Professional Documents
Culture Documents
The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Design
The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Design
Uploaded by
amit4513Copyright:
Available Formats
You might also like
- Chaste - Resume RNDocument4 pagesChaste - Resume RNJohn Daniel BayanNo ratings yet
- Prodcution Quercetin PDFDocument8 pagesProdcution Quercetin PDFHamdin Kifahul MuhajirNo ratings yet
- Part 2. Tadalafil AnalogsDocument3 pagesPart 2. Tadalafil AnalogsAndrei StoicaNo ratings yet
- Molecules: Antiparkinson ProdrugsDocument23 pagesMolecules: Antiparkinson ProdrugsShasha elshaNo ratings yet
- Enfoque Ambiental Xu2014 Article DioxinAndDioxin-LikeCompoundsSDocument7 pagesEnfoque Ambiental Xu2014 Article DioxinAndDioxin-LikeCompoundsSJefersson TiqueNo ratings yet
- In Vitro Stability and in Vivo Pharmacokinetic Studies of A Model Opioid Peptide, H-Tyr - Ala-Gly-Phe - Leu-OH (DADLE), and Its Cyclic ProdrugsDocument9 pagesIn Vitro Stability and in Vivo Pharmacokinetic Studies of A Model Opioid Peptide, H-Tyr - Ala-Gly-Phe - Leu-OH (DADLE), and Its Cyclic ProdrugskhurramwmNo ratings yet
- Ijppp 0000020Document6 pagesIjppp 0000020ZevannayasmineNo ratings yet
- Nicotinamide Adenine Dinucleotide Phosphate - WikipediaDocument24 pagesNicotinamide Adenine Dinucleotide Phosphate - WikipediaBashiir NuurNo ratings yet
- Karimi 2020Document13 pagesKarimi 2020Nelson Daniel Marcano AguileraNo ratings yet
- DPI O'DonnellDocument9 pagesDPI O'DonnellNadia DivakovaNo ratings yet
- Reisser2002 Ic50Document4 pagesReisser2002 Ic50Jesús Rafael Méndez NateraNo ratings yet
- The Inhibitory Effects of Boldine, Glaucine, and Probucol On Tpa-Induced Down Regulation of Gap Junction FunctionDocument9 pagesThe Inhibitory Effects of Boldine, Glaucine, and Probucol On Tpa-Induced Down Regulation of Gap Junction Functionmonu kashyapNo ratings yet
- 3 PaperDocument10 pages3 PaperMehran BashirNo ratings yet
- Analytical Biochemistry: Liang-Jun Yan, Michael J. ForsterDocument7 pagesAnalytical Biochemistry: Liang-Jun Yan, Michael J. ForsterGadiezz Iy-ma NieaNo ratings yet
- Involvement of the γ Isoform of cPLA in the Biosynthesis of Bioactive N-AcylethanolaminesDocument14 pagesInvolvement of the γ Isoform of cPLA in the Biosynthesis of Bioactive N-AcylethanolaminesRobert MargineanNo ratings yet
- De Novo Biosynthesis and Radiolabeling ofDocument9 pagesDe Novo Biosynthesis and Radiolabeling ofElizabeth Parral HerreraNo ratings yet
- tmp5B01 TMPDocument14 pagestmp5B01 TMPFrontiersNo ratings yet
- Bioorganic & Medicinal Chemistry LettersDocument5 pagesBioorganic & Medicinal Chemistry Lettersneha bhatiaNo ratings yet
- Structure and Regulation of Human Phospholipase DDocument10 pagesStructure and Regulation of Human Phospholipase Dxtang2No ratings yet
- Anti Tubercular ActivityDocument34 pagesAnti Tubercular ActivityRamya Gopala KrishnanNo ratings yet
- J. Biol. Chem.-2011-Okumoto-44367-79Document14 pagesJ. Biol. Chem.-2011-Okumoto-44367-79Romana MasnikosaNo ratings yet
- Effect of A Cordless Retraction Paste Material On Implant Surfaces: An in Vitro StudyDocument11 pagesEffect of A Cordless Retraction Paste Material On Implant Surfaces: An in Vitro StudyPaul BudionganNo ratings yet
- Van Rooy 2012Document6 pagesVan Rooy 2012It's RohanNo ratings yet
- Diketopiperazines RevDocument27 pagesDiketopiperazines RevIsaí MillánNo ratings yet
