Professional Documents
Culture Documents
Treatment of Vaginal Candidiasis For The Prevention of Preterm Birth A Systematic Review and Meta-Analysis
Treatment of Vaginal Candidiasis For The Prevention of Preterm Birth A Systematic Review and Meta-Analysis
Uploaded by
wennnykOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Treatment of Vaginal Candidiasis For The Prevention of Preterm Birth A Systematic Review and Meta-Analysis
Treatment of Vaginal Candidiasis For The Prevention of Preterm Birth A Systematic Review and Meta-Analysis
Uploaded by
wennnykCopyright:
Available Formats
Roberts et al.
Systematic Reviews (2015) 4:31
DOI 10.1186/s13643-015-0018-2
RESEARCH
Open Access
Treatment of vaginal candidiasis for the
prevention of preterm birth: a systematic
review and meta-analysis
Christine L Roberts*, Charles S Algert, Kristen L Rickard and Jonathan M Morris
Abstract
Background: Recognition that ascending infection leads to preterm birth has led to a number of studies that have
evaluated the treatment of vaginal infections in pregnancy to reduce preterm birth rates. However, the role of
candidiasis is relatively unexplored. Our aim was to undertake a systematic review and meta-analysis to assess
whether treatment of pregnant women with vulvovaginal candidiasis reduces preterm birth rates and other adverse
birth outcomes.
Methods: We undertook a systematic review and meta-analysis of published randomised controlled trials (RCTs) in
which pregnant women were treated for vulvovaginal candidiasis (compared to placebo or no treatment) and
where preterm birth was reported as an outcome. Trials were identified by searching the Cochrane Central Register
of Controlled Trials, Medline and Embase databases to January 2014. Trial eligibility and outcomes were pre-specified.
Two reviewers independently assessed the studies against the agreed criteria and extracted relevant data using a
standard data extraction form. Meta-analysis was used to calculate pooled rate ratios (RR) and 95% confidence
intervals (CI) using a fixed-effects model.
Results: There were two eligible RCTs both among women with asymptomatic candidiasis, with a total of 685 women
randomised. Both trials compared treatment with usual care (no screening for, or treatment of, asymptomatic
candidiasis). Data from one trial involved a post-hoc subgroup analysis (n = 586) of a larger trial of treatment of 4,429
women with asymptomatic infections in pregnancy and the other was a pilot study (n = 99). There was a significant
reduction in spontaneous preterm births in treated compared with untreated women (meta-analysis RR = 0.36,
95% CI = 0.17 to 0.75). Other outcomes were reported by one or neither trial.
Conclusions: This systematic review found two trials comparing the treatment of asymptomatic vaginal candidiasis in
pregnancy for the outcome of preterm birth. Although the effect estimate suggests that treatment of asymptomatic
candidiasis may reduce the risk of preterm birth, the result needs to be interpreted with caution as the primary driver
for the pooled estimate comes from a post-hoc (unplanned) subgroup analysis. A prospective trial with sufficient power
to answer the clinical question does treatment of asymptomatic candidiasis in early pregnancy prevent preterm
birth is warranted.
Systematic review registration: PROSPERO CRD42014009241
Keywords: Pregnancy, Preterm birth, Premature infant, Candida, Candidiasis, Yeasts, Randomised controlled trial,
Met-analysis
* Correspondence: christine.roberts@sydney.edu.au
Kolling Institute of Medical Research, University of Sydney, St Leonards, NSW,
Australia
2015 Roberts et al.; licensee BioMed Central. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Roberts et al. Systematic Reviews (2015) 4:31
Background
Preterm birth is a major pregnancy complication affecting 5% to 18% of births worldwide [1,2]. Infants born
preterm are at increased risk of death, significant neonatal complications, long-term adverse health outcomes
and developmental impairment [3-5].
Preterm birth (birth before 37 completed weeks of gestation) results from either spontaneous onset of labour
(including preterm prelabour rupture of the membranes)
or a clinical decision that planned birth should occur
because of pregnancy complications. The cause of
spontaneous preterm birth is often unknown, but
intrauterine infection is implicated in up to 40%
[4,6,7]. The likely pathway to intrauterine infection is
ascending genital tract infection [6-9]. Genital tract infection is more frequent among women with spontaneous preterm births at lower gestational ages [7,10].
Importantly, infection may occur before or early in
pregnancy, may be asymptomatic and may remain
undetected [7,11].
The role of infection in preterm birth is thought to
be a chronic process, with early pregnancy a period
of vulnerability to establishment of inflammatory responses that may be the trigger for preterm parturition
[6,9,11]. Organisms detected in the uterus before
membrane rupture are typically of low virulence, probably accounting for both the chronicity of intrauterine
infections and the frequent absence of overt clinical signs
of infection [6,8].
Pregnancy increases the frequency of vaginal Candida
colonization [12]. This is thought to be the consequence
of increased levels of circulating oestrogens and deposition of glycogen and other substrates in the vagina during pregnancy [12]. Candida colonisation may disrupt
normal vaginal flora so that there is a decrease in lactobacilli and an increase in proinflammatory organisms
[9,13]. However, few studies have assessed the associations between candidiasis and preterm birth. A systematic review of treatment trials for symptomatic
candidiasis during pregnancy assessed cure (negative
culture or symptom relief posttreatment) but not
pregnancy outcomes [14].
Studies utilising population-based data from Hungary
reported that vaginal clotrimazole treatment of candidiasis during pregnancy was associated with a 34% to 64%
reduction in the prevalence of preterm birth [15-17]. In
contrast, two cohort studies found no significant association between preterm birth and moderate to heavy
growth of Candida species among women at 22 to
30 weeks gestation [18,19]. Therefore, our aim was to
undertake a systematic review and meta-analysis to
assess whether the treatment of pregnant women
with vulvovaginal candidiasis reduces preterm birth rates
and other adverse birth outcomes. The importance of
Page 2 of 9
reducing preterm birth rates warranted performing a
meta-analysis of randomised clinical trials, which might
amass sufficient statistical power to provide clear evidence
about a possible protective effect.
Methods
Search strategy
The study procedure and outcomes were pre-specified
[20]. We identified relevant studies by searching the
Cochrane Central Register of Controlled Trials, Medline
and Embase from database inception through 31 January
2014. There were no language restrictions. The database searches were supplemented by hand-searching
the reference lists of relevant reviews and potentially
eligible studies. Search terms (using keywords and
Medical Subject Headings (MeSH), all exploded) included (candida or candidiasis or candidosis or
yeasts) and (pregnancy or preterm/premature birth)
and antifungal agents. Conference and meeting abstracts
were not included, and no attempt was made to identify
unpublished studies or contact the authors of published
studies.
Eligibility criteria
Randomised controlled trials (RCT) in which pregnant
women were treated for symptomatic or asymptomatic
vulvovaginal candidiasis and where preterm birth was reported as an outcome were the pre-specified eligibility criteria [20]. Only RCTs that compared treatment (imidazoles
or other proven therapeutic agents) with placebo or
no intervention were of interest. Quasi-randomised
designs, such as alternate allocation or the use of medical record numbers, were not eligible. Mycologically
confirmed diagnoses of vulvovaginal candidiasis (i.e. a
positive culture and/or microscopy for yeast) were
required.
