Professional Documents
Culture Documents
Management of Duodenal Trauma: Review
Management of Duodenal Trauma: Review
Uploaded by
AladesuruOlumideAdewaleCopyright:
Available Formats
You might also like
- Post Test 5Document18 pagesPost Test 5amarisanti98% (49)
- AtlsDocument9 pagesAtlsabjah100% (1)
- Abdominal TraumaDocument52 pagesAbdominal TraumaDONALD UNASHENo ratings yet
- Jay Patrick Vitamin C ArticlesDocument63 pagesJay Patrick Vitamin C ArticlesKrys Weaver0% (1)
- Management of Duodenal Trauma: Chinese Journal of Traumatology (English Edition) February 2011Document5 pagesManagement of Duodenal Trauma: Chinese Journal of Traumatology (English Edition) February 2011dr muddssar sattarNo ratings yet
- Evaluation and Management of Splenic Injury in Blunt Abdominal TraumaDocument32 pagesEvaluation and Management of Splenic Injury in Blunt Abdominal TraumaImam Hakim SuryonoNo ratings yet
- Multilevel Duodenal Injury After Blunt TraumaDocument5 pagesMultilevel Duodenal Injury After Blunt TraumaHanny RusliNo ratings yet
- WES GuidelineDocument28 pagesWES Guidelinesolo surgical forumNo ratings yet
- Surgicalmanagementof Abdominaltrauma: Hollow Viscus InjuryDocument11 pagesSurgicalmanagementof Abdominaltrauma: Hollow Viscus Injurysyairodhi rodziNo ratings yet
- Blunt Abdominal Trauma: Severity Factors in Hollow Viscus InjuriesDocument4 pagesBlunt Abdominal Trauma: Severity Factors in Hollow Viscus InjuriesRajan KarmakarNo ratings yet
- A1504050119 PDFDocument19 pagesA1504050119 PDFImam Hakim SuryonoNo ratings yet
- Trauma ColonDocument7 pagesTrauma Colonricardo arreguiNo ratings yet
- Posterior Urethral Valves (PUV) - Children's Hospital of PhiladelphiaDocument5 pagesPosterior Urethral Valves (PUV) - Children's Hospital of PhiladelphiaAndri Feisal NasutionNo ratings yet
- V23I2 05 FREE DrChouhan PDFDocument7 pagesV23I2 05 FREE DrChouhan PDFBimo PramestaNo ratings yet
- The Management of Pancreatic Injuries: JEJ Krige, E Jonas, SR Thomson and SJ BeningfieldDocument11 pagesThe Management of Pancreatic Injuries: JEJ Krige, E Jonas, SR Thomson and SJ BeningfieldHenry Espinoz ChavNo ratings yet
- EScholarship UC Item 14n977sgDocument7 pagesEScholarship UC Item 14n977sgcindyamandaNo ratings yet
- Urological Injuries During Colorectal SurgeryDocument8 pagesUrological Injuries During Colorectal Surgeryfatima chrystelle nuñalNo ratings yet
- Tbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite: DOI: 10.1590/S0100-69912014000300016Document4 pagesTbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite: DOI: 10.1590/S0100-69912014000300016Hanny RusliNo ratings yet
- American College of Surgeons (ACS)Document8 pagesAmerican College of Surgeons (ACS)perkakas78No ratings yet
- Duodenal Trauma: Luke R Johnston, Gary Wind and Matthew J BradleyDocument9 pagesDuodenal Trauma: Luke R Johnston, Gary Wind and Matthew J BradleyHenry Espinoz ChavNo ratings yet
- Abdomen CerradoDocument32 pagesAbdomen CerradoNina JácomeNo ratings yet
- B - Bile Duct Injuries in The Era of Laparoscopic Cholecystectomies - 2010Document16 pagesB - Bile Duct Injuries in The Era of Laparoscopic Cholecystectomies - 2010Battousaih1No ratings yet
- Management of Duodenal InjuriesDocument11 pagesManagement of Duodenal InjuriesZam HusNo ratings yet
- 1 PB PDFDocument11 pages1 PB PDFTheodore LiwonganNo ratings yet
- Abdomen TraumaDocument74 pagesAbdomen TraumajeevanNo ratings yet
- Pancreatic TraumaDocument11 pagesPancreatic TraumaAriniDwiYulianNo ratings yet
- Rhode Island Hospital: Related Emedicine TopicsDocument6 pagesRhode Island Hospital: Related Emedicine TopicsApril Shane OreiroNo ratings yet
- Erik Pancreatic TraumaDocument31 pagesErik Pancreatic TraumaIgnatius JesinNo ratings yet
- Complicationsafter Pancreaticoduodenectomy: Robert SimonDocument10 pagesComplicationsafter Pancreaticoduodenectomy: Robert SimonŞükriye AngaNo ratings yet
- Clinical Review: Modern Management of Splenic TraumaDocument7 pagesClinical Review: Modern Management of Splenic TraumaputraNo ratings yet
- Diagnosis and Treatment of Perforated or Bleeding Peptic Ulcers 2013 WSES PositionDocument15 pagesDiagnosis and Treatment of Perforated or Bleeding Peptic Ulcers 2013 WSES PositionDauz ArashNo ratings yet
- 1757 7241 17 13 PDFDocument5 pages1757 7241 17 13 PDFzafira anandaNo ratings yet
- DPLDocument5 pagesDPLngenevaNo ratings yet
- Peitzman Trauma HepáticoDocument11 pagesPeitzman Trauma HepáticoLety Carmona ArevaloNo ratings yet
