2-J7. Ifbreathing difficult y or mother repor ts an y other abnormali ty,examine the bab y as onJ2-J7.
NEXT : Additional care of a small bab y (or twin)
ADDITIONAL CARE OF A SMALL BABY (OR TWIN)
Use this char t for additional care of a small bab y: preter m,1-2 months ear ly or weighing 1500g- <2500g. Refer to hospital a ver y small bab y: >2 months ear ly,weighing
<1500-g
Additional care of a small baby (twin)
N
EW
BO
RN
CARE
J11
CARE AND MONITORING
Pl an to k eep the small bab y long er before discharging . Al lowvisits to the mother and bab y.
Gi vespecial suppor t for breastfeeding the small bab y (or twins) K4: Encourage the mother to breastfeed e ver y 2-3 hours. Assess breastfeeding daily: attachment, suckling, duration and frequency of feeds, and bab y satisfaction with the feed J4 K6. If alter native feeding method is used, assess the total daily amount of milk giv en. Wei gh daily and assess w eight g ainK7.
Ensure additional war mth for the small bab y K9: Ensure the room is v erywarm(2528C). Teach the mother ho w to k eep the small bab y war m in skin-to-skin contact Provide extra blank ets for mother and bab y. Ensure h ygieneK10. DO NO Tbath the small bab y.Was h as needed.
Assess the small bab y daily: Measure temperature Assess breathing (bab y must be quiet, not cr ying): listen for g runting; count breaths per minute, repeat the count if >60 or <30; look for chest in-dra wing Look for jaundice (first 10 da ys of life): first 24 hours on the abdom en,then on palms and soles.
Pl an to discharg e when: Breastfeeding w ell Gaining w eight adequately on 3 consecutiv e days Bodytemperature betw een 36.5 and 37.5C on 3 consecutiv e days Mother able and confident in caring for the bab y No mater nal concer ns. Assess the bab y for discharg e.
RESPONSE T O ABNORMAL FI NDINGS
Ifthe small bab y is not suckling effectiv ely and does not ha veother dang er sign s,consider alternativ e feeding me thodsK5-K6. Teach the mother ho w to hand express b reast milkdirectly into the bab ysmouthK5 Teach the mother to express breast milk and cup feed the bab y K5-K6 Determine appropriate amount for daily feeds b y ag e K6. Iffeeding difficulty p ersists for 3 da ys,or weight loss g reater than 10% of bir th weight and no other problems, refer for breastfeeding counselling and manag ement.
Ifdi fficult to k eep bod y temperature within the nor mal rang e (36.5C to 37.5C): Keep the bab y in sk in-to-skin contact with the mother as much as possible If bod y temperature belo w 36.5C persists for 2 hours despite skin-to-skin contact with mo , assess the bab y J2-J8. Ifbreathing difficult y,assess the bab y J2-J8. Ifjaundice, refer the bab y for phototherap y. Ifany mater nal concer n,assess the bab y and respond to the mother J2-J8.
Ifthe mother and ba byare not able tostay,ensure daily (home) visits or send to hospital.
N
EW
BO
RN
CARE
J12 Assess replacement f eeding
ASSESS REPLA CEMENT FEEDING
If mother chose replacement feeding assess the feeding in ever y bab y as par t of the examination.
Advise the mother on how to relieve eng orgement K8. If mother is complaining of breast pain, also assess the mother s breasts J9.
ASK, CHECK RECORD
Ask the mother Wh at are y ou feeding the bab y? How are y ou feeding y our bab y? Has your bab y fed in the pre vious hour? Isthere an y difficulty? How much milk is bab y taking per feed? Isyour bab y satisfied with the feed? Haveyoufed your bab y an y other foods or drinks? Doyou ha veanyconcerns?
If bab y more than one da y old: How man y times has y our bab y fed in 24 hours? How much milk is bab y taking per day?
How do y our breasts feel?
LOOK, LISTEN, FEEL
Observe a feed Ifthe bab y has not fed in the previous hour, ask the mother to feed the bab y and obser vefeeding for about 5 minutes. Ask her to prepare the feed.
Look Isshe holding the cup to the bab ys lips? Isthe bab y aler t,opens e yesand mouth? Isthe bab y sucking and s wallowing the milk effectiv ely,spilling little?
If mother has fed in the last hour, ask her to tell y ou when her bab y is willing to feed ag ain.
SIGNS
Sucking and s wallowing adequate amount of milk, spilling little. Feeding 8 times in 24 hours on demand da y and night.
Not yet fed (first 6 hours of life). Not fed b y cup. Not sucking and s wallowing effectively , spilling Not feeding adequa te amount per da y. Feeding less than 8 times per 24 hours. Receiving other foods or drinks. Sever al da ys old and inadequate wei ght g ain.
Not sucking (after 6 hours of ag e). Stopped feeding .
TREAT AND AD VISE
Encourag e the mo ther to continue feeding b y cup on demandK6.
Teach the mother replacement feeding G8. Teach the mother cup feeding K6. Advise to feed more freque ntly, ondemand, dayand night. Advise the mother tostop feeding the bab y other foods or drin ks or b y bottle. Reassessatthe next feed or follo w-up visit in 2 da ys.
Refer bab y urg ently to hospital K14.
CLASSIFY
FEEDING WELL
FEEDING DIFFIC ULTY
NOTABLE T O FEED
J8 IF SWELLING, BRUISES OR
MALFORMATION
J9 ASSESS THE MOTHERS BREASTS IF
COMPLAINING OF NIPPLE OR
BREAST PAIN
J10 CARE OF THE NEWBORN
J11 ADDITIONAL CARE OF A
SMALL BABY (OR TWIN)
J12 ASSESS REPLACEMENT FEEDING
Examinine routinely all babies around an hour of birth, for
discharge, at routine and follow-up postnatal visits in the first weeks
of life, and when the provider or mother observes danger signs.
Use the chart Assess the mothers breasts if the mother is
complaining of nipple or breast pain J9 .
During the stay at the facility, use the Care of the newborn chart
J10 . If the baby is small but does not need referral, also use the
Additional care for a small baby or twin chart J11 .
Use the Breastfeeding, care, preventive measures and treatment
for the newborn sections for details of care, resuscitation and
treatments K1-K13 .
Use Advise on when to return with the baby K14 for advising the
mother when to return with the baby for routine and follow-up
visits and to seek care or return if baby has danger signs. Use
information and counselling sheets M5-M6 .
For care at birth and during the first hours of life, use Labour and
delivery D19.
ALSO SEE:
Counsel on choices of infant feeding and HIV-related issues G7-G8 .
Equipment, supplies and drugs L1-L5 .
Records N1-N7 .
Baby died D24.
Examine the newborn
N
E
W
B
O
R
N
C
A
R
E
ASK, CHECK RECORD
Check maternal and
newborn record or ask
the mother:
How old is the baby?
Preterm (less than 37 weeks
or 1 month or more early)?
Breech birth?
Difficult birth?
Resuscitated at birth?
Has baby had convulsions?
Ask the mother:
Do you have concerns?
How is the baby feeding?
Is the mother very ill or transferred?
LOOK, LISTEN, FEEL
Assess breathing (baby must be
calm)
listen for grunting
count breaths: are they 30-60
per minute? Repeat the count
if elevated
look at the chest for in-drawing.
Look at the movements: are
they normal and symmetrical?
Look at the presenting part
is there swelling and bruises?
Look at abdomen for pallor.
Look for malformations.
Feel the tone: is it normal?
Feel for warmth. If cold, or
very warm, measure temperature.
Weigh the baby.
SIGNS
Normal weight baby
(2500-g or more).
Feeding well suckling effectively
8 times in 24 hours, day and night.
No danger signs.
No special treatment needs or
treatment completed.
Small baby, feeding well and gaining
weight adequately.
Body temperature
35-36.4C.
Mother not able to breastfeed
due to receiving special
treatment.
Mother transferred.
TREAT AND ADVISE
If first examination:
Ensure care for the newborn J10 .
Examine again for discharge.
If pre-discharge examination:
Immunize if due K13.
Advise on baby care K2 K9-K10 .
Advise on routine visit at age 3-7 days K14.
Advise on when to return if danger
signs K14.
Record in home-based record.
If further visits, repeat advices.
Re-warm the baby skin-to-skin K9 .
If temperature not rising after 2 hours, reassess
the baby.
Help the mother express breast milk K5 .
Consider alternative feeding methods until mother is
well K5-K6 .
Provide care for the baby, ensure warmth K9 .
Ensure mother can see the baby regularly.
Transfer the baby with the mother if possible.
Ensure care for the baby at home.
CLASSIFY
WELL BABY
MILD
HYPOTHERMIA
MOTHER NOT ABLE
TO TAKE CARE FOR BABY
NEXT: If preterm, birth weight <2500 g or twin
EXAMINE THE NEWBORN
Use this chart to assess the newborn after birth, classify and treat, possibly around an hour; for discharge (not before 12 hours); and during the first week of life at rou-
tine, follow-up, or sick newborn visit. Record the findings on the postpartum record N6 .
Always examine the baby in the presence of the mother.
J2
If preterm, birth weight <2500 g or twin
ASK, CHECK RECORD
Baby just born.
Birth weight
<1500-g
1500-g to <2500-g.
Preterm
<32 weeks
33-36 weeks.
Twin.
LOOK, LISTEN, FEEL
If this is repeated visit,
assess weight gain
SIGNS
Birth weight <1500g.
Very preterm <32 weeks
or >2 months early).
Birth weight 1500g-<2500g.
Preterm baby (32-36 weeks
or 1-2 months early).
Several days old and
weight gain inadequate.
Feeding difficulty.
Twin
TREAT AND ADVISE
Refer baby urgently to hospital K14.
Ensure extra warmth during referral.
Give special support to breastfeed the
small baby K4 .
Ensure additional care for a small baby J11 .
Reassess daily J11 .
Do not discharge before feeding well, gaining weight
and body temperature stable.
If feeding difficulties persist for 3 days and
otherwise well, refer for breastfeeding counselling.
Give special support to the mother to breastfeed
twins K4 .
Do not discharge until both twins can go home.
CLASSIFY
VERY SMALL BABY
SMALL BABY
TWIN
IF PRETERM, BIRTH WEIGHT <2500-G OR TWIN
N
E
W
B
O
R
N
C
A
R
E
J3
NEXT: Assess breastfeeding
Assess breastfeeding
N
E
W
B
O
R
N
C
A
R
E
ASK,CHECK RECORD
Ask the mother
How is the breastfeeding going?
Has your baby fed in the previous
hour?
Is there any difficulty?
Is your baby satisfied with the feed?
Have you fed your baby any other
foods or drinks?
How do your breasts feel?
Do you have any concerns?
If baby more than one day old:
How many times has your baby fed
in 24 hours?
To assess replacement feeding see J12
.
LOOK, LISTEN, FEEL
Observe a breastfeed.
If the baby has not fed in the previous
hour, ask the mother to put the
baby on her breasts and observe
breastfeeding for about 5 minutes.
Look
Is the baby able to attach correctly?
Is the baby well-positioned?
Is the baby suckling effectively?
If mother has fed in the last hour, ask
her to tell you when her baby is willing
to feed again.
SIGNS
Suckling effectively.
Breastfeeding 8 times in 24 hours
on demand day and night
Not yet breastfed (first hours of life).
Not well attached.
Not suckling effectively.
Breastfeeding less than 8 times per
24 hours.
Receiving other foods or drinks.
Several days old and inadequate
weight gain.
Not suckling (after 6 hours of age).
Stopped feeding.
TREAT AND ADVISE
Encourage the mother to continue breastfeeding on
demand K3 .
Support exclusive breastfeeding K2-K3 .
Help the mother to initiate breastfeeding K3 .
Teach correct positioning and attachment K3 .
Advise to feed more frequently, day and night.
Reassure her that she has enough milk.
Advise the mother to stop feeding the baby other
foods or drinks.
Reassess at the next feed or follow-up visit in 2 days.
Refer baby urgently to hospital K14.
CLASSIFY
FEEDING WELL
FEEDING DIFFICULTY
NOT ABLE TO FEED
NEXT: Check for special treatment needs
ASSESS BREASTFEEDING
Assess breastfeeding in every baby as part of the examination.
If mother is complaining of nipple or breast pain, also assess the mothers breasts J9 .
J4
Check for special treatment needs
ASK, CHECK RECORD
Check record for
special treatment needs
Has the mother had
within 2 days of delivery:
fever >38C?
infection treated with antibiotics?
Membranes ruptured >18 hours
before delivery?
Mother tested RPR-positive?
Mother tested HIV-positive?
is or has been on ARV
has she received
infant feeding counselling?
Is the mother receiving TB treatment
which began <2 months ago?
LOOK, LISTEN, FEEL SIGNS
Baby <1 day old and membranes
ruptured >18 hours before delivery,
or
Mother being treated with
antibiotics for infection,
or
Mother has fever >38C.
Mother tested RPR-positive.
Mother known to be HIV-positive.
Mother has not been
counselled on infant feeding.
Mother chose breastfeeding.
Mother chose replacement feeding.
Mother started TB treatment
<2 months before delivery.
TREAT AND ADVISE
Give baby 2 IM antibiotics for 5 days K12.
Assess baby daily J2-J7 .
Give baby single dose of benzathine penicillin K12.
Ensure mother and partner are treated F6 .
Follow up in 2 weeks.
Give ARV to the newborn G9
.
Counsel on infant feeding options G7
.
Give special counselling to mother who is breast
feeding G8
.
Teach the mother replacement feeding.
Follow up in 2 weeks G8
.
Give baby isoniazid propylaxis for 6 months K13.
Give BCG vaccination to the baby only when babys
treatment completed.
Follow up in 2 weeks.
CLASSIFY
RISK OF
BACTERIAL INFECTION
RISK OF
CONGENITAL SYPHILIS
RISK OF
HIV TRANSMISSION
RISK OF
TUBERCULOSIS
NEXT: Look for signs of jaundice and local infection
CHECK FOR SPECIAL TREATMENT NEEDS
N
E
W
B
O
R
N
C
A
R
E
J5
Look for signs of jaundice and local infection
N
E
W
B
O
R
N
C
A
R
E
ASK, CHECK RECORD
What has been applied to the
umbilicus?
LOOK, LISTEN, FEEL
Look at the skin, is it yellow?
if baby is less than 24 hours old,
look at skin on the face
if baby is 24 hours old or more,
look at palms and soles.
Look at the eyes. Are they swollen
and draining pus?
Look at the skin, especially around
the neck, armpits, inguinal area:
Are there skin pustules?
Is there swelling, hardness or
large bullae?
Look at the umbilicus:
Is it red?
Draining pus?
Does redness extend to the skin?
SIGNS
Yellow skin on face and
only <24 hours old.
Yellow palms and soles and
24 hours old.
Eyes swollen and draining pus.
Red umbilicus or skin around it.
Less than 10 pustules
TREAT AND ADVISE
Refer baby urgently to hospital K14.
Encourage breastfeeding on the way.
If feeding difficulty, give expressed breast milk by cup K6 .
Give single dose of appropriate antibiotic for eye
infection K12.
Teach mother to treat eyes K13.
Follow up in 2 days. If no improvement or worse,
refer urgently to hospital.
Assess and treat mother and her partner for possible
gonorrhea E8 .
Teach mother to treat umbilical infection K13.
If no improvement in 2 days, or if worse, refer
urgently to hospital.
Teach mother to treat skin infection K13.
Follow up in 2 days.
If no improvement of pustules in 2 days or more,
refer urgently to hospital.
CLASSIFY
JAUNDICE
GONOCOCCAL
EYE INFECTION
LOCAL
UMBILICAL
INFECTION
LOCAL SKIN
INFECTION
NEXT: If danger signs
LOOK FOR SIGNS OF JAUNDICE AND LOCAL INFECTION
J6
If danger signs
SIGNS
Any of the following signs:
Fast breathing
(more than 60 breaths per minute).
Slow breathing
(less than 30 breaths per minute).
Severe chest in-drawing
Grunting
Convulsions.
Floppy or stiff.
Fever (temperature >38C).
Temperature <35C or not rising
after rewarming.
Umbilicus draining pus or umbilical
redness and swelling extending to
skin
More than 10 skin pustules
or bullae, or swelling, redness,
hardness of skin.
Bleeding from stump or cut.
Pallor.
TREAT AND ADVISE
Give first dose of 2 IM antibiotics K12.
Refer baby urgently to hospital K14.
In addition:
Re-warm and keep warm during referral K9 .
Treat local umbilical infection before referral K13.
Treat skin infection before referral K13.
Stop the bleeding.
CLASSIFY
POSSIBLE
SERIOUS
ILLNESS
NEXT: If swelling, bruises or malformation
IF DANGER SIGNS
N
E
W
B
O
R
N
C
A
R
E
J7
If swelling, bruises or malformation
N
E
W
B
O
R
N
C
A
R
E
SIGNS
Bruises, swelling on buttocks.
Swollen head bump on
one or both sides.
Abnormal position of legs
(after breech presentation).
Asymmetrical arm movement,
arm does not move.
Club foot
Cleft palate or lip
Odd looking, unusual appearance
Open tissue on head,
abdomen or back
Other abnormal appearance.
TREAT AND ADVISE
Explain to parents that it does not hurt the baby,
it will disappear in a week or two and no special
treatment is needed.
DO NOT force legs into a different position.
Gently handle the limb that is not moving,
do not pull.
Refer for special treatment if available.
Help mother to breastfeed. If not successful,
teach her alternative feeding methods K5-K6 .
Plan to follow up.
Advise on surgical correction at age of several months.
Refer for special evaluation.
Cover with sterile tissues soaked with
sterile saline solution before referral.
Refer for special treatment if available.
Manage according to national guidelines.
CLASSIFY
BIRTH INJURY
MALFORMATION
SEVERE
MALFORMATION
NEXT: Assess the mothers breasts if complaining of nipple or breast pain
IF SWELLING, BRUISES OR MALFORMATION
J8
NEXT: Return to
J2
and complete the classification, then go to
J10
Assess the mothers breasts if complaining of nipple or breast pain
ASK, CHECK RECORD
How do your breasts feel?
LOOK, LISTEN, FEEL
Look at the nipple for fissure
Look at the breasts for:
swelling
shininess
redness.
Feel gently for painful part of the
breast.
Measure temperature.
Observe a breastfeed
if not yet done J4 .
SIGNS
No swelling, redness or tenderness.
Normal body temperature.
Nipple not sore and no fissure
visible.
Baby well attached.
Nipple sore or fissured.
Baby not well attached.
Both breasts are swollen,
shiny and patchy red.
Temperature <38C.
Baby not well attached.
Not yet breastfeeding.
Part of breast is painful,
swollen and red.
Temperature >38C
Feels ill.
TREAT AND ADVISE
Reassure the mother.
Encourage the mother to continue breastfeeding.
Teach correct positioning and attachment K3 .
Reassess after 2 feeds (or 1 day). If not better,
teach the mother how to express breast milk from
the affected breast and feed baby by cup, and
continue breastfeeding on the healthy side.
Encourage the mother to continue breastfeeding.
Teach correct positioning and attachment K3 .
Advise to feed more frequently.
Reassess after 2 feeds (1 day). If not better, teach
mother how to express enough breast milk before
the feed to relieve discomfort K5 .
Encourage mother to continue breastfeeding.
Teach correct positioning and attachment K3 .
Give cloxacillin for 10 days F5 .
Reassess in 2 days. If no improvement or worse,
refer to hospital.
If mother is HIV+ let her breastfeed on the healthy
breast. Express milk from the affected breast and
discard until no fever K5 .
If severe pain, give paracetamol F4 .
CLASSIFY
BREASTS
HEALTHY
NIPPLE
SORENESS
OR FISSURE
BREAST
ENGORGEMENT
MASTITIS
ASSESS THE MOTHERS BREASTS IF COMPLAINING OF NIPPLE OR BREAST PAIN
N
E
W
B
O
R
N
C
A
R
E
J9
CARE OF THE NEWBORN
Use this chart for care of all babies until discharge.
Care of the newborn
N
E
W
B
O
R
N
C
A
R
E
J10
CARE AND MONITORING
Ensure the room is warm (not less than 25C and no draught).
Keep the baby in the room with the mother, in her bed or within easy reach.
Let the mother and baby sleep under a bednet.
Support exclusive breastfeeding on demand day and night.
Ask the mother to alert you if breastfeeding difficulty.
Assess breastfeeding in every baby before planning for discharge.
DO NOT discharge if baby is not yet feeding well.
Teach the mother how to care for the baby.
Keep the baby warm K9
Give cord care K10
Ensure hygiene K10
.
DO NOT expose the baby in direct sun.
DO NOT put the baby on any cold surface.
DO NOT bath the baby before 6 hours.
Ask the mother and companion to watch the baby and alert you if
Feet cold
Breathing difficulty: grunting, fast or slow breathing, chest in-drawing
Any bleeding.
Give prescribed treatments according to the schedule K12.
Examine every baby before planning to discharge mother and baby J2-J9 .
DO NOT discharge before baby is 12 hours old.
RESPOND TO ABNORMAL FINDINGS
If the baby is in a cot, ensure baby is dressed or wrapped and covered by a blanket.
Cover the head with a hat.
If mother reports breastfeeding difficulty, assess breastfeeding and help the mother with positioning
and attachment J3
If the mother is unable to take care of the baby, provide care or teach the companion K9-K10
Wash hands before and after handling the baby.
If feet are cold:
Teach the mother to put the baby skin-to-skin K13.
Reassess in 1 hour; if feet still cold, measure temperature and re-warm the baby K9
.
If bleeding from cord, check if tie is loose and retie the cord.
If other bleeding, assess the baby immediately J2-J7
.
If breathing difficulty or mother reports any other abnormality, examine the baby as on J2-J7
.
NEXT: Additional care of a small baby (or twin)
ADDITIONAL CARE OF A SMALL BABY (OR TWIN)
Use this chart for additional care of a small baby: preterm, 1-2 months early or weighing 1500g-<2500g. Refer to hospital a very small baby: >2 months early, weighing <1500g
Additional care of a small baby (twin)
N
E
W
B
O
R
N
C
A
R
E
J11
CARE AND MONITORING
Plan to keep the small baby longer before discharging.
