Professional Documents
Culture Documents
Mabes Fluid and Electrolytes
Mabes Fluid and Electrolytes
Uploaded by
MabesOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mabes Fluid and Electrolytes
Mabes Fluid and Electrolytes
Uploaded by
MabesCopyright:
Available Formats
FLUID AND ELECTROLYTES
Homeostasis
Maintenance of constant internal equilibrium in a biologic system that involves positive & negative feedback mechanisms. State of equilibrium in the internal environment, maintained by adaptive responses that promote healthy survival Balance of body fluids and electrolytes play an important role
3. Transport cellular waste products to lungs & kidneys for elimination 4. Normal cellular chemical functioning 5. Lubricates, insulates, and cushions tissues 6. Hydrolysis of food in GIT (Addition of water for food breakdown) 7. Universal Solvent for electrolytes and non electrolytes
Electrolytes
Water Content of the Body
Infants 70 to 80% of body weight Adult 60% of body weight Elderly 65 y/o up 40 to 50% of body weight Muscle, skin and blood have the highest amount of water Fat cells and skeleton has low water content Varies with age, gender, & body mass or body fat. 1kg of body weight = 1L of body water
Factors that influence amt of Body Fluid
1. Age younger (greater muscle mass; low in fat tissues) older (muscle mass decreases; body water declines when aging) 2. Gender men (greater muscle mass and lower fat tissues) women (lesser muscle mass and more fat tissues) 3. Body Mass thin (lean tissue is rich in water) obese (fat cells contain less water) Remember: Greater muscle mass = H20 content Lesser muscle mass = H20 content Adipose tissues have H20 content b/c fat cells contain less water.
Active chemicals in body fluids that carries positive (cations) & negative (anions) electrical charges Expressed in milliequivalents per liter (mEq/L), a measure of electrochemical activity of 1mg of Hydrogen (H+). Cations and anions are equal in mEq/L in a solution Electrolyte concentrations differ in compartments Sources a. Dietary intake (food and oral liquids) b. IVF and TPN solutions c. Medications
Functions of Electrolytes
1. 2. 3. 4. 1. 2. 3. 4. 5.
Maintains fluid balance Maintains fluid volume & osmolality Regulates acid base balance Transmits neuromuscular reactions Sodium Potassium Calcium Magnesium Hydrogen Ion (H+) released by acids
Major Cations
Major Anions
1. Chloride 2. Bicarbonate base or alkali that have low H+ concentration 3. Phosphate 4. Sulfate 5. Proteinate
Functions of Body Water
1. Maintains normal blood volume 2. Transports oxygen and nutrients to and from the cells & other substances such as hormones & enzymes
Major Electrolytes Major Cations Sodium (Na) Potassium (K+) Calcium (Ca++) Magnesium (Mg++) Total Cations Major Anions Chloride (Cl-) Bicarbonate (HCO3 ) Proteinate Organic Acids Phosphate (HPO4 ) Sulfate (SO4 ) Total Anions
ICF
ECF (mEq/L) 142 5 5 2 154 103 26 17 5 2 1 154
b. Maintains blood volume
3 Compartments of Extracellular Fluids 1. Interstitial Space (Interstitium)
40 150 10 200
40 10 150 200
Contains fluids that surround the cells in body tissues 2/3 of ECF 11 12L in an Adult Lymph is an interstitial fluid Function: Intracellular Communication (i.e. transports wastes from cell thru lymph directly to plasma)
2. Intravascular Space
ECF has low concentration of K+ and can only tolerate small changes in K+ concentrations. Release of large amounts of intracellular K+ caused by cell and tissue trauma is dangerous Sodium concentration affects overall concentration of ECF. It regulates the volume of body fluids. o Sodium gain or retention = fluid retention or volume of body fluid o Sodium Loss = fluid loss, vol. of body fluids o Sodium Potassium Pump maintains high extracellular concentration of Na+ and Intracellular concentration of K+
Fluids within the blood vessels that contains PLASMA, the circulating blood volume Average blood volume in an Adult is 6L o 3L of Plasma o 3L Blood Cells RBCS, WBCS, Platelets Measured with Blood Tests Higher Protein Content Major Functions o Transport oxygen and nutrients and other substances such as electrolytes, enzymes, & hormones o Transport wastes to and from the cells
Body Fluids Distribution: Two Fluid Compartments or Spaces 1. Intracellular Compartment (ICF)
Ex. Plasma carries oxygen from lungs and glucose from GIT to the capillary wall of vascular system. Oxygen and glucose move across capillary wall into interstitial & across cell membrane into cells; opposite route is for waste products CO2 is transported from cells to the lungs & metabolic wastes to kidneys for elimination.
