Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
26 viewsEmergency and Disaster Nursing
Emergency and Disaster Nursing
Uploaded by
chupzptEmergency and Disaster Nursing
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Fdocuments - Us - Microscada Pro Sys 600 9 Abb LTD 10 Microscada Pro 1mrs756118 Operation ManualDocument182 pagesFdocuments - Us - Microscada Pro Sys 600 9 Abb LTD 10 Microscada Pro 1mrs756118 Operation ManualchupzptNo ratings yet
- ABBVU-PGGA-36052 ABB SoftwareVulnerabilityHandlingAdvisory SYS600 SentinelHASPDocument5 pagesABBVU-PGGA-36052 ABB SoftwareVulnerabilityHandlingAdvisory SYS600 SentinelHASPchupzptNo ratings yet
- Ieee Recommended Practice For Network Communication in ElectricDocument140 pagesIeee Recommended Practice For Network Communication in ElectricchupzptNo ratings yet
- Challenges IEC 61850 Substation CommissioningDocument7 pagesChallenges IEC 61850 Substation CommissioningchupzptNo ratings yet
- SPAA 120 C and SPAA 121 C Feeder Protection Relay: User S Manual and Technical DescriptionDocument76 pagesSPAA 120 C and SPAA 121 C Feeder Protection Relay: User S Manual and Technical DescriptionchupzptNo ratings yet
- Spacom ModulesDocument5 pagesSpacom ModuleschupzptNo ratings yet
- ABB IS2 SwitchboardDocument308 pagesABB IS2 SwitchboardchupzptNo ratings yet
- IEEE and IEC StandardsDocument11 pagesIEEE and IEC StandardschupzptNo ratings yet
Emergency and Disaster Nursing
Emergency and Disaster Nursing
Uploaded by
chupzpt0 ratings0% found this document useful (0 votes)
26 views24 pagesEmergency and Disaster Nursing
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentEmergency and Disaster Nursing
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
0 ratings0% found this document useful (0 votes)
26 views24 pagesEmergency and Disaster Nursing
Emergency and Disaster Nursing
Uploaded by
chupzptEmergency and Disaster Nursing
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
You are on page 1of 24
When we accept tough jobs as. a and wade into them with joy and enthusiasm, miracles
‘challenge joy and en
Harry $ Truman
ON ELA aU LCA az aa rea
(SI
oO
Emergency and Disaster Nursing
Linda Bucher
‘LEARNING ‘OBJECTIVES.
1. Apply the sequential steps in tage, the primary survey andthe secondary survey to a patient in an
emergency situation.
2. Describe the pathophysiology, assessment, and collaborative care of select environmental emergencies,
including hyperthermia, hypothermia, submersion injury, and animal bites.
5. Describe the pathophysiology, assessment, and collaborative care of select toxcologic emergencies.
4 iferentiate between the various types and victims of volence
5 enti the agents mos likely to be used in a terrorist attack
6. Diferentate the esponsibilties of health care providers the community, and selec federal agencies in
e emergency and mas casualty incident preparedness.
Electronic Resources
‘Supplemental content related to Chapter 69 can be found
Companion cD
+ Stess Busting Kt for Nursing Students
+ NCLEX Examination Review Questions :
+ Comprehensive Glossary
Content Updates
Key Points Printable and CO/MP3 Download) +
+ Concept Map Creator .
KEY TERMS
bioterrorism, p. 1838
‘emergency . 1642
heat cramps, p. 1828
heat exhaustion, p. 1829,
heatstroke, p. 1829
bypothermia, p. 1851
jaw-thrust maneuver, p. 1823,
mass casualty incident, p. 1842
triage, p. 1822
Evolve Website @ZI0Z9
htp//evoleesevercom/Lewis/medsurg
+ Key Ter Flash Cards
Electronic Caleulators
Weblinks
panded Aucio Glossary
Most patients with lfeshreatening or potentially life-threatening
problems arrive atthe hospital through the emergency department
(ED). Many more patients report tothe ED for less urgent cond
tions.! Over 80 million people visit EDs annually, and this number
is increasing fora variety of reasons (@2., the inability to see a
primary care provider, the aging population, shorter hospital stays
resulting in fequentreadmissions, and lack of health insurance or
primary care provider)? These factors have resulted in chronic
overcrowding and long wait times in many EDs.!
‘Emergency nurses care for patients of all ages and with a vari
ety of problems. However, some EDs specialize in certain patient
populations or conditions, such as pediatric ED or trauma ED. The
Emergency Nurses Assocation (ENA) is the specialty nursing or-
ization aimed at advancing emergency nursing practice. The
provides standards of care for nurses working inthe ED, as
well asa certification process that allows nurses to become a ceti-
fied emergency nurse (CEN).‘ This certification validates the
knowledge that a nurse needs to provide competent care in emer-
‘gency settings.
Emergency management of patients with various medical, sur
gical, and traumatic emergencies is presented throughout this
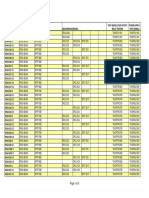
bbook. Tables that highlight emergency management of specific
problems are presented in the related chapters. Table 69-1 lists
each emergency management table by title, number, and page.
‘This chapter focuses on triage, initial assessment, and manage-
‘ment of the trauma patient and selected emergency conditions not
addressed elsewhere in this book, including heat- and cold-related
emergencies, submersion injures, bites, stings, and poisonings. In
addition, an overview of issues related to violence and emergency
and disaster preparedness is presented,
Reviewed by Carlyn Cary, RN, MSN, CEN, Staff Nurse, Emergency Deparent, Virus West Jersey Hospital Marlon, Marton, NJ; and Virginia Crocker, RN MS, CEN,
Clinical Nurse Specialist, Emergency Deparment, Winchester Hospi, Winchester, Mase.
1821
1822 Section 12 Nursing Care in Spec
ized Settings
CARE OF THE EMERGENCY PATIENT
Recognition of life-threatening illness or injury is one of the
‘most important aspects of emergency care. Before a diagnosis
‘can be made, recognition of dangerous clinical signs and symp-
toms with initiation of interventions to reverse or prevent a crisis
Bvt EMERGENCY MANAGEMENT
CSI Emergency Management Tabl
Title Chapter
‘Redominal aura a
Page
7018
‘Acute abdominal pain a 1035,
Acute sot tissue jury 63 692
Anaphylactic shock 4 230
Chemical urns 2 489
Chest pain x 806
Chest wauma 2 586
Cocaine and amphetamine toxicity 2 175
Depressant drugs, overdose of 2 178
Diabetic ketoacicis 4 1280
Dysthytnis 36 848
Eloctrcal burns 25 480
Eye iniuy 2 221
Fractured extremity 63 r612
Head injry 87 1484
Hypertnermia 6 1890
Hypothermia 69 1832
Inhalation njcy 25 480
Sexual assaut| 54 1810
Shock 6 1785;
Spinal cord injury et 1596
Stroke 58 1511
‘Submesion injuries eo 1833
Thermal burns 25 490
Thorac injures a 586
Tonie-cloni eezures 59 1837
is essential, This process begins with the first patient contact
‘The emergency nurse is usually confronted with multiple py
tients who have a variety of problems. Prompt identification
patients requiring immediate treatment and determination of
propriate treatment area are essential nurse competencies in a
busy ED.
