Professional Documents
Culture Documents
Discussion - Alison
Discussion - Alison
Uploaded by
adamforeCopyright:
Available Formats
You might also like
- Positive Learning Framework Creating Learning Environments in Which All Children ThriveDocument6 pagesPositive Learning Framework Creating Learning Environments in Which All Children ThriveDevon SandsNo ratings yet
- Effective Teaching Strategies of Bulacan State University - Sarmiento CampusDocument51 pagesEffective Teaching Strategies of Bulacan State University - Sarmiento CampusPerry Arcilla SerapioNo ratings yet
- A Practical Guide To Implementing Problem-Based Learning in AnesthesiaDocument6 pagesA Practical Guide To Implementing Problem-Based Learning in AnesthesiaMariana Brízido AptxNo ratings yet
- Artikel PBL Dari PubMedDocument8 pagesArtikel PBL Dari PubMedFQFerdianNo ratings yet
- Perception of Students and Faculty On Problem - Based Learning As A Teaching StrategyDocument20 pagesPerception of Students and Faculty On Problem - Based Learning As A Teaching StrategyPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Motivating Learners Through Project-Based LearningDocument10 pagesMotivating Learners Through Project-Based Learningmuhamad hasaniNo ratings yet
- Research Article: Problem Based Learning in Nursing EducationDocument6 pagesResearch Article: Problem Based Learning in Nursing Educationmuhammad zubair khanNo ratings yet
- Wa0010Document11 pagesWa0010api-702415811No ratings yet
- Using Problem Based Learning Method Between 2014 and 2020 With Nursing Students: A Case StudyDocument12 pagesUsing Problem Based Learning Method Between 2014 and 2020 With Nursing Students: A Case Studymalek azisNo ratings yet
- PBL SweeengDocument10 pagesPBL SweeengRichel BulacosNo ratings yet
- Problem Based LearningDocument10 pagesProblem Based LearningFransiska Adriana LarasatiNo ratings yet
- Problem Based Learning at HYMS: A Guide For Students by StudentsDocument57 pagesProblem Based Learning at HYMS: A Guide For Students by StudentsSampurnaPatrenNo ratings yet
- The Future of Modular System of Medical Education: A Teachers' PerspectiveDocument8 pagesThe Future of Modular System of Medical Education: A Teachers' PerspectiveDilawar JanNo ratings yet
- What We Think We Know About The Tutor in Problem-Based LearningDocument6 pagesWhat We Think We Know About The Tutor in Problem-Based LearningroromutiaraNo ratings yet
- HealthcareDocument11 pagesHealthcarewmyartawanNo ratings yet
- El Aprendizaje Indagatorio Mediante Un Proceso Guiado Mejora La Retención de La Información A Largo PlazoDocument9 pagesEl Aprendizaje Indagatorio Mediante Un Proceso Guiado Mejora La Retención de La Información A Largo PlazoGooPop Stoore ChileNo ratings yet
- Introduction To Project Pased LearningDocument10 pagesIntroduction To Project Pased Learninggenius2020No ratings yet
- PCP PlanDocument20 pagesPCP Planapi-316013445100% (1)
- PAYOT - Prevalent Issues On PBLDocument2 pagesPAYOT - Prevalent Issues On PBLpayotrheamaeNo ratings yet
- Impact of Problem-Based Learning On Students'Critical Thinking Dispositions, Knowledge Acquisition and RetentionDocument13 pagesImpact of Problem-Based Learning On Students'Critical Thinking Dispositions, Knowledge Acquisition and RetentionAndrés Cisneros SolariNo ratings yet
- Promoting Problem-Based Learning (PBL) in Engineering Courses at The Universiti Teknologi MalaysiaDocument10 pagesPromoting Problem-Based Learning (PBL) in Engineering Courses at The Universiti Teknologi Malaysiauamiranda3518No ratings yet
- Peer Observation A5 - FinalDocument16 pagesPeer Observation A5 - Finalapi-250421371No ratings yet
- 8626 - Assignment 2 (AG)Document28 pages8626 - Assignment 2 (AG)maalikNo ratings yet
- EJ1089733Document8 pagesEJ1089733Bbrah XcxNo ratings yet
- Linqvodidaktika Serbest Is Seltenet EnverliDocument9 pagesLinqvodidaktika Serbest Is Seltenet EnverligunayNo ratings yet
- Problem Based LearningDocument69 pagesProblem Based LearningPedro Almeida100% (1)
