Professional Documents
Culture Documents
Gardner H Witnsessed Short Fall Mimicking Sbs Peds Neurosurg 2007 43 433-351
Gardner H Witnsessed Short Fall Mimicking Sbs Peds Neurosurg 2007 43 433-351
Uploaded by
api-289577018Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gardner H Witnsessed Short Fall Mimicking Sbs Peds Neurosurg 2007 43 433-351
Gardner H Witnsessed Short Fall Mimicking Sbs Peds Neurosurg 2007 43 433-351
Uploaded by
api-289577018Copyright:
Available Formats
Case Report
Pediatr Neurosurg 2007;43:433435
DOI: 10.1159/000106399
Received: March 15, 2005
Accepted after revision: May 17, 2007
A Witnessed Short Fall Mimicking
Presumed Shaken Baby Syndrome
(Inflicted Childhood Neurotrauma)1
Horace B. Gardner
Manitou Springs, Colo., USA
Key Words
Shaken baby syndrome Inflicted childhood neurotrauma
Fall Trauma Subdural hematoma Retinal hemorrhage
Abstract
A witnessed fall backwards of an infant from a sitting position resulted in the subdural hematoma and retinal hemorrhages characteristic of presumed shaken baby syndrome.
Violent shaking is not necessary to produce these findings.
Copyright 2007 S. Karger AG, Basel
An 11-month-old Asian infant was witnessed by a 5year-old sibling to fall backwards from a sitting position,
the head striking a carpeted floor. The infant immediately cried, vomited and exhibited some seizure-like activity including tongue biting and curling in of the right
hand. The infant was seen within the hour by the emergency room physician, who noted hypertonicity, gaze deviated to the left and responsiveness to noxious stimuli.
Three hours later a large acute left frontal temporoparietal subdural hematoma was removed surgically. Although the preoperative CT scan was read as an acute on
1
As mentioned in the Editorial, this article should be read in conjunction with the other two papers dealing with child abuse.
2007 S. Karger AG, Basel
10162291/07/04350433$23.50/0
Fax +41 61 306 12 34
E-Mail karger@karger.ch
www.karger.com
Accessible online at:
www.karger.com/pne
chronic subdural hematoma with no hydrocephalus,
both the operating surgeon and a second pediatric neurosurgeon asked for a second opinion, felt the subarachnoid spaces were enlarged, consistent with benign external hydrocephalus, and only fresh blood was noted at surgery. Thirty-one hours after the fall, an ophthalmologic
exam by a pediatric ophthalmologist revealed diffuse
pre-/intraretinal hemorrhages, mostly posterior pole,
with a fundus drawing depicting multiple hemorrhages.
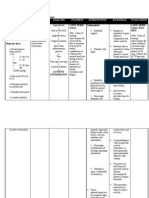
One week later, repeat ophthalmologic exam by the same
examiner noted 4 quadrants of bilateral pre- and intraretinal dot, flame-shaped and white-centered hemorrhages OU hemorrhages extend beyond equator difficult to ascertain whether they extend to ora serrata
(fig. 1 and 2). No disc edema was recorded on both exams. In deposition, the hemorrhages were mentioned to
be at different levels (also stated as multiple layers) that
extend to periphery. The infant did well following the
surgery and was returned to the parents. Further history
revealed 2 previous falls while learning to stand, a common occurrence in this age group.
Due to the presence of both intracranial and intraocular hemorrhage, abuse was suspected and a skeletal survey done, which was normal. Referral to social services
found the family to be a stable one. The witness gave the
same description of the fall to the mother in the mothers
native language and to 2 separate social workers (first on
the day of the incident and then 2 days later) in English,
Horace B. Gardner, MD
318 Oklahoma Road
Manitou Springs, CO 80829 (USA)
Tel./Fax +1 719 685 9143
E-Mail horacebgardner@yahoo.com
Fig. 1. Fundus drawing, right eye, 7 days after surgery. + is the
fovea, dots represent intraretinal hemorrhages, short lines represent flame-shaped hemorrhages, circles represent superficial (pre
or sub internal limiting membrane) hemorrhages and double circles white centered hemorrhages.
