Professional Documents
Culture Documents
Myths About Hypertension
Myths About Hypertension
Uploaded by
Del MabelCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- USMLE Step 1 Lecture Notes PharmacologyDocument165 pagesUSMLE Step 1 Lecture Notes PharmacologyAris OverallNo ratings yet
- Program at Glance WECOC 2021-Updated Juli 2021Document1 pageProgram at Glance WECOC 2021-Updated Juli 2021Bambang SupriadiNo ratings yet
- Practice Test Medical Surgical Nursing 150 Items PDFDocument9 pagesPractice Test Medical Surgical Nursing 150 Items PDFPondang Reviewers BulacanNo ratings yet
- A Rare Case of Peripartum CardiomyopathyDocument3 pagesA Rare Case of Peripartum CardiomyopathyKarina PuspaseruniNo ratings yet
- 2016 Guidelines For The Management of Thyroid Storm From Japan Thyroid AssociationDocument40 pages2016 Guidelines For The Management of Thyroid Storm From Japan Thyroid AssociationMartha RosanaNo ratings yet
- Etiology and Management of EdemaDocument14 pagesEtiology and Management of EdemaFavio Alvarez De BejarNo ratings yet
- Noncardiac Surgery For Children With Congenital Heart DiseaseDocument51 pagesNoncardiac Surgery For Children With Congenital Heart DiseaseJZNo ratings yet
- AneedzDocument60 pagesAneedzMjd ObiedNo ratings yet
- Patofisologi Gagal JantungDocument38 pagesPatofisologi Gagal JantungRizqy JoeandriNo ratings yet
- Venous CongestionDocument20 pagesVenous CongestionLittle Miss CeeNo ratings yet
- Shock in ObstetricsDocument38 pagesShock in ObstetricsBeulah AlexNo ratings yet
- Evaluation of The Adult With Dyspnea in The Emergency DepartmentDocument16 pagesEvaluation of The Adult With Dyspnea in The Emergency DepartmentmericenteNo ratings yet
- CARDIODocument34 pagesCARDIOKevin Patrick PadolinaNo ratings yet
- MS Practice Questions With RationaleDocument13 pagesMS Practice Questions With RationaleRey Gil Flee GabonadaNo ratings yet
- ESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDocument5 pagesESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDini SuhardiniNo ratings yet
- Syncope AFPDocument12 pagesSyncope AFP李英誠No ratings yet
- NCM 109 (Prelims) - Lesson 2Document18 pagesNCM 109 (Prelims) - Lesson 2nianNo ratings yet
- Kaplan Cirugia No Cardiaca PDFDocument584 pagesKaplan Cirugia No Cardiaca PDFNalemi JTNo ratings yet
- Salt & Fluid Management Programme: Information For Healthcare ProfessionalsDocument33 pagesSalt & Fluid Management Programme: Information For Healthcare ProfessionalsmelyanaNo ratings yet
- Cardiology FMDocument25 pagesCardiology FMtrushaNo ratings yet
- Cardiology HFDocument11 pagesCardiology HFdhayemaruNo ratings yet
- Critical Case in Congenital Heart Disease, What's The Sign and Initial Treatment For Them (Prof. Dr. Dr. Mulyadi M.djer, SpA (K) )Document69 pagesCritical Case in Congenital Heart Disease, What's The Sign and Initial Treatment For Them (Prof. Dr. Dr. Mulyadi M.djer, SpA (K) )tyesNo ratings yet
- Cardio RenalDocument11 pagesCardio RenalAgung WistaraNo ratings yet
- Domingo, Precious Mae TDocument56 pagesDomingo, Precious Mae Tbevzie datuNo ratings yet
- Kode Penjelasan Keterangan: ObgynDocument14 pagesKode Penjelasan Keterangan: Obgynanon_507132438No ratings yet
- BNP & Nt-Pro BNPDocument7 pagesBNP & Nt-Pro BNPyehezkieldwardNo ratings yet
- Mou&Sin&Exp&Gui&Cri&Car&1 STDocument642 pagesMou&Sin&Exp&Gui&Cri&Car&1 STDragutin PetrićNo ratings yet
- DigoxinDocument20 pagesDigoxinAbdulRehmanChaudaryNo ratings yet
- 2020-02 Report On Blu Room Heart PatientsDocument16 pages2020-02 Report On Blu Room Heart PatientsBlu RoomNo ratings yet
- Pulmonary EdemaDocument28 pagesPulmonary EdemaMohammed Elias100% (1)
Myths About Hypertension
Myths About Hypertension
Uploaded by
Del MabelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Myths About Hypertension
Myths About Hypertension
Uploaded by
Del MabelCopyright:
Available Formats
I.
