Professional Documents
Culture Documents
Mortality in Typhoid Intestinal Perforation-A Declining Trend
Mortality in Typhoid Intestinal Perforation-A Declining Trend
Uploaded by
aura0090 ratings0% found this document useful (0 votes)
9 views3 pagesThis study analyzed 40 patients treated for typhoid intestinal perforation over one year. The average age was 35.75 years and most patients were male. Abdominal pain was the most common symptom. Surgical intervention and appropriate antibiotics were found to reduce mortality from typhoid intestinal perforation, with complications occurring in 42.5% of postoperative patients. The study concluded that early recognition, timely surgery and effective perioperative care can lower the mortality rate of typhoid intestinal perforation.
Original Description:
habgweiknfsa
Original Title
jcdr-7-1946
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis study analyzed 40 patients treated for typhoid intestinal perforation over one year. The average age was 35.75 years and most patients were male. Abdominal pain was the most common symptom. Surgical intervention and appropriate antibiotics were found to reduce mortality from typhoid intestinal perforation, with complications occurring in 42.5% of postoperative patients. The study concluded that early recognition, timely surgery and effective perioperative care can lower the mortality rate of typhoid intestinal perforation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
9 views3 pagesMortality in Typhoid Intestinal Perforation-A Declining Trend
Mortality in Typhoid Intestinal Perforation-A Declining Trend
Uploaded by
aura009This study analyzed 40 patients treated for typhoid intestinal perforation over one year. The average age was 35.75 years and most patients were male. Abdominal pain was the most common symptom. Surgical intervention and appropriate antibiotics were found to reduce mortality from typhoid intestinal perforation, with complications occurring in 42.5% of postoperative patients. The study concluded that early recognition, timely surgery and effective perioperative care can lower the mortality rate of typhoid intestinal perforation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 3
Journal of Clinical and Diagnostic Research.
2013 Sept, Vol-7(9): 1946-1948 1946 1946
DOI: 10.7860/JCDR/2013/6632.3366
Original Article
Mortality in Typhoid Intestinal
PerforationA Declining Trend
Key words: Typhoid fever, Intestinal perforation, Mortality
ABSTRACT
Background: Typhoid fever is an important public health
problem in developing countries. Intestinal perforation is one
of the leading fatal complications of typhoid fever. Typhoid
perforation occurs more commonly in terminal ileum. Morbidity
and Mortality associated with typhoid perforation are high
(9-22%). However this study aims to know whether there are
any changes of the same.
Aim: To analyse the clinical presentation, management,
complications, morbidity and mortality associated with typhoid
intestinal perforation and assess changing trends in mortality in
typhoid intestinal perforation.
Material & Methods: This is a retrospective observational study.
Cases regarding the study have been analyzed by reviewing the
patient records. It includes 40 patients who were diagnosed
with typhoid intestinal perforation, admitted and treated in the
Department of General Surgery from February 2011 to January
2012.
Results: A total of 40 patients were considered for the study
and their mean age was 35.75 years. 80% of patients were
male. Pain abdomen was their main symptom which lasted for
an average of 2.95 days. Leukocytosis (11,000 cells/cumm)
was present in 57.5% patients. Single perforation was present
in 31(77.5%) patients and primary closure was done in 30 of
them. Culture sensitivity showed E coli as the main organism.
Complications were seen in 42.5% of patients in postoperative
period.
Conclusion: Early recognition, timely surgical intervention with
appropriate surgery and antibiotics, and effective peri-operative
care reduces the mortality in typhoid intestinal perforation.
ANUPAMA PUJAR K.
1
, ASHOK A.C.
2
, RUDRESH H.K.
3
, SRIKANTAIAH H.C.
4
, GIRISH K.S
5
, SUHAS K.R.
6
INTRODUCTION
Typhoid fever is a febrile illness caused by Salmonella typhi, a
gram negative bacillus. This infection remains an important public
health problem in developing countries [1]. The most dreaded
complications are haemorrhage and intestinal perforation. Typhoid
fever is a predominant cause of nontraumatic intestinal perforation
in developing countries [2]. The high incidence of perforation in most
of the developing countries has been attributed to late diagnosis, the
emergence of multidrug resistant and virulent strains of Salmonella
Typhi [1]. Frequency of perforation varies between 0.8% and 18%
[3]. Perforation occurs in the terminal ileum secondary to necrosis
of Peyers patches about 23 weeks after the onset of disease.