- What Is Project Based Learning and Problem Based LearningDocument5 pagesWhat Is Project Based Learning and Problem Based LearningMashitah Abdul HalimNo ratings yet
- FD Midterm ExamDocument6 pagesFD Midterm ExamRocky Christopher FajardoNo ratings yet
- PBL GuideDocument30 pagesPBL GuideNur Afiqa AzalanNo ratings yet
- PBL, SCL & PoblDocument4 pagesPBL, SCL & PoblKhairul Azhar Abdul LizaNo ratings yet
- Canadian Medical Education JournalDocument4 pagesCanadian Medical Education JournalannegirlNo ratings yet
- I Believe All of Us Are Also Concern About The Implementation of PBL Will Oppose To Our KSSR Science Standard?Document6 pagesI Believe All of Us Are Also Concern About The Implementation of PBL Will Oppose To Our KSSR Science Standard?chew97No ratings yet
- Reviewer For Final Examination in Teaching Technology in Elementary GradesDocument9 pagesReviewer For Final Examination in Teaching Technology in Elementary Gradestoriojocelyn16No ratings yet
- What Is PBL?Document26 pagesWhat Is PBL?Vhim GutierrezNo ratings yet
- The Comprehension of Problem Based Learning Model As The Preparation On PPLDocument6 pagesThe Comprehension of Problem Based Learning Model As The Preparation On PPLMuktiarniNo ratings yet
- Use of Portfolios by Medical Students SignificanceDocument7 pagesUse of Portfolios by Medical Students SignificanceKaro MotiNo ratings yet
- BahavoivalDocument14 pagesBahavoivalAymen JamalNo ratings yet
- Module 1 - Introduction To Problem-Based LearningDocument4 pagesModule 1 - Introduction To Problem-Based LearningLuz Adriana MejiaNo ratings yet
- Bazarte Chapter 1234 1Document63 pagesBazarte Chapter 1234 1Kenjie AmorNo ratings yet
- Context Based LearningDocument6 pagesContext Based LearningSravan Kumar PatibandlaNo ratings yet
- Orientation Programme For New TeacherDocument10 pagesOrientation Programme For New Teacherarchim_azymaNo ratings yet
- Project Based Learning.. Written ReportdocxDocument5 pagesProject Based Learning.. Written ReportdocxCHAVEZ, EVER A.No ratings yet
- Critical Reading Final Task ArticleDocument6 pagesCritical Reading Final Task ArticleMuhammad IlhamNo ratings yet
- Wafa Ibrahim S Alotaibi - Research ProposalDocument10 pagesWafa Ibrahim S Alotaibi - Research Proposalmeraj21No ratings yet
- Why Don'T We Adopt Professional Development School For Indonesian Field Experience Practice?Document8 pagesWhy Don'T We Adopt Professional Development School For Indonesian Field Experience Practice?Widya RatnaNo ratings yet
- Project Based Learning (TTT)Document4 pagesProject Based Learning (TTT)Choukri Brahim HammacheNo ratings yet
- The Strengths and Weaknesses of The Implementation of Project Based Learning: A ReviewDocument7 pagesThe Strengths and Weaknesses of The Implementation of Project Based Learning: A ReviewSulaiman YahyaNo ratings yet
- Development of A Questionnaire To Measure Teachers Studentcentred Perspectives Based On The Onion Model - 2022 - BioMed Central LTDDocument9 pagesDevelopment of A Questionnaire To Measure Teachers Studentcentred Perspectives Based On The Onion Model - 2022 - BioMed Central LTDKang MuksinNo ratings yet
- AMEE 135 Permelee Lecture Free Curriculm Med Tes 2020Document9 pagesAMEE 135 Permelee Lecture Free Curriculm Med Tes 2020Silvina TabordaNo ratings yet
- Lesson 2-WPS OfficeDocument17 pagesLesson 2-WPS OfficeJohn Mark MapusaoNo ratings yet
- The Role of Teacher in PBLDocument10 pagesThe Role of Teacher in PBLfarchanNo ratings yet
- The Effects of The Implementation Problem Oriented Learning Modules Implications For Teaching TechniquesDocument12 pagesThe Effects of The Implementation Problem Oriented Learning Modules Implications For Teaching TechniquesBella SakedanNo ratings yet
- Curriculum Case StudyDocument9 pagesCurriculum Case Studyapi-458907281No ratings yet
- PBL - Nor Azuanee Mukhtar Mp101439Document16 pagesPBL - Nor Azuanee Mukhtar Mp101439Azuanee AzuaneeNo ratings yet
