Professional Documents
Culture Documents
Uterine Fibroids
Uterine Fibroids
Uploaded by
salamredOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Uterine Fibroids
Uterine Fibroids
Uploaded by
salamredCopyright:
Available Formats
Uterine Fibroids
Amber M. Shiflett MD
Bryan D. Cowan MD
Basics
Description
Uterine myomas are benign, smooth muscle cell tumors, also called fibroids
and leiomyomas.
Described by location, although most myomas involve >1 layer of the uterus:
o
Subserosal: Projects into the pelvis, causing irregular uterine contour;
may be pedunculated
Intramural: Within uterine wall
Submucosal: Projects into the uterine cavity
May arise from cervix or broad ligament
Range from microscopic to easily palpable; size described in gestational
weeks
May be single or multiple
Most common solid pelvic tumor in women
Most common indication for hysterectomy
Age-Related Factors
Develop during hormonally active reproductive years; ~70% of women at age 45
demonstrate fibroids on sonography.
Staging
Based on the location of the fibroid:
Submucous location: Type 0, I, II
Intramural location (confused with Submucosal Type II)
Subserous location
Epidemiology
True incidence and prevalence are unknown because myomas are usually
asymptomatic
If symptomatic, typically in women between the ages of 30 and 40
Black women are 23 times more likely to develop myomas than white
women
Black women tend to be younger at both time of diagnosis and hysterectomy,
have higher uterine weights, and are more likely to be anemic
Risk Factors
Nulliparity
Obesity
Black race
Genetics
Family and twin studies suggest a genetic predisposition
Associated with hereditary syndromes:
o
Reed syndrome: Uterine and subcutaneous myomas
Bannayan-Zoana syndrome: Uterine myomas, lipomas, hemangioma
Familial hereditary leiomyomas and renal cell carcinoma (linked to a
genetic defect in the Krebs cycle [fumarate hydratase])
Pathophysiology
Abnormal uterine bleeding:
o Increased vascularity and venous congestion
o
Increased surface area of uterine cavity
Compression of pelvic structures
Acute pelvic pain:
Torsion of pedunculated myoma
Protrusion of submucosal myoma through cervix
Infarction as myoma outgrows blood supply
Impaired fertility:
o
Mechanical obstruction or distortion of uterine cavity may interfere
with implantation or with ovum or sperm transport.
Associated Conditions
Iron-deficiency anemia
Endometritis
Adenomyosis
Impaired fertility
Diagnosis
Signs and Symptoms
History
Menstrual, sexual, obstetric histories
Quantify blood loss during menses
Review of Systems
Pelvic/Reproductive:
o Heavy, prolonged, painful menses (submucosal myomas):
May be associated with fatigue, pallor, shortness of breath,
palpitations
Pelvic pressure or fullness
Acute pelvic pain
GI:
Increased abdominal girth
Constipation, tenesmus (posterior myomas)
Urinary:
o
Frequency, urgency (anterior myomas)
Physical Exam
Enlarged, firm, irregular uterus
Peritoneal signs (infarcted myoma)
Conjunctival pallor, tachycardia
Tests
Lab
hCG, CBC, type and cross before surgery
Imaging
TVU to confirm diagnosis, evaluate for ovarian neoplasm
Sonohysterogram to locate intramural lesions
Abdominal plain films may show concentric calcifications
MRI to visualize individual myomas
Hysterosalpingography to define extent of submucous myomas before surgery
or to evaluate uterine cavity and patency of fallopian tubes
Renal US to evaluate for urinary obstruction
Differential Diagnosis
Abnormal uterine bleeding:
o Anovulation
o
Endometrial hyperplasia or malignancy
Pelvic pain:
o
Endometriosis
Adenomyosis
Ectopic pregnancy
Torsion or rupture of ovarian cyst
PID
Pelvic mass:
o
Pregnancy
Adenomyosis
Uterine polyp
Ovarian mass:
Functional cyst
Benign neoplasm
Malignancy
Leiomyosarcoma
Treatment
General Measures
Control severe bleeding and pain
Treat iron-deficiency anemia
Medication (Drugs)
Can reduce myoma size and uterine volume as well as bleeding
Goal is to temporarily reduce symptoms and myoma size
May be sufficient for women nearing menopause
Side effects and expense limit long-term use
None shown to improve fertility
Myomas regain pretreatment size within 34 months after drug is stopped.
OCPs may prevent but will not treat established myomas.
3 classes have demonstrated effective reduction of fibroids: GnRH-agonist,
GnRH-antagonist, and progesterone antagonists.
