Professional Documents
Culture Documents
31 Uro Hydrocele 111211112520 Phpapp02
31 Uro Hydrocele 111211112520 Phpapp02
Uploaded by
ppc_20Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
31 Uro Hydrocele 111211112520 Phpapp02
31 Uro Hydrocele 111211112520 Phpapp02
Uploaded by
ppc_20Copyright:
Available Formats
HYDROCELE 02
HYDROCELE
Shuja Tahir, FRCS(Edin), FCPS (Hon)
ETIOLOGY & PATHOPHYSIOLOGY
Hydrocole is collection of fluid in persistant tunica vaginalis in males. It is collection of serous fluid resulting from a defect or irritation in the tunica vaginalis of the scrotum. Hydroceles also may arise in the spermatic cord in males or the canal of Nuck in females. FREQUENCY Hydrocele is estimated to affect 1% of adult men. More than 80% of newborn boys have a patent processus vaginalis, but most close spontaneously within 18 months of age. Most hydroceles are congenital and are noted in children aged 1-2 years of age. The incidence of hydrocele is rising with the increasing survival rate of premature infants and with increasing use of the peritoneal cavity for ventriculoperitoneal (VP) shunts, dialysis, and renal transplants. Hydrocele is a disease observed only in males. Chronic or secondary hydroceles usually occur in men older than 40 years. Hydrocele is bilateral in 7-10% of cases. Hydrocele often is associated with hernia, especially on the right side of the body in infants and children. ETIOLOGY Most pediatric hydroceles are congenital; however, malignancy, infection, and circulatory compromise are possible causes of hydrocele. Hydrocele of the cord is associated with pathologic closure of the distal processus vaginalis, which allows fluid pooling in the mid portion of the spermatic cord. Communicating hydrocele is caused by failed closure of the processus vaginalis at the internal ring. Noncommunicating hydrocele results from pathologic closure of the processus vaginalis and trapping of peritoneal fluid.
Hydrocele (trans illumination test)
Hydrocele (ultrasound scan)
Hydrocele (ultrasound scan)
SURGERY - UROLOGICAL PROBLEMS
258
HYDROCELE 03
Adult-onset hydrocele may be secondary to orchitis or epididymitis. Hydrocele also can be caused by malignancy, tuberculosis and by tropical infections such as filariasis. Testicular torsion may cause a reactive hydrocele in 20% of cases. The clinician may be mis-led by focusing on the hydrocele, which delays the diagnosis of torsion. Tumor, especially germ cell tumors or tumors of the testicular adnexa may cause hydrocele. Traumatic (ie, hemorrhagic) hydroceles are common. Ipsilateral hydrocele occurs in as many as 70% of patients after renal transplantation. Radiation therapy is associated with cases of hydrocele. Exstrophy of the bladder may lead to hydrocele. Hydrocele may arise from Ehlers-Danlos syndrome. Hydrocele may result from a change in the type or volume of peritoneal fluid, like in patients undergoing peritoneal dialysis and those with a ventriculoperitoneal shunt. PATHOPHYSIOLOGY Embryologically, the processus vaginalis is a diverticulum of the peritoneal cavity. It descends with the testes into the scrotum via the inguinal canal around the 28th gestational week with gradual
closure through infancy and childhood. Hydroceles are classified into three principal types. CONGENITAL These are also called a communicating (congenital) hydroceles. Patent processus vaginalis permits flow of peritoneal fluid into the scrotum. Indirect inguinal hernias are associated with this type of hydrocele. ACQUIRED It is also called noncommunicating hydrocele. Patent processus vaginalis is present, but no communication with the peritoneal cavity occurs. HYDROCELE OF CORD Closure of the tunica vaginalis is defective. The distal end of the processus vaginalis closes correctly, but the mid portion of the processus remains patent. The proximal end may be open or closed in this type of hydrocele. SECONDARY HYDROCELE Adult hydroceles are usually late-onset (secondary). Late-onset hydroceles may present acutely following local injury, infections, and radiotherapy; these may present chronically from gradual fluid accumulation. Morbidity may result from chronic infection after surgical repair. This type of hydrocele can adversely affect fertility.