Study selection
The titles and abstracts of all potential studies identified
for inclusion as a result of the search strategy were independently assessed for inclusion by two reviewers. The
two reviewers also assessed the full papers of potentially
eligible studies or where eligibility was unclear. Discrepancies at both stages of study selection were resolved
through discussion.
Risk of bias
The two review authors also independently assessed the
risk of bias (as low, high, or unclear) for each study
using the following pre-specified criteria: random sequence generation, allocation concealment, blinding of
participants and personnel, blinding of outcome assessment and completeness of outcome data [20]. Again,
discrepancies were resolved through discussion.
Roberts et al. Systematic Reviews (2015) 4:31
Primary outcome
Preterm birth (<37 completed weeks of gestation) following spontaneous onset of labour or following preterm
prelabour rupture of membranes.
Secondary infant outcomes
1. Any birth before 37 weeks
2. Medically indicated birth (by labour induction or
prelabour caesarean section) before <37 weeks
3. Birth before 32 weeks
4. Birth weight less than the tenth percentile for
gestational age
5. Birth weight <2,500 g
6. Apgar score of less than 7 at 5 min
7. Respiratory distress syndrome
8. Use of mechanical ventilation
9. Duration of mechanical ventilation
10. Intraventricular haemorrhage
11. Retinopathy of prematurity
12. Chronic lung disease
13. Necrotising enterocolitis
14. Perinatal mortality (stillbirth or neonatal death)
15. Admission to neonatal intensive care unit
16. Neonatal length of hospital stay
17. Breastfeeding
Secondary maternal outcomes
1.
2.
3.
4.
Preterm prelabour rupture of the membranes
Spontaneous pregnancy loss <20 weeks gestation,
Mode of birth
Duration of maternal hospitalisation at the time
of birth
5. Maternal views/satisfaction with the therapy
6. Maternal anxiety
Data extraction
Data were extracted independently by the two reviewers,
and disagreements were resolved by discussion. A
standard data extraction form was used to extract
data on study characteristics, methods and study results. All data on study results were entered into an
Excel Spreadsheet.
Data synthesis
Characteristics, main findings and risk of bias assessment were tabulated for each study. The raw data presented in the included studies were used to determine
the outcome rates for intervention and control groups of
each study. Where data were missing (incomplete
follow-up on all women), the results reported in the
studies as the numerator (no information on those lost
to follow-up) and denominator (all women randomised)
Page 3 of 9
were used; no imputation of outcomes was made. There
were two pre-specified subgroup analyses for the primary outcome: symptomatic and asymptomatic candidiasis, and commencing treatment before 20 weeks
gestation versus after 20 weeks gestation. For each dichotomous outcome of interest within individual studies,
relative risks (RR) and 95% confidence intervals (CIs)
were calculated according to the intention to treat. The
assumption of homogeneity of treatment effect between
studies was assessed using Cochrans Q test statistic and
the I2 test. Meta-analysis was used to calculate pooled
risk ratios (RR) and 95% confidence intervals (CI) using
a fixed-effects model (Mantel-Haenszel), unless the assumption of homogeneity was rejected (P < 0.1) when a
random effects model would be used. Statistical analyses
were performed using the metan command in STATA
(STATA statistical software version 11.0, STATA, College
Station, USA).
Results
Literature search results
A total of 1,014 unique articles were identified (Figure 1).
Of these 17 underwent full review as potentially eligible
or where the eligibility was unclear from the title and
abstract [21-37]. Three papers compared treatment versus placebo or no intervention for pregnant women
with candidiasis [29,35,37] but only two had the outcome of preterm birth and were eligible for inclusion
(Table 1) [29,35].
Characteristics of included studies
Both studies included women with asymptomatic vaginal
candidiasis and both compared treatment with clotrimazole to no treatment (Table 1) [29,35]. Spontaneous preterm birth was the primary outcome for both studies. As
spontaneous preterm birth was the only outcome available from both studies, none of the other planned metaanalysis outcomes could be assessed. There were no
relevant studies assessing symptomatic candidiasis where
preterm birth was the outcome.
The aim of the study by Kiss and colleagues was to
assess whether general screening for, and treatment of,
asymptomatic vaginal infections (bacterial vaginosis,
candidiasis and/or trichomoniasis) was effective in reducing the rate of preterm birth and late miscarriage [29].
Women who were culture positive for any of the three
conditions (n = 4,429) were randomised to treatment
(appropriate to the organism: clindamycin, clotrimazole
and/or metronidazole, respectively) or to usual care
(culture result not revealed and no treatment). There
was no pre-specified subgroup analysis by infection type
so the information on treatment of asymptomatic candidiasis from this trial was extracted from the published
paper post-hoc.
Roberts et al. Systematic Reviews (2015) 4:31
Page 4 of 9
Figure 1 Summary of evidence search and selection.
Drawing on post-hoc subgroup analyses of the Kiss
trial, Roberts and colleagues undertook a pilot study
with the specific aim of assessing treatment of asymptomatic candidiasis to prevent preterm birth [35]. The
study design was essentially the same although the eligibility criteria were limited to women with asymptomatic
candidiasis.
The asymptomatic Candida colonisation rate was
14.1% (15 to 19 weeks gestation) in the Kiss et al. study
and 19.6% (12 to 19 weeks gestation) in the Roberts
et al. study. Kiss et al. reported that women were to be
retested, and if necessary retreated, at 24 to 27 weeks.
However, overall, only 22% of women in the entire treatment arm had a follow-up gram stain and of these 27%
still had a vaginal infection present, including 78 (27%)
with candidiasis, all of whom were retreated. Roberts
et al. report a posttreatment colonisation rate of 48% on
average 10 weeks after recruitment but asymptomatic
women were not offered further treatment.
Risk of bias
Both studies utilised computer random number generation and central randomisation procedures. In the Kiss
et al. study, women who were randomised to clotrimazole treatment (and their obstetricians) were not blinded
to their treatment allocation. However, the untreated
group (93% of women screened) included both women
without infections and those with asymptomatic infections who were randomised to usual care. Clinicians and
women were blinded to the colonisation-status within
this group. Roberts et al. used a similar method but
women allocated to clotrimazole treatment were notified
and treated by the study personnel. So, although the
women in the treatment arm were not blinded, clinicians
were blinded to treatment allocation unless it was revealed during the subsequent pregnancy management.
Like the Kiss et al. study, the untreated group (90% of
participants) included women with and without asymptomatic candidiasis and the clinicians and women were
blinded to this information. This partial blinding of
participants and personnel to exposure status was considered unlikely to affect results. Furthermore, the assessment of outcomes from medical records was blinded
and gestational age determination is not subjective
(based on ultrasound dating and date of birth). The candidiasis subgroup analysis in the Kiss et al. study was
not pre-specified but extracted post-hoc from the published paper. Furthermore, Kiss et al. did not report loss
to follow-up and exclusions by treatment arm or infection subgroups so the number of women with candidiasis for whom outcome data were missing could not be
determined. However, overall 3.2% women were lost to
follow-up and there were 3.0% post-randomisation exclusions (1.5% multiple pregnancies; 1.5% did not fulfil
the inclusion criteria). The follow-up rate was 99% in
the Roberts et al. study (outcome information was
missing for one woman) with no post-randomisation
exclusions.