Perforation of terminal ileum is a cause of obscure peritonitis
particularly in patients with severe toxic state, delaying diagnosis and
surgical intervention [2]. Despite decades of improvements made
in patient care, the morbidity and mortality of patients with typhoid
perforation remains high, and this is related to multiple factors
[4]. However, early surgical intervention is regarded as denitive
treatment along with preoperative resuscitation and postoperative
intensive care [3].
AIMS AND OBJECTIVES
To analyse the clinical presentation, operative ndings, surgical
procedures, postoperative complications, morbidity and mortality
associated with intestinal perforation due to typhoid fever in a
tertiary care center and to study changing trends in mortality in
typhoid intestinal perforation.
MATERIAL AND METHODS
This study included 40 patients, diagnosed with typhoid intestinal
perforation admitted and treated in the Department of General
Surgery from February 2011 to January 2012. Retrospectively
the cases were analyzed by reviewing the patient records after
approval from the ethical committee. The cases were evaluated
with regard to age, gender, clinical features, investigations, intra
operative ndings, type of surgery, morbidity and mortality. All
G
e
n
e
r
a
l
S
u
r
g
e
r
y
S
e
c
t
i
o
n
patients initially presented to the emergency department because
of acute abdomen. They were subjected to erect Xray abdomen,
chest Xray PA view, complete blood count, urine analysis, renal
function test, serum electrolytes, ultrasound abdomen. All patients
underwent surgery after preoperative resuscitation within 6 hours of
admission. All were given 3
rd
generation Cephalosporins (preferably
Ceftriaxone) with Metronidazole, with or without Amikacin.
STATISTICAL ANALYSIS
Descriptive statistics comprising of percentage (proportion) and
mean ( standard deviation) were used to describe the patient
characteristics and morbidity/mortality prole.
RESULTS
Out of the 40 patients, 32 (80%) were male. The youngest was 14
years old and oldest was 65 years with mean age of 35.75 years.
Twenty three (57.5%) patients presented with intestinal perforation
within seven days of onset of fever [Table/Fig-1]. The most
common presentation was pain abdomen seen in 38 patients
with mean duration of 2.95 days. Twenty one patients had history
of pain abdomen less than 2 days. Bowel disturbances were
present in seventeen (42.5%) patients, Out of whom 8 patients
had constipation, 7 patients had loose stools and 2 patients had
vomiting. Comorbidities were also present in two patients. One
patient had hypertension and another patient had diabetes. Eleven
patients were diagnosed to have typhoid fever and received
antibiotics prior to hospitalisation for perforation.
On examination 30 (75%) patients had diffuse peritonitis, eight
(20%) patients had localised peritonitis whereas 2 (5%) patients
had no peritonitis. Twenty three (57.5%) patients had leukocytosis
(>11000cells/cumm), and only one patient had leukocyte count
less than 4000cells/cumm. Neutrophils were more than 80% in
24 (60%) patients. A simple erect chest Xray demonstrated gas
under diaphragm in 34 (85%) patients. Remaining patients were
subjected to ultrasound/CT scan for diagnosis.
www.jcdr.net Anupama Pujar K. et al., Changing Trends in Typhoid Intestinal Perforation
Journal of Clinical and Diagnostic Research. 2013 Sept, Vol-7(9): 1946-1948 1947 1947
Key words: Typhoid fever, Intestinal perforation, Mortality
be because of the compromised nutritional status in patients who
had been ill for more than two weeks and perforate.
Typhoid intestinal perforation is seen during the second and third
decades of life [3,7]. In this series mean age was 35.75 years.In
a study by Atamanalp et al., [8], mean age was 36.3 years and in
a study by Sumer et al., [3] mean age was 37 years. It has been
found that being male is an independent risk factor for intestinal
perforation [9]. Khan et al., reported typhoid perforation more
common in males than females [10].
The most common symptoms are pain abdomen and fever [11].
In these series 38 patients presented with pain abdomen. Other
features are abdominal distension, constipation, vomiting and
loose stools. Guarding has been reported as the most common
physical nding [3].
In this study 85% patients had pneumoperitoneum demonstrated
on chest Xray and erect Xray abdomen. This is consistent with
study by Chalya et al., [1]. Leukopenia is the feature of typhoid
fever. In our series 57.5% had leucocytosis. 2.5% had leukopenia,
rest had normal total leukocyte count. A study by Santillana et al.,
leucocytosis was recorded in 59.5% of patients [12]. Leucocytosis in
typhoid fever suggests increased severity of typhoid perforation [9].
