Professional Documents
Culture Documents
Health Care Industry in India
Health Care Industry in India
Uploaded by
Amit KumarOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Health Care Industry in India
Health Care Industry in India
Uploaded by
Amit KumarCopyright:
Available Formats
Health Care Industry In India A Paper Highlighting the Present Scenario and a Possible strategy to make the sector
attractive Submitted by: Rahul Raizada Email id: Rraizada@gmail.com Contact Address: B-18 Qutub Institutional Area New Delhi -16 FORE School of Management
Table of Contents I. Introduction. 4 II. Private Health Care Facilities and Providers. 4 A. Government Policy. 5 III. Utilization of Private Health Care Facilities. 5 IV. The Cost of Private Health Care. 6 A. Expenditure. 6 B. Financing. 6 V. Policy Concerns. 6 VI. Regulating the Private Health Care in India. 8 A. Current Regulations. 8 B. Assessment of Regulation. 9 VII. The Challenges Ahead and A Possible Strategy. 9 A. Health Infrastructure in Public Sector. 9 B. Financing related Issues. 10 C. Shape of Private Sector in Medicine. 11
D. Regulatory Issues. 12 1. Consumer Protection Act (COPRA) 12 2. Medical Council of India and State medical Councils (SMCs) 13 3. The Nursing Homes Act 13 VIII. References. 14 List of Tables Table 1: Typology of Regulations. 6
Glossary NHP National Health Policy O&M Operation and Maintenance PHC Public Healthcare Centers CHC Central healthcare Centers GDP Gross Domestic Product NGO Non Government Organization COPRA Consumer Protection Act
I. Introduction =============== The private sector plays an important role in India's health care delivery system. Through a wide network of health care facilities, this sector caters to the needs of both urban and rural populations and has expanded widely to meet increasing demands. Utilization patterns indicate that health care seekers depend highly on the private sector. Despite the widespread public infrastructure, a higher proportion of health services are provided by the private sector than by government facilities. The private health care sector has grown significantly over time. The growth of this sector has been further triggered by a number of factors, including a liberalized economic policy, rapid influx of medical technology, growing deficits of public sector hospitals, and a rising middle income class. Its growth has
profound implications for the existing character of the Indian health care system and its future course. Recent studies indicate that private health care significantly affects both the cost and quality of available health care services in India. Although cases of superfluous and high cost of services rendered by private physicians and hospitals have been reported, there is no evidence that these result in any greater use of public facilities. Significantly, despite the problems resulting from the growth of the private sector, there has been little effort to draw up appropriate market or regulatory mechanisms to ensure its desirable growth. This is unfortunate since it is well known that leaving the health care to the market forces does not necessarily lead to an effective and efficient health care system. The role of the state and self-regulatory bodies is important in minimizing the unintended and undesirable consequences emanating form the growth of the private sector. At some point of time it becomes imperative for the stakeholders to address the issues of equity, efficiency and quality of care in this sector. The paper makes an attempt to address the role of these stakeholders in addressing various concerns. The papers specifically discusses (a) the exiting status of regulations (self-regulation or government legislations) to monitor and control the private health care sector practices; (b) the performance of these legislations in ensuring appropriate development of this sector; and (c) The possible strategy for implementation of the reform process. This paper addresses these questions in the context of the experience of India. After describing the broad characteristics of the private health sector in India, it examines the major policy concerns originating from its growth. It assesses the current regulatory environment and its implications for the process of health reform.
II. Private Health Care Facilities and Providers ================================================ The structure of the health care system in India is complex and it includes various types of providers. These providers practice in different systems of medicines and facilities. The providers and facilities in India can be broadly classified by using three dimensions: ownership styles (public, not-for-profit, and for-profit); systems of medicine (allopathic, homeopathic, and traditional); and types of organization (hospitals, dispensaries, and clinics). These dimensions are interdependent and overlapping in nature. Using the ownership criterion, the health care system can be divided into four broad sectors: (1) The public sector, including government-run hospitals,
dispensaries, clinics, primary health care centers and sub-centers, and paramedics; (2) The not-for-profit sector, including voluntary health programs, charitable institutions, missions, churches, and trusts; (3) The organized private sector, including general practitioners (having at least a bachelor's degree or equivalent in medicine), private hospitals and small private hospitals (popularly known as nursing homes), registered medical practitioners, dispensaries and other licensed practitioners; and (4) The private informal sector, including practitioners not having any formal qualifications (e.g., faith healers, herbalists, priests, tantriks, hakims, and vaidyas).