3. Transcellular Space
Contains fluids within the cells 2/3 of total body fluids of an adult & located primarily in skeletal muscle mass 42% of total body weight Potassium is the most prevalent cation Phosphates & Sulfates are the most prevalent anions Major Functions: a. Normal cellular chemical functioning b. Cellular metabolism
Smallest division of ECF but an important fluid compartment. Approximately 1L in Adult Includes fluids in CSF, pericardial, pleural spaces (lungs), peritoneal (GIT), synovial spaces (joints, bursae, tendons), intracolular, digestive secretions, sweat
2. Extracellular Compartment (ECF) Contains fluids outside the cells 1/3 of total body fluids in Adult Sodium is the most prevalent cation Chloride is the most prevalent anion
Fluid Compartments are separated by:
1. Semi Permeable Membrane (ICF ECF)
Major Functions a. Transport system to & from the cell
Permeable to water but impermeable to sodium and potassium (needs active transport ATP & NaK+ Pump)
2. Capillary Wall (Interstitial Plasma) Permeable to water but impermeable to protein Permeable allows water and solutes
Semi permeable (Selective Permeability)
Magnitude of this force depends on the amt of dissolved substances (dissolved solutes) No. of dissolved substances determines the osmolality of solution, which influences fluid movement between 2 compartments.
3 Terms Associated with Osmosis: 1. Osmotic pressure
allows water but not all solutes
Solutes
Substances dissolved in a solution Body solutes are electrolytes, oxygen, carbon dioxide, glucose, proteins, amino acids Types of Solutes a. Colloids large substances that doesnt readily dissolve to solutions Protein is the major colloid in vascular system b. Crystalloids salts that dissolve readily Solvent Liquid substance that dissolves the solute Water is the universal solvent for electrolytes & non electrolytes Ex. Sugar (solute) added to Coffee (solvent)
Regulation of Fluid Compartments
(Mechanisms Controlling Fluid & Electrolyte Movement)
Amount of hydrostatic pressure to stop flow of water by osmosis Primarily determined by solute concentration in a solution Water moves from LESS CONCENTRATED TO A MORE CONCENTRATED AREA
2. Oncotic Pressure (Colloid Osmotic P.) Osmotic pressure exerted by Plasma Proteins (i.e. Albumin) Osmotic pressure exerted by Colloids Protein is the major colloid in vascular system 3. Osmotic Diuresis Urine output caused by excretion of substances in urine Glucose, mannitol, or contrast agents
Osmoles
Standard unit of osmotic pressure amt of dissolved substances in a solution
Osmolality
Body fluids normally shift between the two major compartments to maintain equilibrium between spaces for homeostasis Energy is required or theres expenditure for movement to occur ATP Sodium Potassium Pump energy
No. of osmoles per kg of solution Concentration of solute per kg of blood & urine Expressed as milliosmoles per kilogram (mOsm/kg) of solution
Active Transport
Osmolarity
Passive Transport
no energy expenditure or energy not required for movement to occur Osmosis, Diffusion, and Filtration
No. of osmoles per liter of solution Concentration of solution per liter expressed as milliosmoles per liter of solution (mOsm/L)
P A S S I V E T R A N S P O R T Osmosis (ECF ICF) Fluid moves between compartments across a
semi-permeable membrane from LOW TO HIGH SOLUTE CONCENTRATION AREAS until the solutions on both sides of the membrane are equal in solute concentrations
NaK+ Pump located in cell membrane which moves Na+ from cell into ECF (low to high) intracellular concentration of K+ in cell is maintained by pumping K+ into the cell Na+K+ Pump maintains higher concentration of extracellular Na and intracellular K+ Cell membrane pump that exchange Na and K+ ions.
Tonicity
Fluid tension within ECF or ICF that describes relationship between solutes and water Ability of all solutes to cause an osmotic driving force that promotes water movement between compartments. Determines normal cell hydration & cell size. Sodium, glucose, mannitol dont readily cross cell membrane (effective osmoles affecting water movement)
ICF)
Diffusion (ECF
Movement of solutes from HIGHER TO LOWER SOLUTE CONCENTRATION AREAS Occurs through random movement of molecules and ions Occurs in solids, liquids, gases Membrane that separates 2 compartments must be permeable for diffusion to occur. Examples of Diffusion o Exchange of O2 & CO2 between pulmonary capillaries and alveoli o Sodium move from ECF where sodium concentration is to the ICF where its concentration is low.