Widal test has been used in developing countries for diagnosing
typhoid fever but it has low sensitivity, specicity and positive
predictive value which changes with the geographical areas [13].
Typhidot is an immunochromatographic test which is easy and
rapid to perform and turn around time is one hour [14]. The gold
standard blood culture takes 2 to 4 days. In this study Widal was
positive in 32 patients (80%). In a study by Rahman et al., Widal
was positive in 75.90% of cases [15]. Typhidot was done in 15
patients and in seven patients it was positive. Five patients who
were widal negative showed typhidot positive.
Typhoid perforation mainly affects the terminal 40 cm of the ileum
in 72%78% of cases; the jejunum, caecum, colon and gallbladder
to lesser degree [16]. Rare case of appendicular perforation due
to typhoid has been reported in literature [17]. In this study 38
All the patients underwent midline laparotomy. Single perforation
of ileum was noted in 31(77.5%) patients, 5(12.5%) patients had
2 perforations and more than 2 perforations were present in
4(10%). Size of perforation varied from 0.5cm to 2cm. Location of
perforation was within 20cm from ileocaecal junction in 29(72.5%)
patients, 2040cm from ileocaecal junction in 9(22.5%) patients
and 2(5%) patients had perforation beyond 40cm from ileocaecal
junction. Peritoneal collection was purulent in 20(50%) patients,
feculent in 13(32.5%) patients and bile stained in 5(12.5%) patients.
Length of inamed bowel was less than 20cm from ileocaecal
junction in 31(77.5%) patients, 2040cm in 6(15%) patients and
3(7.5%) patients had bowel inammation more than 40cm from
ileocaecal junction.
The choice of surgical procedure was depended on patients general
condition, peritoneal contamination, inamed bowel, location and
number of perforation. Primary closure of perforation was done in
30(75%) patients out of 31 patients with single perforation. One
patient with single perforation had extensive bowel inammation
and feculent collection underwent resection anastomosis and
ileostomy. Eight patients who had 2 and more perforations
underwent resection and anastomosis with loop ileostomy. One
patient who had multiple perforations at ileocaecal junction
underwent right hemi colectomy and ileocolic anastomosis.
Postoperative recovery was uneventful in 23(57.5%) patients.
Seventeen (42.5%) patients had complications as shown in [Table/
Fig-2]. One patient underwent ultrasound guided aspiration for
intraabdominal collection. One patient developed enterocutaneous
stula which was managed conservatively. Three patients required
mechanical ventilation in postoperative period. Culture revealed
E coli as the main organism in 13 (32.5%) patients [Table/Fig-3],
Widal test was positive in 32 (80%) patients. Typhidot was done in
11 patients. It was positive in 7 patients.
Thirteen (32.5%) patients were discharged within 10 days. Twenty
ve (62.5%) patients were discharged between 10 to 30 days and
only 2 (5%) patients stayed in the hospital for more than a month.
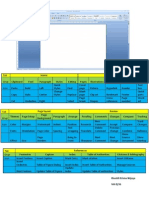
[Table/Fig-1]: Distribution of duration of fever
of patients studied. (Mean SD: 8.467.76)
Duration of fever (days) Number of
patients
%
Nil 4 10.0
<7 23 57.5
7-14 3 7.5
14-21 7 17.5
>21 3 7.5
Total 40 100.0
Sl No. Study [References] Year No of Patients Studied Number of Mortality (%)
1 Kouame et al., [29] 1995-1998 64 22 (34%)
2 Agbakwuru et al., [27] 1988-2001 105 17 (16.2%)
3 Ansari et al., [25] 2003-2008 44 6 (13.36)%
4 Saxe et al., [29] 2003 112 18 (16%)
5 Sumer et al., [3] 1994-2010 22 1 (4.5%)
6 Our study 2011-2012 40 nil
[Table/Fig-4]: Comparison of mortality in different studies
[Table/Fig-2]: Distribution of post-operative
complications in patients studied
Complications Number of
patients (n=40)
%
Nil 23 57.5
Present 17 42.5
Surgical site infections 9 22.5
Chest complication 6 15.0
Enterocutaneous stula 1 2.5
Intra-abdominal abscess 1 2.5
[Table/Fig-3]: Distribution of organisms
isolated on culture of peritoneal collection
C/S Number of patients %
1. E coli 13 32.5
2. Enterococcus 5 12.5
3. ESBL (E-coli) 1 2.5
4. Klebsiella 4 10.0
5. None 17 42.5
Total 40 100.0
[Table/Fig-5]: Decline in mortality in typhoid perforation
DISCUSSION
Typhoid perforation usually occurs in 2
nd
to 3
rd
week of fever [1,3].
