Professional Documents
Culture Documents
Team 1 Morpot - 13 Juni 2014 (B)
Team 1 Morpot - 13 Juni 2014 (B)
Uploaded by
Armando Halauwet0 ratings0% found this document useful (0 votes)
12 views2 pagesMrs. Rissa, a 24-year-old woman, presented to the emergency department with diarrhea, nausea, vomiting, decreased appetite, and abdominal pain since that morning. On examination, she appeared sickly but was alert and oriented with stable vital signs. Her abdominal exam was notable for tenderness in the umbilicus. Laboratory tests revealed no abnormalities aside from findings consistent with gastroenteritis. She was admitted and prescribed IV and oral medications to treat her symptoms and prevent dehydration, with a soft diet and IV fluids planned. Her condition was assessed as gastroenteritis.
Original Description:
morport
Original Title
Team 1 Morpot - 13 Juni 2014 (b)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMrs. Rissa, a 24-year-old woman, presented to the emergency department with diarrhea, nausea, vomiting, decreased appetite, and abdominal pain since that morning. On examination, she appeared sickly but was alert and oriented with stable vital signs. Her abdominal exam was notable for tenderness in the umbilicus. Laboratory tests revealed no abnormalities aside from findings consistent with gastroenteritis. She was admitted and prescribed IV and oral medications to treat her symptoms and prevent dehydration, with a soft diet and IV fluids planned. Her condition was assessed as gastroenteritis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
12 views2 pagesTeam 1 Morpot - 13 Juni 2014 (B)
Team 1 Morpot - 13 Juni 2014 (B)
Uploaded by
Armando HalauwetMrs. Rissa, a 24-year-old woman, presented to the emergency department with diarrhea, nausea, vomiting, decreased appetite, and abdominal pain since that morning. On examination, she appeared sickly but was alert and oriented with stable vital signs. Her abdominal exam was notable for tenderness in the umbilicus. Laboratory tests revealed no abnormalities aside from findings consistent with gastroenteritis. She was admitted and prescribed IV and oral medications to treat her symptoms and prevent dehydration, with a soft diet and IV fluids planned. Her condition was assessed as gastroenteritis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
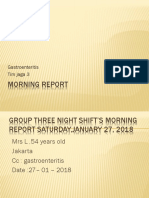
Mrs.
Rissa, 24 years old
UGD RS UKI Cawang
CC : diarrhea Thursday , June 13
th
2014, 18.30 PM
Findings Assesment Therapy Planning
Diarrhea since this morning before admission.
Nausea (+), vomited 4 times a day.
Decreased appetite.
umbilicus pain (+).
Hypertension (-).
Diabetes mellitus (-).
PHYSICAL EXAMINATION
Appearance : being sick
GCS : E4V5M6
Awareness: Composmentis, BP : 110/70 mmHg, HR : 88x/min,
RR : 25x/min, T : 36,7C
Head: Normocephaly
Eye : pale conjunctiva -/-, icteric sclera -/-
THT : normal
Mouth : normal
Neck : lymph nodes not enlarge, JVP : 5-2 cmH2O
Thorax
Ins : symmetric
Pal : vocal fremitus sound symmetric
Per : sonor right = left
Aus : basic sound of breath vesicular, wheezing (-/-), ronchi (-/-)
Heart : Heart sound I & II regular, murmur (-), gallop (-)
Abdominal
Ins : flat
Aus : bowel sound 6x/min
Per : timpani, percution pain (-)
Pal : supel, tenderness in the umbilicus (+)
Extremities
warm acral, CRT < 2 s, edema -/-
LAB FINDING
Gastroenteritis
Pro Hospitalized
Diet : soft diet unstimulate
IVFD : II RL / 24 hour
Mm/
Omeprazole 2x40 mg
(IV)
Ondancetron 2x4 mg
(IV)
Ranitidine
domperidon
Check H2TL &
complete urine in
the room
-H2TL:
Hemoglobin : 11,1 g/dl
Haematocrite : 31,5 %
Leucocyte: 6.400 /ul
Thrombocyte : 129 .000 /ul
- Casual Plasma Glucose: 78 mg/dl
-ELECTROLYTE
Natrium : 145 mmol/L
Kalium : 3,8 mmol/L
Clorida : 105 mmol/L
You might also like
- Team 1 Morpot - 05 Juni 2014Document2 pagesTeam 1 Morpot - 05 Juni 2014Armando HalauwetNo ratings yet
- Mrs. Amelia Manurung, 42years Ugd Rs Uki Cawang CC: Abdominal Pain Monday, July 07 2014, 17:45:01PMDocument2 pagesMrs. Amelia Manurung, 42years Ugd Rs Uki Cawang CC: Abdominal Pain Monday, July 07 2014, 17:45:01PMFerjiRNo ratings yet
