Professional Documents
Culture Documents
1 s2.0 S009923991200163X Main
1 s2.0 S009923991200163X Main
Uploaded by
Reeba Mary PrinceCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Mms Protocol 2000Document2 pagesMms Protocol 2000bagus918No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Diabetes Mellitus Type 2 Schematic DiagramDocument1 pageDiabetes Mellitus Type 2 Schematic DiagramJhe Lyn82% (11)
- Mediastinum Sesat Ix-1Document23 pagesMediastinum Sesat Ix-1kelly christyNo ratings yet
- Watchtower: Jury Trial Day 5, Candace Conti v. WatchtowerDocument192 pagesWatchtower: Jury Trial Day 5, Candace Conti v. WatchtowersirjsslutNo ratings yet
- 1 s2.0 S009923991200516X MainDocument3 pages1 s2.0 S009923991200516X MainReeba Mary PrinceNo ratings yet
- 1 FP2 FPD Lecture 2011pdfDocument309 pages1 FP2 FPD Lecture 2011pdfReeba Mary PrinceNo ratings yet
- Restorative1 1 GudDocument44 pagesRestorative1 1 GudReeba Mary PrinceNo ratings yet
- Viva Questions 1Document15 pagesViva Questions 1Reeba Mary PrinceNo ratings yet
- 2012 Pall Care For Pancreas CancerDocument6 pages2012 Pall Care For Pancreas CancerFilip IonescuNo ratings yet
- How To Download Gordis Epidemiology E Book 6Th Edition Ebook PDF Ebook PDF Docx Kindle Full ChapterDocument36 pagesHow To Download Gordis Epidemiology E Book 6Th Edition Ebook PDF Ebook PDF Docx Kindle Full Chapterandrew.taylor131100% (34)
- Gynaecological History TakingDocument16 pagesGynaecological History TakingnelsonNo ratings yet
- GuidelineDocument213 pagesGuidelinedragutin7petri7No ratings yet
- B. NSG 120.2 ChecklistDocument78 pagesB. NSG 120.2 ChecklistAsh TrendzNo ratings yet
- Kontrak Belajar Gadar Igd BaruDocument14 pagesKontrak Belajar Gadar Igd BaruAstridNo ratings yet
- Effectiveness of Interventions To Improve Antidepressant Medication Adherence: A Systematic ReviewDocument22 pagesEffectiveness of Interventions To Improve Antidepressant Medication Adherence: A Systematic ReviewJaviera Rodríguez DelgadoNo ratings yet
- Toxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofDocument5 pagesToxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofFrancis AbuludeNo ratings yet
- SALTAPSDocument24 pagesSALTAPSFatima Tu ZahraNo ratings yet
- BCCH Diabetic Ketoacidosis Protocol Toolkit: Endocrinology & Diabetes UnitDocument16 pagesBCCH Diabetic Ketoacidosis Protocol Toolkit: Endocrinology & Diabetes UnitaseelNo ratings yet
- Log Sheet 2Document4 pagesLog Sheet 2SHAFIQNo ratings yet
- 6-Article Text-48-2-10-20200611Document4 pages6-Article Text-48-2-10-20200611anggimerlina52No ratings yet
- Balanced Diet: Bhavya Mds I Year Department of Conservative Dentistry & EndodonticsDocument76 pagesBalanced Diet: Bhavya Mds I Year Department of Conservative Dentistry & EndodonticsMayank AggarwalNo ratings yet
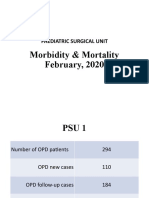
- Morbidity & Mortality (February, 2020)Document14 pagesMorbidity & Mortality (February, 2020)Wai GyiNo ratings yet
- Biology Investigatory Project On HypothyroidismDocument8 pagesBiology Investigatory Project On Hypothyroidismsagarparida6428No ratings yet
- J500210089 Muhammad Rizqy Noer Tuanaya Tugas Jurnal Bahasa Indonesia 2022Document14 pagesJ500210089 Muhammad Rizqy Noer Tuanaya Tugas Jurnal Bahasa Indonesia 2022kiki tuanaya1No ratings yet
- Dial YseDocument314 pagesDial YseSeda Muse KusNo ratings yet
- Acute TonsillitisDocument34 pagesAcute TonsillitisArvindhan100% (1)
- FF Japanese Gastric Cancer Treatment Guidelines 2018 (5th Edition) SpringerLinkDocument1 pageFF Japanese Gastric Cancer Treatment Guidelines 2018 (5th Edition) SpringerLinkFlaviu Ionuț FaurNo ratings yet
- Padlan Getigan and PartnersDocument4 pagesPadlan Getigan and PartnersMichaelandKaye DanaoNo ratings yet
- Virus ShapesDocument2 pagesVirus Shapessarath chandNo ratings yet
- CvadDocument11 pagesCvadNjideka A.No ratings yet
- Refractive Amblyopia: I Wayan Ardy Paribrajaka (1871122001)Document17 pagesRefractive Amblyopia: I Wayan Ardy Paribrajaka (1871122001)ratihpdewiNo ratings yet
- IV. Modul 10 - Pengelolaan NyeriDocument97 pagesIV. Modul 10 - Pengelolaan NyeriGrace Noviyanthi SinambelaNo ratings yet
- Blood Result Interpretation BookletDocument129 pagesBlood Result Interpretation BookletsithumNo ratings yet
- Bio Powerpoint 3Document10 pagesBio Powerpoint 3Romina SalazarNo ratings yet
1 s2.0 S009923991200163X Main
1 s2.0 S009923991200163X Main
Uploaded by
Reeba Mary PrinceOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1 s2.0 S009923991200163X Main
1 s2.0 S009923991200163X Main
Uploaded by
Reeba Mary PrinceCopyright:
Available Formats
Experimental Formation of Dentin-like Structure in the Root
Canal Implant Model Using Cryopreserved Swine Dental Pulp
Progenitor Cells
Kostas Kodonas, DDS, MSc,* Christos Gogos, DDS, PhD,* SeramPapadimitriou, DVM, DDS, PhD,
Kokona Kouzi-Koliakou, MD, PhD,
and Dimitrios Tziafas, DDS, PhD*
Abstract
Objectives: The purpose of the present study was to
present histological and immunohistochemical evidence
showing the regenerative capacity of swine dental pulp
stem cells (S-DPSCs) seeded on organic or synthetic
scaffolds and implanted as hybrid root implants in
the jaw bone of minipigs. Methods: Immature perma-
nent incisor teeth and unerupted premolars at the early
root-forming stage were extracted from three 7-month-
old minipigs, and mesenchymal stem/progenitor
cells were isolated from dental pulp. Cells were
cryopreserved in liquid nitrogen. A year later, new
permanent incisor and premolar teeth were extracted;