Triage
Triage, « French word meaning “to sor,” refers to the process of
rapidly determining patient acuity, tis one of the most important
skills needed by the emergency nurse. The triage
process is based on the premise that patients who have a threat 10
life, vision, or limb should be treated before other patients,
{A triage system identifies and categorizes patients so that the
‘most critical are treated first. The ENA and American College of
Emergency Physicians support the use of a five-level triage sys
tem.’ The Emergency Severity Index (ESI) is a five-level triage
system that incorporates concepts of illness severity and resource
utilization (e.g., electrocardiogram, laboratory work, radiology
studies, intravenous fluids) to determine who should be treated
firs’ (Table 69-2), The ESI includes a triage algorithm that the
‘nurse uses to assign an ESI level to patients presenting to the ED
(Fig, 69-1), Initially, patients are assessed for any threat
(eg. Is the patient apneic?), Patients who do not meet the criteria
for ESI-1 or ESI-2 are next evaluated for the number of anticipated
resources they may need. Patients are assigned to ESI level 3, 4, or
5 based on this determination. Vital signs are required for patients
assigned to ESI level 3, Patients with abnormal vital signs may be
reassigned fo ESI level 2° The use of triage systems such as th
ESI can provide a mechanism for EDs to predict short-term hos}
tal resource and stating needs.*
After the emergency nurse completes the initial assessment 0
determine the presence of actual or potential threats folie, appro-
priate interventions are initiated forthe patient’s condition. A his
to life
TABLE 69-2 We ee ek)
gy, diseuptive
pyohiate patient
Tevel
Definition ESI-1 ESL? ESI-3 ES-4 ESI-S
Staiy ofvtat Unstable “Treatened Sable Stable Sable
function (ASC)
Life treat oF organ Obvious Let but not aways Untely but pssile No No
‘throat ‘covous
How soon patent immediatly Mites Upto the Cod be delayed Cou be delayed
should bo seen
by physician
Expected resource High resource High resource intensty; Medumiigh resource Low resource Low source
intonsty intensity tat ‘rule ofen com: intensity mula iter one intensity, exam
2 bedsioe plex dagrostic Gagosie studies Simple agnostic. nation only
ominously; often Stusils fequent or re obser study ora simple
mobilization of Conautation conie- on er compiex procedure
team response ‘ous pemete) proceaure
mmentonng
Exomples Consac ares Cet pain probaby _Abominl pain or Closed exvemity Cod symptoms,
Tnubate trauma reslteg fom ynecologe trauma, simple roe burn,
patent severe ischemia, miele sorter unlessinn—_laveration,cytiis, recheck
‘overdose, SOS ‘rouma ress severe dates, ‘ype mgane (eg, wound)
response eid ip acre
‘wih feverandietn- —_eldery patent
‘Reims wih pormison, Copyright 190, Richard C, Woe, MD, and David R Eel MD.
ACs, Aiceay, behing, ciclaton SIDS, sdlen nl death syndrome.
Tio nendan |
Sl ee)
e Ne
!
High-Fek shootin?
Conhse/lathogic/ doit?
Severe poin/ direst
Yes
<3mo />180/ >50/
e AGIA Emergency Severity index Tage Agorhm, version 4
tory is obtained simultaneously with the assessment. A systematic
approach to the inital patient assessment decreases the time re-
4uired to identify potential threats and minimizes the risk of over:
looking a life-threatening condition. Two systematic approaches,
primary survey and a secondary survey, were initially developed
for use with the trauma patient, but these can be easily applied to
assessment of any emergency patie
Primary Survey
The primary survey (Table 69-3) focuses on airway, breathin
circulation, and disability and serves to identify life-threatening
conditions so that appropriate interventions can be initiated
Life-threatening conditions related to airway, breathing, circula-
tion, and disability (Table 69-4) may be identified at any point
during the primary survey. When this occurs, interventions are
started immediately and before proceeding to the next step of
the survey.
A= Airway with Cervical Spine Stabilization and/or
Immobilization. Nearly ll immediate trauma deaths occur be-
cause of airway obstruction, Saliva, bloody secretions, vomitus,
laryngeal trauma, dentures, facil t
‘can obstruct the airway. Patients at risk for airway compromise in-
clude those who have seizures, near-drowning, anaphylaxis, for-
body obstruction, oF cardiopulmonary arrest. fan airway is
ou ‘obstruction of ulow occurs and hypo, aid
and death may result
Primary signs and symptoms in a patient with a compromised
airway include dyspnea, inability to vocalize, presence of foreign
1ma, fractures, and the tongue
Chapter 69
Emergency and Disaster Nursing 1823
body in the airway, and trauma to the face or neck. Airway maine-
nance should progress rapidly from the least 10 the most invasive
method. Treatment includes opening the airway using the jaw-
thrust maneuver (avoiding hyperextension ofthe neck) (Fig. 69.
suctioning and/or removal of foreign bedly, insertion of a nasopha:
ryngeal oF an oropharyngeal airway (wil use gagging if patent is
conscious), and endotracheal intubation. If unable to intubate be-
cause of airway obstruction, an emergency cricothyridotomy or
tracheotomy should be performed (see Chapter 27), Patients should
be ventilated with 100% oxygen using a bag-valve-mask (BVM)
Debycration + Tachycardia fds,
+ Thyrotoxcose Weak, thready pulse + Obtain ECs.
* Diabetes + Tampere 09 6"F (975° G)10 104° F + Obtain blond for eecrlyes and CBC.
oc) * Insen uray cathter
Drugs
+" Phenothiazines Heatstroke Ongoing Monitoring
+ Treyeleantiseprossants Hot, dy skin "Motor A, aligns, level of
Diretee + Atered mental stats (9, ranging from consciousness.
+ Montor cardiac rhythm, O» saturation,
+ BeAdrenerge Blockors + Hypotension lectrottes, and urinary output. |
+ Antnistemnes © Taenyoaraa ‘+ Monitor uire for development of
© Weakness rmyogiobinua,
Other Temperature >104° F140") + Monitor clting studies for development of
lisseminatod intravascular coagulation.
ACs, Airway, rcahng, Scan, BV, agave mks CRC. compete ioe coun; CNW cena serous ater, CG. elececaioga IV IHvaNenOw
hot weather and physical exercise is imperative, Patients should
also be instructed on the early signs of and interventions for heat:
related stress.
COLD-RELATED EMERGENCIES
Cold injuries may be localized (Frostbite) or systemic (hypother:
‘mia Contributing factors include age, duration of exposure, envi
‘ronmental temperature, homelessness, preexisting conditions (e..
diabetes mellitus, peripheral vascular disease), medications that
‘suppress shivering (opioids, heroin, psychotropic agents, and anti
femeties), and alcohol intoxication, which causes peripheral vaso-
dilation, increases sensations of warmth, and depresses shivering,
‘Smokers have an increased risk of cold-related injury asa result of
the vasoconstrictive effects of nicotine.
Frostbite
Frostbite can be described as “true tissue freezing.” which results
in the formation of ice crystals in the tissues and cells. Peripheral
‘vasoconstriction isthe initial response 10 cold stress and results in
1 decrease in blood flow and vascular stasis. As cellular tempera-
ture decreases and ice crystals form in intracellular spaces. intra
cellular sodium and chloride inerease, the cell membrane is de-
stroyed, and organelles are damaged. These alterations result in
edema, Depth of frostbite is the result of ambient temperature,
length of exposure, type and condition (wet or dry) of clothing,
and contact with metal surfaces. Other factors that affect severity
include skin color (dark-skinned people are more prone to frost-
bite). lack of acclimatization, previous episodes, exhaustion, and
poor peripheral vascular st
‘Superficial frostbite involves skin and subcutaneous tissue, usu-
ally the ears, nose, fingers, and toes. The skin appearance will
(BIGGS ema ad ter formation 24 hus ater site in occur
sgn an aca covred bya thy ed boot
n of tingling
Bea ‘Gangrenous necross 6 weeks atter the frostbite injury shown in
rg 693.
cof deep thermal injury with mottling gradually progressing to
gangrene (Fig. 69-4) The affected extremity is immersed in a
circulating water bath (102° to 108” F [38.9° to 42.2° C)) until
distal flush occurs. After rewarming, the extremity should be ele-
vated to reduce edema Significant edema may begin within
3 hours, with blistering in 6 hours to days. Intravenous analgesia
is always required in severe frostbite because ofthe pain associ-
ated wit tissue thawing. Tetanus prophylaxis should be given,
and the patient should be evaluated for systemic hypothermia,
‘Amputation may be required ifthe injured area is untreated or
treatment is unsuccessful. The patient may be admitted to the
ital for observation over 24 to 48 hours with bed rest, eleva-
‘ofthe injured part, and prophylactic antibiotics if tbe wound
at rsk for infection
Hypothermia
‘Hypothermia, defined a a core temperature less than 95°F (35°C),
‘occurs when heat produced by the body cannot compensate for heat
lost to the environment. From 55% to 60% of all body beat i lost as
radiant energy, with the greatest loss from the head, thorax, and
Jungs (with each breath). Wet clothing increases evaporative heat
Joss 5 times greater than normal; immersion in cold water increases
beat loss by a factor of 25. Environmental exposure to freezing tem-
peratures, cold winds, and wet, damp terrain in the presence of
physical exhaustion, inadequate clothing, and/or inexperience pre-
disposes individuals to hypothermia. Near-drowning and water
immersion are also associated with hypothermia,
‘The elderly are more prone to hypothermia due to decreased
body fat, diminished energy reserves, decreased basal metabolic
rate, decreased shivering response, decreased sensory perception,
chronic medical conditions, and medications that ater body de-
fenses. In addition, certain drugs, alcohol, and diabetes are consid-
eed risk factors for hypothermia.