For both studies, the risk of bias was considered low
for all aspects assessed: random sequence generation,
Study
Study period
and location
Study population
Study size (Candidiasis)
Intervention
Kiss et al.
2001 to 2002, 25
non-hospital-based
obstetricians Vienna,
Austria
Women with singleton
pregnancies, 150 to 196 weeks
gestation, no symptoms of
vaginal infection, bleeding or
contractions, Mean age [SD]:
28.9 [5.6], 48% primipara
98% white ethnicity, Carriage
rate of asymptomatic
candidiasis: 14.1%
586, 294 randomised
to treatment 292
randomised to usual
care
Vaginal clotrimazole Usual care (vaginal
Spontaneous preterm birth
0.1 g for 6 days
culture result not
(<37 weeks gestation)
revealed, no treatment)
Healthy Austria (Fonds
Gesundessterreich)
grant PNr.205/V/12 and
Federal Ministry of Education,
Science, and Culture grant,
GZ 70.069/1-Pr4/2000, no
competing interests declared.
Women with singleton
pregnancies, 120 to 196 weeks
gestation, no symptoms
vaginal infection, mean age
[SD]: 32.2 [54.4], 45%
primipara, ethnicity not
reported, carriage rate of
asymptomatic candidiasis:
19.6%
99, 50 randomised to
Vaginal clotrimazole Usual care (vaginal
Spontaneous preterm birth
treatment, 49 randomised 0.1 g for 6 days
culture result not
(<37 weeks gestation); any
to usual care
revealed, no treatment) preterm birth; pregnancy
complications (gestational
diabetes; antepartum
haemorrhage); mode of
delivery (spontaneous
vaginal, instrumental
caesarean section), birth
weight (<2,500, 2,500 to
3,999, 4,000 g); nursery
admission.
One author supported by an
Australian National Health
and Medical Research Council
Fellowship. No competing
interests declared.*
Roberts et al. 2008 to 2009, single
tertiary obstetric
hospital, Sydney,
Australia
Comparison
Available outcomes among Funding and competing
women with candidiasis
interests
Roberts et al. Systematic Reviews (2015) 4:31
Table 1 Characteristics of randomised controlled trials assessing treatment of vaginal candidiasis to prevent preterm birth
SD, standard deviation; *three authors of this paper are also authors of this systematic review.
Page 5 of 9
Roberts et al. Systematic Reviews (2015) 4:31
allocation concealment, blinding of participants and
personnel, blinding of outcome assessment and completeness of outcome data. However, neither study had a
published protocol so it is possible that there was selective choice for reporting of secondary outcomes. Acknowledged funding for the trials was from government
sources, and there is no suggestion (although not explicitly stated) that the trial treatment was provided by a
pharmaceutical company (Table 1).
Data synthesis
The only outcome available from both studies was spontaneous preterm birth. Meta-analysis showed an overall
reduction in spontaneous preterm birth (RR = 0.36, 95%
CI = 0.17 to 0.75) with similar point estimates from both
studies but little contribution (and very wide confidence
intervals) around the estimate from the pilot study by
Roberts et al. (Figure 2). While Roberts et al. reported
on subsequent pregnancy complications, labour induction, mode of delivery, birth weight and nursery admissions, no other outcomes were available from the Kiss
trial.
Discussion
This systematic review found two trials comparing the
treatment of asymptomatic vaginal candidiasis in pregnancy with usual care (no screening and no treatment of
asymptomatic vaginal candidiasis) for the outcome of
preterm birth. The findings provide support for the hypothesis that treatment of asymptomatic candidiasis may
reduce the risk of preterm birth. Although the two studies had similar methods, treatment regimens and findings among general maternity populations in different
countries, the result needs to be interpreted with caution
as the primary driver for the pooled estimate is a posthoc subgroup analysis of the Kiss trial. We believe that
the meta-analysis result supports the need for a larger
trial that specifically addresses the question of whether
the treatment of asymptomatic candidiasis early in
Page 6 of 9
pregnancy can reduce the risk of spontaneous preterm
birth. If a simple, inexpensive intervention is demonstrated to reduce spontaneous preterm birth, this
would change current maternity care internationally.
A significant reduction in preterm birth would not
only reduce perinatal mortality and morbidity, but
also have major resource implications, such as reduced need for neonatal intensive care and childhood
hospitalisations.
The two trials reported different colonisation rates of
asymptomatic candidiasis (14.1% and 19.6%) [29,35].
This reflects population baseline characteristics and
slightly varying gestational age ranges for recruitment.
Other studies report colonisation rates that range from
14% to 38% for symptomatic candidiasis at 22 to 30
weeks gestation but do not report asymptomatic rates
[18,19,38]. Some of the population risk factors for candidiasis are also risk factors for preterm birth including
African-American women, low socioeconomic status,
smoking, maternal medical conditions and bacterial
vaginosis [16,18,29].
Both trials included in the meta-analysis used a similar
design, described by Roberts et al. as a Prospective,
Randomised, Open-label, Blinded-Endpoint (PROBE)
design. PROBE designs have been used in cardiovascular
disease trials [39-46], and the two trials in this review
may be the first obstetric trials to use this design. Features include strict randomisation and allocation concealment procedures, and blinding of those assessing the
trial endpoints [41]. The drug interventions are typically
commercially available as indicated in the Roberts trial
[35]. Consequently, as the treatment protocol adheres
closely to routine clinical practice, the results from a
PROBE design may be more generalisable to the pragmatic management of patients than double-blind,
placebo-controlled trials [41,45]. A potential disadvantage of a placebo-controlled trial for answering this
preterm birth prevention question is that a vaginally administered placebo may be biologically active as it would
Figure 2 Meta-analysis of spontaneous preterm birth among women with asymptomatic candidiasis: clotrimazole versus usual care.
Roberts et al. Systematic Reviews (2015) 4:31
have to contain an alcohol preservative that could have
an independent effect on vaginal flora [35].
Clotrimazole, the treatment used in both the included
studies, is classified as a category A drug meaning it has
been used by a large number of pregnant women and
women of childbearing age without any proven increase
in the frequency of malformations or other direct or indirect harmful effects on the fetus having been observed
[47]. Large population-based studies have not demonstrated risks to the fetus following exposure to clotrimazole in pregnancy [48]. Randomised trials of treatment
of symptomatic candidiasis in pregnancy provide
evidence for the use of topical imidazoles (such as clotrimazole), rather than nystatin or hydrargaphen, for
successful eradication of Candida from the vagina. Furthermore, the susceptibility of both Candida albicans
and non-albicans Candida vaginal isolates to azole antifungal agents, such as clotrimazole, supports the continued practice of azole antifungal agents for empirical
therapy of Candida vaginitis [49].