pulp tissue was removed; and pieces of root canals of
the extracted teeth, containing collagen or Poly(lactic-
co-glycolic acid) scaffolds seeded with the autologous
cryopreserved DPSCs, were implanted into the fresh
post-extraction socket of the mini pig jaw. The resulting
constructs were harvested after 6 and 10 weeks and
evaluated by histological and immunohistochemical
analyses. Results: Six weeks postoperatively, the
central canal space of the root implants showed degrad-
ing scaffold material. New extracellular matrix had been
deposited in a polar predentin-like pattern on the canal
dentinal walls by cuboidal nonpolarized cells. Ten weeks
postoperatively, newly formed organic matrix had been
consistently deposited on the canal walls. The presence
of a continuous layer of polarized cells showing typical
columnar morphology adjacent to the newly deposited
organic matrix was evident. Conclusions: The interac-
tions of S-DPSCs with the dentin matrix of roots im-
planted in the jawbone of minipigs constitute a model
to study in vivo organization and differentiation poten-
tial of DPSCs. (J Endod 2012;38:913919)
Key Words
Dental pulp, dentin, minipig, stem cells, tissue engi-
neering
I
n regenerative dentistry, stemcellbased therapies represent a promising approach to
replace damaged dental structures and restore functions of the compromised dental
pulp (1, 2). As tissue engineering applications, they involve the use of three basic key
elements, including stem cells, molecular signals to induce cell differentiation, and
scaffolds as an appropriate environment for cell proliferation and differentiation (3).
Postnatal dental stem cells have been isolated from a variety of tissues (4, 5). To
date, ve different human dental stem/progenitor cells have been isolated, including
dental pulp stem cells (DPSCs) (6), stem cells from exfoliated deciduous teeth (7),
stem cells from apical papilla (8), periodontal ligament stem cells (9), and dental
follicle progenitor cells (10).
In order to support organization and vascularization of the newly formed tissue,
cells must be organized into highly porous three-dimensional scaffolds. Regarding their
composition, several scaffold materials have been used for dental tissue engineering
including organic collagen scaffolds (11); hydroxyapatite or tricalciumphosphate scaf-
folds (12); and nonorganic polymer Poly(lactic-co-glycolic acid) (PLGA) (13, 14),
polyglycolic acid (PGA) (14), or Poly-L-lactic acid (PLLA) scaffolds (15).
The purpose of the present study was to present histological and immunohisto-
chemical evidence showing the regenerative capacity of swine dental pulp stem cells
(S-DPSCs) seeded on organic or synthetic scaffolds and implanted as hybrid root
implants in the jaw bone of minipigs.
Materials and Methods
Isolation and Characterization of DPSCs
All animal and stem cell experiments were approved by the National Institute of
Animal Care and the Ethic Committee of Aristotle University of Thessaloniki. DPSCs
were isolated from three 7-month-old minipigs. Immature permanent incisor teeth
and unerupted premolars at the early root forming stage were extracted. The teeth
were denuded of any soft tissue and stored by placing them crown down in transport
medium (Dulbecco modied Eagle medium [DMEM], Life Technologies, Rockville,
MD) containing penicillin-streptomycin (Pen:Strep; Gemini Bio-Products, West Sacra-
mento, CA). All specimens were directly transported to the laboratory for further pro-
cessing. After the teeth were denuded from any soft tissues attached to the external root
surface including root apical papilla tissue and vertically sectioned in half by mechanical
fracture, the pulp tissue was carefully separated from the tooth, cut into 2 mm
3
-sized
pieces, and washed in phosphate buffered saline.
DPSCs were isolated using the enzymatic digestion method. In detail, pulp-derived
cells were detached by exposure to 20 mg/mL collagenase and 10 mg/mL dispase for
From the *Department of Endodontology, School of Dentistry;
Companion Animals Clinic; and
Laboratory of Histology-Embryology, Medical School, Aristotle
University of Thessaloniki, Thessaloniki, Greece.
Address requests for reprints to Dr Kostas Kodonas, Department of Endodontology, School of Dentistry, Aristotle University of Thessaloniki, GR54124 Thessaloniki,
Greece. E-mail address: kkodonas@dent.auth.gr
0099-2399/$ - see front matter
Copyright 2012 American Association of Endodontists.
doi:10.1016/j.joen.2012.02.005
Basic ResearchBiology
JOE Volume 38, Number 7, July 2012 Direction of Isolated Swine Pulp Stem Cells to Form Dentin 913
60 minutes at 37
C. After the digestion was complete, the enzyme
mixture was neutralized by the addition of medium. Cell suspensions
were then cultured in supplemented media and placed at 37
C in
a humidied atmosphere consisting of 18% O
2
and 5% CO
2
for 1
week. After reaching 80% conuence, 5% of the sample was used
to conrm that the cells met the minimal criteria required to be consid-
ered mesenchymal stem cells (MSCs) according to the International
Society for Cell Therapy position paper (16). More specically, the
expression of cell surface antigen markers for MSCs including STRO-
1, CD90, CD105, and CD146 (BD Pharmingen) and control markers
including CD45 and CD14 (BDPharmingen) were examined by owcy-
tometry (Cytomics FC 500 Flow Cytometer; Beckman Coulter, Fullerton,
CA). The remaining cells were cryopreserved.