- Accounting Students Problem Based Learning AcceptanceDocument7 pagesAccounting Students Problem Based Learning AcceptanceAdi AliNo ratings yet
- Effectiveness of Problem-Based Learning Implementation: KeywordsDocument13 pagesEffectiveness of Problem-Based Learning Implementation: KeywordsImmas Andaru WinantiNo ratings yet
- Running Head: Curriculum Proposal 1Document31 pagesRunning Head: Curriculum Proposal 1Hum NjorogeNo ratings yet
- Lee 2018Document12 pagesLee 2018some oneNo ratings yet
- A Guide for Culturally Responsive Teaching in Adult Prison Educational ProgramsFrom EverandA Guide for Culturally Responsive Teaching in Adult Prison Educational ProgramsNo ratings yet
- Teachers’ Perceptions of Their Literacy Professional DevelopmentFrom EverandTeachers’ Perceptions of Their Literacy Professional DevelopmentNo ratings yet
- Lesson PlanDocument2 pagesLesson Planapi-357043228No ratings yet
- A Study On Problems of Learning MathematicsDocument3 pagesA Study On Problems of Learning MathematicsSneha Sara SajeevNo ratings yet
- Summary of Five Educational PhilosophiesDocument2 pagesSummary of Five Educational PhilosophiesKheona MartinNo ratings yet
- Manning Selling 3ce Ch04 (Communication Types)Document21 pagesManning Selling 3ce Ch04 (Communication Types)shaalienNo ratings yet
- RUBRICS FOR LESSON PLAN and BLOGDocument3 pagesRUBRICS FOR LESSON PLAN and BLOGMariel Suaiso AngelesNo ratings yet
- Revised Bloom's Taxonomy - ProjectDocument7 pagesRevised Bloom's Taxonomy - Projectdewi agustinaNo ratings yet
- Art Allows Us To Connect With Our Inner SelvesDocument3 pagesArt Allows Us To Connect With Our Inner SelvesPacita MaraonNo ratings yet
- My Pet ReadingDocument5 pagesMy Pet ReadingeilamieraNo ratings yet
- Philosophy Grade 11 - ABM Jan. 6-9,2020Document5 pagesPhilosophy Grade 11 - ABM Jan. 6-9,2020Melody LandichoNo ratings yet
- CSLPA Workshop: EDF 4210 Educational PsychologyDocument24 pagesCSLPA Workshop: EDF 4210 Educational PsychologyKomal KhanNo ratings yet
- Affirmative Side DebateDocument2 pagesAffirmative Side DebateKim LiatNo ratings yet
- Netball PE ReflectionDocument6 pagesNetball PE ReflectionClara CalhounNo ratings yet
- FullDocument136 pagesFullAnn NmayaNo ratings yet
- A Critical Analysis of The Writings of Amos RapoportDocument11 pagesA Critical Analysis of The Writings of Amos RapoportmaxwalkerdreamNo ratings yet
- A Holistic Approach To Improving Thinking SkillsDocument6 pagesA Holistic Approach To Improving Thinking Skillszedrijnali100% (1)
- Hots and Lots in Bloom TaxonomyDocument16 pagesHots and Lots in Bloom TaxonomyNurul RahmayaniNo ratings yet
- 5th Grade Science Lesson Plan - PortfolioDocument2 pages5th Grade Science Lesson Plan - Portfolioapi-475320683No ratings yet
- Deaf Space - ResearchDocument2 pagesDeaf Space - Researcharmein 007No ratings yet
- Rubric Technology Based Assessment-Powtoon Animated Video: Criteria 4 3 2 1Document4 pagesRubric Technology Based Assessment-Powtoon Animated Video: Criteria 4 3 2 1zainudinNo ratings yet
- How To Study A Reading Assignment: The PQRST Method (Preview, Question, Read, State, Test)Document4 pagesHow To Study A Reading Assignment: The PQRST Method (Preview, Question, Read, State, Test)Gobi DurairajNo ratings yet
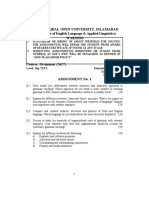
- Allama Iqbal Open University, Islamabad: (Department of English Language & Applied Linguistics) WarningDocument2 pagesAllama Iqbal Open University, Islamabad: (Department of English Language & Applied Linguistics) WarningranaaliahmedNo ratings yet
- Pro. Ed 2Document10 pagesPro. Ed 2Reynald MatiasNo ratings yet
- Module 8 Working With DepEd FormsDocument4 pagesModule 8 Working With DepEd FormsJenelyn VentozaNo ratings yet
- Teaching With Contrived ExperiencesDocument7 pagesTeaching With Contrived ExperiencesRialyn BaguioNo ratings yet
- Developing EFL Vocabulary Through Speaking and Lis PDFDocument6 pagesDeveloping EFL Vocabulary Through Speaking and Lis PDFSelemane PaquelequeNo ratings yet
