Professional Documents
Culture Documents
6.original Article Tinea Pedis A Clinical Dilemma in Bangladeshi Population PDF
6.original Article Tinea Pedis A Clinical Dilemma in Bangladeshi Population PDF
Uploaded by
ayukarinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
6.original Article Tinea Pedis A Clinical Dilemma in Bangladeshi Population PDF
6.original Article Tinea Pedis A Clinical Dilemma in Bangladeshi Population PDF
Uploaded by
ayukarinaCopyright:
Available Formats
Journal of Pakistan Association of Dermatologists 2010; 20: 23-27.
Original Article
Tinea pedis: a clinical dilemma in Bangladeshi
population
M. A. Wahab*, Rokeya Begum*, Biswas Shaheen Hassan*, Md. Zafrul Islam*, Ishrat
Bhuiyan*, Lubna Khondker**
*Department of Dermatology & Venereology, Bangabandhu Sheikh Mujib Medical University,
Dhaka, Bangladesh.
**Department of Medical Statistics, Bangabandhu Sheikh Mujib Medical University, Dhaka,
Bangladesh.
Abstract Background Tinea pedis is an important public health problem because of the increase in
immunosuppressive states. Large scale studies in Asia are scarce, and the baseline incidence of tinea
pedis is not firmly established.
Objective To find out the clinical types of tinea pedis among the Bangladeshi population.
Patients and methods 200 clinically suspected cases of tinea pedis were included in this study. In all
cases, samples were collected for KOH microscopy and culture. Clinical pattern and associated
relevant factors were noted according to a predetermined protocol.
Results Papulosquamous tinea pedis was the most common clinical pattern in 80 (40%) followed by
intertriginous type in 70 (35%) patients. Hyperkeratotic pattern was found less commonly in 45
(22.5%) patients followed by bullous pattern in 5 (2.5%) patients.
Conclusion The incidence of papulosquamous type of tinea pedis is relatively higher among the
Bangladeshi population than other countries.
Key words
Tinea pedis, Bangladesh.
Introduction
Tinea pedis (athletes foot) is an infection of the
feet caused by dermatophytic fungi. It may last
for a short or long time and may recur after
treatment.1,2 Among all fungal infections, tinea
pedis is the most common.3 The exact incidence
and prevalence of the disease are unknown.
Tinea pedis is contagious and can be passed
Address for correspondence
Dr. Md. Abdul Wahab
MBBS; DDV; MCPS; FCPS; FRCP (Glasgow)
Associate Professor
Department of Dermatology & Venereology,
Bangabandhu Sheikh Mujib Medical University,
Shahbag, Dhaka-1000, Bangladesh.
Email: wahab_skinvd@yahoo.com
through direct contact or contact with items such
as shoes, stocking and shower or pool surfaces.4
Tinea pedis may be itchy, painful or
asymptomatic at all.5 The 20-50 years age group
is most commonly affected and males
outnumber females.6 The disease may present in
any of the four forms: a) papulosquamous type scaly and with some papular lesions on dorsum
of the foot and may also involve plantar aspect;
b) interdigital type (intertriginous) - it is the
most common presentation of tinea pedis and an
infection of the web spaces, particularly between
the 4th and 5th toes; c) hyperkeratotic type welldemarcated erythema with minute papules on
margin, fine white scaling and hyperkeratosis
confined to heels, soles and lateral border of
23
Journal of Pakistan Association of Dermatologists 2010; 20: 23-27.
feet; and d) vesiculo-bullous type - tense
vesicles larger than 3mm in diameter,
vesiculopustules or bullae on the thin skin of the
sole and periplantar areas.7,8
There are a few studies available regarding the
incidence and prevalence of clinical types of
tinea pedis. So our study was designed to see
which of the clinical variants of tinea pedis is
more prevalent in Bangladesh.