A. Government Policy -------------------Improving public health for all is documented in the constitution of India as one of the primary duties of the state. To achieve this, the planning process of the country provides a broad framework to the states to develop their health services infrastructure, as well as facilities for medical education and research. Since the inception of the planning process, the state and central governments have experienced a number of constraints in implementing the health programs effectively. In 1982, the National Health Policy (NHP) acknowledged these constraints and suggested an integrated and comprehensive approach towards the future development of health care services. To mitigate the problem of limited resources, the policy document recommended that the states design processes to encourage the practice by private medical professionals and investment by non-government agencies in establishing curative centers. States were also encouraged to provide organized, logistical, financial and technical support to voluntary agencies active in the health field. The policy thrust of NHP in promoting the private and voluntary health curative services has been one important step towards providing clear direction to the states. These directions were supposed to help the state governments develop their own strategies to utilize untapped resources and strengthen their ability to meet the growing health needs of people.
III. Utilization of Private Health Care Facilities ================================================== The data and studies suggest that differences in income or location
(rural/urban) do not have much influence on the propensity to use different types of facilities. The private health care services are utilized by all social classes. In a survey of the utilization of health facilities by two slum communities in Bombay, found that both communities used private sector facilities more frequently for short-term and minor ailments. However, in acute cases of illnesses requiring hospitalization, they used public facilities, primarily for cost rather than quality considerations.
IV. The Cost of Private Health Care ===================================
A. Expenditure -------------Public expenditure on health care in India is composed of spending by central government, state governments, and local bodies. Private health care spending includes the out-of-pocket costs incurred by households and expenditure by the private non-household institutional sector. The share of private household and non-household expenditure has frequently been reported to be more than two-thirds of the total health expenditure. Total health expenditure as a percentage of the national domestic product was about 5 percent in 1997 (as suggested by studies). One can expect that, given the rate of inflation and the increase in the demand for health care services over the years, the expenditure in absolute terms must have gone up significantly.
B. Financing -----------The way health care expenditures are financed has important implications for the health care system. A study revealed that people borrowed about Rs. 28.52 per capita (about 16 percent of total health care expenditure) a year to finance their health costs. In some individual cases, borrowing was as high as their annual incomes. Insurance coverage for health care expenditure is very limited in India although the government initiated comprehensive health insurance schemes for the employees in the government and formal private sectors. In a recent survey it was recorded that only 4% of the workers availed this cover.
V. Policy Concerns ==================
It is very difficult to ascertain whether the presence of private health care provision has made any impact on health outcomes and whether the states having higher availability of private health care provision do really exhibit significant differences. It would require observing health status and utilization patterns over a long period of time. However, it could be correctly assumed that the utilization of the private health care facilities is quite significant and this would undoubtedly have an impact on health status. There are obviously both positive and negative aspects about the role of private health care institutions. On the negative side, the growth of private sector in the country has raised several controversies as regards quality, cost of care, equity and efficiency.
Some of major concerns are: i. The scale at which private health care services are produced since it is considered to have significant effect on the cost and quality. In a competitive market, the scale of operations is expected to be optimized by employing the best number and mix of services. This optimization should minimize the overall cost of operations and affect cost efficiency and effectiveness. ii. With the relatively large amount out-of-pocket costs incurred by households and expenditure by the private non-household institutional sector. Private household and non-household expenditure has frequently been reported to be more than two thirds of the total health expenditure. What is being spent on these services? Do people get their value of money? What do people do in case of catastrophic illnesses?