The cell-freezing medium consisted of DMEM containing 10% he-
tastarch, human albumin, and dimethyl sulfoxide. After the cells were
transferred to cryovials, the process of cooling them to the temperature
of liquid nitrogen (196
C) was performed gradually in stages; the
procedure included a decrease from room temperature to 7
C at
a 1.5
C/min rate of cooling, from 7
C to 40
C at a 0.5
C/min
rate of cooling, from 40
C to 100
C at a 6
C/min rate of cooling,
and a decrease from 100
C to 196
C at a rapid cooling rate.
One year later, the ow cytometric analysis was repeated to eval-
uate the effect of cryopreservation on the biological properties of the
DPSCs. In detail, the vials were removed from the liquid nitrogen and
incubated in a 37
C bath to thaw. Culture media was added to the cells,
and the cell suspension was centrifuged at 1,000 rpm for 10 minutes.
Cells were then cultured, ow cytometric analysis was repeated (5% of
the sample), and the rest of the sample was seeded onto collagen or
PLGA scaffolds.
Cell Seeding on Collagen or PLGA Scaffolds
A type 1 atelocollagen honeycomb sponge (AteloCell, CSH-10; Ko-
ken Co Ltd, Tokyo, Japan) from bovine origin with an average pore size
of 300 mm was used as scaffold material. Each sponge was further
divided into 1 1 mm
3
pieces and subsequently sanitized in 70%
ethanol and washed in phosphate-buffered saline.
Biodegradable polymer 50/50 poly(DL-lactide-CO-Glycolide-
PLGA; Lactel Absorbable Polymers, Pelham, AL) scaffolds were fabri-
cated using the salt leaching technique as previously described
(14, 17). A 17% (w/v) solution was prepared by dissolving PLGA
polymer in chloroform. Sodium chloride crystals (75150 mm in
diameter) were added to the PLGA solution in a weight ratio of 20:1
and mixed thoroughly. After solvent evaporation, the scaffold
constructs were cut into 1 1 mm
3
pieces. Deionized water was
used to leach out the salt particles. The resulting polymerized PLGA
scaffolds were sanitized in 70% ethanol solution and washed in
phosphate-buffered saline.
Each collagen or PLGA scaffold was seeded by adding 50 to 60 mL
of the cryovial context (containing 3 10
6
of the cryopreserved
S-DPSCs) suspended in 60 mL DMEM. The constructs were placed in
six-well plates and incubated at 37
C in 5% CO
2
overnight to allow
cell attachment.
Transplantation of Seeded Scaffolds Using the Root
Implant Model
The autologous S-DPSCs were implanted into the jawbone of the
adult minipigs using organic (collagen) and synthetic (PLGA) scaffolds
in a new hybrid root implant model. The root implants were manufac-
tured by using the middle part of the root of freshly extracted swine
maxillary and mandibular incisors. After extraction, the tooths crown
as well as the apical and coronal portion of each root were sectioned
with a slow-speed diamond saw (Isomet Buehler, Lake Bluff, IL) under
cooling with sterile water and then discarded. The remaining root
segments, which were 5 to 6 mm in length, were denuded from any
soft tissues attached to the external root surface using a surgical scalpel.
The dental pulp tissue of the remaining root canal was removed me-
chanically with endodontic les and by immersing the root segment
into 3%sodiumhypochlorite for 5 minutes. Before lling the root canal
with the seeded scaffolds, they were subsequently washed in distilled
sterile water at 37
C. Finally, the root canals were lled with the collagen
scaffolds containing S-DPSCs and then implanted into the fresh post-
extraction sockets of the minipig jaw(Fig. 1). A total of 32 root implants
were manufactured and used in this study, whereas ve implants with
empty canal space and ve containing collagen or PLGA scaffolds
without DPSCs served as negative control samples. The resulting
constructs were harvested after 6 and 10 weeks.
Histological and Immunohistochemical Examination
All recovered implants were immediately xed in 10% (w/v)
phosphate-buffered paraformaldehyde and decalcied in Morse solu-
tion (22.5% formic acid and 10% sodium citrate) for 8 weeks. After
being dehydrated by passing through a graded series of ethanol and
cleared in xylene, the decalcied samples were embedded in parafn.
Consecutive tissue sections were cut fromthe parafn blocks into 5-mm
slices and stained with hematoxylin-eosin and Masson trichrome stain.
Immunohistochemical analysis was performed with the Dako
detection kit (Real EnVision Detection System Kit; Dako, Glostrup,
Figure 1. Root canal implant model: the root canals were lled with the collagen scaffolds containing DPSCs (arrow in A) and then implanted into the fresh post-
extraction sockets of the minipig jaw (arrow in B).
Basic ResearchBiology
914 Kodonas et al. JOE Volume 38, Number 7, July 2012
Denmark). The primary antibodies used were afnity-puried human
antimouse Dentin Matrix Protein-1 (DMP-1, LFMb-31: sc-73633; Santa
Cruz Biotechnology, Inc, Heidelberg, Germany) and human antimouse
bone sialophosphoprotein II (BSP-II, LFMb-25: sc-73630; Santa Cruz
Biotechnology, Inc). Parafn sections were deparafnized in xylene, re-
hydrated, washed in Tris-buffered saline (TBS), and subjected to heat-
induced epitope retrieval using the target retrieval solution according to
manufacturers instructions. After inactivating endogenous peroxidase,
the sections were incubated with primary antibodies (1:50 dilution for
both DMP-1 and BSP-II) for 60 minutes. Color development was per-
formed with a Dako envision kit (DakoCytomation, Glostrup, Denmark)
according to the manufacturer. Tissue sections were counterstained
with hematoxylin.
