Professional Documents
Culture Documents
Response From BCBSTX
Response From BCBSTX
Uploaded by
Houston ChronicleOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Response From BCBSTX
Response From BCBSTX
Uploaded by
Houston ChronicleCopyright:
Available Formats
Our behavioral health care team serves to help determine what coverage is provided for
the appropriate level of care and services for our members according to their benefits
plan. We start with a utilization review by a licensed behavioral health provider who can
authorize care or continuation of care. If it is believed that medical necessity for
continued care is no longer met, the case is reviewed by a specialty provider who may
continue to authorize the care or issue a denial if medical necessity for the level of care
is no longer met. If it is believed that medical necessity is no longer being met the
provider requesting the services is offered an opportunity for a peer to peer review prior
to a final medical necessity determination. The review may result in continued
authorization of care or denial if medical necessity is not met.
Please note that for cases involving psychiatric care, the review is done by a boardcertified psychiatrist. For care delivered by a non-psychiatric provider, review may be
done by a psychiatrist or licensed doctoral level psychologist.
In all cases involving an adverse determination the member or provider may request an
appeal that includes a review performed by a like specialty provider not previously
involved in reviewing this case. The review may result in an overturn of the denial with
continued authorization of care or in upholding the denial. In most cases if the denial
was upheld, a members' benefit plan may allow for a review by an independent review
organization (IRO) that involves a like specialty provider not affiliated with BCBSTX. The
determination made by the IRO is binding on the plan.
BCBSTX fully supports mental health parity and designs and implements all members'
benefits accordingly. Our Behavioral Health Division makes medical necessity
determinations in collaboration with the provider, the member and when appropriate,
their family support system. These decisions are based on multiple determinants,
including nationally recognized medical necessity level of care criteria and clinical
practice guidelines, severity of illness, treatment history and clinical response, and
support system at home."
Marina Angelica Coryat
Senior Manager, Media & Community Relations
Southeast Texas Region
You might also like
- Printable 2024 March Madness NCAA Men's Basketball Tournament BracketDocument1 pagePrintable 2024 March Madness NCAA Men's Basketball Tournament BracketHouston Chronicle100% (1)
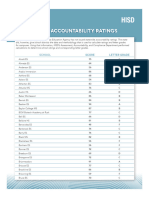
- HISD 2023 School Accountability RatingsDocument10 pagesHISD 2023 School Accountability RatingsHouston ChronicleNo ratings yet
- Collaborative Practice AgreementDocument3 pagesCollaborative Practice Agreementapi-228554702No ratings yet
- New Freedom Ops LLC Iop P&PDocument51 pagesNew Freedom Ops LLC Iop P&Pmike iovinoNo ratings yet
- Professional Disclosure StatementDocument2 pagesProfessional Disclosure Statementapi-253915117100% (2)
- ASI Treatment Planning ManualDocument22 pagesASI Treatment Planning Manualdrmss100% (1)