VI. Regulating the Private Health Care in India ===============================================
A. Current Regulations ---------------------The central and state governments in India have promulgated several pieces of legislation to safeguard the health of population. The existing set of regulations related to health care can be broadly divided into following three categories: i. Drugs Related
ii. Practice Related iii. Facilities Related Table 1: Typology of Regulations Aspects of Private Practice Legislations/Declarations/Standards Drug Related Pharmacy Act Drugs and Cosmetics Act Dangerous Drugs Act Drugs and Magic Remedies Act Drugs Control Act Drugs Price Order Poisons Act Medical and Toilet Preparation Act Narcotic Drugs and Psychotropic Substances Act Practice Related Criminal Law Civil Law (Law of Contract, Law of Tort) Consumer Protection Act Indian Medical Council Act Human Organ Transplant Act Medical Termination of Pregnancy Pre-natal Diagnostic Techniques (Regulation and Prevention of Misuse) Act Declaration of Geneva
Facilities (including Technology, Manpower) Related Nursing Home Act Nurses, Midwives and Health Visitors Act Public Nuisance Act Minimum Wage Act Bureau of Indian Standards
B. Assessment of Regulation --------------------------The laws pertaining to health care in India are effective in protecting the interests of the patients; but the main area of concern is about their proper enforcement. Some reasons, which could be attributed for these regulations and policy have remained a problem: i. The implementation and enforcement of rules and regulations have been weak. ii. Since health is a state subject in India, the response to different laws has varied from state to state (e.g., case of Nursing Home Act). iii. There has been considerable amount of resistance from various constituents of the private health care sector (particularly private providers) to accept in principle the applicability of certain regulation to their profession (e.g., Consumer Protection Act). iv. The response of the medical profession to develop rules, norms and various mechanisms for self-regulation has been poor (e.g., Medical Council Act). v. Many regulations have not been updated and, therefore, have lost their relevance (e.g., Nursing Home Act). vi. The ministries of health and other departments do not consider concerns related to private sector growth as a high priority on the policy agenda. With the new economic policy regime, it has become fashionable to say that the markets will take care of these concerns.
VII. The Challenges Ahead and A Possible Strategy
=================================================
A. Health Infrastructure in Public Sector ----------------------------------------Issues in regard to public and private health infrastructure are different and both of them need attention but in different ways. Rural public infrastructure must remain in mainstay for wider access to health care for all without imposing undue burden on them. Side by side the existing set of public hospitals at district and sub-district levels must be supported by good management and with adequate funding and user fees and out contracting services, all as part of a functioning referral net work. This demands better routines more accountable staff and attention to promote quality. Many reputed public hospitals have suffered from lack of autonomy inadequate budgets for non-wage O&M leading to faltering and poorly motivated care. All these are being tackled in several states are part health sector reform, and will reduce the waste involved in simpler cases needlessly reaching tertiary hospitals direct. These, attempts must persist without any wavering or policy changes or periodic denigration of their past working. More autonomy to large hospitals and district public health authorities will enable them to plan and implement decentralized, flexible locally controlled services and remove the dichotomy between hospital and primary care services. Further most preventive services can be delivered by down staging to a public heath nurse much of what a doctor alone does now. Such long-term commitment for demystification of medicine and down staging of professional help has been lost among the politicians bureaucracy and technocracy after the decline of the PHC movement. One consequence is the huge regional disparities between states, which are getting stagnated in the transition at, different, stages and sometimes, polarized in the transition. Some feasible steps in revitalizing existing infrastructure i. The adoption of a ratio based approach for creating facilities and other mpuls has led to shortfalls estimated up to twenty percent. It functions well where ever there is diligent attention to supervised administrative routines such as orderly drugs procurement adequate O&M budgets and supplies and credible procedures for redressal of complaints. ii. The Central funding should constitute 25% of total public expenditure in health against the present 15% (which has been already put forward by NHP 2001 in a draft proposal). iii. The immediate task would be to look deepening the range of work done at all levels of existing centers and in particular
strengthen the referral links and fuller and flexible utilization of PHC/CHCs. iv. Tertiary hospitals had been given concessional land, customs exemption and liberal tax breaks against a commitment to reserve beds for poor patients for free treatments. No procedures exist to monitor this and the disclosure systems are far from transparent, redressal of patient grievances is poor and allegations of cuts and commissions to promote needless procedure are common. This should come under the preview. In a market economy, health care is subject to three links, none of which should become out of balance with the other - the link between state and citizens' entitlement for health, the link between the consumer and provider of health services and the link between the physician and patient.