Allow visits to the mother and baby.
Give special support for breastfeeding the small baby (or twins) K4 :
Encourage the mother to breastfeed every 2-3 hours.
Assess breastfeeding daily: attachment, suckling, duration and frequency of feeds, and baby
satisfaction with the feed J4 K6
.
If alternative feeding method is used, assess the total daily amount of milk given.
Weigh daily and assess weight gain K7
.
Ensure additional warmth for the small baby K9 :
Ensure the room is very warm (2528C).
Teach the mother how to keep the small baby warm in skin-to-skin contact
Provide extra blankets for mother and baby.
Ensure hygiene K10 .
DO NOT bath the small baby. Wash as needed.
Assess the small baby daily:
Measure temperature
Assess breathing (baby must be quiet, not crying): listen for grunting; count breaths per minute,
repeat the count if >60 or <30; look for chest in-drawing
Look for jaundice (first 10 days of life): first 24 hours on the abdomen, then on palms and soles.
Plan to discharge when:
Breastfeeding well
Gaining weight adequately on 3 consecutive days
Body temperature between 36.5 and 37.5C on 3 consecutive days
Mother able and confident in caring for the baby
No maternal concerns.
Assess the baby for discharge.
RESPONSE TO ABNORMAL FINDINGS
If the small baby is not suckling effectively and does not have other danger signs, consider
alternative feeding methods K5-K6 .
Teach the mother how to hand express breast milk directly into the babys mouth K5
Teach the mother to express breast milk and cup feed the baby K5-K6
Determine appropriate amount for daily feeds by age K6 .
If feeding difficulty persists for 3 days, or weight loss greater than 10% of birth weight and
no other problems, refer for breastfeeding counselling and management.
If difficult to keep body temperature within the normal range (36.5C to 37.5C):
Keep the baby in skin-to-skin contact with the mother as much as possible
If body temperature below 36.5C persists for 2 hours despite skin-to-skin contact with mother,
assess the baby J2-J8 .
If breathing difficulty, assess the baby J2-J8 .
If jaundice, refer the baby for phototherapy.
If any maternal concern, assess the baby and respond to the mother J2-J8 .
If the mother and baby are not able to stay, ensure daily (home) visits or send to hospital.
N
E
W
B
O
R
N
C
A
R
E
J12
Assess replacement feeding
ASSESS REPLACEMENT FEEDING
If mother chose replacement feeding assess the feeding in every baby as part of the examination.
Advise the mother on how to relieve engorgement K8 . If mother is complaining of breast pain, also assess the mothers breasts J9 .
ASK, CHECK RECORD
Ask the mother
What are you feeding the baby?
How are you feeding your baby?
Has your baby fed in the previous
hour?
Is there any difficulty?
How much milk is baby taking per
feed?
Is your baby satisfied with the feed?
Have you fed your baby any other
foods or drinks?
Do you have any concerns?
If baby more than one day old:
How many times has your baby fed
in 24 hours?
How much milk is baby taking per
day?
How do your breasts feel?
LOOK, LISTEN, FEEL
Observe a feed
If the baby has not fed in the
previous hour, ask the mother to
feed the baby and observe feeding
for about 5 minutes. Ask her to
prepare the feed.
Look
Is she holding the cup to the babys
lips?
Is the baby alert, opens eyes and
mouth?
Is the baby sucking and swallowing
the milk effectively, spilling little?
If mother has fed in the last hour, ask
her to tell you when her baby is willing
to feed again.
SIGNS
Sucking and swallowing adequate
amount of milk, spilling little.
Feeding 8 times in 24 hours on
demand day and night.
Not yet fed (first 6 hours of life).
Not fed by cup.
Not sucking and swallowing effectively,
spilling
Not feeding adequate amount per day.
Feeding less than 8 times per 24
hours.
Receiving other foods or drinks.
Several days old and inadequate
weight gain.
Not sucking (after 6 hours of age).
Stopped feeding.
TREAT AND ADVISE
Encourage the mother to continue feeding by cup on
demand K6 .
Teach the mother replacement feeding G8 .
Teach the mother cup feeding K6 .
Advise to feed more frequently, on demand, day and
night.
Advise the mother to stop feeding the baby other foods
or drinks or by bottle.
Reassess at the next feed or follow-up visit in 2 days.
Refer baby urgently to hospital K14.
CLASSIFY
FEEDING WELL
FEEDING DIFFICULTY
NOT ABLE TO FEED
Breastfeeding, care, preventive measures and treatment for the newborn
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K1
BREASTFEEDING, CARE, PREVENTIVE MEASURES AND TREATMENT FOR THE NEWBORN
Counsel on breastf eeding (1)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K2
COUNSEL ON BREASTFEEDING
Counsel on impor tance of exclusiv e breastfeeding
during pregnancy and after bir th
INCLUDE P ARTNER OR O THER F AMILY MEMBERS IF POSSIBLE
Explain to the mother that: Breast milk contains exactly the nutrients a bab y needs is easily dig ested and efficiently used b y the bab ysbody protects a bab y ag ainst infection. Babies should star t breastfeeding within 1 hour of bir th.They should not ha veanyother food or drink before the y star t to breastfeed. Babies should be exclusiv ely breastfed for the first 6 months of life.
Breastfeeding helps bab ysdevelopment and mother/bab y attachment can help dela y a ne w pregnancy (see D27for breastfeeding and fa mily planning).
For counselling if mother HIV-positiv e,see G7.
Help the mother to init iate breast feeding
within 1 hour , when bab y is read y
After bir th,let the bab y rest comfor tablyon the mot herschest in skin-to-skin contact. Tel l the mother to he lp the ba byto her breast w hen the bab y seems to be read y,usually within the first hour . Signs of readiness to breastfeed are: babylooking around /moving mouth open searching. Check that position and attachment are cor rect at the first feed. Of fer to help the mothe r at an y timeK3. Let the bab y release the breast b y her/himself; then offer the second breast. If the bab y does not feed in 1 hour , examine the bab yJ2J9. If health y,leave the bab y with the mother to tr y later . Assess in 3 hours, orearli er if the bab y is small J4. If the mother is ill and unable to breastfeed, help her to express breast milk and feed the bab y by cupK6. On da y 1 express in a spoon and feed b y spoon. If mother cannot br eastfeed at all, use one of the follo wing options: donated heat-trea ted breast milk. If not a vai lable, then commercial infant for mula. If not a vai lable, then home-made for mula from modified animal milk.
Counsel on breastf eeding (2)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K3
Support exclusive breastfeeding
Keep the mother and bab y tog ether in bed or within easy reach. DO NO Tseparate them. Encourage breastfeeding on demand, day and night, aslong as the bab y wants. A bab y needs to feed da y and night, 8 or more times in 24 hours fro m bir th.Only on the first da y maya full-ter m bab y sleep man y hours after a g ood feed. A small bab y should be encourag ed to feed, day and night, atleast 8 times in 24 hours from birth. Help the mother w hene vershe wants, and especially if she is a first ti me or adolescent mothe r. Let bab y release the breast, then offer the second breast. If mother must be absent, let her express breast milk and let somebod y else feed the exp ressed breast milk to the bab y by cup.
DO NO Tforce the bab y to tak e the breast. DO NO Tinterrupt feed before bab y wants. DO NO Tgi veanyother feeds or water . DO NO Tuse ar tificial teats or pacifiers.
Advise the mother on medication and breastfeeding Most dr ugs giv en to the mother in this guide are safe and the bab y can be breastf ed. If mother is taking cotrimoxazole or fansidar , monitor bab y for jaundice.
Teach cor rect positioni ng and attach ment
for breastfeeding
Showthe mother ho w to hold her bab y.She should: makesure the bab yshead and bod y are in a straight line makesure the bab y is fac ing the breast, the bab ysnose is opposi te her nipple hold the bab ysbodyclose to her bod y support the bab yswho le bod y,not just the neck and shoulders Showthe mother ho w to help her bab y to att ach. She shoul d: touch her bab yslips with her nipple wait until her bab ysmouth is opened wide mov e her bab y quick ly onto her breast, ai ming the infant s lowerlip well belo w the nipple. Look for signs of g ood attachment: more of areola visi ble abo vethe bab y's mouth mouth wide open lower lip tur ned outwards baby's chin touching breast Look for signs of effect ivesuckling (that is, slow,deep sucks, sometimes pausing). If the attachment or suckling is not g ood, tryagain. Then reass ess. If breast eng orgement , express a small amount of breast milk before star ting breastfeeding to soften nipple area so that it is ea sier for the bab y to attach.
If mother is HIV-pos itive, see G7 for specia l counse lling to the mother who is HIV-positive and breastfeeding.
If mother chose repl acement feedings, see G8.
Counsel on breastf eeding (3)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K4
COUNSEL ON BREASTFEEDING
Givespecial suppor t to breastfeed
the small bab y (preter m and/or lo w bir th weight)
COUNSEL THE MOTHER: Reassure the mother that she can breastfeed her small bab y and she has enou gh milk. Explain that her milk is the best food for such a small bab y.Feeding for her/him is e venmore important than for a big bab y. Explain ho w the milk s appearance chang es: milk in the first da ys is thick and y ellow , then it becomes thinner and w hiter. Both are g ood for the bab y. A small bab y does not feed as w ell as a big bab y in the first da ys: maytire easily and suck w eakly at first maysuckle for shor ter periods before resting mayfall asleep during feeding mayhave long pauses betw een suckling and ma y feed long er does not alwa ys wak e up for feeds. Explain that breastfeeding will become easier if the bab y suckles and s timulates the breast her/ himself and w hen the bab y becomes bigg er. Encourage skin-to-skin contact since it mak es breastfeeding easier .
HELP THE MOTHER: Initiate breastfeeding within 1 hour of bir th. Feed the bab y ever y 2-3 hours. Wa kethe bab y for feeding , evenifshe/he does not wak e up alone, 2 hours after the last feed. Always start the feed with breastfeeding before offering a cup. Ifnecessary , improv e the milk flo w (let the mother express a little breast milk before attaching the bab y to the breast) . Keep the bab y long er at the breast. Al lowlong pauses or long , slowfeed. Do not inter rupt feed if the baby is still tr ying. If the bab y is not y et suckling w ell and long enough, dowhatev er works better in y our setting: Let the mother express breast milk into bab ysmouthK5. Let the mother express breast milk and feed bab y by cupK6. On the first da y express breast milk into, and feed colostr um b y spoon. Teach the mother to obser veswallowing if giving expressed breast mi lk. Wei gh the bab y daily (if accurate and precise scales a vai lable), record and assess w eight g ainK7.
Givespecial suppor t to breas tfeed twins
COUNSEL THE MOTHER: Reassure the mother that she has enough breast milk for tw o babies. Encourage her that twins ma y tak e long er to esta blish breastfeeding since the y are frequently bor n preter m and with lo w bir th weight.
HELP THE MOTHER: Start feeding one bab y at a ti me until breastfeeding is w ell established. Help the mother find the best method to feed the twins: If one is w eaker , encourage her to mak e sure that the w eaker twin g ets enough milk. If necessar y,she can expr ess mil k for he r/him and feed her/him b y cup af ter initial breastfeeding . Daily alter nate the sid e each ba byis offered.
Counsel on breastf eeding (3)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K4
COUNSEL ON BREASTFEEDING
Givespecial suppor t to breastfeed
the small bab y (preter m and/or lo w bir th weight)
COUNSEL THE MOTHER: Reassure the mother that she can breastfeed her small bab y and she has enou gh milk. Explain that her milk is the best food for such a small bab y.Feeding for her/him is e venmore important than for a big bab y. Explain ho w the milk s appearance chang es: milk in the first da ys is thick and y ellow , then it becomes thinner and w hiter. Both are g ood for the bab y. A small bab y does not feed as w ell as a big bab y in the first da ys: maytire easily and suck w eakly at first maysuckle for shor ter periods before resting mayfall asleep during feeding mayhave long pauses betw een suckling and ma y feed long er does not alwa ys wak e up for feeds. Explain that breastfeeding will become easier if the bab y suckles and s timulates the breast her/ himself and w hen the bab y becomes bigg er. Encourage skin-to-skin contact since it mak es breastfeeding easier .
HELP THE MOTHER: Initiate breastfeeding within 1 hour of bir th. Feed the bab y ever y 2-3 hours. Wa kethe bab y for feeding , evenifshe/he does not wak e up alone, 2 hours after the last feed. Always start the feed with breastfeeding before offering a cup. Ifnecessary , improv e the milk flo w (let the mother express a little breast milk before attaching the bab y to the breast) . Keep the bab y long er at the breast. Al lowlong pauses or long , slowfeed. Do not inter rupt feed if the baby is still tr ying. If the bab y is not y et suckling w ell and long enough, dowhatev er works better in y our setting: Let the mother express breast milk into bab ysmouthK5. Let the mother express breast milk and feed bab y by cupK6. On the first da y express breast milk into, and feed colostr um b y spoon. Teach the mother to obser veswallowing if giving expressed breast mi lk. Wei gh the bab y daily (if accurate and precise scales a vai lable), record and assess w eight g ainK7.
Givespecial suppor t to breas tfeed twins
COUNSEL THE MOTHER: Reassure the mother that she has enough breast milk for tw o babies. Encourage her that twins ma y tak e long er to esta blish breastfeeding since the y are frequently bor n preter m and with lo w bir th weight.
HELP THE MOTHER: Start feeding one bab y at a ti me until breastfeeding is w ell established. Help the mother find the best method to feed the twins: If one is w eaker , encourage her to mak e sure that the w eaker twin g ets enough milk. If necessar y,she can expr ess mil k for he r/him and feed her/him b y cup af ter initial breastfeeding . Daily alter nate the sid e each ba byis offered.
Alternative feeding methods (2)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K6
ALTERNA TIVE FEEDING METHODS
Cup feeding expressed breast milk
Teach the mother to feed the bab y with a cup. Donot feed the bab y yourself. The mother should: Measure the quantity of milk in the cup Hold the bab y sitting semi-upright on her lap Hold the cup of milk to the bab yslips: rest cup lightly on lo werlip touch edg e of cup to outer par t of upper lip tip cup so that milk just reaches the bab yslips but do not pour the milk into the bab ysmouth. Babybecomes aler t,opens mouth and e yes, and star ts to feed. The bab y will suck the milk, spilling some. Small babies will star t to tak e milk into their mouth using the tongue. Babyswallows the milk. Babyfinishes feeding w hen mouth closes or w hen not interested in t aking more. If the bab y does not tak e the calculated amount: Feed for a long er time or feed more often Teach the mother to measure the bab ysintake over24hours, not just at each feed. If mother does not express enough milk in the first fe w da ys,or if the mother cannot brea stfeed at all,use one of the follo wing feeding options: donated heat-treated breast milk home-made or commercial for mula. Feed the bab y by cup if the mother is not a vai lable to do so. Babyis cup feeding w ell if required amount of milk is s wallow ed,spilling little, and weight g ain is maintained.
Quantity to feed b y cup
Start with 80 ml/kg bod y weight per da y for da y 1.Increase total v olume b y 10-20ml /kg per da y, until bab y tak es 150 ml /kg/day . See table belo w. Divide total into 8 feeds. Gi veevery2-3 hours to a sma ll sizeorill bab y. Check the bab ys24 hour intak e.Size of individual feeds ma y vary . Continue until bab y tak es the req uiredquantity. Was h the cup with water and soap after each feed.
APPRO XIMATE QUANTITY T O FEED BY CU P (IN ML) EVER Y 2-3 HOUR S FROM BIRTH (BY WEIGHT)
We ight (kg) Day0 1 2 3 4 5 6 7
1.5-1.9 15ml 17ml19ml 21ml 23ml 25ml 27ml 27+ml
2.0-2.4 20ml 22ml25ml 27ml 30ml 32ml 35ml 35+ml
2.5+ 25ml 28ml30ml 35ml 35ml 40+ml 45+ml 50+ml
Signs that bab y is recei ving
adequate amount of milk
Babyis satisfied wit h the fe ed. Wei ght loss is less than 10% in the first w eek of life. Babygai ns at least 160-g in the follo wingweek s or a minimum 300 -g in the fi rst month. Babywet s ever y da y as frequently as bab y is feeding . Baby s stool is changing from dark to light bro wn or y ellowbyday3.
Wei gh and assess weight gain
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K7
WEIGH AND ASSESS WEIGHT GAIN
Wei gh bab y in the first month of life
WEIGH THE BABY Monthly if bir th weight nor mal and breastfeeding w ell.Ever y 2 w eeks if replacement feeding or treatment with isoniazid. When the bab y is brought for examination because not feeding w ell,or ill.
WEIGH THE SMALL BABY Ever y da y until 3 consecutiv e times g aining w eight (at least 15-g/da y). Week ly until 4-6 w eeks of ag e (reached ter m).
Assess w eight g ain
Use this table for guidance w hen assessing w eight g ain in the first month oflife
Age Acceptable weight loss/gain in the first month of life
1 week Loss up to 10%
2-4 weeks Gain at least 160 g per w eek (at least 15g/day)
1 month Gain at least 300 g in th e first mo nth
If weighing daily with a precise and accur ate scale
First week Noweight loss or total less than 10%
Afterward daily g ain in small babie s at least 20 g
Scale maintenance
Daily/weekly wei ghing requires p recise and accur ate scale (10 -g increm ent): Calibrate it daily accor ding to instr uctions. Check it for accurac y acco rding to instr uctions.
Simple spring scales are not prec ise enough for daily/ week ly weighing .
K2
COUNSEL ON BREASTFEEDING (1)
Counsel on importance of exclusive breast
feeding
Help the mother to initiate breastfeeding
K3
COUNSEL ON BREASTFEEDING (2)
Support exclusive breastfeeding
Teach correct positioning and attachment for
breastfeeding
K4
COUNSEL ON BREASTFEEDING (3)
Give special support to breastfeed the small
baby (preterm and/or low birth weight)
Give special support to breastfeed twins
K5
ALTERNATIVE
FEEDING METHODS (1)
Express breast milk
Hand express breast milk directly into the
babys mouth
K6
ALTERNATIVE
FEEDING METHODS (2)
Cup feeding expressed breast milk
Quantity to feed by cup
Signs that baby is receiving adequate amount
of milk
K7
WEIGH AND ASSESS WEIGHT GAIN
Weigh baby in the first month of life
Assess weight gain
Scale maintenance
Other breastf eeding suppor t
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K8
OTHER BREASTFEEDING SUPPORT
Givespecial suppor t to the mother
whoisnot yet breastfeeding
(Mother or bab y ill, orbabytoo small to suckle) Teach the mother to express breast milk K5. Help her if necessar y. Use the milk to feed the bab y by cup. If mother and bab y are separated, help the mother to see the bab y or infor m her about the bab ys condition at least twice daily . If the bab y was refer red to another institution, ensure the bab y gets the mother s expressed breast milk if possible. Encourage the mother to breastfeed w hen she or the bab y reco ver s.
If the bab y does not ha vea mother
Givedonated heat treated breast milk or home-based or commercial fo rmula by cup. Teach the carer ho w to prepare milk and feed the bab y K6. Follo w up in 2 w eeks; w eigh and assess w eight g ain.
Advise the mother w ho is not breastfee ding
at all on ho w to reli eveengor gement
(Babydied or stillbor n,mother chose replacement feeding) Breasts ma y be uncomfor table for a w hile. Avoid stimulating the breasts. Support breasts with a w ell-fitting bra or c loth. Donot bind the breasts tightly a s this ma y incr ease her discomfor t. Apply a compress. Wa rmt h is com fortable for some mothers, ot hers prefer a cold compress to reduce s wel ling. Teach the mother to express enough milk to relie vediscomfor t.Expressing can be done a fewtimes a day when the breasts are o ver full. It does not need to be done if the mother is uncomfor table. It will be less than her bab y would tak e and will not stimulate increased milk production. Relie vepain. An analg esic such as ibuprofen, orparacetamol ma y be used. Some women use plant products such as teas made from herbs, or plan ts such as ra w cabbag e lea vespl aced directly on the breast to reduce pain and s wel ling. Advise to seek care if br eastsbecome painful, swollen, red, if she feels ill or temperature greater than 38C.
Pharmacological treatments to reduce mi lk suppl y are no t recomm ended. The abo vemethods are co nsidered more effectiv e in the long ter m.
Ensure war mth for the baby
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K9
ENSURE WARMTH FOR THE BABY
Keep the bab y war m
ATBIRTH AND WITHIN THE FIRST HOUR(S) War m deliv eryroom: for the bir th of the bab y the room temperature should be 25-28C, nodr aught. Drybaby: immediately after bir th,place the bab y on the mother s abdomen or on a war m,clean and drysurface. Drythe w hole bod y and hair thoroughly , with a dr y cloth. Skin-to-skin contact: Lea vethe bab y on the mother s abdomen (before cord cut) or chest (after cord cut) after bir th for at least 2 hours. Coverthe bab y with a soft dr y cloth. If the mother cannot k eep the bab y skin-to-skin because of complications, wr ap the bab y in a clean, dry , warmcloth and place in a cot. Coverwi th a blank et.Use a radiant wa rme r if roomnot war mor bab y small.
SUBSEQUENTL Y (FIRST D AY) Explain to the mother that k eeping bab y war mis impor tant for the bab y to remain healt hy. Dress the bab y or wrap in soft dr y clean cloth. Coverthe head with a cap for the first fe w da ys,especially if baby is small. Ensure the bab y is dressed or wrapped and co ver ed with a blank et. Keep the bab y within easy reach of the mother . Do not separate them(ro oming-in). If the mother and bab y must be separated, ensure bab y is dressed or wra pped and co ver ed with a blanket. Assess war mth e ver y 4 hours b y touching the bab ysfeet: if feet are cold use skin-to-skin conta ct,add extra blank et and reassess (see Re warmthe ne wborn). Keep the roomfor the mother and bab y war m.If the roomis not war menough, al ways cover the bab y with a blank et and/or use skin-to-skin contact.
ATHOME Explain to the mother that babies need one more la yerofcl othes than other childre n or adults. Keep the roomor par t of the roomwar m,especially in a cold climate. During the da y,dress or wrap the bab y. At night, let the bab y sleep with the mother or within easy reach to facil itate breastfeedin g.