Despite the interest in infection as a risk factor for
preterm birth, we found only two trials (including a
small pilot study) to contribute to this review. Perhaps
as Candida is considered a vaginal commensal organism
[13], the role of candidiasis in preterm birth has not
been pursued with the same attention as bacterial vaginosis and other vaginal organisms [11,50-53]. However, it
is also possible that some relevant studies that could
change the finding of the meta-analysis in the direction
of no association were missed as only controlled vocabulary search terms were used and the search was limited
to published studies.
Rather than pregnancy outcomes, previous research
has mostly focussed on the question of best treatment
for eradicating Candida colonisation in pregnant women
with symptomatic candidiasis. The availability of only
two trials precludes the opportunity to explore issues
like heterogeneity and any impact of reporting biases in
sensitivity and subgroup analyses. Only one outcome
(spontaneous preterm birth) was available from both
studies, and future trials should consider other potential
pregnancy outcomes and treatment side effects [54].
Although we identified 11 treatment trials of symptomatic candidiasis in pregnancy, all were published
before 1985, only one compared treatment to placebo
and none reported pregnancy outcomes, only the rate
of Candida eradication [25,36,37,55-62]. Furthermore,
the seven studies that reported gestational age at recruitment all included women who were too advanced in pregnancy to have an impact on preterm
birth [25,36,37,56,58,60,62].
Inclusion in the meta-analysis of some women with
missing outcome information is unlikely to change the
conclusions. From the Kiss et al. trial, the extent of
Page 7 of 9
missing data on the outcome of preterm birth for
women with candidiasis could not be determined but
was approximately 3% among all women with asymptomatic infections. One woman (of 99) in the Roberts
et al. trial was missing information on birth outcome.
Only Roberts et al. reported other birth outcomes for
the treated and untreated groups of women but this
was limited by small event numbers: any preterm
birth (RR = 0.65; 95% CI = 0.11 to 3.74), spontaneous
vaginal birth (RR = 1.03; 95% CI = 0.64 to 1.64), instrumental vaginal birth (RR = 0.88; 95% CI = 0.39 to
1.98), caesarean section (RR = 1.09; 95% CI = 0.66 to
1.80), birth weight <2,500 g (RR = 0.98; 95% CI = 0.14
to 6.68) and nursery admission (RR = 1.31; 95% CI = 0.31
to 5.54). The remaining pre-specified outcomes were not
reported in either of the included studies.
The rationale of the two included trials is that early
treatment of vaginal infections is necessary for effective
prevention of infection-related preterm birth, as early
pregnancy is the period of greatest risk for the establishment of inflammatory responses to low virulence organisms that increase the risk of preterm birth [6-9].
Treatment later in pregnancy may have limited effect in
preventing preterm parturition if the inflammatory
responses are not fully reversible [4]. Importantly,
treatment does not necessarily eradicate Candida in
all women nor prevent recolonisation. Posttreatment
Candida eradication rates (assessed at 3 to 6 weeks) for
symptomatic candidiasis in pregnancy range from 69% to
100% (five trials, median 88%) [14] and for asymptomatic
candidiasis was 73% (assessed at 4 to 5 weeks) in the Kiss
trial [29] and 52% (assessed at 10 weeks) in the Roberts
trial [35]. However, it is not clear whether posttreatment colonisation represents persistent colonisation or
recolonisation.
Conclusion
The findings of this review, that treating asymptomatic
candidiasis in early pregnancy may reduce spontaneous
preterm birth rates, need to be interpreted with caution.
The findings are based on only two published trials (a
pilot study and a post-hoc subgroup analysis with data
from 685 women who had 34 spontaneous preterm
births) both using clotrimazole and both in asymptomatic women, and the post-hoc subgroup analysis was the
primary driver for the pooled estimate. Furthermore,
there were insufficient data on other important infant
and maternal outcomes. This systematic review suggests
that a trial with sufficient power to answer the clinical
question does treatment of asymptomatic candidiasis in
early pregnancy prevent preterm birth is warranted.
Competing interests
Authors CLR, KLR and JMM are authors on one of the included trials [35].
The authors have no other competing interests to declare.
Roberts et al. Systematic Reviews (2015) 4:31
Authors contributions
CLR, CSA and JMM conceived the study and drafted the study protocol. CLR
performed the literature searches. CLR and KLR assessed the literature and
extracted data. CSA undertook the statistical analyses and provided statistical
expertise. All authors participated in the interpretation of the results, critically
reviewed drafts of the manuscript, and read and approved the final manuscript.
Acknowledgements
This work was supported by an Australian National Health and Medical
Research Council (NHMRC) Project Grants (#632544; #APP1078624). CLR is
supported by a NHMRC Senior Research Fellowship (#APP1021025). The
NHMRC had no role in design; in the collection, analysis, and interpretation
of data; in the writing of the manuscript; and in the decision to submit the
manuscript for publication.
Received: 7 August 2014 Accepted: 24 February 2015
References
1. Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al.
National, regional, and worldwide estimates of preterm birth rates in the
year 2010 with time trends since 1990 for selected countries: a systematic
analysis and implications. Lancet. 2012;379(9832):216272.
2. Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C, Group GR. Global
report on preterm birth and stillbirth: definitions, description of the
burden and opportunities to improve data. BMC Pregnancy Childbirth.
2010;10(1):S1.
3. Iams JD, Romero R, Culhane JF, Goldenberg RL. Primary, secondary, and
tertiary interventions to reduce the morbidity and mortality of preterm
birth. Lancet. 2008;371(9607):16475.
4. Oliver RS, Lamont RF. Infection and antibiotics in the aetiology, prediction
and prevention of preterm birth. J Obstet Gynaecol. 2013;33(8):76875.
5. Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth
from infancy to adulthood. Lancet. 2008;371(9608):2619.
6. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of
preterm birth. Lancet. 2008;371(9606):7584.
7. Riggs MA, Klebanoff MA. Treatment of vaginal infections to prevent preterm
birth: a meta-analysis. Clin Obstet Gynecol. 2004;47(4):796807. discussion
881792.
8. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm
delivery. N Engl J Med. 2000;342(20):15007.
9. Jefferson KK. The bacterial etiology of preterm birth. Advin Appl Microbiol.
2012;80:122.
10. Gravett MG, Rubens CE, Nunes TM, Group GR. Global report on preterm
birth and stillbirth (2 of 7): discovery science. BMC Pregnancy Childbirth.
2010;10(1):S2.
11. Lamont RF, Nhan-Chang CL, Sobel JD, Workowski K, Conde-Agudelo A,
Romero R. Treatment of abnormal vaginal flora in early pregnancy with
clindamycin for the prevention of spontaneous preterm birth: a systematic
review and metaanalysis. Am J Obstet Gynecol. 2011;205(3):17790.
12. Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369(9577):196171.
13. Cassone A. Vulvovaginal Candida albicans infections: pathogenesis, immunity
and vaccine prospects. BJOG. 2014, doi: 10.1111/1471-0528.12994.
14. Young GL, Jewell D. Topical treatment for vaginal candidiasis (thrush) in
pregnancy. Cochrane Database Syst Rev. 2001;4:CD000225.