B. Financing related Issues --------------------------Fair financing of the costs of health care is an issue in equity and it has two aspects, Firstly how much is spent by Government on publicly funded health care and on what aspects? And secondly how huge does the burden of treatment fall on the poor seeking health care? Health spending in India at 6% of GDP is among the highest levels estimated for developing countries. In per capita terms it is higher than in China Indonesia and most African countries but lower than in Thailand. PHC approach was also intended to test the extent to which non-doctor based healthcare was feasible through effective down staging of the delivery of simpler aspects of a care as is done in several countries through nurse practitioners and physician assistants, physician assistants etc can each get trained and recognized to work in allotted areas under referral/supervision of doctors. This may indeed be more acceptable to the medical profession than the draft NHP proposal to restart licentiates in medicine as in the thirties and give them shorter periods of training to serve rural areas. Such a licentiate system cannot now be recalled against the profession's opposition nor would people accept two level services. Some feasible steps in revitalizing existing financing schemes i. It is important to promote delivery systems substantially outside government channel either through NGOs or through registered societies at State and district levels. Although this may not be a long term feasibility strategy since by passing the government is
neither practical nor sustainable but clearly this may by a better approach than leaving it to the market and welcome as path breaking of innovative efforts as a precursor to launching a public program.
C. Shape of Private Sector in Medicine -------------------------------------Over the last several decades, independent private medical practice has become widespread but has remained stubbornly urban with polyclinics, nursing homes and hospitals proliferating often through doctor entrepreneurs. Tertiary hospitals in major cities are in many cases run by business houses and use corporate business strategies and hi-tech specialization to create demand and attract those with effective demand or the critically vulnerable at increasing costs. Standards in some of them are truly world class and some who work there are outstanding leaders in their areas. But given the commodification of medical care as part of a business plan it has not been possible to regulate the quality, accountability and fairness in care through criteria for accreditation, transparency in fees, medical audit, accountable record keeping, credible grievance procedures etc. such accreditation, standard setting and licensure systems are best done under self regulation, but self regulation systems in India medical practice have been deficient in many respects creating problem in credibility. Acute care has become the key priority and continues to attract manpower and investment into related specialty education and facilities for technological improvement. Common treatments, inexpensive diagnostic procedures and family medicine are replaced and priced out of the reach of most citizens in urban areas. Public health spending accounts for 25% of aggregate expenditure the balance being out of pocket expenditure incurred by patients to private practitioners of various hues. Privatization has to be distinguished from private medical practice, which has always been substantial within our mixed economy. What is critical however is the rapid commercialization of private medical practice in particular uneven quality of care. There are complex reasons for this trend. i. The high scarcity cost of good medical education,. ii. The reward differential between public and corporate tertiary hospitals leading to the reluctance of the young professional to be lured away from the market to public service in rural areas
iii. There is the compulsion of returns on investment whenever expensive equipment in installed as part of practice. Increasingly, this has shifted the balance from individual practice to institutionalizes practice, in hospitals, polyclinics,- Etc. this conjunction explodes into unbearable cost escalation when backed by a third party payer system/- This in turn induces increases in insurance premiums making such cover beyond the capacity to pay. There is a distinct possibility of such cycles of cost escalation periodically occurring in the future, promoted further by global transfer of knowledge and software, tele-medicine etc. especially after the advent of predictive medicine and gene manipulation.
D. Regulatory Issues --------------------
1. Consumer Protection Act (COPRA) The following are some recommendations (as stated by some researchers) to make COPRA more effective: i. One major problem envisaged by the enactment of this Act is the emergence of a defensive medical culture because of which the cost of care is likely to increase considerably. To overcome this, the medical councils and associations should look at the charge structure for various procedures. Already some concerns have been raised in the Parliament about the fees charged by doctors. The committee of the upper house recommended that doctors should notify the Medical Council of India of their schedule-of-fee charges and the Council, in turn, should make this information available to the public. ii. The Act, at present, has no provision for punishing people who file false cases. There is strong apprehension among the providers that the number of false cases will increase and the legislation will be used for harassing and blackmailing the providers. To minimize the misuse of this legislation, it is suggested that there should a screening committee to review the cases before they are formally taken up for hearing by the consumer forums. The responsibility of the screening committee should also be to categorize cases in such a way that only medical negligence cases posing damage or loss to patient should be pursued further. Other matters should be referred to the medical council. iii. Most of the doctors feel that the absence of medical professionals on the panel of councils is one major drawback of the COPRA. It was pointed out that the providers in the health
sector were not involved in the process of enacting COPRA until late in its development. It is argued that non-medical people serve judgment when they are not qualified to make an accurate assessment about medical evidence. It is suggested that medical people be better represented, especially in medical negligence cases. iv. There should be an orientation program for newly graduated doctors who want to start private practice.
