Professional Documents
Culture Documents
Chemotherapeutic Agents: - Antibiotics - Antifungals - Antivirals - Antiprotozoal - Antihelmintics - Anticancer Drugs
Chemotherapeutic Agents: - Antibiotics - Antifungals - Antivirals - Antiprotozoal - Antihelmintics - Anticancer Drugs
Uploaded by
Ahsen BilalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chemotherapeutic Agents: - Antibiotics - Antifungals - Antivirals - Antiprotozoal - Antihelmintics - Anticancer Drugs
Chemotherapeutic Agents: - Antibiotics - Antifungals - Antivirals - Antiprotozoal - Antihelmintics - Anticancer Drugs
Uploaded by
Ahsen BilalCopyright:
Available Formats
B
I
M
M
1
1
8
Chemotherapeutic Agents
Antibiotics
Antifungals
Antivirals
Antiprotozoal
Antihelmintics
Anticancer drugs
B
I
M
M
1
1
8
Antibiotics
General Aspects:
Principle:
inhibit growth of bacteria without harming the host
Drug must penetrate body tissue to reach bacteria (exception: GI infection)
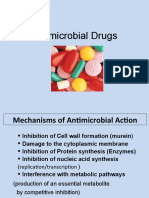
(unique targets: cell wall, protein synthesis, metabolic pathways)
Bacteria targeted must be within the spectrum of the AB
Drug can be bactericidal or bacteriostatic
Different agents can be combined for synergistic effect
(Note: not all combinations are useful, e.g. cell wall synthesis inhibitors loose effectiveness
when combined with bacteriostatic drugs)
Identification of the invasive microorganism necessary for optimal treatment
General side effect:
Alteration in normal body flora
GI tract harbors symbiotic bacteria which are killed by AB =>
resistant bacteria repopulate the niche = secondary or superinfection
(most common: overgrowth of Clostridium difficile)
B
I
M
M
1
1
8
Antibiotics
Resistance:
loss of efficacy of a given AB against a particular strain
Frequently: Staphylococcus aureus, pseudomonas aeruginosa, mycobacterium
tuberculosii
Acquisition:
Spontaneous mutation
Adaption: drug metabolism (!-lactamase); alternative metabolic pathways
Gene transfer: plasmids (via conjugation and transduction); transposons
Manifestation:
Microbes may increase manufacture of drug-metabolizing enzymes (penicillins)
Microbes may cease active uptake of certain drugs (tetracyclines)
Changes in receptors which decrease antibiotic binding and action
Microbes may synthesize compounds that antagonize drug actions
Antibiotic use promotes the emergence of drug-resistant microbes
(especially the use of broad-spectrum antibiotics)
!!! The more ABs are used, the greater the chance of resistance !!!
B
I
M
M
1
1
8
Antibiotics
Resistance avoided/delayed by:
Using AB only when absolutely needed and indicated:
AB often abused for viral infections (diarrhea, flu-symptoms, etc.)
Starting with narrow-spectrum drugs
Limiting use of newer drugs
(Minimizing giving antibiotics to livestock)
Identifying the infecting organism
Defining the drug sensitivity of the infecting organism
Considering all host factors:
site of infection, inability of drug of choice to penetrate the site of infection, etc.
Using AB combinations only when indicated:
Severe or mixed infections, prevention of resistance (tuberculosis)
Worldwide more than 500 metric tons antibiotics are used anually !!!