Results
A total of 3 to 15 10
6
cells were obtained from each tooth. The
DPSCs were positive for CD90 (strong expression), CD105, and CD146
(slight expression) and negative for STRO-1 (Fig. 2). Regarding control
markers, the DPSC cultures were more than 95%negative for CD45 and
CD14. Similar results were obtained before and after the cryopreserva-
tion procedure for the MSC markers. S-DPSCs grew at similar rates,
became conuent after similar culture periods, and expressed the
same cell surface markers.
At the time of retrieval, a number of implants appeared to be in
a process of eruption, whereas the external root surfaces exhibited
resorption lacunae with well-organized odontoclasts (Fig. 3A). In
a number of specimens, epithelial proliferation was seen along the
external root surfaces and invaginating epithelium was observed inside
the root canal (Fig. 3B).
Six weeks postoperatively, the central canal space of the root
implants showed proliferating cells lling the voids of the degrading
collagen (Fig. 4A) or PLGA (data not shown) scaffold. New extracellular
matrix had been occasionally deposited in a polar predentin-like
pattern on the canal dentinal walls by nonpolarized cuboidal cells
(Fig. 4B). The remaining voids at the central root canal space revealed
unresorbed scaffold material, meaning that the remaining voids at the
central root canal space revealed scaffold material that has not been
resorbed.
Ten weeks postoperatively, newly formed organic matrix had been
consistently deposited on the canal walls. The presence of a continuous
layer of polarized or nonpolarized cells showing columnar or spindle-
shaped morphology, respectively, associated with the newly deposited
organic matrix of tubular morphology was evident (Fig. 5).
An examination of empty root canal implants or implants
containing only the scaffold material (control) revealed extended
resorption of the root canal dentin walls and the absence of any cellular
activity because the canal space appeared in most cases empty or
containing remnants of the scaffold material at both examination
periods irrespectively of the type of scaffold material used. Immunohis-
tochemical analyses conrmed the expression of DMP and BSP in sites
in which odontoblast-like cell differentiation and newly formed organic
matrix deposition occurred. More specically, the newly formed
odontoblastic-like cell layer lining along the existing canal walls stained
positive for DMP antibody (Fig. 6). BSP was intensely expressed in the
newly formed organic matrix, scaffold remnants, and differentiating
cells (Fig. 7).
Discussion
In the current study, it is evaluated whether the isolation, preser-
vation, and application of autologous mesenchymal DPSCs in the
jawbone of miniature pigs could constitute an experimental model to
study dynamics of stem cellbased root tissue engineering in swine
teeth. Minipigs are considered ideal animals for dental research based
on their following characteristics: growth patterns similar to those in
humans, sufcient amount of rapid growth to allow studies to be
Figure 2. The expression of the cell surface antigens (I) CD90, (II) CD146, (III) CD105, and (IV) STRO-1 in dental pulp stem/progenitor cells isolated from
immature swine teeth. DPSCs strongly expressed CD90, slightly expressed CD105 and CD146, and were negative for STRO-1.
Basic ResearchBiology
JOE Volume 38, Number 7, July 2012 Direction of Isolated Swine Pulp Stem Cells to Form Dentin 915
performed in a specied length of time, physiology similar to that of hu-
mans, easy access to teeth, and low maintenance costs (18, 19).
Much of the excitement that surrounds stem cell research is
related to their ability to differentiate into all of the primary cell types
found in the body (20, 21). An important feature of DPSCs is their
odontoblastic differentiation potential (6). Gronthos et al (6) were
the rst to isolate stemcells fromhuman dental pulp. The ex vivo poten-
tial of the human DPSCs to self-renew and differentiate into chondro-
blasts, osteoblasts, neurons, adipocytes, and odontoblast-like cells
has been shown (12, 22, 23). Regarding in vivo characterization,
it had been reported that transplanted DPSCs mixed with
hydroxyapatite/tricalcium phosphate form ectopic pulpdentin-like
tissue complexes in mice (6, 24). The formation of pulp-like and
dentin-like tissue has been shown also on subcutaneous root canal
implants containing synthetic scaffolds seeded with stem-progenitor
cells from apical papilla and dental pulp (25). Finally, the recent study
of Iohara et al (26) showed complete pulp regeneration after in situ
transplantation of DPSCs into the pulpectomized root canal.
The rst step of tissue engineering approaches is to isolate cells
with the correct phenotype (27). One of the criteria for dening multi-
potent stromal cells is adherence to cell surface molecules composed of
positive and negative selection markers (28). Several cell surface
markers have been used for MSC identication including CD44,
CD105, CD29, CD61, CD146, CD166, and CD90 (28). The porcine
DPSC population has been shown to be positive for CD31, CD105,
CD146, and CD150 and slightly positive for CD34, CD90, and a-smooth
muscle actin (22). It has also been suggested that porcine-derived pulp
cells strongly express CD105 and are slightly positive for CD90 but are
negative for CD31, CD34, CD45, and CD146 (29). In this study, minipig
DPSCs were found to be positive for CD90 (strong expression), CD105,
and CD146 (slight expression) and negative for STRO-1 (Fig. 2).