- Molecules 16 04104Document18 pagesMolecules 16 04104Josué VelázquezNo ratings yet
- Cell-Specific mRNA Alterations in Na+, K+-ATPase α and β Isoforms and FXYD in Mice Treated Chronically with Carbamazepine, an Anti-Bipolar DrugDocument8 pagesCell-Specific mRNA Alterations in Na+, K+-ATPase α and β Isoforms and FXYD in Mice Treated Chronically with Carbamazepine, an Anti-Bipolar DrugGading AuroraNo ratings yet
- Metode NADPHDocument16 pagesMetode NADPHYovi AviantoNo ratings yet
- Adrenergic Agents: Shengquan LiuDocument36 pagesAdrenergic Agents: Shengquan LiuAnaliza Kitongan LantayanNo ratings yet
- Vit e Loaded PLGADocument14 pagesVit e Loaded PLGACătălina RădulescuNo ratings yet
- Thermodynamic Study of Cu - Binding To The DAHK and GHK Peptides by Isothermal Titration Calorimetry (ITC) With The Weaker Competitor GlycineDocument28 pagesThermodynamic Study of Cu - Binding To The DAHK and GHK Peptides by Isothermal Titration Calorimetry (ITC) With The Weaker Competitor Glycinemazinasi53No ratings yet
- Bioorganic & Medicinal ChemistryDocument8 pagesBioorganic & Medicinal ChemistryEdgar AponteNo ratings yet
- Journal of Drug Delivery Science and TechnologyDocument5 pagesJournal of Drug Delivery Science and TechnologyFaizhal Dimas LeksonoNo ratings yet
- Stability and Enzymatic Studies With Omeprazole:Hydroxypropyl - CyclodextrinDocument10 pagesStability and Enzymatic Studies With Omeprazole:Hydroxypropyl - CyclodextrinPharma StpNo ratings yet
- Dib Sample PaperDocument6 pagesDib Sample Papervenkatesab DNo ratings yet
- Optimización Estructural y Evaluación Biológica de Derivados Sustituidos de BisfenolDocument18 pagesOptimización Estructural y Evaluación Biológica de Derivados Sustituidos de Bisfenolmaria joseNo ratings yet
- Hepatotoxicity in Rats Treated With Dimethylformamide or Toluene or BothDocument7 pagesHepatotoxicity in Rats Treated With Dimethylformamide or Toluene or BothmuammarNo ratings yet
- BIO 120 Exer 7Document4 pagesBIO 120 Exer 7Asi Jen100% (1)
- Bioorganic & Medicinal Chemistry Letters: Sciverse SciencedirectDocument7 pagesBioorganic & Medicinal Chemistry Letters: Sciverse SciencedirectHM BelphegorNo ratings yet
- Anti 10 PDFDocument5 pagesAnti 10 PDFTetteh JudeNo ratings yet
- Li BerkeleyoneDocument6 pagesLi BerkeleyoneVõ Quốc CườngNo ratings yet
- Nitric Oxide, CGMP, and Hormone Regulation of Active Sodium TransportDocument6 pagesNitric Oxide, CGMP, and Hormone Regulation of Active Sodium TransportMichael Daley100% (1)
- Discovery of A Highly Selective and Efficient Reagent For Formation of Intramolecular Disulfide Bonds in PeptidesDocument7 pagesDiscovery of A Highly Selective and Efficient Reagent For Formation of Intramolecular Disulfide Bonds in PeptidesSveti JeronimNo ratings yet
- Ijms 21 01505Document37 pagesIjms 21 01505Ary MfNo ratings yet
- Blanckaert 2009Document8 pagesBlanckaert 2009Peter BlanckaertNo ratings yet
- Life Sciences Assignment: The Sodium-Potassium PumpDocument6 pagesLife Sciences Assignment: The Sodium-Potassium PumpShivam MishraNo ratings yet
- Docosahexaenoic AcidDocument10 pagesDocosahexaenoic AcidCrina LupuNo ratings yet
- Articulo Quimica Medicinal 3Document16 pagesArticulo Quimica Medicinal 3Jose Antonio Espinosa TorresNo ratings yet