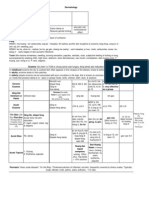
Table 1 Age and sex distribution and duration of
illness (N=200)
Age (years)
20-30
30-40
40-50
50-60
Duration (months)
< 3 months
3-6 months
> 6 months
Male
(n=122)
N (%)
Female
(n=78)
N (%)
15 (7.5)
37 (18.5)
40 (20)
30 (15)
18 (9)
23 (11.5)
22 (11)
15 (7.5)
50 (25)
42 (21)
30 (15)
25 (12.5)
28 (14)
25 (12.5)
Patients and methods
200 clinically diagnosed patients of tinea pedis,
confirmed by KOH microscopy and mycologic
culture, attending Bangabandhu Sheikh Mujib
Medical University, Shaheed Suhrawardy
Hospital, Combined Military Hospital, Dhaka,
Bangladesh during June, 2006 to May, 2009
were included in the study. The patients
consisted of 122 males and 78 females aged
between 20 to 60 years (mean age 40.9514.36
years). Patients aged below 20 years and above
60
years,
recently
or
chronically
immunocompromised and having serious
systemic illness were excluded from the study.
A complete history including age, family
history, duration and site of involvement was
taken. Clinical examination was performed and
types of tinea pedis were noted. Investigations
included only KOH microscopy and culture.
Data were edited by checking consistency and
analyzed by software SPSS method.
Results
Two hundred patients of tinea pedis were
enrolled in the study. The mean age of patients
was 40.9514.36 years, with age range 20-60
years. Gender distribution in different age
groups is shown in Table 1. Males were more
affected than females (p<0.05). Duration of
disease is also shown in Table 1. However,
Table 2 Distribution of the patients by positive
family history (N=200)
Age group (years)
N (%)
20-30
3 (1.5)
30-40
5 (2.5)
40-50
8 (4)
50-60
4 (2)
Total
20 (10)
Table 3 Comparative study of direct microscopy and
culture (N=200)
KOH +ve KOH ve
Total
N (%)
N (%)
N (%)
Culture
120 (60)
32 (16)
152 (76)
+ve
Culture
20 (10)
28 (14)
48 (24)
ve
Total
140 (70)
60 (30)
200 (100)
Table 4 Clinical pattern of tinea pedis (N=200)
Clinical pattern
N (%)
Papulosquamous
80 (40)
Intertriginous
70 (35)
Hyperkeratotic
45 (22.5)
Vesico-bullous
05 (2.5)
Table 5 Distribution of the patients by clinical
pattern of tinea pedis and family history (N=200)
Clinical pattern
Positive
Negative
family history family history
Papulosquamous
7 (3.5%)
73 (36.5%)
Intertriginous
5 (2.5%)
65 (32.5%)
Hyperkeratotic
8 (04%)
37(18.5%)
Vesico-bullous
0 (0%)
05 (2.5%)
there was no significant difference between
various groups (p>0.05). Table 2 shows
statistically significant difference between
different age groups and level of positive family
24
Journal of Pakistan Association of Dermatologists 2010; 20: 23-27.
Figure 1 Tinea pedis: papulosquamous type.
Figure 3 Tinea pedis: hyperkeratotic type.
Figure
2
Tinea
(intertriginous).
pedis:
interdigital
type
history, although positive family history was
present in 3 (1.5%) patients in 20-30 years age
group, 5 (2.5%) patients in 30-40 years age
group, 8 (4%) patients in 40-50 years age group
and 4 (2%) in 50-60 years age group.
Table 3 shows the frequency of positive KOH
microscopy and fungal culture in Saborauds
dextrose agar media. Fungal culture were
positive in 152 (76%) cases and among them
120 (60%) were also positive in KOH
microscopy. KOH microscopy was positive in
140 (70%) cases and among them, 120 (60%)
were culture positive. The chi-square test was
done and the difference was found statistically
significant (p< 0.05).
Figure 4 Tinea pedis: vesico-bullous type.
The distribution of clinical pattern of tinea pedis
is shown in Table 4. It was observed that
papulosquamous type was the most common
type (Figure 1) seen in 80 (40%) patients
followed by intertriginous type (Figure 2) in 70
(35%) and hyperkeratotic type (Figure 3) in 45
(22.5%) patients. The least common was vesicobullous type (Figure 4) present in 5 (2.5%)
patients.