PRESENTATIONS
ASYMPHTOMATIC Most hydroceles are asymptomatic or subclinical. Onset, duration, and severity of signs and symptoms are evaluated. Relevant genitourinary (GU) history, sexual history, recent trauma, exercise, or systemic illnesses are identified. SCROTAL SWEELING Most common presentation is a painless enlarged scrotum. SCROTAL DISCOMFORT Sensation of heaviness, fullness, or dragging may be felt by the patient. Patients occasionally report mild discomfort radiating along the inguinal area to the mid portion of the back. PAIN Hydrocele usually is not painful; pain may be an indication of an accompanying acute epididymal infection. The size may decrease with recumbency
SURGERY - UROLOGICAL PROBLEMS
259
HYDROCELE 04
or increase in the upright position. Chronically formed hydroceles appear to be larger in size than acutely formed ones. SYSTEMIC SYMPTOMS Fever, chills, nausea, or vomiting are absent in uncomplicated hydrocele. GU symptoms are absent in uncomplicated hydrocele. Hydroceles are located superior and anterior to the testis, in contrast to spermatoceles, which lie superior and posterior to the testis. The size and the palpable consistency of hydroceles can vary with position. Hydrocele usually becomes smaller and softer after lying down, it usually becomes larger and tenser after prolonged standing. Systemic signs of toxicity are absent. The patient is usually afebrile with normal vital signs. Abdominal or testicular tenderness is absent. No abdominal distension is present. Bowel sounds cannot be auscultated in the scrotum unless an associated hernia is present. Unless an infection causes an acute hydrocele, no
erythema or scrotal discoloration is observed. Transillumination A light source shined through the scrotum causes the hydrocele to illuminate. The bowel also may transilluminate; thus, positive transillumination findings are not diagnostic of hydrocele. Positive transillumination findings should not stop the clinician from investigating serious causes or comorbid conditions that may be associated with secondary hydrocele. This procedure is not reliable for final diagnosis. Transillumination test is usually positive. A light source shines brightly through a hydrocele. Transillumination is common, and diagnostic for hydrocele. Transillumination may be observed with other etiologies of scrotal swelling (eg, hernia). DIFFERENTIAL DIAGNOSIS Indirect inguinal hernia Epididymitis Traumatic injury to the testicle
INVESTIGATIONS
BLOOD EXAMINATION A CBC with differential count may indicate the existence of an inflammatory process. Urinalysis may detect proteinuria or pyuria. ULTRASOUND SCAN It is used to confirm the diagnosis. It may be useful to identify abnormalities in the testis, complex cystic masses, tumors, appendages, spermatocele, or associated hernia. In the context of pain or testicular bleeding after trauma, an imaging test can differentiate between a hydrocele and incarcerated bowel. Hydrocele appears as a cystic mass within the spermatic cord (hydrocele of the cord) or as mass surrounding the testicle. DOPPLER ULTRASOUND FLOW STUDY This study is recommended to assess perfusion, even if an acute scrotum is clinically unlikely. This must be performed urgently if there is suspicion of testicular torsion or of traumatic hemorrhage into a hydrocele or testes. Sensitivity of Doppler ultrasound
SURGERY - UROLOGICAL PROBLEMS
260
HYDROCELE 05
is 86-100%; specificity is up to 100%. Limited availability of this test within a clinically useful period reduces its usefulness. TESTICULAR SCINTIGRAPHY This nuclear scan is particularly useful, especially in children, if testicular torsion is suspected. Decreased or absent flow to one testis or a testicular pole indicates torsion. Sensitivity for torsion can be 90%, but it is decreased with infancy, early torsion,
incomplete torsion, and following detorsion. Specificity for torsion can be 90%, but it is decreased in the presence of scrotal fluid collections (such as hydrocele, hernia, abscess and hematocele). X-RAY ABDOMEN Abdominal x-ray findings usually are normal in patients with hydrocele. If films demonstrate an obstructive gas pattern, they may help to differentiate between incarcerated hernia and hydrocele.