‘Hypothermia mimics cerebral or metabolic disturbances caus-
ing ataxia, confusion, and withdrawal, so the patient may be mis-
diagnosed. Peripheral vasoconstriction is the body's first attempt
to conserve heat. As cold temperatures persist, shivering and
movement are the body's only mechanisms for producing heat.
results when core temperature falls below 82.4° F (28° C),
death usually occurs when core temperature falls below 78° F
O*
Core temperature below 86° F (30° C) is severe and potentially
life threatening. Assessment findings in hypothermia are variable
sand dependent on core temperature (Table 69-9). Patients with
Chapter 69 Emergency and Disaster Nursing 1831
‘mild hypothermia (93.2° to 96.8° F [34° to 36° C}) have shivering,
lethargy, confusion, rational to irrational behavior, and minor heart
rate changes. Shivering disappears at temperatures less than 92°F
(G3.3° ©). Moderate hypothermia (86° to 93.2° F [30° to 34° C})
causes rigidity, bradycardia, slowed respiratory rate, blood pres-
‘sure obtainable only by Doppler, metabolic and respiratory acido-
sis, and hypovolemia.
‘As core temperature drops, basal metabolic rate decreases two
or three times. The cold myocardium is extremely irritable, mak-
ing it valnerable to dysrhythmis (e.g, atrial and ventricular fibril-
lation). Decreased renal blood flow decreases glomerular filtration
rate, which impairs water reabsorption and leads to dehydration,
‘The hematocrit increases as intravascular volume decreases. Cold
blood becomes thick and acts asa thrombus, placing the patient at
risk for stroke, myocardial infarction, pulmonary emboli, acute tu-
bular necrosis, and renal failure. Decreased blood flow leads to
lactic acid accumulation from anaerobic metabolism and subse-
quent metabolic acidosis,
Profound hypothermia (less than 86° F (30° C}) makes the per-
son appear dead. Metabolic rate, heart rate, and respirations are so
slow that they may be difficult to detect. Reflexes are absent and
the pupils fixed and dilated. Profound bradycardia, asystole, or
ventricular fibrillation may be present. Every effort is made to
warm the patient to at least 90° F (32.2° C) before the person is
pronounced dead. The cause of death is usually refractory ventric-
‘lar fibrillation,
Care. Treatment of hypothermia focuses on
managing and maintaining ABCs, rewarming the patient, correcting
dehydration and acidosis, and treating cardiac dysthythmias (see
‘Table 69-9), Passive or active external rewarming is used for mild
hypothermia. Passive external rewarming involves moving the pa-
tient to a warm, dry place, removing damp clothing, and placing
warm blankets on the patient. Gentle handling is essential to prevent
stimulation ofthe cold myocardium. Active external rewarming in-
volves body-to-body contact, uid- or air-filled warming blankets,
‘or radiant heat lamps. The patient should be closely monitored for
‘marked vasodilation and hypotension during rewarming.
‘Active core rewarming is used for moderate to profound hypo-
thermia and refers to heat applied directly tothe core. Techniques
include heated (107.6° to 148° F [42° to 46° C), humidified oxy-
‘gem; warmed IV fluids (109.4° F [43° C); and peritoneal, gastric, or
colonic lavage with warmed fluids. Hemodialysis or cardiopulmo-
nary bypass may also be considered in profound hypothermia
‘Core temperature should be carefully monitored during re-
‘warming procedures. Warming places the patient at risk for afer-
drop, a further drop in core temperature, which occurs when cold
peripheral blood returns to the central circulation. Rewarming
shock can produce hypotension and dysrhythmias. Thus patients
with moderate to profound hypothermia should have the core
‘warmed before the extremities. Rewarming should be discontinued
‘once the core temperature reaches 95° F (35° C):
Patient teaching should focus on how to avoid future cold-
related problems. Essential information includes dressing in layers
for cold weather, covering the head, carrying high-carbohydrate
foods for extra calories, and developing a plan for survival should
an injury occur.
SUBMERSION INJURIES
‘Submersion injury results when a person becomes hypoxic due
to submersion in a substance, usually water. Approximately 8000
deaths occur from submersion injuries annually in the United
1832 Section 12 _ Nursing Care in Specialized Settings
r
i
i
potital EMERGENCY MANAGEMENT
oo ea
Hospital Acquired
© Cold fats
‘in to com)
Etiology ‘Assessment Findings Interventions
Environmental + Core body temperature: Initial
Prolonged exposure to old Mid hypothermia: 95.2"-96.8° F G4"-96"C) + Remove patient from cold envionment.
Prolonged submersion Moderate hypothermia: 86°-88.2"F Manage and mantain ABC.
+ Inadequate clthing fr environmental (00-34 6) + Provise righsow Oz via non-rebreathor
temperature Profound hypothermia: <86"F (30° 0) mask or BVM,
‘+ Shivering, diminished or absent at core body + Anticipate intubation fr eminished or
Metabolic temperature =92"F (333° 0) absent gag refs.
+ Hypostycemia + Hypoventation + Faowam patent:
+ Hypotnyroism * Hypoiension Passive: Remove wet clothing, apply dry
‘Altered mental status (ranging from contu-
+ ofoxia (absence of reflexes) ‘Active extemal: Use body-to-body contact,
© Blood administration © Pale, cyanotic skin apply eating devices (e.g, alec
* Inadequate warming or rewarming inthe ED + lve, white, or frozen extremities warming blankets) or radiant ight
or sugery * Dysthymias: bradycardia, ail Fixllaion, Active core warming: Administer warmed
+ Adminstration of peuromuscular blocking ventricular filation, aystole 'V us; heated, humicied 0:
agents Fixed, cated pups pertoneal, gastric, or colonic lavage wit
warmed fu.
Other * Anticipate the need for hemodialysis
+ Phenethiazines Ccarciopulmonary bypass.
+ Barbiturates| * Warm central trunk frst in patients with pro
+ Alcohol found hypothermia to mit rewarming shock.
: Tama + Establish IV access with two large-bore
Clothing and warm blankets, administer
warm fds,
catheters for fui resustation.
‘Assess for othe injuries.
‘Keop patients head covered with warm, dy
‘owes, or stocking cap to limit los of hoat
‘Treat patient gently to avoid increased car
ac imtabity,
Ongoing Monitoring
Monitor ABCs, level of consciousness,
temperature, vital sans.
Monitor O, saturation, cardiac rythm.
Monitor electrolytes, glucose.
ABCs, Away, being culation, BVM, fag valve-nask: ED. emergency depart, V7, invavenow.
States. Forty percent of these victims are children under 5 years of
age. The primary risk factors for submersion injury include inabil-
ity to swim, use of alcohol or drugs, trauma, seizures, hypother-
‘mia, and stroke
Drowning is death from suffocation after submersion in water
or other fluid medium. Near-drowning is defined as survival from
potential drowning. Jmmersion syndrome occurs with immersion
in cold water, which leads to stimulation of the vagus nerve and
potentially fatal dysrhythmias (e.., bradycardia).
Death from a submersion injury is caused by hypoxia secon
dary to aspiration and swallowing of fluid, usually water. Swal-
lowed water may cause vomiting and additional aspiration. A ma-
jority of drowning victims aspirate water into the pulmonary tree
and develop pulmonary edema. Victims who do not aspirate fluid
develop intense bronchospasm and airway obstruction, the cause
of death in “dry drowning.” Regardless of what fluid is aspirated
into the pulmonary tree, the ultimate result is pulmonary edem:
‘The osmotic gradient caused by aspirated fluid causes fuid imbal-
ances in the body. Hypotonic fresh water is rapidly absorbed into
the circulatory system through the alveoli, Fresh water may be
contaminated with chlorine, mud, and algae, causing the break
down of lung surfactant, fluid seepage, and pulmonary edema
Hypertonic salt water draws protein-rich fluid from the vascular
space into the alveot
in hypoxia, Fig, 69
freshwater aspiration,
‘The body attempts to compensate for hypoxia by shunting
blood to the lungs. This results in inereased pulmonary pressures
and deteriorating respiratory status. More and more blood is
shunted through the alveoli. However, the blood is not adequately
oxygenated, so the hypoxemia worsens. Anaerobic metabolism.
‘occurs, which leads to lactic acidosis.
The assessment findings of a patient with a submersion injury
are listed in Table 69-10. Aggressive resuscitation efforts and the
‘mammalian diving reflex improve survival of near-drowning vic~
tims even after submersion in cold water for long periods of time?”
old water lowers the body's metabolic rate and oxygen demand.