Fig. 2. Fundus drawing, left eye, 7 days after surgery. For explanation of symbols please see legend of fig. 1.
even reenacting the fall with a stuffed animal, showing it
to be a fall backwards from a sitting position with the
child striking the occiput. Of 5 treating physicians, 3
agreed this was accidental trauma consistent with the
history (the operating neurosurgeon, a neurologist and
the ICU pediatrician), while 2 felt it was non-accidental
(a pediatrician and the pediatric ophthalmologist) and
the court dismissed all charges. The child is doing well
over 2 years following the surgery.
Pittman [1] has noted in the absence of other evidence
of inflicted injury, the presence of a subdural hematoma
in a child with external hydrocephalus is, by itself, insufficient to prove abuse. Although Piatt [2] has cautioned
(also in the setting of external hydrocephalus) retinal
hemorrhage may not be pathognomonic of abusive injury, ocular findings are often accepted as such other evidence. This is based on a shearing theory with eye and
brain findings being independent evidence of trauma
with infants only suffering from the ocular findings of
retinal hemorrhage, retinoschisis and perimacular retinal folds if they have been violently shaken. However, if
the ocular findings can occur without such shaking, indeed if they may be secondary to the intracranial pathology, they are of no value in determining etiology.
The combination of intracranial bleeding and intraocular hemorrhaging has been noted to occur with wit-
nessed short falls, including one recorded on videotape
[3] and with massive head injury without acceleration/deceleration [4], the latter case including retinoschisis and
perimacular folds, findings promulgated as even more
diagnostic of shaking. The description of the fall and subsequent clinical course in this case are remarkably similar to the 3 cases of the 26 described by Aoki and Masuzawa [5], where an occipital impact after a fall backwards
from a sitting position was followed shortly by generalized tonic convulsive activity.
External hydrocephalus is unlikely to have existed in
all 40 Japanese cases under the age of 2 reported by Aoki
and Masuzawa [5] and Ikeda et al. [6] as well as the cases witnessed by Lantz et al. [4] and Plunkett [3]. It was
thought to be present in this case by the operating surgeon and by a pediatric neurosurgeon asked for a second
opinion but was said not to be present by the radiologist.
Unless and until the ocular findings of presumed shaken baby syndrome are shown to occur with and only
with severe ocular shaking, they should not be considered independent evidence of abuse in cases of subdural
hemorrhage in infants nor pathognomonic of such
abuse.
434
Pediatr Neurosurg 2007;43:433435
Gardner
References
Fall Mimicking Shaken Baby Syndrome
1 Pittman T: Significance of a subdural hematoma in a child with external hydrocephalus.
Pediatr Neurosurg 2003;39:5759.
2 Piatt JH Jr: A pitfall in the diagnosis of child
abuse: external hydrocephalus, subdural hematoma and retinal hemorrhages. Neurosurg Focus 1999;7:e4.
3 Plunkett J: Fatal pediatric head injuries
caused by short-distance falls. Am J Forens
Med Pathol 2001; 22:112.
4 Lantz PE, Sinal SH, Stanton CH, Weaver RG
Jr: Perimacular retinal folds from childhood
head trauma. BMJ 2004;328:754756.
5 Aoki N, Masuzawa H: Infantile acute subdural hematoma. J Neurosurg 1984; 61: 273
280.
6 Ikeda A, Sato O, Tsugane R, Shibuya N,
Yamamoto I, Shimoda M: Infantile acute
subdural hematoma. Childs Nerv Syst 1987;
3:1922.