B
I
M
M
1
1
8
Antibiotics
Classification:
Cell wall synthesis inhibitors
Beta-lactams (penicillins, cephalosporins, aztreonam, imipenem)
Poly-peptides (bacitracin, vancomycin)
Protein synthesis inhibitors
Aminoglycosides
Tetracyclins
Macrolides
Chloramphenicol
Clindamycin
Folate antagonists
Sulfonamides
Trimethoprim
Quinolones
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Bacterial cell wall:
Three types:
Gram-negative (e.g. E.coli, Salmonella)
Few peptidoglycan layers
(Lipopolysaccheride)
Gram-positive (e.g. Staphylococci, Listeria)
Many peptidoglycan layers
(Lipoteichoic acid)
Stains w/ crystal-violet/iodine
Acid-fast positive (Mycobacteria)
Cell wall contains waxy substance
(Mycolic acid)
Stain w/ acid fast test (heating required)
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Beta-lactam antibiotics:
1928 - Alexander Fleming observes the antibacterial effects of Penicillin
1940 - Florey and Chain extract Penicillin
Classification:
Penicillins
Narrow spectrum penicillinase sensitive
Narrow spectrum penicillinase resistant
Broad spectrum penicillins
Extended-spectrum penicillins
Cephalosporines
Carbapenems
Monobactams
Vancomycin, Bacitracin
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Penicillins
Inhibit transpeptidase required for cross-linking peptidoglycan chains
Also inactivate an inhibitor of an autolytic bacterial enzyme => lysis
Narrow spectrum penicillinase (= !-lactamase) sensitive
Benzylpenicillin
Naturally occuring
Poor oral availability (sensitive to stomach acid)
=> given by injection
Active against gram-positive bacteria
Phenoxymethylpenicillin
Better oral availability (acid resistant)
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Narrow spectrum penicillinase (= !-lactamase) resistant
Methicillin
Semisynthetic
Poor oral availability (only parenteral)
Active against gram-pos bacteria
Mostly used for Staphylococcus aureus
Oxacillin
Good oral availability
Cloxacillin
Dicloxacillin
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Broad spectrum penicillinase (= !-lactamase) sensitive
(= Aminopenicillins)
Ampicillin
Semisynthetic
Good oral availability
Active against gram-pos and gram-neg bacteria
Active against enterobacteria
Amoxicillin
Excellent oral availability
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Extended spectrum penicillinase (= !-lactamase) sensitive
(= Carboxypenicillins)
Carbenicillin
Semisynthetic
Poor oral availability
Active against gram-pos and gram-neg bacteria
Active against Pseudomonas aeruginosa, Klebsiella
Ticarcillin
Mezlocillin
Pipercillin
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Cephalosporines
Derived from Cephalosporium sp. (same antibiotic mechanism as penicillins)
Cross-allergies with penicillins are common
Some CSs antagonize Vitamin K => bleeding
Some CSs block alcohol oxidation => disulfiram effect
Classified into generations:
1-4
Increasing activity against gram-negative bacterial and anaerobes
Increasing resistance to destruction by beta-lactamases
Increasing ability to reach cerebrospinal fluid
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
First generation !-lactamase sensitive
Cefazolin
Naturally occuring
Active against gram-positive bacteria
Cephalexin
Second generation !-lactamase sensitive
Cefaclor
Some activity against gram-neg bacteria
Cefamandole
Cefoxitin
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Third generation mostly !-lactamase resistant
Cefotaxime
Active against gram-negative bacteria
Active against Pseudomonas aeruginosa
Active against enterobacteria, gonococcus
Penetrates the CNS => used for meningitis
Ceftriaxone
Fourth generation mostly !-lactamase restistant
Cefepime
Broadest antimicrobial spectrum of any drug
Used for MDR bacteria and mixed
infections
Cefpirome
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Beta-lactamase inhibitors
Clavulanic acid
Irreversible inhibitor of !-lactamase
Good oral absorption
Combined with amoxicillin or ticarcillin
Sulbactam
B
I
M
M
1
1
8
Antibiotics - Cell wall synthesis inhibitors
Vancomycin
Only effective against gram-positive bacteria
Poor oral absorption => used for GI infections
Used to be the Magic bullet for methicillin-resistant
staphylococci, but now staph are becoming V-resistant.
Dose-related ototoxocity:
Tinnitus, high-tone deafness; can progress to total deafness
Bacitracin
Mixture of polypeptides
Serious nephrotoxicity => only topical use
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Protein synthesis inhibitors:
Inhibit either the 30s or 50s ribosomal subunit
(bacterial ribosomal subunits differ from
mammalian ones => drugs are selective
for bacterial protein synthesis)
Class based on chemical structure
of the compounds
Drugs need to enter bacteria =>
entry inhibition is a point of drug resistance
Classification:
Aminoglycosides (bactericidal)
Tetracyclins
Macrolides
Chloramphenicol
Clindamycin
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Aminoglycosides
Broad spectrum antibiotics (bactericidal)
Penetration into cell requires an oxygen-dependent transport => anaerobes are
resistant
(Chloramphenicol blocks this transport => inhibits AG uptake into bacteria;
Penicillins weaken the cell wall => promote AG uptake)
Poor oral absorption (very polar) => parenteral administration
Narrow therapeutic range - severe side effects:
Ototoxicity: destruction of outer hair cells in organ of Corti
Nephrotoxicity: killing of proximal tubular cells
Neuromuscular toxicity: blockage of presynaptic ACh release => respiratory suppression
Elimination almost completely by glomerular filtration
(impaired kidney function => concentration of AG increases => toxicity)
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Aminoglycosides
Gentamicin
Tobramycin
Streptomycin
Neomycin
Kanamycin
Amikacin
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Tetracyclines
Penetration into cell requires an energy-dependent transport not present in mammals
Oral absorption impaired by food (insoluble chelates with Ca, Mg => caution w/ antacids)
Side effects:
Incorporation into teeth and bone => staining of teeth; retardation of bone growth
(not used in children and during pregnancy)
Photosensitivity
Broad spectrum antibiotics (bacteriostatic)
Also useful for treating rickettsial diseases (Rocky mountain spotted fever), Spirochetes
(Lyme disease), Mycoplasma (pneumonia)
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Tetracyclines
Tetracycline
From Streptomyces sp.