Do not put the bab y on an y cold or w et surface. Do not bath the bab y at bir th.Wai t at least 6 hours before bathing . Do not swaddle wrap too tightly . Swaddling mak es them cold. Do not leavethe bab y in direct sun.
Keep a small bab y war m
The room for the bab y shoul d be war m (not less than 25C) with no draught. Explain to the mother the importance of war mth for a small baby. After bir th,encourage the mother to k eep the bab y in skin-to-skin contact as long as possible. Advise to use extra cl othes, socks and a cap, bl ankets, tokeep the bab y war m or w hen the bab y is not with the mother . Was h or bath a bab y in a v erywarmroom, in war m wate r.After bathing , dryimmediately and thoroughly. Keep the bab y war m after the bath. Avoid bathing small babies. Check frequently if f eet are war m.If cold, rewarmthe bab y (see b elow). Seek care if the bab ysfeetremain cold after re warming .
Rewar m the bab y skin-to -skin
Before re warming , remov e the bab yscold clothing . Place the ne wborn skin-to-skin on the mother s chest dressed in a pre-war med shir t open at the front, a napp y (diaper), hat andsocks. Cov er the infant on the mother s chest wi th her clothes and an additional (pre-war med) blank et. Check the temperatu re ever y hour until nor mal. Keep the bab y with t he mothe r until the bab ysbodytemperature is in nor mal rang e. If the bab y is small , encourage the mother to k eep the bab y in skin-to-skin contact for as long as possible, dayand night . Be sure the tempera ture of the room w here the re warming takesplace is at least 25C. If the bab ystemperature is not 36.5C or more after 2 hours of re warming , reasses s the bab y J2J7. If refer ral needed, keep the bab y in skin-to-skin position/contact with the mother or othe accompanyin g the bab y.
Other baby care
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K10
OTHER BABY CARE
Alwa ys wash hands before and after taking care of the bab y.DO NO T share supplies with other babies.
Cord care
Was h hands before and after cord care. Put nothing on the stump. Fold napp y (diaper) belo w stump. Keep cord stump loosely co ver ed with clean clothes. If stump is soiled, wash it with clean water and soap. Dry it thoroughly with clean cloth. If umbilicus is red or draining pus or blood, examine the bab y and manag e accordingly J2J7. Explain to the mother that she should seek care if the umbilicus is r ed or draining pus or blood.
DONOTbandagethe stump or abdomen. DONOTapply an y substances or medicine to stump. Avoid touching the stump unnecessarily .
Sleeping
Use the bednet da y and night for a sleeping bab y. Let the bab y sleep on her/his back or on the side. Keep the bab y awayfrom smok e or people smoking . Keep the bab y,especially a small bab y,away from sick children or adu lts.
Hygiene (washing , bathing)
ATBIRTH:
Only remo veblood or mecon ium.
DO NO Tremov e vernix. DO NO Tbathe the bab y until at least 6 hours of ag e.
LATER AND A T HOME:
Was h the face, neck,underar ms dail y. Was h the buttocks w hen soiled. Dry thor oughly. Bath w hen necessar y: Ensure the room is wa rm,nodraught Use war m water fo r bathing Thoroughly dr y the ba by,dress and co verafter bath.
OTHER BABY CARE:
Use cloth on bab ysbottom to collect stool. Di spose of the stool as for w omans pads. Was h hands.
DO NO Tbathe the bab y before 6 hours old or if the bab y is cold. DO NO Tapply an ything in the bab yseyes except an antimicrobial at birth.
SMALL BABIES REQ UIRE MORE CAREFUL ATTE NTION:
The room must be w armer when changing , washing, bathing and examining a small bab y.
Newbor n resuscitation
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K11
NEWBORN RESUSCITA TION
Startresuscitation within 1 minute of bir th if bab y is not breathing or is g asping for breath.
Observe universal precautions to prevent infection A4.
Keep the bab y war m
Clamp and cut the cord if necessar y. Tra nsfer the bab y to a dr y,clean and war m surface. Informthe mother that the bab y has difficulty initiating breathing and that youwi ll help the bab y to breathe. Keep the bab y wrapped and under a radiant heater if possible.
Open the airwa y
Position the head so it is slightly extended. Suction first the mouth and then the nose. Introduce the suction tube into the ne wborn s mouth 5-cm from lips and suck w hile withdra wing. Introduce the suction tube 3-cm into each nostril and suck w hile withdra wing until no mucus. Repeat each suction if necessar y but no more than twice and no more than 20 seconds in total.
If still no breathing , VENTILATE:
Place mask to co verchin,mouth, and nose. Formseal. Squeeze bag attached to the mask with 2 fing ers or w hole hand, according to bag size, 2 or 3 times. Observ e rise of chest. Ifchest is not rising: reposition head check mask seal. Squeeze bag harder with w hole hand. Once g ood seal and chest rising , ventilate at 40 squeezes per minute u ntil ne wborn starts crying or breathing spontaneously .
If breathing or c ryi ng,stop v entilatin g
Look at the chest for in -drawing . Count breaths per min ute. If breathing more tha n 30 breaths per minute and no se ver e chest in-dra wing: do not v entilate an y more put the bab y in skin-to-skin contact on mother s chest and continue care as on D19 monitor e ver y 15 minutes for breathing and war mth tell the mother that t he bab y will probably be w ell.
DO NO Tleavethe bab y alone
If breathing les s than 30 breat hs per minute or
severe chest in-dr awi ng:
continue v entilating arr angefor immediate refer ral explain to the mother w hat happened, what y ou are doi ng and w hy ventilate during refer ral record the e vent on the refer ral for m and la bour recor d.
If no breathing or g asping at all
after 20 minutes of v entilat ion
Stop v entilating.The baby is dea d. Explain to the mother and g ivesupportiv e careD24. Record the e vent.
Tre at and immunize the baby (1)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FO
R
TH
E NEW
B
O
RN
K12
TREAT THE BABY
Tre at the bab y
Determine appropriate dr ugs and dosag e for the bab yswei ght. Tel l the mother the reasons for giving the dr ug to the bab y. Giveintramuscular antibiotics in thigh. Use a ne w syring e and needle f or each antibiotic.
TEACH THE MO THER T O GIVE TREATMENT TOTHE BABY ATHOME Explain carefully ho w to giv e the treatment. Label and packag e each dr ug separately . Check mother s understanding before she lea vesthe clinic. Demonstrate ho w to measure a dose. Wat ch the mother practice measuring a dose b y herself. Wat ch the mother giv e the first dose to the bab y.
Give2 IM antibiotics (first w eek of life)
Givefirst dose of both ampicillin and g entamicin IM in thigh before ref err al for possible se rious illness, severe umbilical infection or se ver e skin infection. Giveboth ampicillin and g entamicin IM for 5 da ys in asymptomatic bab ies classified at risk of infection. Giveintramuscular antibiotics in thigh. Use a ne w syring e and needle f or each antibiotic.
Ampicillin IM Gentamicin IM Dose : 50 mg per kg Dose : 5 mg per kg every12 hours every24 hours if ter m; Add 2.5 ml sterile water 4 mg per kg e ver y 24 hours if preter m
We ight to 500 mg vial = 200 mg/ml 20 mg per 2 ml vial = 10 mg/ml
1.0 1.4 kg 0. 35 ml 0.5 ml
1.5 1.9 kg 0. 5 ml 0.7 ml
2.0 2.4 kg 0. 6 ml 0.9 ml
2.5 2.9 kg 0. 75 ml 1.35 ml
3.0 3.4 kg 0. 85 ml 1.6 ml
3.5 3.9 kg 1ml 1.85 ml
4.0 4.4 kg 1.1 ml 2.1 ml
GiveIM benzathine penicill in
to bab y (single dose) ifmother tested RPR-posit ive
Benzathine penicill in IM Dose: 50000 u nits/kg once Add 5 ml sterile water to vial containi ng 1.2 milli on units = 1.2 millio n units/(6 ml total v olume) Wei ght =200 000 units/ml
1.0 - 1.4 kg 0. 35 ml
1.5 - 1.9 kg 0. 5 ml
2.0 - 2.4 kg 0. 6 ml
2.5 - 2.9 kg 0. 75 ml
3.0 - 3.4 kg 0. 85 ml
3.5 - 3.9 kg 1.0 ml
4.0 - 4.4 kg 1.1 ml
GiveIM antibiotic for possible g onococcal e yeinfection
(single dose)
Ceftriaxone (1st choice) Kanamycin (2nd choice) Dose : 50 mg per kg onc e Dose : 25 mg per kg onc e,max 75 mg We ight 250 mg per 5 ml vial=mg/ml 75 mg per 2 ml via l = 37.5 mg/ml
1.0 - 1.4 kg 1ml 0.7ml
1.5 - 1.9 kg 1.5 ml 1 ml
2.0 - 2.4 kg 2ml 1.3ml
2.5 - 2.9 kg 2. 5 ml 1.7 ml
3.0 - 3.4 kg 3ml 2ml
3.5 - 3.9 kg 3. 5 ml 2 ml
4.0 - 4.4 kg 4ml 2ml
Tre at and immunize the baby (2)
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K13
Tre at local infection
TEACHMOTHER TOTREAT LOCAL INFECTION
Explain and sho w ho w the treatment is giv en. Wat ch her as she car ries out the first treatment. Ask her to let y ou kno w if the local infection g ets worse and to retur n to the clinic if possible. Tre at for 5 da ys.
TREAT SKIN PUSTULES OR UMBILICAL INFECTION
Do the following 3 times daily: Was h hands with clean water and soap. Gently wash off pus and cr usts with boiled and cooled water and soap . Drythe area with clean cloth. Pai nt with g entian violet. Was h hands.
TREAT EYE INFECTION
Do the following 6-8 times daily: Was h hands with clean water and soap. Wetcl ean cloth with boiled and cooled water . Use the w et cloth to g ently wash off pus from the bab yseyes. Apply 1% tetracycline e yeointment in each e ye3 times daily . Was h hands.
REASSESS IN 2 D AYS:
Assess the skin, umbilicus or e yes. If pus or redness remains or is w orse, refer to hospital. If pus and redness ha veimprov ed,tell the mother to continue treating local infection at home.
Giveisoniazid (INH) proph ylaxis to ne wborn
If the mother is diagn osed as ha ving tuber culosis and star ted treatmen t less than 2 months before de livery: Give5-mg/kg isoniaz id (INH) orally once a da y for 6 months (1 tablet = 200-mg). DelayBCG v accination until INH treatment completed, orrepeat BCG. Reassure the mother that itissafe to breastfeed the bab y. Follo w up the bab y ever y 2 w eeks, or according to national g uidelines, to ass ess weight g ain.
Immunize the ne wborn
GiveBCG, OPV-0, Hepatitis B (HB-1) v accine in the fi rst w eek of lif e,preferably before discharg e. If un-immunized ne wborn first seen 1-4 w eeks of ag e,giveBCG only . Record on immunizat ion car d and child record. Advise whe n to retur n for next immunization.
Age Vaccine
Birth< 1 week BCG OPV-0 HB1
6 weeks DPT OPV-1 HB-2
GiveARVmedicine to ne wborn
Givethe first dose of ARV medic ines to ne wborn 812 hours after bir th: GiveNevirapine 2 mg/kg once only . GiveZidovudine 4 mg/kg e ver y 12 hours. If the ne wborn spillsorvomits within 30 minutes repeat the dos e.
Teach mother to gi veoral ar v medic ines at home
Explain and sho w ho w the medicine is giv en. Was h hands. Demonstrate ho w to measure the d ose on the spoon. Begin feeding the bab y by cup. Givemedicine b y spoon before the end of the feed. Complete the feed. Wat ch her as she car ries out the next treatment. Explain to the mother tha t she should watch her bab y afte r giving a dose of Zido vudine. If bab y vomits or spills within 30 minutes, she should repeat the dose. GiveZidovudine every12 hours for 7 da ys.
K8 OTHER BREASTFEEDING SUPPORT
Give special support to the mother who is not
yet breastfeeding
Advise the mother who is not breastfeeding at
all on how to relieve engorgement
If the baby does not have a mother
K9 ENSURE WARMTH FOR THE BABY
Keep the baby warm
Keep a small baby warm
Rewarm the baby skin-to-skin
K10 OTHER BABY CARE
Cord care
Sleeping
Hygiene
K11 NEWBORN RESUSCITATION
Keep the baby warm
Open the airway
If still not breathing, ventilate...
If breathing or crying, stop ventilating
If not breathing or gasping at all after 20
minutes of ventilation
K12
TREAT AND IMMUNIZE THE BABY (1)
Treat the baby
Give 2 IM antibiotics (first week of life)
Give IM benzathine penicillin to baby (single
dose) if mother tested RPR positive
Give IM antibiotic for possible gonococcal eye
infection (single dose)
K13 TREAT AND IMMUNIZE THE BABY (2)
Treat local infection
Give isoniazid (INH) prophylaxis to newborn
Immunize the newborn
Advise when to retur n with the baby
BREASTFEEDING,
CARE, PREVENTIVE M
EASURES
AND TREATM
ENT FOR
TH
E NEW
B
ORN
K14
ADVISE WHEN T O RETURN WITH THE BABY
Formaternal visits see schedule on D28.
Routine visits
Return Postnatal visit Wi thin the first w eek, preferably wi thin 2-3 da ys Immunization visit Atage 6 weeks (If BCG, OPV-0 and HB-1 givenin the first w eek of life)
Follo w-up visits
If the problem w as: Retur n in Feeding difficulty 2 da ys Red umbilicus 2 da ys Skin infection 2 da ys Eyeinfection 2 days Thrush 2days Mother has either : breast eng orgement or 2days mastitis. 2 da ys Lowbirthwei ght, and either fi rst w eek of life or 2 da ys not adequately g aining w eight 2 days Lowbirthwei ght, and either ol der than 1 w eek or 7 da ys gaining w eight adequately 7 da ys Orphan bab y 14days INH proph ylaxis 14 days Tre ated for possible cong enital syphilis 14 da ys Mother HIV-positiv e 14days
Advise the mother to s eek care for the bab y
Use the counselling sh eet to ad vise the mother w hen to seek care,or when to retur n,if the bab y has an y of thes e dang er signs:
RETURN OR GO TOTHE HOSPIT AL IMMEDIA TELYIF THE BABY HAS
di fficulty breathing . convulsions. feverorfeels cold. bl eeding. di arr hoea. verysmall, just bor n. not feeding at all.
GO T O HEAL TH CENTRE AS QUICKLY AS POSSI BLE IF THE BABY HAS
di fficu lty feeding . pus from e yes. skin pustules. yellowskin. acord stump w hich is red or draining pus. feeds <5 t imes in 24 hour s.
Refer bab y urg ently to hospital
Af ter eme rgency treatment, explain the need for refer ral to the mother/father . Or ganize safe transpor tation. Al ways send the mothe r with the bab y,if possible. Send refer ral note with the bab y. Informthe r eferr al centre if possible b y radi o or telephone.
DURING TRANSPORT ATI ON
Keep th e bab y war m by skin- to-skin contact with mother or someone else. Coverthe bab y with a blank et and co verher/his head with a cap. Pr otect the bab y from direct sunshine. Encourage breastfeeding during the journe y. Ifthe bab y does not breastfeed and jour neyis more than 3 ho urs, consider giving expressed breas milk b y cup K6.
K14 ADVISE WHEN TO RETURN
WITH THE BABY
Routine visits
Follow-up visits
Advise the mother to seek care for the baby
Refer baby urgently to hospital
This section has details on breastfeeding, care of the baby,
treatments, immunization, routine and follow-up visits and urgent
referral to hospital.
General principles are found in the section on good care A1-A6 .
If mother HIV-positive, see also G7-G11.
Counsel on breastfeeding (1)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K2
COUNSEL ON BREASTFEEDING
Counsel on importance of exclusive breastfeeding
during pregnancy and after birth
INCLUDE PARTNER OR OTHER FAMILY MEMBERS IF POSSIBLE
Explain to the mother that:
Breast milk contains exactly the nutrients a baby needs
is easily digested and efficiently used by the babys body
protects a baby against infection.
Babies should start breastfeeding within 1 hour of birth. They should not have any other food or
drink before they start to breastfeed.
Babies should be exclusively breastfed for the first 6 months of life.
Breastfeeding
helps babys development and mother/baby attachment
can help delay a new pregnancy (see D27 for breastfeeding and family planning).
For counselling if mother HIV-positive, see G7 .
Help the mother to initiate breastfeeding
within 1 hour, when baby is ready
After birth, let the baby rest comfortably on the mothers chest in skin-to-skin contact.
Tell the mother to help the baby to her breast when the baby seems to be ready, usually within the
first hour. Signs of readiness to breastfeed are:
baby looking around/moving
mouth open
searching.
Check that position and attachment are correct at the first feed. Offer to help the mother at any time K3 .
Let the baby release the breast by her/himself; then offer the second breast.
If the baby does not feed in 1 hour, examine the baby J2J9. If healthy, leave the baby with the
mother to try later. Assess in 3 hours, or earlier if the baby is small J4 .
If the mother is ill and unable to breastfeed, help her to express breast milk and feed the baby by
cup K6 . On day 1 express in a spoon and feed by spoon.
If mother cannot breastfeed at all, use one of the following options:
donated heat-treated breast milk.
If not available, then commercial infant formula.
If not available, then home-made formula from modified animal milk.
Counsel on breastfeeding (2)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K3
Support exclusive breastfeeding
Keep the mother and baby together in bed or within easy reach. DO NOT separate them.
Encourage breastfeeding on demand, day and night, as long as the baby wants.
A baby needs to feed day and night, 8 or more times in 24 hours from birth. Only on the first day
may a full-term baby sleep many hours after a good feed.
A small baby should be encouraged to feed, day and night, at least 8 times in 24 hours from
birth.
Help the mother whenever she wants, and especially if she is a first time or adolescent mother.
Let baby release the breast, then offer the second breast.
If mother must be absent, let her express breast milk and let somebody else feed the expressed
breast milk to the baby by cup.
DO NOT force the baby to take the breast.
DO NOT interrupt feed before baby wants.
DO NOT give any other feeds or water.
DO NOT use artificial teats or pacifiers.
Advise the mother on medication and breastfeeding
Most drugs given to the mother in this guide are safe and the baby can be breastfed.
If mother is taking cotrimoxazole or fansidar, monitor baby for jaundice.
Teach correct positioning and attachment
for breastfeeding
Show the mother how to hold her baby. She should:
make sure the babys head and body are in a straight line
make sure the baby is facing the breast, the babys nose is opposite her nipple
hold the babys body close to her body
support the babys whole body, not just the neck and shoulders
Show the mother how to help her baby to attach. She should:
touch her babys lips with her nipple
wait until her babys mouth is opened wide
move her baby quickly onto her breast, aiming the infants lower lip well below the nipple.
Look for signs of good attachment:
more of areola visible above the baby's mouth
mouth wide open
lower lip turned outwards
baby's chin touching breast
Look for signs of effective suckling (that is, slow, deep sucks, sometimes pausing).
If the attachment or suckling is not good, try again. Then reassess.
If breast engorgement, express a small amount of breast milk before starting breastfeeding to soften
nipple area so that it is easier for the baby to attach.
If mother is HIV-positive, see G7 for special counselling to the mother who is HIV-positive and
breastfeeding.
If mother chose replacement feedings, see G8 .
Counsel on breastfeeding (3)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K4
COUNSEL ON BREASTFEEDING
Give special support to breastfeed
the small baby (preterm and/or low birth weight)
COUNSEL THE MOTHER:
Reassure the mother that she can breastfeed her small baby and she has enough milk.
Explain that her milk is the best food for such a small baby. Feeding for her/him is even more
important than for a big baby.
Explain how the milks appearance changes: milk in the first days is thick and yellow, then it
becomes thinner and whiter. Both are good for the baby.
A small baby does not feed as well as a big baby in the first days:
may tire easily and suck weakly at first
may suckle for shorter periods before resting
may fall asleep during feeding
may have long pauses between suckling and may feed longer
does not always wake up for feeds.
Explain that breastfeeding will become easier if the baby suckles and stimulates the breast her/
himself and when the baby becomes bigger.
Encourage skin-to-skin contact since it makes breastfeeding easier.
HELP THE MOTHER:
Initiate breastfeeding within 1 hour of birth.
Feed the baby every 2-3 hours. Wake the baby for feeding, even if she/he does not wake up alone,
2 hours after the last feed.
Always start the feed with breastfeeding before offering a cup. If necessary, improve the milk flow
(let the mother express a little breast milk before attaching the baby to the breast).
Keep the baby longer at the breast. Allow long pauses or long, slow feed. Do not interrupt feed if the
baby is still trying.
If the baby is not yet suckling well and long enough, do whatever works better in your setting:
Let the mother express breast milk into babys mouth K5 .
Let the mother express breast milk and feed baby by cup K6 . On the first day express breast
milk into, and feed colostrum by spoon.
Teach the mother to observe swallowing if giving expressed breast milk.
Weigh the baby daily (if accurate and precise scales available), record and assess weight gain K7 .
Give special support to breastfeed twins
COUNSEL THE MOTHER:
Reassure the mother that she has enough breast milk for two babies.
Encourage her that twins may take longer to establish breastfeeding since they are frequently born
preterm and with low birth weight.
HELP THE MOTHER:
Start feeding one baby at a time until breastfeeding is well established.
Help the mother find the best method to feed the twins:
If one is weaker, encourage her to make sure that the weaker twin gets enough milk.
If necessary, she can express milk for her/him and feed her/him by cup after initial breastfeeding.
Daily alternate the side each baby is offered.
Alternative feeding methods (1)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K5
ALTERNATIVE FEEDING METHODS
Express breast milk
The mother needs clean containers to collect and store the milk.
A wide necked jug, jar, bowl or cup can be used.
Once expressed, the milk should be stored with a well-fitting lid or cover.
Teach the mother to express breast milk:
To provide milk for the baby when she is away. To feed the baby if the baby is
small and too weak to suckle
To relieve engorgement and to help baby to attach
To drain the breast when she has severe mastitis or abscesses.
Teach the mother to express her milk by herself. DO NOT do it for her.
Teach her how to:
Wash her hands thoroughly.