2. Medical Council of India and State medical Councils (SMCs) The character of medical care in India has changed drastically and these changes present many challenges. These challenges need to be addressed by the MCI. In order to do so, however, the basic structure and financing of the MCI has to be strengthened to make it an effective organization. The role of the MCI and SMCs as regulators has been less than impressive in India. They have failed to regulate the medical profession and to set adequate standards to safeguard the interest of patients, particularly in the area of medical practice. As first step, the role of regulating education should be separated from the role of regulating practice. This would require a separate commission to establish adequate standards and ensure the implementation of basic minimum standards.
3. The Nursing Homes Act The NHAs do not specify minimum standards for nursing homes should uphold. Since legislation such as the Nursing Home Act does not normally specify the standards, the medical associations or the Medical Council of India could do this. The standard setting agency should then be empowered to implement those standards. The process of registration and renewal should be tightened and should be strictly implemented. The local supervising authorities should be made responsible for registration and renewal of registration. The Ministry of Health in India should take a broad view of the regulation of Nursing Homes in India and should lay down basic policy guidelines for all states.
VIII. References ================ Bhat, Ramesh. 1996. "Regulating the Private Health Care Sector in
India: The Case of Consumer Protection Act." Health Policy and Planning, forthcoming. Chatterjee, Meera. 1988. Implementing Health Policy. New Delhi: The Centre for Policy Research. Central Bureau of Health Intelligence. 1985 and 1988. Directory of Hospitals in India. New Delhi: Ministry of Health & Family Welfare, Government of India. Jesani, A. and S. Anantharam. 1989. "Private Sector and Privatisation in the Health Care Services." Bombay: Foundation for Research in Community Health. National Council of Applied Economic Research. 1991. Household Survey of Medical Care, New Delhi: National Council of Applied Economic Research.
You might also like
- Respiratory Care Anatomy and Physiology 3rd Edition Will Beachey Test BankDocument12 pagesRespiratory Care Anatomy and Physiology 3rd Edition Will Beachey Test BankOcean0% (1)
- Zhu's Scalp AcupunctureDocument17 pagesZhu's Scalp AcupunctureJosé Mário100% (16)
- Principle of Legitimate Cooperation: Rosanna Bucag, UST SNDocument3 pagesPrinciple of Legitimate Cooperation: Rosanna Bucag, UST SNROSANNA BUCAG50% (2)
- Healthcare Industry in IndiaDocument18 pagesHealthcare Industry in IndiaDarryl CordeiroNo ratings yet
- Indian Medical Devices Sector ReportDocument33 pagesIndian Medical Devices Sector ReportPradip SinghiNo ratings yet
- Medikabazaar JD - SCMDocument3 pagesMedikabazaar JD - SCMVishu CoderedNo ratings yet
- 2011 Er Relational Exercise Pharma PDFDocument4 pages2011 Er Relational Exercise Pharma PDFArpit GulatiNo ratings yet
- Scope of Physiotherapy PracticeDocument16 pagesScope of Physiotherapy PracticeEinstein Jerome83% (6)
- Laparoscopic UrologyDocument1,202 pagesLaparoscopic UrologyNuc Alexandru100% (3)
- Gastric CancerDocument25 pagesGastric CancerAndreea SubcinschiNo ratings yet
- AYushman Bharat AnalysisDocument12 pagesAYushman Bharat Analysisravi767457507No ratings yet
- Health Insurance in IndiaDocument11 pagesHealth Insurance in IndiaUpender DhullNo ratings yet