‘The mammalian diving reflex causes apnea, bradycardia, and pe-
ripheral vasoconstriction and further decreases metabolic ate.
Blood flow is redistributed to the most vital organs (ie., heart,
lungs, brain).
impairing alveolar ventilation and resulting
shows the pulmonary effects of saltwater and
Collaborative Care @
Treatment of submersion injures focuses on conecting hypo
eel alec uloareefocpearing | ae
lps lgie Renae rewaralag whos lypetarala i pre
Chapter 69 Emergency and Disaster Nursing 1833
cnt. Initial evaluation involves assessment of airway, cervical
spine, breathing, and circulation, Other interventions are listed in
Se 69-10,
‘Mechanical ventilation with positive end-expiratory pressure or
‘Continuous positive airway pressure may be used to improve gas
FIG. 6925 Pulmonary effects of water aspiration
exchange across the alveolar-capillary membrane when significant
pulmonary edema is present. Ventilation and oxygenation are the
primary techniques used to treat respiratory acidosis. Mannitol
(Osmitrol) or furosemide (Lasix) may be given to decrease free
water and treat cerebral edema,
Deterioration in neurologic status suggests cerebral edema,
worsening hypoxia, or profound acidosis. Near-drowning vietims
may also have head and neck injuries that cause prolonged altera
tions in level of consciousness. All victims of near-drowning
should be observed in a hospital for a minimum of 4 to 6 hours.
Additional observation is needed for patients who have preexisting
comorbidities (e.g., cardiovascular disease). Peumonia and cere=
bral edema have been reported in patients who were essentially
free of symptoms immediately after the near-drowning episode but
later developed problems. Delayed pulmonary edema (also known
as secondary drowning) can occur and is defined as delayed death
from drowning due to pulmonary complications,
‘Teaching should focus on water safety and minimizing the risks
for drowning. Swimming poo! gates should be locked: life jackets
should be used on all watercraft, including inner tubes and rafts
and water survival skills (eg, swimming lessons) should be a pri-
ority. The dangers of combining alcohol and drugs with swimming
and other water sports should be emphasized”
BITES AND STINGS
‘Animals, spiders, and insects cause injury and even death by biting
or stinging. Morbidity is a result of either direct tissue damage or
lethal toxins. Direct tissue damage is a product of animal size,
characteristics ofthe animals teth, and strength of the jaw. Tissue
may be lacerated, crushed, or chewed while toxins released
RUC EMERGENCY MANAGEMENT
CST submersion Injuries
Etiology ‘Assessment Findings Interventions
aby to swim or exhaustion wile Pulmonary Initial
swimming + infective breathing “Manage and martan ABCs
* Entrapment or entanglement wih objects in Oyspnaa Assume cervical spine injury nal rowing
water + Respratory dstoss Victims and sabize andlor mmebitze
* Loss of ability to move secondary to trauma, + Respiratory arrest carvieal spine.
stroke hypothermia, myocartal infarction” + Crackles, ones + Provide 100% O, via non-roreathr mask or
+ Poor judgment du to alcohol or drugs * Gough with pink-fothy sputum BVM
© Seaure whe n water + Gyanosis + Anticipate need for intubation gag retex's
absent.
Cardiac + Estabish IV access with wo large-bore
+ Tachycardia ‘catheters fr fa esusctation and ise
* Bradyearia ‘warmed fui if appropriate
+ Dystythmia + Assess for other ines
+ Hypotension * Remove wet dthing and cover wih warm
+ Garda: arest blankets
+ Obtain temperature and begin rewarming it
Other pacer
+ Parse + Obiain cervical pine and chest xays.
+ Exhaustion + insert gat tube
+ Coma
+ Cosxisting iess (eM or inury ‘Ongoing Monitoring
(€9,. conical spine iniy) + Monitor ABCs, vita signs, evel of
+ Gore temperatire aight elevated or below consciousness.
rormel depending on water temperature arc) + MontorO, saturation, care rythm.
length of submersion ‘Monitor temperature and maintan
oxmothermia,
+ Monitor for signs of acute respiratory faire
ACs, Airway, behing, circulation; BVM, bag-alve-mank; IV inravenos; MT myocardial infarction
Erne)
1834
Section 12
Nursing Care in Specialized Settings
through teeth, fangs, stingers, spines, or tentacles have local or
systemic effects. Death associated with animal bites is due to
blood loss, allergic reactions, or lethal toxins. Injuries caused by
Insects, spiders, ticks. snakes. animals (e.g., dogs. cats, rodents),
‘and humans are described here
Hymenopteran Stings
‘The Hymenoptera family includes bees, yellow jackets, hornets,
wasps, and fire ants. Stings can cause mild discomfort ot life-
threatening anaphylaxis (see Chapters 14 and 67), Venom may be
cytotoxic, hemolytic, allergenic, or vasoactive. Symptoms may
begin immediately or be delayed up to 48 hours. Reactions are
more severe with multiple stings. Most hymenopterans sting re:
peatedly, However, the domestic honey bee stings only once, usu:
ally leaving a barbed stinger with an attached venom sac in the
skin so that release of venom continues. ATticanized honey bees
(killer bees) which look and sting like domestic bees have mi
‘grated into North America, If threatened, these bees aggressively
swarm and repeatedly sting their victims (e.g, humans, animals).
‘These attacks can be fatal
I'stung, the stinger should be removed with a scraping motion
with a fingernail, knife, or needle. Tweezers squeeze the stinger
‘and may cause more venom release. However, the fastest method
‘of removing the stinger is ultimately the best, so if weezers are
available, they can be used.
“Manifestations vary from stinging, burning, swelling, and itching
to edema, headache, fever, syncope, malaise, nausea, vomiting,
wheezing, bronchospasm, laryngeal edema, and hypotension. Treat.
‘ment depends on the severity of the reaction. Mild reactions are
treated with elevation, cool compresses, antipruritic lotions, and oral
antihistamines, Rings, watches, and restrictive clothing are removed
More severe reactions require intramuscular or IV antihistamines
(eg, diphenhydramine (Benadryl)), subcutaneous epinephrine, and
corticosteroids (e-g., dexamethasone [Decadron]). Allergic reactions
and anaphylaxis are discussed in Chapter 14.
Spider Bites (Arachnid)
Although there are 20,000 species of venomous spiders in the
‘world, only 50 species cause illnes. Two venomous spiders found
in the United States are the black widow spider and the brown re-
clase spider2* Their venom can eause a localized reaction or sys-
temie anaphylaxis. Tarantulas appear more dangerous than they
actually are because thei bite causes only localized stinging and
pain, Other types of spiders telease Venom when they bite and may
cause allergi reactions in some individuals, but they are not con-
sidered poisonous.
Black Widow Spiders. Black widow spiders are the most
feared of al spiders. The female's venom is especially poisonous
to people. Both the female and male are black in color (Fig. 69-6).
The female rarely leaves the web, biting defensively if disturbed
Black widow spiders are found among fallen branches, among
firewood, and under objects of many kinds, including furniture,
outhouse seas, and trash,
‘The black widow spider venom is neurotoxic. When bitten, the
patient will feel a pinprickclike sensation and a tiny, ed bite mark
will appear. Approximately 15 to 60 minutes late, the patient will
report severe pain that will increase over the next 12 t0 48 hours
Systemic symptoms will develop 30 minutes alter envenomation
(the imoducton of poisonous venoms into the body by a bite ora
sting). These can include nausea, vomiting, abdominal eramping
hypertension, dyspnea, paresthesias. and tachycardia, Symptoms
FIG. 69-6 Female tack widow spider The fully gronn female is about
1.2 am (05 in) ong and «jet Back, war hourglass shaped red mack onthe
Underside ofthe abdomen. Te feral’ sing potions to humans Males are
‘only about half slong and usuaby have four pas of ed dos along the sides
the abdomen, Males ae rarely Seen and when they metre, they lose ther poi
sonous abit
usually peak 2 t0 3 hours after onset; however, muscle spasms and
jon can recur for 12 to 24 hours. Chest and abdominal
‘abdominal rigidity, whereas bites on the upper body lead to
chest, back, and shoulder rigidity. A black widow spider bit is not
prominent and can be easly missed, Patents not aware of the bit
can be misdiagnosed, because symptoms mimic a perforated ulcer,
appendicitis, pancreatitis, or other abdominal emergency
‘Treatment includes cooling the area to slow the acto
neurotoxin, IV access should be established and oxygen adminis
tered as needed, The wound shouldbe cleaned and tetanus a
laxis given as appropriate. Muscle spasns are treated with cle
gluconate, diazepam (Valium), or methocarbamol (Robaxin), Se-
Xere pain may requite opioid analgesia. Although antivenin is,
rarely used, it can be used for severe reactions, young children, or
adulls with hypertension or cardiac disease
Brown Recluse Spiders. Brown recluse spiders are usually
found in dark areas such as garages, cosets, and boxes. The spider,
common in the southeaster, south-central, and southwestem
United States. is a light brown color with a characteristic dark
brown fiddle shape that extends from the eyes down the back. The
venom is cytotoxic, so local tissue effects can be dramatic. Ini-
tially, the bite is insignificant, with a local reaction (ez. itching,
erythema) beginning in 6 to 12 hours. A painful, bluish-purple
purpura develops in a ring around the bite and eventually may
progress to a necrotic uleerating wound by 7 to 14 days, though it
‘may take as long as 6 months. The wound can extend deep into
tissue and may persist for weeks. Occasionally, systemic manifes
tations of envenomation occur and ean include fever, chills, join
pain, malaise, nausea, and vomiting.®
‘Treatment depends on severity of the reaction. Treatment is
necessary when there is bleb or bulla formation, intense pain, and
signs of rapidly progressive ischemia and necrosis. Initial inte
ventions include cleansing the bite with mild antiseptic soap.