Facilitated Diffusion
Allows substances to cross cell membrane with assistance of specific carrier molecules (PROTEINS) to accelerate diffusion but no energy is expended
T R A N S P O R T
AC T I V E
Energy must be expended for the movement to occur against a concentration gradient ATP is the energy source Physiologic pump (Na+K+ Pump) moves fluid from LOWER TO HIGHER CONCENTRATED AREAS Sodium concentration in ECF is , it tends to enter cell by diffusion (high to low) offset by
Filtration
Movement of water & solutes by Hydrostatic Pressure from HIGH TO LOW PRESSURE AREAS Hydrostatic pressure in capillaries filters fluids out of IVC (plasma) into interstitial. Allows kidneys to filter 180L of plasma/day. Ex. Hemodialysis
retention of excess water
Fluid Shifts 1) Plasma to Interstitial Fluid = E D E M A
Hydrostatic Pressure Plasma Oncotic Pressure Interstitial Oncotic Pressure
2) Interstitial Fluid to Plasma Normal movements of fluids thru capillary wall into tissues depend on: Plasma Interstitial 1. Hydrostatic Pressure
Edema
Plasma Osmotic or Oncotic Pressure Therapeutic Action: Wear compression stockings or hose
Pressure exerted by the fluids on the walls of blood vessels at arterial & venous ends resulting from cardiac contraction (pumping action) Major force that pushes fluids out of blood vessels (plasma) into tissue space (interstitial) from HIGH PRESSURE TO LOW PRESSURE AREAS Pressure exerted by plasma proteins Pulls interstitial fluid into blood vessels (plasma)
2. Osmotic Pressure
Accumulation of fluid in interstitial spaces Localized result of traumatic injury from accident or surgery, local inflammatory processes or burns Generalized (Anasarca) excessive accumulation of fluid in interstitial space throughout the body as a result of cardiac, renal or liver failure
Fluid Spacing
Remember: ARTERIAL END of capillary: HP > OP = fluids and solutes move out of the capillary VENOUS END of capillary, OP > HP = fluids and some solutes move into the capillary Balance of Hydrostatic & Osmotic Pressure regulates movement of water between Interstitial and Intravascular Direction of fluid movement depends on the differences of Hydrostatic Pressure and Osmotic Pressure Water deficit (ECF) is associated w/ symptoms that result from cell shrinkage as water is pulled into vascular system Water excess (ECF) develops from gain or Average Daily Intake and Output in a Normal Adult Intake (mL) Output (mL) Oral Liquids 1300 Urine (Kidneys) 1500 Water in 1000 Stool or Feces 200 Food Water 300 Insensible Lungs 300 Produced Skin 600 by Metabolism Total 2600 Total 2600
1. First spacing normal distribution of fluid in ICF and ECF 2. Second spacing abnormal accumulation of interstitial fluid 3. Third spacing (Third Space Fluid Shift) Fluid is not lost but unavailable for use by either ICF or ECF Loss of ECF into a space that doesnt contribute to equilibrium between ECF and ICF Clinical Manifestations Initial Sign: Decreased UO despite adequate fluid intake Decreased BP & CVP Increased Heart Rate Edema Increased Body Weight Imbalanced I & O Fluid shifts out Intravascular Space (Plasma) Kidneys receives less blood Kidneys compensate by urine output Occurs in the ff Clients Ascites, Burns, Massive Bleeding, Peritonitis, Bowel Obstruction
Systemic Routes of Gains & Losses of F & E
Organs involved in Homeostasis
Gains Dietary Intake of food & fluids or enteral feeding Parenteral Fluids (through IV PN, TPN) Water produced by oxidation of food Losses Kidney : Urine Output Skin Loss: Sensible & Insensible losses Lungs: Insensible loss GI Tract Others Kidneys Major organ responsible in excreting fluids thru urination. Average daily urine volume is 1 2L in Adult General rule: Output is 1ml of urine per kilogram of body weight per hour (1ml/kg/h) in all age groups. Skin (Sensible Perspiration) Visible water & electrolyte loss thru sweating (Excessive or profuse sweating diaphoresis) Vary from 0 1000ml or more per hour, depending on factors such as environmental temperature. Chief solutes in sweat: Na, Cl, K Skin (Insensible Perspiration) Non visible water loss from skin by evaporation approximately 600ml daily. No electrolytes are lost Increases insensible water loss: a. Fever thru lungs &skin b. Loss of natural barrier like major burns Lungs (Insensible Loss) Eliminate water vapour approx 300 ml/day Loss increases in a dry climate and increased RR and depth such as: o hyperventilation o hyperpnea o continuous coughing Gastrointestinal Tract (GI Losses) 100 200 mL daily Because fluid is reabsorbed in the small intestine, vomiting, diarrhea & fistulas cause large losses.