- Health Infrastructure in IndiaDocument34 pagesHealth Infrastructure in IndiamithraaNo ratings yet
- A Comparative Study On Patient Satisfaction Among Public and Private Hospitals in City of Pune, MaharashtraDocument8 pagesA Comparative Study On Patient Satisfaction Among Public and Private Hospitals in City of Pune, MaharashtraSaurav BhowmikNo ratings yet
- Emerging Health Insurance in India-An Overview - J AnithaDocument17 pagesEmerging Health Insurance in India-An Overview - J AnithaSwayam Suraj NayakNo ratings yet
- Indian Healthcare IndustryDocument15 pagesIndian Healthcare IndustryAkshun GulatiNo ratings yet
- Healthcare in India: Changing The Financing Strategy: Ravi DuggalDocument9 pagesHealthcare in India: Changing The Financing Strategy: Ravi DuggalsanjnuNo ratings yet
- Research Analysis On Healthcare Sector in India and Strategies AdoptedDocument62 pagesResearch Analysis On Healthcare Sector in India and Strategies AdoptedManasvi Deshpande100% (1)
- DTH Industry in IndiaDocument4 pagesDTH Industry in Indiacoolleo123No ratings yet
- Synopsis of ProjectDocument67 pagesSynopsis of ProjectInSoMniA9991% (11)
- CSR ReportDocument13 pagesCSR Reportrishabh agarwalNo ratings yet
- Pharmaceutical Industry in IndiaDocument11 pagesPharmaceutical Industry in IndiaSudarshan MahajanNo ratings yet
- Presenting Group No.6 (Sec.A) )Document10 pagesPresenting Group No.6 (Sec.A) )james_theme007100% (1)
- Healthcare in IndiaDocument91 pagesHealthcare in IndiaThanusha ThanushaNo ratings yet
- A Study On Swachh Bharat Abhiyan and Management LessonsDocument2 pagesA Study On Swachh Bharat Abhiyan and Management LessonsarcherselevatorsNo ratings yet
- Indian MSME SectorDocument4 pagesIndian MSME SectorPranav MishraNo ratings yet
- Apollohospitals 100225124833 Phpapp01Document24 pagesApollohospitals 100225124833 Phpapp01Parvathi AishwaryaNo ratings yet
- Universal - Health - Coverage - in - India - A Long Road AheadDocument8 pagesUniversal - Health - Coverage - in - India - A Long Road AheadrenjithNo ratings yet
- Project Report-Prashant GamreDocument61 pagesProject Report-Prashant GamreHarish KundapurNo ratings yet
- Project Report of International Hospital BanditaDocument99 pagesProject Report of International Hospital Banditapolly1963No ratings yet
- National Law Institute University, Bhopal: Economics - I Topic: Ayushman Bharat and ItsDocument18 pagesNational Law Institute University, Bhopal: Economics - I Topic: Ayushman Bharat and ItsAnay MehrotraNo ratings yet
- Consumerism and Rise of Indian Middle ClassDocument12 pagesConsumerism and Rise of Indian Middle ClassPulkit AroraNo ratings yet
- Project Report On HCL - Market ResearchDocument50 pagesProject Report On HCL - Market ResearchDileep Kumar MishraNo ratings yet
- Rural DevelopmentDocument11 pagesRural DevelopmentAhmed HajiNo ratings yet
- Automobile Industry in IndiaDocument37 pagesAutomobile Industry in IndiaKiran DuggarajuNo ratings yet
- Analysis of Abbott India LTDDocument14 pagesAnalysis of Abbott India LTDNachiket ParabNo ratings yet
- Analysis of Consumer Engagement For Gateway Software Solutions For Preferred Online Classifieds PlatformDocument55 pagesAnalysis of Consumer Engagement For Gateway Software Solutions For Preferred Online Classifieds PlatformRakesh RakiNo ratings yet
- Ey Global Analysis of Health Insurance in IndiaDocument10 pagesEy Global Analysis of Health Insurance in IndiaRachita PrakashNo ratings yet
- Stages in New Service Development ProcessDocument5 pagesStages in New Service Development ProcessRagarjuna Naidu PogunuluNo ratings yet