Oxytetracycline
Minocycline
Doxycycline
Used to treat rosacea and prevent rhinophyma
No food interaction
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Macrolides
Narrow spectrum antibiotics similar to penicillin (bacteriostatic or bactericidal)
=> good alternative for patients w/ penicillin allergy
Few side effects (GI disturbances), similar food interaction as tetracyclines
Also used for treating Mycoplasma (pneumonia) and Legionella (Legionnaires disease)
Erythromycin
From Streptomyces erythreus
Azithromycin
Very long half-life (>24 h)
Convient use (Z-Pak, Zithromax) - 6 pill regimen
Clarithromycin
Used for H. pylori infection
B
I
M
M
1
1
8
Antibiotics - Protein synthesis inhibitors
Chloramphenicol
Very broad spectrum (almost all bacteria except Pseudomonas aeruginosa)
Very severe side effects
Bone marrow depression => fatal aplastic anemia
Reserved for life-threatening, otherwise treatment-resistant infections
Clindamycin
Medium broad spectrum (gram-positive organisms, anaerobes)
Used for treatment of penicillin-resistant cocci
Side effects: Colitis (triggered by toxin from clindamycin-resistant Clostridium difficile =>
combined w/ vancomycin to kill C. difficile)
B
I
M
M
1
1
8
Antibiotics - Folate Antagonsits
Folate antagonists
Bacteria can not absorb folic acid => synthesis from p-amino-benzoic acid (PABA)
required (Folic acid is a vitamin for humans => synthesis pathway is restricted to
bacteria => selective drug target)
Folate antagonsists block folate synthesis => inhibition of nucleotide synthesis =>
bacteriostatic effect
(pus provides alternative source for nucleotides => drugs are inactive in the presence
of pus or necrotic tissue)
B
I
M
M
1
1
8
Antibiotics - Folate Antagonists
Sulfonamides
Structural analogues of PABA => compete with PABA for Dihydropteroate-synthase
Used for infected burns, STDs, toxoplasmosis
Note:
Many local anesthetics are PABA-esters => they antagonize folate antagonists
Sulfadiazine
Sulfadimidine
Sulfamethoxazole
B
I
M
M
1
1
8
Antibiotics - Folate Antagonists
Trimethoprim
Resembles pteridine moiety of folates => compete with folates for Dihydrofolate-
reductase
Use similar to sulfonamides
Combined with Sulfomethoxazole (synergistic effect) = Co-trimoxazole (Bactrim)
Used for urinary tract infections
B
I
M
M
1
1
8
Antibiotics - Quinolones
Quinolones
Synthetic inhibitors of DNA-Gyrase (= Topoisomerase II), a bacterial enzyme that
winds and unwinds DNA (required for supercoiling the bacterial genome) =>
inhibition of DNA synthesis and transcription
Very broad spectrum, bactericidal - well tolerated
Al and Mg interfer with absorption (antacids!)