TREATMENT
ASPIRATION Aspiration of a hydrocele reveals a clear amber fluid. Aspiration is not therapeutic because the fluid generally reaccumulates quickly. Aspiration of hydroceles is not recommended because it is associated with a high rate of immediate recurrence and with a risk of introducing an infection. If an associated hernia is present, risk of perforating a loop of bowel also exists. EMERGENCY CARE Differentiating between a hydrocele and an acute scrotum (eg, testicular torsion, strangulated hernia) is important. As many as 50% of acute scrotum cases are initially misdiagnosed. Transillumination is not diagnostic and cannot rule out an acute scrotum. Ultrasound examination, imaging and Doppler evaluation of testicular blood flow is indicated when an acute scrotum is suspected. ACUTE SCROTAL PROBLEMS Traumatic hemorrhage into a hydrocele or testes ! Testicular torsion with or without a secondary
hydrocele. Ischemic testicle in children
SURGICAL TREATMENT Hydrocele is treated through inguinal incisions with high ligation of the patent processus vaginalis (herniotomy) and excision of the distal sac. ! Herniotomy ! Eversion of sac ! Lords operation Spontaneous closure is unlikely in children older than 1 year. Infants with hydrocele are observed for 1-2 years. Surgical treatment is offered afterwards. COMPLICATIONS An extremely large hydrocele may impinge on the testicular blood supply. The resulting ischemia can cause testicular atrophy and subsequent impairment of fertility. Hemorrhage into the hydrocele can result from testicular trauma. Incarceration or strangulation of an associated hernia may occur.
SURGERY - UROLOGICAL PROBLEMS
261
HYDROCELE 06
SURGICAL COMPLICATIONS Accidental injury to the vas deferens can occur during inguinal surgery for hydrocele. Postoperative wound infections occur in 2% of patients undergoing surgery for hydrocele. Postoperative hemorrhagic hydrocele is not uncommon, but it usually resolves spontaneously. Direct injury to the spermatic vessels may occur. PROGNOSIS The prognosis for congenital hydrocele after surgery is excellent. Most congenital cases resolve by the end of the first year of life. Persistent congenital hydrocele is readily corrected surgically. The prognosis of hydrocele presenting
later in life depends upon the etiology of the hydrocele. Adult-onset hydrocele is not uncommonly associated with an underlying malignancy. MISCELLANEOUS Medical/Legal Pitfalls In a patient with signs and symptoms of an acute scrotum, the presence of a hydrocele and a finding of positive transilluminance does not rule out testicular torsion. Immediate definitive tests are indicated to rule out torsion because testicular survival is poor after 4 hours of ischemia. A reasonable search for possible etiologies should be documented. SPECIAL CONCERNS Pediatric: Most cases resolve without intervention. Geriatric: Hydroceles in this group rarely resolve without surgical intervention.
REFERENCES
1. 2. 3. Blaivas M, Brannam L. Testicular ultrasound. Emerg Med Clin North Am. Aug 2004;22(3):723-48, ix. [Medline]. Jayanthi VR. Adolescent urology. Adolesc Med Clin. Oct 2004;15(3):521-34. [Medline]. McAchran SE, Dogra V, Resnick MI. Office urologic ultrasound. Urol Clin North Am. Aug 2005;32(3):337-52, vii.
4. 5.
Schul MW, Keating MA. The acute pediatric scrotum. J Emerg Med. Sep-Oct 1993;11(5):565-77. [Medline]. Skoog SJ, Conlin MJ. Pediatric hernias and hydroceles. The urologist''s perspective. Urol Clin North Am. Feb 1995;22(1):119-30. [Medline]. Tanagho EA, McAninch JW. Disorders of the spermatic cord. In: Smith's General Urology. 1992;620-3. [Medline].
6.