- Characterization of A Theme C Glycoside Hydrolase Family 9 Endo-Beta-Glucanase From A Biogas Reactor MetagenomeDocument7 pagesCharacterization of A Theme C Glycoside Hydrolase Family 9 Endo-Beta-Glucanase From A Biogas Reactor MetagenomeKhairul NasrizalNo ratings yet
- Asher Kalir Et Al - N - Allyl Analogues of Phencyclidine: Chemical Synthesis and Pharmacological PropertiesDocument5 pagesAsher Kalir Et Al - N - Allyl Analogues of Phencyclidine: Chemical Synthesis and Pharmacological PropertiesBic0000No ratings yet
- Paper Gen PBP4Document4 pagesPaper Gen PBP4Leo FigueroaNo ratings yet
- Nicotinamide Adenine Dinucleotide - WikipediaDocument116 pagesNicotinamide Adenine Dinucleotide - WikipediaBashiir NuurNo ratings yet
- Zns 9173Document9 pagesZns 9173JuanokNo ratings yet
- Angelo BanaresDocument11 pagesAngelo BanaresNathan Russel PangilinanNo ratings yet
- EugeniPIller PNAS 11Document12 pagesEugeniPIller PNAS 11Felix Ernst KesslerNo ratings yet
- Blei 2018Document4 pagesBlei 2018luke100% (1)
- Polygala TenuifoliaDocument5 pagesPolygala TenuifoliaTuấn Nguyen AnhNo ratings yet
- Dopamine Receptor SignalingDocument42 pagesDopamine Receptor SignalingHir SavaNo ratings yet
- Redox Biology: John B. Hibbs JR., Zdenek Vavrin, James E. CoxDocument14 pagesRedox Biology: John B. Hibbs JR., Zdenek Vavrin, James E. CoxNidya Aryanda KNo ratings yet
- Zhao Et Al. - 2009 - Decreased TK Activity Contributes To Impaired Hippocampal Neurogenesis in TDDocument10 pagesZhao Et Al. - 2009 - Decreased TK Activity Contributes To Impaired Hippocampal Neurogenesis in TDmarej312No ratings yet
- An Electroporation Protocol For Efficient DNA Transfection in PC12 CellsDocument11 pagesAn Electroporation Protocol For Efficient DNA Transfection in PC12 CellsnaganathNo ratings yet
- Thesis Statement - Louis DavidDocument3 pagesThesis Statement - Louis DavidLoushitNo ratings yet
- BSI - Case Report Form Design IssuesDocument19 pagesBSI - Case Report Form Design IssuesKatti VenkataramanaNo ratings yet
- Provisional RestorationsDocument9 pagesProvisional RestorationsshivaprasadmNo ratings yet
- Sampleresponseletters PDFDocument4 pagesSampleresponseletters PDFlevanah87369No ratings yet
- HyperthermiaDocument2 pagesHyperthermiapamgee100% (11)
- Waterleau - Ebrochure Lucas - EngDocument10 pagesWaterleau - Ebrochure Lucas - EngAlaa SalemNo ratings yet
- Review ArticleDocument18 pagesReview Articlenasution hariNo ratings yet
- Assessment and Management of The Unconscious PatientDocument6 pagesAssessment and Management of The Unconscious PatientRed DevilNo ratings yet
- The Mind's Own Physician: A Scientific Dialogue With The Dalai Lama On The Healing Power of MeditationDocument20 pagesThe Mind's Own Physician: A Scientific Dialogue With The Dalai Lama On The Healing Power of MeditationNew Harbinger Publications75% (4)
- Country Paper IndiaDocument63 pagesCountry Paper IndiaShashank16No ratings yet
- CG252 2012-07 Common Ground MagazineDocument40 pagesCG252 2012-07 Common Ground MagazineCommonGroundBCNo ratings yet
- Dr. Ayushi Verma, BDS: Professtional SummaryDocument2 pagesDr. Ayushi Verma, BDS: Professtional SummaryAyushi VermaNo ratings yet
- PsycoanalyticDocument55 pagesPsycoanalyticAdarsh S MelparampilNo ratings yet
- SPGDT Hospital: DR I Ketut Wiargitha, SPB (K) Trauma, FinacsDocument68 pagesSPGDT Hospital: DR I Ketut Wiargitha, SPB (K) Trauma, FinacsOgizWaraNo ratings yet