Myths About Hypertension
1. Hypertension is an "asymptomatic" disease.
It is well-recognized that the majority of people with hypertension in the United States have stage 1 or 2 (mild or moderate) hypertension, and as a result might experience few or no symptoms during the early years of their hypertension. Remember, however, that hypertension does progressive damage to blood vessels, and the first symptom of untreated or inadequately-treated hypertension might be a disabling stroke or possibly a fatal heart attack. Congestive heart failure also is a common result of inadequately-treated hypertension. Be aware that the five-year mortality of individuals experiencing a first episode of congestive heart failure is 50 percent. Yet, for many hypertensive individuals, these major cardiovascular events are preventable with aggressive, optimal treatment and long-term control. It is also of particular interest that several recent clinical studies assessing quality of life measures have shown that treated and controlled hypertensive patients actually experience a better quality of life than those individuals in control groups. These studies suggest that there are in fact, subtle symptoms in untreated or uncontrolled hypertensive people that can actually be improved by aggressive treatment and control of blood pressure.
2. A "normal" systolic blood pressure equals 100 plus your age.
Until a decade ago, this statement was a commonly quoted assumption regarding the natural history of blood pressure with aging. It suggested that a systolic blood pressure of 170 was normal in a 70-year-old individual. Today, we know this to be absolutely false. We now have sufficient clinical evidence for older Americans with both systolic and diastolic hypertension, and particularly in isolated systolic hypertension (ISH), that verify the benefits of aggressive treatment of blood pressure in older Americans. There is very firm data supporting treatment of systolic blood pressure down to 150 mm Hg in older hypertensive people. Therefore, this marker is an appropriate initial goal in most older patients with ISH. For many, a blood pressure below 140/90 mm Hg represents an appropriate treatment goal today.
3. The systolic blood pressure does not matter if the diastolic blood pressure is below 90 mm Hg.
For many years, hypertension was classified on the basis of diastolic blood pressure, and the systolic blood pressure was not even considered. Recommendations for the treatment of hypertension were also based on diastolic blood pressure readings with no attention paid to the systolic reading. Fortunately, these misconceptions were corrected with studies during the past decade that addressed systolic blood pressure. We now know that the systolic blood pressure is actually a better predictor of cardiovascular risk (stroke, heart attack, congestive heart failure) than is the diastolic blood pressure.
4. Older patients will not take their antihypertensive medicines.
It has long been assumed that older hypertensive individuals are not optimally compliant with medicines prescribed for high blood pressure. It had been assumed that health beliefs or decreases in cognitive function with aging would necessarily result in a decrease in compliance with medicine regimens. To the contrary, studies in the elderly hypertensive patient population have revealed that the older subgroup over age 65 are not only more compliant with medicines prescribed in carefully controlled clinical trials, but they also achieve the target blood pressure goals in those studies in a higher percentage of cases. It is believed that the key is adequate education of the hypertensive patient, regardless of age. Health providers must offer adequate education regarding hypertension together with the importance and benefits of taking regular medicine.