This study presents morphological, histological, and immunohis-
tochemical evidence characterizing dental pulp progenitors interaction
with dentin by seeding progenitor/stem cells onto collagen scaffolds,
lling pieces of root canals with the cell/scaffold construct, and using
them as root implants in the post-extraction minipig socket. According
to the results, 6 weeks postoperatively the central canal space of the root
implants showed degrading collagen scaffold and proliferating cells
lling the voids (Fig. 4A). At a higher magnication, new extracellular
matrix had been occasionally deposited in a polar predentin-like
pattern on the canal dentinal walls by nonpolarized cuboidal cells
(Fig. 4B). Histological analysis 10 weeks postoperatively showed
more signicant changes. Newly formed organic matrix had been
consistently deposited on the canal walls, and in some cases the forma-
tion of a continuous layer of newly deposited organic layer of uniform
thickness was evident (Fig. 5). However, in most cases, these observa-
tions were coupled by the fact that at longer evaluation periods implant
eruption and root resorption were evident (Fig. 3A).
The results of this study come in agreement with previously pub-
lished data (23). Gronthos et al (12) showed dentin-pulp complex-like
tissue regeneration in subcutaneous implants of DPSCs mixed with
hydroxyapatite/tricalcium phosphate ceramic powder. Ever since, the
regeneration of dentin-like or pulp-like tissues has been elucidated
by many studies using subcutaneous implants of DPSCs seeded on
cell adhesive hydrogels (30, 31), synthetic scaffolds (13, 15, 32),
ceramic scaffolds, (33) or organic scaffolds (11, 34). However, one
of the main issues addressed was the absence of the typical
odontoblast morphology of the newly formed cells (23). In this study,
Figure 4. Six weeks postoperatively, the central canal space of the root implants showed degrading collagen scaffold (S) and proliferating progenitor/stem cells
lling the voids (arrow in A). New extracellular matrix had been occasionally deposited in a polar predentin-like pattern on the canal dentinal walls (d) by non-
polarized cuboidal cells (arrows in B) (hematoxylin-eosin stain, original magnications, A: 4 and B: 10).
Figure 3. Mason trichrome stain of a root implant 10 weeks postoperatively depicting (A) resorption lacunae with well-organized odontoclasts at the external root
surface (arrows in A) and (B) the invaginating epithelium (e) inside the root canal (original magnications, A: 4 and B: 4).
Basic ResearchBiology
916 Kodonas et al. JOE Volume 38, Number 7, July 2012
the expression pattern of DMP-1 and BSP-II (Figs. 6 and 7) indicated
that DPSCs retained odontogenic potential in vivo. The presence of
columnar polarized cells adjacent to the newly deposited organic
matrix of tubular predentin-like form along with the positive immuno-
staining for DMP-I and BSP-II strongly support the presence of
odontoblast-like cells in the bioengineered cell-dentin interface.
Representing the natural tooth-forming site, the mandibular or
maxillary jawbone has been previously used in dental tissue engineering
experiments (32, 35). In regenerative endodontics, using alternative
sites of implantation with the potential to improve understanding of
the role of the natural environment of odontogenesis to the
developmental prole of bioengineered structures by means of
vascularization and appropriate physical orientation is important
(32). This study showed that at the time of retrieval a number of implants
appeared to be in a process of eruption, whereas the external root
surfaces exhibited resorption lacunae with well-organized odontoclasts
(Fig. 3A). Unlike other studies, no periodontal-like tissue had been
observed at the bone-implant interface (35). Such a reaction seems
to be completely logical considering the sequence of events during
wound healing. Although root implants were considered autografts, in
some cases they exerted their antigenic effect by triggering a complex
and intricately regulated sequence of events of the host. This represented
an attempt of the host to wall off a site of persistent infection in the
socket by inducing epithelial cell proliferation. Consequently, in
a number of specimens, epithelial proliferation was seen along the
external root surfaces, and in some cases invaginating epithelium was
observed inside the root canal (Fig. 3B). These observations emphasize
the role of the local environment of the implantation site during exper-
imental procedures.
Considering the necessity of the vascular nutrient support of the
newly formed tissue, it becomes more than obvious that the implant
structure and design should support angiogenesis. Despite the fact
that angiogenic factors were not used, endothelial cell migration and
proliferation to the regenerated sites could be favored by the high vascu-
lature of cancellous bone and the blood clot organization after tooth
transplantation. In addition to that, it has been documented that the large
opening (>2 mm) of the root canal implant may also affect the nutrient
supply positively (25). Nevertheless, a histological examination revealed
the presence of necrotic tissue at the central area of some root implants.
This could be explained by the limited invasion of the scaffold structure
by the host vasculature, indicating an unfavorable host reaction. It
has been speculated that using a scaffold with an average pore size of
300 mm may favor mineralized tissue support, but smaller pore sizes
are considered essential to provide a matrix for angiogenesis (13).
The use of existing dentin surfaces has been reported before in
DSC-mediated experiments (15, 25). It has been sufciently shown
that dentin can induce the odontogenic differentiation of progenitor
cells by releasing embedded growth factors like transforming growth
factor-b1 and providing a favorable surface to which cells are
attached and immobilized (36). Consequently, extrinsic bioactive mole-
cules were not used in this study (37), whereas the use of sodiumhypo-
chlorite as a disinfectant and conditioning agent for the removal of
organic pulp residues did not seem to impair dentins molecular and
positional signals. On the contrary, it had been previously documented
that 3% sodium hypochlorite enhances the exposure of transforming
growth factor-b1 on dentin samples (38), whereas a 10-minute appli-
cation of 5.25% sodium hypochlorite induces clastic activity at the cell-
dentin interface (39).
A key component in tissue engineering is scaffold design (40).
Scaffolds serve as a template for cellular interactions, support angiogen-
esis, and provide a biomimetic structure that supports tissue regener-
ation after in vivo transplantation (41, 42). This study used organic
Figure 6. Immunohistochemical analyses of a root canal implant 10 weeks
postoperatively. DMP-I immunostaining was detected in the newly formed
matrix (arrows) and the associated odontoblast-like cell layer (arrowheads)
(original magnication, 25).