- Findings Assesment Therapy Planning: Abdominal PainDocument2 pagesFindings Assesment Therapy Planning: Abdominal PainAgustina Anggraeni PurnomoNo ratings yet
- Morport 8 Juni 2014Document5 pagesMorport 8 Juni 2014Agustina Anggraeni PurnomoNo ratings yet
- Morport 12 Juni 2014Document12 pagesMorport 12 Juni 2014Agustina Anggraeni PurnomoNo ratings yet
- "Morning Report": Christian University of IndonesiaDocument12 pages"Morning Report": Christian University of IndonesialettasamudraNo ratings yet
- "Morning Report": Department of Internal MedicineDocument12 pages"Morning Report": Department of Internal MedicineAdli NurfakhriNo ratings yet
- Morpot 29 JuliDocument2 pagesMorpot 29 JuliAdli NurfakhriNo ratings yet
- Morning Report: Department of Internal MedicineDocument19 pagesMorning Report: Department of Internal MedicinedwityanoviariNo ratings yet
- Morning Report: Gastroenteritis Tim Jaga 3Document31 pagesMorning Report: Gastroenteritis Tim Jaga 3Bintang TrianaNo ratings yet
- Morning Report: Departement of Surgery February 15rd 2017Document17 pagesMorning Report: Departement of Surgery February 15rd 2017Deasy Arindi PutriNo ratings yet
- Case ReportDocument38 pagesCase ReportDiLa NandaRiNo ratings yet
- Morpot 13092014Document15 pagesMorpot 13092014Lodewyk Kefas JoshoaNo ratings yet
- SUPERVISOR: Dr. Johannes Saing, M.Ked (Ped), Sp.A (K) : Presented By: Saravana Selvi Sanmugam (110100426)Document46 pagesSUPERVISOR: Dr. Johannes Saing, M.Ked (Ped), Sp.A (K) : Presented By: Saravana Selvi Sanmugam (110100426)Saravana Selvi SanmugamNo ratings yet
- Morning Report: Department of Internal MedicineDocument12 pagesMorning Report: Department of Internal MedicineandrirombeNo ratings yet
- Morpot 31 Agustus 2015 Kelompok 1Document11 pagesMorpot 31 Agustus 2015 Kelompok 1Kharisma PertiwiNo ratings yet
- Bab 3Document17 pagesBab 3Saravana Selvi SanmugamNo ratings yet
- Findings Assessment Therapy PlanningDocument23 pagesFindings Assessment Therapy PlanningAdeliaNo ratings yet
- Final CaseDocument45 pagesFinal Case_carido_No ratings yet
- Morning Report: Name: DM Albert, DM Vira, DM Elvin Konsulen: Dr. Alders, Sp. BDocument18 pagesMorning Report: Name: DM Albert, DM Vira, DM Elvin Konsulen: Dr. Alders, Sp. BElvin DergongNo ratings yet
- Morport Kel 1 - A PrintDocument12 pagesMorport Kel 1 - A PrintAdhityaWPutraNo ratings yet
- Physical Examination Generalised StatusDocument10 pagesPhysical Examination Generalised StatusregarskidNo ratings yet
- Nurul Hayati DR AgungDocument17 pagesNurul Hayati DR AgungAgung Pratama YudhaNo ratings yet
- Morport Team 4 (11 Januari 2016)Document11 pagesMorport Team 4 (11 Januari 2016)Mikha Tiar Ida HutabaratNo ratings yet
- ConsultsDocument16 pagesConsultsRaq KhoNo ratings yet
- Morning Report: Department of Internal MedicineDocument11 pagesMorning Report: Department of Internal MedicineAyunita PermataNo ratings yet
- Morning Report: Monday, 2 Sept 2013 Physician in ChargeDocument22 pagesMorning Report: Monday, 2 Sept 2013 Physician in ChargeAchmad ZainudinNo ratings yet
- Morning Report: Department of Internal MedicineDocument11 pagesMorning Report: Department of Internal MedicineAyunita PermataNo ratings yet
- Morning Report June 10, 2017 Dept of Internal Medicine G26Document21 pagesMorning Report June 10, 2017 Dept of Internal Medicine G26Deasy Arindi PutriNo ratings yet
- Morning Report GEA-15DesDocument12 pagesMorning Report GEA-15DeszakyalfathuNo ratings yet
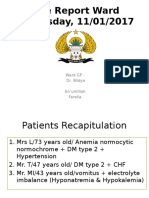
- Case Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaDocument39 pagesCase Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaFarella KartikaNo ratings yet
- Mrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningDocument2 pagesMrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningAgustina Anggraeni PurnomoNo ratings yet
- Aki Et Causa Gastroenteritis Acute and DM Type 2Document26 pagesAki Et Causa Gastroenteritis Acute and DM Type 2Vitya ResanindyaNo ratings yet
- Night Report 1 MarchDocument34 pagesNight Report 1 MarchRatu Qurroh AinNo ratings yet
- Morning Report: DM Yunri DM CenDocument19 pagesMorning Report: DM Yunri DM CenYunriNo ratings yet