- Skills of A Successful TrainerDocument16 pagesSkills of A Successful TrainerShivani BansalNo ratings yet
- 243 961 1 PBDocument7 pages243 961 1 PBeunbi nirNo ratings yet
- Oup Focus Visible Thinking PDFDocument5 pagesOup Focus Visible Thinking PDFFranc NearyNo ratings yet
- Stages of Growth and DevelopmentDocument3 pagesStages of Growth and DevelopmentJaney Cunanan100% (6)
- Weekly Learning Plan EnglishDocument6 pagesWeekly Learning Plan EnglishEvelyn DEL ROSARIONo ratings yet
Discussion - Alison
Discussion - Alison
Uploaded by
adamforeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Discussion - Alison
Discussion - Alison
Uploaded by
adamforeCopyright:
Available Formats
Discussion When assessing the feasibility and implications of incorporating PBL into the curriculum, we need to first understand
students perceptions towards PBL and their readiness for that style of learning. To do so, we need an understanding of their current curriculum and its gaps in addressing the learning needs of students. What do students think about PBL and SDL? What was their readiness? Why is this important? because students may have pre-conceived notions about what PBL and SDL is all about will this affect how they approach the sessions? this will influence how they approach the project by measuring their understandings before and after, we get a good idea of how their ideas change What was their outlook on small group learning? Perceptions about fellow classmates? Why is this important? Because PBL depends on functioning as a group and learning from each other.. need to trust classmates these perceptions may influence how sessions run Measuring perceptions is important because it could be compared with perceptions after PBL is incorporated We need to know where the students are coming from to know where PBL can take them
Understanding Problem-Based Learning and Self-Directed Learning As problem-based learning (PBL) is still considered a non-traditional learning style and one that is not currently a focus within the curriculum for medical students in Guyana, it was important to elicit the students understanding of what PBL encompassed. Students generally identified PBL as a process of group discussion based on clinical scenarios. After completing the three-week pilot project, students identified more specific components of PBL such as using ones own interests and gaps in knowledge to guide learning. This demonstrates that students developed a deeper understanding of PBL after only three tutorial sessions. This is significant because to maximize effectiveness of the group process, students should have a concrete understanding of the goals of PBL and how its approach differs from didactic learning. Without this understanding, students may enter into their tutorials expecting to be taught by their tutor, and the ability of PBL to foster self-directed learning may be missed. If PBL is being incorporated into an existing medical curriculum, it is important for all participating members to have a clear understanding of both the benefits and shortfalls of PBL and why it is being adopted by the institution. Similarly to understanding the foundation of problem-based learning, awareness of self-directed learning (SDL) is another integral component to being able to incorporate this method into a curriculum. Students understood SDL as a self-motivated and independent process, using ones preferred learning styles. It was viewed as a manageable and comfortable way to learn. It is apparent that students currently use SDL as a way to supplement and enhance their learning within the didactic curriculum, by reading extra resources about a specific topic on their own time. Students familiarity with using SDL is a factor that would facilitate integration of PBL into the permanent curriculum. Integrating PBL would allow the students to move from using SDL as a learning supplement to using it as a primary mode of life-long learning.