- Osteotomy The BasicsDocument13 pagesOsteotomy The BasicsHari25885No ratings yet
- Suturing TechniquesDocument5 pagesSuturing TechniquesAndikaPurbaNo ratings yet
- Animal BitesDocument5 pagesAnimal BitesvyalylaNo ratings yet
- Goodman & Snyder: Differential Diagnosis For Physical Therapists, 5th EditionDocument2 pagesGoodman & Snyder: Differential Diagnosis For Physical Therapists, 5th EditionZainab WaqarNo ratings yet
- Allergy Skin TestsDocument6 pagesAllergy Skin TestsAnindya Putri KusumajatiNo ratings yet
- Careersguide Medical WritingDocument40 pagesCareersguide Medical Writingbeiza1979100% (1)
- Role Play DiareDocument7 pagesRole Play DiareNi Putu aristaNo ratings yet
- DiureticsDocument29 pagesDiureticsSaravanan RajagopalNo ratings yet
- Ultra Month 12Document8 pagesUltra Month 12Milton JuniorNo ratings yet
- Dual DiagnosisDocument4 pagesDual DiagnosisKaroll Martinez DiazNo ratings yet
- 01 Ultra Violet SterilizationDocument14 pages01 Ultra Violet SterilizationNur Sayyid UmarNo ratings yet
- CareplanDocument2 pagesCareplanapi-381090302No ratings yet
- Lysine: An Effective Adjunct Treatment For Herpes Simplex Virus OutbreaksDocument3 pagesLysine: An Effective Adjunct Treatment For Herpes Simplex Virus OutbreaksHerpesSimplexVirus100% (9)
- Public Health Needs Assessment Profile and Health Promotion Proposal by Theresa Lowry Lehnen Specialist Nurse Practitioner in Conjunction With Surrey University 2005Document46 pagesPublic Health Needs Assessment Profile and Health Promotion Proposal by Theresa Lowry Lehnen Specialist Nurse Practitioner in Conjunction With Surrey University 2005Theresa Lowry-LehnenNo ratings yet
- NCP Activity NavidasDocument2 pagesNCP Activity NavidasFran LanNo ratings yet
The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Design
The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Design
Uploaded by
amit4513Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Design
The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Design
Uploaded by
amit4513Copyright:
Available Formats
The Open Medicinal Chemistry Journal, 2008, 2, 97-100
97
Open Access
The Utility of Oligopeptidase in Brain-Targeting Delivery of an Enkephalin Analogue by Prodrug Design
K. Prokai-Tatrai*,1, H.-S. Kim2 and L. Prokai3
Department of Pharmacology and Neuroscience, University of North Texas Health Science Center, Fort Worth, TX, USA
2 3 1
College of Agricultural and Life Sciences, Kangwon National University, Korea
Department of Molecular Biology and Immunology, University of North Texas Health Science Center, Fort Worth, TX, USA
Abstract: In a brain-targeting prodrug approach for a metabolically stable enkephalin analogue DADLE, specific enzymes are utilized for in vivo prodrug activation. Prolyl oligopeptidase (POP) may be especially useful in this regard. In vitro metabolic stability of the putative metabolites of prodrugs having various spacers has shown that POP provides significantly faster release of DADLE from conjugates having dipeptidyl spacer (specifically Xaa-Pro or Xaa-Ala) than alternative peptidases utilized when single amino acids are used as spacers. In vitro half-lives measured in rat brain homogenate showed excellent correlation with CNS-mediated analgesia using the tail-flick model in rats providing, thus, an in vivo substantiation of the prodrug approach relying on POP as the peptidase to release DADLE.