- Housecalls 101: Policy and Procedure Manual for Medical Home VisitsFrom EverandHousecalls 101: Policy and Procedure Manual for Medical Home VisitsNo ratings yet
- Printed From The Texas Medical Association Web SiteDocument6 pagesPrinted From The Texas Medical Association Web Sitepaulrich_chanNo ratings yet
- AAMFT Code of Ethics PDFDocument10 pagesAAMFT Code of Ethics PDFHec ChavezNo ratings yet
- Mental Health Services ICN903195Document20 pagesMental Health Services ICN903195noxinqwertyNo ratings yet
- SW 4441 Anika Davis Field Placement Setting PaperDocument7 pagesSW 4441 Anika Davis Field Placement Setting Paperapi-282542988100% (1)
- Complementary Alternative ModalitiesDocument5 pagesComplementary Alternative ModalitiesRinal BaradNo ratings yet
- Advanced Nurse Practitioners: Nurse Practitioner Scope of PracticeDocument9 pagesAdvanced Nurse Practitioners: Nurse Practitioner Scope of Practicecelina deboralNo ratings yet
- LA CAID CertificationofNeedforPsychHospitalDocument3 pagesLA CAID CertificationofNeedforPsychHospitalbaricsamelindaNo ratings yet
- Chief Psychiatrist Discharge Planning PDFDocument8 pagesChief Psychiatrist Discharge Planning PDFMaddy HuckelNo ratings yet
- (TRX) HomeHealth-Intermediate-Clinical-Comprehensive Assessment-ScriptDocument3 pages(TRX) HomeHealth-Intermediate-Clinical-Comprehensive Assessment-ScriptsundayjabikemNo ratings yet
- What Is The Role of Regulatory Agencies in Continuous Quality ImprovementDocument14 pagesWhat Is The Role of Regulatory Agencies in Continuous Quality ImprovementJana-Tae KerrNo ratings yet
- Managed CareDocument5 pagesManaged CareMutia Poetry MandelaNo ratings yet
- Program DescriptionDocument17 pagesProgram DescriptionNichole KilbournNo ratings yet
- NewJersey06 12 Core FunctionsDocument11 pagesNewJersey06 12 Core FunctionsChinchusha T JanardhananNo ratings yet
- Standards, Challenges & Scope of Psychiatric Nursing Multi-Disciplinary Team & Role of NurseDocument66 pagesStandards, Challenges & Scope of Psychiatric Nursing Multi-Disciplinary Team & Role of NurseJoric MagusaraNo ratings yet
- Typeddsfd ConsentDocument12 pagesTypeddsfd ConsentNeil OsborneNo ratings yet
- Swbest Practices PDFDocument6 pagesSwbest Practices PDFMary Grace Dionisio-RodriguezNo ratings yet
- Palliative Care Needs Assessment GuidanceDocument13 pagesPalliative Care Needs Assessment GuidanceDedes SahpitraNo ratings yet
- PT As Patient Client ManagerDocument39 pagesPT As Patient Client Managerpihabo3594No ratings yet
- Prelim Exam 22Document2 pagesPrelim Exam 22Zgama AbdulrahmanNo ratings yet
- PTDischarge Planning Reminder FinalDocument2 pagesPTDischarge Planning Reminder Finalbesho 2013No ratings yet
- Untitled Document - Edited - 2023-07-21T000028.015Document5 pagesUntitled Document - Edited - 2023-07-21T000028.015Phillis MwangiNo ratings yet
- Professional Disclosure StatementDocument3 pagesProfessional Disclosure Statementapi-642170591No ratings yet
- Nursing Code of EthicsDocument2 pagesNursing Code of EthicsClarissa HeatonNo ratings yet
- Section 5 State Resources, Policy, and ReimbursementDocument5 pagesSection 5 State Resources, Policy, and ReimbursementAnne de AndradeNo ratings yet
- ABA Service AgreementDocument3 pagesABA Service AgreementEva BrownNo ratings yet
- Interact Treatment Manual & Participant Workbook: Based on the Self Help Theory of Jim MaclaineFrom EverandInteract Treatment Manual & Participant Workbook: Based on the Self Help Theory of Jim MaclaineNo ratings yet