1. 2. 3. 4. 5. 6.
Kidneys Lungs Heart Pituitary Gland (Anterior & Posterior Pituitary) Adrenal Gland Parathyroid Glands
Regulation of Water Balance
1. 2. 3. 4. 5. 6.
Renal Regulation Cardiac Regulation Hypothalamic Regulation Pituitary Regulation Adrenal Cortical Regulation Gastrointestinal Regulation
Effects of Stress in Fluid & Electrolyte Balance Kidneys Function & Renal Regulation
Primary organs for the regulation of fluid and
electrolyte balance. Filters 180L of plasma daily Excretes 1 2 L of urine daily. Kidney or renal tubules are the site of action of Aldosterone and ADH
Major functions of kidneys for fluid balance 1. Regulates ECF volume & osmolality by selective retention or excretion body fluids. 2. Regulates electrolyte levels in ECF by selective electrolyte retention and secretion 3. Regulates pH of ECF by retention of H+
4. Excretes metabolic wastes & toxic substances.
Heart & Blood Vessels Function
THIRST occurs Person increases Oral Intake of Fluids
c. Pituitary Regulation (ADH Mechanism) Under the control of Hypothalamus,
Pumping action of heart (cardiac contraction) circulates blood thru kidneys to allow urine formation and renal perfusion.
Lung Function Removes 300mL of water daily by exhalation Increases Insensible water losses
Hypothalamic Regulation a. Osmoreceptors
Hyperpnea (abnormally deep respiration) Hyperventilation Continuous coughing Mechanical ventilation with excessive moisture decreases fluid loss. Maintains acid-base balance
Located in hypothalamus senses the ff: a. Plasma Volume (fluid deficit) b. Plasma Osmolality c. Changes in sodium concentration Stimulates thirst and ADH release Result in increased free water, decreased plasma osmolarity & plasma volume. Increased Osmotic pressure Dehydration of neurons
posterior pituitary releases ADH, a water conserving hormone (retains water) Functions of ADH o Maintains osmotic pressure by controlling retention or excretion of water by the kidneys o Regulates Blood volume Absence or presence of ADH determines if urine is concentrated (UO) or diluted (UO) Other factors that stimulates ADH release Stress Surgery Nicotine
ANTIDIURETIC HORMONE REGULATION MECHANISMS
Plasma Osmolarity or Plasma Volume (Fluid Deficit)
Blood volume or BP Volume receptor Atria and great veins
Osmoreceptors in hypothalamus
Hypothalamus Posterior pituitary gland
ADH
Kidney / Renal tubules
Release impulses to Posterior Pitutary Gland Increase ADH release Kidney tubules (Alters kidneys permeability to water) H20 reabsorption Urine Output (Na reabsorption & K+ excretion)
b. Thirst Mechanisms
Stress, Surgery, Heat, Narcotics , Anesthetics, Heat, Nicotine, Antineoplastic agents
H2O reabsorption and UO
free water plasma volume or blood volume
plasma osmolarity
Anesthetics Morphine
Adrenal Cortical Regulation
Thirst influences oral intake of fluids Oral intake is controlled by the thirst center located in hypothalamus Plasa Osmolality Plasma Volume (fluid deficit) Hypothalamic neurons are stimulated by Intracellular dehydration
Adrenal cortex releases hormones to regulate both water and electrolytes o Glucocorticoids o Mineralcorticoids
a. Aldosterone
mineralocorticoid secreted by ZONA GLUMERULOSA OF ADRENAL CORTEX Retains sodium and excretes potassium
Hyperaldosteronism () = sodium and water retention and potassium loss Hypoaldosteronism () = sodium and water loss and potassium retention adrenocortical hormone If secreted in large amounts or administered as corticosteroid therapy results to sodium and fluid retention
PTH influences the ff: o Bone resorption o Calcium absorption from intestine o Calcium reabsorption from renal tubules. GIT accounts most of the water intake Eliminated by GI tract in feces Small nerve receptors located in Left Atrium & Carotid Aortic Arches that detect changes in pressure within blood vessels & transmit this info in CNS