Figure 5. (A) Hematoxylin-eosin stain and (B) Mason trichrome stain of a root implant 10 weeks postoperatively showing that newly formed organic matrix had
been consistently deposited on the canal walls (white arrows) adjacent to a continuous layer of polarized cells showing typical columnar or spindle-shaped
morphology (black arrows) (original magnications, A: 40 and B: 25).
Basic ResearchBiology
JOE Volume 38, Number 7, July 2012 Direction of Isolated Swine Pulp Stem Cells to Form Dentin 917
and synthetic scaffolds to explore whether the difference in the nature or
design characteristics of the scaffold material affects DPSC-mediated
dentin regeneration. Type I collagen presents similar biological charac-
teristics with live tissues because it is one of the main components of the
dentin-pulp complex (43). It has been shown that it is a stable, biode-
gradable, and cytocompatible material that is suitable for being used as
a scaffold in stem cellbased regenerative endodontic procedures (34,
4447). PLGA scaffolds are widely used in dental tissue engineering
experiments and have been shown to provide an excellent
environment for cell attachment and angiogenesis (13, 14, 25).
Besides the fact that neither of the materials used in this study proved
to be more suitable to support S-DPSC differentiation, it is clearly
understood that the solvent/casting leaching technique used to
fabricate synthetic polymers is a reliable method that allows size,
shape, and porosity utilization to the specic characteristics of the
application area involved each time.
Regarding the scaffold biodegradation process, Sumita et al (47)
observed that the collagen sponge had completely degraded by 8 weeks
in vivo, and this study showed the presence of unresolved collagen scaf-
fold even after 10 weeks. In vitro studies have shown that 83% of the
total mass of ultrafoam collagen scaffolds (size 5 2 mm) can be
resolved in less than 4 weeks (48, 49). On the other hand, regarding
the use of synthetic scaffolds for tissue engineering of hybrid tooth-
bone constructs, Zhang et al (32) observed unresolved scaffold mate-
rial 20 weeks postoperatively, which is in accordance with our results at
all observation periods. Considering that scaffold degradation should
correlate with newly formed tissue deposition, choosing not only the
appropriate material but also the appropriate scaffold size becomes
essential.
Cryopreserved stem cellbased applications may lead to an
increased understanding of the underlying molecular mechanisms
involved in the tissue degeneration and regeneration processes. As evi-
denced by the present study and in accordance with many others, dental
pulp stem/progenitor cells can be readily established from the dental
pulp of developing swine teeth. Despite the fact that their unique pheno-
typic expression is dened by specic temporospatial epitheliomesen-
chymal interactions that are difcult to replicate during experimental
conditions, this study presents evidence of dense organized extracel-
lular matrix deposition by cells expressing appropriate tissue-
identifying protein markers. These results reect the dental pulp
progenitors lineage commitment as well as the role of the microenvi-
ronments underlying molecular mechanisms involved in the tissue
degeneration and regeneration processes.
Acknowledgments
The authors deny any conicts of interest related to this study.
References
1. Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of
current status and a call for action. J Endod 2007;33:37790.
2. Murray PE, Garcia-Godoy F. The outlook for implants and endodontics: a review of
the tissue engineering strategies to create replacement teeth for patients. Dent Clin
North Am 2006;50:299315.
3. Nor JE. Tooth regeneration in operative dentistry. Oper Dent 2006;31:63342.
4. Gage FH. Mammalian neural stem cells. Science 2000;287:14338.
5. Weissman IL. Translating stem and progenitor cell biology to the clinic: barriers and
opportunities. Science 2000;287:14426.
6. Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp
stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A 2000;97:1362530.
7. Miura M, Gronthos S, Zhao M, et al. SHED: stem cells from human exfoliated decid-
uous teeth. Proc Natl Acad Sci U S A 2003;100:580712.
8. Sonoyama W, Liu Y, Yamaza T, et al. Characterization of the apical papilla and its
residing stem cells from human immature permanent teeth: a pilot study.
J Endod 2008;34:16671.
9. Seo BM, Miura M, Sonoyama W, Coppe C, Stanyon R, Shi S. Recovery of stem cells
from cryopreserved periodontal ligament. J Dent Res 2005;84:90712.
10. Morsczeck C, Gotz W, Schierholz J, et al. Isolation of precursor cells (PCs) from
human dental follicle of wisdom teeth. Matrix Biol 2005;24:15565.
11. Prescott RS, Alsanea R, Fayad MI, et al. In vivo generation of dental pulp-like tissue
by using dental pulp stem cells, a collagen scaffold, and dentin matrix protein 1 after
subcutaneous transplantation in mice. J Endod 2008;34:4216.
12. Gronthos S, Brahim J, Li W, et al. Stem cell properties of human dental pulp stem
cells. J Dent Res 2002;81:5315.
13. El-Backly RM, Massoud AG, El-Badry AM, Sherif RA, Marei MK. Regeneration of
dentine/pulp-like tissue using a dental pulp stem cell/poly(lactic-co-glycolic) acid
scaffold construct in New Zealand white rabbits. Aust Endod J 2008;34:5267.
14. Young CS, Terada S, Vacanti JP, Honda M, Bartlett JD, Yelick PC. Tissue engineering
of complex tooth structures on biodegradable polymer scaffolds. J Dent Res 2002;
81:695700.
15. Cordeiro MM, Dong Z, Kaneko T, et al. Dental pulp tissue engineering with stem
cells from exfoliated deciduous teeth. J Endod 2008;34:9629.
16. Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for dening multipotent
mesenchymal stromal cells. The International Society for Cellular Therapy position
statement. Cytotherapy 2006;8:3157.
17. Lin HR, Kuo CJ, Yang CY, Shaw SY, Wu YJ. Preparation of macroporous biodegrad-
able PLGA scaffolds for cell attachment with the use of mixed salts as porogen addi-
tives. J Biomed Mater Res 2002;63:2719.
18. Oltramari PV, Navarro RL, Henriques JF, Capelozza AL, Granjeiro JM. Dental and
skeletal characterization of the BR-1 minipig. Vet J 2007;173:399407.