providing cool compresses, and elevating the affected extremity
Analgesia, tetanus prophylaxis, antihistamines, corticosteroids,
and antibiotics for prevention of secondary infection may also
some patients. Hyperbaric oxygen therapy may also be const
ered to enhance tissue healing. Dapsone (Avlosulfon), a poly
morphonuclear leukocyte inhibitor, has been used for patients
with deep crater wounds, bat efficacy has not been validated. Pa
of the
o— eh.
t
FIG. 69-7 Tick removal A, Use tvcezrs to rasp the tick close tothe skin
B, With 6 steady moti, pull he t's body any fom the sin. Oo not be
ried 4 the teks mouthparts feman in the skin. Once the mouthparts ae
ved om the ret ofthe tc, can no longer vans ease.
tients with systemic manifestations are hospitalized and moni
toted for hemolysis, disseminated intravascular coagulation, and
acute renal failure”
Tick Bites
Ticks are found throughout the United States, but they are most
common inthe northwestern, Rocky Mountain, and the northeastern
regions. Emergencies associated with tick bites include Lyme dis:
Rocky Mountain spotted fever, and tick paralysis. Disease is
ed by an infected tick or by the release of neurotoxin. Ticks re
se a neurotoxic venom as long as the tick head is attached tothe
body. Therefore removal ofthe attached tick is essential for effective
tweatment. Forceps or tweezers may be used to safely remove the
tick by grasping atthe point of entry and pulling upward ina steady
‘motion (Fig. 69-7). After the tick is removed, the skin should be
leaned with soap and water. Do not use a hot match, petroleum
jelly, nal polish, or other products to remove the tick.§*
Lyme disease is the most common arthropod-bome disease in
the United States. Symptoms appear within 2 10 30 days of a bite
from the Lxodid (hard) tick and result from exposure to the spiro-
chete Borrelia burgdorferi that is found on the tick. The initial
stage ofthis disease is characterized by nonspecific flu-like symp-
toms (e.g. headache, stiff neck, fatigue) and a characteristic bull's
eye rash—an expanding circular area of redness of 5 em diameter
‘or more. Symptoms will disappear in 2 weeks if not treated, Mono:
articular arthritis, meningitis, and neuropathies occur days or
‘weeks after the initial symptoms. Chronic arthritis and myocarditis,
characterize the later stage of the disease, which can develop sev
cral months to 2 years after the initial skin lesion, Treatment in-
cludes doxyeycline (Vibramycin) and cefuroxime. (Lyme disease
is discussed in Chapter 65.)
Rocky Mountain spotied fever is caused by Ricketsia rickemsi,
‘bacteria that is spread to humans by the /xodid tick. I has an
cubation period of 2 to 14 days, and a pink. macular rash appears
‘on the palms. wrists, soles, feet, and ankles within 10 days of ex-
sure, Other symptoms include fever, chills, malaise, myalgias,
@ each, Dingncis is often cfc inthe eal sage, and
fhout treatment it can be fatal. Antibiotic therapy with doxyc
cline (Vibramycin) is the treatment of choice
Tick paralysis accurs 5 to 7 day’ afler exposure to & neurotoxin
Introduced by a wood tick or dog tick. Classie symptoms are Mac-
1835
Emergency and Disaster Nursing
Pit viper
[venomous snake)
®
‘Wiangle-shaped hood
Anal plete
Single row
of subeaudl
plotes
Rotle(ratlesnake)
FIG. 69-8 Pipe (2 ype of venomous snake),
FIG, 69-9 western cara snake
1 venom rom this sake is newton
cid ascending paralysis, which develops over I to 2 days, Without
tick removal, the patient dies as respiratory muscles become para
lyzed, Tick removal leads to return of muscle movement, usually
within 48 to 72 hours
Snakebites
Only 375 of the 3000 species of snakes in the world are poisonous,
Poisonous snakes indigenous to the United States are members of
the Crotalidae and Elapidae family. Crotalidae, or pit vipers, in
clude rattlesnakes, copperheads, and water moccasins (Fig. 69:8)
Coral snakes belong 10 the Elapidae family. Coral snakes do not
exhibit the triangular head of pit vipers but are recognized by their
bright colors. Coral snakes always have a blunt black snout and
‘ed, yellow, and black rings that completely encircle the body (Fig.
{69.9), Coral snakes are poisonous non-pit vipers.
‘Venom from the pit viper is hemolytic, whereas coral snake
venom is neurotoxie. Envenomation occurs in approximately 75%
© 80% of all snakebites. If swelling does not occur within
30 minutes after the bite, envenomation is unlikely. Local reaction
is characterized by one or two fang matks associated with pain,
bruising, and edema within 36 hours of injury, petechiae, ecehy-
‘mosis, and erythema. Loss of function and necrosis ofthe affected
Jimb may occur 16 to 36 hours after the bite. Systemic reactions
Include nausea and vomiting, dizziness, tachycardia, muscle fas
ciculations, gastrointestinal (Gl) bleeding, and respiratory prob:
lems. The patient may experience a metallic or rubber taste. Neu
rologic symptoms such as constricted pupils, drowsiness, weakness,
fasciculations, muscle weakness, and seizures oceur with neuro:
problems associated with systemic
toxic venom,
fore ond
1836
Nursing Care in Specialized Settings
Pee mes
TABLE 69-11
paresthesia
listo moderate
‘no eystemic reactons
Moderate: Fang marks, progressive sweling beyond
bite, mid systemic reaction fe... nausea,
ving, parethesias, hypotension)
Envenomation Signs and Symptoms ~ Number of Vials of Antivenint
one Fang mar, no toca swell, Femorhage No aver, tetanus propa, observation
-Mid: Fang marks, local sweting of hands or feet, pain,
Init dose: 4-6 vias (3000-4500 ma) intused over: infusion
‘shoud be initiated slowiy for he frst 10 min to detect any
allergic reactions; final control of symptoms isnot achieved,
‘dose may be repeated once
Actiona agian 2 vals ever 6h for 18 hr
"Polya! Crouse avon one Fab (COPD
For Ctl exsenomation (eg atesnaks,coppetheas)
‘envenomation include severe hemorrhage, renal failure, and hypo.
volemic shock.
Treatment focuses on preventing the spread of venom. Rings,
watches, and restrictive clothing should be removed, and then the
affected limb should be immobilized at the level of the heart. lee
and touriquets are not recommended. Incision of the wound is
controversial. If done within 3 minutes of injury with the appropri
ate device (e.g., Sawyer extractor), 5% to 30% of the venom may
‘be removed. Caffeine, alcohol, and smoking increase the spread of
venom and should be avoided.
ED management includes vascular access with a large-bore
(14. to 16-gauge) catheter and administration of crystalloids to
maintain blood pressure. Diagnostic tests include complete blood
‘count, urinalysis, coagulation studies, blood urea nitrogen, creati-
nine, creatine kinase, and electrolytes. Other measures include as:
sessment of extremity swelling, usually through documentation of
circumference every 30 to 60 minutes, Pain should be treated with
acetaminophen (Tylenol). Aspirin and nonsteroidal antinflamma
tory drugs should be avoided because they may exacerbate bleed:
ing: opioids may cause respiratory depression, Tetanus prophy’
laxis should be administered as needed (see Table 69-6). Secondary
infection caused by microorganisms in the snake's mouth or other
contaminants may require antibiotic therapy. Debridement or fas
ciotomy (see Chapter 25) is necessary in some patients, Antivenin
(polyvalent Crotalidae antivenin ovine Fab (CroFab)) therapy is
used in mild to moderate reactions; the amount of antivenin re
‘quired depends on the timing, type, and severity of envenomation
(Table 69-11), Incomplete dosage is the most common cause of
treatment failure.