- Blunt Abdominal TraumaDocument24 pagesBlunt Abdominal TraumaDen SinyoNo ratings yet
- 3Document8 pages3polomska.kmNo ratings yet
- Gastroduodenal PerforationDocument4 pagesGastroduodenal PerforationMaresp21No ratings yet
- Abdominal TraumaDocument10 pagesAbdominal TraumadeddybedahmksNo ratings yet
- Editorial - Operative Strategies in Pancreatic Trauma - Keep It Safe and SimpleDocument4 pagesEditorial - Operative Strategies in Pancreatic Trauma - Keep It Safe and SimpleFauz RamadhanNo ratings yet
- 1 s2.0 S2213576621002050 MainDocument6 pages1 s2.0 S2213576621002050 MainHusnul HanifaNo ratings yet
- Jiang 2012Document9 pagesJiang 2012DH SiriruiNo ratings yet
- 10 Yang Sebenarnya PDFDocument29 pages10 Yang Sebenarnya PDFSriarbiatiNo ratings yet
- Delayed Presentation of Isolated Jejunal Perforation Following Accidental TraumaDocument2 pagesDelayed Presentation of Isolated Jejunal Perforation Following Accidental TraumapricillyaNo ratings yet
- Operative Management of Anastomotic Leaks After Colorectal SurgeryDocument6 pagesOperative Management of Anastomotic Leaks After Colorectal SurgeryJorge OsorioNo ratings yet
- Current Therapy of Trauma and Surgical Critical CareDocument4 pagesCurrent Therapy of Trauma and Surgical Critical CareAgung TananNo ratings yet
- Duodenal Injuries ReviewDocument7 pagesDuodenal Injuries Revieweztouch12No ratings yet
- Art TH 2012Document9 pagesArt TH 2012Pamela ParedesNo ratings yet
- Current Management of Hepatic TraumaDocument11 pagesCurrent Management of Hepatic TraumaPerla RuizNo ratings yet
- 3 BaruDocument17 pages3 BaruAnditha Namira RSNo ratings yet
- Challenges in The Maagement of Pancreatic and Duodenal InjuriesDocument6 pagesChallenges in The Maagement of Pancreatic and Duodenal InjuriesOpl OplNo ratings yet
- Via BiliarDocument7 pagesVia Biliarahs ahnNo ratings yet
- Duodenal Injuries: E. Degiannis and K. BoffardDocument7 pagesDuodenal Injuries: E. Degiannis and K. BoffardDaniel Suarez ParapatNo ratings yet
- Abdominal Trauma, PenetratingDocument10 pagesAbdominal Trauma, PenetratingdeddybedahmksNo ratings yet
- Kumar - Burst Abdomen Related Factor and Postoperative Challenge For SurgeonsDocument5 pagesKumar - Burst Abdomen Related Factor and Postoperative Challenge For Surgeonsrhyzik reeNo ratings yet
- TraumaDocument10 pagesTraumaIda_Maryani94No ratings yet
- Renal Trauma Medscape PDFDocument21 pagesRenal Trauma Medscape PDFPatricia Prabawati LCNo ratings yet
- Duodenal Injuries: E. Degiannis and K. BoffardDocument7 pagesDuodenal Injuries: E. Degiannis and K. BoffardriftaNo ratings yet
- Analysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerDocument10 pagesAnalysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerNurul Fitrawati RidwanNo ratings yet
- GuidelinesDocument26 pagesGuidelinesmsc3nNo ratings yet
- Ab PenetranteDocument29 pagesAb PenetranteNina JácomeNo ratings yet
- Classification and Management of Bile Duct Injuries: EditorialDocument6 pagesClassification and Management of Bile Duct Injuries: EditorialSINAN SHAWKATNo ratings yet
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDocument10 pagesAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahNo ratings yet
- Case Studies of Postoperative Complications after Digestive SurgeryFrom EverandCase Studies of Postoperative Complications after Digestive SurgeryNo ratings yet
- Leg or Foot Amputation Pref CardDocument2 pagesLeg or Foot Amputation Pref CardPerrilyn PereyNo ratings yet
- Anamesis & Fisis BedahDocument15 pagesAnamesis & Fisis BedahIriamana Liasyarah MarudinNo ratings yet
- Chest and Abdominal Injuries: Forensic Medicine by Yazan AbueidehDocument54 pagesChest and Abdominal Injuries: Forensic Medicine by Yazan AbueidehRayyan Alali100% (1)
- TecarDocument9 pagesTecarMarco PastoreNo ratings yet
- 9-12 BurnsDocument32 pages9-12 BurnsralukNo ratings yet
- Basic Clinical SkillsDocument15 pagesBasic Clinical SkillsPriza RazunipNo ratings yet
- HemoperitoneumDocument14 pagesHemoperitoneumMiguel MuunguiiaNo ratings yet
- TrumaDocument13 pagesTrumaShrestha Anjiv100% (1)
- Research Paper RaptorDocument3 pagesResearch Paper Raptorapi-318114801No ratings yet
- National Registry Skill SheetsDocument21 pagesNational Registry Skill SheetsKemzo AbarquezNo ratings yet
- Trauma Triad of DeathDocument5 pagesTrauma Triad of DeathTomNo ratings yet
- TLS Chapter1Document27 pagesTLS Chapter1TeojNo ratings yet