19. Weaver ME, Jump EB, McKean CF. The eruption pattern of deciduous teeth in mini-
ature swine. Anat Rec 1966;154:816.
20. Wobus AM. Potential of embryonic stem cells. Mol Aspects Med 2001;22:14964.
21. Wobus AM, Boheler KR. Embryonic stem cells: prospects for developmental biology
and cell therapy. Physiol Rev 2005;85:63578.
22. Iohara K, Zheng L, Ito M, Tomokiyo A, Matsushita K, Nakashima M. Side population
cells isolated from porcine dental pulp tissue with self-renewal and multipotency for
dentinogenesis, chondrogenesis, adipogenesis, and neurogenesis. Stem Cells 2006;
24:2493503.
23. Zhang W, Walboomers XF, Van Kuppevelt TH, et al. In vivo evaluation of human
dental pulp stem cells differentiated towards multiple lineages. J Tissue Eng
Regen Med 2008;2:11725.
24. Batouli S, Miura M, Brahim J, et al. Comparison of stem-cell-mediated osteogenesis
and dentinogenesis. J Dent Res 2003;82:97681.
25. Huang GT, Yamaza T, Shea LD, et al. Stem/progenitor cell-mediated de novo regen-
eration of dental pulp with newly deposited continuous layer of dentin in an in vivo
model. Tissue Eng Part A 2010;16:60515.
26. Iohara K, Imabayashi K, Ishizaka R, et al. Complete pulp regeneration after pulpec-
tomy by transplantation of CD105+ stem cells with stromal cell-derived factor-1.
Tissue Eng Part A 2011;17:191120.
27. Huang GT, Sonoyama W, Chen J, Park SH. In vitro characterization of human dental
pulp cells: various isolation methods and culturing environments. Cell Tissue Res
2006;324:22536.
28. Kemp KC, Hows J, Donaldson C. Bone marrow-derived mesenchymal stem cells.
Leuk Lymphoma 2005;46:153144.
29. Agata H, Kagami H, Watanabe N, Ueda M. Effect of ischemic culture conditions on the
survival and differentiation of porcine dental pulp-derived cells. Differentiation
2008;76:98193.
Figure 7. Ten weeks postoperatively, BSP-II was intensely expressed in the
newly formed organic matrix and differentiating cells of the root canal implant
(original magnication, 10).
Basic ResearchBiology
918 Kodonas et al. JOE Volume 38, Number 7, July 2012
30. Galler KM, Hartgering JD, Cavender AC, Schmalz G, DSouza RN. A customized self-
assembling peptide hydrogel for dental pulp tissue engineering. Tissue Eng Part A
2012;18:17684.
31. Galler KM, Cavender AC, Koeklue U, Suqqs LJ, Schmalz G, DSouza RN. Bioengi-
neering of dental stem cells in a Pegylated brin gel. Regen Med 2011;6:191200.
32. Zhang W, Abukawa H, Troulis MJ, Kaban LB, Vacanti JP, Yelick PC. Tissue engi-
neered hybrid tooth-bone constructs. Methods 2009;47:1228.
33. Takeda T, Tezuka Y, Horiuchi M, et al. Characterization of dental pulp stem cells of
human tooth germs. J Dent Res 2008;87:67681.
34. Zhang W, Walboomers XF, van Kuppevelt TH, Daamen WF, Bian Z, Jansen JA. The
performance of human dental pulp stem cells on different three-dimensional scaf-
fold materials. Biomaterials 2006;27:565868.
35. Marei MK, Saad MM, El-Ashwah AM, Ei-Backly RM, Al-Khodary MA. Experimental
formation of periodontal structure around titanium implants utilizing bone marrow
mesenchymal stem cells: a pilot study. J Oral Implantol 2009;35:10629.
36. Tziafas D, Kodonas K. Differentiation potential of dental papilla, dental pulp, and
apical papilla progenitor cells. J Endod 2010;36:7819.
37. Sloan AJ, Perry H, Matthews JB, Smith AJ. Transforming growth factor-beta isoform
expression in mature human healthy and carious molar teeth. Histochem J 2000;32:
24752.
38. Zhao S, Sloan AJ, Murray PE, Lumley PJ, Smith AJ. Ultrastructural localisation of
TGF-beta exposure in dentine by chemical treatment. Histochem J 2000;32:
48994.
39. Galler KM, DSouza RN, Federlin M, et al. Dentin conditioning codetermines cell fate
in regenerative endodontics. J Endod 2011;37:153641.
40. Graziano A, dAquino R, Cusella-De Angelis MG, et al. Scaffolds surface geometry
signicantly affects human stem cell bone tissue engineering. J Cell Physiol 2008;
214:16672.
41. Boneld W. Designing porous scaffolds for tissue engineering. Philos Transact A
Math Phys Eng Sci 2006;364:22732.
42. Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis.
Biomaterials 2005;26:547491.
43. Linde A. Dentin matrix proteins: composition and possible functions in calcication.
Anat Rec 1989;224:15466.
44. Carmichael DJ, Dick HM, Dodd CM. Histologic effects of antigenically altered
collagen as a heterograft for mammalian pulp exposures. Arch Oral Biol 1974;
19:11216.
45. Bimstein E, Shoshan S. Enhanced healing of tooth-pulp wounds in the dog by en-
riched collagen solution as a capping agent. Arch Oral Biol 1981;26:97101.
46. Pieper JS, Oosterhof A, Dijkstra PJ, Veerkamp JH, van Kuppevelt TH. Preparation and
characterization of porous crosslinked collagenous matrices containing bioavail-
able chondroitin sulphate. Biomaterials 1999;20:84758.
47. Sumita Y, Honda MJ, Ohara T, et al. Performance of collagen sponge as a 3-D scaf-
fold for tooth-tissue engineering. Biomaterials 2006;27:323848.