Animal and Human Bites
Every year over 2 million animal bites are reported in the United
States.) Children are at greatest risk. The most significant prob-
lems associated with animal bites are infection and mechanical
destruction of the skin, muscle, tendons, blood vessels, and bon
‘The bite may cause a simple laceration or be associated with crush
injury, puncture wound, or tearing or avulsion of tissue. The sever-
ity of injury depends on animal size, vietim size, and anatomic lo-
cation of the bite. Animal bites from dogs and cats are most com-
‘mon, with wild or domestic rodents (e.g., squirrels, hamsters)
following dogs and cats as the third most frequent offenders in re
ported animal bites.”
Dog bites usually occur on the extremities; however, facial bites
are common in small children, Most victims own the dogs that bite
them, Dog bites may involve significant tissue damage with fatal
ties reported, usually in children. Skull fractures with intracranial
injury and death may occur in children less than 2 years old. Dis-
Figuring wounds of the face should be evaluated by a plastic
surgeon.
‘Cat bites cause deep puncture wounds that can involve tendons
and joint capsules and result in a greater incidence of infection
(30% to 50%). Septic arthritis, osteomyelitis, and tenosynovitis,
have been reported in cat bites. The most common causative or
zanisms of infections from cat und dog bites are from the Pastew
rella species (eg, P.canis), This organism is found in the mouths
ff most healthy cats and dogs."
Human bites also cause puncture wounds or lacerations and
carry a high risk of infection from oral bacterial flora, most com
monly Staphylococcus aureus and streptococci, and hepatitis vi-
rus." Hands, fingers, ears, nose, vagina, and penis are the most
common sites of human bites and are frequently a result of vio-
lence or sexual activity. Boxer’s fracture (fracture of the fourth or
fifth metacarpal) is often associated with an open wound when e
knuckles strike teeth. The human jaw has great crushing ab
causing laceration, puncture, crush injury, soft tissue tearing,
even amputation, More than 40 potential pathogens found in the
‘human mouth aceount for an infection rate of approximately 50%
in cases where vietims did not seek medical intervention within
24 hours of injury.
Collaborative Care. Initial treatment for animal and hu-
man bites includes cleaning with copious irrigation, debride-
ment, tetanus prophylaxis, and analgesies as needed. Prophylac-
tie antibiotics are used for animal and human bites at risk for
infection, such as wounds over joints, those greater than 6 0
12 hours old, puncture wounds, and bites of the hand or foot. In
dividuals at greatest risk of infection are infants, older adults,
immunosuppressed patients, aleoholics, diabetics, and people
taking corticosteroids
Puncture wounds ate left open, whereas lacerations are loosely
sutured. Wounds over joints are splinted, However, initial closure
is reserved only for facial wounds. The patient is admitted for IV
antibiotic therapy when an infection is present. There
creased incidence of cellulitis, osteomyelitis, and septic arthritis in
these patients. Animal and human bites must be reported to the
police in many states.
‘Consideration of rabies prophylaxis is an essential component in
‘management of animal bites. A neurotoxic virus found in the saliva
cof some mammals causes rabies. If untreated, the condition is fatal
in humans. Rabies exposure should be considered if an animal a
tack was not provoked, involved a wild animal, or involved ad
te animal not immunized agin abies, Rabies propyl “oo
"ways given when the animal eannot be found or & carnivorous W
‘animal causes the bite. An initial injection of rabies immune globu-
lin (RIG [BayRab)) to provide passive immunity starts the prophy~
Emergency and Disaster Nursing
1837
‘Acids and alkalis
+ Acios toiet bowel cleaner
antrust compounds
+ Akal: eran cleaners, cish-
‘washing detergents, ammonia
+ Aspien and asprin-containing
ragicatone
Bleaches
Carton monoxide
Cyanide
Ethylene alycol
Nonsteroidal antintlammatory
rugs
‘Teyolic antidepressants
(eg, amitripiyine (levi)
‘Alcohol, barbiturates,
benzodiazepines, cocaine,
hallucinogens, stimulants
saphoresis, nausea and vomiting
‘Phase 2: 24-28 h: right oper quadrant pan,
decreaced urine output, mined nausea,
Ute rise
‘Phase 3: 72-96 hr: nausea and vomiting,
‘malaise jaundice, hypoglycemia, enlarged iver,
possible coagulopathies, including DIC
Phase 4:7-8 days after ingestion: recover,
resoluon of symploms, LFTs return to normal
Excess salvation, dysphagia, epigastric pain, ne
‘mont; burns of mouth, esophagus, and
Tachyonea. tachycardia, hyperthermia, seizures pu-
monary edema, occult biesdinghemornage,
metaboie acidosis
Irtation of ips, mouth, and eyes. superical nur to
‘esophagus; chemeal pneumonia and pulmonary
era
Dyspnea, nesdache, tachypnea, contusion,
impaired judgment cyanosis, respiratory
epression
‘Almond oder to breath, neadache, dizziness,
nausea, confusion, hypertension. bradycardia
folowed by hypotension ard tachycardia
tachypnea folowod by bradypnea and respiratory
‘Sweet aromatic odor to breath, nausea and vom
ing, sured speech, ataia,lthargy, respiratory
depression
Vomiting (often bloody), dlarhea (atten blood,
{ever hypargyeema Isthargy, hypotension,
Gastroenteritis, abdominal pain, drowsiness,
nystagmus, hepatic and eral damage
In low doses: anticholinergic eftects, agitation
hypertension, tachycardia; in high doses: central
‘nervous systom depression, dysthythmias,
Inypotension, respiratory depression
See Cnapter 12
ison Manifestations: Treatment
cause vomiting IV form avalabie on expermertal
basis)
Immediate dition water, mk), corticosteroids (or akal
‘bus nduced vomiting contraindicated
Gastrc lavage, activated charcoal, une akalnizatio,
hemodiays for severe acute ingestion, tation
‘and mechanical ventilation, supportive care
Washing of exposed skin and eyes, ction wth water
‘and milk. gastric lavage, prevention of vomiting and
aspicton
Removal from source, administration of 19086 O; via
ror-tebreather mass, BVM. or intubation ac
‘mechanical venation. consider nyperbare oxygen
therapy
“Amy ntrate (asa) IV soclum nitrate, NV sodium
thiosulfate, supportive care
Gastic lavage, activated charcoal, supportive care
asin avage, chelation therapy (seleroxamne
[Pesteral)
GGastic lavage, actvated charcoal, supportive care
Muldose activated charcoal, gastric lavage, serum
‘akanzation wih sodium bicarbonate, intubation and
mechanical ventiation.suppertve care: never induce
vomtng
‘Soe Chapter 12
AVM, Bag valve mask, DIC. diemaicd avascular
Iaxis regimen. This is followed by a series of five injections of ho:
‘man diploid cell vaccine (HDCV [RabAvert}) on days 0, 3. 7. M4
and 28 t0 provide active immunity. Dosage is based on the patients
‘weight. (Rabies is discussed in Chapter 57.)
POISONINGS
Severity of the poisoning depends on type, concentration, and
route of exposure, Toxins can affect every tissue of the body, $0
‘symptoms can be seen in any bexly system. Specific management of
absorption, enhancing
implementation of toxin-specic interventions. The local poison
control center is available 24 hours a day and should be consulted
for the most current treatment protocols for specific poisons
‘Options for decreasing absorption of poisons include gastric la
vag, dermal cleansis
activated charcoal, ig. and eye strigation
Gastric lavage involves oral in
re ofa large-diameter (36- 10
42-French) gastric tube for installation of copious amounts of
Tine, The head of the bed should be elevated or the patient placed
‘om the side to prevent aspiration, Patients with an altered level of
‘consciousness or diminished gag reflex must be intubated before
lavage. Lav
is contraindicated in patients who in
{s, co-ingested sharp objects, or ingested nontoxic substances,
sed caustic
Seetion 12 Nursing Care in Specialized Settings
Gastric lavage must be performed within 2 hours of ingestion of
most poisons to be effective.” Problems associated with lavage
include epistaxis, esophageal perforation, and aspiration
The most effective intervention for management of poisonings
is administration of activated charcoal orally or via a gastric tube
‘within 60 minutes of poison ingestion." Many toxins adhere to
charcoal and are excreted through the GI tract rather than absorbed
into the circulation. Activated charcoal does not absorb ethanol
hydrocarbons, alkali, ion, boric acid, lithium, methanol. or cya
nde, Adults receive 50 to 100g of charcoal. For some toxins (e,
‘Phenobarital) muliple-dose chareoal may be required." Con:
sto charcoal administration include diminished bowel
gestion of substance poorly absorbed by
Charcoal can absorb and neutralize antidotes (e-.,
Neacetyleysteine [Mucomyst} for acetaminophen toxicity) and
these should not be given immediately before, with, o shortly
charcoal.»