Sit or stand comfortably and hold a clean container underneath her breast.
Put her first finger and thumb on either side of the areola, behind the nipple.
Press slightly inwards towards the breast between her finger and thumb.
Express one side until the milk flow slows. Then express the other side.
Continue alternating sides for at least 20-30 minutes.
If milk does not flow well:
Apply warm compresses.
Have someone massage her back and neck before expressing.
Teach the mother breast and nipple massage.
Feed the baby by cup immediately. If not, store expressed milk in a cool, clean and safe place.
If necessary, repeat the procedure to express breast milk at least 8 times in 24 hours. Express as
much as the baby would take or more, every 3 hours.
When not breastfeeding at all, express just a little to relieve pain K5 .
If mother is very ill, help her to express or do it for her.
Hand express breast milk
directly into the babys mouth
Teach the mother to express breast milk.
Hold the baby in skin-to-skin contact, the mouth close to the nipple.
Express the breast until some drops of breast milk appear on the nipple.
Wait until the baby is alert and opens mouth and eyes, or stimulate the baby lightly to awaken her/
him.
Let the baby smell and lick the nipple, and attempt to suck.
Let some breast milk fall into the babys mouth.
Wait until the baby swallows before expressing more drops of breast milk.
After some time, when the baby has had enough, she/he will close her/his mouth and
take no more breast milk.
Ask the mother to repeat this process every 1-2 hours if the baby is very small
(or every 2-3 hours if the baby is not very small).
Be flexible at each feed, but make sure the intake is adequate by checking daily weight gain.
Alternative feeding methods (2)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K6
ALTERNATIVE FEEDING METHODS
Cup feeding expressed breast milk
Teach the mother to feed the baby with a cup. Do not feed the baby yourself. The mother should:
Measure the quantity of milk in the cup
Hold the baby sitting semi-upright on her lap
Hold the cup of milk to the babys lips:
rest cup lightly on lower lip
touch edge of cup to outer part of upper lip
tip cup so that milk just reaches the babys lips
but do not pour the milk into the babys mouth.
Baby becomes alert, opens mouth and eyes, and starts to feed.
The baby will suck the milk, spilling some.
Small babies will start to take milk into their mouth using the tongue.
Baby swallows the milk.
Baby finishes feeding when mouth closes or when not interested in taking more.
If the baby does not take the calculated amount:
Feed for a longer time or feed more often
Teach the mother to measure the babys intake over 24 hours, not just at each feed.
If mother does not express enough milk in the first few days, or if the mother cannot breastfeed at
all, use one of the following feeding options:
donated heat-treated breast milk
home-made or commercial formula.
Feed the baby by cup if the mother is not available to do so.
Baby is cup feeding well if required amount of milk is swallowed, spilling little, and weight gain is
maintained.
Quantity to feed by cup
Start with 80 ml/kg body weight per day for day 1. Increase total volume by 10-20 ml/kg per day,
until baby takes 150 ml/kg/day. See table below.
Divide total into 8 feeds. Give every 2-3 hours to a small size or ill baby.
Check the babys 24 hour intake. Size of individual feeds may vary.
Continue until baby takes the required quantity.
Wash the cup with water and soap after each feed.
APPROXIMATE QUANTITY TO FEED BY CUP (IN ML) EVERY 2-3 HOURS FROM BIRTH (BY WEIGHT)
Weight (kg) Day 0 1 2 3 4 5 6 7
1.5-1.9 15ml 17ml 19ml 21ml 23ml 25ml 27ml 27+ml
2.0-2.4 20ml 22ml 25ml 27ml 30ml 32ml 35ml 35+ml
2.5+ 25ml 28ml 30ml 35ml 35ml 40+ml 45+ml 50+ml
Signs that baby is receiving
adequate amount of milk
Baby is satisfied with the feed.
Weight loss is less than 10% in the first week of life.
Baby gains at least 160-g in the following weeks or a minimum 300-g in the first month.
Baby wets every day as frequently as baby is feeding.
Babys stool is changing from dark to light brown or yellow by day 3.
Weigh and assess weight gain
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K7
WEIGH AND ASSESS WEIGHT GAIN
Weigh baby in the first month of life
WEIGH THE BABY
Monthly if birth weight normal and breastfeeding well. Every 2 weeks if replacement feeding or
treatment with isoniazid.
When the baby is brought for examination because not feeding well, or ill.
WEIGH THE SMALL BABY
Every day until 3 consecutive times gaining weight (at least 15-g/day).
Weekly until 4-6 weeks of age (reached term).
Assess weight gain
Use this table for guidance when assessing weight gain in the first month of life
Age Acceptable weight loss/gain in the first month of life
1 week Loss up to 10%
2-4 weeks Gain at least 160 g per week (at least 15 g/day)
1 month Gain at least 300 g in the first month
If weighing daily with a precise and accurate scale
First week No weight loss or total less than 10%
Afterward daily gain in small babies at least 20 g
Scale maintenance
Daily/weekly weighing requires precise and accurate scale (10-g increment):
Calibrate it daily according to instructions.
Check it for accuracy according to instructions.
Simple spring scales are not precise enough for daily/weekly weighing.
Other breastfeeding support
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K8
OTHER BREASTFEEDING SUPPORT
Give special support to the mother
who is not yet breastfeeding
(Mother or baby ill, or baby too small to suckle)
Teach the mother to express breast milk K5 . Help her if necessary.
Use the milk to feed the baby by cup.
If mother and baby are separated, help the mother to see the baby or inform her about the babys
condition at least twice daily.
If the baby was referred to another institution, ensure the baby gets the mothers expressed breast
milk if possible.
Encourage the mother to breastfeed when she or the baby recovers.
If the baby does not have a mother
Give donated heat treated breast milk or home-based or commercial formula by cup.
Teach the carer how to prepare milk and feed the baby K6
.
Follow up in 2 weeks; weigh and assess weight gain.
Advise the mother who is not breastfeeding
at all on how to relieve engorgement
(Baby died or stillborn, mother chose replacement feeding)
Breasts may be uncomfortable for a while.
Avoid stimulating the breasts.
Support breasts with a well-fitting bra or cloth. Do not bind the breasts tightly as this may increase
her discomfort.
Apply a compress. Warmth is comfortable for some mothers, others prefer a cold compress to
reduce swelling.
Teach the mother to express enough milk to relieve discomfort. Expressing can be done a few times
a day when the breasts are overfull. It does not need to be done if the mother is uncomfortable. It
will be less than her baby would take and will not stimulate increased milk production.
Relieve pain. An analgesic such as ibuprofen, or paracetamol may be used. Some women use plant
products such as teas made from herbs, or plants such as raw cabbage leaves placed directly on
the breast to reduce pain and swelling.
Advise to seek care if breasts become painful, swollen, red, if she feels ill or temperature greater than 38C.
Pharmacological treatments to reduce milk supply are not recommended.
The above methods are considered more effective in the long term.
Ensure warmth for the baby
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K9
ENSURE WARMTH FOR THE BABY
Keep the baby warm
AT BIRTH AND WITHIN THE FIRST HOUR(S)
Warm delivery room: for the birth of the baby the room temperature should be 25-28C, no draught.
Dry baby: immediately after birth, place the baby on the mothers abdomen or on a warm, clean and
dry surface. Dry the whole body and hair thoroughly, with a dry cloth.
Skin-to-skin contact: Leave the baby on the mothers abdomen (before cord cut) or chest (after cord
cut) after birth for at least 2 hours. Cover the baby with a soft dry cloth.
If the mother cannot keep the baby skin-to-skin because of complications, wrap the baby in a clean,
dry, warm cloth and place in a cot. Cover with a blanket. Use a radiant warmer if room not warm or baby
small.
SUBSEQUENTLY (FIRST DAY)
Explain to the mother that keeping baby warm is important for the baby to remain healthy.
Dress the baby or wrap in soft dry clean cloth. Cover the head with a cap for the first few days, especially if
baby is small.
Ensure the baby is dressed or wrapped and covered with a blanket.
Keep the baby within easy reach of the mother. Do not separate them (rooming-in).
If the mother and baby must be separated, ensure baby is dressed or wrapped and covered with a
blanket.
Assess warmth every 4 hours by touching the babys feet: if feet are cold use skin-to-skin contact, add
extra blanket and reassess (see Rewarm the newborn).
Keep the room for the mother and baby warm. If the room is not warm enough, always cover the baby
with a blanket and/or use skin-to-skin contact.
AT HOME
Explain to the mother that babies need one more layer of clothes than other children or adults.
Keep the room or part of the room warm, especially in a cold climate.
During the day, dress or wrap the baby.
At night, let the baby sleep with the mother or within easy reach to facilitate breastfeeding.
Do not put the baby on any cold or wet surface.
Do not bath the baby at birth. Wait at least 6 hours before bathing.
Do not swaddle wrap too tightly. Swaddling makes them cold.
Do not leave the baby in direct sun.
Keep a small baby warm
The room for the baby should be warm (not less than 25C) with no draught.
Explain to the mother the importance of warmth for a small baby.
After birth, encourage the mother to keep the baby in skin-to-skin contact as long as possible.
Advise to use extra clothes, socks and a cap, blankets, to keep the baby warm or when the baby is
not with the mother.
Wash or bath a baby in a very warm room, in warm water. After bathing, dry immediately and
thoroughly. Keep the baby warm after the bath. Avoid bathing small babies.
Check frequently if feet are warm. If cold, rewarm the baby (see below).
Seek care if the babys feet remain cold after rewarming.
Rewarm the baby skin-to-skin
Before rewarming, remove the babys cold clothing.
Place the newborn skin-to-skin on the mothers chest dressed in a pre-warmed shirt open at the
front, a nappy (diaper), hat and socks.
Cover the infant on the mothers chest with her clothes and an additional (pre-warmed) blanket.
Check the temperature every hour until normal.
Keep the baby with the mother until the babys body temperature is in normal range.
If the baby is small, encourage the mother to keep the baby in skin-to-skin contact for as long as
possible, day and night.
Be sure the temperature of the room where the rewarming takes place is at least 25C.
If the babys temperature is not 36.5C or more after 2 hours of rewarming, reassess the baby J2J7 .
If referral needed, keep the baby in skin-to-skin position/contact with the mother or other person
accompanying the baby.
Other baby care
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K10
OTHER BABY CARE
Always wash hands before and after taking care of the baby. DO NOT share supplies with other babies.
Cord care
Wash hands before and after cord care.
Put nothing on the stump.
Fold nappy (diaper) below stump.
Keep cord stump loosely covered with clean clothes.
If stump is soiled, wash it with clean water and soap. Dry it thoroughly with clean cloth.
If umbilicus is red or draining pus or blood, examine the baby and manage accordingly J2J7 .
Explain to the mother that she should seek care if the umbilicus is red or draining pus or blood.
DO NOT bandage the stump or abdomen.
DO NOT apply any substances or medicine to stump.
Avoid touching the stump unnecessarily.
Sleeping
Use the bednet day and night for a sleeping baby.
Let the baby sleep on her/his back or on the side.
Keep the baby away from smoke or people smoking.
Keep the baby, especially a small baby, away from sick children or adults.
Hygiene (washing, bathing)
AT BIRTH:
Only remove blood or meconium.
DO NOT remove vernix.
DO NOT bathe the baby until at least 6 hours of age.
LATER AND AT HOME:
Wash the face, neck, underarms daily.
Wash the buttocks when soiled. Dry thoroughly.
Bath when necessary:
Ensure the room is warm, no draught
Use warm water for bathing
Thoroughly dry the baby, dress and cover after bath.
OTHER BABY CARE:
Use cloth on babys bottom to collect stool. Dispose of the stool as for womans pads. Wash hands.
DO NOT bathe the baby before 6 hours old or if the baby is cold.
DO NOT apply anything in the babys eyes except an antimicrobial at birth.
SMALL BABIES REQUIRE MORE CAREFUL ATTENTION:
The room must be warmer when changing, washing, bathing and examining a small baby.
Newborn resuscitation
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K11
NEWBORN RESUSCITATION
Start resuscitation within 1 minute of birth if baby is not breathing or is gasping for breath.
Observe universal precautions to prevent infection A4 .
Keep the baby warm
Clamp and cut the cord if necessary.
Transfer the baby to a dry, clean and warm surface.
Inform the mother that the baby has difficulty initiating breathing and that you will help the baby to breathe.
Keep the baby wrapped and under a radiant heater if possible.
Open the airway
Position the head so it is slightly extended.
Suction first the mouth and then the nose.
Introduce the suction tube into the newborns mouth 5-cm from lips and suck while withdrawing.
Introduce the suction tube 3-cm into each nostril and suck while withdrawing until no mucus.
Repeat each suction if necessary but no more than twice and no more than 20 seconds in total.
If still no breathing, VENTILATE:
Place mask to cover chin, mouth, and nose.
Form seal.
Squeeze bag attached to the mask with 2 fingers or whole hand, according to bag size, 2 or 3 times.
Observe rise of chest. If chest is not rising:
reposition head
check mask seal.
Squeeze bag harder with whole hand.
Once good seal and chest rising, ventilate at 40 squeezes per minute until newborn starts crying or
breathing spontaneously.
If breathing or crying, stop ventilating
Look at the chest for in-drawing.
Count breaths per minute.
If breathing more than 30 breaths per minute and no severe chest in-drawing:
do not ventilate any more
put the baby in skin-to-skin contact on mothers chest and continue care as on D19
monitor every 15 minutes for breathing and warmth
tell the mother that the baby will probably be well.
DO NOT leave the baby alone
If breathing less than 30 breaths per minute or
severe chest in-drawing:
continue ventilating
arrange for immediate referral
explain to the mother what happened, what you are doing and why
ventilate during referral
record the event on the referral form and labour record.
If no breathing or gasping at all
after 20 minutes of ventilation
Stop ventilating.The baby is dead.
Explain to the mother and give supportive care D24 .
Record the event.
Treat and immunize the baby (1)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K12
TREAT THE BABY
Treat the baby
Determine appropriate drugs and dosage for the babys weight.
Tell the mother the reasons for giving the drug to the baby.
Give intramuscular antibiotics in thigh. Use a new syringe and needle for each antibiotic.
Give 2 IM antibiotics (first week of life)
Give first dose of both ampicillin and gentamicin IM in thigh before referral for possible serious
illness, severe umbilical infection or severe skin infection.
Give both ampicillin and gentamicin IM for 5 days in asymptomatic babies classified at risk of
infection.
Give intramuscular antibiotics in thigh. Use a new syringe and needle for each antibiotic.
Ampicillin IM Gentamicin IM
Dose: 50 mg per kg Dose: 5 mg per kg
every 12 hours every 24 hours if term;
Add 2.5 ml sterile water 4 mg per kg every 24 hours if preterm
Weight to 500 mg vial = 200 mg/ml 20 mg per 2 ml vial = 10 mg/ml
1.0 1.4 kg 0.35 ml 0.5 ml
1.5 1.9 kg 0.5 ml 0.7 ml
2.0 2.4 kg 0.6 ml 0.9 ml
2.5 2.9 kg 0.75 ml 1.35 ml
3.0 3.4 kg 0.85 ml 1.6 ml
3.5 3.9 kg 1 ml 1.85 ml
4.0 4.4 kg 1.1 ml 2.1 ml
Give IM benzathine penicillin
to baby (single dose) if mother tested RPR-positive
Benzathine penicillin IM
Dose: 50 000 units/kg once
Add 5 ml sterile water to vial
containing 1.2 million units
= 1.2 million units/(6ml total volume)
Weight = 200 000 units/ml
1.0 - 1.4 kg 0.35 ml
1.5 - 1.9 kg 0.5 ml
2.0 - 2.4 kg 0.6 ml
2.5 - 2.9 kg 0.75 ml
3.0 - 3.4 kg 0.85 ml
3.5 - 3.9 kg 1.0 ml
4.0 - 4.4 kg 1.1 ml
Give IM antibiotic for possible gonococcal eye infection
(single dose)
Ceftriaxone (1st choice) Kanamycin (2nd choice)
Dose: 50 mg per kg once Dose: 25 mg per kg once, max 75 mg
Weight 250 mg per 5 ml vial=mg/ml 75 mg per 2 ml vial = 37.5 mg/ml
1.0 - 1.4 kg 1 ml 0.7 ml
1.5 - 1.9 kg 1.5 ml 1 ml
2.0 - 2.4 kg 2 ml 1.3 ml
2.5 - 2.9 kg 2.5 ml 1.7 ml
3.0 - 3.4 kg 3 ml 2 ml
3.5 - 3.9 kg 3.5 ml 2 ml
4.0 - 4.4 kg 4 ml 2 ml
Treat and immunize the baby (2)
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K13
Teach the mother to give treatment to the baby at home
Explain carefully how to give the treatment. Label and package each drug separately.
Check mothers understanding before she leaves the clinic.
Demonstrate how to measure a dose.
Watch the mother practice measuring a dose by herself.
Watch the mother give the first dose to the baby.
Treat local infection
TEACH MOTHER TO TREAT LOCAL INFECTION
Explain and show how the treatment is given.
Watch her as she carries out the first treatment.
Ask her to let you know if the local infection gets worse and to return to the clinic if possible.
Treat for 5 days.
TREAT SKIN PUSTULES OR UMBILICAL INFECTION
Do the following 3 times daily:
Wash hands with clean water and soap.
Gently wash off pus and crusts with boiled and cooled water and soap.
Dry the area with clean cloth.
Paint with gentian violet.
Wash hands.
TREAT EYE INFECTION
Do the following 6-8 times daily:
Wash hands with clean water and soap.
Wet clean cloth with boiled and cooled water.
Use the wet cloth to gently wash off pus from the babys eyes.
Apply 1% tetracycline eye ointment in each eye 3 times daily.
Wash hands.
REASSESS IN 2 DAYS:
Assess the skin, umbilicus or eyes.
If pus or redness remains or is worse, refer to hospital.
If pus and redness have improved, tell the mother to continue treating local infection at home.
Give isoniazid (INH) prophylaxis to newborn
If the mother is diagnosed as having tuberculosis and started treatment
less than 2 months before delivery:
Give 5-mg/kg isoniazid (INH) orally once a day for 6 months (1 tablet = 200-mg).
Delay BCG vaccination until INH treatment completed, or repeat BCG.
Reassure the mother that it is safe to breastfeed the baby.
Follow up the baby every 2 weeks, or according to national guidelines, to assess weight gain.
Immunize the newborn
Give BCG, OPV-0, Hepatitis B (HB-1) vaccine in the first week of life, preferably before discharge.
If un-immunized newborn first seen 1-4 weeks of age, give BCG only.
Record on immunization card and child record.
Advise when to return for next immunization.
Age Vaccine
Birth < 1 week BCG OPV-0 HB1
6 weeks DPT OPV-1 HB-2
Give ARV medicine to newborn
Give the first dose of ARV medicines to newborn 812 hours after birth:
Give Nevirapine 2 mg/kg once only.
Give Zidovudine 4 mg/kg every 12 hours.
If the newborn spills or vomits within 30 minutes repeat the dose.
Teach mother to give oral ARV medicines at home
Explain and show how the medicine is given.
Wash hands.
Demonstrate how to measure the dose on the spoon.
Begin feeding the baby by cup.
Give medicine by spoon before the end of the feed.
Complete the feed.
Watch her as she carries out the next treatment.
Explain to the mother that she should watch her baby after giving a dose of Zidovudine. If baby
vomits or spills within 30 minutes, she should repeat the dose.
Give Zidovudine every 12 hours for 7 days.
Advise when to return with the baby
B
R
E
A
S
T
F
E
E
D
I
N
G
,
C
A
R
E
,
P
R
E
V
E
N
T
I
V
E
M
E
A
S
U
R
E
S
A
N
D
T
R
E
A
T
M
E
N
T
F
O
R
T
H
E
N
E
W
B
O
R
N
K14
ADVISE WHEN TO RETURN WITH THE BABY
For maternal visits see schedule on D28 .
Routine visits
Return
Postnatal visit Within the first week, preferably
within 2-3 days
Immunization visit At age 6 weeks
(If BCG, OPV-0 and HB-1
given in the first week of life)
Follow-up visits
If the problem was: Return in
Feeding difficulty 2 days
Red umbilicus 2 days
Skin infection 2 days
Eye infection 2 days
Thrush 2 days
Mother has either:
breast engorgement or 2 days
mastitis. 2 days
Low birth weight, and either
first week of life or 2 days
not adequately gaining weight 2 days
Low birth weight, and either
older than 1 week or 7 days
gaining weight adequately 7 days
Orphan baby 14 days
INH prophylaxis 14 days
Treated for possible congenital syphilis 14 days
Mother HIV-positive 14 days
Advise the mother to seek care for the baby
Use the counselling sheet to advise the mother when to seek care, or when to return, if
the baby has any of these danger signs:
RETURN OR GO TO THE HOSPITAL IMMEDIATELY IF THE BABY HAS
difficulty breathing.
convulsions.
fever or feels cold.
bleeding.
diarrhoea.
very small, just born.
not feeding at all.
GO TO HEALTH CENTRE AS QUICKLY AS POSSIBLE IF THE BABY HAS
difficulty feeding.
pus from eyes.
skin pustules.
yellow skin.
a cord stump which is red or draining pus.
feeds <5 times in 24 hours.
Refer baby urgently to hospital
After emergency treatment, explain the need for referral to the mother/father.
Organize safe transportation.
Always send the mother with the baby, if possible.
Send referral note with the baby.
Inform the referral centre if possible by radio or telephone.
DURING TRANSPORTATION
Keep the baby warm by skin-to-skin contact with mother or someone else.
Cover the baby with a blanket and cover her/his head with a cap.
Protect the baby from direct sunshine.
Encourage breastfeeding during the journey.
If the baby does not breastfeed and journey is more than 3 hours, consider giving expressed breast
milk by cup K6 .