Pediatr Neurosurg 2007;43:433435
435
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- SSRN Id2483551Document42 pagesSSRN Id2483551api-289577018No ratings yet
- نماذج اسئلة طب اسنان 1Document5 pagesنماذج اسئلة طب اسنان 1hm90No ratings yet
- SSRN Id2627324Document11 pagesSSRN Id2627324api-289577018No ratings yet
- SSRN Id2544367Document31 pagesSSRN Id2544367api-289577018No ratings yet
- SSRN Id2606419Document42 pagesSSRN Id2606419api-289577018No ratings yet
- 216 FTPDocument8 pages216 FTPapi-289577018No ratings yet
- Are The Symptoms of Serious Infant Head Injury Always Immediate? (No)Document8 pagesAre The Symptoms of Serious Infant Head Injury Always Immediate? (No)api-289577018No ratings yet
- CMR 1510975 20140416Document3 pagesCMR 1510975 20140416api-289577018No ratings yet
- InnisDocument6 pagesInnisapi-289577018No ratings yet
- 2 FTPDocument3 pages2 FTPapi-289577018No ratings yet
- Shaken Baby Syndrome or Scurvy?: C. Alan B. Clemetson, M.DDocument4 pagesShaken Baby Syndrome or Scurvy?: C. Alan B. Clemetson, M.Dapi-289577018No ratings yet
- Canmedaj00439 0082Document2 pagesCanmedaj00439 0082api-289577018No ratings yet
- Brmedj00111 0029aDocument1 pageBrmedj00111 0029aapi-289577018No ratings yet
- UpdatebrainimagingnaiDocument109 pagesUpdatebrainimagingnaiapi-289577018No ratings yet
- Advanced Hemodynamic Monitoring With Swan GanzDocument1 pageAdvanced Hemodynamic Monitoring With Swan GanzDr.Biswajit jenaNo ratings yet
- Trichuris Trichiura: Lecture By: Maha Gamal AldeinDocument20 pagesTrichuris Trichiura: Lecture By: Maha Gamal AldeinMohammad DweibNo ratings yet
- APA - The Risks of Social IsolationDocument10 pagesAPA - The Risks of Social IsolationnaiaradafneNo ratings yet
- Male InfertilityDocument75 pagesMale InfertilityArielle janaNo ratings yet
- Fda 1571Document2 pagesFda 1571Nitin KashyapNo ratings yet
- Approach To Thrombocytopenia: Dr. Ahmed Mahdy - Kbim - R4Document23 pagesApproach To Thrombocytopenia: Dr. Ahmed Mahdy - Kbim - R4Ahmed MahdyNo ratings yet
- Ultrasound-Guided Lumbar Central Neuraxial Block 2016Document8 pagesUltrasound-Guided Lumbar Central Neuraxial Block 2016drkis20100% (1)
- JPHMP s088-s094Document7 pagesJPHMP s088-s094HibibiNo ratings yet
- Face PresentationDocument29 pagesFace PresentationMadhu Bala100% (1)
- Redzi 100mgDocument2 pagesRedzi 100mgkashifNo ratings yet
- U2 - Online Lab: Blood PressureDocument15 pagesU2 - Online Lab: Blood PressureAmandaSherman89% (9)
- SuturingDocument3 pagesSuturingKiran RamloganNo ratings yet
- COVID-19: A Window of Opportunity For Positive Healthcare ReformsDocument4 pagesCOVID-19: A Window of Opportunity For Positive Healthcare ReformsTeuku Revandi Johas TRJNo ratings yet
- New England Journal Medicine: The ofDocument9 pagesNew England Journal Medicine: The ofLaura GutierrezNo ratings yet
- CMRF Form TelanaganaDocument1 pageCMRF Form Telanaganasrisai onlinecenter100% (3)
- Non Medical Prescribing Using The British National Formulary PDFDocument6 pagesNon Medical Prescribing Using The British National Formulary PDFRyan MwNo ratings yet
- NCP - Activity IntoleranceDocument2 pagesNCP - Activity IntolerancePaolo Belleza92% (12)
- Care of New Traumatic SCI Patients in JamaicaDocument32 pagesCare of New Traumatic SCI Patients in JamaicaRory DixonNo ratings yet
- Bleeding NCPDocument13 pagesBleeding NCPBiway Regala100% (1)
- ESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDocument5 pagesESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDini SuhardiniNo ratings yet
- Perception of Health Promotion in UnaniDocument5 pagesPerception of Health Promotion in UnaniShahid BukhariNo ratings yet
- FCM L1 - The Philippines Cancer Control Program (PCCP)Document7 pagesFCM L1 - The Philippines Cancer Control Program (PCCP)Jessa BidionesNo ratings yet
- MP 12430Document42 pagesMP 12430Mourya AnkurNo ratings yet
- Skin Tightening: Fotona 4D ProtocolDocument1 pageSkin Tightening: Fotona 4D ProtocolMichele CarvalhoNo ratings yet
- Kunj Sakit MeiDocument178 pagesKunj Sakit MeiParnart ChristineNo ratings yet
- Careplan Week2Document2 pagesCareplan Week2api-302138606No ratings yet
- Grand Rounds FinalDocument67 pagesGrand Rounds Finalapi-439712011No ratings yet
- What Is A Medical Coder?Document13 pagesWhat Is A Medical Coder?Udaai NairNo ratings yet
- Cancer NotesDocument5 pagesCancer NotesChesedel Jobien M. LimlinganNo ratings yet