- PJ Medical HandbookDocument210 pagesPJ Medical HandbookJared A. Lang100% (3)
- Recognition & Treatment of Pneumothorax Hemothorax, Flail Chest, Stove in ChestDocument59 pagesRecognition & Treatment of Pneumothorax Hemothorax, Flail Chest, Stove in ChestAnusha VergheseNo ratings yet
- Accident and Emergency MedicineDocument391 pagesAccident and Emergency MedicineKhalid Labadi100% (7)
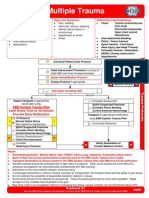
- Multiple Trauma: EMS System Trauma Plan Limit Scene Time To 10 Minutes Provide Early NotificationDocument1 pageMultiple Trauma: EMS System Trauma Plan Limit Scene Time To 10 Minutes Provide Early NotificationKelly JacksonNo ratings yet
- Primary SurveyDocument25 pagesPrimary Surveyapi-98304344No ratings yet
- Fire Works InjuryDocument39 pagesFire Works Injurynnaesor_1091No ratings yet
- 1 Early Management of Trauma Patient in The HospitalDocument23 pages1 Early Management of Trauma Patient in The HospitalkgnmatinNo ratings yet
- Zygomatic Bone FracturesDocument5 pagesZygomatic Bone FracturesAgung SajaNo ratings yet
- Abdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureDocument6 pagesAbdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureEvelyn GrandaNo ratings yet
- Chemical Eye Injuries PDFDocument4 pagesChemical Eye Injuries PDFGeraldine TGNo ratings yet
- Emergensi Urologi UiiDocument83 pagesEmergensi Urologi UiitrianaamaliaNo ratings yet
- Clinical Skill Handout Forensic Medicine and MedicolegalDocument20 pagesClinical Skill Handout Forensic Medicine and MedicolegalCici MutiaNo ratings yet
- Preparation of The Resuscitation Room and PatientDocument7 pagesPreparation of The Resuscitation Room and PatientRaydoon SadeqNo ratings yet
- AllRefer Health - PerichondritisDocument2 pagesAllRefer Health - PerichondritisandosaputraNo ratings yet
- Disaster Management Plan: Sir J.J. Group of Hospitals, MumbaiDocument100 pagesDisaster Management Plan: Sir J.J. Group of Hospitals, MumbaiektapatelbmsNo ratings yet
Management of Duodenal Trauma: Review
Management of Duodenal Trauma: Review
Uploaded by
AladesuruOlumideAdewaleOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Duodenal Trauma: Review
Management of Duodenal Trauma: Review
Uploaded by
AladesuruOlumideAdewaleCopyright:
Available Formats
. 61 .
Chinese Journal of Traumatology 2011; 14(1):61-64
Review
Management of duodenal trauma
CHEN Guo-qing and YANG Hua*
AbstractDuodenal trauma is uncommon but
nowadays seen more and more frequently due to the increased automobile accidents and violent events. The management of duodenal trauma can be complicated, especially
when massive injury to the pancreatic-duodenal-biliary complex occurs simultaneously. Even the patients receive surgeries in time, multiple postoperative complications and high
mortality are common. To know and manage duodenal
trauma better, we searched the recent related literature in
PubMed by the keywords of duodenal trauma, therapy, di-
agnosis and abdomen. It shows that because the diagnosis
and management are complicated and the mortality is high,
duodenal trauma should be treated in time and tactfully.
And application of new technology can help improve the
management. In this review, we discussed the incidence,
diagnosis, management, and complications as well as mortality of duodenal trauma.
Key words: Duodenum; Wounds and injuries;
Diagnosis; Therapeutics
related reviews and extracted the useful information they
provided. Then we searched every related study in these
reviews and found the needed information. Some of the
references were also the source of information. Finally
twelve studies were included and we reviewed the information about incidence, diagnosis, management, complications after surgery and mortality. The detailed information we obtained is shown as follows.
uodenal trauma is not often encountered in
clinic but recently it has an increased incidence because of frequent automobile accidents and violent events.1 Due to its complicated
anatomies, the diagnosis of duodenal trauma is difficult.
The diagnostic accuracy is low and the rate of missed
diagnosis is high. After duodenal trauma is confirmed,
a surgery should be carried out as soon as possible.
And the surgery should be given according to the location of trauma and the adjacent organs. However, even
the surgery is applied in time, the incidence of complications and mortality rate are still high.