- Ashish Giri, AN OVERVIEW OF AYURVEDIC INDUSTRY, MBA Projects, Marketing, MRP, SIP, Mba Research Projects Papers, Ayurvedic Ayurvedic Project, Ayurvedic SectorDocument93 pagesAshish Giri, AN OVERVIEW OF AYURVEDIC INDUSTRY, MBA Projects, Marketing, MRP, SIP, Mba Research Projects Papers, Ayurvedic Ayurvedic Project, Ayurvedic Sectorashish_giri1012161494% (18)
- PPT of NBFC SDocument56 pagesPPT of NBFC Sfm949No ratings yet
- ITC Limited Sustainable DevelopmentDocument25 pagesITC Limited Sustainable DevelopmentVaibhav DeshmukhNo ratings yet
- Indian Healthcare IndustryDocument41 pagesIndian Healthcare Industrydmathur1234No ratings yet
- DPR Chhattisgarh PDFDocument138 pagesDPR Chhattisgarh PDFAmit SinhaNo ratings yet
- Chapter 1Document51 pagesChapter 1dipin krishnaNo ratings yet
- Future Trends of Marketing Research Approach - An OverviewDocument79 pagesFuture Trends of Marketing Research Approach - An OverviewSarang Rokade50% (2)
- Make in India FinalDocument20 pagesMake in India FinalanushkaNo ratings yet
- Beti Bachao-Beti PadhaoDocument14 pagesBeti Bachao-Beti Padhaojai LakhinanaNo ratings yet
- Customer's Perceptions Toward Health Insurance Empirical Study in Ahmadabad Region PresentationDocument37 pagesCustomer's Perceptions Toward Health Insurance Empirical Study in Ahmadabad Region Presentationsanjaydesai173_86318No ratings yet
- ASCI Case StudyDocument3 pagesASCI Case Studyneha100% (1)
- CB NotesDocument142 pagesCB NotesPriya Priya100% (1)
- Impact of Agricultural Sector On Indian EconomyDocument17 pagesImpact of Agricultural Sector On Indian EconomyAmit Dandapath100% (6)
- Summer Training Project Report ON: "Manchitra"Document57 pagesSummer Training Project Report ON: "Manchitra"Himani GugnaniNo ratings yet
- Impact of Covid-19 Pandemic On Indian Economy 2Document9 pagesImpact of Covid-19 Pandemic On Indian Economy 2Ayushi PatelNo ratings yet
- The Role of Small Scale Industries in IndiaDocument23 pagesThe Role of Small Scale Industries in IndiaHemantSharmaNo ratings yet
- Metro ReportDocument56 pagesMetro ReportTaniya BhattacharjeeNo ratings yet
- Rural Markets (HUL vs. ITC)Document77 pagesRural Markets (HUL vs. ITC)Jay LohanaNo ratings yet
- Acpprojectonnewspaper 150525122135 Lva1 App6891 PDFDocument123 pagesAcpprojectonnewspaper 150525122135 Lva1 App6891 PDFVarun SainiNo ratings yet
- Data - Analysis On Rape VictimsDocument11 pagesData - Analysis On Rape VictimsHarish BNo ratings yet
- Internship Project Report On Mobile-Health Applications For The Efficient Delivery of Health Care Facility To People: - A Survey On Woodland RPGDocument42 pagesInternship Project Report On Mobile-Health Applications For The Efficient Delivery of Health Care Facility To People: - A Survey On Woodland RPGBishal RoyNo ratings yet
- A Study of HRD Climate in The Hospitals and Its Impact On Patient SatisfactionDocument86 pagesA Study of HRD Climate in The Hospitals and Its Impact On Patient SatisfactionMiteshNo ratings yet
- Healthcare Financing Infrastructure PaperDocument25 pagesHealthcare Financing Infrastructure Papersri_cbmNo ratings yet
- Project Report On Health Care Hospital SDocument25 pagesProject Report On Health Care Hospital Ssidhushinde009No ratings yet
- wg11 HeasysDocument44 pageswg11 Heasysasdf789456123No ratings yet
- Health Insurance and Third Party Administrators Issues and ChallengesDocument25 pagesHealth Insurance and Third Party Administrators Issues and ChallengesANish AhmedNo ratings yet
- Private Sector Health Services in Bangladesh - An Exploratory StudyDocument37 pagesPrivate Sector Health Services in Bangladesh - An Exploratory Studyhornzz0% (1)
- Healthcare IndustryDocument3 pagesHealthcare IndustryAbhijeetNo ratings yet