GnRH agonists:
o
Cause hypoestrogenic state:
Leuprolide: 3.75 mg IM monthly or 11.25 mg IM depot every 3
months
Nafarelin: 400 g intranasally b.i.d. (alternate nostrils)
Goserelin: 3.6 mg implant SC every 28 days
Reduce uterine size by up to 65% and induce amenorrhea in most
women
Maximum response achieved by 3 months
Associated with hot flushes, headaches, vaginal dryness, mood swings,
joint and muscle stiffness, and reversible bone loss, although addition
of HRT may reduce side effects
Not well studied beyond 6 months' use
GnRH-antagonists are not FDA approved for treatment of myomas in the US.
Mifepristone, selective estrogen response modifiers, and interferon-alfa may
have benefit, but their use is largely investigational.
P.193
Surgery
Indications for surgery:
o Contraindication to or intolerance of drug therapy
o
Failure of medical management to control abnormal bleeding or
anemia
Concern for malignancy
Mass effect causing pain, pressure, or urinary or GI tract symptoms
Distortion of uterine cavity causing infertility or repeated pregnancy
loss
Carries risk of infection, bleeding, damage to adjacent organs, adhesion
formation
Hysterectomy:
Definitive treatment
Indicated for extensive disease, suspected malignancy, and myomas in
association with other pelvic abnormalities
Significant improvement in symptoms, quality of life
Appropriate only if future pregnancy not desired
Abdominal myomectomy:
o
Removal of myomas via laparotomy while preserving uterus
Indicated for multiple myomas or uterus larger than 16 weeks in size
Preferred in women desiring future pregnancy
Removal of multiple myomas may involve more time and greater
blood loss than hysterectomy
Considerations after myomectomy:
o
Adhesions may impair fertility
Postpone pregnancy for healing to occur
Cesarean delivery is probably preferable
Laparoscopic myomectomy:
o
Removal of myomas via laparoscope while preserving uterus
Indicated for 1 or 2 easily accessible myomas <8 cm in diameter and
uterine size <16 weeks
Risk of uterine rupture during pregnancy is controversial
Hysteroscopic myomectomy:
o
Removal of submucosal myomas via transcervical operative endoscope
May be performed as same-day surgery with local anesthesia and
sedation
More effective when combined with endometrial ablation, but ablation
precludes future pregnancy
Myolysis:
o
Coagulation/Freezing of myoma
May carry increased risk of adhesions and uterine rupture
Uterine artery embolization:
o
Fluoroscopic guidance: Gel, beads, or coils are introduced through a
catheter in the common femoral artery to the uterine artery
Disrupts blood supply, causing degeneration
Minimally invasive procedure under conscious sedation, with more
rapid recovery
Usually requires overnight hospitalization for pain control
Resolution of bleeding symptoms in up to 90% at 6 months, but
limited studies
Associated with significant pain and fever; sepsis and death have been
reported
Disruption of blood supply to ovaries and endometrium causing
permanent amenorrhea reported in up to 3% of women <40
Unknown effects on later fertility and pregnancy
High-intensity focused ultrasound (HIFU):
o
Technique using HIFU in the MRI
This technique uses array focusing to generate heat in tissue areas of
the fibroid.
No surgery is required.
Currently, patients are in the MRI unit for ~34 hours.
This technique is developmental.
Alert
Rapid growth (increase in uterine size by 6 weeks in 1 year) in a nonpregnant woman,
growth in a menopausal woman, or new pain suggest malignancy and should prompt
surgical removal
Followup
Disposition
Issues for Referral
Refer to fertility specialist if infertility
Urology if ureteral obstruction
Interventional radiologist for uterine artery embolization or HIFU
Pregnancy Considerations
Most myomas do not grow in pregnancy; when they do, most of the growth is
in the 1st trimester.
Large myomas may be associated with pain and premature labor.
Increased risk of abruption, preterm labor, and rupture of membranes if
placenta overlies myoma.
Prognosis
Most symptomatic women require surgery
May recur after myomectomy:
o
Risk increases with number of myomas
Up to 50% recurrence at 5 years
Up to 25% require 2nd surgery
Regress during menopause
HRT may stimulate growth
Patient Monitoring
Serial exam or US every 612 months to determine growth pattern if
asymptomatic:
o Examine at same time in cycle to limit effects of hormonal stimulation
on tumor size
Watchful waiting may be appropriate for large, asymptomatic myomas in
women approaching menopause if malignancy has been excluded.