25
Journal of Pakistan Association of Dermatologists 2010; 20: 23-27.
Table 5 shows the relationship between clinical
pattern of tinea pedis and family history of
disease. Family history was infrequent in all
types of tinea pedis (p< 0.05).
Discussion
Tinea pedis is a dermatophytosis of the feet. Of
all fungal infections, it is the most common type.
The risk of tinea pedis increases by wearing
closed shoes, especially if they are plastic lined,
wetting of feet for prolonged time, hyperhidrosis
and minor skin or nail injury. Disease severity
ranges from mild to severe and it may last for a
short or long time. It may persist or recur, but
generally responds well to treatment. Long term
medication and preventive measures may be
needed.9-13
In the present study, 200 patients with tinea
pedis were enrolled. The mean age of the
patients was 40.9514.36 years. The age of the
study population was 20-60 years. Among 2030 years males were 15 (7.5%) and female were
18 (9%), among 30-40 years male were 37
(18.5%) and female were 23 (11.5%), among
40-50 years male were 40 (20%) and female
were 22 (11%), and among 50-60 years male
were 30 (15%) and female were 15 (7.5%).
These findings are consistent with those of
Daniel et al.14 and Foster et al.15 Regarding
duration of the disease in our study, maximum
patients were of less than 3 months duration 75
(37.5%) followed by 3-6 months 70 (35%), these
findings were consistent with the previous
data.1,11,15,16 1.5% in 20-30 years age group, 2.5%
in 30-40 years age group, 4% in 40-50 years and
2% in 50-60 years age group gave positive
family history which was different from those by
Allens et al.16, Attye et al.17 and Pickup et al.18
where they found more percentage of family
history.
Out of 200 patients having tinea pedis, the
most common variant was papulosquamous type
80 (40%) followed by intertriginous pattern 70
(35%) which was not consistent with the
findings of El-Segini et al.19 and Nishimoto20
where they found intertriginous pattern was
most common.
Conclusion
In the present study, the incidence of
papulosquamous type of tinea pedis was
relatively higher among the Bangladeshi
population.
References
1.
2.
3.
4.
5.
6.
7.
8.
Sobera JO, Elewski BE. Fungal Diseases.
In: Bolognia JL, Jorizzo JL, Rapini RP, eds.
Dermatology, Volume 1. New York: Mosby;
2003. P. 1171-98.
Habif TP, ed. Clinical Dermatology, 3rd edn.
St. Louis: Mosby; 1996. P. 366-369.
Verma S, Heffernan, MP. Superficial fungal
infection: dermatophytosis, onychomycosis,
tinea nigra, piedra. In: Wolff K, Goldsmith
LA, Katz SI et al., eds. Fitzpatricks
Dermatology in General Medicine, 7th edn,
Volume 2. New York: McGraw Hill
Medical; 2008. P. 1807-21.
Elewski BE, Hazen PG. The superficial
mycoses and the dermatophytes. J Am Acad
Dermatol 1989; 21: 655-73.
Singh KA, Srivastava KS. A clinicocytological study on tinea pedis at Ranchi.
Studies 1994; 60: 68-71.
Elewski BE, Elgart ML, Jacobs PH et al.
Guidelines of care for superficial mycotic
infections of the skin: Tinea corporis, tinea
cruris, tinea faciei, tinea manuum, and tinea
pedis. J Am Acad Dermatol 1996; 34: 282-6.
Szepietowski JC, Reich A, Garlowska E et
al. Factors influencing coexistence of toenail
onychomycosis with tinea pedis and other
dermatomycoses. Arch Dermatol 2006; 142:
1279-84.
Hapcioglu B, Yegenoglu Y, Disci R et al.
Epidemiology of superficial mycosis (tinea
pedis, onychomycosis) in elementary school
children in Istanbul, Turkey. Coll Antropol
2006; 30: 119-24.