SURGERY - UROLOGICAL PROBLEMS
262
You might also like
- Heart and Cardiovascular AssessmentDocument4 pagesHeart and Cardiovascular AssessmentvHORSEYNo ratings yet
- Kelompok C PBL 2014Document30 pagesKelompok C PBL 2014Ulfi PutriadiNo ratings yet
- Obstetrics and Gynecology Case Management Conference - Chronic HypertensiveDocument104 pagesObstetrics and Gynecology Case Management Conference - Chronic HypertensiveHarold MaglalangNo ratings yet
- Field Apraisal Report Final 11Document10 pagesField Apraisal Report Final 11Raja100% (1)
- HYDROCELEDocument3 pagesHYDROCELESean Patrick Acoba100% (2)
- Spinal AnesthesiaDocument29 pagesSpinal AnesthesiadenekeNo ratings yet
- Intestinal Obstruction in Paediatrics - James GathogoDocument21 pagesIntestinal Obstruction in Paediatrics - James GathogoMalueth Angui100% (1)
- Acute PeritonitisDocument4 pagesAcute PeritonitisSatrio Tri HadmokoNo ratings yet
- Large Bowel Obstruction by Nic MDocument42 pagesLarge Bowel Obstruction by Nic MRisky OpponentNo ratings yet
- Incisional HerniaDocument13 pagesIncisional HerniaMaya Dewi permatasariNo ratings yet
- Carcinoma StomachDocument43 pagesCarcinoma StomachRukman Mecca100% (1)
- Pneumonperitoneum A Review of Nonsurgical Causes PDFDocument7 pagesPneumonperitoneum A Review of Nonsurgical Causes PDFDellysa Eka Nugraha TNo ratings yet
- Phimosis and ParaphimosisDocument3 pagesPhimosis and ParaphimosisJoshua PowersNo ratings yet
- Congenital Heart Disease - A Case StudyDocument13 pagesCongenital Heart Disease - A Case Studydna2life0% (1)
- Salpingitis: Sumber: 1. Dorland 2. Williams Gynecology 3. Better Health Channel Fact Sheet - SalpingitisDocument6 pagesSalpingitis: Sumber: 1. Dorland 2. Williams Gynecology 3. Better Health Channel Fact Sheet - Salpingitisearthbend_tophNo ratings yet
- Pyothorax / Purulent Pleuritis / Empyema Thoracis: Prepared By: Sharmin SusiwalaDocument22 pagesPyothorax / Purulent Pleuritis / Empyema Thoracis: Prepared By: Sharmin SusiwalaAnkan Dey100% (1)
- Pyloric StenosisDocument5 pagesPyloric StenosisMichael AlexanderNo ratings yet
- GASTROSCHISISDocument4 pagesGASTROSCHISISVin Custodio100% (1)
- Hisprung DiseaseDocument12 pagesHisprung DiseaseEky Madyaning NastitiNo ratings yet
- Clinical Manifestations and Diagnosis of Urinary Tract Obstruction and Hydroneph PDFDocument32 pagesClinical Manifestations and Diagnosis of Urinary Tract Obstruction and Hydroneph PDFAmjad Saud0% (1)
- HydroceleDocument6 pagesHydroceleIk-mal AzzarinNo ratings yet
- Horseshoe KidneyDocument26 pagesHorseshoe KidneyarjunjaidevNo ratings yet
- Pathological Changes of DM - 2023Document53 pagesPathological Changes of DM - 2023Visura PrabodNo ratings yet
- Poisoning in ChildrenDocument11 pagesPoisoning in ChildrenAndriana HalfienNo ratings yet
- Management of Patients With Intestinal and Rectal DisordersDocument33 pagesManagement of Patients With Intestinal and Rectal DisordersDoneva Lyn MedinaNo ratings yet
- Hirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshDocument48 pagesHirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshArchana Mahata100% (1)
- Cirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDocument21 pagesCirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDan ChicinasNo ratings yet