Annual bone mineral density studies if GnRH agonist are continued >6
months; consider calcium and bisphosphonate therapy
Bibliography
ACOG Committee on Gynecologic Practice. Uterine artery embolization. Obstet
Gynecol 2004;103:403404.
de Kroon CD, et al. Saline infusion sonography in women with abnormal uterine
bleeding: An update of recent findings. Curr Opin Obstet Gynecol 2006;18(6):653
657.
Griffiths A, et al. Surgical treatment of fibroids for subfertility. Cochrane Database
Syst Rev. 2006;3:CD003857.
Practice Committee of the American Society for Reproductive Medicine. Myomas
and reproductive function. Fertil Steril. 2006 Nov;86(5 suppl):S194-49.
Speroff L, et al. Clinical Gynecologic Endocrinology and Infertility, 7th ed.
Lippincott, Williams, & Wilkins 2005: 136140, 10431044.
Stewart EA, Morton CC. The genetics of uterine leiomyomata: What clinicians need
to know. Obstet Gynecol. 2006;107(4):917921.
Sudarshan S, et al. Mechanisms of disease: Hereditary leiomyomatosis and renal cell
cancera distinct form of hereditary kidney cancer. Nat Clin Pract Urol.
2007;4(2):104110.
Wallach EE, et al. Uterine myomas: An overview of development, clinical features,
and management. Obstet Gynecol. 2004;104:393406.
White AM, et al. Uterine fibroid embolization. Tech Vasc Interv Radiol. 2006;9(1):2
6.
Miscellaneous
Synonym(s)
Fibroid
Fibroleiomyoma
Fibroma
Fibromyoma
Leiomyofibroma
Myofibroma
Myoma
Leiomyoma
Clinical Pearls
Most women undergo hysterectomy to treat symptomatic uterine fibroids.
Myomectomy is selected to preserve the uterus for women who wish future
pregnancies, or women who desire retention of the uterus.
Endoscopy is used to treat easily accessible uterine fibroids by laparoscopy, or
pedunculated submucous fibroids (hysteroscopy).
Less invasive treatments are now available, but must be considered
developmental; include uterine artery embolization, HIFU, cryolysis, and radio
frequency ablation.
Abbreviations
GnRHGonadotropin-releasing hormone
HCGHuman chorionic gonadotropin
HIFUHigh-intensity focused ultrasound
HRTHormone replacement therapy
OCPOral contraceptive pill
PIDPelvic inflammatory disease
TVUTransvaginal ultrasound
Codes
ICD9-CM
218.0 Submucous leiomyoma of uterus
218.1 Intramural leiomyoma of uterus
218.2 Subserous leiomyoma of uterus
218.9 Leiomyoma of uterus, unspecified
Patient Teaching
ACOG Patient Education Pamphlets: Uterine fibroids
You might also like
- Fibroids Miracle Cure: The Ultimate Fibroids Diet To Heal NaturallyFrom EverandFibroids Miracle Cure: The Ultimate Fibroids Diet To Heal NaturallyRating: 3.5 out of 5 stars3.5/5 (7)
- Uterine Fibroids & EndometriosisDocument82 pagesUterine Fibroids & EndometriosisDuncan Jackson67% (3)
- OBGYN Revision NotesDocument9 pagesOBGYN Revision NotesJoanne Bowers100% (3)
- Myoma Uteri/Fibroids/ Leiomyomata: Symptoms of Uterine Myoma May IncludeDocument3 pagesMyoma Uteri/Fibroids/ Leiomyomata: Symptoms of Uterine Myoma May IncludeDiane MargretNo ratings yet
- Case 2: Gumalo, Glethel Heruela, Michelle Jalandoni, IreenaDocument44 pagesCase 2: Gumalo, Glethel Heruela, Michelle Jalandoni, IreenaMichelle ThereseNo ratings yet
- OB-GYN 101: Uterine LeiomyomaDocument3 pagesOB-GYN 101: Uterine Leiomyomamadmax500No ratings yet
- 18 - Fibroid + Uterine MalignancyDocument23 pages18 - Fibroid + Uterine MalignancyVersion 1No ratings yet
- Uterine Leiomyoma and Benign Ovarian Tumors 24.8.2022 PDFDocument48 pagesUterine Leiomyoma and Benign Ovarian Tumors 24.8.2022 PDFZayNo ratings yet