‘Skin and ocular decontamination involves removal of toxins
from eyes and skin using copious amounts of water or saline. With
the exception of mustard gas, most toxins can be saely removed
with water or saline. Water mixes with mustard gas and releases
chlorine gas. AS a general rule, dry substances should be brushed
from the skin and clothing before water is used. Powdered ime
should not be removed with water: it should just be brushed off.
Personal protective equipment (e.g, gloves. gowns, goggles. esp
rators) should be wor for decontamination to prevent secondary
exposure, Decontamination procedures are usually done by those
specially tained in hazardous material decontamination before the
patient arrives atthe hospital and again, atthe hospital, if neces-
sary. Decontamination takes priority over all interventions except
basic life-support techniques
Elimination of poisons is increased through administaion of
cathantics, whole-bowel irigation, hemodialysis, hemoperfusion,
urine alkalinization, chelating agents. and antidotes. Cathartcs.
such as sorbitol, are given together with the first dose of activated
charcoal 0 stimulate intestinal motility and increase elimination.
Multiple doses of cathartics should be avoided because of poten-
tilly fatal electrolyte abnormalities. Whole-bowi! ieigation is
controversial and involves. administration of a nonabsorbable
bowel evacu . GoLYTELY). The solution is ad-
ministered every 4 10 6 hours until stools are clear. Ths process
cam be effective for swallowed objects such as eocaine-filled bal-
loons or eondoms, and heavy metals suchas lead and mercury
‘There isa high risk of electrolyte imbalance due to fluid and elec
trolyte losses with this procedure."
Hemosialysis and hemoperfusion are reserved for patients who
develop severe acidosis from ingestion of toxic substances (ez.
aspirin). Other interventions include alkalinization and chelation
therapy. Sodium bicarbonate administration raises the pH (greater
than 7.5), which is particularly effective for phenobarbital and
salicylate poisoning. Vitamin C may be added to 1V fluids to en
hance excretion of amphetamines and quinidine. Chelation therapy
‘may be considered for heavy metal poisoning (e.g. edetate cal
cium disodium (Calcium EDTA] for lead poisoning). A limited
‘number of true antidotes are available, and many’ ofthese agents
are themselves toxic.°
Education for toxic emergencies focuses on how the poisoning
‘occurred. Patients who experience poisoning because ofa suicide
attempt of related to substance abuse should be evaluated by a
‘mental health counselor and then referred for alcohol or drug de
tonification or scheduled for follow-up with a mental health pr-
traindicati
sounds, ileus, and
charcoal
solution (¢
fessional. The Occupational Safety and Health Administration
should isoning related to an occupational hay
aluate all po
VIOLENCE @
Violence is the acting out of the emotions of fear and/or anger 0
‘cause harm fo someone oF something. It may be the result of or
ganic disease (e-g., temporal lobe epilepsy). psychosis (e..
Schizophrenia), ot antisocial behavior (e.g., assault, homicide).
‘The patient cared for in the ED may be the vietim of violence or
the perpetrator of violence. Violence can take place in a variety of
settings, including the home, community, and workplace. EDs
have been identified as high-risk areas for workplace violence."
Measures to protect staf include the use of on-site security person-
nel and police officers, metal detectors, surveillance cameras, and
locked access doors. Research has shown that ED nurses believe
‘many of these measures are inadequate, making them vulnerable
to violence at work. Comprehensive workplace violence preven
tion plans should be implemented and evaluated in every ED.”
Domestic violence is a patter of coercive behavior in a rela.
tionship that involves fear, humiliation, intimidation, neglect, and
or intentional physical, emotional, financial, or sexual injury (see
Chapter 54 for information on
is found in all professions, cultures, socioeconomic groups. age
groups, and genders. Although men can be vietims of domesti vi
lence, most victims are women, chikdren, and the elderly. It has
bbcen reported that 1.5 million women and 834,000 men treated at
EDs have been battered (assaulted) by spouses, significant others,
or individuals known to them. As many as 20% of battered females
are pregnant at the time of the assault."
ED nurses are well situated to conduct domestic viol
screening (e.g., Do you feel safe at home’ Are you being hurt
anyone?), and routine screening for this risk factor is required
Bartiers to conducting effective screening include limited privacy
for screening, lack of time, and lack of knowledge about how to
‘obtain information regarding domestic violence. The development
and implementation of specific policies, procedures, and staf edu
cation programs can improve the domestic violence screening
practices of ED staff." For any patient who is found to be a victim
of abuse, appropriate interventions such as making referrals, pro:
viding emotional support, and informing vietims about their op-
tions (e., safe house, legal rights) should be initiated." See Re
sources at the end of this chapter for additional information on
domestic violence,
AGENTS OF TERRORISM
‘The threat of terrorism is an ongoing concern Terrorism involves
‘overt actions such as the dispensing of disease pathogens (... bh
terrorism) or other agents (e.g. chemical, radiologicinuclear, ex
plosive devices) as weapons for the express purpose of causing
harm. Prompt recognition and identification of potential health haz
ards are essential in the preparedness of health care professionals.
Table 69-13 summarizes general information regarding bio:
logic agents of terrorism. The pathogens most likely to be used in
4 bioterrorist attack are anthrax, smallpox, botulism, plague, tu
remia, and hemorrhagic fever.
‘Among the agents considered likely 10 be biologic weapog
those hat ase ata, pag and tlre out be <@®
fectively with commercially available antibioties if sufficient sl
exual assault), Domestic violence
plies were available and the organisms were not resistant. Smallpox
cean be prevented or ameliorated by vaccination even when first
given after exposure, Botulism can be treated with antitoxin, There
TABLE 69-13
Clinical
Chapter 69
Transmissibility
Emergency and Disaster Nursin
eed
Treatment
Gas
“Anthrax
Bacius antracis
Inhalation
Bacteral spores multiply nthe
Toxins cause hemorhage and
estructon of ung tissue
High morality rate
Cutaneous
195% of antivax infectons
Least lethal orm
‘Spores enter skin through cuts
or abrasions |
Handling of contaminated animal
skin products
“Toxins destroy surounding tissue
sstrointestinal
Ingestion of contaminated,
undercooked meat
Intestinal lesions in leur or
[cute inflammation of intestines
Smallpox
Varola major and minor viuses
Unite States ended routine
vaccination in 1971
Global eradication declare in
1080
Botulism
Clostiaium botulinum
‘Spote-orming anaerobe
Found in si
Seven diferent toxins
Lethal bacterial neurotoxin
Can de within 24 nr
Incubation period 1-2 days to 6 wie
Abrupt onset
Dyspnea
Diaphoress
Fever
Coogh
Chest pain
Septicemia
Shock
Meningitis
Respratory tature
\Weened meciastium (seen on chest
xray)
Incubation period: up to 12 days
‘Small papule resembles an sect bite
Advances o a depressed, black ulcer
‘Swollan lymph noes in achacent
Esema
Nausea,
Vomiting
Hematemesis
Diariea
‘Abdominal pain
Ascites
Sepsis
Incubation period: 717 days
Suaiden onset of symptoms.