Readiness for small-group learning Prior to the PBL project, we asked about medical students perceptions of working with their classmates. For students to prosper in a team-based learning environment, it is important for them to trust each other, collaborate, and appreciate the value of learning from their peers. Interestingly, the students expressed mixed feelings about working with and learning from their peers, which we believe may be partly due to their existing didactic curriculum. Without the opportunity to collaborate and problemsolve with their peers on a regular basis, students may be unable to develop highly positive professional impressions of each other. However, students acknowledged that working in groups improves efficiency on health-care teams and would help them to think positively about these interactions in the future. Evidently, there was a desire among students to enhance these team-based, collaborative experiences during their undergraduate medical education. Implementing PBL into the curriculum would address these desires. The surgical clerks descriptions of small group learning both before and after the PBL pilot project demonstrated an overall positive change in attitude. Some of the most common positive terms used were: willing, effective, and optimistic. The negative terms included skeptical, distracting, and unsure. However, the number of negative words used to describe small group learning greatly decreased following the PBL pilot. This demonstrates that overall, students had a positive impression of PBL during the pilot project. Tutor feedback and moving forward In follow-up discussion with the local tutors (surgical staff), several strengths of the PBL pilot project were identified including: (1) it encouraged interaction between both students and tutors and helped to break barriers; (2) students learned to take on more responsibility; (3) a process of self-realization occurred through the learning process; and (4) it was a targeted way to discuss a topic which met the needs of students. Some of the challenges identified by the tutors were as follows: (1) staff members faced a lack of time and incentive to prepare for/facilitate the sessions due to excessive workloads and difficulty scheduling; (2) some students lost interest in the tutorial because it did not involve an evaluation component; (3) there was a need for increased clarity on the roles of students and tutors in the group process; and (4) self-directed learning was a challenge for the students because they are used to didactic teaching. In conclusion, the PBL pilot project received positive feedback from both the surgical clerks and participating staff at GPHC. Students learned from the PBL sessions, felt that its method was equal if not superior to didactic teaching, and developed more positive impressions of small-group learning. They acknowledged that team-working skills are important to develop and would help them become better clinicians in the future. The surgical clerks at GPHC seemed ready and willing to take on PBL as a component of their learning. The staff tutors also advocated that PBL be incorporated into the curriculum. They offered several suggestions on moving forward with the program: (1) educating all faculty and students on the purpose of PBL and the evidence supporting it as a learning methodology; (2) including an evaluation component to tutorial sessions; and (3) training more tutors and creating a case bank. Permanent implementation of PBL into the surgical clerkship rotation would be the first step, with the involvement of other faculties being a possibility in the future.
You might also like
- Positive Learning Framework Creating Learning Environments in Which All Children ThriveDocument6 pagesPositive Learning Framework Creating Learning Environments in Which All Children ThriveDevon SandsNo ratings yet