Equipment, supplies, drugs and laboratory tests
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
,
D
R
U
G
S
A
N
D
L
A
B
O
R
A
T
O
R
Y
T
E
S
T
S
L1
EQUIPMENT, SUPPLIES, DRUGS AND LABORATORY TESTS
Equipment, supplies, drugs and tests for pregnancy and postp artumcare
EQ
U
IPM
EN
T
, SU
PPLIES,
D
RU
GS AN
D
LABO
RATO
RY TESTS
L2
EQUIPMENT , SUPPLIES, DRUGS AND TESTS FOR R OUTINE AND EMERGENCY PREGNANCY AND POSTP ARTUM CARE
War m and clean room
Examination table or bed with clean linen Li ght source Heat source
Hand washing
Cl ean water supply Soap Nail br ush or stick Cl ean to wel s
Was te
Bucketfor soiled pads and s wabs Receptacle for soiled linens Container for sharps disposal
Sterilization
Instrument sterilizer Jar for forceps
Miscellaneous
Wa ll clock Torch with extra batteries and bulb Log book Records Refrigerator
Equipment
Bl ood pressure machine and stethoscope Bodythermometer Fetal stethoscope Babyscale
Supplies
Gl oves : ut ility sterile or highly disinfected long sterile for manual remo valofpl acenta Ur inary catheter Syringes and needles IVtubing Suture material for tear or episiotomy repair Antiseptic solution (iodophors or chlorhexidine) Spirit (70% alcohol) Swabs Bl each (chlorine base compound) Impregnated bednet Condoms
Tes ts
RPR testing kit Pr oteinuria sticks Container for catching urine HI V testing kit (2 t ypes) Haemoglobin testing kit
Disposable deliv erykit
Pl astic sheet to place under mother Cord ties (sterile) Sterile blade
Drugs
Ox ytocin Er gometrine Magnesium sulphate Calcium gluconate Di azepa m Hydralazine Ampici llin Gentamicin Metronidazole Benzathine penicillin Cl oxacillin Amoxycillin Ceftriaxone Tr imethoprim + sulfamethoxazole Cl otrimazole v aginal pessar y Erythromycin Ci profloxacin Tetracycline or doxycycline Ar themether or quinine Chloroquine tablet Li gnocaine Adrenaline Ri nger lactate Normal saline 0.9% Gl ucose 50% soluti on Wa ter for injection Paracetamol Gentian violet Iron/folic acid tablet Mebendazole Sulphadoxine-p yrimethamine Nevirapine (adult, infant) Zi dovudine (AZT) (adult, infant) Lamivudine (3TC)
Vaccine
Tetanus toxoid
Laborator y tests (1)
EQ
U
IPM
EN
T
, SU
PPLIES,
D
RU
GS AN
D
LABO
RATO
RY TESTS
L4
LABORA TORY TESTS
Check urine for protein
Label a clean container . Gi vewoman the clean container and explain w here she can urinate. Teach woman ho w to collect a clean-catch urine sample. Ask her to: Cl ean vulv a with water Spread labia with fing ers Ur inate freely (urine should not dribble o vervulva;this will r uin sample) Catch the middle par t of the stream of urine in the cup. Remov e container bef ore urine stops. Analyse urine for protein using either dipstick or boiling method.
DIPSTICK METHOD
Di p coated end of paper dipstick in urine sample. Shakeoff excess b y tapping ag ainst side of container . Wa it specified time (see dipstick instr uctions). Compare with colour char t on label. Colours rang e from y ellow(negativ e) through y ellow-g reen and green-blue for positiv e.
BOI LING METHOD
Put urine in test tube and boil top half. Boiled par t ma y become cloud y.After boiling allo w the test tube to stand. Athick precipitate at the bottom of the tube indicates p rotein. Add 2-3 drops of 2-3% acetic acid after boiling the urine (e venifur ine is not cloud y) Ifthe urine remains cloud y,protein is present in the urine. Ifcl oudyurine becomes clear , protein is not present. Ifboiled urine was not cloud y to begin with, but becomes cloud y when acetic acid is added, protein is present.
Check haemoglobin
Dr awblood with syri ngeand needl e or a st erilelancet. Insertbelowinstructions for meth od used loc ally.
____________________________________________________________________
____________________________________________________________________
EQ
U
IPM
EN
T
, SU
PPLIES,
D
RU
GS AN
D
LABO
RATO
RY TESTS
L6 Per formRapid HIV test (type of test use depends on the nation al policy )
PERFORM RAPID HIV TEST (TYPE OF TEST USE DEPENDS ON THE NA TIONAL POLI CY)
Explain the procedure and seek consent according to the national pol icy. Use test kits recommended b y the national and/or inter national bodies and follo w the instr uctions of the HIV rapid test selected. Pr epare y our w orksheet, label the test, and indicate the test batch num ber and expir y date. Check that expir y time has not lapsed. We ar glo veswhen dra wing blood and follo w standard safety precautio ns for waste disposal. Informthe w omen w hen to retur n to the clinic for their test results (s ame da y or the y will ha veto come ag ain). Dr awblood for all tests at the same time (tests for Hb , syphilis and HIV can often be coupled at the same time). Use a sterile needle and syring e when dra wing blood from a v ein. Use a lancet w hen doing a fing er prick. Perfor m the test follo wing manufacturer s instr uctions. Interpret the results as per the instr uctions of the HIV rapid test sele cted. Ifthe first test result is neg ative, nofurther testing is done. Record the result as Neg ativefor HIV . Ifthe first test result is positiv e,perfor m a second HIV rapid test u sing a different test kit. Ifthe second test is also positiv e,record the result as P ositive for HIV . Ifthe first test result is positiv e and second test result is neg ative, record the result as inconclusive. Repeat the test after 6 w eeks or refer the w oman to hospital for a confir matory test. Send the results to the health w orker . Respect confidentiality A2. Record all results in the logbook.
Equipment, suplies and dr ugs
Per formrapid plasmareagin (RPR) test for syphilis
Seek consent.
Explain procedure.
Use a sterile needle and syring e.Drawup 5 ml blood from a v ein. Put in a clear test tube.
Let test tube sit 20 minutes to allo w ser um to separate (or centrifug e 3-5 minutes at 2 000 3000-rpm). In the separated sample, serumwi ll be on top.
Use sampling pipette to withdra w some of the ser um. Tak e care not to include an y red blood cells from the lo werpartof the separated sampl e.
Hold the pipette v ertically overa t est card circle. Squeeze teat to allo w one drop (50 -l) of ser um to fall onto a circle. Spread the drop to fill the circle using a toothpick or other clean spreader .
Important: Several samples ma y be tested on one card. Becareful not to contaminate the remaining test cir cles.Use a clean spreader for ever y sample. Carefully label each sample with a patients name or number .
At tach dispensing needle to a syring e.Shakeantigen.* Drawup enough antig en for the number of tests to be done (one drop per test).
Holding the syring e vertically , allowexactly one drop of antig en (20 -l) to fall onto each test sample . DO NO T stir .
Rotate the test card smoothly on the palm of the hand for 8 minutes.** (Or rotate on a mechanical rotator .)
* Mak e sure antig en was refrig erated (not frozen) and has not expired.
** Room temperature should be 73-85F (22.829.3C).
Laborator y tests (2) Per formrapid plasmareagin (RPR) test for syphilis
EQ
U
IPM
EN
T
, SU
PPLIES AN
D
D
RU
GS
L5
EQ
U
IPM
EN
T
, SU
PPLIES,
D
RU
GS AN
D
LABO
RATO
RY TESTS
PERFORM RAPID PLASMAREA GIN (RPR) TEST FOR SYPHILIS
Interpreting results
Af ter 8 minutes r otat ion, inspect the card in g ood light. Turnor lif t the card to see whe ther there is clumping (react iveresult). Most test cards include neg ativeand positiv e contr ol circ les for comparison.
1. Non-reactive (no clumping or only slight roughness) Neg ativefor syphilis 2.Reactive (highly visi ble clumping) - P ositive for syphilis 3. We akly reactive (minimal clumping) - P ositive for syphilis
NOTE: Wea kly reactiv e can al so be more fi nely g ranulated and difficult to see than in this illsu
EXAMPLE OF A TEST CARD
1 2 3
Equipment, suplies and dr ugs
War m and clean room
Deliver y bed: a bed that suppor ts the w oman in a semi-sitting or lying in a lateral position, wi th remo vable stir rups (only for repairing the perineum or instr umental deliv ery) Cl ean bed linen Curtains if more than one bed Cl ean surface (for alter native deliver y position) Wo rk surface for resuscitation of ne wborn near deliv erybeds Li ght source Heat source Room ther mometer
Hand washing
Cl ean water supply Soap Nail br ush or stick Cl ean to wel s
Was te
Container for sharps disposal Receptacle for soiled linens Bucketfor soiled pads and s wabs Bowl and plastic bag for placenta
Sterilization
Instrument sterilizer Jar for forceps
Miscellaneous
Wa ll clock Torch with extra batteries and bulb Log book
Equipment, supplies and dr ugs for childbir th care
EQ
U
IPM
EN
T
, SU
PPLIES AN
D
D
RU
GS
L3
EQ
U
IPM
EN
T
, SU
PPLIES,
D
RU
GS AN
D
LABO
RATO
RY TESTS
EQUIPMENT , SUPPLIES AND DRUGSFOR CHILDBIRTH CARE
Equipment
Bl oodpr essure machine and stethoscope Bodythermometer Fetal stethoscope Babyscale Self inflating bag and mask - neon atal size Mucusextractor with suction tube
Deliver y instr uments (sterile)
Scissors Needle holder Ar teryforceps or clamp Di ssecting forceps Spongeforceps Vaginal speculum
Supplies
Gl oves: ut ility sterile or highly disinfected long sterile for manual remo valofpl acenta Long plastic apron Ur inary catheter Syringes and needles IVtubing Suture material for tear or episiotomy repair Antiseptic solution (iodophors or chlorhexidine) Spirit (70% alcohol) Swabs Bl each (chlorine-base compound) Cl ean (plastic) sheet to pla ce under mother Sanitary pads Cl ean to wel s for dr ying and wrapping the bab y Cord ties (sterile) Bl anket for the bab y Babyfeeding cup Impregna ted bednet
Drugs
Ox ytocin Er gometrine Magnesium sulphate Calcium gluconate Di azepa m Hydralazine Ampici llin Gentamicin Metronidazole Benzathine penicillin Li gnocaine Adrenaline Ri nger lactate Normal saline 0.9% Wa ter for injection Eye anti microbial (1% silv er nitrate or 2.5% po vidone iodine) Tetracycline 1% e yeointment Vi tamin A Izoniazid Nevirapine (adult, infant) Zi dovudine (AZT) (adult, infant) Lamivudine (3TC)
Vaccine
BCG OPV Hepatitis B
Contracept ives
(seeDecision-making tool for family planning provide rsand clients )
Tes t
RPR test ing kits HI V testing kits (2 types) Haemoglobin testing kit
L2
EQUIPMENT, SUPPLIES, DRUGS
AND TESTS FOR ROUTINE AND
EMERGENCY CARE
L3 EQUIPMENT, SUPPLIES AND DRUGS
FOR CHILDBIRTH CARE
L4 LABORATORY TESTS (1)
Check urine for protein
Check haemoglobin
L5 LABORATORY TESTS (2)
Perform rapid plamareagin (RPR) test for
syphilis
L6 LABORATORY TESTS (3)
Perform rapid test for HIV
Equipment, supplies, drugs and tests for pregnancy and postpartum care
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
,
D
R
U
G
S
A
N
D
L
A
B
O
R
A
T
O
R
Y
T
E
S
T
S
L2
EQUIPMENT, SUPPLIES, DRUGS AND TESTS FOR ROUTINE AND EMERGENCY PREGNANCY AND POSTPARTUM CARE
Warm and clean room
Examination table or bed with clean linen
Light source
Heat source
Hand washing
Clean water supply
Soap
Nail brush or stick
Clean towels
Waste
Bucket for soiled pads and swabs
Receptacle for soiled linens
Container for sharps disposal
Sterilization
Instrument sterilizer
Jar for forceps
Miscellaneous
Wall clock
Torch with extra batteries and bulb
Log book
Records
Refrigerator
Equipment
Blood pressure machine and stethoscope
Body thermometer
Fetal stethoscope
Baby scale
Supplies
Gloves:
utility
sterile or highly disinfected
long sterile for manual removal of placenta
Urinary catheter
Syringes and needles
IV tubing
Suture material for tear or episiotomy repair
Antiseptic solution (iodophors or chlorhexidine)
Spirit (70% alcohol)
Swabs
Bleach (chlorine base compound)
Impregnated bednet
Condoms
Alcohol-based handrub
Tests
Syphilis testing (e.g. RPR)
Proteinuria dip sticks
Container for catching urine
HIV testing kit (2 types)
Haemoglobin testing kit
Disposable delivery kit
Plastic sheet to place under mother
Cord ties (sterile)
Sterile blade
Drugs
Oxytocin
Ergometrine
Magnesium sulphate
Calcium gluconate
Diazepam
Hydralazine
Ampicillin
Gentamicin
Metronidazole
Benzathine penicillin
Cloxacillin
Amoxycillin
Ceftriaxone
Trimethoprim + sulfamethoxazole
Clotrimazole vaginal pessary
Erythromycin
Ciprofloxacin
Tetracycline or doxycycline
Arthemether or quinine
Chloroquine tablet
Lignocaine
Adrenaline
Ringer lactate
Normal saline 0.9%
Glucose 50% solution
Water for injection
Paracetamol
Gentian violet
Iron/folic acid tablet
Mebendazole
Sulphadoxine-pyrimethamine
Nevirapine (adult, infant)
Zidovudine (AZT) (adult, infant)
Lamivudine (3TC)
Vaccine
Tetanus toxoid
Equipment, suplies and drugs
Warm and clean room
Delivery bed: a bed that supports the woman in a semi-sitting or
lying in a lateral position, with removable stirrups (only for repairing
the perineum or instrumental delivery)
Clean bed linen
Curtains if more than one bed
Clean surface (for alternative delivery position)
Work surface for resuscitation of newborn near delivery beds
Light source
Heat source
Room thermometer
Hand washing
Clean water supply
Soap
Nail brush or stick
Clean towels
Waste
Container for sharps disposal
Receptacle for soiled linens
Bucket for soiled pads and swabs
Bowl and plastic bag for placenta
Sterilization
Instrument sterilizer
Jar for forceps
Miscellaneous
Wall clock
Torch with extra batteries and bulb
Log book
Records
Refrigerator
Equipment, supplies and drugs for childbirth care
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
A
N
D
D
R
U
G
S
L3
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
,
D
R
U
G
S
A
N
D
L
A
B
O
R
A
T
O
R
Y
T
E
S
T
S
EQUIPMENT, SUPPLIES AND DRUGS FOR CHILDBIRTH CARE
Equipment
Blood pressure machine and stethoscope
Body thermometer
Fetal stethoscope
Baby scale
Self inflating bag and mask - neonatal size
Mucus extractor with suction tube
Delivery instruments (sterile)
Scissors
Needle holder
Artery forceps or clamp
Dissecting forceps
Sponge forceps
Vaginal speculum
Supplies
Gloves:
utility
sterile or highly disinfected
long sterile for manual removal of placenta
Long plastic apron
Urinary catheter
Syringes and needles
IV tubing
Suture material for tear or episiotomy repair
Antiseptic solution (iodophors or chlorhexidine)
Spirit (70% alcohol)
Swabs
Bleach (chlorine-base compound)
Clean (plastic) sheet to place under mother
Sanitary pads
Clean towels for drying and wrapping the baby
Cord ties (sterile)
Blanket for the baby
Baby feeding cup
Impregnated bednet
Alcohol-based handrub
Drugs
Oxytocin
Ergometrine
Magnesium sulphate
Calcium gluconate
Diazepam
Hydralazine
Ampicillin
Gentamicin
Metronidazole
Benzathine penicillin
Lignocaine
Adrenaline
Ringer lactate
Normal saline 0.9%
Water for injection
Eye antimicrobial (1% silver nitrate or 2.5% povidone iodine)
Tetracycline 1% eye ointment
Vitamin A
Izoniazid
Nevirapine (adult, infant)
Zidovudine (AZT) (adult, infant)
Lamivudine (3TC)
Vaccine
BCG
OPV
Hepatitis B
Contraceptives
(see Decision-making tool for family planning providers and clients)
Test
Syphilis testing (e.g. RPR)
Proteinuria dip sticks
Container for catching urine
HIV testing kits (2 types)
Haemoglobin testing kit
Laboratory tests (1)
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
,
D
R
U
G
S
A
N
D
L
A
B
O
R
A
T
O
R
Y
T
E
S
T
S
L4
LABORATORY TESTS
Check urine for protein
Label a clean container.
Give woman the clean container and explain where she can urinate.
Teach woman how to collect a clean-catch urine sample. Ask her to:
Clean vulva with water
Spread labia with fingers
Urinate freely (urine should not dribble over vulva; this will ruin sample)
Catch the middle part of the stream of urine in the cup. Remove container before urine stops.
Analyse urine for protein using either dipstick or boiling method.
DIPSTICK METHOD
Dip coated end of paper dipstick in urine sample.
Shake off excess by tapping against side of container.
Wait specified time (see dipstick instructions).
Compare with colour chart on label. Colours range from yellow (negative) through yellow-green and
green-blue for positive.
BOILING METHOD
Put urine in test tube and boil top half. Boiled part may become cloudy. After boiling allow the test
tube to stand. A thick precipitate at the bottom of the tube indicates protein.
Add 2-3 drops of 2-3% acetic acid after boiling the urine (even if urine is not cloudy)
If the urine remains cloudy, protein is present in the urine.
If cloudy urine becomes clear, protein is not present.
If boiled urine was not cloudy to begin with, but becomes cloudy when acetic acid is added,
protein is present.
Check haemoglobin
Draw blood with syringe and needle or a sterile lancet.
Insert below instructions for method used locally.
____________________________________________________________________
____________________________________________________________________
Equipment, suplies and drugs
Perform rapid plasmareagin (RPR) test for syphilis
Seek consent.
Explain procedure.
Use a sterile needle and syringe. Draw up 5 ml blood from a vein. Put in a clear test tube.
Let test tube sit 20 minutes to allow serum to separate (or centrifuge 3-5 minutes at 2000
3000-rpm). In the separated sample, serum will be on top.
Use sampling pipette to withdraw some of the serum.
Take care not to include any red blood cells from the lower part of the separated sample.
Hold the pipette vertically over a test card circle. Squeeze teat to allow one drop (50-l) of serum to
fall onto a circle. Spread the drop to fill the circle using a toothpick or other clean spreader.
Important: Several samples may be tested on one card. Be careful not to contaminate the
remaining test circles. Use a clean spreader for every sample. Carefully label each sample with a
patients name or number.
Attach dispensing needle to a syringe. Shake antigen.*
Draw up enough antigen for the number of tests to be done (one drop per test).
Holding the syringe vertically, allow exactly one drop of antigen (20-l) to fall onto each test sample.
DO NOT stir.
Rotate the test card smoothly on the palm of the hand for 8 minutes.**
(Or rotate on a mechanical rotator.)
* Make sure antigen was refrigerated (not frozen) and has not expired.
** Room temperature should be 73-85F (22.829.3C).
Laboratory tests (2) Perform rapid plasmareagin (RPR) test for syphilis
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
A
N
D
D
R
U
G
S
L5
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
,
D
R
U
G
S
A
N
D
L
A
B
O
R
A
T
O
R
Y
T
E
S
T
S
PERFORM RAPID PLASMAREAGIN (RPR) TEST FOR SYPHILIS
Interpreting results
After 8 minutes rotation, inspect the card in good light. Turn or lift the card to see whether there
is clumping (reactive result). Most test cards include negative and positive control circles for
comparison.
1. Non-reactive (no clumping or only slight roughness) Negative for syphilis
2. Reactive (highly visible clumping) - Positive for syphilis
3. Weakly reactive (minimal clumping) - Positive for syphilis
NOTE: Weakly reactive can also be more finely granulated and difficult to see than in this illsutration.
EXAMPLE OF A TEST CARD
1 2 3
E
Q
U
I
P
M
E
N
T
,
S
U
P
P
L
I
E
S
,
D
R
U
G
S
A
N
D
L
A
B
O
R
A
T
O
R
Y
T
E
S
T
S
L6
Perform Rapid HIV test
PERFORM RAPID HIV TEST (TYPE OF TEST USE DEPENDS ON THE NATIONAL POLICY)
Explain the procedure and seek consent according to the national policy.
Use test kits recommended by the national and/or international bodies and follow the instructions
of the HIV rapid test selected.
Prepare your worksheet, label the test, and indicate the test batch number and expiry date. Check
that expiry time has not lapsed.
Wear gloves when drawing blood and follow standard safety precautions for waste disposal.
Inform the women when to return to the clinic for their test results (same day or they will have to
come again).
Draw blood for all tests at the same time (tests for Hb, syphilis and HIV can often be coupled at the
same time).
Use a sterile needle and syringe when drawing blood from a vein.
Use a lancet when doing a finger prick.
Perform the test following manufacturers instructions.
Interpret the results as per the instructions of the HIV rapid test selected.
If the first test result is negative, no further testing is done. Record the result as Negative for HIV.
If the first test result is positive, perform a second HIV rapid test using a different test kit.
If the second test is also positive, record the result as Positive for HIV.
If the first test result is positive and second test result is negative, record the result as
inconclusive. Repeat the test after 6 weeks or refer the woman to hospital for a confirmatory test.
Send the results to the health worker. Respect confidentiality A2 .
Record all results in the logbook.
Information and counselling sheets
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M1
INFORMATION AND COUNSELLING SHEETS
CARE DURING PREGNANCY
Care during pregnancy
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
GM2
Visit the health w orker during pregnancy
Gotothe health centre if y ou think y ou are pregnant. Itisimportant to begin care as ear ly in y our pregnancy as possible. Vi sit the health centre at least 4 times during y our pregnancy , evenifyou do not ha veanyproblems. The health w orker will tell y ou when to retur n. Ifatany time y ou ha veanyconcerns about y our or y our bab yshealth, goto the health cen tre. During y our visits to the health centre, the health w orker will: Check y our health and the prog ress of the pregnancy Help y ou mak e a bir th plan Answer questions or concer ns y ou ma y ha ve Pr ovi de treatment for malaria and anaemia Gi veyoua t etanus toxoid immunization Advise and counsel on: breastfeeding bi rthspacing after deliv ery nutrition HI V counselling and testing correct and consistent condom use laborator y tests ot her matters related to y our and y our bab yshealth. Bring y our home-based mater nal record to e ver y visit.