b. Cortisol
Gastrointestinal Regulation
Baroreceptors
Factors affecting Aldosterone Secretion Renin Angiotension Aldosterone System
a. Renin b. Aldosterone released as: serum sodium decreases serum potassium increases ACTH increases
Decreased Renal Perfusion ( Plasma Volume), Juxtaglumerular cell in Kidneys Releases enzyme RENIN Angiotensin I formed by liver is converted to Angiotension II by ACE (Angiotensin Converting Enyzmes) Vasoconstriction of arterial smooth muscle * increased atrial pressure* Activates SNS
Stimulates Anterior Pituitary Gland ACTH release ZONA GLUMERULOSA OF ADRENAL CORTEX ALDOSTERONE release Kidney Tubules Na+ reabsorption H20 reabsorbed by Sodium K+ excretion Plasma Volume (Blood Volume) Parathyroid Function Embedded in thyroid gland Regulates calcium & phosphate balance by
Functions: a. Responds to circulating blood volume changes b. Regulates PNS & SNS neural activity c. Regulates Endocrine activities d. Responds to Atrial Pressure Decrease SNS stimulation Constricts renal arterioles Aldosterone release GFR & Na+ and Water reabsorption
parathyroid gland hormone (PTH)
Cardiac Regulation: Atrial Natruiretic Factor
28-amino-acid peptide released by CARDIAC ATRIA of the heart due to: a. SNS Stimulation b. Increased Atrial Pressure (Vasoconstricition) c. Angiotensin II stimulation d. Endothelin (vasoconstrictor of vascular smooth muscle released from damaged endothelial cells in kidneys) Causes vasodilation and increased urinary excretion of sodium and water Action is opposite to Angiotensin Aldosterone system it decreases BP &volume
Increases release due to: a. condition that results volume expansion (exercise, pregnancy) b. hypoxia c. Increase cardiac filling pressures (Na intake, heart failure, chronic renal failure, atrial tachycardia, vasoconstrictor agents - Epinephrine)
Increased Level Acute heart failure Hyperthyroidism Subarachnoid hemmorhage Small cell lung cancer Decreased Level Chronic heart failure Meds: urea (ureaphil) and prazosin (minipres Gerontologic Considerations 1. Reduced homeostatic mechanisms cardiac, renal, and respiratory function 2. Decreased respiratory function causes impaired pH (acid base imbalance) 3. Decreased Renal function Elevated serum creatinine Dehydration 4. Decreased body fluids 5. Multiple meds affects renal & cardiac function 6. Presence of concomitant conditions (preexisting chronic illnesses)
You might also like
- Lower Secondary Science 9 Learner Book AnswersDocument34 pagesLower Secondary Science 9 Learner Book AnswersVANSHIKA AGARWAL81% (16)
- Diet Wellness PlusDocument10 pagesDiet Wellness Plusapi-283335037100% (1)
- Physiology Comprehensive Exam Pointers PDFDocument108 pagesPhysiology Comprehensive Exam Pointers PDFRaynalynGimoros100% (1)
- (K) Gastroenteritis and Fluid VolumeDocument1 page(K) Gastroenteritis and Fluid Volumeapi-3769252No ratings yet
- Upper Limb: Organization FunctionDocument33 pagesUpper Limb: Organization FunctionAhmed Nabiel El-Jaliel100% (1)
- Сharacteristics of Excitable TissuesDocument27 pagesСharacteristics of Excitable TissuesNasik100% (4)
- 3.14 Chapter 3 Water and Electrolytes Balance and ImblanceDocument140 pages3.14 Chapter 3 Water and Electrolytes Balance and ImblanceShourav SarkarNo ratings yet
- Experiment 3 Glassware Cleaning and Chemical Storage 3.1 ObjectivesDocument17 pagesExperiment 3 Glassware Cleaning and Chemical Storage 3.1 ObjectivesMaldini JosnonNo ratings yet
- Varices Esophagus PDFDocument7 pagesVarices Esophagus PDFDimas ErlanggaNo ratings yet
- PELVISDocument68 pagesPELVISDevsya DodiaNo ratings yet
- Osteology Lower Limb, by DR IramDocument76 pagesOsteology Lower Limb, by DR IramimmmiNo ratings yet