In order to review the diagnosis and management of
duodenal trauma, we searched the recent related literature in PubMed by the keywords of duodenal trauma,
therapy, diagnosis and abdomen. We first retrieved the
DOI: 10.3760/cma.j.issn.1008-1275.2011.01.012
Department of General Surgery, Xingqiao Hospital,
Third Military Medical University, Chongqing 400037, China
(Chen GQ and Yang H)
*Corresponding author: Tel: 86-23-68755705, E-mail:
Chin J Traumatol 2011; 14(1):61-64
Incidence
Due to the increased incidence of traffic accidents
and unpredicted injuries, duodenal injuries are seen
more and more frequently.1 The reported incidence of
duodenal injury ranges from 3.7% to 5% in the literature and it is often accompanied by other abdominal
injuries because of the close anatomic relationship to
the liver, gallbladder, pancreas, etc.2 The majority of
duodenal injuries are caused by penetrating trauma.
Blunt injury is infrequent but difficult to diagnose because of its vague clinical symptoms and signs. It is
reported that the second portion of the duodenum is
injured most commonly, approximately in one third of
the cases reported.3
hwbyang@126.com
This research was supported by the National Natural
Science Foundation of China (NSFC 30973113; NSFC
81020108023) and Chongqing Science & Technology
Commission (CSTC2008BA5006).
Diagnosis
The anatomy of the duodenum is unique and complex because of its close relationship to adjacent
structures. Lying deep within the abdomen, the duode-
. 62 .
num is well protected in the retroperitoneal space.
Duodenal trauma has such clinical characteristics as
follows: (1) low diagnostic accuracy before operation,
with the rate of definite diagnosis before operation always below 10%,4 (2) accompanied by other injuries,
due to the special and complicated anatomy of the
duodenum, (3) high incidence of missed diagnosis during operation, which can reach 20%,5 and (4) high incidence of postoperative complications and mortality rate,
which can reach as high as 50%.6
The diagnostic accuracy of duodenum injury is low
because it has no specifical clinical symptoms and
signs. And because of the special anatomy of
duodenum, the injury may not present with any peritoneal irritation sign, especially when the second and third
parts of duodenum are injured. If other abdominal organs are injured simultaneously, the diagnosis would
become more confusing. It has been shown that if the
interval between injury and operation is longer than 24
hours, the injury would be considered as a severe one,7
from which we can see the importance of early
diagnosis. Thus the following clinical signs detected
should be particularly emphasized: (1) abdominal pain
especially when the right upper quadrant is injured. And
if the pain is intensified progressively with apparent peritoneal stimulation and radiation pain to the small of the
back, the duodenum is very likely injured. (2) Retching
or vomiting with blood in the vomitus. (3) Abdominal distension especially in the upper quadrant with infrequent
or muted borborygmus. (4) Anterior sacral crepitus in
digital rectal examination. (5) Detection of fluid like bile
or intestinal juice by diagnostic abdominocentesis.
However, surgeons need to know that negative results
cannot exclude the possibility of duodenum injury.
Abdominal plain films, ultrasonic test and CT scan
can also help the diagnosis of duodenum injury. Retroperitoneal air, free intraperitoneal air or other signs such
as obliteration of the psoas muscle shadow and scoliosis of the lumbar vertebrae can give a clue of injury.8
Under the circumstance of absence of positive signs,
air or water-soluble radiopaque contrast medium can
be injected through a nasogastric tube just before the
abdominal film is taken. If leakage happens, rupture of
duodenum can be confirmed. Barium is forbidden, as it
is hard to clear up during surgery and may cause infection after surgery.
Chinese Journal of Traumatology 2011; 14(1):61-64
Laparoscopy also helps diagnosis. If possible,
duodenoscopy can find the rupture directly, but unfortunately it is not suitable for traumatic patients. Although
routine laboratory tests are not helpful in the preoperative diagnosis of duodenal rupture, some authors find
that the serum amylase is an important marker. Serum
amylase is elevated in 50% of patients with duodenal
or upper gastrointestinal injury.9
Explorative laparotomy remains the ultimate diagnostic test if a high degree of suspicion of duodenal injury continues. The explorative procedures should be
careful, comprehensive, accurate and quick. The duodenum should be explored if such signs appear: (1) free
gas or fluid looking like bile with undetermined origin; (2)
extraction of intestinal juice or fluid like bile from retroperitoneal hematoma; and (3) edema, hematoma, ecchymosis or crepitus in the periduodenal retroperitoneum
or root of mesentery and mesocolon. It requires a careful detection for an accompanied injury to the pancreas
as well as the bile duct and the ampulla, especially
when the second portion of duodenum is injured. Severe duodenal injury, according to Snyder and his
coworkers10, is associated with the following factors: (1)
missile or blunt injury; (2) injury of the first or second
portion of the duodenum; and (3) adjacent common duct
injury. Besides if serum amylase level is elevated, a diligent search for duodenal rupture is required. The presence of a normal serum amylase level, however, does
not exclude a duodenal injury.
Management
The principle of duodenal injury treatment is to take
the overall situation into account and handle matters in
order of importance and urgency. Blocksom and his
coworkers11 reported that if the systolic pressure is lower
than 90 mm Hg before surgery, the mortality can reach
46%; and if the patient needs a transfusion more than
1 000 ml, his hospital stay will be apparently longer.
