Professional Documents
Culture Documents
Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - Hydrocephalus
Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - Hydrocephalus
Uploaded by
Robert MontgomeryOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - Hydrocephalus
Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - Hydrocephalus
Uploaded by
Robert MontgomeryCopyright:
Available Formats
PAPILLOEDEMA
1. Introduction
2. Classification of papilloedema
Early
Established (acute)
Longstanding (chronic)
Atrophic (secondary optic atrophy)
Circulation of cerebrospinal fluid
Causes of raised intracranial pressure
Hydrocephalus
(a) Subarachnoid space
Circulation of cerebrospinal fluid
(b) Lateral ventricle
(c) Third ventricle
(d) Aqueduct
(e) Fourth ventricle
a
b
c
e
d
1. Space-occupying lesions
Causes of Raised Intracranial Pressure
2. Blockage of ventricular system
3. Obstruction of CSF absorption
4. Benign intracranial hypertension
(pseudotumour cerebri)
5. Diffuse cerebral oedema
6. Hypersecretion of CSF
Hydrocephalus
Dilated cerebral ventricles
Communicating - obstruction to CSF flow in basilar
cisterns or cerebral subarachnoid space
Non-communicating - obstruction to CSF flow in ventricular
system or at exit of foramina of fourth ventricle
Early papilloedema
VA - normal
Mild disc hyperaemia
Indistinct disc margins - initially nasal
Mild venous engorgement
Normal optic cup
Spontaneous venous pulsation - absent (also absent in 20% of normals)
Established papilloedema (acute)
VA - usually normal
Severe disc elevation and hyperaemia
Very indistinct disc margins
Obscuration of small vessels on disc
Marked venous engorgement
Reduced or absent optic cup
Haemorrhages + cotton-wool spots
Macular star
Longstanding papilloedema (chronic)
VA - variable
Marked disc elevation but less hyperaemia
Disc margins - indistinct
Variable venous engorgement
Absent optic cup
Atrophic papilloedema (secondary optic atrophy)
VA - severely decreased
Mild disc elevation
Indistinct disc margins
Disc pallor with few crossing vessels
Absent optic cup
You might also like
- Cyanotic Heart DiseaseDocument47 pagesCyanotic Heart Disease87-Saranya MNo ratings yet
- Short Cases 700 SlidesDocument703 pagesShort Cases 700 SlidesStefanie VirniaNo ratings yet
- HydrocephalusDocument39 pagesHydrocephalusAjeng Aristiany Rahawarin100% (2)
- Sudden Loss of Vision & Optic NeuropathyDocument30 pagesSudden Loss of Vision & Optic NeuropathyIshak IzharNo ratings yet
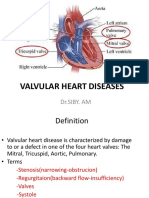
- Valvular Heart Disease Medical Surgical NursingDocument75 pagesValvular Heart Disease Medical Surgical NursingGodfrey Franco88% (8)
- 58 Pa Pill OedemaDocument8 pages58 Pa Pill OedemaAnonymous IruFyBNo ratings yet
- Classification of PapilloedemaDocument6 pagesClassification of PapilloedemaYustia SariNo ratings yet
- Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - HydrocephalusDocument8 pagesPapilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - HydrocephalusmksharmaaNo ratings yet
- Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - HydrocephalusDocument8 pagesPapilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - HydrocephalusAdPutriPutriNo ratings yet
- Week 6 Disturbances in CirculationDocument83 pagesWeek 6 Disturbances in CirculationHans CortezNo ratings yet
- HydrocephalusDocument39 pagesHydrocephalusspiritNo ratings yet
- Chronic Venous Insufficiency - (Cvi)Document48 pagesChronic Venous Insufficiency - (Cvi)Andrei EfremovNo ratings yet
- 25) Aetiology and Pathogenesis of Valvular Heart DiseaseDocument34 pages25) Aetiology and Pathogenesis of Valvular Heart DiseaseGurrajvin Singh0% (1)
- Hydro Cep Hal UsDocument65 pagesHydro Cep Hal UsKrisna MuhammadNo ratings yet
- Pediatric Cardiology: D R J O S E M N U Ñ E ZDocument24 pagesPediatric Cardiology: D R J O S E M N U Ñ E ZTim HoseinNo ratings yet
- Hydrocephalous MMC - 1Document40 pagesHydrocephalous MMC - 1Ibn-e- qaisarNo ratings yet
- #5 Neonatal Cardiac AnomaliesDocument93 pages#5 Neonatal Cardiac AnomaliesSittie Hania100% (2)
- Nurological Emergencies د.عارفDocument54 pagesNurological Emergencies د.عارفMohammad BelbahaithNo ratings yet
- CVS Last Version (25-9)Document182 pagesCVS Last Version (25-9)DaNy Chiriac0% (1)
- HydrocephalussDocument32 pagesHydrocephalussElvisNo ratings yet
- Hydrocephalus WPS OfficeDocument16 pagesHydrocephalus WPS OfficeOeyi Mutia SatifaNo ratings yet
- Clinical Aspect of Maternal and Child NursingDocument21 pagesClinical Aspect of Maternal and Child NursingMarianne CoracheaNo ratings yet
- Congenital Heart DefectsDocument73 pagesCongenital Heart DefectsStaen KisNo ratings yet
- Head &neck Examination 1Document43 pagesHead &neck Examination 1omod415No ratings yet