- Uterine FibroidDocument46 pagesUterine FibroidAfiqi FikriNo ratings yet
- AdenomyosisDocument4 pagesAdenomyosissalamredNo ratings yet
- Uterine Leiomyoma - Endometriosis.Document48 pagesUterine Leiomyoma - Endometriosis.Inna CazacliuNo ratings yet
- EndometriosisDocument6 pagesEndometriosissalamredNo ratings yet
- Uterine FibroidsDocument42 pagesUterine FibroidsNabila YahayaNo ratings yet
- Impey Obs and Gynae Revision Notes PDFDocument9 pagesImpey Obs and Gynae Revision Notes PDFRoiseNo ratings yet
- Uterine Fibroids PDFDocument3 pagesUterine Fibroids PDFmervat_aastNo ratings yet
- Fibroid General InfoDocument6 pagesFibroid General InfoDurosawo Adeolu TimothyNo ratings yet
- Nursing Management of Myomatous/Uterine FibroidsDocument38 pagesNursing Management of Myomatous/Uterine FibroidsEcaroh Hew Smailliw100% (1)
- GynecologyDocument18 pagesGynecologyLuai Tuma KhouryNo ratings yet
- Dysfunctional Uterine BleedingDocument8 pagesDysfunctional Uterine BleedingJet BautistaNo ratings yet
- Ovarian Cysts: Functional Cysts and Are Always BenignDocument9 pagesOvarian Cysts: Functional Cysts and Are Always BenignElvisNo ratings yet
- Case 5Document5 pagesCase 5irma suwandi sadikinNo ratings yet
- 1.HEAVY MENSTRUAL BLEEDING, FibroidsDocument33 pages1.HEAVY MENSTRUAL BLEEDING, FibroidsAyubNo ratings yet
- Uterine FibroidsDocument30 pagesUterine Fibroidsbabudocs1No ratings yet
- The Management of Uterine Leiomyomas: Egypt - Damietta General HospitalDocument158 pagesThe Management of Uterine Leiomyomas: Egypt - Damietta General HospitalKhaye MendozaNo ratings yet
- Abnormal Uterine BleedingDocument45 pagesAbnormal Uterine BleedingdrmuhammadhaziqNo ratings yet
- Benign Pelvic Tumors - Sundhed - DKDocument6 pagesBenign Pelvic Tumors - Sundhed - DKPavel BerlinschiNo ratings yet
- Fibroids PowerpointDocument27 pagesFibroids Powerpointteritohaha100% (3)
- Gynaecology Passmed PlabDocument49 pagesGynaecology Passmed PlabDoctor daveNo ratings yet
- EndometriosisDocument46 pagesEndometriosisManoj Ranadive0% (1)
- Sakila MurmuDocument47 pagesSakila MurmuSakila murmuNo ratings yet
- Clinicopathologic Case Presentation OB-Gyne Department: Lopez, Vicheryl MDocument47 pagesClinicopathologic Case Presentation OB-Gyne Department: Lopez, Vicheryl Mvicheryl100% (1)
- FibroidDocument40 pagesFibroiddeepaNo ratings yet
- EndometriosisDocument4 pagesEndometriosisAno DzamelashviliNo ratings yet
- Also Called Uterine Leiomyoma, Myoma, Myomata Uteri, FibromyomaDocument25 pagesAlso Called Uterine Leiomyoma, Myoma, Myomata Uteri, Fibromyomashygirl72No ratings yet
- Presentation 1Document20 pagesPresentation 1Mohamad HafyfyNo ratings yet
- EndometrisisDocument10 pagesEndometrisisAmmarNo ratings yet
- Myoma: By: Vabiayu Putri Opponent: Farida Aryani Mariana Ulfah Sandy WijayaDocument37 pagesMyoma: By: Vabiayu Putri Opponent: Farida Aryani Mariana Ulfah Sandy WijayaRaafika StudivianiNo ratings yet
- 11abnormal Uterine BleedingDocument32 pages11abnormal Uterine BleedingAkinbani MoyosoreNo ratings yet
- UMS Short and Long CaseDocument116 pagesUMS Short and Long CaseRosniza RosliNo ratings yet
- Uterus FibroidsDocument25 pagesUterus FibroidsPrincess C. SultanNo ratings yet
- OB/GynDocument11 pagesOB/GynAnonymous TYyF7Ul9o100% (2)
- Breast CancerDocument6 pagesBreast CancercchiechieNo ratings yet
- Abnormal Uterine BleedingDocument45 pagesAbnormal Uterine BleedingdrmuhammadhaziqNo ratings yet