However in developing countries cases are reported early within
the rst week of illness [5]. In this study duration of fever was less
than 7 days in 57.5% of cases. The reason observed behind this
though unproven could be because of low immunity, change in
the virulence of the bacteria, hypersensitivity of Peyers patches to
bacteria [1]. The patients who perforated during the rst two weeks
of the illness appear to have a better prognosis [6]. This may also
patients had perforation in terminal 40 cm of ileum. Only two
patients had perforation proximally, at mid ileal level. Pathological
changes are not just restricted to perforation sites. The diseased
gut is characterised by diffuse nonspecic enterocolitis with
hypertrophy, necrosis and ulceration of intestinal and mesenteric
lymphatic tissue. This is the reason for the gut in patients suffering
from typhoid fever, mainly terminal 60 cm to be oedematous and
friable [2]. In this study the diseased bowel was less than 20 cm in 31
(77.5%) patients. This may be because our patients had perforation
Anupama Pujar K. et al., Changing Trends in Typhoid Intestinal Perforation www.jcdr.net
Journal of Clinical and Diagnostic Research. 2013 Sept, Vol-7(9): 1946-1948 1948 1948
in early course of disease. Once perforation occurs peritoneal
contamination depends on duration of perforation and number of
perforations. In this study majority (77.5%) had single perforation. It
has been reported that multiple perforations have signicantly high
mortality compared to those with single perforation [1].
Early surgery is the optimal treatment in typhoid perforations
despite appropriate antibiotics. It ceases the source of further
faecal contamination of peritoneal cavity [18]. In this study surgical
intervention was done within 6 hours of admission. Several surgical
procedures have been described in the form of simple closure,
wedge excision with simple closure of perforation, bowel resection
and anastomosis with or without ileostomy. Laparoscopic perforation
closure has been reported by Ramachandran et al., [19] and Sinha et
al., [20]. In this study primary closure was done in 75% patients. 25%
had an extensive procedure. Beniwal et al., [21] suggested primary
closure is the choice of treatment. Shah et al., founded resection
anastomosis and copious peritoneal lavage is the best surgical option
[22]. Malik et al., showed primary ileostomy to be the successful
procedure [18]. Husain et al., suggested closure of ileal perforation
with omental patch technique prevents the leak [23].
The main organism grown in peritoneal uid culture was E coli 13
(32.5%) patients. This is consistent with the study by Sitaram et al.,
[24]. Most common complication in this study was surgical site infection
which is similar to a study by Ansari et al., [25]. Enterocutaneous stula
was found in 1 (2.5%) patient similar to study by Sumer et al., [3]. This
was managed conservatively. Fistula closed spontaneously. In a study
by Ansari et al., stula was found in 13.4% patients [25] Major cause of
postoperative morbidity in perforation peritonitis according to Jhobta
et al., is respiratory complication [26]. In this study 6 patients (15%)
developed respiratory complication and 3 patients needed mechanical
ventilation in the postoperative period.
In developing countries mortality rates from typhoid perforation have
been reported to range from 922%[1].There was no mortality in our
series as compared to other studies [Table/Fig-4 and 5]. Agbakwuru
et al., who reported mortality rate of 16.2% [27] where in the patients
were operated 24 to 48 hours after diagnosis. Ansari et al., reported
mortality of 13.36% [25] where the patient presented with mean
duration of pain abdomen of 5.6 days. In their study 4 out of 6 deaths
were due to development of faecal stula. In our series, most of our
patients (57.5%) presented within the rst week of fever and the mean
duration of pain abdomen was 2.95 days. Koume et al., reported
high mortality due to complications related to ileostomy [28]. Saxe
et al., attributes mortality in his study to persistent sepsis which he
says could have been prevented by using broad spectrum antibiotics
[29]. There was no mortality in our study probably due to early and
appropriate surgical intervention, effective pre and peri-operative
resuscitation, post-operative intensive care procedures, good
ileostomy care and delivery of broad spectrum antibiotics. Sumer et
al., reported low mortality attributed to similar reasons [3].