So we should pay attention to controlling bleeding, correcting shock and preventing infection during the early
treatment of duodenum injury. At the same time, patients need to receive surgeries as soon as possible to
control bleeding completely, correct shock further and
recover the intestinal continuity. The operation methods should be based on the factors of injury site and
type, time interval, individual situation and severity of
peritoneum pollution.
. 63 .
Chinese Journal of Traumatology 2011; 14(1):61-64
The vast majority of duodenal injuries may be managed by simple procedures such as debridement and
primary repair or resection and anastomosis. The detailed choices of operation are as follows.
For intramural haematoma, which develops in the
submucosal or subserosal layers, it is not perforated.
Open the serosa, evacuate the haematoma without violating the mucosa and repair the wall of bowel carefully.
However, controversially others believe that operation
will increase the incidence of perforation and to leave
the hematoma intact is better. Nasogastric decompression after operation is enough.12
If the range of duodenum injury is less than 50% of
the circumference, with regular injury border, adequate
blood supply and without serious peritoneum pollution,
the injury could be closed transversely and the decompression of duodenum could be achiev ed by
jejunostomy. It is believed that 75%-85% of duodenum
injury could be closed primarily and the incidence of
duodenal fistula is less than 10%.13
If the range of duodenum injury is more than 50% of
the circumference or primary closure of the defect may
narrow the lumen of the bowel or result in undue tension and subsequent breakdown of the suture lines,
segment al resection and primary end-to-end
duodenoduodenostomy are advised, especially when
the first, second or third part of duodenum is injured.14 If
a large part of duodenum is lost, suture of two ends will
be impossible without causing undue tension on the
suture line. If a large tissue of the first part of duodenum is lost, surgeries of duodenal diverticulization
should be carried out, which include closure of the
duodenal injury, gastric antrectomy with end-to-side
gastrojejunostomy, tube duodenostomy, and generous
drainage in the region of the duodenal repair.15 The main
problem of duodenal diverticulization is that it is a timeconsuming operation, and thus not recommended in
hemodynamically unstable patients or when several
accompanied injuries are presented. Otherwise if such
injury is distal to the ampulla of Vater, closure of distal
duodenum and Roux-en-Y duodenojejunostomy is
appropriate. If the injury happens to the second part of
duodenum, because of the limited mobilization of this
part, a direct anastomosis of Roux-en-Y over the injury
in an end-to-side fashion is appropriate. This method
can be also applied to other parts when the primary
anastomosis is impossible.
If the patient has massiv e peripancreatic
hemorrhage, proximal pancreatic duct or ampullary injuries that preclude the possibility of reconstruction,
pancreaticoduodenectomy should be applied.16 Snyder
reported that ampullary injuries had an incidence of only
3%. Howerer in a study of Asensio and colleagues17
which included 170 pat ients who underwent
pancreaticoduodenectomy in 50 reported series, the
overall mortality rate reached 33%. So pancreaticoduodenectomy should be applied carefully.
Finally, it should be emphasized that the best operation methods are those relatively simple and close
to physiological condition ones, such as primary suture,
tube duodenostomy and initial anastomosis. In
gastrostomy, duodenostomy or jejunostomy, a drainage tube should be used. It is applied for decompression of the duodenum and protection of the duodenal
suture line. It had fav orable results with tube
decompression: a fistula rate of 2.3% with tube decompression and 11.8% without.18 External drainage should
also be performed because of the early detection and
control of duodenal fistula.
Complications and mortality
The most serious complication following the treatment of duodenal injury is duodenal fistula. In a collective review of 15 series containing 1 408 patients with
duodenal injuries, Asensio and colleagues17 reported
an average incidence of duodenal fistula for 6.6%. Other
complications reported with duodenal trauma include
intra-abdominal abscess, pancreatitis, duodenal obstruction and bile duct fistula. The overall mortality rate
of duodenal injuries remains to be significant, with an
average incidence of 17%.
Conclusion
Exploratory laparotomy remains the final diagnostic test if a high suspicion of duodenal injury continues
after all auxiliary examinations are applied. Most duodenal injuries can be managed by simple repair. More
complicated injuries need more sophisticated operation techniques and are followed by a high incidence of
postoperative complications especially the duodenal
fistula and high mortality. Tube decompression and
external drainage are necessary and helpful. The
perioperative nutrition support and reasonable applica-
. 64 .
Chinese Journal of Traumatology 2011; 14(1):61-64
tion of antibiotics are also beneficial.
9. Asensio JA, Demetriades D, Hanpeter DE, et al. Management of pancreatic injuries. Curr Probl Surg 1999;36(5):325-419.
REFERENCES
10. Snyder WH 3rd, Weigelt JA, Watkins WL, et al. The surgical management of duodenal trauma. Precepts based on a review
1. Ivatury RR. Duodenal injuries: small but lethal lesions.
Cirujano General 2003; 25(1):59-65.
of 247 cases. Arch Surg 1980;115(4):422-429.