- Locg MHConditionsDocument14 pagesLocg MHConditionshemedisafari840No ratings yet
- Best Interests DecisionDocument4 pagesBest Interests Decisiondknorsyafinaz pgadnanNo ratings yet
- Policies and Procedure ManualDocument4 pagesPolicies and Procedure ManualPrabha GuptaNo ratings yet
- Palliative Care Needs Assessment GuidanceDocument13 pagesPalliative Care Needs Assessment Guidancenovia100% (1)
- Ethical, Legal, and Economic Foundations of The Educational Process - BUGHAO, MARIA ANGELIKADocument4 pagesEthical, Legal, and Economic Foundations of The Educational Process - BUGHAO, MARIA ANGELIKAMaria Angelika BughaoNo ratings yet
- VITAL WorkLife Physician InterventionDocument2 pagesVITAL WorkLife Physician InterventionVITAL WorkLifeNo ratings yet
- The Safe & Effective Care EnvironmentDocument140 pagesThe Safe & Effective Care EnvironmentMoreiyamNo ratings yet
- Patient Self Determination Act: Mississippi Advance Health-Care DirectiveDocument17 pagesPatient Self Determination Act: Mississippi Advance Health-Care DirectiveKristin JonesNo ratings yet
- Nursing Care Plans (NCP) : Ultimate Guide and DatabaseDocument2 pagesNursing Care Plans (NCP) : Ultimate Guide and DatabaseRana AlaseeriNo ratings yet
- Chapter 3: Continuum of Care: Keltner: Psychiatric Nursing, 5 EditionDocument7 pagesChapter 3: Continuum of Care: Keltner: Psychiatric Nursing, 5 EditionWarrenPeaceNo ratings yet
- Professional Disclosure Statement 6 2016 For WeeblyDocument3 pagesProfessional Disclosure Statement 6 2016 For Weeblyapi-314123316No ratings yet
- TRICARE Behavioral Health Care ServicesDocument4 pagesTRICARE Behavioral Health Care ServicesMatthew X. HauserNo ratings yet
- ADCIP4CLBDocument7 pagesADCIP4CLBConsuelo BrownNo ratings yet
- Refusal of Treatment: 6.1. Can A Patient Refuse Treatment?Document8 pagesRefusal of Treatment: 6.1. Can A Patient Refuse Treatment?Joe SoNo ratings yet
- Clinical Teaching ON Geriatric AssessmentDocument9 pagesClinical Teaching ON Geriatric AssessmentANITTA SNo ratings yet
- Case StudyDocument5 pagesCase StudyShairuz Caesar Briones DugayNo ratings yet
- AccreditationDocument57 pagesAccreditationSara AlfyNo ratings yet
- Referrals 2016 PDFDocument24 pagesReferrals 2016 PDFTim BautistaNo ratings yet
- JciDocument5 pagesJcialfredsamuelNo ratings yet
- AHP - Family Nurse PractitionerDocument6 pagesAHP - Family Nurse PractitionerMaria Fudji HastutiNo ratings yet
- Minimising The Use of Restrictive PracticesDocument4 pagesMinimising The Use of Restrictive PracticesEicis HizonNo ratings yet
- Implementation ProcessDocument28 pagesImplementation ProcessREVATHI H KNo ratings yet
- NHS CHC Public Information Leaflet FinalDocument16 pagesNHS CHC Public Information Leaflet FinalSlowfingerNo ratings yet
- A Brief OverviewDocument10 pagesA Brief Overviewphat lippNo ratings yet
- PD DHS Clinic Nurse ConsultantDocument5 pagesPD DHS Clinic Nurse ConsultantHarjotBrarNo ratings yet
- Gail Carlson, MPH PH.D, State Health Education Specialist, University of Missouri ExtensionDocument9 pagesGail Carlson, MPH PH.D, State Health Education Specialist, University of Missouri ExtensionRahmat ShahNo ratings yet
- Aod Client HandbookDocument35 pagesAod Client HandbookkwonjuNo ratings yet
- Full SC Training SlidesDocument151 pagesFull SC Training Slidesapi-737922285No ratings yet
- Overview of The Health AssessmentDocument4 pagesOverview of The Health AssessmentDharyn KhaiNo ratings yet