Mostly fluorinated = Fluoroquinolones (except nalidixic acid = first quinolone)
B
I
M
M
1
1
8
Antibiotics - Quinolones
Quinolones
Nalidixic acid
Oldest quinolone
Only used for urinary tract infections
Improvement through structure-activity relationship:
Adding fluorine at position 6 will significantly increase activity
Substitution of piperazinyl-ring at position-7 will give the drug antipseudomonal activity
Ciprofloxacin
Most commonly used quinolone (Cipro)
Very broad spectrum => used for emergencies
(B. anthracis attacks in 2001)
Levofloxacin
Ofloxacin
Norfloxacin
Travofloxacin
B
I
M
M
1
1
8
Antibiotics - Summary
You might also like
- Antimicrobial AgentsDocument14 pagesAntimicrobial AgentsAllyssa TolibasNo ratings yet
- Biosel-Mikro Mekanisme Antibiotik 2022Document45 pagesBiosel-Mikro Mekanisme Antibiotik 20226. Putu Arbita DivyaNo ratings yet
- Vet - II Pharmacology - Tutorial For 2024Document74 pagesVet - II Pharmacology - Tutorial For 2024yomifgaramuNo ratings yet
- Farmakologi Obat AntibiotikDocument27 pagesFarmakologi Obat AntibiotikRecofol100% (1)
- Chapter 12 Powerpoint LDocument50 pagesChapter 12 Powerpoint LDennis Nabor Muñoz, RN,RMNo ratings yet
- Antimicrobial Agents: Prof. Khaled H. Abu-ElteenDocument133 pagesAntimicrobial Agents: Prof. Khaled H. Abu-ElteenMing GamonganNo ratings yet
- Cell Wall Synthesis Inhibitors-Lecture 1Document29 pagesCell Wall Synthesis Inhibitors-Lecture 1Kwanele MvelaseNo ratings yet
- Antibacterial and Antiinfective AgentsDocument80 pagesAntibacterial and Antiinfective AgentsAbbeygale GalanNo ratings yet
- Chapter 10. ChemotherapyDocument157 pagesChapter 10. ChemotherapyAbel GirmaNo ratings yet
- Antimicrobial DrugsDocument37 pagesAntimicrobial DrugsNicoleNo ratings yet
- Antibiotics (Part 1) : General Microbiology MLAB 213Document76 pagesAntibiotics (Part 1) : General Microbiology MLAB 213Norman DamaaNo ratings yet
- Infectious DrugsDocument72 pagesInfectious DrugsArianne Mari BalingitNo ratings yet
- Mechanism of Drug ResistanceDocument105 pagesMechanism of Drug ResistanceHimani AggarwalNo ratings yet
- Anti InfectivesDocument4 pagesAnti InfectivespaderamosNo ratings yet
- Antimicrobial ChemotherapyDocument12 pagesAntimicrobial ChemotherapyArvi MandaweNo ratings yet
- Microbiology and Parasitology Week 3. ABCDDocument21 pagesMicrobiology and Parasitology Week 3. ABCDohsehuns wifeuNo ratings yet
- AntibioticsDocument101 pagesAntibioticsdentistmai24No ratings yet
- Farmakologi Obat AntibiotikDocument27 pagesFarmakologi Obat Antibiotikroby gultomNo ratings yet
- Antimicrobial drugsDocument83 pagesAntimicrobial drugsmokhtarNo ratings yet
- AntibioticsDocument64 pagesAntibioticsogatojohnsonNo ratings yet
- Beta Lactams LectureDocument59 pagesBeta Lactams Lecturexmd6787qpqNo ratings yet
- Chapter-9 Antibiotic and Emergence of Resistance - 1Document27 pagesChapter-9 Antibiotic and Emergence of Resistance - 1Hillani TadesseNo ratings yet
- Microbiology Assignmentt xxx123Document16 pagesMicrobiology Assignmentt xxx123ADITYAROOP PATHAKNo ratings yet
- Bacterial Cell Wall Synthesis InhibitorsDocument30 pagesBacterial Cell Wall Synthesis InhibitorsBYAWELE JAIRUS WANGUSANo ratings yet
- Controlling Microbial Growth in Vivo Using Antimicrobial AgentsDocument3 pagesControlling Microbial Growth in Vivo Using Antimicrobial AgentsMaria Gloria Aquino BorjaNo ratings yet
- AntibacterialsDocument54 pagesAntibacterialspooja pandeyNo ratings yet
- Bacterial Cell Wall InhibitorsDocument30 pagesBacterial Cell Wall InhibitorsBYAWELE JAIRUS WANGUSANo ratings yet
- Microbiology Assignmentt TradeDocument14 pagesMicrobiology Assignmentt TradeADITYAROOP PATHAKNo ratings yet