- Acute Cholecystitis SMT IV 2021Document43 pagesAcute Cholecystitis SMT IV 2021Dandi PremaNo ratings yet
- Complication of Peptic Ulcer: Department of Surgery S. S. Medical College Rewa and Associate GMH and SGMH RewaDocument76 pagesComplication of Peptic Ulcer: Department of Surgery S. S. Medical College Rewa and Associate GMH and SGMH RewaBrajesh MouryaNo ratings yet
- Hypertrophic Pyloric StenosisDocument17 pagesHypertrophic Pyloric StenosisMohammed Fareed100% (1)
- Endometrial Polyps: Irregular Menstrual BleedingDocument4 pagesEndometrial Polyps: Irregular Menstrual BleedingLuke ObusanNo ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- Esophageal CancerDocument40 pagesEsophageal Cancerapi-282115150No ratings yet
- Hiatal Hernia AchalasiaDocument22 pagesHiatal Hernia AchalasiaDhen MarcNo ratings yet
- Perforated Peptic UlcerDocument68 pagesPerforated Peptic UlcerSaibo BoldsaikhanNo ratings yet
- Surgical JaundiceDocument40 pagesSurgical JaundiceAbdulsalam DostNo ratings yet
- IntussusceptionDocument33 pagesIntussusceptionNovendi RizkaNo ratings yet
- Peptic Ulcer DiseaseDocument18 pagesPeptic Ulcer DiseasechetankumarbhumireddyNo ratings yet
- Presentation of Upper GI EndosDocument44 pagesPresentation of Upper GI EndosHaqmal0% (1)
- 7.peptic Ulcer DiseaseDocument20 pages7.peptic Ulcer DiseaseHayat AL AKOUMNo ratings yet
- Clinical Review: Acute CholecystitisDocument5 pagesClinical Review: Acute CholecystitisElsa SimangunsongNo ratings yet
- Pyloric StenosisDocument11 pagesPyloric StenosisJustin CharlesNo ratings yet
- Renal Cyst: Jump To Navigationjump To SearchDocument6 pagesRenal Cyst: Jump To Navigationjump To SearchManoj PradhanNo ratings yet
- Albendazole in PediatricsDocument38 pagesAlbendazole in PediatricsKishore ChandkiNo ratings yet
- Opd CaseDocument13 pagesOpd CaseRaven CièlNo ratings yet
- Biliary AtresiaDocument8 pagesBiliary AtresiaBrooke MauriNo ratings yet
- Urinary Retention 2Document3 pagesUrinary Retention 2Agli AdhityaNo ratings yet
- Compartment Syndrome: Sebelas Maret UniversityDocument8 pagesCompartment Syndrome: Sebelas Maret Universitykhrisna satyaksaNo ratings yet
- Gastrointestinal EndosDocument28 pagesGastrointestinal EndosAqeel AhmedNo ratings yet
- Pancreatic Cancer (Cancer of The Pancreas) : Patient Discussions: FindDocument13 pagesPancreatic Cancer (Cancer of The Pancreas) : Patient Discussions: FindMoses ZainaNo ratings yet
- Intestinal Obstruction: EpidemiologyDocument11 pagesIntestinal Obstruction: EpidemiologyBereket temesgenNo ratings yet
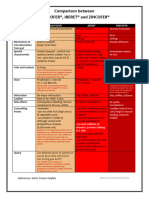
- Comparison Between Maltofer-Iberet-Zincofer TAMBAHANDocument4 pagesComparison Between Maltofer-Iberet-Zincofer TAMBAHANhomesweethomestaytciNo ratings yet
- Ileus MeconiumDocument27 pagesIleus MeconiumDebby TamaraNo ratings yet
- Case Study Presented by Group 22 BSN 206: In-Depth View On CholecystectomyDocument46 pagesCase Study Presented by Group 22 BSN 206: In-Depth View On CholecystectomyAjiMary M. DomingoNo ratings yet
- Final Hernioplasty Compilation RevisedDocument58 pagesFinal Hernioplasty Compilation RevisedRaidis PangilinanNo ratings yet
- Case Presentation - GASTRODocument46 pagesCase Presentation - GASTROalidudeNo ratings yet
- Horseshoe KidneyDocument6 pagesHorseshoe KidneyVerli Fajriati NofliNo ratings yet