15. Banhidy F, Acs N, Puho EH, Czeizel AE. Rate of preterm births in pregnant
women with common lower genital tract infection: a population-based
study based on the clinical practice. J Matern Fetal Neonatal Med.
2009;22(5):4108.
16. Czeizel AE, Fladung B, Vargha P. Preterm birth reduction after clotrimazole
treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol.
2004;116(2):15763.
17. Czeizel AE, Rockenbauer M. A lower rate of preterm birth after clotrimazole
therapy during pregnancy. Paediatr Perinat Epidemiol. 1999;13(1):5864.
18. Cotch MF, Hillier SL, Gibbs RS, Eschenbach DA. Epidemiology and outcomes
associated with moderate to heavy Candida colonization during pregnancy.
Am J Obstet Gynecol. 1998;178(2):37480.
19. McGregor JA, French JI, Parker R, Draper D, Patterson E, Jones W, et al.
Prevention of premature birth by screening and treatment for common
genital tract infections: results of a prospective controlled evaluation. Am J
Obstet Gynecol. 1995;173(1):15767.
Page 8 of 9
20. Roberts CL, Algert CS, Morris JM. Treating vaginal candidiasis for the
prevention of preterm birth: protocol for a systematic review and metaanalysis. .http://hdl.handle.net/2123/11552.
21. Bloch B, Kretzel A. Econazole nitrate in the treatment of candidal vaginitis. S
Afr Med J Suid-Afrikaanse Tydskrif Vir Geneeskunde. 1980;58(8):3146.
22. Campomori A, Bonati M. Fluconazole treatment for vulvovaginal candidiasis
during pregnancy. Ann Pharmacother. 1997;31(1):1189.
23. Chaisilwattana P, Bhiraleus P. A comparative study of 3-day and 6-day
clotrimazole therapy in patients with vaginal candidosis. J Med Assoc
Thai. 1986;69(8):4327.
24. Culbertson C. MONISTAT: a new fungicide for treatment of vulvovaginal
candidiasis. Am J Obstet Gynecol. 1974;120(7):9736.
25. Dunster GD. Vaginal candidiasis in pregnancy - a trial of clotrimazole.
Postgrad Med J. 1974;50 Suppl 1:868.
26. Fedi B, Marchetti E, Pelini G, Tanini R. Vulvovaginal candidiasis in pregnancy:
Treatment with clotrimazole. Boll Soc Ital Biol Sper. 1979;55(16):158892.
27. Fernandez Del Castillo C, Perez De Salazar JL, Jesus Diaz Loya FD.
Clotrimazole treatment of female genital infection by Candida albicans.
Ginecol Obstet Mex. 1978;43(259):299309.
28. Higton BK. A trial of clotrimazole and nystatin in vaginal candidiasis.
Postgrad Med J. 1974;50 Suppl 1:958.
29. Kiss H, Petricevic L, Husslein P. Prospective randomised controlled trial of an
infection screening programme to reduce the rate of preterm delivery. BMJ.
2004;329(7462):371.
30. Lecart C, Claerhout F, Franck R, Godts P, Lilien C, Macours L, et al. A new
treatment of vaginal candidiasis: three-day treatment with econazole. Eur J
Obstet Gynecol Reprod Biol. 1979;9(2):1257.
31. Lucisano F, Loiudice L. Treatment of Candida vulvovaginitis with a new
imidazole derivative. Minerva Ginecol. 1979;31(12):7784.
32. Nahmanovici C. Treatment of vaginal candidosis with three 80-mg
terconazole vaginal suppositories: results of a multicentre study in
France. Gynakol Rundsch. 1985;25 Suppl 1:528.
33. Pawlaczyk M, Friebe Z, Pawlaczyk MT, Sowinska-Przepiera E, Wlosinska J. The
effect of treatment for vaginal yeast infection on the prevalence of bacterial
vaginosis in early pregnancy. Acta Dermatovenerol Croat. 2006;14(1):269.
34. Pigott PV. An evaluation of a modified nystatin vaginal tablet in a multicentre study. Curr Med Res Opin. 1972;1(3):15965.
35. Roberts CL, Rickard KR, Kotsiou G, Morris JM. Treatment of asymptomatic
vaginal candidiasis in pregnancy to prevent preterm birth: an open-label
pilot randomised controlled trial. BMC Pregnancy Childbirth. 2011;11:18.
36. Rubin A, Russell JM, Mauff A. Efficacy of econazole in the treatment of
candidiasis and other vaginal discharges. S Afr Med J Suid-Afrikaanse
Tydskrif Vir Geneeskunde. 1980;57(11):4078.
37. Ruiz-Velasco V, Rosas-Arceo J. Prophylactic clotrimazole treatment to
prevent mycoses contamination of the newborn. Int J Gynaecol
Obstet. 1978;16(1):701.
38. Polk BF. Association of Chlamydia trachomatis and Mycoplasma hominis
with intrauterine growth retardation and preterm delivery. Am J Epidemiol.
1989;129(6):124757.
39. Amarenco P, Davis S, Jones EF, Cohen AA, Heiss WD, Kaste M, et al.
Clopidogrel plus aspirin versus warfarin in patients with stroke and aortic
arch plaques. Stroke. 2014;45(5):124857.
40. Cooper-DeHoff RM, Aranda Jr JM, Gaxiola E, Cangiano JL, Garcia-Barreto D,
Conti CR, et al. Blood pressure control and cardiovascular outcomes in
high-risk Hispanic patients - findings from the International Verapamil
SR/Trandolapril Study (INVEST). Am Heart J. 2006;151(5):10729.
41. Hansson L, Hedner T, Dahlof B. Prospective randomized open blinded
end-point (PROBE) study. A novel design for intervention trials. Prospective
Randomized Open Blinded End-Point. Blood Press. 1992;1(2):1139.
42. Mancia G, Omboni S, Group CS. Candesartan plus hydrochlorothiazide fixed
combination vs previous monotherapy plus diuretic in poorly controlled
essential hypertensive patients. Blood Press Suppl. 2004;2:117.
43. Mizuno K, Nakaya N, Ohashi Y, Tajima N, Kushiro T, Teramoto T, et al.
Usefulness of pravastatin in primary prevention of cardiovascular events in
women: analysis of the Management of Elevated Cholesterol in the Primary
Prevention Group of Adult Japanese (MEGA study). Circulation.
2008;117(4):494502.
44. Sharman JE, Marwick TH, Gilroy D, Otahal P, Abhayaratna WP, Stowasser M,
et al. Randomized trial of guiding hypertension management using central
aortic blood pressure compared with best-practice care: principal findings
of the BP GUIDE study. Hypertension. 2013;62(6):113845.
Roberts et al. Systematic Reviews (2015) 4:31
Page 9 of 9
45. Smith DH, Neutel JM, Lacourciere Y, Kempthorne-Rawson J. Prospective,
randomized, open-label, blinded-endpoint (PROBE) designed trials yield the
same results as double-blind, placebo-controlled trials with respect to ABPM
measurements. J Hypertens. 2003;21(7):12918.