26
Journal of Pakistan Association of Dermatologists 2010; 20: 23-27.
9.
10.
11.
12.
13.
14.
Kenna ME, Elewski BE. A U.S.
epidemiologic survey of superficial fungal
diseases. J Am Acad Dermatol 1996; 35:
539-42.
Krejci-Manwaring J, Schulz MR, Feldman
SR et al. Skin disease among Latino farm
workers in North Carolina. J Agricultural
Safety and Health 2006; 12: 155-63.
Hay RJ, Moore MK. Mycology: tinea pedis.
In Burn T, Breathnach S, Cox N, Griffiths
C, editors. Rooks Textbook of Dermatology,
5th edn. London: Blackwell Science; 2004.
p. 31.32-5.
Sharma NL, Gupta ML, Sharma RC et al.
Superficial mycoses in Simla. Ind J
Dermatol Venereol Leprol 1983; 49: 266-9.
Tsuboi R. Human beta-defensin-2, an
antimicrobial peptide, is elevated in scales
collected from tinea pedis patients. Int J
Dermatol 2006; 45: 1389-90.
Daniel CR, Jellinek NJ. The pedal fungus
reservoir. Arch Dermatol 2006; 142:1344-6.
15. Foster KW, Gahannoum MA, Elewski BE.
Epidemiologic surveillance of cutaneous
fungal infection in the United States from
1999-2002. J Am Acad Dermatol 2004; 50:
748-52.
16. Allen S, Christmas TI, McKinney W et al.
The Auckland skin clinic tinea pedis and
erythrasma study. NZ Med J 1990; 103: 3913.
17. Attye A, Auger P, Joly J. Incidence of occult
athlete's foot in swimmers. Eur J Epidemiol
1990; 6: 244-7.
18. Pickup TL, Adams BB. Prevalence of tinea
pedis in professional and college soccer
players versus non-athletes. Clin J Sport
Med 2007; 17: 52-4.
19. El-Segini Y, Schill WB, Weyers W. Bullous
tinea pedis in an elderly man. Mycoses 2002;
45: 428-30.
20. Nishimoto K. An epidemiological survey of
dermatomycoses in Japan, 2002. Japanese J
Med Mycology 2006; 47: 103-11.
For online version of JPAD visit www.jpad.org.pk
27
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Microbial Diseases of The Skin and Eyes (Microbiology Chapter 21)Document82 pagesMicrobial Diseases of The Skin and Eyes (Microbiology Chapter 21)Katrina Isabel100% (1)
- Pyogenic Cocci - Lec 1 - Staphylococcus 2008Document7 pagesPyogenic Cocci - Lec 1 - Staphylococcus 2008Shama Al-ShadidiNo ratings yet
- Shama Article Nahrain Novel ApproachDocument4 pagesShama Article Nahrain Novel ApproachShama Al-ShadidiNo ratings yet
- Species Identification Revealed That Trichophyton Mentagrophytes Was TheDocument2 pagesSpecies Identification Revealed That Trichophyton Mentagrophytes Was TheShama Al-ShadidiNo ratings yet
- MSC Medial Mycology SyllabusDocument2 pagesMSC Medial Mycology SyllabusShama Al-ShadidiNo ratings yet
- Candida Albicans: in Vitro Inhibition Of: Morphological Transition by Analgesic CompoundsDocument2 pagesCandida Albicans: in Vitro Inhibition Of: Morphological Transition by Analgesic CompoundsShama Al-ShadidiNo ratings yet
- 7 Spirochetes TrponemaDocument7 pages7 Spirochetes TrponemaShama Al-ShadidiNo ratings yet
- 7 Spirochetes TrponemaDocument7 pages7 Spirochetes TrponemaShama Al-ShadidiNo ratings yet
- Melting PointDocument4 pagesMelting PointShama Al-ShadidiNo ratings yet
- Meltingpoint PDFDocument4 pagesMeltingpoint PDFShama Al-ShadidiNo ratings yet