- Stevens Johnson DiseaseDocument5 pagesStevens Johnson DiseaseShammy RNNo ratings yet
- Anatomy of The Female Reproductive SystemDocument9 pagesAnatomy of The Female Reproductive SystemPinkeyinthecityNo ratings yet
- Histopath Topic 3 PrelimDocument103 pagesHistopath Topic 3 PrelimKatrina JornadalNo ratings yet
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Truth About The Weird PandemicDocument63 pagesTruth About The Weird PandemicHarshita ShivanagowdaNo ratings yet
- Chapter 5 - Exemptions From GSTDocument35 pagesChapter 5 - Exemptions From GSTkarnimasoni12No ratings yet
- Cover Letter: ThankingDocument4 pagesCover Letter: ThankingSree Raja Sekhar KatamNo ratings yet
- Belize: Statutory Instrument No. 65 of 2020 Arrangement of RegulationsDocument26 pagesBelize: Statutory Instrument No. 65 of 2020 Arrangement of RegulationsOladele OsinugaNo ratings yet
- Congenital Lobar EmphysemaDocument4 pagesCongenital Lobar EmphysemaIjahss JournalNo ratings yet
- Chapter 2 Reviews of Related LiteratureDocument5 pagesChapter 2 Reviews of Related Literatureabu harisNo ratings yet
- Carmen 2022Document242 pagesCarmen 2022Aleiah Jean LibatiqueNo ratings yet
- Converting Driving Licence PDFDocument2 pagesConverting Driving Licence PDFKarthik KichuNo ratings yet
- Essential PainDocument30 pagesEssential PainL P PutriNo ratings yet
- Urinary Incontinence From Harrison's IMDocument2 pagesUrinary Incontinence From Harrison's IMnashey08No ratings yet
- Pediatrics Case StudyDocument27 pagesPediatrics Case StudyPhelanCoy100% (1)
- 6665 PDFDocument4 pages6665 PDFerindah puspowatiNo ratings yet
- Acute PancreatitisDocument9 pagesAcute PancreatitisDaniel HeSaNo ratings yet
- Tasneef 2019 UpdateDocument2 pagesTasneef 2019 UpdateYL LYNo ratings yet
- Chapter 2Document12 pagesChapter 2DannyNo ratings yet
- First-Generation Antipsychotic Medications - Pharmacology, Administration, and Comparative Side Effects - UpToDateDocument18 pagesFirst-Generation Antipsychotic Medications - Pharmacology, Administration, and Comparative Side Effects - UpToDateAdolfo SánchezNo ratings yet
- Amca Blueprints Clinical Medical Assistant Cert Exam 8449 Amca Clinical MedicalDocument9 pagesAmca Blueprints Clinical Medical Assistant Cert Exam 8449 Amca Clinical MedicalBoraNo ratings yet
- Kuliah Pioderma DR Asih BudiastutiDocument56 pagesKuliah Pioderma DR Asih BudiastutiunisoldierNo ratings yet
- My ReportDocument1 pageMy ReportUsman AnwarNo ratings yet
- PHCS AspectsDocument14 pagesPHCS AspectskasmedleyNo ratings yet
- Karya Ilmiah Akhir NersDocument27 pagesKarya Ilmiah Akhir NersSyaputri ChairulNo ratings yet
- Clinical Case of A Patient With Aortic Periprosthetic InfectionDocument4 pagesClinical Case of A Patient With Aortic Periprosthetic InfectionAthenaeum Scientific PublishersNo ratings yet
- BiMed Devices - EngDocument124 pagesBiMed Devices - EngBobNo ratings yet
- Laguna Kosmetik Lutronic Aesthetic Accufit™Document2 pagesLaguna Kosmetik Lutronic Aesthetic Accufit™kberenangNo ratings yet
- 8 - Clinical Outcome in Periradicular Surgery Effect of Patient - and Tooth-Related Factors - A Multicenter StudyDocument8 pages8 - Clinical Outcome in Periradicular Surgery Effect of Patient - and Tooth-Related Factors - A Multicenter StudykochikaghochiNo ratings yet
- MouthwashDocument2 pagesMouthwashMohamed BeshiNo ratings yet