- Effective Teaching Strategies of Bulacan State University - Sarmiento CampusDocument51 pagesEffective Teaching Strategies of Bulacan State University - Sarmiento CampusPerry Arcilla SerapioNo ratings yet
- A Practical Guide To Implementing Problem-Based Learning in AnesthesiaDocument6 pagesA Practical Guide To Implementing Problem-Based Learning in AnesthesiaMariana Brízido AptxNo ratings yet
- Artikel PBL Dari PubMedDocument8 pagesArtikel PBL Dari PubMedFQFerdianNo ratings yet
- Perception of Students and Faculty On Problem - Based Learning As A Teaching StrategyDocument20 pagesPerception of Students and Faculty On Problem - Based Learning As A Teaching StrategyPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Motivating Learners Through Project-Based LearningDocument10 pagesMotivating Learners Through Project-Based Learningmuhamad hasaniNo ratings yet
- Research Article: Problem Based Learning in Nursing EducationDocument6 pagesResearch Article: Problem Based Learning in Nursing Educationmuhammad zubair khanNo ratings yet
- Wa0010Document11 pagesWa0010api-702415811No ratings yet
- Using Problem Based Learning Method Between 2014 and 2020 With Nursing Students: A Case StudyDocument12 pagesUsing Problem Based Learning Method Between 2014 and 2020 With Nursing Students: A Case Studymalek azisNo ratings yet
- PBL SweeengDocument10 pagesPBL SweeengRichel BulacosNo ratings yet
- Problem Based LearningDocument10 pagesProblem Based LearningFransiska Adriana LarasatiNo ratings yet
- Problem Based Learning at HYMS: A Guide For Students by StudentsDocument57 pagesProblem Based Learning at HYMS: A Guide For Students by StudentsSampurnaPatrenNo ratings yet
- The Future of Modular System of Medical Education: A Teachers' PerspectiveDocument8 pagesThe Future of Modular System of Medical Education: A Teachers' PerspectiveDilawar JanNo ratings yet
- What We Think We Know About The Tutor in Problem-Based LearningDocument6 pagesWhat We Think We Know About The Tutor in Problem-Based LearningroromutiaraNo ratings yet
- HealthcareDocument11 pagesHealthcarewmyartawanNo ratings yet
- El Aprendizaje Indagatorio Mediante Un Proceso Guiado Mejora La Retención de La Información A Largo PlazoDocument9 pagesEl Aprendizaje Indagatorio Mediante Un Proceso Guiado Mejora La Retención de La Información A Largo PlazoGooPop Stoore ChileNo ratings yet
- Introduction To Project Pased LearningDocument10 pagesIntroduction To Project Pased Learninggenius2020No ratings yet
- PCP PlanDocument20 pagesPCP Planapi-316013445100% (1)
- PAYOT - Prevalent Issues On PBLDocument2 pagesPAYOT - Prevalent Issues On PBLpayotrheamaeNo ratings yet
- Impact of Problem-Based Learning On Students'Critical Thinking Dispositions, Knowledge Acquisition and RetentionDocument13 pagesImpact of Problem-Based Learning On Students'Critical Thinking Dispositions, Knowledge Acquisition and RetentionAndrés Cisneros SolariNo ratings yet
- Promoting Problem-Based Learning (PBL) in Engineering Courses at The Universiti Teknologi MalaysiaDocument10 pagesPromoting Problem-Based Learning (PBL) in Engineering Courses at The Universiti Teknologi Malaysiauamiranda3518No ratings yet
- Peer Observation A5 - FinalDocument16 pagesPeer Observation A5 - Finalapi-250421371No ratings yet
- 8626 - Assignment 2 (AG)Document28 pages8626 - Assignment 2 (AG)maalikNo ratings yet
- EJ1089733Document8 pagesEJ1089733Bbrah XcxNo ratings yet
- Linqvodidaktika Serbest Is Seltenet EnverliDocument9 pagesLinqvodidaktika Serbest Is Seltenet EnverligunayNo ratings yet
- Problem Based LearningDocument69 pagesProblem Based LearningPedro Almeida100% (1)
- What Is Project Based Learning and Problem Based LearningDocument5 pagesWhat Is Project Based Learning and Problem Based LearningMashitah Abdul HalimNo ratings yet
- FD Midterm ExamDocument6 pagesFD Midterm ExamRocky Christopher FajardoNo ratings yet
- PBL GuideDocument30 pagesPBL GuideNur Afiqa AzalanNo ratings yet
- PBL, SCL & PoblDocument4 pagesPBL, SCL & PoblKhairul Azhar Abdul LizaNo ratings yet