- Final Limited IEQ & Lead in Drinking Water Report-Various HISD Education FacilitiesDocument18 pagesFinal Limited IEQ & Lead in Drinking Water Report-Various HISD Education FacilitiesHouston ChronicleNo ratings yet
- R4 Tee TimesDocument2 pagesR4 Tee TimesHouston ChronicleNo ratings yet
- NCAA Women's BracketDocument1 pageNCAA Women's BracketHouston Chronicle100% (1)
- 2567 UMMC Inspection 1-8-21Document72 pages2567 UMMC Inspection 1-8-21Houston ChronicleNo ratings yet
- NFL Statement On Denzel PerrymanDocument1 pageNFL Statement On Denzel PerrymanHouston ChronicleNo ratings yet
- 2024 2025 Proficiency Screening Teachers 20 Feb 2024Document31 pages2024 2025 Proficiency Screening Teachers 20 Feb 2024Houston ChronicleNo ratings yet
- Rachel Hooper InvoicesDocument35 pagesRachel Hooper InvoicesHouston ChronicleNo ratings yet
- Houston Astros 2024 Spring Training RosterDocument1 pageHouston Astros 2024 Spring Training RosterHouston Chronicle100% (1)
- UH Football Depth Chart Vs UTSADocument1 pageUH Football Depth Chart Vs UTSAHouston ChronicleNo ratings yet
- Media Release For Free and Reduced-Price MealsDocument2 pagesMedia Release For Free and Reduced-Price MealsHouston ChronicleNo ratings yet
- Ltr. Re - City Is Granted Governmental ImmunityDocument1 pageLtr. Re - City Is Granted Governmental ImmunityHouston ChronicleNo ratings yet
- Ed Anderson TranscriptDocument53 pagesEd Anderson TranscriptHouston ChronicleNo ratings yet
- Full Statement From Rep. Sheila Jackson LeeDocument1 pageFull Statement From Rep. Sheila Jackson LeeHouston ChronicleNo ratings yet
- HISD Special Education Action PlanDocument4 pagesHISD Special Education Action PlanHouston ChronicleNo ratings yet
- Astroworld Redacted FinalDocument1,266 pagesAstroworld Redacted FinalHouston Chronicle100% (2)
- 2023 Shriners Children's Charleston Classic BracketDocument1 page2023 Shriners Children's Charleston Classic BracketHouston ChronicleNo ratings yet
- 2567 UMMC 12-17 Through 12-21-21Document97 pages2567 UMMC 12-17 Through 12-21-21Houston ChronicleNo ratings yet
- 2023 Preseason All-Big 12 Football TeamDocument1 page2023 Preseason All-Big 12 Football TeamHouston ChronicleNo ratings yet
- TDECU Stadium Pricing MapDocument1 pageTDECU Stadium Pricing MapHouston ChronicleNo ratings yet
- Astroworld Tragedy Final Report (Redacted)Document1,266 pagesAstroworld Tragedy Final Report (Redacted)Houston ChronicleNo ratings yet
- Hecht Dissent On Crane vs. McLaneDocument16 pagesHecht Dissent On Crane vs. McLaneHouston ChronicleNo ratings yet
- Blacklock Dissent On Crane vs. McLaneDocument4 pagesBlacklock Dissent On Crane vs. McLaneHouston ChronicleNo ratings yet
- HISD Board of Managers ApplicantsDocument4 pagesHISD Board of Managers ApplicantsHouston Chronicle100% (1)
- 2023 NCAA Tournament BracketDocument1 page2023 NCAA Tournament BracketHouston Chronicle100% (1)
- FB23 TDECU Stadium Pricing MapDocument1 pageFB23 TDECU Stadium Pricing MapHouston ChronicleNo ratings yet
- Houston Astros 2023 Spring Training ScheduleDocument1 pageHouston Astros 2023 Spring Training ScheduleHouston ChronicleNo ratings yet
- Davis EmailDocument3 pagesDavis EmailHouston ChronicleNo ratings yet
- Houston Astros Preliminary 2023 Spring Training RosterDocument1 pageHouston Astros Preliminary 2023 Spring Training RosterHouston ChronicleNo ratings yet