Care for y ourself during pregnancy
Eat more and healthier foods, including more fr uits and v egetables, beans, meat, fish, eggs, cheese, milk. Takeiron tablets e ver y da y as explained b y the health w orker . Rest when y ou can. Avoid lifting hea vy objects. Sleep under a bednet treated with insecticide. Donot tak e medication unless prescribed at the health centre. Donot drink alcohol or smok e. Use a condom cor rectly in e ver y sexual relation to pre vent sexually tra nsmitted infection (STI) or HIV/AIDS if y ou or y our companion are at risk of infection.
PREGNANCY IS A SPECIAL TIME. CARE FOR YOURSELF AND Y OUR BABY .
Routine visits to the healt h centre
1st visitBefore 4 months 2nd visit 6-7 months 3rd visit 8months 4th visit 9months
Knowthe signs of labo ur
If y ou ha veanyof these s igns, goto the he althcentre as soon as y ou can. If these signs conti nue for 12 hours or more, you need to g o immedia tely. Painful contraction s ever y 20 minutes or less . Bag of water break s. Bl oodysticky discharg e.
When to seek care on dang er signs
Go to the hospital or health centreimmediately, day or nig ht,DO NO T wait,ifany of the follo wing signs: vaginal bleeding convulsions/fits sever e headaches with blur red vision feverand too w eak to g et out of bed sever e abdominal pain fast or difficult breat hing.
Go to the health centr eas soon as possibl e ifany of the following signs: fever abdominal pain water breaks and not inlabour after 6 hours feel ill swollen fing ers, face and legs.
PREPARING A BIRTH AND EMERGENCY PLAN
Preparing a bir th and emergency plan
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EET
S
M3
Preparing a bir th plan
The health w orker will pro vide y ou with infor mation to help y ou prepare a bir th plan. Based on y our health condition, the health w orker can mak e sugg estions as to w here it w ould be best to deliv er. Whether in a hospital, health centre or at home, itisimportant to deliv er with a skilled attendan t.
ATEVERY VISIT T O THE HEALTH CENTRE, REVIEWAND DISCUSS Y OUR BIRTH PLAN. The plan can chang e if complications develop.
Planning for deliv eryat home
Wh o do y ou choose to be the skilled attendant for deliv ery? Wh o will suppor t you during labour and deliv ery? Wh o will be close b y for at least 24 hours after deliv ery? Wh o will help y ou to care for y our home and other children? Or ganize the follo wing: Aclean and war m room or cor ner of a room. Home-based mater nal record. A clean deliv erykit which includes soap, a stick to clean under the nails, a new razor blade to cu t the bab yscord, 3 pieces of string (about 20 cm. each) to tie the cord. Cl ean cloths of different sizes: for the bed, for dr ying and wrapping the bab y,for cleaning the babyseyes, and for y ou to use as sanitar y pads. Wa rmcovers for y ou and the bab y. Wa rmspot for the bir th with a clean surface or clean cloth. Bowls: tw o for washing and one for the placenta. Pl astic for wrapping the placenta. Bucketsof clean water and some wa y to heat this water . For hand washing, water,soap and a to welorcl oth for dr ying hands of the bir th attendant. Fr esh drinking water , fluids and food for the mother .
Preparing an emerg ency plan
Topl an for an emerg ency, consider: Wh ere should y ou g o? How will y ou g et there? Wi ll you ha veto pa y for transpor t to g et there? Ho w muc h will it cost? Wh at costs will y ou ha veto pa y at the health centre? Ho w will y ou pa y for this? Can you star t saving for these possible costs no w? Wh o will g o with y ou to the health centre? Wh o will help to care for y our home and othe r chil dren w hile y ou are a way?
Planning for deliv eryat the hospital orhealth centre
How will y ou g et there? Wil l you ha veto pa y for transpor t to g et ther e? How much will it cos t to deliv er at the facility? Ho w will y ou pa y for t his? Can you star t saving for these costs no w? Wh o will g o with y ou and suppo rtyouduringlabour and deliv ery? Wh o will help y ou while y ou are a wayand care for y our home and othe r children? Bring the follo wing: Home-based mater nal record. Cl ean cloths of dif ferent sizes: for the bed, for dr ying and wrapping the bab y,and for y ou to use as sanitary pads. Cl ean clothes for youand the bab y. Food and water fo r you and the suppor t person.
CARE FOR THE MO THER AFTER BIRTH
Care for the mother after bir th
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EETS
M4
Care of the mother
Eat more and healthier foods, including more meat, fi sh,oils, coconut, nuts, cereals, beans, vegetables, fruits, cheese and milk. Takeiron tablets as explained b y the health w orker . Rest when y ou can. Dr ink plenty of clean, safe water . Sleep under a bednet treated with insecticide. Donot tak e medication unless prescribed at the health centre. Donot drink alcohol or smok e. Use a condom in e ver y sexual relation, ifyou or y our companion are a t risk of sexually transmi tted infections (STI) or HIV/AIDS . Wa sh all o verdaily,parti cularly the perineum. Changepad e ver y 4 to 6 hours. Wa sh pad or dispose of it safely .
Family planning
You can become pregnant within se ver al weeks after deliv eryif y ou ha vesexual relations and are not breastfeeding exclusiv ely. Talk to the health w orker about choosing a family planning method w hich best meets y our and y our partner sneeds.
Routine visits to the health cent re
Fir st week after bir th:
____________________________________________________________________
____________________________________________________________________
6 weeks after bir th: ____________________________________________________________________
____________________________________________________________________
When to seek care for dang er signs
Go to hospital or healt h centre immediately , dayor night, DONOTwait,if an y of the follo wing signs: Vaginal bleeding has in creased. Fi ts. Fast or difficult breat hing. Feverand too w eak to g et out of bed. Sever e headaches with blur red vision.
Go to health centre as soon as possibl e ifany of the following signs: Swollen, red or tender breasts or nipples. Pr oblems urinating , or leaking . Increased pain or infect ion in the per ineum. Infection in the area of the wound. Smelly v aginal discharg e.
CARE AFTER AN AB ORTION
Care after an abor tion
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EET
S
M5
Self-care
Rest for a fe w da ys,especially if y ou feel tired. Changepads e ver y 4 to 6 hours. Was h used pad or dispose of it s afely. Wa sh perineum. Donot havesexual intercourse until bleeding stops. You and y our par tner should use a condom cor rectly in e ver y act of sexual in tercourse if at risk of STI or HIV . Returnto the health w orker as indicated.
Family planning
Remember y ou can become pregnant as soon as y ou ha vesexual relations. Use a family planning method to pre vent an unwanted pregnancy . Talk to the health w orker about choosing a family planning method w hich best meets y our and y our partner sneeds.
Knowthese dang er signs
If y ou ha veanyof these si gns, goto the he althcentre immediately , dayor night. DONOT wait: Increased bleeding or continued bleeding for 2 da ys. Fever , feeling ill. Di zziness or fainting . Abdominal pain. Backache. Nausea, vomiting. Foul-smelling v aginal disch arge.
Additional suppor t
The health w orker can help y ou identify persons or g roups whocan pro vide y ou with additional supp ortif y ou should need it.
CARE FOR THE BABY AFTER BIRTH
Care for the baby after bir th
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EETS
M6
Care of the ne wborn
KEEP Y OUR NEWB ORN CLEAN Wa sh y our bab ysface and neck daily . Bathe her/him w hen necessar y.After bathing , thoroughly dr y your bab y and then dress and k eep her/him war m. Wa sh bab ysbottom w hen soiled and dr y it thoroughly . Wa sh y our hands with soap and water before and after handling y our bab y,especially after touching her/his bottom.
CARE FOR THE NEWB ORNS UMBILICAL CORD Keep cord stump loosely co ver ed with a clean cloth. Fold diaper and clothes belo w stump. Donot put an ything on the stump. Ifstump area is soiled, wash with clean water and soap. Then dr y completely wit h clean cloth. Wa sh y our hands with soap and water before and after care.
KEEP Y OUR NEWB ORN WARM Incold climates, keep at least an area of the room war m. Newborns need more clothing than other children or adults. Ifcold,put a hat on the bab yshead.During cold nights, coverthe bab y with an extra blank et.
OTHER AD VICE Let the bab y sleep on her/his back or side. Keep the bab y awayfrom smok e.
Routine visits to the health cent re
First week after bir th:
____________________________________________________________________
____________________________________________________________________
At 6 weeks :
____________________________________________________________________
____________________________________________________________________
At these visits y our bab y wil l be v accinated. Haveyour bab y immunize d.
When to seek care for dang er signs
Go to hospital or healt h centre immediately , dayor night, DONOT wait,ifyour bab y has an y of the follo wing signs: Di fficult breathing Fi ts Fever Feels cold Bl eeding Stops feeding Di arr hoea.
Go to the health centre as soon as possibl e ifyour bab y has an y of the follo wing signs: Di fficulty feeding . Feeds less than e ver y 5 hours. Pus coming from the eyes. Irritated cord with pus or bl ood. Yelloweyes or skin.
BREASTFEEDING
Breastfeeding
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EET
S
M7
Breastfeeding has man y advantages
FOR THE BABY During the first 6 months of life, the bab y needs nothing more than bre ast milk not water , not other milk, not cereals, not teas, not juices. Breast milk contains exactly the water and nutrients that a bab ysbodyneeds. It is easily dig ested and efficiently used b y the bab ysbody . It helps protect ag ainst infections and allergie s and helps the bab ysgrow th and de vel opment.
FOR THE MOTHER Postpartum bleeding can be reduced due to uterine contractions caused bythe bab yssucking. Breastfeeding can help dela y a ne w pregnancy .
FOR THE FIRST 6 MONTHS OF LIFE, GIVE ONL Y BREAST MILK TOYOUR BABY , DAYAND NIGHT AS OFTEN AND AS LONG AS SHE/HE WANTS .
Sugg estions for successful breastfeeding
Immediately after bir th,keepyour bab y in the bed with y ou,or within easy reach. Startbreastfeeding within 1 hour of bir th. The bab yssuck stimulates y our milk production. The more the bab y feeds, the more milk y ou will produce. Ateach feeding , let the bab y feed and release y our breast, and then offer y our second breast. Atthe next feeding , alternate and begin with the second breast. Gi veyour bab y the first milk (colostr um). It is nutritious and has antibo dies to help k eep y our bab y health y. Atni ght, let y our bab y sleep with y ou,within easy reach. Wh ile breastfeeding , you should drink plenty of clean, safe water . You should eat more and healthier foods and rest w hen y ou can.
The health w orker can suppo rtyouin
starting and maintai ning breastfe eding
The health w orker can help y ou to cor rectly position the bab y and ens ure she/he attaches to the breast. This will reduce breast problems for the mother . The health w orker can sho w y ou ho w to express milk from y our breas t with y our hands. Ifyou should need to lea vethe bab y with another caretak er for shor t periods, you can lea veyour milk and it can be giv en to the bab y in a cup. The health w orker can put y ou in cont act wit h a brea stfee ding suppor t group.
If you ha ve an y difficulti es with br eastfeeding , see the health w orker immediately .
Breastfeeding and family planning
During the first 6 month s afte r bir th,if y ou breastfeed exclusiv ely,day and night, and your menstruation has not r eturned, you are protected ag ainst another pregnancy . Ifyou do not meet t hese requirements, orifyou wish to use another family planning method w hile breastfeeding, di scuss the dif ferent options a vai lable with the health w orker .
M2
CARE DURING PREGNANCY
Visit the health worker during pregnancy
Care for yourself during pregnancy
Routine visits to the health centre
Know the signs of labour
When to seek care on danger signs
M3
PREPARING A BIRTH AND
EMERGENCY PLAN
Preparing a birth plan
Planning for delivery at home
Preparing an emergency plan
Planning for delivery at the hospital or health
centre
M4
CARE FOR THE MOTHER
AFTER BIRTH
Care of the mother
Family planning
Routine visits to the health centre
When to seek care for danger signs
M5 CARE AFTER AN ABORTION
Self-care
Family planning
Know these DANGER signs
Additional support
M6 CARE FOR THE BABY
AFTER BIRTH
Care of the newborn
Routine visits to the health centre
When to seek care for danger signs
M7 BREASTFEEDING
Breastfeeding has many advantages for the
baby and the mother
Suggestions for successful breastfeeding
Health worker support
Breastfeeding and family planning
CLEAN HOME DELIVER Y
Regardless of the site of deliver y,it is strongly recommended that all women deliver with a skilled attendant.
Fora woman who prefers to deliver at home the following recommendations are provided for a clean home deliver y to be reviewed during antenatal care visits.
Clean home deliver y (1)
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EETS
M8
Deliver y at home with an attendant
Ensure the attendant and other family members kno w the emerg ency plan and are a ware of dang er signs for y ourself and y our bab y. Ar range for a suppor t person to assist the attendant and to sta y with y ou during labour and after deliver y. Havethese supplies org anized for a clean deliv ery:new razor blade, 3 pieces of string about 20-cm each to tie the cord, and clean cloths to co verthe bir th place. Pr epare the home and the supplies indicated for a safe bir th: Cl ean, warmbirthplace with fresh air and a source of light Cl ean war m blank et to co veryou Cl ean cloths: for dr ying and wrapping the bab y for cleaning the bab yseyes touse as sanitar y pads after bir th todry your bod y after washing for bir th attendant to dr y her hands. Cl ean clothes for y ou to w ear after deliv ery Fr esh drinking water , fluids and food for y ou Bucketsof clean water and soap for washing , for y ou and the skill ed attendant Means to heat water Three bo wls, twofor washing and one for the placenta Pl astic for wrapping the placenta Bucketfor y ou to urinate in.
Instructions to mother and famil y
for a clean and safer d eliver y at home
Makesure there is a cle an deliv erysurface for the bir th of the bab y. Ask the attendant to wash her hands before touching y ou or the bab y.The nails of the attendant should be shor t and cl ean. Wh en the bab y is bor n,placeher/him on y our abdomen/chest w here it is war m and clean. Dry the baby thoroughly and wipe the face with a clean cloth. Then co verwi th a clean dr y clot h. Cut the cord w hen it stops pulsating , using the disposable deliv erykit, according to instr uctions. Wa it for the placenta todeliver on its o wn. Makesure y ou and y our bab y are war m.Hav e the bab y near y ou,dressed or wrapped and w ith head covered with a cap. Startbreastfeeding w hen the bab y sho ws signs of readiness, wi thin the first hour of bir th. Di spose of placenta ___ __________________________________________ (describe cor rect, safe culturally accepted wa y to dispose of plac enta)
DO NO Tbeal one for th e 24 hour s after deliv ery . DO NO Tbath the bab y on the fi rst da y.
Clean home deliver y (2)
IN
FO
RM
ATIO
N
AN
D
CO
U
N
SELLIN
G SH
EET
S
M9
Avoid harmful practices
FOR EXAMPLE: DO NO Tuse local medications to hasten labour . DO NO Twait for waters to stop before g oing to health facility . DO NO Tinsertanysubstances into the v agina during labour or after del iver y. DO NO Tpush on the abdomen during labour or deliv ery . DO NO Tpull on the cord to deliv er the placenta. DO NO Tput ashes, cow dung or other substance on umbilical cord/stump.
____________________________________________________________________
____________________________________________________________________
Encourage helpful traditional practices:
____________________________________________________________________
____________________________________________________________________
Danger signs during deliv ery
If y ou or y our bab y has an y of these signs, goto the hos pital or health cent re immedia tely, dayor night, DO NO Twait.
MOTHER Ifwaters break and not i n labour after 6 hours. Labour pains (contra ctions) continue for more than 12 hours. Heavybl eeding (soaks more than 2-3 pads in 15 minutes). Pl acenta not expelled 1 ho ur afte r bir th of bab y.
BABY Verysmall. Di fficulty in breathing . Fi ts. Fever . Feels cold. Bl eeding. Not able to feed.
Routine visits to the health cent re
Gotothe health cen tre or ar range a home vi sit by a skilled attendant as soon as possible after deliver y,preferably within the first da ys,for the examination of y ou and y our bab y and to receiv e prev entive measures. Gofor a routine pos tpartum visit at 6 w eeks.
M8 CLEAN HOME DELIVERY (1)
Delivery at home with an attendant
Instructions to mother and family for a clean
and safer delivery at home
M9 CLEAN HOME DELIVERY (2)
Avoid harmful practices
Encourage helpful traditional practices
Danger signs during delivery
Routine visits to the health centre
These individual sheets have key information for the mother, her
partner and family on care during pregnancy, preparing a birth
and emergency plan, clean home delivery, care for the mother
and baby after delivery, breastfeeding and care after an abortion.
Individual sheets are used so that the woman can be given
the relevant sheet at the appropriate stage of pregnancy and
childbirth.
CARE DURING PREGNANCY
Care during pregnancy
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
M2
Visit the health worker during pregnancy
Go to the health centre if you think you are pregnant. It is important to begin care as early in your
pregnancy as possible.
Visit the health centre at least 4 times during your pregnancy, even if you do not have any problems.
The health worker will tell you when to return.
If at any time you have any concerns about your or your babys health, go to the health centre.
During your visits to the health centre, the health worker will:
Check your health and the progress of the pregnancy
Help you make a birth plan
Answer questions or concerns you may have
Provide treatment for malaria and anaemia
Give you a tetanus toxoid immunization
Advise and counsel on:
breastfeeding
birthspacing after delivery
nutrition
HIV counselling and testing
correct and consistent condom use
laboratory tests
other matters related to your and your babys health.
Bring your home-based maternal record to every visit.
Care for yourself during pregnancy
Eat more and healthier foods, including more fruits and vegetables, beans, meat, fish, eggs, cheese, milk.
Take iron tablets every day as explained by the health worker.
Rest when you can. Avoid lifting heavy objects.
Sleep under a bednet treated with insecticide.
Do not take medication unless prescribed at the health centre.
Do not drink alcohol or smoke.
Use a condom correctly in every sexual relation to prevent sexually transmitted infection (STI) or
HIV/AIDS if you or your companion are at risk of infection.
PREGNANCY IS A SPECIAL TIME. CARE FOR YOURSELF AND YOUR BABY.
Routine visits to the health centre
1st visit Before 4 months
2nd visit 6-7 months
3rd visit 8 months
4th visit 9 months
Know the signs of labour
If you have any of these signs, go to the health centre as soon as you can.
If these signs continue for 12 hours or more, you need to go immediately.
Painful contractions every 20 minutes or less.
Bag of water breaks.
Bloody sticky discharge.
When to seek care on danger signs
Go to the hospital or health centre immediately, day or night, DO NOT wait, if any of the following signs:
vaginal bleeding
convulsions/fits
severe headaches with blurred vision
fever and too weak to get out of bed
severe abdominal pain
fast or difficult breathing.
Go to the health centre as soon as possible if any of the following signs:
fever
abdominal pain
water breaks and not in labour after 6 hours
feel ill
swollen fingers, face and legs.
PREPARING A BIRTH AND EMERGENCY PLAN
Preparing a birth and emergency plan
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M3
Preparing a birth plan
The health worker will provide you with information to help you prepare a birth plan. Based on your
health condition, the health worker can make suggestions as to where it would be best to deliver.
Whether in a hospital, health centre or at home, it is important to deliver with a skilled attendant.
AT EVERY VISIT TO THE HEALTH CENTRE, REVIEW AND DISCUSS YOUR BIRTH PLAN.
The plan can change if complications develop.
Planning for delivery at home
Who do you choose to be the skilled attendant for delivery?
Who will support you during labour and delivery?
Who will be close by for at least 24 hours after delivery?
Who will help you to care for your home and other children?
Organize the following:
A clean and warm room or corner of a room.
Home-based maternal record.
A clean delivery kit which includes soap, a stick to clean under the nails, a new razor blade to cut
the babys cord, 3 pieces of string (about 20 cm. each) to tie the cord.
Clean cloths of different sizes: for the bed, for drying and wrapping the baby, for cleaning the
babys eyes, and for you to use as sanitary pads.
Warm covers for you and the baby.
Warm spot for the birth with a clean surface or clean cloth.
Bowls: two for washing and one for the placenta.
Plastic for wrapping the placenta.
Buckets of clean water and some way to heat this water.
For handwashing, water, soap and a towel or cloth for drying hands of the birth attendant.
Fresh drinking water, fluids and food for the mother.
Preparing an emergency plan
To plan for an emergency, consider:
Where should you go?
How will you get there?
Will you have to pay for transport to get there? How much will it cost?
What costs will you have to pay at the health centre? How will you pay for this?
Can you start saving for these possible costs now?
Who will go with you to the health centre?
Who will help to care for your home and other children while you are away?
Planning for delivery at the hospital or health centre
How will you get there? Will you have to pay for transport to get there?
How much will it cost to deliver at the facility? How will you pay for this?
Can you start saving for these costs now?
Who will go with you and support you during labour and delivery?
Who will help you while you are away and care for your home and other children?
Bring the following:
Home-based maternal record.
Clean cloths of different sizes: for the bed, for drying and wrapping the baby, and for you to use as
sanitary pads.
Clean clothes for you and the baby.
Food and water for you and the support person.
CARE FOR THE MOTHER AFTER BIRTH
Care for the mother after birth
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M4
Care of the mother
Eat more and healthier foods, including more meat, fish, oils, coconut, nuts, cereals, beans,
vegetables, fruits, cheese and milk.
Take iron tablets as explained by the health worker.
Rest when you can.
Drink plenty of clean, safe water.
Sleep under a bednet treated with insecticide.
Do not take medication unless prescribed at the health centre.
Do not drink alcohol or smoke.
Use a condom in every sexual relation, if you or your companion are at risk of sexually transmitted
infections (STI) or HIV/AIDS.
Wash all over daily, particularly the perineum.
Change pad every 4 to 6 hours. Wash pad or dispose of it safely.
Family planning
You can become pregnant within several weeks after delivery if you have sexual relations and are not
breastfeeding exclusively.
Talk to the health worker about choosing a family planning method which best meets your and your
partners needs.