46. Vinereanu D, Gherghinescu C, Ciobanu AO, Magda S, Niculescu N,
Dulgheru R, et al. Reversal of subclinical left ventricular dysfunction by
antihypertensive treatment: a prospective trial of nebivolol against
metoprolol. J Hypertens. 2011;29(4):80917.
47. Therapuetic Goods Association: Prescribing medicines in pregnancy.
http://www.tga.gov.au/hp/medicines-pregnancy.htm#.VC3d41eJA44I
(accessed September 2014).
48. Czeizel AE, Toth M, Rockenbauer M. No teratogenic effect after clotrimazole
therapy during pregnancy. Epidemiology. 1999;10(4):43740.
49. Richter SS, Galask RP, Messer SA, Hollis RJ, Diekema DJ, Pfaller MA.
Antifungal susceptibilities of Candida species causing vulvovaginitis and
epidemiology of recurrent cases. J Clin Microbiol. 2005;43(5):215562.
50. Brocklehurst P, Gordon A, Heatley E, Milan SJ. Antibiotics for treating
bacterial vaginosis in pregnancy. Cochrane Database Syst Rev.
2013;1:CD000262.
51. Brocklehurst P, Rooney G. Interventions for treating genital chlamydia
trachomatis infection in pregnancy. Cochrane Database Syst Rev.
2000;2:CD000054.
52. Glmezoglu AM, Azhar M. Interventions for trichomoniasis in pregnancy.
Cochrane Database Syst Rev. 2011;5:CD000220.
53. Raynes GC, Roberts CL, Gilbert GL. Antibiotics for ureaplasma in the vagina
in pregnancy. Cochrane Database Syst Rev. 2011;9:CD003767.
54. Roberts CL, Morris JM, Rickard KR, Giles WB, Simpson JM, Kotsiou G, et al.
Protocol for a randomised controlled trial of treatment of asymptomatic
candidiasis for the prevention of preterm birth [ACTRN12610000607077].
BMC Pregnancy Childbirth. 2011;11:19.
55. Davis JE, Frudenfeld JH, Goddard JL. Comparative evaluation of Monistat
and Mycostatin in the treatment of vulvovaginal candidiasis. Obstet
Gynecol. 1974;44(3):4036.
56. Del Palacio-Hernanz A, Sanz-Sanz F, Rodriquez-Noriega A. Double-blind
investigation of R-42470 (terconazole cream 0.4%) and clotrimazole
(cream 1%) for the topical treatment of mycotic vaginitis. Chemioterapia.
1984;3:1925.
57. Lebherz TB, Ford LC. Candida albicans vaginitis: the problem is diagnosis,
the enigma is treatment. Chemotherapy. 1982;28 Suppl 1:739.
58. McNellis D, McLeod M, Lawson J, Pasquale SA. Treatment of vulvovaginal
candidiasis in pregnancy. A comparative study. Obstet Gynecol.
1977;50(6):6748.
59. Milne LJ, Brown AD. Comparison of nystatin (Nystan) and hydrargaphen
(Penotrane) in the treatment of vaginal candidosis in pregnancy. Curr Med
Res Opin. 1973;1(9):5247.
60. Pasquale SA, Lawson J, Sargent Jr EC, Newdeck JP. A doseresponse study
with Monistat cream. Obstet Gynecol. 1979;53(2):2503.
61. Qualey JR, Cooper C. Monistat cream (miconazole nitrate) a new agent for
the treatment of vulvovaginal candidiasis. J Reprod Med. 1975;15(3):1235.
62. Tan CG, Milne LJR, Good CS, Loudon JDO. A comparative trial of six day
therapy with clotrimazole and nystatin in pregnant patients with vaginal
candidiasis. Postgrad Med J. 1975;50(1):1025.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
You might also like
- TLE Hairdressing Grade 8 - 9Document25 pagesTLE Hairdressing Grade 8 - 9Roswlle50% (2)
- Leitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseDocument7 pagesLeitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseEdgar SimmonsNo ratings yet
- Pregnancy HypertensionDocument9 pagesPregnancy Hypertensionabi tehNo ratings yet
- Treatment of Asymptomatic Vaginal Candidiasis in Pregnancy To Prevent Preterm Birth An Openlabel Pilot Randomized ContrDocument7 pagesTreatment of Asymptomatic Vaginal Candidiasis in Pregnancy To Prevent Preterm Birth An Openlabel Pilot Randomized ContrariestianiNo ratings yet
- Asymptomatic Bacterial Vaginosis and Intermediate Flora As Risk Factors For Adverse Pregnancy OutcomeDocument16 pagesAsymptomatic Bacterial Vaginosis and Intermediate Flora As Risk Factors For Adverse Pregnancy OutcomealvilNo ratings yet
- Effect of Dydrogesterone On Treatment of Threatened Miscarriage: A Systematic Review and Meta-AnalysesDocument10 pagesEffect of Dydrogesterone On Treatment of Threatened Miscarriage: A Systematic Review and Meta-AnalysesShirleyNo ratings yet
- Premature Rupture of Membranes at Term: A Meta-Analysis of Three Management SchemesDocument3 pagesPremature Rupture of Membranes at Term: A Meta-Analysis of Three Management SchemesYuliana Eka SintaNo ratings yet
- OB Journal AppraisalDocument2 pagesOB Journal AppraisalAlloiBialbaNo ratings yet
- Uog 20140Document11 pagesUog 20140vincentharlling90No ratings yet
- Aogs 12933Document11 pagesAogs 12933Warawiri 11No ratings yet
- Bacterial Vaginosis Draft Evidence ReviewDocument206 pagesBacterial Vaginosis Draft Evidence Reviewaisa mutiaraNo ratings yet
- Management of Premature Rupture of Membranes: Ashraf Olabi and Lucy Shikh MousaDocument7 pagesManagement of Premature Rupture of Membranes: Ashraf Olabi and Lucy Shikh MousaDesi SafiraNo ratings yet
- Maternal and Neonatal Outcomes in Electively Induced Low-Risk Term PregnanciesDocument16 pagesMaternal and Neonatal Outcomes in Electively Induced Low-Risk Term Pregnanciessri afniNo ratings yet
- Desi Rahayu (153112540120468Document53 pagesDesi Rahayu (153112540120468Bella FebriyantiNo ratings yet
- Best Papers From The Last 10 YearsDocument103 pagesBest Papers From The Last 10 YearsLopez Lopez Jose AngelNo ratings yet
- NIH Public Access: Author ManuscriptDocument14 pagesNIH Public Access: Author ManuscriptRafael FigueroaNo ratings yet
- Maternal and Perinatal Outcomes After Elective Labor Induction at 39 Weeks in Uncomplicated Singleton Pregnancies - A Meta-Analysis-sotiriadis2018Document27 pagesMaternal and Perinatal Outcomes After Elective Labor Induction at 39 Weeks in Uncomplicated Singleton Pregnancies - A Meta-Analysis-sotiriadis2018trongnguyen2232000No ratings yet