- Canadian Medical Education JournalDocument4 pagesCanadian Medical Education JournalannegirlNo ratings yet
- I Believe All of Us Are Also Concern About The Implementation of PBL Will Oppose To Our KSSR Science Standard?Document6 pagesI Believe All of Us Are Also Concern About The Implementation of PBL Will Oppose To Our KSSR Science Standard?chew97No ratings yet
- Reviewer For Final Examination in Teaching Technology in Elementary GradesDocument9 pagesReviewer For Final Examination in Teaching Technology in Elementary Gradestoriojocelyn16No ratings yet
- What Is PBL?Document26 pagesWhat Is PBL?Vhim GutierrezNo ratings yet
- The Comprehension of Problem Based Learning Model As The Preparation On PPLDocument6 pagesThe Comprehension of Problem Based Learning Model As The Preparation On PPLMuktiarniNo ratings yet
- Use of Portfolios by Medical Students SignificanceDocument7 pagesUse of Portfolios by Medical Students SignificanceKaro MotiNo ratings yet
- BahavoivalDocument14 pagesBahavoivalAymen JamalNo ratings yet
- Module 1 - Introduction To Problem-Based LearningDocument4 pagesModule 1 - Introduction To Problem-Based LearningLuz Adriana MejiaNo ratings yet
- Bazarte Chapter 1234 1Document63 pagesBazarte Chapter 1234 1Kenjie AmorNo ratings yet
- Context Based LearningDocument6 pagesContext Based LearningSravan Kumar PatibandlaNo ratings yet
- Orientation Programme For New TeacherDocument10 pagesOrientation Programme For New Teacherarchim_azymaNo ratings yet
- Project Based Learning.. Written ReportdocxDocument5 pagesProject Based Learning.. Written ReportdocxCHAVEZ, EVER A.No ratings yet
- Critical Reading Final Task ArticleDocument6 pagesCritical Reading Final Task ArticleMuhammad IlhamNo ratings yet
- Wafa Ibrahim S Alotaibi - Research ProposalDocument10 pagesWafa Ibrahim S Alotaibi - Research Proposalmeraj21No ratings yet
- Why Don'T We Adopt Professional Development School For Indonesian Field Experience Practice?Document8 pagesWhy Don'T We Adopt Professional Development School For Indonesian Field Experience Practice?Widya RatnaNo ratings yet
- Project Based Learning (TTT)Document4 pagesProject Based Learning (TTT)Choukri Brahim HammacheNo ratings yet
- The Strengths and Weaknesses of The Implementation of Project Based Learning: A ReviewDocument7 pagesThe Strengths and Weaknesses of The Implementation of Project Based Learning: A ReviewSulaiman YahyaNo ratings yet
- Development of A Questionnaire To Measure Teachers Studentcentred Perspectives Based On The Onion Model - 2022 - BioMed Central LTDDocument9 pagesDevelopment of A Questionnaire To Measure Teachers Studentcentred Perspectives Based On The Onion Model - 2022 - BioMed Central LTDKang MuksinNo ratings yet
- AMEE 135 Permelee Lecture Free Curriculm Med Tes 2020Document9 pagesAMEE 135 Permelee Lecture Free Curriculm Med Tes 2020Silvina TabordaNo ratings yet
- Lesson 2-WPS OfficeDocument17 pagesLesson 2-WPS OfficeJohn Mark MapusaoNo ratings yet
- The Role of Teacher in PBLDocument10 pagesThe Role of Teacher in PBLfarchanNo ratings yet
- The Effects of The Implementation Problem Oriented Learning Modules Implications For Teaching TechniquesDocument12 pagesThe Effects of The Implementation Problem Oriented Learning Modules Implications For Teaching TechniquesBella SakedanNo ratings yet
- Curriculum Case StudyDocument9 pagesCurriculum Case Studyapi-458907281No ratings yet
- PBL - Nor Azuanee Mukhtar Mp101439Document16 pagesPBL - Nor Azuanee Mukhtar Mp101439Azuanee AzuaneeNo ratings yet
- Accounting Students Problem Based Learning AcceptanceDocument7 pagesAccounting Students Problem Based Learning AcceptanceAdi AliNo ratings yet
- Effectiveness of Problem-Based Learning Implementation: KeywordsDocument13 pagesEffectiveness of Problem-Based Learning Implementation: KeywordsImmas Andaru WinantiNo ratings yet
- Running Head: Curriculum Proposal 1Document31 pagesRunning Head: Curriculum Proposal 1Hum NjorogeNo ratings yet