Keywords: Enkephalin, DADLE, prolyl oligopeptidase (POP), brain-targeting prodrug, antinociception. INTRODUCTION Enkephalins are opioids and potential neuropharmaceuticals for pain relief without the undesired side-effects associated with the use of morphine and other alkaloid analgesics [1]. These endogenous linear pentapeptides are, however, easily degraded by peptidolytic enzymes [2] rendering their action short-lasting, unless peptidase inhibitors are used simultaneously [3]. Therefore, a wide variety of analogues with increased in vivo stability have been designed and evaluated. A -opioid receptor-selective enkephalin analogue Tyr-D-Ala-Gly-Phe-D-Leu (DADLE), is a representative of such compounds [4]. In spite of adequate metabolic stability of DADLE and the majority of synthetic neuropeptide analogues, these agents still face a formidable obstacle, the blood brain barrier (BBB), in terms of reaching the central nervous system (CNS) upon systemic administration [5]. The BBB, acting as a lipoidal bilayer, practically excludes the entry of these hydrophilic substances into the brain by passive transport. Additionally, BBB may also represent an enzymatic barrier for peptides. As such, the limited bioavailability of the otherwise promising peptide-based neuropharmaceuticals presents a major disadvantage for practical drug development. Invasive and non-invasive strategies have been developed to outwit the BBB [6]. Among non-invasive methods, prodrug design is perhaps the most versatile chemical manipulation technique that bioreversibly modifies the parent
*Address correspondence to this author at the Department of Pharmacology & Neuroscience, University of North Texas Health Science Center, Fort Worth, TX 76107, USA; Tel: 1-817-735-0617; Fax: 1-817-735-2118; E-mail: kprokai@hsc.unt.edu 1874-1045/08
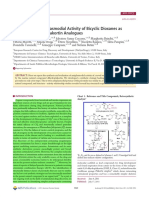
peptide for improving CNS bioavailability and targeting. A specific approach within prodrug design is the use of a braintargeting chemical delivery system (BTCDS) [7]. BTCDS, as a prodrug, is biologically inactive per se [8] and requires in vivo enzymatic conversion(s) to the biologically active agent and provides enhanced drug delivery to the brain, the site of action. In peptide-based BTCDS, the lipophilic 1,4dihydrotrigonellyl transport moiety [7] is covalently attached to the N-terminus of the parent peptide via spacer amino acid(s). In the brain, however, a coenzyme associated with numerous oxidoreductases and cellular respiration oxidizes the dihydropyridine to permanently charged N-methylpyridinium (trigonellyl, T+), analogously to the oxidation of NAD (P)H to NADP+ [7]. The oxidized BTCDS apparently cannot leave the brain by passive transport, and it has not been identified as a potential substrate for endogenous efflux transporters either [9]. A strategically selected spacer ensures, then, the release of the parent peptide in the brain by specific peptidases [10, 11] that remove the T+-Spacer moiety [11] from the oxidized BTCDS. Previously, we have reported a successful application of this approach to transport DADLE [11, 12] into the brain (Fig. 1). The C-terminus of DADLE was esterified with highly lipophilic alcohols, such as cholesterol (Ch-OH) to furnish adequate lipophilicity of the BTCDS necessary to BBB transport [9]. This ester group can easily be cleaved by lipases and/or esterases during or after diffusion through the BBB. Alanine (Ala) or proline (Pro)-based spacer (S) was originally chosen because of the suggested involvement of alanyl and prolyl aminodipeptidyl peptidases (EC 3.4.14.2 and/or EC 3.4.14.5) [13] in the enkephalinergic transmission in the brain. However, as it turned out [14], these enzymes can also be utilized for the release of other neuropeptides,
2008 Bentham Open
98 The Open Medicinal Chemistry Journal, 2008, Volume 2
Prokai-Tatrai et al.
such as thyrotropin releasing hormone, from the corresponding oxidized BTCDS. Additionally, peptidyl glycine amidating monooxygenase (PAM) may also be exploited for peptide-based brain-targeting prodrug design [14,15]. In vivo substantiation of the approach for DADLE shown in Fig. (1) was done by monitoring the antinociceptive effect produced after intravenous (iv) administration of BTCDSs in rats. Although BTCDSs containing either Pro or Ala spacer (1a and 1b, respectively) showed a profound, centrallymediated and long-lasting analgesia, 1a was more potent than 1b in terms of producing a quicker onset and longer duration of tail-flick latencies [12]. Consequently, we concluded that the spacer was the most important architectural element of the BTCDS (1a-d) to manipulate the rate of DADLE release and, thus, the production of analgesia by utilizing specific peptidases (probably EC 3.4.14.2 