- CoinsDocument1 pageCoinsAmit KumarNo ratings yet
- Business Plan Localsports - Co.In: Karthick Paulraj, Megha Pant, Ankit Agarwal, Amit Kumar SinghDocument16 pagesBusiness Plan Localsports - Co.In: Karthick Paulraj, Megha Pant, Ankit Agarwal, Amit Kumar SinghAmit KumarNo ratings yet
- Janata PartyDocument12 pagesJanata PartyAmit KumarNo ratings yet
- Chapter 1Document39 pagesChapter 1Amit KumarNo ratings yet
- Chapter 4 Questionnaire & AnalysisDocument21 pagesChapter 4 Questionnaire & AnalysisAmit KumarNo ratings yet
- Amity Business School: MBA Class of 2011 Semester IIIDocument15 pagesAmity Business School: MBA Class of 2011 Semester IIIAmit KumarNo ratings yet
- A Case of Patient AI, Who Came in Due To Sore ThroatDocument16 pagesA Case of Patient AI, Who Came in Due To Sore ThroatLovelle LopezNo ratings yet
- Alicia Vick Personal StatementDocument5 pagesAlicia Vick Personal Statementapi-310904234No ratings yet
- MRI of Enthesitis in As (Including PsA)Document7 pagesMRI of Enthesitis in As (Including PsA)wandering_bearNo ratings yet
- Mobilization With MovementDocument8 pagesMobilization With Movementapi-661333402No ratings yet
- Chair Position: Presented by - Hemam Shankar SinghDocument35 pagesChair Position: Presented by - Hemam Shankar SinghFaye Nervanna Alecha Alferez100% (1)
- General AnesthesiaDocument26 pagesGeneral Anesthesiabhargovish_6918389No ratings yet
- Questionnaire Survey of Working Relationships Between Nurses and Doctors in University Teaching Hospitals in Southern NigeriaDocument22 pagesQuestionnaire Survey of Working Relationships Between Nurses and Doctors in University Teaching Hospitals in Southern NigeriaMin MinNo ratings yet
- 7 3 MR 950 Quick Guide and TroubleshootingDocument7 pages7 3 MR 950 Quick Guide and TroubleshootingsedNo ratings yet
- Admitting and Discharging Patients.Document15 pagesAdmitting and Discharging Patients.FatimaIvanCeniza100% (1)
- Mandatory PhilHealth Coverage of Senior Citizens Pursuant To RA 10645 02.22.2015Document33 pagesMandatory PhilHealth Coverage of Senior Citizens Pursuant To RA 10645 02.22.2015Ralph Julius L. Mendoza100% (1)
- Snap IV Instructions PDFDocument2 pagesSnap IV Instructions PDFCamila Andrea Bravo BugueñoNo ratings yet
- RosierDocument3 pagesRosierYunitaHandayaniNo ratings yet
- Dr. Mohammed Shahedur Rahman Khan Bronchial Asthma Management Aspects - Current and FutureDocument32 pagesDr. Mohammed Shahedur Rahman Khan Bronchial Asthma Management Aspects - Current and FutureShahadat Hossain BabuNo ratings yet
- Laparoscopic CholecystectomyDocument41 pagesLaparoscopic CholecystectomyLim MelaniNo ratings yet
- Meniscal Repair. Jaoos PDFDocument10 pagesMeniscal Repair. Jaoos PDFkarenNo ratings yet
- Investigatory Project On AnalgesicsDocument30 pagesInvestigatory Project On AnalgesicsAnurag Singh100% (1)
- Lock - Inventing A New DeathDocument20 pagesLock - Inventing A New Deathmaru1981No ratings yet
- The RADICAL Framework For Implementing and Monitoring Healthcare Risk ManagementDocument11 pagesThe RADICAL Framework For Implementing and Monitoring Healthcare Risk ManagementRangga PradanaNo ratings yet
- AAnch HospitalDocument8 pagesAAnch HospitalAANCH hospitalNo ratings yet
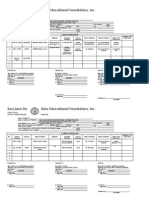
- San Juan de Dios Educational Foundation, IncDocument6 pagesSan Juan de Dios Educational Foundation, Incmae- athenaNo ratings yet
- ThyroidectomyDocument52 pagesThyroidectomyWindelyn Gamaro100% (4)
- Tyrosinemia m2Document31 pagesTyrosinemia m2linaleenNo ratings yet
- Breech SimulationDocument10 pagesBreech SimulationRahmawati Dianing PangestuNo ratings yet