- Lee 2018Document12 pagesLee 2018some oneNo ratings yet
- A Guide for Culturally Responsive Teaching in Adult Prison Educational ProgramsFrom EverandA Guide for Culturally Responsive Teaching in Adult Prison Educational ProgramsNo ratings yet
- Teachers’ Perceptions of Their Literacy Professional DevelopmentFrom EverandTeachers’ Perceptions of Their Literacy Professional DevelopmentNo ratings yet
- Lesson PlanDocument2 pagesLesson Planapi-357043228No ratings yet
- A Study On Problems of Learning MathematicsDocument3 pagesA Study On Problems of Learning MathematicsSneha Sara SajeevNo ratings yet
- Summary of Five Educational PhilosophiesDocument2 pagesSummary of Five Educational PhilosophiesKheona MartinNo ratings yet
- Manning Selling 3ce Ch04 (Communication Types)Document21 pagesManning Selling 3ce Ch04 (Communication Types)shaalienNo ratings yet
- RUBRICS FOR LESSON PLAN and BLOGDocument3 pagesRUBRICS FOR LESSON PLAN and BLOGMariel Suaiso AngelesNo ratings yet
- Revised Bloom's Taxonomy - ProjectDocument7 pagesRevised Bloom's Taxonomy - Projectdewi agustinaNo ratings yet
- Art Allows Us To Connect With Our Inner SelvesDocument3 pagesArt Allows Us To Connect With Our Inner SelvesPacita MaraonNo ratings yet
- My Pet ReadingDocument5 pagesMy Pet ReadingeilamieraNo ratings yet
- Philosophy Grade 11 - ABM Jan. 6-9,2020Document5 pagesPhilosophy Grade 11 - ABM Jan. 6-9,2020Melody LandichoNo ratings yet
- CSLPA Workshop: EDF 4210 Educational PsychologyDocument24 pagesCSLPA Workshop: EDF 4210 Educational PsychologyKomal KhanNo ratings yet
- Affirmative Side DebateDocument2 pagesAffirmative Side DebateKim LiatNo ratings yet
- Netball PE ReflectionDocument6 pagesNetball PE ReflectionClara CalhounNo ratings yet
- FullDocument136 pagesFullAnn NmayaNo ratings yet
- A Critical Analysis of The Writings of Amos RapoportDocument11 pagesA Critical Analysis of The Writings of Amos RapoportmaxwalkerdreamNo ratings yet
- A Holistic Approach To Improving Thinking SkillsDocument6 pagesA Holistic Approach To Improving Thinking Skillszedrijnali100% (1)
- Hots and Lots in Bloom TaxonomyDocument16 pagesHots and Lots in Bloom TaxonomyNurul RahmayaniNo ratings yet
- 5th Grade Science Lesson Plan - PortfolioDocument2 pages5th Grade Science Lesson Plan - Portfolioapi-475320683No ratings yet
- Deaf Space - ResearchDocument2 pagesDeaf Space - Researcharmein 007No ratings yet
- Rubric Technology Based Assessment-Powtoon Animated Video: Criteria 4 3 2 1Document4 pagesRubric Technology Based Assessment-Powtoon Animated Video: Criteria 4 3 2 1zainudinNo ratings yet
- How To Study A Reading Assignment: The PQRST Method (Preview, Question, Read, State, Test)Document4 pagesHow To Study A Reading Assignment: The PQRST Method (Preview, Question, Read, State, Test)Gobi DurairajNo ratings yet
- Allama Iqbal Open University, Islamabad: (Department of English Language & Applied Linguistics) WarningDocument2 pagesAllama Iqbal Open University, Islamabad: (Department of English Language & Applied Linguistics) WarningranaaliahmedNo ratings yet
- Pro. Ed 2Document10 pagesPro. Ed 2Reynald MatiasNo ratings yet
- Module 8 Working With DepEd FormsDocument4 pagesModule 8 Working With DepEd FormsJenelyn VentozaNo ratings yet
- Teaching With Contrived ExperiencesDocument7 pagesTeaching With Contrived ExperiencesRialyn BaguioNo ratings yet
- Developing EFL Vocabulary Through Speaking and Lis PDFDocument6 pagesDeveloping EFL Vocabulary Through Speaking and Lis PDFSelemane PaquelequeNo ratings yet
- Skills of A Successful TrainerDocument16 pagesSkills of A Successful TrainerShivani BansalNo ratings yet
- 243 961 1 PBDocument7 pages243 961 1 PBeunbi nirNo ratings yet
- Oup Focus Visible Thinking PDFDocument5 pagesOup Focus Visible Thinking PDFFranc NearyNo ratings yet
- Stages of Growth and DevelopmentDocument3 pagesStages of Growth and DevelopmentJaney Cunanan100% (6)
- Weekly Learning Plan EnglishDocument6 pagesWeekly Learning Plan EnglishEvelyn DEL ROSARIONo ratings yet