- Drugs, Microbes, Host - The Elements of ChemotherapyDocument23 pagesDrugs, Microbes, Host - The Elements of ChemotherapyRechell ValmoresNo ratings yet
- Ic. Cell Wall Synthesis InhibitorsDocument47 pagesIc. Cell Wall Synthesis InhibitorsTariku BogaleNo ratings yet
- TNB 11 Antibacterials III Penicillin Beta Lactam and Other Cell Wall InhibitorsDocument85 pagesTNB 11 Antibacterials III Penicillin Beta Lactam and Other Cell Wall InhibitorsYsabelle DamasoNo ratings yet
- Chemotherapy Part1 Lecture 8 Cephalosporin AddedDocument47 pagesChemotherapy Part1 Lecture 8 Cephalosporin Addedkamelshehata940No ratings yet
- Antibacterial AgentsDocument73 pagesAntibacterial AgentsAnzo SimonNo ratings yet
- Cell Wall Inhibitor PPT SlideDocument47 pagesCell Wall Inhibitor PPT Slidekhawaja sahabNo ratings yet
- Antimicrobial Chemotherapeutic AgentsDocument41 pagesAntimicrobial Chemotherapeutic Agentscyrilsenior06No ratings yet
- Antibioticresistance PowerpointDocument51 pagesAntibioticresistance PowerpointDiah AyuningrumNo ratings yet
- 5.2 Antimicrobial Resistance EditDocument23 pages5.2 Antimicrobial Resistance EditWong ShuanNo ratings yet
- Antimicrobial Drugs: Prof DR Thamer Mutlag JasimDocument51 pagesAntimicrobial Drugs: Prof DR Thamer Mutlag JasimFlorinda PllanaNo ratings yet
- Antimicrobcell Wall InhibitorsDocument21 pagesAntimicrobcell Wall Inhibitorsymeen9829No ratings yet
- Antibiotics 1Document64 pagesAntibiotics 1Justin Ancog100% (1)
- Micro 5Document37 pagesMicro 5Ha LeemNo ratings yet
- Antibioticresistance PowerpointDocument51 pagesAntibioticresistance PowerpointOdy100% (1)
- Antimicrobial Drugs: Fading Miracle?Document51 pagesAntimicrobial Drugs: Fading Miracle?Tamta SajaiaNo ratings yet
- Antibiotic Resistance PowerpointDocument51 pagesAntibiotic Resistance PowerpointAmir IntizarNo ratings yet
- Topic 16.1 - Inhibiting The Growth of Pathogens in Vivo Using Anti-Microbial AgentsDocument25 pagesTopic 16.1 - Inhibiting The Growth of Pathogens in Vivo Using Anti-Microbial AgentsMashimallowNo ratings yet
- Antimicrobial Drugs: Fading Miracle?Document51 pagesAntimicrobial Drugs: Fading Miracle?Sharma AmitNo ratings yet
- Antibacterial AgentsDocument44 pagesAntibacterial Agentsbelindasithole965No ratings yet
- 6 AntibioticsDocument86 pages6 AntibioticsSalih IntajNo ratings yet
- AntibioticsDocument47 pagesAntibioticsIon CiorescuNo ratings yet
- Microbiology Lec 4 by Shatha M.AliDocument32 pagesMicrobiology Lec 4 by Shatha M.Aliمحمد عماد علي احمدNo ratings yet
- Introduction To ChemotherapyDocument75 pagesIntroduction To ChemotherapymariamanoNo ratings yet
- AntibioticDocument84 pagesAntibioticDr. Kalavati PrajapatiNo ratings yet
- Cell Wall Synthesis Inhibitors: Pharmacology Seminar Group: A1Document113 pagesCell Wall Synthesis Inhibitors: Pharmacology Seminar Group: A1Lola KhatimNo ratings yet
- Classification and Characteristics of Antibiotics OoQeaTSDocument7 pagesClassification and Characteristics of Antibiotics OoQeaTSvenkybyagari1129No ratings yet
- AntimicrobialsDocument53 pagesAntimicrobialsKhupe KafundaNo ratings yet
- Lecture 7 Chemotherapeutic AgentDocument54 pagesLecture 7 Chemotherapeutic AgentjowditzNo ratings yet
- 22 - Disease Biology PDFDocument28 pages22 - Disease Biology PDFashutosh samalNo ratings yet
- Resistance To AntimicrobialsDocument5 pagesResistance To AntimicrobialsLuqman Al-Bashir FauziNo ratings yet
- Antimicrobial DrugsDocument20 pagesAntimicrobial Drugsmaria adventia martinNo ratings yet
- Antimicrobial Therapy in Veterinary MedicineFrom EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreRating: 4 out of 5 stars4/5 (1)