5. Older patients seldom reach target blood pressure with treatment.
It has long been a myth that older patients have blood pressures that respond less well to antihypertensive treatment. Further, it has long been assumed that, when treated, it is difficult to achieve recommended target blood pressure goals. On the contrary, recent clinical trials in the elderly have also put this myth to rest with evidence that clearly demonstrates that older populations are not only more compliant, but also achieve target blood pressure goals in a higher percentage than younger people. Obviously, we must change the attitudes of both patients and providers to recognize the importance and potential benefits of aggressive treatment of high blood pressure in older Americans.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- USMLE Step 1 Lecture Notes PharmacologyDocument165 pagesUSMLE Step 1 Lecture Notes PharmacologyAris OverallNo ratings yet
- Program at Glance WECOC 2021-Updated Juli 2021Document1 pageProgram at Glance WECOC 2021-Updated Juli 2021Bambang SupriadiNo ratings yet
- Practice Test Medical Surgical Nursing 150 Items PDFDocument9 pagesPractice Test Medical Surgical Nursing 150 Items PDFPondang Reviewers BulacanNo ratings yet
- A Rare Case of Peripartum CardiomyopathyDocument3 pagesA Rare Case of Peripartum CardiomyopathyKarina PuspaseruniNo ratings yet
- 2016 Guidelines For The Management of Thyroid Storm From Japan Thyroid AssociationDocument40 pages2016 Guidelines For The Management of Thyroid Storm From Japan Thyroid AssociationMartha RosanaNo ratings yet
- Etiology and Management of EdemaDocument14 pagesEtiology and Management of EdemaFavio Alvarez De BejarNo ratings yet
- Noncardiac Surgery For Children With Congenital Heart DiseaseDocument51 pagesNoncardiac Surgery For Children With Congenital Heart DiseaseJZNo ratings yet
- AneedzDocument60 pagesAneedzMjd ObiedNo ratings yet
- Patofisologi Gagal JantungDocument38 pagesPatofisologi Gagal JantungRizqy JoeandriNo ratings yet
- Venous CongestionDocument20 pagesVenous CongestionLittle Miss CeeNo ratings yet
- Shock in ObstetricsDocument38 pagesShock in ObstetricsBeulah AlexNo ratings yet
- Evaluation of The Adult With Dyspnea in The Emergency DepartmentDocument16 pagesEvaluation of The Adult With Dyspnea in The Emergency DepartmentmericenteNo ratings yet
- CARDIODocument34 pagesCARDIOKevin Patrick PadolinaNo ratings yet
- MS Practice Questions With RationaleDocument13 pagesMS Practice Questions With RationaleRey Gil Flee GabonadaNo ratings yet
- ESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDocument5 pagesESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDini SuhardiniNo ratings yet
- Syncope AFPDocument12 pagesSyncope AFP李英誠No ratings yet
- NCM 109 (Prelims) - Lesson 2Document18 pagesNCM 109 (Prelims) - Lesson 2nianNo ratings yet
- Kaplan Cirugia No Cardiaca PDFDocument584 pagesKaplan Cirugia No Cardiaca PDFNalemi JTNo ratings yet
- Salt & Fluid Management Programme: Information For Healthcare ProfessionalsDocument33 pagesSalt & Fluid Management Programme: Information For Healthcare ProfessionalsmelyanaNo ratings yet
- Cardiology FMDocument25 pagesCardiology FMtrushaNo ratings yet
- Cardiology HFDocument11 pagesCardiology HFdhayemaruNo ratings yet
- Critical Case in Congenital Heart Disease, What's The Sign and Initial Treatment For Them (Prof. Dr. Dr. Mulyadi M.djer, SpA (K) )Document69 pagesCritical Case in Congenital Heart Disease, What's The Sign and Initial Treatment For Them (Prof. Dr. Dr. Mulyadi M.djer, SpA (K) )tyesNo ratings yet
- Cardio RenalDocument11 pagesCardio RenalAgung WistaraNo ratings yet
- Domingo, Precious Mae TDocument56 pagesDomingo, Precious Mae Tbevzie datuNo ratings yet
- Kode Penjelasan Keterangan: ObgynDocument14 pagesKode Penjelasan Keterangan: Obgynanon_507132438No ratings yet
- BNP & Nt-Pro BNPDocument7 pagesBNP & Nt-Pro BNPyehezkieldwardNo ratings yet
- Mou&Sin&Exp&Gui&Cri&Car&1 STDocument642 pagesMou&Sin&Exp&Gui&Cri&Car&1 STDragutin PetrićNo ratings yet
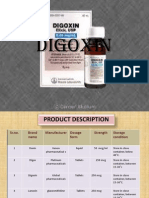
- DigoxinDocument20 pagesDigoxinAbdulRehmanChaudaryNo ratings yet
- 2020-02 Report On Blu Room Heart PatientsDocument16 pages2020-02 Report On Blu Room Heart PatientsBlu RoomNo ratings yet
- Pulmonary EdemaDocument28 pagesPulmonary EdemaMohammed Elias100% (1)