- Renal Session 2 PDFDocument101 pagesRenal Session 2 PDFDokki ScanNo ratings yet
- HydrocephalusDocument19 pagesHydrocephalusBhavik ChopdaNo ratings yet
- Core Curriculum Lecture 17 Renal Abnormalities (Excluding MaDocument82 pagesCore Curriculum Lecture 17 Renal Abnormalities (Excluding MaHamis MayambalaNo ratings yet
- Ch12 HeartDocument130 pagesCh12 HeartNoelle Grace Ulep BaromanNo ratings yet
- Valve Disease AtfDocument32 pagesValve Disease Atfyahomed519No ratings yet
- Vascular Disorders of RetinaDocument46 pagesVascular Disorders of RetinaSubash BasnetNo ratings yet
- Scanning Technique of KidneysDocument103 pagesScanning Technique of KidneysPhuntsho OngmoNo ratings yet
- Penyakit Jantung KongenitalDocument30 pagesPenyakit Jantung KongenitalrintiikNo ratings yet
- Penyakit Jantung Bawaan - IDocument44 pagesPenyakit Jantung Bawaan - IEkisliefvirjou Adelihira HidraNo ratings yet
- Feeling Blue, A Presentation: Ronald MbwasiDocument29 pagesFeeling Blue, A Presentation: Ronald MbwasiALL KINDS By Milseni KNo ratings yet
- 3 - Valvular Heart DiseasesDocument43 pages3 - Valvular Heart DiseasesHamzehNo ratings yet
- The Retina AtfDocument34 pagesThe Retina Atfmarina wezlyNo ratings yet
- Congenital Heart DiseasesDocument27 pagesCongenital Heart DiseasesJumar ValdezNo ratings yet
- Papilloedema and Optic AtrophyDocument27 pagesPapilloedema and Optic AtrophyRobert MontgomeryNo ratings yet
- University of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingDocument69 pagesUniversity of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingErica Veluz LuyunNo ratings yet
- HF & APO Group 5 Year 5 2012Document38 pagesHF & APO Group 5 Year 5 2012topper1101No ratings yet
- Kabwe Central Hospital: "Hydrocephalus"Document39 pagesKabwe Central Hospital: "Hydrocephalus"Emmanuel MukukaNo ratings yet
- Hydrocephalus: Presented by DR Elvis Frimpong Peprah AapcDocument22 pagesHydrocephalus: Presented by DR Elvis Frimpong Peprah AapcKofi YeboahNo ratings yet
- Hyperemia CongestionDocument40 pagesHyperemia CongestionBikash PuriNo ratings yet
- 991111 EUS教學 (6) 重點式急診心臟超音波之應用Document67 pages991111 EUS教學 (6) 重點式急診心臟超音波之應用juice119100% (5)
- Valvular Heart DiseaseDocument42 pagesValvular Heart DiseaseareeparambilNo ratings yet
- Rheumatic Fever and Heart DiseaseDocument30 pagesRheumatic Fever and Heart DiseaseerikarobertNo ratings yet
- Achd LectureDocument48 pagesAchd LecturedrmdsaeedNo ratings yet
- Congenital Heart DiseaseDocument22 pagesCongenital Heart DiseaseDiosa MedinaNo ratings yet
- Cardiac Physical ExamDocument45 pagesCardiac Physical ExamARIANNE JOY TAMARAY100% (1)
- Mata Tenang Visus Turun MendadakDocument75 pagesMata Tenang Visus Turun MendadakDianMuliasariNo ratings yet
- Fitz Cardiology Paces NotesDocument26 pagesFitz Cardiology Paces NotesMuhammad BilalNo ratings yet
- Congenital Heart Defect EDITDocument57 pagesCongenital Heart Defect EDITnicholasacquah680No ratings yet
- Ntroduction To The Physical ExaminationDocument4 pagesNtroduction To The Physical ExaminationAngelica NenitaNo ratings yet
- Sirosis HatiDocument17 pagesSirosis HatiAndrianto WongkarNo ratings yet
- Acyanotic Heart Disease& Fetal Circulation: Guided By, Dr.K.Sivakanthan Consultant PaediatricianDocument98 pagesAcyanotic Heart Disease& Fetal Circulation: Guided By, Dr.K.Sivakanthan Consultant PaediatricianVijayakanth VijayakumarNo ratings yet
- Aortic Regurgitation: Vitrag24-Www - Medic ComDocument68 pagesAortic Regurgitation: Vitrag24-Www - Medic ComAlshare NisreenNo ratings yet
- Hematology Notes for Medical StudentsFrom EverandHematology Notes for Medical StudentsRating: 5 out of 5 stars5/5 (1)
- Multidrug-Resistant Tuberculosis (MDR-TB) : 2012 UpdateDocument2 pagesMultidrug-Resistant Tuberculosis (MDR-TB) : 2012 UpdateRobert MontgomeryNo ratings yet
- The Extended FAST Exam: ObjectivesDocument16 pagesThe Extended FAST Exam: ObjectivesRobert MontgomeryNo ratings yet
- Asphyxia: Forensic Medicine Rs Bhayangkara Porong Fakultas Kedokteran Universitas Muhammadiyah MalangDocument7 pagesAsphyxia: Forensic Medicine Rs Bhayangkara Porong Fakultas Kedokteran Universitas Muhammadiyah MalangRobert MontgomeryNo ratings yet
- Interprofessional Education PDFDocument3 pagesInterprofessional Education PDFRobert MontgomeryNo ratings yet
- Nephrotic Syndrome IDocument12 pagesNephrotic Syndrome IRobert MontgomeryNo ratings yet
- Daftar Pustaka EdiarDocument1 pageDaftar Pustaka EdiarRobert MontgomeryNo ratings yet
- Managing Acute Pain in The Developing WorldDocument8 pagesManaging Acute Pain in The Developing WorldRobert MontgomeryNo ratings yet
- Papilloedema and Optic AtrophyDocument27 pagesPapilloedema and Optic AtrophyRobert MontgomeryNo ratings yet