CONCLUSION
Typhoid intestinal perforation is a major surgical health problem
in tropical countries particularly in those where, standard of living
is low which leads to unhygienic environment. Early recognition,
timely surgical intervention, appropriate antibiotics and surgical
technique and perioperative care play key role in reducing mortality
in typhoid intestinal perforation. However, this is a retrospective
observational study. This has all the limitations of retrospective
study, to come to any opinion. This warrants a prospective study
to come to a denitive conclusion.
REFERENCES
[1] Chalya LP, Mabula BJ, et al. Typhoid intestinal perforations at a university
teaching hospital in northwestern Tanzania: A surgical experience of 104 cases
in a resource-limited setting. World journal of emergency surgery. 2012;7:4.
[2] Wani AR, Parray QF, et al. Nontraumatic terminal ileal perforation. World journal
of emergency surgery. 2006 Mar;1:7.
[3] Sumer A, Kemik O, et al. Outcome of surgical treatment of intestinal perforation
in Typhoid Fever. World journal of Gastroenterol. 2010 Sept; 16(33):4164-68.
[4] Edino TS, Yakubu AA, et al. Prognostic Factors in Typhoid ilealperforation:A
Prospective Study of 53 Cases. Journal of the national medical association.
2007 Sept. 9;99:1042-45.
[5] Uba AF, Chirdan LB, et al. Typhoid intestinal perforation in children:A continuing
scourge in a developing country. PediatrSurgInt. 2007;23:33-39.
[6] Adesunkanmi AR, Ajao OG. Prognostic factors in typhoid ilealperforation:A
prospective study in 50 patients. J R CollSurg Edinb.1997Dec;42(6):395-99
[7] Eggleston FC, Santoshi B, et al. Typhoid Perforation of the Bowel. Ann surg.
1979 July;190(1):31-35.
[8] Atamanalp SS, Aydinli B, et al. Typhoid intestinal perforations:twenty-six year
experience. World J Surg. 2007 Sept;31(9):1883-88.
[9] Hosoglu S, Aldemir M, Akalin S, et al. Risk Factors for Enteric Perforation in
Patients with Typhoid Fever. 2004;160(1): 46-50.
[10] Khan M, Coovadia YM, et al. Inuence of gender on clinical features, laboratory
ndings,and complications of typhoid fever. Am J Trop Med Hyg. 1999; 61(1): 41-46.
[11] Ugwu BT, Yiltok SJ, et al. Typhoid intestinal perforation in North Central Nigeria.
West Afr J Med. 2005;24(1);1-6
[12] Santillana M. Surgical complications of typhoid fever: enteric perforation. World
J of Surg. 1991;15:170-75.
[13] Sherwal BL, Dhamija RK, et al. A Comparative Study of Typhidot and WidalTest
in Patients of Typhoid fever. JIACM. 2004;5 (3):244-46.
[14] Jesudason MV, Sivakumar S. Prospective evaluation of rapid diagnostic test
Typhidot for typhoid fever. Indian J Med Res. 123. 2000 April: 513-16.
[15] Rahman AU, Nawz M. The choice of surgical procedure in typhoid ileal-
perforation. JPMI. 2011;14(2):46-51.
[16] Ukwenya AY, Ahmed A, et al. Progress in management of typhoid perforation.
Annals of African Medicine. 2011;10(4):259-65.
[17] Golakai VK, Makunike R. Perforation of terminal ileum and appendix in typhoid
enteritis:Report of two cases. East Afr Med J. 1997Dec;74(12):796-99.
[18] Malik MA, Laghari AA, Mallah Q. Different Surgical Options and Ileostomy in
Typhoid Perforation. World Journal of Medical Sciences. 2006;1(2):112-16.
[19] Ramachandran CS, Agarwal S, et al. Laparoscopic surgical management
of perforation peritonitis in enteric fever: A preliminary study. Surg Laparosc
Endosc Percutan Tech. 2004 June; 14(3):122-24.
[20] Sinha R, Sharma N, Joshi M. Laparoscopic repair of small bowel perforation.
JSLS. 2005;9(4):399-402.
[21] Beniwal US, Jindal P, Sharma J, et al. Comparative study of operative procedures
in typhoid perforation. Indian J Surg. 2003;65(2):172-77
[22] Shah AA, Wani KA, Wazir BS. The ideal treatment of typhoid enteric perforation
resection anastomosis. Int Surg. 1999;84(1):35-38
[23] Husain M, Khan RN, Rehmani B, Haris H. Omental Patch Technique for the ileal
Perforation secondary to Typhoid Fever. The Saudi Journal of Gastroenterology.