- Research Article: Bacterial Vaginosis, Educational Level of Pregnant Women, and Preterm Birth: A Case-Control StudyDocument5 pagesResearch Article: Bacterial Vaginosis, Educational Level of Pregnant Women, and Preterm Birth: A Case-Control Studynurul maghfirahNo ratings yet
- Bakker 2012Document10 pagesBakker 2012ieoNo ratings yet
- Amn Inf2Document9 pagesAmn Inf2Melih CivanNo ratings yet
- Bjo 12328Document12 pagesBjo 12328Afiqah So JasmiNo ratings yet
- Immanuel Simmons2017 Article ScreeningAndTreatmentForEarlyDocument11 pagesImmanuel Simmons2017 Article ScreeningAndTreatmentForEarlyLizbeth RomeroNo ratings yet
- Journal Club Presentation For Meta-Analysis of Vaginal Progesterone vs. CerclageDocument43 pagesJournal Club Presentation For Meta-Analysis of Vaginal Progesterone vs. CerclageAlioudNo ratings yet
- Short-Term Effects of BreastfeedingDocument54 pagesShort-Term Effects of BreastfeedingAnonymous Zk4Go4facONo ratings yet
- Management of Hepatitis B Infected Pregnant Women: A Cross-Sectional Study of ObstetriciansDocument7 pagesManagement of Hepatitis B Infected Pregnant Women: A Cross-Sectional Study of Obstetricianslina ukagoNo ratings yet
- Journal Reading Periodontitis and preeclampsia-BORDocument70 pagesJournal Reading Periodontitis and preeclampsia-BORbobbyrianto2210No ratings yet
- Preeclampsia Screening Evidence Report and Systematic Review For The US Preventive Services Task ForceDocument16 pagesPreeclampsia Screening Evidence Report and Systematic Review For The US Preventive Services Task ForceRoberto López MataNo ratings yet
- Pi Is 0020729213005055Document4 pagesPi Is 0020729213005055Winna Eka PNo ratings yet
- Timing of Administration of Prophylactic Antibiotics For Caesarean Section: A Systematic Review and Meta-AnalysisDocument9 pagesTiming of Administration of Prophylactic Antibiotics For Caesarean Section: A Systematic Review and Meta-AnalysissriNo ratings yet
- Hubungan Antara Vaginosis Bakterial Dan Persalinan Preterm: Hepta Lidia, Ova Emilia, Moch. AnwarDocument10 pagesHubungan Antara Vaginosis Bakterial Dan Persalinan Preterm: Hepta Lidia, Ova Emilia, Moch. AnwarJimmy LahabamaNo ratings yet
- Reduccion de Transmision CochraneDocument6 pagesReduccion de Transmision Cochranesara lopezNo ratings yet
- Dyq 030Document10 pagesDyq 030Marlintan Sukma AmbarwatiNo ratings yet
- Wolf Et Al MultivitaminsDocument30 pagesWolf Et Al MultivitaminsAnonymous 2GBzrE3XNo ratings yet
- Antenatal Fetal AssessmentDocument7 pagesAntenatal Fetal AssessmentFitriana Nur RahmawatiNo ratings yet
- What Is HUAM?: Content/uploads/2013/03/chapter14 - Uterine - Act - Monitor94.pdf?414ed1Document3 pagesWhat Is HUAM?: Content/uploads/2013/03/chapter14 - Uterine - Act - Monitor94.pdf?414ed1uthasutarsaNo ratings yet
- Smo 3Document6 pagesSmo 3Irini BogiagesNo ratings yet
- Cesarienne Apres Declenchement Du TravailDocument9 pagesCesarienne Apres Declenchement Du TravailTchimon VodouheNo ratings yet
- 4.牟方详 -En-Effect of Granulocyte Colony-Stimulating Factor on Clinical Pregnancy Outcomes of Recurrent Miscarriage and Recurrent Implantation Failure Cases - a Meta-AnalysisDocument15 pages4.牟方详 -En-Effect of Granulocyte Colony-Stimulating Factor on Clinical Pregnancy Outcomes of Recurrent Miscarriage and Recurrent Implantation Failure Cases - a Meta-AnalysisjohnheshanxiNo ratings yet
- Who Can Provide Effective and Safe Termination of Pregnancy Care? A Systematic ReviewDocument9 pagesWho Can Provide Effective and Safe Termination of Pregnancy Care? A Systematic ReviewAgung HaryadiNo ratings yet
- Grabovac 2017Document12 pagesGrabovac 2017Karindha Handayani HelisusantoNo ratings yet
- TranslateDocument12 pagesTranslateMulia AndaraNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyDr. Ivo Basílio Jr.No ratings yet
- Scientrfic Basis For The Content of Routine Antenatal CareDocument14 pagesScientrfic Basis For The Content of Routine Antenatal CareRusdySpotrNo ratings yet
- Outcome of Neonates Born To Mothers With Premature Rupture of MembranesDocument5 pagesOutcome of Neonates Born To Mothers With Premature Rupture of MembranesDevi SilalahiNo ratings yet
- Research Article: Bacterial Vaginosis, Educational Level of Pregnant Women, and Preterm Birth: A Case-Control StudyDocument5 pagesResearch Article: Bacterial Vaginosis, Educational Level of Pregnant Women, and Preterm Birth: A Case-Control Studynurul maghfirahNo ratings yet
- 9 PDFDocument9 pages9 PDFAnggun SetiawatiNo ratings yet
- DownloadDocument6 pagesDownloadKai GgNo ratings yet
- ResearchDocument20 pagesResearchtedypsNo ratings yet
- Antiretroviral Therapy (ART) For Treating HIV Infection in ART-eligible Pregnant WomenDocument3 pagesAntiretroviral Therapy (ART) For Treating HIV Infection in ART-eligible Pregnant WomenmuisNo ratings yet
- Obstetric Complications in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-AnalysisDocument26 pagesObstetric Complications in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-AnalysisPany Chandra LestariNo ratings yet
- 31 - OMS Diarrhée Et Pneumonie PDFDocument54 pages31 - OMS Diarrhée Et Pneumonie PDFsasNo ratings yet
- Me Gustó Como Escribieron en Esta RevisionDocument8 pagesMe Gustó Como Escribieron en Esta RevisionRolando Miranda PeñaNo ratings yet
- ANS Before 24 WeeksDocument11 pagesANS Before 24 WeeksmadhuNo ratings yet
- Mycoplasma Genitalium Infection and FemaleDocument9 pagesMycoplasma Genitalium Infection and FemaleFebri gerpilianNo ratings yet
- Cervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisDocument17 pagesCervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisNi Wayan Ana PsNo ratings yet
- Outcomes of Term Induction in Trial of Labor After.19Document9 pagesOutcomes of Term Induction in Trial of Labor After.19harold.atmajaNo ratings yet
- Bacterial Vaginosis Jurnal ReadingDocument27 pagesBacterial Vaginosis Jurnal ReadingWahyu Permata LisaNo ratings yet