- Key of SEQs Heart, Nerve and Muscle Revision TestDocument11 pagesKey of SEQs Heart, Nerve and Muscle Revision TestMudassar Roomi100% (2)
- Fluid & Electrolite Management in Surgical WardsDocument97 pagesFluid & Electrolite Management in Surgical WardsBishwanath PrasadNo ratings yet
- Regulation RespirationDocument34 pagesRegulation Respirationkiedd_04100% (2)
- Gluteal Region, Posterior Compartment of The Thigh and Popliteal FossaDocument4 pagesGluteal Region, Posterior Compartment of The Thigh and Popliteal FossaSteph SantosNo ratings yet
- The Human ThoraxDocument71 pagesThe Human Thoraxbayenn100% (2)
- Kidney 1 PDFDocument8 pagesKidney 1 PDFحسين فاضل حسين طالبNo ratings yet
- Fluids and ElectrolytesDocument69 pagesFluids and ElectrolytesHarold DiasanaNo ratings yet
- Upper Limb 0809 PDFDocument59 pagesUpper Limb 0809 PDFasdaNo ratings yet
- Physio Reviewer Renal To Acid BaseDocument11 pagesPhysio Reviewer Renal To Acid BaseNicole ChanNo ratings yet
- Physiology of MicturitionDocument44 pagesPhysiology of MicturitionEkiran BabajideNo ratings yet
- Physiology of RespirationDocument2 pagesPhysiology of RespirationIOSRjournalNo ratings yet
- Heart Muscle: The Heart As A Pump and FunctionDocument4 pagesHeart Muscle: The Heart As A Pump and Functionmcwnotes100% (1)
- Cutaneous Circulation: DR Pushpa Lata Sachan Associate Professor CIMS&H, LucknowDocument19 pagesCutaneous Circulation: DR Pushpa Lata Sachan Associate Professor CIMS&H, LucknowNishankumar JhaNo ratings yet
- Renal Control of Acid Base BalanceDocument5 pagesRenal Control of Acid Base BalanceEuniceSimNo ratings yet
- Thoracic Inlet Syndrome and Cervical RibDocument28 pagesThoracic Inlet Syndrome and Cervical RibRabin DasNo ratings yet
- FBC Interpretation and Function of Blood ComponentsDocument7 pagesFBC Interpretation and Function of Blood ComponentsFrancesca LiNo ratings yet
- Upper LimbDocument90 pagesUpper Limbapi-324160601100% (1)
- Physiology Final Exams JULY 8, 2020Document17 pagesPhysiology Final Exams JULY 8, 2020Ndor BariboloNo ratings yet
- A&P 2 Respiratory Lecture NotesDocument31 pagesA&P 2 Respiratory Lecture NotesBethanyNo ratings yet
- Physiology of The Gastrointestinal Tract (Git)Document98 pagesPhysiology of The Gastrointestinal Tract (Git)jballungayNo ratings yet
- Chapter 16Document9 pagesChapter 16g_komolafeNo ratings yet
- Anatomy of Urinary Bladder and UrethraDocument16 pagesAnatomy of Urinary Bladder and UrethraAmalina ZolkefleeNo ratings yet
- Thyroid & Parathyroid GlandsDocument21 pagesThyroid & Parathyroid GlandsAzizan HannyNo ratings yet
- Asthama & COPDDocument84 pagesAsthama & COPDAbdullah BhattiNo ratings yet
- Pleura PericardiumDocument39 pagesPleura PericardiumHere LeafsNo ratings yet
- Blood Pressure Regulation-2Document40 pagesBlood Pressure Regulation-2Juliza FelicianoNo ratings yet
- Circumflex Scapular: Dorsum of Thoracodorsal: Latissmus DorsiDocument4 pagesCircumflex Scapular: Dorsum of Thoracodorsal: Latissmus Dorsispeedy.catNo ratings yet
- Fluid, Electrolyte, and Acid Balance SherwoodDocument32 pagesFluid, Electrolyte, and Acid Balance SherwoodEvan PermanaNo ratings yet
- 2006 PhysioDocument18 pages2006 Physioanaeshkl100% (1)
- BloodDocument38 pagesBloodchukwukerechimezirimNo ratings yet
- Nerve and Muscle PhysiologyDocument82 pagesNerve and Muscle PhysiologychandsriNo ratings yet
- Arrhythmia ReviewDocument33 pagesArrhythmia ReviewMark Hammerschmidt100% (3)
- Chapter 21 Muscle Blood FlowDocument17 pagesChapter 21 Muscle Blood Flowelmedina omeragicNo ratings yet
- 11-Acid-Base BalanceDocument28 pages11-Acid-Base BalanceKathlene BarasiNo ratings yet
- Blood Supply of The GITDocument66 pagesBlood Supply of The GITgtaha80No ratings yet
- Upper LimbDocument54 pagesUpper LimbMar YNo ratings yet
- Anterior Compartment of Arm & Cubital FossaDocument24 pagesAnterior Compartment of Arm & Cubital FossaSky StoneNo ratings yet