2011 May;17(3):208-11.
[24] Sitaram V, Fenn AS, Moses BV, Khanduri P. TyphoidIleal perforations: a retrospective
study. Annals of the Royal College of Surgeons of England. 1990; 72(6), 347-49.
[25] Ansari AG, et al. Management of typhoid ileal perforations: a surgical experience of
44cases. Gomal Journal of Medical Sciences. 2009 January-June; 7(1):27-30.
[26] Jhobta RS, Attri AK, Kaushik R, et al. Spectrum of perforation peritonitis in India-review
of 504 consecutive cases. World Journal of Emergency Surgery. 2006. Sept;1:26.
[27] Agbakwuru EA, et al. A review of typhoid perforation in rural African hospital.
WAJM. 2003. Jan-March.22(1):22-25
[28] Kouame J, et al. Typhoid ileal perforation surgical experience of 64 cases.
Actachir belg. 2004.104:445-47
[29] Saxe JM, Cropsey R. Is operative management effective in treatment of
perforated typhoid. The American Journal of Surgery. 2005.189:342-44.
PARTICULARS OF CONTRIBUTORS:
1. Assistant Professor, M.S. Ramaiah Medical College, Bangalore, India.
2. Professor, M.S. Ramaiah Medical College, Bangalore, India.
3. Professor, M.S. Ramaiah Medical College, Bangalore, India.
4. Associate Professor, Department of Surgery, M.S. Ramaiah Medical College, Bangalore, India.
5. Assistant Professor, M.S. Ramaiah Medical College, Bangalore, India.
6. Postgraduate Student, M.S. Ramaiah Medical College, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Anupama Pujar K.,
No 1165, 5
th
main, 4
th
block, Hbr Layout, Bangalore560043, India.
Phone: 9740190687, E-mail: anupamapujar@rediffmail.com
FINANCIAL OR OTHER COMPETING INTERESTS: None.
Date of Submission: Jun 04, 2013
Date of Peer Review: Jun 19, 2013
Date of Acceptance: Jul 28, 2013
Date of Publishing: Sept 10, 2013
You might also like
- Conservative Management of Perforated Peptic UlcerDocument4 pagesConservative Management of Perforated Peptic UlcerAfiani JannahNo ratings yet
- GJMS Vol-7-1 PDFDocument4 pagesGJMS Vol-7-1 PDFgraceflowerNo ratings yet
- Abdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduDocument4 pagesAbdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduSavitri Maharani BudimanNo ratings yet
- Typhoid Perforation NepalDocument3 pagesTyphoid Perforation NepalMagdalena PranataNo ratings yet
- Spectrum of Perforation Peritonitis in Delhi: 77 Cases ExperienceDocument5 pagesSpectrum of Perforation Peritonitis in Delhi: 77 Cases ExperienceAhmad Rahmat Ramadhan TantuNo ratings yet
- Article 370Document5 pagesArticle 370Luis Alfredo LucioNo ratings yet
- A Clinical Study On Extrapulmonary TuberculosiDocument10 pagesA Clinical Study On Extrapulmonary TuberculosinayemamasruraNo ratings yet
- Or3 PDFDocument5 pagesOr3 PDFAkshay PatilNo ratings yet
- Clinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceDocument5 pagesClinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceSarah DaniswaraNo ratings yet
- Acute Cholecystitis: From ER To Surgery: Riginal RticleDocument5 pagesAcute Cholecystitis: From ER To Surgery: Riginal RticleKrystel Joy AuroNo ratings yet
- Intestinal Tuberculosis: A Diagnostic Challenge: © 2017 John Wiley & Sons LTDDocument6 pagesIntestinal Tuberculosis: A Diagnostic Challenge: © 2017 John Wiley & Sons LTDLily SmithNo ratings yet
- Modern Management of Pyogenic Hepatic Abscess: A Case Series and Review of The LiteratureDocument8 pagesModern Management of Pyogenic Hepatic Abscess: A Case Series and Review of The LiteratureAstari Pratiwi NuhrintamaNo ratings yet
- Iarjmsr 1 (3) 100-105Document7 pagesIarjmsr 1 (3) 100-105jinuNo ratings yet
- Serosal Appendicitis: Incidence, Causes and Clinical SignificanceDocument3 pagesSerosal Appendicitis: Incidence, Causes and Clinical SignificancenaufalrosarNo ratings yet
- Pattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?Document4 pagesPattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?neildamiNo ratings yet
- Etiological Pattern and Outcome of Non-Variceal Upper G.I. BleedingDocument5 pagesEtiological Pattern and Outcome of Non-Variceal Upper G.I. BleedingJawad ZafarNo ratings yet
- Prise en Charge Therapeutique Des Abces Du Foie A Propos de 40 Cas Au Service de Medecine Interne de Lhopital Cheikh ZayedDocument19 pagesPrise en Charge Therapeutique Des Abces Du Foie A Propos de 40 Cas Au Service de Medecine Interne de Lhopital Cheikh ZayedIJAR JOURNALNo ratings yet
- Challenges and Outcome of Wilms' Tumour Management in A Resource-Constrained SettingDocument3 pagesChallenges and Outcome of Wilms' Tumour Management in A Resource-Constrained Settingcallisto3487No ratings yet
- Peritonsillar Abscess: Pattern and Treatment Intervention in A Tertiary Health Institution in Sokoto MetropolisDocument4 pagesPeritonsillar Abscess: Pattern and Treatment Intervention in A Tertiary Health Institution in Sokoto Metropolismuhammad hasan fuadyNo ratings yet
- Adeno CaDocument4 pagesAdeno CaPutri Wulan SukmawatiNo ratings yet
- 1 s2.0 S1743919113000307 Main PDFDocument5 pages1 s2.0 S1743919113000307 Main PDFkunkkonkNo ratings yet
- Risk Factor TaiwanDocument5 pagesRisk Factor TaiwanMira ApriliaNo ratings yet
- Annsurg00166 0011Document8 pagesAnnsurg00166 0011Muhammad FadillahNo ratings yet
- Original Article: Clinical Study of Perforations of Small BowelDocument7 pagesOriginal Article: Clinical Study of Perforations of Small BowelGarry WidjajaNo ratings yet
- 4 Murali Et AlDocument4 pages4 Murali Et AleditorijmrhsNo ratings yet
- Clinical Presentation of Abdominal TuberculosisDocument4 pagesClinical Presentation of Abdominal TuberculosisRizky AmaliahNo ratings yet
- PimpaleDocument6 pagesPimpaleMariano BritoNo ratings yet
- 1749-7922-6-37 - SalinDocument5 pages1749-7922-6-37 - SalinAnonymous InJS6aYZNo ratings yet
- Etiology, Treatment Outcome and Prognostic Factors Among Patients With Secondary Peritonitis at Bugando Medical Centre, Mwanza, TanzaniaDocument13 pagesEtiology, Treatment Outcome and Prognostic Factors Among Patients With Secondary Peritonitis at Bugando Medical Centre, Mwanza, Tanzaniayossy aciNo ratings yet
- Jurnal Ebn PerikarditisDocument13 pagesJurnal Ebn Perikarditistino prima dito100% (1)
- Ijms V3i5p101Document12 pagesIjms V3i5p101Oscar HustorioNo ratings yet
- Hiller 2015Document7 pagesHiller 2015Muhamad Ilhamsyah DandungNo ratings yet
- Cholelithiasis: Causative Factors, Clinical Manifestations and ManagementDocument6 pagesCholelithiasis: Causative Factors, Clinical Manifestations and ManagementmusdalifahNo ratings yet
- Nadhimyounis 2014Document4 pagesNadhimyounis 2014Gabriella Kezia LiongNo ratings yet
- A Clinical Study of Tuberculous Cervical LymphadenDocument5 pagesA Clinical Study of Tuberculous Cervical LymphadenAgung DewanggaNo ratings yet
- C01110916 PDFDocument8 pagesC01110916 PDFLestari Chye PouedanNo ratings yet
- A Clinicohaematological Profile of Splenomegaly: Varsha S. Dabadghao, Arundhati G.Diwan, Amol M. RaskarDocument9 pagesA Clinicohaematological Profile of Splenomegaly: Varsha S. Dabadghao, Arundhati G.Diwan, Amol M. RaskarLianSiahaanNo ratings yet
- Gallbladder Perforation: Experience of 35 Cases at A Tertiary Care HospitalDocument6 pagesGallbladder Perforation: Experience of 35 Cases at A Tertiary Care HospitalIJAR JOURNALNo ratings yet
- Stevens JohsonDocument8 pagesStevens JohsonDaily RomeroNo ratings yet