11. Blocksom JM, Tyburski JG, Sohn RL, et al. Prognostic
2. Fraga GP, Biazotto G, Villaca MP, et al. Duodenal trauma:
determinants in duodenal injuries. Am Surg 2004;70(3):248-255.
factors related to morbimortality. Rev Col Bras Cir 2008;35(2):
12. Degiannis E, Boffard K. Duodenal injuries. Br J Surg 2000;
94-102.
87:1473-1479.
3. Girgin S, Gedik E, Yagmur Y, et al. Management of duode-
13. Asensio JA, Petrone P, Roldan G, et al. Pancreatic and
nal injury: our experience and the value of tube duodenostomy.
duodenal injuries. Complex and lethal. Scand J Surg 2002;91(1):
Ulus Travma Acil Cerrahi Derg 2009;15(5):467-472.
81-86.
4. Cogbill TH, Moore EE, Feliciano DV, et al. Conservative
14. Timaran CH, Martinez O, Ospina JA. Prognostic factors
management of duodenal trauma: a multicenter perspective. J
and management of civilian penetrating duodenal trauma. J Trauma
Trauma 1990;30(12):1469-1475.
1999;47(2):330-335.
5. Astarcioglu H, Kocdor MA, Sokmen S, et al. Comparison
15. Ginzburg E, Carrillo EH, Sosa JL, et al. Pyloric exclusion
of different surgical repairs in the treatment of experimental duode-
in the management of duodenal trauma: is concomitant gastroje-
nal injuries. Am J Surg 2001;181(4):309-312.
junostomy necessary? Am Surg 1997;63(11):964-966.
6. Wisner DH, Victor NS, Holcroft JW. Priorities in the man-
16. Digiannis E, Saasdia R. Controversies in management of
agement of multiple traumas: intracranial versus intra-abdominal
penetrating injuries of the pancreas. S Afr J Surg 1999;37(2):38-40.
injury. J Trauma 1993;35(2):271-276.
7. Brooks AJ, Boffard KD. Current technology: laparoscopic
surgery in Trauma. Trauma 1999;1:53-60.
8. Jayaraman MV, Mayo-Smith WW, Movson JS, et al. CT
17. Asensio JA, Feliciano DV, Britt LD, et al. Management of
duodenal injuries. Curr Probl Surg 1993;30(11):1023-1093.
18. Ivatury RR, Nassoura ZE, Simon RJ, et al. Complex duodenal injuries. Surg Clin North Am 1996;76(4):797-812.
of the duodenum: an overlooked segment gets its due. Radiographics
2001;21:S147-S160.
(Received September 30, 2010)
Edited by LIU Gui-e
You might also like
- Post Test 5Document18 pagesPost Test 5amarisanti98% (49)
- AtlsDocument9 pagesAtlsabjah100% (1)
- Abdominal TraumaDocument52 pagesAbdominal TraumaDONALD UNASHENo ratings yet
- Jay Patrick Vitamin C ArticlesDocument63 pagesJay Patrick Vitamin C ArticlesKrys Weaver0% (1)
- Management of Duodenal Trauma: Chinese Journal of Traumatology (English Edition) February 2011Document5 pagesManagement of Duodenal Trauma: Chinese Journal of Traumatology (English Edition) February 2011dr muddssar sattarNo ratings yet
- Evaluation and Management of Splenic Injury in Blunt Abdominal TraumaDocument32 pagesEvaluation and Management of Splenic Injury in Blunt Abdominal TraumaImam Hakim SuryonoNo ratings yet
- Multilevel Duodenal Injury After Blunt TraumaDocument5 pagesMultilevel Duodenal Injury After Blunt TraumaHanny RusliNo ratings yet
- WES GuidelineDocument28 pagesWES Guidelinesolo surgical forumNo ratings yet
- Surgicalmanagementof Abdominaltrauma: Hollow Viscus InjuryDocument11 pagesSurgicalmanagementof Abdominaltrauma: Hollow Viscus Injurysyairodhi rodziNo ratings yet
- Blunt Abdominal Trauma: Severity Factors in Hollow Viscus InjuriesDocument4 pagesBlunt Abdominal Trauma: Severity Factors in Hollow Viscus InjuriesRajan KarmakarNo ratings yet
- A1504050119 PDFDocument19 pagesA1504050119 PDFImam Hakim SuryonoNo ratings yet
- Trauma ColonDocument7 pagesTrauma Colonricardo arreguiNo ratings yet
- Posterior Urethral Valves (PUV) - Children's Hospital of PhiladelphiaDocument5 pagesPosterior Urethral Valves (PUV) - Children's Hospital of PhiladelphiaAndri Feisal NasutionNo ratings yet
- V23I2 05 FREE DrChouhan PDFDocument7 pagesV23I2 05 FREE DrChouhan PDFBimo PramestaNo ratings yet
- The Management of Pancreatic Injuries: JEJ Krige, E Jonas, SR Thomson and SJ BeningfieldDocument11 pagesThe Management of Pancreatic Injuries: JEJ Krige, E Jonas, SR Thomson and SJ BeningfieldHenry Espinoz ChavNo ratings yet
- EScholarship UC Item 14n977sgDocument7 pagesEScholarship UC Item 14n977sgcindyamandaNo ratings yet
- Urological Injuries During Colorectal SurgeryDocument8 pagesUrological Injuries During Colorectal Surgeryfatima chrystelle nuñalNo ratings yet
- Tbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite: DOI: 10.1590/S0100-69912014000300016Document4 pagesTbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite Tbe-Cite: DOI: 10.1590/S0100-69912014000300016Hanny RusliNo ratings yet
- American College of Surgeons (ACS)Document8 pagesAmerican College of Surgeons (ACS)perkakas78No ratings yet
- Duodenal Trauma: Luke R Johnston, Gary Wind and Matthew J BradleyDocument9 pagesDuodenal Trauma: Luke R Johnston, Gary Wind and Matthew J BradleyHenry Espinoz ChavNo ratings yet
- Abdomen CerradoDocument32 pagesAbdomen CerradoNina JácomeNo ratings yet
- B - Bile Duct Injuries in The Era of Laparoscopic Cholecystectomies - 2010Document16 pagesB - Bile Duct Injuries in The Era of Laparoscopic Cholecystectomies - 2010Battousaih1No ratings yet
- Management of Duodenal InjuriesDocument11 pagesManagement of Duodenal InjuriesZam HusNo ratings yet
- 1 PB PDFDocument11 pages1 PB PDFTheodore LiwonganNo ratings yet
- Abdomen TraumaDocument74 pagesAbdomen TraumajeevanNo ratings yet
- Pancreatic TraumaDocument11 pagesPancreatic TraumaAriniDwiYulianNo ratings yet
- Rhode Island Hospital: Related Emedicine TopicsDocument6 pagesRhode Island Hospital: Related Emedicine TopicsApril Shane OreiroNo ratings yet
- Erik Pancreatic TraumaDocument31 pagesErik Pancreatic TraumaIgnatius JesinNo ratings yet
- Complicationsafter Pancreaticoduodenectomy: Robert SimonDocument10 pagesComplicationsafter Pancreaticoduodenectomy: Robert SimonŞükriye AngaNo ratings yet
- Clinical Review: Modern Management of Splenic TraumaDocument7 pagesClinical Review: Modern Management of Splenic TraumaputraNo ratings yet
- Diagnosis and Treatment of Perforated or Bleeding Peptic Ulcers 2013 WSES PositionDocument15 pagesDiagnosis and Treatment of Perforated or Bleeding Peptic Ulcers 2013 WSES PositionDauz ArashNo ratings yet
- 1757 7241 17 13 PDFDocument5 pages1757 7241 17 13 PDFzafira anandaNo ratings yet
- DPLDocument5 pagesDPLngenevaNo ratings yet
- Peitzman Trauma HepáticoDocument11 pagesPeitzman Trauma HepáticoLety Carmona ArevaloNo ratings yet
- Blunt Abdominal TraumaDocument24 pagesBlunt Abdominal TraumaDen SinyoNo ratings yet
- 3Document8 pages3polomska.kmNo ratings yet
- Gastroduodenal PerforationDocument4 pagesGastroduodenal PerforationMaresp21No ratings yet
- Abdominal TraumaDocument10 pagesAbdominal TraumadeddybedahmksNo ratings yet
- Editorial - Operative Strategies in Pancreatic Trauma - Keep It Safe and SimpleDocument4 pagesEditorial - Operative Strategies in Pancreatic Trauma - Keep It Safe and SimpleFauz RamadhanNo ratings yet
- 1 s2.0 S2213576621002050 MainDocument6 pages1 s2.0 S2213576621002050 MainHusnul HanifaNo ratings yet
- Jiang 2012Document9 pagesJiang 2012DH SiriruiNo ratings yet
- 10 Yang Sebenarnya PDFDocument29 pages10 Yang Sebenarnya PDFSriarbiatiNo ratings yet
- Delayed Presentation of Isolated Jejunal Perforation Following Accidental TraumaDocument2 pagesDelayed Presentation of Isolated Jejunal Perforation Following Accidental TraumapricillyaNo ratings yet
- Operative Management of Anastomotic Leaks After Colorectal SurgeryDocument6 pagesOperative Management of Anastomotic Leaks After Colorectal SurgeryJorge OsorioNo ratings yet
- Current Therapy of Trauma and Surgical Critical CareDocument4 pagesCurrent Therapy of Trauma and Surgical Critical CareAgung TananNo ratings yet
- Duodenal Injuries ReviewDocument7 pagesDuodenal Injuries Revieweztouch12No ratings yet
- Art TH 2012Document9 pagesArt TH 2012Pamela ParedesNo ratings yet
- Current Management of Hepatic TraumaDocument11 pagesCurrent Management of Hepatic TraumaPerla RuizNo ratings yet
- 3 BaruDocument17 pages3 BaruAnditha Namira RSNo ratings yet
- Challenges in The Maagement of Pancreatic and Duodenal InjuriesDocument6 pagesChallenges in The Maagement of Pancreatic and Duodenal InjuriesOpl OplNo ratings yet
- Via BiliarDocument7 pagesVia Biliarahs ahnNo ratings yet
- Duodenal Injuries: E. Degiannis and K. BoffardDocument7 pagesDuodenal Injuries: E. Degiannis and K. BoffardDaniel Suarez ParapatNo ratings yet
- Abdominal Trauma, PenetratingDocument10 pagesAbdominal Trauma, PenetratingdeddybedahmksNo ratings yet