- DR - Prasanjit Chowdhury (Jit) Mbbs (Jzmu) Intern Doctor, U-1 (JMCH)Document52 pagesDR - Prasanjit Chowdhury (Jit) Mbbs (Jzmu) Intern Doctor, U-1 (JMCH)Doctor JitNo ratings yet
- Case 16 (Leiomyoma)Document7 pagesCase 16 (Leiomyoma)Efren Catimbang Jr.No ratings yet
- SodaPDF Converted Obg Med RevisionDocument113 pagesSodaPDF Converted Obg Med RevisionswamysamsonNo ratings yet
- Perimenopausal Bleeding and Bleeding After MenopauseDocument5 pagesPerimenopausal Bleeding and Bleeding After MenopauseAnonymous KwWTUPjXNo ratings yet
- Endometriosis and AdenomyosisDocument36 pagesEndometriosis and Adenomyosishacker ammerNo ratings yet
- 2 2019 02 09!12 08 16 PMDocument34 pages2 2019 02 09!12 08 16 PMPrakask BalanNo ratings yet
- Appendicitis, Acute: Pelvic Inflammatory DiseaseDocument16 pagesAppendicitis, Acute: Pelvic Inflammatory DiseaseLittle SleepybirdNo ratings yet
- 05 - MyomaDocument88 pages05 - Myomapreeti.paul173No ratings yet
- Myoma Uteri: Pregnancy PubertyDocument9 pagesMyoma Uteri: Pregnancy PubertyJaja RamosNo ratings yet
- PolypsDocument2 pagesPolypsjsdlzjNo ratings yet
- Medicine AssignmentDocument73 pagesMedicine AssignmentSahdhana IyerNo ratings yet
- Obsetrics and GynaecologyDocument7 pagesObsetrics and GynaecologyAbedinego MalukaNo ratings yet
- Alternativesto Hysterectomy: Management of Uterine FibroidsDocument17 pagesAlternativesto Hysterectomy: Management of Uterine FibroidsMarco Julcamoro AsencioNo ratings yet
- Endometriosis: by Jane LyttletonDocument8 pagesEndometriosis: by Jane Lyttletonitsik12886No ratings yet
- Hysterectomy A-Z: Why, When, How and What afterFrom EverandHysterectomy A-Z: Why, When, How and What afterRating: 4 out of 5 stars4/5 (2)
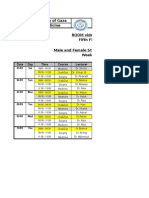
- Islamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1Document2 pagesIslamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1salamredNo ratings yet
- MCQ On MenopauseDocument4 pagesMCQ On Menopausesalamred100% (3)
- Ortho OSCE 2008Document3 pagesOrtho OSCE 2008salamredNo ratings yet
- Choose The Best Appropriate Answerfor Each of The Following QuestionsDocument12 pagesChoose The Best Appropriate Answerfor Each of The Following QuestionssalamredNo ratings yet
- RadiologyDocument5 pagesRadiologysalamredNo ratings yet
- ةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologyDocument14 pagesةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologysalamredNo ratings yet
- MCQ Psy Exam Group BDocument17 pagesMCQ Psy Exam Group BsalamredNo ratings yet
- MCQs Psy Exam44 First GroupDocument7 pagesMCQs Psy Exam44 First Groupsalamred100% (3)
- Longitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionDocument4 pagesLongitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionsalamredNo ratings yet
- Dr:-Ashraf .I. ObaidDocument22 pagesDr:-Ashraf .I. ObaidsalamredNo ratings yet
- MCQDocument11 pagesMCQsalamredNo ratings yet
- Systemic Lupus Erythematosus (Sle) : Presented By: Dr. Walaa MousaDocument13 pagesSystemic Lupus Erythematosus (Sle) : Presented By: Dr. Walaa MousasalamredNo ratings yet
- A) Basic Surgical SciencesDocument27 pagesA) Basic Surgical SciencessalamredNo ratings yet
- SurgeryDocument10 pagesSurgeryIbrahem Y. NajjarNo ratings yet
- اسبيرو طويل مهم جدا الثلاثاءDocument22 pagesاسبيرو طويل مهم جدا الثلاثاءsalamredNo ratings yet
- Forceps Delivery and Vacuum ExtractionDocument8 pagesForceps Delivery and Vacuum ExtractionsalamredNo ratings yet
- Vulvovaginal CandidiasisDocument5 pagesVulvovaginal CandidiasissalamredNo ratings yet