- Chapter 17Document6 pagesChapter 17g_komolafe100% (1)
- AIIMS November 2006 AnatomyDocument5 pagesAIIMS November 2006 Anatomyprasun_vNo ratings yet
- Super Simplified Pathology Hematology - Dr. Priyanka SachdevDocument500 pagesSuper Simplified Pathology Hematology - Dr. Priyanka SachdevMohd SaquibNo ratings yet
- Syncope: - Selvarathi KDocument27 pagesSyncope: - Selvarathi KSelvarathi KandhaswamyNo ratings yet
- Lymphatic Drainage of Abdomen: Learning ObjectivesDocument5 pagesLymphatic Drainage of Abdomen: Learning ObjectivesUloko ChristopherNo ratings yet
- Gross Anatomy of Posterior Compartment of The ThighDocument20 pagesGross Anatomy of Posterior Compartment of The ThighOnah ArinzeNo ratings yet
- Lower LimbDocument24 pagesLower LimbLola KhatimNo ratings yet
- Upper Extremities Ortho SG3Document119 pagesUpper Extremities Ortho SG3Nuhu Bankwhot100% (1)
- DKA Management Protocol - Docx PaulosDocument3 pagesDKA Management Protocol - Docx PaulosMiraf MesfinNo ratings yet
- SPIROMETRYDocument5 pagesSPIROMETRYJayarubini JeyapalNo ratings yet
- @CNSMedicalBook ThoraxDocument103 pages@CNSMedicalBook ThoraxGemechis Merga100% (1)
- Spa PPT - FinalDocument45 pagesSpa PPT - FinalShivam DwivediNo ratings yet
- Jugular Venous PressureDocument9 pagesJugular Venous Pressuremoh86-No ratings yet
- Synovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSynovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Bowel Diversion: Parameter Colostomy IleostomyDocument1 pageBowel Diversion: Parameter Colostomy IleostomyMabesNo ratings yet
- Prof Ad BON and NursesDocument7 pagesProf Ad BON and NursesMabesNo ratings yet
- CHN GapuzDocument23 pagesCHN GapuzMabes100% (1)
- Mabes Fluid and Electrolyte ImbalancesDocument15 pagesMabes Fluid and Electrolyte ImbalancesMabesNo ratings yet
- Triage PrinciplesDocument2 pagesTriage PrinciplesMabesNo ratings yet
- Therapeutic Diet NutritionistDocument3 pagesTherapeutic Diet NutritionistMabesNo ratings yet
- Commonly Asked Emergency DrugsDocument17 pagesCommonly Asked Emergency DrugsrianneNo ratings yet
- PainDocument3 pagesPainMabesNo ratings yet
- Asepsis and InfectionDocument6 pagesAsepsis and InfectionMabes100% (1)
- Blood Transfusion Purpose: 9. Check Blood For Presence of BubblesDocument2 pagesBlood Transfusion Purpose: 9. Check Blood For Presence of BubblesMabes100% (1)
- Decubitus Ulcer / Pressure SoresDocument1 pageDecubitus Ulcer / Pressure SoresMabesNo ratings yet
- PositioningDocument3 pagesPositioningMabesNo ratings yet
- Parenteral Therapy:: Intravenous Therapy (IVT) or VenipunctureDocument3 pagesParenteral Therapy:: Intravenous Therapy (IVT) or VenipunctureMabes100% (1)
- Suture and NeedlesDocument5 pagesSuture and NeedlesMabesNo ratings yet
- Nervous SystemDocument11 pagesNervous SystemMabesNo ratings yet
- Enema Administration: Size of Rectal TubeDocument3 pagesEnema Administration: Size of Rectal TubeMabesNo ratings yet
- Taste and SmellDocument1 pageTaste and SmellMabesNo ratings yet
- Roses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.Document249 pagesRoses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.MabesNo ratings yet
- All Nursing TheoriesDocument26 pagesAll Nursing TheoriesMabesNo ratings yet
- Fat Soluble VitaminsDocument5 pagesFat Soluble VitaminsMabesNo ratings yet
- Basic or InstrumentsDocument21 pagesBasic or InstrumentsMabes100% (1)
- Nutritional Recommendation For Cardiovascular DiseaseDocument5 pagesNutritional Recommendation For Cardiovascular DiseaseMabesNo ratings yet
- Factors That Affect Eating and NurtritureDocument3 pagesFactors That Affect Eating and NurtritureMabesNo ratings yet
- Water Soluble VitaminsDocument6 pagesWater Soluble VitaminsMabesNo ratings yet