- Development of Type I Gastric Carcinoid in Patients With Chronic Atrophic GastritisDocument9 pagesDevelopment of Type I Gastric Carcinoid in Patients With Chronic Atrophic GastritisAbristaSeptikasariNo ratings yet
- Clinical, Imaging, and Endoscopic Profile of Patients With Abdominal TuberculosisDocument6 pagesClinical, Imaging, and Endoscopic Profile of Patients With Abdominal TuberculosisINDRINo ratings yet
- Abdominal Tuberculosis: A Diagnostic Dilemma - PMCDocument9 pagesAbdominal Tuberculosis: A Diagnostic Dilemma - PMCDiptanshu ShekharNo ratings yet
- Bedah Digestif - Jurnal LaparotomiDocument9 pagesBedah Digestif - Jurnal LaparotomiDenny EmiliusNo ratings yet
- A Retrospective Analysis of Complications of Pelvic Exenteration - A Single Institution Experience of 6 YearsDocument6 pagesA Retrospective Analysis of Complications of Pelvic Exenteration - A Single Institution Experience of 6 YearsPremier PublishersNo ratings yet
- A Prospective Study of Predictors For Post Laparotomy Abdominal Wound DehiscenceDocument4 pagesA Prospective Study of Predictors For Post Laparotomy Abdominal Wound DehiscencemelisaberlianNo ratings yet
- Pattern of ThyroidDocument6 pagesPattern of ThyroidUmaieyaal AnnarajahNo ratings yet
- Surgical Interventions in Abdominal Tuberculosis: A Clinico-Pathological StudyDocument5 pagesSurgical Interventions in Abdominal Tuberculosis: A Clinico-Pathological StudySatwinder KaurNo ratings yet
- Absceso Hepatico PiogenoDocument6 pagesAbsceso Hepatico PiogenoPablo Eduardo AmadorNo ratings yet
- Impact of Postoperative Morbidity On Long-Term Survival After OesophagectomyDocument10 pagesImpact of Postoperative Morbidity On Long-Term Survival After OesophagectomyPutri PadmosuwarnoNo ratings yet
- Research Article Challenges Encountered During The Treatment of Acute Mesenteric IschemiaDocument9 pagesResearch Article Challenges Encountered During The Treatment of Acute Mesenteric IschemiaDyah RendyNo ratings yet
- WJH 3 130bacteremiaDocument7 pagesWJH 3 130bacteremiaLasiaf AlaskaNo ratings yet
- Types Sites and Causes of Mechanical Intestinal ObDocument5 pagesTypes Sites and Causes of Mechanical Intestinal ObPutra FebdianNo ratings yet
- Journal of Clinical and Translational Endocrinology: Case ReportsDocument5 pagesJournal of Clinical and Translational Endocrinology: Case ReportsKartikaa YantiiNo ratings yet
- Artikel TreatmentDocument8 pagesArtikel TreatmentFaiz MubarokNo ratings yet
- Abcesele FicatuluiDocument4 pagesAbcesele FicatuluiMihaela AlinaNo ratings yet
- Uses of ERCP in The Management of Post-Cholecystectomy ComplicationsDocument6 pagesUses of ERCP in The Management of Post-Cholecystectomy ComplicationsAliA.RamadhanNo ratings yet
- Study of Etiology LALAJUNDocument3 pagesStudy of Etiology LALAJUNDavid Al HavizNo ratings yet
- 2014 Article 639Document8 pages2014 Article 639Anida HasnaNo ratings yet
- CHSJ 2011.2.04Document4 pagesCHSJ 2011.2.04Billy PeterNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Pristian Class X-4 22Document1 pagePristian Class X-4 22aura009No ratings yet
- Tab Grup Clipboard Icon: Rivaldi Krisna Wijaya VIII E/35Document1 pageTab Grup Clipboard Icon: Rivaldi Krisna Wijaya VIII E/35aura009No ratings yet
- Tugas ArtikelDocument4 pagesTugas Artikelaura009No ratings yet
- Questions:: V (4i + (2t + 2 1/3) J) M SDocument2 pagesQuestions:: V (4i + (2t + 2 1/3) J) M Saura009No ratings yet
- A Study of Typhoid Fever in Five Asian Countries: Disease Burden and Implications For ControlsDocument9 pagesA Study of Typhoid Fever in Five Asian Countries: Disease Burden and Implications For Controlsaura009No ratings yet