- Kumar - Burst Abdomen Related Factor and Postoperative Challenge For SurgeonsDocument5 pagesKumar - Burst Abdomen Related Factor and Postoperative Challenge For Surgeonsrhyzik reeNo ratings yet
- TraumaDocument10 pagesTraumaIda_Maryani94No ratings yet
- Renal Trauma Medscape PDFDocument21 pagesRenal Trauma Medscape PDFPatricia Prabawati LCNo ratings yet
- Duodenal Injuries: E. Degiannis and K. BoffardDocument7 pagesDuodenal Injuries: E. Degiannis and K. BoffardriftaNo ratings yet
- Analysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerDocument10 pagesAnalysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerNurul Fitrawati RidwanNo ratings yet
- GuidelinesDocument26 pagesGuidelinesmsc3nNo ratings yet
- Ab PenetranteDocument29 pagesAb PenetranteNina JácomeNo ratings yet
- Classification and Management of Bile Duct Injuries: EditorialDocument6 pagesClassification and Management of Bile Duct Injuries: EditorialSINAN SHAWKATNo ratings yet
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDocument10 pagesAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahNo ratings yet
- Case Studies of Postoperative Complications after Digestive SurgeryFrom EverandCase Studies of Postoperative Complications after Digestive SurgeryNo ratings yet
- Leg or Foot Amputation Pref CardDocument2 pagesLeg or Foot Amputation Pref CardPerrilyn PereyNo ratings yet
- Anamesis & Fisis BedahDocument15 pagesAnamesis & Fisis BedahIriamana Liasyarah MarudinNo ratings yet
- Chest and Abdominal Injuries: Forensic Medicine by Yazan AbueidehDocument54 pagesChest and Abdominal Injuries: Forensic Medicine by Yazan AbueidehRayyan Alali100% (1)
- TecarDocument9 pagesTecarMarco PastoreNo ratings yet
- 9-12 BurnsDocument32 pages9-12 BurnsralukNo ratings yet
- Basic Clinical SkillsDocument15 pagesBasic Clinical SkillsPriza RazunipNo ratings yet
- HemoperitoneumDocument14 pagesHemoperitoneumMiguel MuunguiiaNo ratings yet
- TrumaDocument13 pagesTrumaShrestha Anjiv100% (1)
- Research Paper RaptorDocument3 pagesResearch Paper Raptorapi-318114801No ratings yet
- National Registry Skill SheetsDocument21 pagesNational Registry Skill SheetsKemzo AbarquezNo ratings yet
- Trauma Triad of DeathDocument5 pagesTrauma Triad of DeathTomNo ratings yet
- TLS Chapter1Document27 pagesTLS Chapter1TeojNo ratings yet
- PJ Medical HandbookDocument210 pagesPJ Medical HandbookJared A. Lang100% (3)
- Recognition & Treatment of Pneumothorax Hemothorax, Flail Chest, Stove in ChestDocument59 pagesRecognition & Treatment of Pneumothorax Hemothorax, Flail Chest, Stove in ChestAnusha VergheseNo ratings yet
- Accident and Emergency MedicineDocument391 pagesAccident and Emergency MedicineKhalid Labadi100% (7)
- Multiple Trauma: EMS System Trauma Plan Limit Scene Time To 10 Minutes Provide Early NotificationDocument1 pageMultiple Trauma: EMS System Trauma Plan Limit Scene Time To 10 Minutes Provide Early NotificationKelly JacksonNo ratings yet
- Primary SurveyDocument25 pagesPrimary Surveyapi-98304344No ratings yet
- Fire Works InjuryDocument39 pagesFire Works Injurynnaesor_1091No ratings yet
- 1 Early Management of Trauma Patient in The HospitalDocument23 pages1 Early Management of Trauma Patient in The HospitalkgnmatinNo ratings yet
- Zygomatic Bone FracturesDocument5 pagesZygomatic Bone FracturesAgung SajaNo ratings yet
- Abdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureDocument6 pagesAbdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureEvelyn GrandaNo ratings yet
- Chemical Eye Injuries PDFDocument4 pagesChemical Eye Injuries PDFGeraldine TGNo ratings yet
- Emergensi Urologi UiiDocument83 pagesEmergensi Urologi UiitrianaamaliaNo ratings yet
- Clinical Skill Handout Forensic Medicine and MedicolegalDocument20 pagesClinical Skill Handout Forensic Medicine and MedicolegalCici MutiaNo ratings yet
- Preparation of The Resuscitation Room and PatientDocument7 pagesPreparation of The Resuscitation Room and PatientRaydoon SadeqNo ratings yet
- AllRefer Health - PerichondritisDocument2 pagesAllRefer Health - PerichondritisandosaputraNo ratings yet
- Disaster Management Plan: Sir J.J. Group of Hospitals, MumbaiDocument100 pagesDisaster Management Plan: Sir J.J. Group of Hospitals, MumbaiektapatelbmsNo ratings yet