48. Meinel L, Karageorgiou V, Fajardo R, et al. Bone tissue engineering using human
mesenchymal stem cells: effects of scaffold material and medium ow. Ann Biomed
Eng 2004;32:11222.
49. Meinel L, Karageorgiou V, Hofmann S, et al. Engineering bone-like tissue in vitro
using human bone marrow stem cells and silk scaffolds. J Biomed Mater Res A
2004;71:2534.
Basic ResearchBiology
JOE Volume 38, Number 7, July 2012 Direction of Isolated Swine Pulp Stem Cells to Form Dentin 919
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Mms Protocol 2000Document2 pagesMms Protocol 2000bagus918No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Diabetes Mellitus Type 2 Schematic DiagramDocument1 pageDiabetes Mellitus Type 2 Schematic DiagramJhe Lyn82% (11)
- Mediastinum Sesat Ix-1Document23 pagesMediastinum Sesat Ix-1kelly christyNo ratings yet
- Watchtower: Jury Trial Day 5, Candace Conti v. WatchtowerDocument192 pagesWatchtower: Jury Trial Day 5, Candace Conti v. WatchtowersirjsslutNo ratings yet
- 1 s2.0 S009923991200516X MainDocument3 pages1 s2.0 S009923991200516X MainReeba Mary PrinceNo ratings yet
- 1 FP2 FPD Lecture 2011pdfDocument309 pages1 FP2 FPD Lecture 2011pdfReeba Mary PrinceNo ratings yet
- Restorative1 1 GudDocument44 pagesRestorative1 1 GudReeba Mary PrinceNo ratings yet
- Viva Questions 1Document15 pagesViva Questions 1Reeba Mary PrinceNo ratings yet
- 2012 Pall Care For Pancreas CancerDocument6 pages2012 Pall Care For Pancreas CancerFilip IonescuNo ratings yet
- How To Download Gordis Epidemiology E Book 6Th Edition Ebook PDF Ebook PDF Docx Kindle Full ChapterDocument36 pagesHow To Download Gordis Epidemiology E Book 6Th Edition Ebook PDF Ebook PDF Docx Kindle Full Chapterandrew.taylor131100% (34)
- Gynaecological History TakingDocument16 pagesGynaecological History TakingnelsonNo ratings yet
- GuidelineDocument213 pagesGuidelinedragutin7petri7No ratings yet
- B. NSG 120.2 ChecklistDocument78 pagesB. NSG 120.2 ChecklistAsh TrendzNo ratings yet
- Kontrak Belajar Gadar Igd BaruDocument14 pagesKontrak Belajar Gadar Igd BaruAstridNo ratings yet
- Effectiveness of Interventions To Improve Antidepressant Medication Adherence: A Systematic ReviewDocument22 pagesEffectiveness of Interventions To Improve Antidepressant Medication Adherence: A Systematic ReviewJaviera Rodríguez DelgadoNo ratings yet
- Toxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofDocument5 pagesToxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofFrancis AbuludeNo ratings yet
- SALTAPSDocument24 pagesSALTAPSFatima Tu ZahraNo ratings yet
- BCCH Diabetic Ketoacidosis Protocol Toolkit: Endocrinology & Diabetes UnitDocument16 pagesBCCH Diabetic Ketoacidosis Protocol Toolkit: Endocrinology & Diabetes UnitaseelNo ratings yet
- Log Sheet 2Document4 pagesLog Sheet 2SHAFIQNo ratings yet
- 6-Article Text-48-2-10-20200611Document4 pages6-Article Text-48-2-10-20200611anggimerlina52No ratings yet
- Balanced Diet: Bhavya Mds I Year Department of Conservative Dentistry & EndodonticsDocument76 pagesBalanced Diet: Bhavya Mds I Year Department of Conservative Dentistry & EndodonticsMayank AggarwalNo ratings yet
- Morbidity & Mortality (February, 2020)Document14 pagesMorbidity & Mortality (February, 2020)Wai GyiNo ratings yet
- Biology Investigatory Project On HypothyroidismDocument8 pagesBiology Investigatory Project On Hypothyroidismsagarparida6428No ratings yet
- J500210089 Muhammad Rizqy Noer Tuanaya Tugas Jurnal Bahasa Indonesia 2022Document14 pagesJ500210089 Muhammad Rizqy Noer Tuanaya Tugas Jurnal Bahasa Indonesia 2022kiki tuanaya1No ratings yet
- Dial YseDocument314 pagesDial YseSeda Muse KusNo ratings yet
- Acute TonsillitisDocument34 pagesAcute TonsillitisArvindhan100% (1)
- FF Japanese Gastric Cancer Treatment Guidelines 2018 (5th Edition) SpringerLinkDocument1 pageFF Japanese Gastric Cancer Treatment Guidelines 2018 (5th Edition) SpringerLinkFlaviu Ionuț FaurNo ratings yet
- Padlan Getigan and PartnersDocument4 pagesPadlan Getigan and PartnersMichaelandKaye DanaoNo ratings yet
- Virus ShapesDocument2 pagesVirus Shapessarath chandNo ratings yet
- CvadDocument11 pagesCvadNjideka A.No ratings yet
- Refractive Amblyopia: I Wayan Ardy Paribrajaka (1871122001)Document17 pagesRefractive Amblyopia: I Wayan Ardy Paribrajaka (1871122001)ratihpdewiNo ratings yet
- IV. Modul 10 - Pengelolaan NyeriDocument97 pagesIV. Modul 10 - Pengelolaan NyeriGrace Noviyanthi SinambelaNo ratings yet
- Blood Result Interpretation BookletDocument129 pagesBlood Result Interpretation BookletsithumNo ratings yet
- Bio Powerpoint 3Document10 pagesBio Powerpoint 3Romina SalazarNo ratings yet