- Brenner and Stevens, Pharmacology 3 © 2010Document5 pagesBrenner and Stevens, Pharmacology 3 © 2010PharAwayNo ratings yet
- Antibiotic Drug Resistance PDFDocument700 pagesAntibiotic Drug Resistance PDFDiego RamosNo ratings yet
- Febril NetropeniDocument352 pagesFebril NetropeniDilessandro PieroNo ratings yet
- Jurnal Antibiotik 2Document11 pagesJurnal Antibiotik 2Achmad YunusNo ratings yet
- DR Retno Budiarti, DR., M.Kes Microbiology Department FK UhtDocument45 pagesDR Retno Budiarti, DR., M.Kes Microbiology Department FK UhtalyaNo ratings yet
- HesterDocument44 pagesHesterDyah tantri WNo ratings yet
- Prescribing in Patients With Liver Disease: Rakesh K TandonDocument4 pagesPrescribing in Patients With Liver Disease: Rakesh K Tandonjoydeep chakrabortyNo ratings yet
- Practice Test 2Document29 pagesPractice Test 2Roscelie KhoNo ratings yet
- Neomycin Is An Aminoglycoside AntibioticDocument5 pagesNeomycin Is An Aminoglycoside AntibioticDeby Nareswari HuslanNo ratings yet
- Review Questions On Antiviral and AntibioticDocument63 pagesReview Questions On Antiviral and AntibioticusedforfunplocNo ratings yet
- 1) Each Question Carries 2 Marks. 2) Every Correct Answer Has Weightage of 2 MarksDocument482 pages1) Each Question Carries 2 Marks. 2) Every Correct Answer Has Weightage of 2 MarksAyushmanNo ratings yet
- Applying Pharmacokinetic/Pharmacodynamic Principles in Critically Ill Patients: Optimizing Ef Ficacy and Reducing Resistance DevelopmentDocument18 pagesApplying Pharmacokinetic/Pharmacodynamic Principles in Critically Ill Patients: Optimizing Ef Ficacy and Reducing Resistance DevelopmentValentina Lcpc CajaleonNo ratings yet
- AntibioticsDocument4 pagesAntibioticsVladimir GurjanovNo ratings yet
- ATI Proctored Nursing Care of Children Exam Study Guide Verified 100Document7 pagesATI Proctored Nursing Care of Children Exam Study Guide Verified 100ianshirow834No ratings yet
- دوائيات ن- lec22-ReducedDocument24 pagesدوائيات ن- lec22-Reducedma22mdmmNo ratings yet
- Leilani O. Estacio, Man RN: Chemotherapeutic Agents, Antibiotics, Immunosuppressive DrugsDocument42 pagesLeilani O. Estacio, Man RN: Chemotherapeutic Agents, Antibiotics, Immunosuppressive DrugsHERLIN HOBAYANNo ratings yet
- Type A Choice Questions (Only One Answer Is Correct) : A. B. C. D. EDocument10 pagesType A Choice Questions (Only One Answer Is Correct) : A. B. C. D. ERAED GhunaimNo ratings yet
- Chapter 12 Powerpoint LDocument50 pagesChapter 12 Powerpoint LDennis Nabor Muñoz, RN,RMNo ratings yet
- Antibiotics 9Document11 pagesAntibiotics 9Beth Morales100% (1)
- I V E C C S 2004: Luid TherapyDocument5 pagesI V E C C S 2004: Luid TherapyCaraiman RalucaNo ratings yet
- DSTFC Chapters 1 5Document70 pagesDSTFC Chapters 1 5Sean MarianoNo ratings yet
- ChemotherapyDocument11 pagesChemotherapyMaria Fudji HastutiNo ratings yet
- Mark Kilimek AUDIO NOTESDocument6 pagesMark Kilimek AUDIO NOTESHannah Perkins100% (2)
- AminoglycosidesDocument23 pagesAminoglycosidesShahid IqbalNo ratings yet
- 2.20140209 Question PaperDocument16 pages2.20140209 Question PaperdrpnnreddyNo ratings yet
- AntibioticsDocument8 pagesAntibioticsمحمد بن صالحNo ratings yet
- Clinical Pharmacy of AntibioticsDocument53 pagesClinical Pharmacy of AntibioticsEkanita DesianiNo ratings yet
- Protocol - Aminoglycoside DosingDocument5 pagesProtocol - Aminoglycoside DosingThomasNo ratings yet
- Antimcrobial Therapy NELSON 2016 288 PagDocument288 pagesAntimcrobial Therapy NELSON 2016 288 PagNorvy CuberosNo ratings yet
- Ototoxic DrugsDocument5 pagesOtotoxic DrugsDr-Firas Nayf Al-ThawabiaNo ratings yet