- Nutrition and Diet Therapy Summary of BookDocument17 pagesNutrition and Diet Therapy Summary of BookMabes100% (2)
- The Concepts of Man and His Basic NeedsDocument5 pagesThe Concepts of Man and His Basic NeedsMabes94% (17)
- Basic Therapeutic DietsDocument3 pagesBasic Therapeutic DietsMabes100% (1)
- Introduction To Nursing TheoriesDocument7 pagesIntroduction To Nursing TheoriesMabes100% (2)
- Mole Concept WorksheetDocument3 pagesMole Concept WorksheetRoland SocoNo ratings yet
- The Science and Practice of Lithium Therapy-Springer International Publishing (2017)Document345 pagesThe Science and Practice of Lithium Therapy-Springer International Publishing (2017)Tony Miguel Saba SabaNo ratings yet
- Chemistry Investigatory ProjectDocument19 pagesChemistry Investigatory ProjectIshita Singh100% (1)
- Nutrient Deficiencies in Lesser Yam (Dioscorea Esculenta) Characterized Using Constant-Water Table Sand CultureDocument10 pagesNutrient Deficiencies in Lesser Yam (Dioscorea Esculenta) Characterized Using Constant-Water Table Sand Cultureiuri_No ratings yet
- ExerciseDocument13 pagesExercised anjilappaNo ratings yet
- Get To Know Potassium Nitrate in Tomato Nutrient ManagementDocument4 pagesGet To Know Potassium Nitrate in Tomato Nutrient ManagementRómulo Del ValleNo ratings yet
- ChlorideDocument3 pagesChlorideMurari VarmaNo ratings yet
- Consumption of Low Tds Water: A Committee Report BY Water Quality Association Science Advisory Committee 1992-1993Document13 pagesConsumption of Low Tds Water: A Committee Report BY Water Quality Association Science Advisory Committee 1992-1993nurhuda majidNo ratings yet
- Fiveland AnnbjørgDocument131 pagesFiveland AnnbjørgAli AliievNo ratings yet
- Hypo Kale MiaDocument13 pagesHypo Kale MiaMuhammad IqbalNo ratings yet
- DOC Carriage of Dangerous GoodsDocument6 pagesDOC Carriage of Dangerous GoodsThếVũKhắcNo ratings yet
- Tissue Salt Primer SchuesslerDocument36 pagesTissue Salt Primer SchuesslerYanka IlarionovaNo ratings yet
- Buffer SolutionDocument8 pagesBuffer SolutionAbubakar UmarNo ratings yet
- Field CropsDocument215 pagesField CropsGary Bhullar100% (2)
- Development of A Cheap and Rapid Method To Determine Calcium in Milk Fractions in An Industrial EnvironmentDocument80 pagesDevelopment of A Cheap and Rapid Method To Determine Calcium in Milk Fractions in An Industrial EnvironmentAndrianNo ratings yet
- Titrasi PresipitasiDocument85 pagesTitrasi PresipitasiayukiwaNo ratings yet
- Manual Autoclave SM200,300,310,500,510-Ver.7Document47 pagesManual Autoclave SM200,300,310,500,510-Ver.7Alfonso Martinez UndaNo ratings yet
- 4 - Water Base Mud System - PTM - HandoutDocument32 pages4 - Water Base Mud System - PTM - HandoutFauzan Rahman Haq100% (1)
- TranspirationDocument31 pagesTranspirationJoan TimbolNo ratings yet
- Is Vitamin K PotassiumDocument10 pagesIs Vitamin K PotassiumSelim HanNo ratings yet
- Form 4 Chapter 3 ExercisesDocument2 pagesForm 4 Chapter 3 ExercisesAnneLeongNo ratings yet
- Salt (Volhard Method)Document3 pagesSalt (Volhard Method)fangirlton100% (1)
- Nutrient Disorders in Rice PosterDocument1 pageNutrient Disorders in Rice Posterhairuddin100% (1)
- Gration Forms A - Ø by K-Capture, While 88 Per Cent Results in Ca - Ø byDocument20 pagesGration Forms A - Ø by K-Capture, While 88 Per Cent Results in Ca - Ø byGNo ratings yet
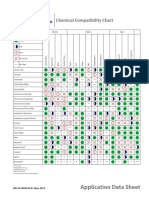
- IND-AS-00899-EN - Chemical Compatibility ChartDocument8 pagesIND-AS-00899-EN - Chemical Compatibility ChartlorenzoNo ratings yet
- Fundamentals of Dairy Chemistry 3rd Ed - Noble P. Wong (Aspen Publishers, Inc. 1999) PDFDocument734 pagesFundamentals of Dairy Chemistry 3rd Ed - Noble P. Wong (Aspen Publishers, Inc. 1999) PDFJe RivasNo ratings yet
- 2ndPUC CHEMISTRY QB PDFDocument114 pages2ndPUC CHEMISTRY QB PDFSiddharth GinimavNo ratings yet