Routine visits to the health centre
First week after birth:
____________________________________________________________________
____________________________________________________________________
6 weeks after birth:
____________________________________________________________________
____________________________________________________________________
When to seek care for danger signs
Go to hospital or health centre immediately, day or night, DO NOT wait, if any of the following signs:
Vaginal bleeding has increased.
Fits.
Fast or difficult breathing.
Fever and too weak to get out of bed.
Severe headaches with blurred vision.
Go to health centre as soon as possible if any of the following signs:
Swollen, red or tender breasts or nipples.
Problems urinating, or leaking.
Increased pain or infection in the perineum.
Infection in the area of the wound.
Smelly vaginal discharge.
CARE AFTER AN ABORTION
Care after an abortion
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M5
Self-care
Rest for a few days, especially if you feel tired.
Change pads every 4 to 6 hours. Wash used pad or dispose of it safely. Wash perineum.
Do not have sexual intercourse until bleeding stops.
You and your partner should use a condom correctly in every act of sexual intercourse if at risk of STI
or HIV.
Return to the health worker as indicated.
Family planning
Remember you can become pregnant as soon as you have sexual relations.
Use a family planning method to prevent an unwanted pregnancy.
Talk to the health worker about choosing a family planning method which best meets your and your
partners needs.
Know these danger signs
If you have any of these signs, go to the health centre immediately, day or night. DO NOT wait:
Increased bleeding or continued bleeding for 2 days.
Fever, feeling ill.
Dizziness or fainting.
Abdominal pain.
Backache.
Nausea, vomiting.
Foul-smelling vaginal discharge.
Additional support
The health worker can help you identify persons or groups who can provide you
with additional support if you should need it.
CARE FOR THE BABY AFTER BIRTH
Care for the baby after birth
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M6
Care of the newborn
KEEP YOUR NEWBORN CLEAN
Wash your babys face and neck daily. Bathe her/him when necessary. After bathing, thoroughly dry
your baby and then dress and keep her/him warm.
Wash babys bottom when soiled and dry it thoroughly.
Wash your hands with soap and water before and after handling your baby, especially after touching
her/his bottom.
CARE FOR THE NEWBORNS UMBILICAL CORD
Keep cord stump loosely covered with a clean cloth. Fold diaper and clothes below stump.
Do not put anything on the stump.
If stump area is soiled, wash with clean water and soap. Then dry completely with clean cloth.
Wash your hands with soap and water before and after care.
KEEP YOUR NEWBORN WARM
In cold climates, keep at least an area of the room warm.
Newborns need more clothing than other children or adults.
If cold, put a hat on the babys head. During cold nights, cover the baby with an extra blanket.
OTHER ADVICE
Let the baby sleep on her/his back or side.
Keep the baby away from smoke.
Routine visits to the health centre
First week after birth:
____________________________________________________________________
____________________________________________________________________
At 6 weeks :
____________________________________________________________________
____________________________________________________________________
At these visits your baby will be vaccinated. Have your baby immunized.
When to seek care for danger signs
Go to hospital or health centre immediately, day or night, DO NOT wait, if your baby has any of the
following signs:
Difficulty breathing
Fits
Fever
Feels cold
Bleeding
Stops feeding
Diarrhoea.
Go to the health centre as soon as possible if your baby has any of the following signs:
Difficulty feeding.
Feeds less than every 5 hours.
Pus coming from the eyes.
Irritated cord with pus or blood.
Yellow eyes or skin.
BREASTFEEDING
Breastfeeding
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M7
Breastfeeding has many advantages
FOR THE BABY
During the first 6 months of life, the baby needs nothing more than breast milk not water, not
other milk, not cereals, not teas, not juices.
Breast milk contains exactly the water and nutrients that a babys body needs. It is easily digested
and efficiently used by the babys body. It helps protect against infections and allergies and helps
the babys growth and development.
FOR THE MOTHER
Postpartum bleeding can be reduced due to uterine contractions caused by the babys sucking.
Breastfeeding can help delay a new pregnancy.
FOR THE FIRST 6 MONTHS OF LIFE, GIVE ONLY BREAST MILK TO YOUR BABY, DAY AND NIGHT
AS OFTEN AND AS LONG AS SHE/HE WANTS.
Suggestions for successful breastfeeding
Immediately after birth, keep your baby in the bed with you, or within easy reach.
Start breastfeeding within 1 hour of birth.
The babys suck stimulates your milk production. The more the baby feeds, the more milk you will
produce.
At each feeding, let the baby feed and release your breast, and then offer your second breast. At the
next feeding, alternate and begin with the second breast.
Give your baby the first milk (colostrum). It is nutritious and has antibodies to help keep your baby
healthy.
At night, let your baby sleep with you, within easy reach.
While breastfeeding, you should drink plenty of clean, safe water. You should eat more and healthier
foods and rest when you can.
The health worker can support you in
starting and maintaining breastfeeding
The health worker can help you to correctly position the baby and ensure she/he attaches to the
breast. This will reduce breast problems for the mother.
The health worker can show you how to express milk from your breast with your hands. If you should
need to leave the baby with another caretaker for short periods, you can leave your milk and it can
be given to the baby in a cup.
The health worker can put you in contact with a breastfeeding support group.
If you have any difficulties with breastfeeding, see the health worker immediately.
Breastfeeding and family planning
During the first 6 months after birth, if you breastfeed exclusively, day and night, and your
menstruation has not returned, you are protected against another pregnancy.
If you do not meet these requirements, or if you wish to use another family planning method while
breastfeeding, discuss the different options available with the health worker.
CLEAN HOME DELIVERY
Regardless of the site of delivery, it is strongly recommended that all women deliver with a skilled attendant.
For a woman who prefers to deliver at home the following recommendations are provided for a clean home delivery to be reviewed during antenatal care visits.
Clean home delivery (1)
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M8
Delivery at home with an attendant
Ensure the attendant and other family members know the emergency plan and are aware of danger
signs for yourself and your baby.
Arrange for a support person to assist the attendant and to stay with you during labour and after
delivery.
Have these supplies organized for a clean delivery: new razor blade, 3 pieces of string about
20-cm each to tie the cord, and clean cloths to cover the birth place.
Prepare the home and the supplies indicated for a safe birth:
Clean, warm birth place with fresh air and a source of light
Clean warm blanket to cover you
Clean cloths:
for drying and wrapping the baby
for cleaning the babys eyes
to use as sanitary pads after birth
to dry your body after washing
for birth attendant to dry her hands.
Clean clothes for you to wear after delivery
Fresh drinking water, fluids and food for you
Buckets of clean water and soap for washing, for you and the skilled attendant
Means to heat water
Three bowls, two for washing and one for the placenta
Plastic for wrapping the placenta
Bucket for you to urinate in.
Instructions to mother and family
for a clean and safer delivery at home
Make sure there is a clean delivery surface for the birth of the baby.
Ask the attendant to wash her hands before touching you or the baby. The nails of the attendant
should be short and clean.
When the baby is born, place her/him on your abdomen/chest where it is warm and clean. Dry the
baby thoroughly and wipe the face with a clean cloth. Then cover with a clean dry cloth.
Cut the cord when it stops pulsating, using the disposable delivery kit, according to instructions.
Wait for the placenta to deliver on its own.
Make sure you and your baby are warm. Have the baby near you, dressed or wrapped and with head
covered with a cap.
Start breastfeeding when the baby shows signs of readiness, within the first hour of birth.
Dispose of placenta _____________________________________________
(describe correct, safe culturally accepted way to dispose of placenta)
DO NOT be alone for the 24 hours after delivery.
DO NOT bath the baby on the first day.
Clean home delivery (2)
I
N
F
O
R
M
A
T
I
O
N
A
N
D
C
O
U
N
S
E
L
L
I
N
G
S
H
E
E
T
S
M9
Avoid harmful practices
FOR EXAMPLE:
DO NOT use local medications to hasten labour.
DO NOT wait for waters to stop before going to health facility.
DO NOT insert any substances into the vagina during labour or after delivery.
DO NOT push on the abdomen during labour or delivery.
DO NOT pull on the cord to deliver the placenta.
DO NOT put ashes, cow dung or other substance on umbilical cord/stump.
____________________________________________________________________
____________________________________________________________________
Encourage helpful traditional practices:
____________________________________________________________________
____________________________________________________________________
Danger signs during delivery
If you or your baby has any of these signs, go to the hospital or health centre immediately,
day or night, DO NOT wait.
MOTHER
If waters break and not in labour after 6 hours.
Labour pains (contractions) continue for more than 12 hours.
Heavy bleeding (soaks more than 2-3 pads in 15 minutes).
Placenta not expelled 1 hour after birth of baby.
BABY
Very small.
Difficulty in breathing.
Fits.
Fever.
Feels cold.
Bleeding.
Not able to feed.
Routine visits to the health centre
Go to the health centre or arrange a home visit by a skilled attendant as soon as possible after
delivery, preferably within the first days, for the examination of you and your baby and to receive
preventive measures.
Go for a routine postpartum visit at 6 weeks.
Records and forms
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N1
Refer ral record
RECO
RD
S AN
D
FO
RM
S
N2
REFERRAL RECORD
WHO IS REFERRING RECORD NUMBER RE FERRE D DATE TI ME
NAME AR RIVAL DATE TI ME
FACILITY
ACCO MPANIED BY THE HEALTH WOR KER
WOMAN
NAME AG E
ADDRESS
MAIN REASONS FOR REFERRAL Emergency Non-emergency Toaccompany the bab y
MAJOR FINDINGS (CLINICA AND BP , TEMP., LAB.)
LAST (BREAST)FEED (TIME)
TREATMENTS GIVEN AND TIME
BEFORE REFERRAL
DURING TRANSPORT
INFORMATION GIVEN T O THE W OMAN AND COMPANION ABOUT THE REASONS FOR REFERRAL
BABY
NAME DA TE AND HOUR OF BIRTH
BIRTH WEIGHT GESTATIONAL A GE
MAIN REASONS FOR REFERRAL Emergency Non-emergency Toaccompany the mother
MAJOR FINDINGS (CLINICA AND TEMP .)
LAST (BREAST)FEED (TIME)
TREATMENTS GIVEN AND TIME
BEFORE REFERRAL
DURING TRANSPORT
INFORMATION GIVEN T O THE W OMAN AND COMPANION ABOUT THE REASONS FOR REFERRAL
Sample for m to be adapted. Revised on 13 June 2003.
Feedback record
RECO
RD
S AN
D
FO
RM
S
N3
FEEDBA CK RECORD
WHO IS REFERRING RECORD NUMBER AD MISSION D ATE TI ME
NAME DI SCHARGE D ATE TI ME
FACILITY
WOMAN
NAME AG E
ADDRESS
MAIN REASONS FOR REFERRAL Emergency Non-emergency Toaccompany the bab y
DIAGNOSES
TREATMENTS GIVEN AND TIME
TREATMENTS AND RECOMMEND ATI ONS ON FURTHER CARE
FOLLO W-UP VISIT WHEN WHERE
PREVENTIVE MEASURES
IF DEA TH: D ATE
CAUSES
BABY
NAME DA TE OF BIRTH
BIRTH WEIGHT AGE AT DISCHAR GE (DAYS )
MAIN REASONS FOR REFERRAL Emergency Non-emergency Toaccompany the mother
DIAGNOSES
TREATMENTS GIVEN AND TIME
TREATMENTS AND RECOMMEND ATI ONS ON FURTHER CAR E
FOLLO W-UP VISIT WHEN WHERE
PREVENTIVE MEASURES
IF DEA TH: D ATE
CAUSES
Sample for m to be adapted. Revised on 25 August 2003.
Labour record
RECO
RD
S AN
D
FO
RM
S
N4
LABOUR RECORD
USE THIS RECORD FOR MONIT ORING DURING LAB OUR, DELIVERY AND POSTP ARTUM RECORD NUMBER
NAME AG E PARITY
ADDRESS
DURING LAB OUR A T ORAFTER BIRTH MO THER A T ORAFTER BIRTH NEWB ORN PLANNED NEWBORN TREATMENT
ADMISSION D ATE BI RTH TIME LIVEBIRTH STILLBIRTH: FRESH MA CERATED
ADMISSION TIME OXYTOCIN TIME GIVEN RESUSCIT ATI ON NO YES
TIME A CTIVE LAB OUR ST ARTED PLA CENTA COMPLETE NO YES BIRTH WEIGHT
TIME MEMBRANES RUPTURED TIME DELIVERED GEST. AGE ----------OR PRETERM NO YES
TIME SECOND ST AGESTARTS ESTIMA TED BLOOD LOSS SECOND B ABY
ENTRY EXAMINA TION
STAGE OF LAB OURNOTIN ACTIVE LAB OUR ACTIVE LAB OUR
NOTIN ACTIVE LAB OUR PLANNED MATERNA L TREA TMENT
HOURS SINCE ARRIVAL 1 2 3 4 5 6 7 8 9 10 11 12
HOURS SINCE RUPTURED MEMBRANES
VAGINAL BLEEDING (0 + ++)
STRONG CONTRACTIONS IN 10 MINUTES
FETAL HEART RA TE (BEA TS PER MINUTE)
T (AXILLARY)
PULSE (BEA TS/MINUTE)
BLOOD PRESSURE (SYST OLIC/DIASTOLIC)
URINE V OIDED
CERVICAL DILAT ATI ON (CM)
PROBLEM TI ME ONSET TREATMENTS OTHER THAN NORMAL SUPPORT IVE CARE
0
0
IF MO THER REFERRED DURING LAB OUR OR DELIVER Y,RECORD TIME AND EXPLAIN
0
Sample for m to be adapted. Revised on 13 June 2003.
Partograph
RECO
RD
S AN
D
FO
RM
S
N5
FINDINGS TIME
Hours in active labour 1 2 3 4 5 6 7 8 9 10 11 12
Hours since r uptured membranes
Rapid assessment B3-B7
Vaginal bleeding (0 + ++)
Amniotic fluid (meconium stained)
Contractions in 10 minutes
Fetal hear t rate (beats/minute)
Urine v oided
T (axillar y)
Pulse (beats/minute)
Blood pressure (systolic/diastolic)
Cervical dilatation (cm)
Deliver y of placenta (time)
Oxytocin (time/giv en)
Problem-note onset/describe belo w
PARTOGRAPH
USE THIS FORM FOR MONIT ORING A CTIVE LAB OUR 10cm
9cm
8cm
7cm
6cm
5cm
4cm
Sample form to be adapted.
Revised on 13 June 2003.
Postpartumrecord
RECO
RD
S AN
D
FO
RM
S
N6
POSTP ARTUM RECORD
MONITORING AFTER BIRTH EVERY5-15 MIN FOR 1ST HOUR 2 HR 3 HR 4 HR 8 HR 12 HR 16 HR 20 HR 24 HR
TIME
RAPID ASSESSMENT
BLEEDING (0 + ++)
UTERUS HARD/R OUND?
MATERNA L: BLOOD PRESSURE
PULSE
URINE V OIDED
VULV A
NEWBORN : BREA THING
WAR MTH
NEWBORN ABNORMAL SIGNS (LIST)
0
TIME FEEDING OBSER VED FEEDING WELL DIFFICULTY
COMMENTS
0
PLANNED TREA TMENT TIMETREATMENT GIVEN
MOTHER
0
0
NEWBORN
0
IF REFERRED (MO THER OR NEWB ORN), RECORD TIME AND EXPLAIN:
0
IF DEA TH (MO THER OR NEWB ORN), DATE , TIME AND CAUSE:
ADVISE AND COUNSEL
MOTHER
Postpartum care and h ygiene
Nutrition
Bi rthspacing and family planning
Danger signs
Follow-up visits
BABY
Exclusive breastfeedi ng
Hygiene, cord care and war mth
Special ad vice if lo w bir th weight
Danger signs
Follow-up visits
PREVE NTIVE MEASURES
FOR MO THER
Iron/folate
Vi tamin A
Mebendazole
Sulphadoxine-p yrimethamine
Tetanus toxoid immuni zation
RPR test result and treatm ent
ARV
FOR BABY
Ri sk of bacte rial infectio n and treatm ent
BCG,OPV-0, Hep-0
RPR result and treatmen t
TBtest result and proph ylaxis
ARV
Sample for m to be adapted. Revised on 25 August 2003.
International formof medical cer tificate of cause of death
RECO
RD
S AN
D
FO
RM
S
N7
INTERNATIONA L FORM OF MEDICAL CERTIFICA TE OF CA USE OF DEA TH
APPRO XIMATE INTERV AL CAUSE OF DEA TH BETWEEN ONSET AND DEATH
I (a). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Disease or condition directly Due to (or as consequenc e of). . . . . . . . . . . leading to death* (b). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Antecedent causes Due to (or as consequenc e of) . . . . . . . . . . . . . . . . . . . . . . Morbid conditions, ifany,giving ( C). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . rise to the abo vecause, stating Due to (or as consequenc e of) . . . . . . . . . . . . . . . . . . . . . . (d). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
II . . . . . . . . . . . . . . . . . . . . . . Other significant conditions contributing to . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . the death, but not related to the disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or condition causing it. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
* This does not mean the mode of d ying, e.g.heart failure, respirator y failure. Itmeans the disease, injuryor complication that caused death.
CONSIDER COLLECTING THE FOLLO WING INFORMA TION III If the deceased is a female, was she Not pregnant Not pregnant, but pregnant within 42 da ys of death Pregnant at the time of death Unknown if pregnant or was pregnant within 42days of death
0IV If the deceased is an infant and less than one month old What was the bir th weight: . . . . . . . . . g Ifexact bir th weight not kno wn, was bab y weighing: 2500 g or more less than 2500 g
N2
REFERRAL RECORD
N3
FEEDBACK RECORD
N4
LABOUR RECORD
N5
PARTOGRAPH
N6
POSTPARTUM RECORD
N7
INTERNATIONAL FORM OF MEDICAL
CERTIFICATE OF CAUSE OF DEATH
Records are suggested not so much for the format as for the content.
The content of the records is adjusted to the content of the Guide.
Modify national or local records to include all the relevant sections needed to record
important information for the provider, the woman and her family, for the purposes of
monitoring and surveillance and official reporting.
Fill out other required records such as immunization cards for the mother and baby.
RECORDS AND FORMS
Referral record
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N2
REFERRAL RECORD
WHO IS REFERRING RECORD NUMBER REFERRED DATE TIME
NAME ARRIVAL DATE TIME
FACILITY
ACCOMPANIED BY THE HEALTH WORKER
WOMAN
NAME AGE
ADDRESS
MAIN REASONS FOR REFERRAL Emergency Non-emergency To accompany the baby
MAJOR FINDINGS (CLINICA AND BP, TEMP., LAB.)
LAST (BREAST)FEED (TIME)
TREATMENTS GIVEN AND TIME
BEFORE REFERRAL
DURING TRANSPORT
INFORMATION GIVEN TO THE WOMAN AND COMPANION ABOUT THE REASONS FOR REFERRAL
BABY
NAME DATE AND HOUR OF BIRTH
BIRTH WEIGHT GESTATIONAL AGE
MAIN REASONS FOR REFERRAL Emergency Non-emergency To accompany the mother
MAJOR FINDINGS (CLINICA AND TEMP.)
LAST (BREAST)FEED (TIME)
TREATMENTS GIVEN AND TIME
BEFORE REFERRAL
DURING TRANSPORT
INFORMATION GIVEN TO THE WOMAN AND COMPANION ABOUT THE REASONS FOR REFERRAL
Sample form to be adapted. Revised on 13 June 2003.
Feedback record
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N3
FEEDBACK RECORD
WHO IS REFERRING RECORD NUMBER ADMISSION DATE TIME
NAME DISCHARGE DATE TIME
FACILITY
WOMAN
NAME AGE
ADDRESS
MAIN REASONS FOR REFERRAL Emergency Non-emergency To accompany the baby
DIAGNOSES
TREATMENTS GIVEN AND TIME
TREATMENTS AND RECOMMENDATIONS ON FURTHER CARE
FOLLOW-UP VISIT WHEN WHERE
PREVENTIVE MEASURES
IF DEATH: DATE
CAUSES
BABY
NAME DATE OF BIRTH
BIRTH WEIGHT AGE AT DISCHARGE (DAYS)
MAIN REASONS FOR REFERRAL Emergency Non-emergency To accompany the mother
DIAGNOSES
TREATMENTS GIVEN AND TIME
TREATMENTS AND RECOMMENDATIONS ON FURTHER CARE
FOLLOW-UP VISIT WHEN WHERE
PREVENTIVE MEASURES
IF DEATH: DATE
CAUSES
Sample form to be adapted. Revised on 25 August 2003.
Labour record
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N4
LABOUR RECORD
USE THIS RECORD FOR MONITORING DURING LABOUR, DELIVERY AND POSTPARTUM RECORD NUMBER
NAME AGE PARITY
ADDRESS
DURING LABOUR AT OR AFTER BIRTH MOTHER AT OR AFTER BIRTH NEWBORN PLANNED NEWBORN TREATMENT
ADMISSION DATE BIRTH TIME LIVEBIRTH STILLBIRTH: FRESH MACERATED
ADMISSION TIME OXYTOCIN TIME GIVEN RESUSCITATION NO YES
TIME ACTIVE LABOUR STARTED PLACENTA COMPLETE NO YES BIRTH WEIGHT
TIME MEMBRANES RUPTURED TIME DELIVERED GEST. AGE WEEKS OR PRETERM
TIME SECOND STAGE STARTS ESTIMATED BLOOD LOSS SECOND BABY
ENTRY EXAMINATION MORE THAN ONE FETUS - SPECIFY FETAL LIE: LONGITUDINAL TRANSVERSE FETAL PRESENTATION: HEAD BREECH OTHER - SPECIFY
STAGE OF LABOUR NOT IN ACTIVE LABOUR ACTIVE LABOUR
NOT IN ACTIVE LABOUR PLANNED MATERNAL TREATMENT
HOURS SINCE ARRIVAL 1 2 3 4 5 6 7 8 9 10 11 12
HOURS SINCE RUPTURED MEMBRANES
VAGINAL BLEEDING (0 + ++)
STRONG CONTRACTIONS IN 10 MINUTES
FETAL HEART RATE (BEATS PER MINUTE)
TEMPERATURE (AXILLARY)
PULSE (BEATS/MINUTE)
BLOOD PRESSURE (SYSTOLIC/DIASTOLIC)
URINE VOIDED
CERVICAL DILATATION (CM)
PROBLEM TIME ONSET TREATMENTS OTHER THAN NORMAL SUPPORTIVE CARE
0
0
IF MOTHER REFERRED DURING LABOUR OR DELIVERY, RECORD TIME AND EXPLAIN
0
Sample form to be adapted. Revised on 13 June 2003.