- Morpot InternaDocument14 pagesMorpot InternaZega AgustianNo ratings yet
- Morning Report: Dinas Jaga 23/09/2019 DM Aldo, DM Agustina, DM RobyDocument23 pagesMorning Report: Dinas Jaga 23/09/2019 DM Aldo, DM Agustina, DM RobyRoby Aditya SuryaNo ratings yet
- Findings Assesment Therapy Planning Clinical FindingDocument1 pageFindings Assesment Therapy Planning Clinical FindingAdli NurfakhriNo ratings yet
- Morning Report: Department of Internal MedicineDocument12 pagesMorning Report: Department of Internal MedicineNurcahyo Tri UtomoNo ratings yet
- Team 1 Morpot 24 Mei 2014Document13 pagesTeam 1 Morpot 24 Mei 2014FerjiRNo ratings yet
- Morning Report: Department of Internal MedicineDocument13 pagesMorning Report: Department of Internal MedicineMariaEllyNobetaHutabaratNo ratings yet
- Morpot 11 Agustus 2015 Kelompok 1Document11 pagesMorpot 11 Agustus 2015 Kelompok 1Novita Sari DewiNo ratings yet
- MR 5 Noppppp 2015Document32 pagesMR 5 Noppppp 2015Wahyu PratamaNo ratings yet
- Morning Report: Department of Internal MedicineDocument13 pagesMorning Report: Department of Internal MedicineSharifah FildaNo ratings yet
- Case Report: Kwashiorkor: BY: JAYA DEV (110100465) Supervisor: Dr. Hj. Tiangsa Sembiring, M.Ked (Ped), Sp.A (K)Document49 pagesCase Report: Kwashiorkor: BY: JAYA DEV (110100465) Supervisor: Dr. Hj. Tiangsa Sembiring, M.Ked (Ped), Sp.A (K)Izaac JdevNo ratings yet
- Emergency Unit Morning Report December 27, 2016: Team 4Document10 pagesEmergency Unit Morning Report December 27, 2016: Team 4Emmeninta FlorensiaNo ratings yet
- LapjagDocument19 pagesLapjagVinnie Juliana YonatanNo ratings yet
- Pre-Res Case Presentation: Jo Anne N. Ramos, MDDocument72 pagesPre-Res Case Presentation: Jo Anne N. Ramos, MDKah Mote KyuNo ratings yet
- Mekong in EnglishDocument8 pagesMekong in EnglishSuri MahdaNo ratings yet
- Case Report: Acute Post-Streptococcal GlomerulonephritisDocument57 pagesCase Report: Acute Post-Streptococcal Glomerulonephritistitis sariNo ratings yet
- Ismael Duty ReportDocument12 pagesIsmael Duty ReportAnonymous C7LSjfNo ratings yet
- Dengue Haemorrhagic Fever: Case ReportDocument37 pagesDengue Haemorrhagic Fever: Case ReportmhimiNo ratings yet
- Morning ReportDocument12 pagesMorning ReportDennis Rafi PrihadiNo ratings yet
- Tetralogy of FallotDocument30 pagesTetralogy of FallotRiYa SHreeNo ratings yet
- Morning Report Dr. Alders - 13519 Ansieta LibertyDocument10 pagesMorning Report Dr. Alders - 13519 Ansieta LibertylmandahaNo ratings yet
- Duty Report Er 23 07 2015Document25 pagesDuty Report Er 23 07 2015Auditya WidyasariNo ratings yet
- Patient M.M: Chioma IkwuegbuDocument16 pagesPatient M.M: Chioma IkwuegbuFernando AnibanNo ratings yet
- Bed Site Teaching DWDocument16 pagesBed Site Teaching DWPutri Utami PratiwiNo ratings yet
- Lapjag 10 Feb 2016 - AnemiaDocument25 pagesLapjag 10 Feb 2016 - AnemiamyoganoNo ratings yet
- Herpes Simplex Keratitis: Chief Complaint: History of Present IllnessDocument13 pagesHerpes Simplex Keratitis: Chief Complaint: History of Present IllnessArmando HalauwetNo ratings yet
- Links For Smoking and Heart Disease: 1. 2. 3. 4. 5. 6. 7. Hyperlipidemia and Heart Disease: 1. 2. 3. 4. 5Document5 pagesLinks For Smoking and Heart Disease: 1. 2. 3. 4. 5. 6. 7. Hyperlipidemia and Heart Disease: 1. 2. 3. 4. 5Armando HalauwetNo ratings yet
- Acute Pyelonephritis in Pregnancy: A Retrospective Analysis of 18 YearsDocument2 pagesAcute Pyelonephritis in Pregnancy: A Retrospective Analysis of 18 YearsArmando HalauwetNo ratings yet
- Rumah Sakit Umum Fkuki SMF Obstetri Ginekologi: Operation ReportDocument2 pagesRumah Sakit Umum Fkuki SMF Obstetri Ginekologi: Operation ReportArmando HalauwetNo ratings yet
- Refrat PyelonefritisDocument12 pagesRefrat PyelonefritisArmando HalauwetNo ratings yet
- Morning Report 2: Department of Internal MedicineDocument11 pagesMorning Report 2: Department of Internal MedicineArmando HalauwetNo ratings yet
- Team 1 Morpot 13 Juni 2014Document13 pagesTeam 1 Morpot 13 Juni 2014Armando HalauwetNo ratings yet
- Team 1 Morpot - 05 Juni 2014Document2 pagesTeam 1 Morpot - 05 Juni 2014Armando HalauwetNo ratings yet