Fever
Headache
Myalia
Lesions that progress from macules
to papules to pustular vesicles
Malaise
Back pain
Incubation period: 12-36 he
Abdominal cramps
Darthea
Nausea
Yomting
Cranial nerve palsies (noni,
dysarthria dyschona, dysphagia)
‘Skeletal muscle paras
Respratorytalure
+ No person-to-person
spread
+ Found i nature ane
‘most commonly infects
wid and domestic:
hooted anmats
+ Spread through direct
‘contact with bacteria
‘and its spores
+ Spores are dormant
‘encapsulated bactora
that become active when
they enter a tving host
+ Hany contagious
* Direct person-to-person
spread
+ Transmited in air
roplets
+ Transmit by handing
contaminated matenaie
+ Spread through ai or
food
+ No person-to-person
spread
+ improperly canned foods
+ Contaminated wound
Antibiotes prevent systamic
rmantostations
Ectve only # woated early
Giprotoxacn (Cipro) s the
treatment of choice
Penciin
Doxyeyetine
Pstexoosure prophylaxis fr
30 days i vaccine avaiable) or
{60 days it vaccine rot
‘avalabe)
Vaceie has limite aval
No known cure
Cidotovir istic) under testing
Isolation fr containment
Vecine avaiable fr tose
exposed
Vaccinia immune globulin (VI)
valatie
Incuce vornting
Enemas
Antonin
Mechanical vetiation
No vaccine avaiable
Toon can be inactivated by
eating food eins to
212° F (100° Cora east
10min
nts of terrorism and are eat
e@ established treatment for viruses that cause hemorrhagic
FChemicals may also be used as
egorized according to their
get organ or effect
(Table 69-14),
For example, sarin isa highly toxie nerve gas that can eause death
‘within minutes of exposure. Itenters the body through the eyes and
skin and acts by paralyzing the respiratory muscles, Antidotes f
nerve agent poisoning include atropine (AwoPen) and pralidoxime
chloride (2-PAM chloride), Multiple doses may be nceded to re
verse the effects of the nerve
1s notmally used in chemical manu
‘enough pe-
Phosgene is a colorless
facturing. If inhaled at h
th concentrations for a Jon
1840
Section 12
Nursing Care in Specialized Settings
Taste 69-15 |[EVen eee
Clinical
jifestations
Pathogen and Description
fague
Yersia pestis + noubaton period: 2-8 days
+ Bactera found in rodents and Hemoptysss
fleas + Cough
Forms + High fever
+ Bubonic (most common) + hits
+ Preumonic| + Myagia
+ Septicamic (most deadly) + Headache
+ Respiratory faire
Lyman nede sweling
Tularemia
Franeisaletlarensic + Incubation period: 3-10 days
+ "Bacteral infectious disease of + Sudden onset
animais + Fever
+ Mortality rate about 35% + Swollen lymph nodes
vithout treatment + Fatigue
+ Sor throat
+ Weight oss
+ Preumonia|
+ Pleural fusion
* Urcerat sore fom tik bite
Hemorthagic Fever
+ Caused by several veuses,
including Marburg, Lassa, Junin,
tnd Ebola
+ Ebola vies
Fever
Conjunctivitis
Headache
fe threatening Malaise
of teaues and organs
Verting
Hypotension
Organ faire
7
eke ak uk eed
Transmissibility
a )
+ Direct person-to-person + Antibiotics only effective if
spread administered immediately
+ Tranamitted through flea Drug of choice: streptomycin
bites gentamicin
+ Ingeition of contams-—*‘Vaccine under development
ated meat + Hospitaization
+ goltion fr containment
+ No person-to-person «+ Gentamicin treatmant of choice
soread + Streptomycin, oxyeyctne. and
+ Aerosol or intradormal Ceprofloracin are alternatives
route “+ Vaccine in development stage
*+ Spread by rabbits and
tks
+ Contaminated food, a,
water
+ Carried by rodents and
mosquitoes
+ Direct person-to-person
spread by body fuids
+ Vins can be aerosolized
‘No intramuscular injections
No antiplatelet drugs
Isolation for containment
Fibavrin (Virazole)efctve in
+ No known treatment available
GF (cyciohexyimettvphosphonofluordate)
VX (Oretry S-2-disopropylaminoety/}
‘methylphosphenothiolto)
Nerve ~ Blood Pulmonary Blister/Vesicants
ae) itycrogen cyanide Phosgene Iiropen end sur mustard
Tabun thy NN-cimetyipnoephoramidoeyanidte) Cyanogen chonde Clore Lew an alate arsenic compounds
Soman fonacoh! may phosphonate) Vi chide 2-chirouyioroarine)
Phosgene oxime
riod, it causes severe respiratory distress, pulmonary edema, and
‘death, Mustard gas is yellow to brown in color and has a garlic-ike
‘odor. The gas irritates the eyes and causes skin burns and blisters
Protocols to treat casualties of chemical exposure are varied and
relate to the specific agent.”
Radiologic/nuelear agents represent another cat
of terrorism. Radiologic dispersal devices (RDS), also known as
“dirty bombs," consist ofa mix of explosives and radioactive mate
rial (eg, pellets). When the deviee is detonated, the blast scatters
radioactive dust, smoke, and other material into the surrounding
‘environment, resulting in radioactive contamination
The main danger from an RRD results from the explosion,
which can cause serious injuries to the casualties. The radioactive
materials used in an RRD (c.g. uranium, fodine-131) do not usu:
ally generate enough radiation to cause immediate serious illness,
‘except to those casualties who are in close proximity to the explo-
ory of agents
sion, However, the radioactive dust and smoke can spread) and
‘cause illness if inhaled. Since radiation cannot be seen, smelled,
felt, or tasted, measures to limit contamination (e-g., covering the
patient's nose and mouth) and decontamination (e.g., shower)
should be initiated!
Ionizing radiation, such as that from a nuclear bomb or damage
{0 a nuclear reactor, represents a serious threat to the safety ofthe
casualties and the environment, Exposure to ionizing radiation
may or may not include skin contamination with radioactive mate-
rial, F external radioactive contaminants are present, devontamina
tion procedures must be initiated immediately, Acute radiation
syndrome develops after a substantial exposure to jonizing @
tion and follows a predictable pattern (Table 69-15)
Explosive devices (eg, TNT, dynamite) that are used as age
‘of terrorism result in one oF more of te following types of injuries:
blast erush, oF penetrating. Blast injuries result from the super
ene
Whole Body Radiation from External Radiation or internal Absorption
Phase of Sublethal Range Lethal Range
Syndrome Feature 0-100 rad 100-200 rad «200-600 rad__—«600-800 rad «600-3000 rad >3000 rad
Prodromal phase Nausea, vomiting ‘None 96-50% 50%-1009% 759%6-1009% 9096-1009% 100%
Time of onast 36h 2a tan =the Mires
Durston 26h <28 he 48 he =48 he NA
Lymphocyte count Unatfacted Mirimaly decreased 1000 at 24 nv 500 at 24h Decreases within Decreases within
ours ours
CONS funtion No impairment No impairment Cogntive impairment Cognitive mparment api incapactation, often aera lucid period
Yor 6-20 for 24h of upto soveal bows
Latent phase ‘sence of >owk 718 98 0-7 days 02 days Nene
(eubotnica) ‘meters
‘Acute radiation + Signs and symptoms None Moderate lkoperia Severe laukopena, purpura, hemormnage Diartea Convusios, sax,
‘ness or *mani- Preumonia Fover ‘roman thay a
fest ness” Hair oos ater 200 rad Erctrohjte &
hase lsturbance
Time of onaat >2 wk 2ays-2 wk 19.daye
Crtical pero Nene 4-6 wk—Mest potential for effective medical 2-14 days 1-48 he a
inteventon g
Organ systom None Homatopolee and respiratory (mucosa) Glract ons
‘ystems Mucosal systems g
Hospitalization 3 o%
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Fdocuments - Us - Microscada Pro Sys 600 9 Abb LTD 10 Microscada Pro 1mrs756118 Operation ManualDocument182 pagesFdocuments - Us - Microscada Pro Sys 600 9 Abb LTD 10 Microscada Pro 1mrs756118 Operation ManualchupzptNo ratings yet
- ABBVU-PGGA-36052 ABB SoftwareVulnerabilityHandlingAdvisory SYS600 SentinelHASPDocument5 pagesABBVU-PGGA-36052 ABB SoftwareVulnerabilityHandlingAdvisory SYS600 SentinelHASPchupzptNo ratings yet
- Ieee Recommended Practice For Network Communication in ElectricDocument140 pagesIeee Recommended Practice For Network Communication in ElectricchupzptNo ratings yet
- Challenges IEC 61850 Substation CommissioningDocument7 pagesChallenges IEC 61850 Substation CommissioningchupzptNo ratings yet
- SPAA 120 C and SPAA 121 C Feeder Protection Relay: User S Manual and Technical DescriptionDocument76 pagesSPAA 120 C and SPAA 121 C Feeder Protection Relay: User S Manual and Technical DescriptionchupzptNo ratings yet
- Spacom ModulesDocument5 pagesSpacom ModuleschupzptNo ratings yet
- ABB IS2 SwitchboardDocument308 pagesABB IS2 SwitchboardchupzptNo ratings yet
- IEEE and IEC StandardsDocument11 pagesIEEE and IEC StandardschupzptNo ratings yet