- Laboratory Diagnosis of Fungal Infections: by Prof. Suzan El-FikyDocument56 pagesLaboratory Diagnosis of Fungal Infections: by Prof. Suzan El-FikyShama Al-Shadidi100% (1)
- Proforma InvoiceDocument1 pageProforma InvoiceShama Al-ShadidiNo ratings yet
- Annular Lesions in Dermatology PDFDocument6 pagesAnnular Lesions in Dermatology PDFYanna RizkiaNo ratings yet
- Fungal InfectionDocument5 pagesFungal InfectionFiras HamidehNo ratings yet
- Classification of Fungi PDFDocument2 pagesClassification of Fungi PDFSajjad Hossain ShuvoNo ratings yet
- Superficial MycosesDocument6 pagesSuperficial MycosesPatrick DycocoNo ratings yet
- Medical Fungus TableDocument3 pagesMedical Fungus Tablesidman47No ratings yet
- Tinea Kruris BahanDocument11 pagesTinea Kruris BahanFebridayanti Nur FitriannisaNo ratings yet
- Communicable DiseasesDocument124 pagesCommunicable DiseasesWendy LucasNo ratings yet
- Dermatology DDXDocument29 pagesDermatology DDXM.Dalani100% (2)
- Skin Physical ExamDocument10 pagesSkin Physical ExamVenkatesan VidhyaNo ratings yet
- DCC 241 MinutesDocument88 pagesDCC 241 MinutesMuhammadAmdadulHoqueNo ratings yet
- FNP: Skin ReviewDocument11 pagesFNP: Skin ReviewOMGStudy100% (2)
- Samenvatting Infectie en InflammatieDocument169 pagesSamenvatting Infectie en InflammatiejeskevandiemenNo ratings yet
- Tinea CapitisDocument9 pagesTinea CapitisadityakafiberkahsmgNo ratings yet
- Chinese Medicine InfoDocument28 pagesChinese Medicine Infopeter911xNo ratings yet
- Anti-Fungal Drugs SushDocument31 pagesAnti-Fungal Drugs SushCheng XinvennNo ratings yet
- Skin Diseases Affecting The VulvaDocument7 pagesSkin Diseases Affecting The VulvaNoraNo ratings yet
- Open Comparative Study of Efficacy and Safety of Ketoconazole Soap and Oral Ketoconazole in Tinea VersicolorDocument5 pagesOpen Comparative Study of Efficacy and Safety of Ketoconazole Soap and Oral Ketoconazole in Tinea VersicolorYohanes WidjajaNo ratings yet
- Mycology NotesDocument9 pagesMycology NotesIya Corpus100% (1)
- Nursing Management of Skin and Parasitic DiseasesDocument14 pagesNursing Management of Skin and Parasitic Diseasesyer tagalajNo ratings yet
- Combined Steroid and AntifungalDocument9 pagesCombined Steroid and AntifungalMega RafikaNo ratings yet
- Fast Ringworm CureDocument69 pagesFast Ringworm Curedownload_all_here50% (2)
- Intertrigo and Secondary Skin InfectionsDocument5 pagesIntertrigo and Secondary Skin Infectionskhalizamaulina100% (1)
- ErytrasmaDocument17 pagesErytrasmaAndrean LinataNo ratings yet
- Flood-Related Skin Diseases A Literature ReviewDocument10 pagesFlood-Related Skin Diseases A Literature ReviewMuhamad Kurnia SandyNo ratings yet
- Presented To:: Lahore College For Women UniversityDocument20 pagesPresented To:: Lahore College For Women Universitydbh8No ratings yet
- Skin Wounds Classifications FullDocument66 pagesSkin Wounds Classifications FullDimas GunawanNo ratings yet
- Pathology Skin Infections (Team Swabeh)Document13 pagesPathology Skin Infections (Team Swabeh)Barron KlaNo ratings yet
- TineaDocument4 pagesTineaFenni OktoberryNo ratings yet
- Peds Shelf NotesDocument74 pagesPeds Shelf NotesRandy BornmannNo ratings yet