Partograph
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N5
FINDINGS TIME
Hours in active labour 1 2 3 4 5 6 7 8 9 10 11 12
Hours since ruptured membranes
Rapid assessment B3-B7
Vaginal bleeding (0 + ++)
Amniotic fluid (meconium stained)
Contractions in 10 minutes
Fetal heart rate (beats/minute)
Urine voided
T (axillary)
Pulse (beats/minute)
Blood pressure (systolic/diastolic)
Cervical dilatation (cm)
Delivery of placenta (time)
Oxytocin (time/given)
Problem-note onset/describe below
PARTOGRAPH
USE THIS FORM FOR MONITORING ACTIVE LABOUR
10 cm
9 cm
8 cm
7 cm
6 cm
5 cm
4 cm
S
a
m
p
l
e
f
o
r
m
t
o
b
e
a
d
a
p
t
e
d
.
R
e
v
i
s
e
d
o
n
1
3
J
u
n
e
2
0
0
3
.
C
E
R
V
I
C
A
L
D
I
L
A
T
A
T
I
O
N
Postpartum record
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N6
POSTPARTUM RECORD
MONITORING AFTER BIRTH EVERY 5-15 MIN FOR 1ST HOUR 2 HR 3 HR 4 HR 8 HR 12 HR 16 HR 20 HR 24 HR
TIME
RAPID ASSESSMENT
BLEEDING (0 + ++)
UTERUS HARD/ROUND?
MATERNAL: BLOOD PRESSURE
PULSE
URINE VOIDED
VULVA
NEWBORN: BREATHING
WARMTH
NEWBORN ABNORMAL SIGNS (LIST)
0
TIME FEEDING OBSERVED FEEDING WELL DIFFICULTY
COMMENTS
0
PLANNED TREATMENT TIME TREATMENT GIVEN
MOTHER
0
0
NEWBORN
0
IF REFERRED (MOTHER OR NEWBORN), RECORD TIME AND EXPLAIN:
0
IF DEATH (MOTHER OR NEWBORN), DATE, TIME AND CAUSE:
ADVISE AND COUNSEL
MOTHER
Postpartum care and hygiene
Nutrition
Birth spacing and family planning
Danger signs
Follow-up visits
BABY
Exclusive breastfeeding
Hygiene, cord care and warmth
Special advice if low birth weight
Danger signs
Follow-up visits
PREVENTIVE MEASURES
FOR MOTHER
Iron/folate
Vitamin A
Mebendazole
Sulphadoxine-pyrimethamine
Tetanus toxoid immunization
RPR test result and treatment
ARV
FOR BABY
Risk of bacterial infection and treatment
BCG, OPV-0, Hep-0
RPR result and treatment
TB test result and prophylaxis
ARV
Sample form to be adapted. Revised on 25 August 2003.
International form of medical certificate of cause of death
R
E
C
O
R
D
S
A
N
D
F
O
R
M
S
N7
INTERNATIONAL FORM OF MEDICAL CERTIFICATE OF CAUSE OF DEATH
APPROXIMATE INTERVAL
CAUSE OF DEATH BETWEEN ONSET AND DEATH
I (a). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Disease or condition directly Due to (or as consequence of) . . . . . . . . . . .
leading to death* (b). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Antecedent causes Due to (or as consequence of) . . . . . . . . . . . . . . . . . . . . . .
Morbid conditions, if any, giving (C). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
rise to the above cause, stating Due to (or as consequence of) . . . . . . . . . . . . . . . . . . . . . .
(d). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . .
II . . . . . . . . . . . . . . . . . . . . . .
Other significant conditions contributing to . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
the death, but not related to the disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
or condition causing it. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
* This does not mean the mode of dying, e.g. heart failure, respiratory failure.
It means the disease, injury or complication that caused death.
CONSIDER COLLECTING THE FOLLOWING INFORMATION
III
If the deceased is a female, was she Not pregnant
Not pregnant, but pregnant within 42 days of death
Pregnant at the time of death
Unknown if pregnant or was pregnant within 42 days of death
0
IV
If the deceased is an infant and less than one month old What was the birth weight: . . . . . . . . . g
If exact birth weight not known, was baby weighing:
2500 g or more
less than 2500 g
G
L
O
S
S
A
R
Y
A
N
D
A
C
R
O
N
Y
M
S
Glossary and acronyms
ABORTION
Termination of pregnancy from
whatever cause before the fetus is
capable of extrauterine life.
ADOLESCENT
Young person 1019 years old.
ADVISE
To give information and suggest to
someone a course of action.
ANTENATAL CARE
Care for the woman and fetus during
pregnancy.
ASSESS
To consider the relevant information
and make a judgement. As used in this
guide, to examine a woman or baby
and identify signs of illness.
BABY
A very young boy or girl in the first
week(s) of life.
BIRTH
Expulsion or extraction of the baby
(regardless of whether the cord has
been cut).
BIRTH AND EMERGENCY PLAN
A plan for safe childbirth developed in
antenatal care visit which considers
the womans condition, preferences
and available resources. A plan to seek
care for danger signs during pregnancy,
childbirth and postpartum period, for
the woman and newborn.
BIRTH WEIGHT
The first of the fetus or newborn
obtained after birth.
For live births, birth weight should
preferably be measured within the first
hour of life before significant postnatal
weight loss has occurred, recorded to
the degree of accuracy to which it is
measured.
CHART
As used in this guide, a sheet
presenting information in the form of
a table.
CHILDBIRTH
Giving birth to a baby or babies and
placenta.
CLASSIFY
To select a category of illness and
severity based on a womans or babys
signs and symptoms.
CLINIC
As used in this guide, any first-level
outpatient health facility such as a
dispensary, rural health post, health
centre or outpatient department of a
hospital.
COMMUNITY
As used in this guide, a group of
people sometimes living in a defined
geographical area, who share common
culture, values and norms. Economic
and social differences need to be taken
into account when determining needs
and establishing links within a given
community.
BIRTH COMPANION
Partner, other family member or friend
who accompanies the woman during
labour and delivery.
CHILDBEARING AGE (WOMAN)
15-49 years. As used in this guide, also
a girl 10-14 years, or a woman more
than 49 years, when pregnant, after
abortion, after delivery.
COMPLAINT
As described in this guide, the
concerns or symptoms of illness or
complication need to be assessed and
classified in order to select treatment.
CONCERN
A worry or an anxiety that the woman
may have about herself or the
baby(ies).
COMPLICATION
A condition occurring during pregnancy
or aggravating it. This classification
includes conditions such as obstructed
labour or bleeding.
CONFIDENCE
A feeling of being able to succeed.
CONTRAINDICATION
A condition occurring during another
disease or aggravating it. This
classification includes conditions such
as obstructed labour or bleeding.
COUNSELLING
As used in this guide, interaction with a
woman to support her in solving actual
or anticipated problems, reviewing
options, and making decisions. It
places emphasis on provider support
for helping the woman make decisions.
DANGER SIGNS
Terminology used to explain to the
woman the signs of life-threatening and
other serious conditions which require
immediate intervention.
EMERGENCY SIGNS
Signs of life-threatening conditions
which require immediate intervention.
ESSENTIAL
Basic, indispensable, necessary.
FACILITY
A place where organized care is
provided: a health post, health centre,
hospital maternity or emergency unit,
or ward.
FAMILY
Includes relationships based on blood,
marriage, sexual partnership, and
adoption, and a broad range of groups
whose bonds are based on feelings
of trust mutual support, and a shared
destiny.
FOLLOW-UP VISIT
A return visit requested by a health
worker to see if further treatment or
referral is needed.
GESTATIONAL AGE
Duration of pregnancy from the
last menstrual period. In this guide,
duration of pregnancy (gestational age)
is expressed in 3 different ways:
Trimester Months Weeks
First less than 4 months less than 16 weeks
Second 4-6 months 16-28 weeks
Third 7-9+ months 29-40+ weeks
GRUNTING
Soft short sounds that a baby makes
when breathing out. Grunting occurs
when a baby is having difficulty
breathing.
Glossary
HOME DELIVERY
Delivery at home (with a skilled
attendant, a traditional birth attendant, a
family member, or by the woman herself).
HOSPITAL
As used in this guide, any health facility
with inpatient beds, supplies and
expertise to treat a woman or newborn
with complications.
INTEGRATED MANAGEMENT
A process of caring for the woman in
pregnancy, during and after childbirth,
and for her newborn, that includes
considering all necessary elements:
care to ensure they remain healthy, and
prevention, detection and management
of complications in the context of her
environment and according to her
wishes.
LABOUR
As used in this guide, a period from
the onset of regular contractions to
complete delivery of the placenta.
LOW BIRTH WEIGHT BABY
Weighing less than 2500-g at birth.
MATERNITY CLINIC
Health centre with beds or a hospital
where women and their newborns
receive care during childbirth and
delivery, and emergency first aid.
MISCARRIAGE
Premature expulsion of a non-viable
fetus from the uterus.
MONITORING
Frequently repeated measurements of
vital signs or observations of danger
signs.
NEWBORN
Recently born infant. In this guide used
interchangeable with baby.
PARTNER
As used in this guide, the male
companion of the pregnant woman
(husband, free union) who is the
father of the baby or the actual sexual
partner.
POSTNATAL CARE
Care for the baby after birth. For the
purposes of this guide, up to two weeks.
POSTPARTUM CARE
Care for the woman provided in the
postpartum period, e.g. from complete
delivery of the placenta to 42 days
after delivery.
PRE-REFERRAL
Before referral to a hospital.
PREGNANCY
Period from when the woman misses
her menstrual period or the uterus can
be felt, to the onset of labour/elective
caesarian section or abortion.
PREMATURE
Before 37 completed weeks of
pregnancy.
PRETERM BABY
Born early, before 37 completed weeks
of pregnancy. If number of weeks not
known, 1 month early.
PRIMARY HEALTH CARE*
Essential health care accessible at a
cost the country and community can
afford, with methods that are practical,
scientifically sound and socially
acceptable. (Among the essential
activities are maternal and child
health care, including family planning;
immunization; appropriate treatment of
common diseases and injuries; and the
provision of essential drugs).
PRIMARY HEALTH CARE LEVEL
Health post, health centre or maternity
clinic; a hospital providing care for
normal pregnancy and childbirth.
PRIORITY SIGNS
Signs of serious conditions which
require interventions as soon as
possible, before they become life-
threatening.
QUICK CHECK
A quick check assessment of the
health status of the woman or her
baby at the first contact with the health
provider or services in order to assess if
emergency care is required.
RAPID ASSESSMENT AND
MANAGEMENT
Systematic assessment of vital
functions of the woman and the most
severe presenting signs and symptoms;
immediate initial management of the
life-threatening conditions; and urgent
and safe referral to the next level of
care.
REASSESSMENT
As used in this guide, to examine the
woman or baby again for signs of a
specific illness or condition to see if
she or the newborn are improving.
RECOMMENDATION
Advice. Instruction that should be
followed.
REFERRAL, URGENT
As used in this guide, sending a woman
or baby, or both, for further assessment
and care to a higher level of care;
including arranging for transport
and care during transport, preparing
written information (referral form),
and communicating with the referral
institution.
REFERRAL HOSPITAL
A hospital with a full range of obstetric
services including surgery and blood
transfusion and care for newborns with
problems.
REINFECTION
Infection with same or a different strain
of HIV virus.
REPLACEMENT FEEDING
The process of feeding a baby who is
not receiving breast milk with a diet
that provides all the nutrients she/
he needs until able to feed entirely on
family foods.
SECONDARY HEALTH CARE
More specialized care offered
at the most peripheral level, for
example radiographic diagnostic,
general surgery, care of women with
complications of pregnancy and
childbirth, and diagnosis and treatment
of uncommon and severe diseases.
(This kind of care is provided by trained
staff at such institutions as district or
provincial hospitals).
SHOCK
A dangerous condition with
severe weakness, lethargy, or
unconsciousness, cold extremeties,
and fast, weak pulse. It is caused by
severe bleeding, severe infection, or
obstructed labour.
SIGN
As used in this guide, physical evidence
of a health problem which the health
worker observes by looking, listening,
feeling or measuring. Examples
of signs: bleeding, convulsions,
hypertension, anaemia, fast breathing.
G
L
O
S
S
A
R
Y
A
N
D
A
C
R
O
N
Y
M
S
Glossary
G
L
O
S
S
A
R
Y
A
N
D
A
C
R
O
N
Y
M
S
SKILLED ATTENDANT
Refers exclusively to people with
midwifery skills (for example, midwives,
doctors and nurses) who have been
trained to proficiency in the skills
necessary to manage normal deliveries
and diagnose or refer obstetric
complications.
For the purposes of this guide, a person
with midwifery skills who:
has acquired the requisite
qualifications to be registered
and/or legally licensed to practice
training and licensing requirements
are country-specific;
May practice in hospitals, clinics,
health units, in the home, or in any
other service setting.
Is able to do the following:
give necessary care and advice
to women during pregnancy and
postpartum and for their newborn
infants;
conduct deliveries on her/his
own and care for the mother and
newborn; this includes provision
of preventive care, and detection
and appropriate referral of
abnormal conditions.
provide emergency care for
the woman and newborn;
perform selected obstetrical
procedures such as manual
removal of placenta and newborn
resuscitation; prescribe and give
drugs (IM/IV) and infusions to
the mother and baby as needed,
including for post-abortion care.
provide health information and
counselling for the woman, her
family and community.
SMALL BABY
A newly born infant born preterm and/
or with low birth weight.
STABLE
Staying the same rather than getting
worse.
STILLBIRTH
Birth of a baby that shows no signs of
life at birth (no gasping, breathing or
heart beat).
SURVEILLANCE, PERMANENT
Continuous presence and observation
of a woman in labour.
SYMPTOM
As used in this guide, a health problem
reported by a woman, such as pain or
headache.
TERM, FULL-TERM
Word used to describe a baby
born after 37 completed weeks of
pregnancy.
TRIMESTER OF PREGNANCY
See Gestational age.
VERY SMALL BABY
Baby with birth weight less than 1500-g
or gestational age less than 32 weeks.
WHO definitions have been used where
possible but, for the purposes of this
guide, have been modified where
necessary to be more appropriate to
clinical care (reasons for modification
are given). For conditions where
there are no official WHO definitions,
operational terms are proposed, again
only for the purposes of this guide.
Acronyms
AIDS Acquired immunodeficiency
syndrome, caused by infection with
human immunodeficiency virus
(HIV). AIDS is the final and most
severe phase of HIV infection.
ANC Care for the woman and fetus
during pregnancy.
ARV Antiretroviral drug, a drug to treat
HIV infection, or to prevent mother-
to-child transmission of HIV.
BCG An immunization to prevent
tuberculosis, given at birth.
BP Blood pressure.
BPM Beats per minute.
FHR Fetal heart rate.
Hb Haemoglobin.
HB-1 Vaccine given at birth to prevent
hepatitis B.
HMBR Home-based maternal record:
pregnancy, delivery and inter-
pregnancy record for the woman
and some information about the
newborn.
HIV Human immunodeficiency virus.
HIV is the virus that causes AIDS.
INH Isoniazid, a drug to treat
tuberculosis.
IV Intravenous (injection or infusion).
IM Intramuscular injection.
IU International unit.
IUD Intrauterine device.
LAM Lactation amenorrhea.
LBW Low birth weight: birth weight less
than 2500 g.
LMP Last menstrual period: a date
from which the date of delivery is
estimated.
MTCT Mother-to-child transmission of HIV.
NG Naso-gastric tube, a feeding tube
put into the stomach through the
nose.
ORS Oral rehydration solution.
OPV-0 Oral polio vaccine. To prevent
poliomyelitis, OPV-0 is given at birth.
QC A quick check assessment of the
health status of the woman or her
baby at the first contact with the
health provider or services in order
to assess if emergency care is
required.
RAM Systematic assessment of
vital functions of the woman and
the most severe presenting signs
and symptoms; immediate initial
management of the life-threatening
conditions; and urgent and safe
referral to the next level of care.
RPR Rapid plasma reagin, a rapid test
for syphilis. It can be performed in
the clinic.
STI Sexually transmitted infection.
TBA A person who assists the mother
during childbirth. In general, a TBA
would initially acquire skills by
delivering babies herself or through
apprenticeship to other TBAs.
TT An immunization against tetanus
> More than
Equal or more than
< Less than
Equal or less than
G
L
O
S
S
A
R
Y
A
N
D
A
C
R
O
N
Y
M
S
ACRONYMS
For more information, please contact:
Department of Making Pregnancy Safer
Family and Community Health, World Health Organization
Avenue Appia 20, CH-1211 Geneva 27, Switzerland
Tel: +41 22 791 4447 / 3346
Fax: +41 22 791 5853
Email: MPSinfo@who.int
For updates to this publication, please visit:
www.who.int/making_pregnancy_safer
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Disease DetectivesDocument2 pagesDisease DetectivesConnor67% (3)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Principles of Prevention and Control of Communicable DiseasesDocument31 pagesPrinciples of Prevention and Control of Communicable DiseasesSam Tagarda100% (16)
- PCB Form Annex A3 Patient Ledger FrontDocument1 pagePCB Form Annex A3 Patient Ledger FrontBeryl de la CruzNo ratings yet
- Doh - Performance Evaluation System (Doh - Pes) : Accomplishment of Work - Your Supervisor'sDocument3 pagesDoh - Performance Evaluation System (Doh - Pes) : Accomplishment of Work - Your Supervisor'sBeryl de la CruzNo ratings yet
- Breastfeeding ProcedureDocument2 pagesBreastfeeding ProcedureBeryl de la CruzNo ratings yet
- Medical MnemonicsDocument158 pagesMedical MnemonicsBeryl de la CruzNo ratings yet
- Office: of The SecretaryDocument2 pagesOffice: of The SecretaryNurse IanNo ratings yet
- Who Pen 2020Document85 pagesWho Pen 2020Faye PalmaresNo ratings yet
- Live Experiences of Pandemic To The Mental Health of The Gas 12 C StudentsDocument63 pagesLive Experiences of Pandemic To The Mental Health of The Gas 12 C StudentsJames Alexander DezaNo ratings yet
- Daniel H Unit 14 Task 1 1Document8 pagesDaniel H Unit 14 Task 1 1Daniel John HaighNo ratings yet
- CKD PredictionDocument6 pagesCKD PredictionMadhu CkNo ratings yet
- DisabilityDocument450 pagesDisabilityTony Kelbrat100% (1)
- Climate Change and Health Impacts - Dr. Robert LaumbachDocument36 pagesClimate Change and Health Impacts - Dr. Robert LaumbachNJCleanWaterNo ratings yet
- FinalBook3 ManagementDynamicsCOVIDPandemicDocument369 pagesFinalBook3 ManagementDynamicsCOVIDPandemicAgneesh DuttaNo ratings yet
- RRL Hypertension ComplianceDocument30 pagesRRL Hypertension ComplianceAngelaTrinidadNo ratings yet
- Psychiatric Pharmacy: New Role of Pharmacists in Mental HealthDocument5 pagesPsychiatric Pharmacy: New Role of Pharmacists in Mental Healthruba azfr-aliNo ratings yet
- RubricDocument2 pagesRubricapi-260145388No ratings yet
- Nightingale's TheoryDocument25 pagesNightingale's TheorySrishti BajajNo ratings yet
- Pediatric Pulmonology - 2021 - Kouis - Pediatric Asthma Symptom Control During Lockdown For The COVID 19 Pandemic in SpringDocument9 pagesPediatric Pulmonology - 2021 - Kouis - Pediatric Asthma Symptom Control During Lockdown For The COVID 19 Pandemic in SpringFuerza Dedicacion OmegaNo ratings yet
- Animal Sciences: Footrot in Sheep and GoatsDocument5 pagesAnimal Sciences: Footrot in Sheep and GoatsHenri YudamuktiNo ratings yet
- Agenda From World Health AssemblyDocument7 pagesAgenda From World Health AssemblyMathewDunckleyNo ratings yet
- Genetic CounselingDocument33 pagesGenetic CounselingSAYMABANU100% (1)
- 01.15.01 Pediatric History Taking and Physical ExamDocument14 pages01.15.01 Pediatric History Taking and Physical ExamMikmik DG100% (1)
- Presents: 15 - 16 July 2021 Holiday Inn Mumbai International AirportDocument13 pagesPresents: 15 - 16 July 2021 Holiday Inn Mumbai International AirportSangram SabatNo ratings yet
- ENGLISH SPM Section C 2Document4 pagesENGLISH SPM Section C 2Mohamad NuraizatNo ratings yet
- The Science of NutritionalDocument738 pagesThe Science of NutritionalMonching Adecer100% (1)
- Primary Health Centre ReportDocument12 pagesPrimary Health Centre ReportAkshay H.100% (1)
- Research (Evacuation Center)Document17 pagesResearch (Evacuation Center)Luego, Brent Jarryd P.No ratings yet
- G.R. No. 227419 - HENRY ESPIRITU PASTRANA v. BAHIA SHIPPING SERVICESDocument5 pagesG.R. No. 227419 - HENRY ESPIRITU PASTRANA v. BAHIA SHIPPING SERVICESJay jogsNo ratings yet
- Knowledge Diversity Book 1Document108 pagesKnowledge Diversity Book 1NiteshminzNo ratings yet
- 003 Part1-Effect of Air PollutionDocument20 pages003 Part1-Effect of Air PollutionPragada ManoharNo ratings yet
- Russian Healing BlanketDocument2 pagesRussian Healing BlanketJames MatthewNo ratings yet
- CTS Group Personal Accident Insurance PolicyDocument12 pagesCTS Group Personal Accident Insurance Policynivasshaan50% (2)
- Bachelor in Hospital Management Paramedical College DurgapurDocument31 pagesBachelor in Hospital Management Paramedical College DurgapurVivek DasNo ratings yet