- Women's Views and Postpartum Follow-Up in The CHIPS Trial (Control of Hypertension in Pregnancy Study)Document9 pagesWomen's Views and Postpartum Follow-Up in The CHIPS Trial (Control of Hypertension in Pregnancy Study)dnnivNo ratings yet
- 1 PBDocument6 pages1 PBArjuna MedagamaNo ratings yet
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- Contraception for the Medically Challenging PatientFrom EverandContraception for the Medically Challenging PatientRebecca H. AllenNo ratings yet
- Prevalence of Vaginal Candidiasis in Pregnancy Among Coastal South Indian Women HnYuDocument3 pagesPrevalence of Vaginal Candidiasis in Pregnancy Among Coastal South Indian Women HnYuEdogawa RakhmanNo ratings yet
- S102 FullDocument6 pagesS102 FullEdogawa RakhmanNo ratings yet
- Prospective Randomised Trial Comparing Traditional Suture Technique With The Dynamic Sliding Loop Suture Technique in The Closure of Skin LacerationsDocument4 pagesProspective Randomised Trial Comparing Traditional Suture Technique With The Dynamic Sliding Loop Suture Technique in The Closure of Skin LacerationsEdogawa RakhmanNo ratings yet
- Pregnancy-Related Pelvic Girdle Pain How Can We Help 0809Document39 pagesPregnancy-Related Pelvic Girdle Pain How Can We Help 0809Edogawa RakhmanNo ratings yet
- 2012 153 4 Comparison of Glutamate Evoked Pain Between The Temporalis and Masseter Muscles in Men and Women 823 829Document7 pages2012 153 4 Comparison of Glutamate Evoked Pain Between The Temporalis and Masseter Muscles in Men and Women 823 829Edogawa RakhmanNo ratings yet
- Female Genital Cutting:: Harmful and Un-IslamicDocument9 pagesFemale Genital Cutting:: Harmful and Un-IslamicEdogawa RakhmanNo ratings yet
- Myofascial Pain Syndrome inDocument17 pagesMyofascial Pain Syndrome inEdogawa RakhmanNo ratings yet
- Chiropractic Advice For Moms-to-Be: What Can You Do? ExerciseDocument2 pagesChiropractic Advice For Moms-to-Be: What Can You Do? ExerciseEdogawa RakhmanNo ratings yet
- 2011 Apr 35Document18 pages2011 Apr 35Edogawa RakhmanNo ratings yet
- Social Anxiety DisorderDocument44 pagesSocial Anxiety DisorderPaü RodriguezNo ratings yet
- Phobias AdaaDocument8 pagesPhobias AdaaEdogawa RakhmanNo ratings yet
- Programmed InstructionDocument17 pagesProgrammed Instructionakhimoloos88% (17)
- Acamprosate A Review of Its Use in Alcohol DependenceDocument14 pagesAcamprosate A Review of Its Use in Alcohol DependenceastrogliaNo ratings yet
- OceanofPDF - Com Dark Psychology and Emotional Manipulation - Donald GolemanDocument358 pagesOceanofPDF - Com Dark Psychology and Emotional Manipulation - Donald GolemanKristine Gerbolingo100% (1)
- HRDDocument16 pagesHRDSuhani jainNo ratings yet
- SCPX Project Line of Fire Presentation ENGDocument22 pagesSCPX Project Line of Fire Presentation ENGGiorgi KenkebashviliNo ratings yet
- Neonatal Ventilation - Neocon 2017-2Document156 pagesNeonatal Ventilation - Neocon 2017-2RAM SOFTWARE100% (2)
- Eco Sanitation - Power Point Presentation in Marathi Language.Document30 pagesEco Sanitation - Power Point Presentation in Marathi Language.shrikant100% (6)
- Dysfunctional FamiliesDocument2 pagesDysfunctional FamiliesJane JasaNo ratings yet
- Helping Patients Who Drink Too MuchDocument40 pagesHelping Patients Who Drink Too MuchdorleemNo ratings yet
- Biocheck C2P - PSK Pharma PDFDocument9 pagesBiocheck C2P - PSK Pharma PDFFari ShaikhNo ratings yet
- The Association Between The Triglyceride To High-Density Lipoprotein Cholesterol Ratio and Low-Density Lipoprotein SubclassesDocument9 pagesThe Association Between The Triglyceride To High-Density Lipoprotein Cholesterol Ratio and Low-Density Lipoprotein SubclassesHendro GunawanNo ratings yet
- Ob Database DXRDocument9 pagesOb Database DXRNMD LIFESAVERNo ratings yet
- Operating Manual: Single and Combination Lights Chromophare E 778, E 668, E 558Document166 pagesOperating Manual: Single and Combination Lights Chromophare E 778, E 668, E 558hluevanoNo ratings yet
- Baseline Chard For OcdDocument2 pagesBaseline Chard For OcdMaryeum MaryeumNo ratings yet
- Cont. Union of Two EventsDocument15 pagesCont. Union of Two EventsharryNo ratings yet
- Machine Learning Techniques To Predict Different Levels of Hospital Care of Covid-19Document26 pagesMachine Learning Techniques To Predict Different Levels of Hospital Care of Covid-19Èlgoog ìnvertionNo ratings yet
- Hema Complex, Sector - 3, Channi Himmat, Jammu/ Zamzam Complex Rambagh SrinagarDocument2 pagesHema Complex, Sector - 3, Channi Himmat, Jammu/ Zamzam Complex Rambagh SrinagarBaljeet KourNo ratings yet
- Interview With A Community Health Nurse: MissDocument4 pagesInterview With A Community Health Nurse: MissCarissa Mae Tapec EstradaNo ratings yet
- Microbiological CheckDocument2 pagesMicrobiological Checkניסים אמאנוNo ratings yet
- Q4 Week1 G9 LASDocument5 pagesQ4 Week1 G9 LASMariejo PalomaresNo ratings yet
- To Save: File - Download As - Microsoft Excel (.XLSX) - Drworkout - FitnessDocument16 pagesTo Save: File - Download As - Microsoft Excel (.XLSX) - Drworkout - FitnessGustavoAguirreValencianaNo ratings yet
- Emergency Evacuation PlanDocument4 pagesEmergency Evacuation PlanSujan AugustinNo ratings yet
- Contact Dermatitis: A Practice ParameterDocument38 pagesContact Dermatitis: A Practice ParameterdhirazhrNo ratings yet
- Health2 2C Feb15Document11 pagesHealth2 2C Feb15Keira McLeanNo ratings yet
- Group 2 - Activity 7Document4 pagesGroup 2 - Activity 7Zofia RanadaNo ratings yet
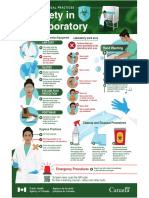
- Biosafety in The LaboratoryDocument1 pageBiosafety in The LaboratoryALFARO CHAT CARMINA ROSARIONo ratings yet
- 31Document15 pages31Amit TamboliNo ratings yet
- What Is Bisexual - Google SearchDocument1 pageWhat Is Bisexual - Google SearchYe etNo ratings yet
- Medial Plantar Flap For Hand ReconstructionDocument7 pagesMedial Plantar Flap For Hand ReconstructionMiguel JohnsonNo ratings yet