and/or EC 3.4.14.5). We have also reasoned that another type of enzymes such as prolyl oligopeptidase (POP, EC 3.4.21.26, that has specific cleaving sites in a peptide sequence [16] may also be used to control peptide release from the oxidized BTCDSs according to the therapeutic objectives. The present studies were undertaken to provide in vitro evidence of this hypothesis [17], together with an in vivo investigation of the pharmacological consequences of introducing Pro-Pro (1c) and Ala-Ala (1d) dipeptidyl spacers into BTCDSs for potential exploitation of POP [16] in braintargeting delivery of DADLE by prodrug design. SYNTHESIS Selected BTCDSs having Pro-Pro or Ala-Ala spacer and Cho ester on their C-termini (1c and 1d, Fig. 1) were synthesized analogously to that of 1a and 1b (S=Pro and S=Ala, respectively) by a segment coupling method we have developed to obtain these types of peptide conjugates [12]. Briefly, Nicotinoyl-(S)-D-Ala-Gly-Phe-OH was prepared by routine Fmoc-based solid phase peptide synthesis (SPPS) in a Synthor 2000 instrument (Peptide International, Louisville, KY) and then coupled to D-Leu-OCho in solution phase using PyBOP/HOBt/DIPEA activation The latter lipophilic ester of the C-terminal amino acid (D-Leu-OH) was prepared by solution-phase Boc-chemistry. Once Nicotinoyl-(S)DADLE-OCho was assembled, column chromatographic purification (silicagel, chloroform/methanol 9:1, v/v) was done. Then the nicotinoyl residue was converted to trigonellyl (T+) using MeI. After the well-established reduction using Na2S2O4 [18] the BTCDSs were obtained. This reduction was conveniently monitored by UV spectroscopy (Lambda 11 UV/Vis Perkin Elmer spectrometer; Perkin Elmer Anal. Inst., Norwalk, CT) in methanol that showed the unequivocal conversion of T+ ( =254 nm) to 1,4-dihydropyridine (T) ( =355 nm). The putative oxidized metabolites 2a-e from which DADLE may be directly released were also synthesized by routine Fmoc-based SPPS. As control, 2g having no spacer moiety was also prepared. All test compounds were thoroughly purified by reversed-phased high performance liquid chromatography (RP-HPLC) and identified by electrospray-ionization mass spectrometry (ESI-MS), as described before [12].
O (S) Spacer DADLE-OCho
N CH3 1a-d O (S) Spacer N CH3 2a-d DADLE 4. Peptidase (EC 3.4.14.2 and/or EC 3.4.14.5 for a,b EC3.4.2126 for c,d) DADLE a: Spacer = Pro b: Spacer = Ala c: Spacer = Pro-Pro d: Spacer = Ala-Ala 1. Passive transport through the BBB 2. Enzymatic oxidation 3. Lipase/esterase
T+
Fig. (1). Schematic illustration of a BTCDS for DADLE, Tyr-DAla-Gly-Phe-D-Leu. OCho represents cholesteryl ester [12].
IN VITRO STABILITY STUDIES Stability studies of the predicted biotransformation products, T+-S-DADLE, of the BTCDSs have been performed in rat brain homogenate [17]. Approximately 250 nmol of 2a-g, dissolved in 100 mL DMSO, was added to 1 mL of freshly made rat brain homogenate (20% w/w, pH 7.4 Tris buffer [19]). For comparison, T+-DADLE (2g), in which DADLE is directly attached to T+ was also studied to underline the importance of the spacer in the molecular architecture of such type of BTCDSs. The mixture was incubated at 37 C in a temperature controlled, shaking water bath. Aliquots (100 L) were taken after 5, 15, 30, 45, 60, and 90 min of incubation, and transferred to 1.5 mL plastic centrifuge tubes containing 200 L of ice-cold 1 M aqueous acetic acid. After centrifugation at 12500g for 15 min, the supernatant was removed and analyzed by microbore HPLC on a system consisting of a ThermoSeparation/Spectra-Physics (Fremont, CA) Spectra Series P200 binary gradient solvent delivery system, a Rheodyne (Cotati, CA) Model 7125 injector valve equipped with a 5 L sample loop, a Spectroflow 757 variable wavelength UV/Vis detector (Kratos Analytical, Manchester, U.K.) operated at 216 nm. As shown in Table 1, the conjugate without a spacer (2g) is extremely stable (t is almost 8 h); thus, no release of DADLE in the brain could be expected from the corresponding prodrug. This finding supports the notion that amidase activity is low in the brain [7]. When a single amino-acid spacer was used and prolyl and alanyl aminodipeptidyl peptidases were the apparent processing enzymes responsible for DADLE release, 2a (S=Pro) was approximately 3-times less stable than 2b (S=Ala). This observation is in agreement with our previous in vivo findings [12]; a more profound and
The Utility of Oligopeptidase in Brain-Targeting Delivery
The Open Medicinal Chemistry Journal, 2008, Volume 2
99
earlier onset of analgesia was produced with Pro (1a) compared to that of Ala (1b) as a spacer (see Table 3). When dipeptidyl spacers (specifically Xaa-Pro or XaaAla) were used where POP is expected to be the processing enzyme [16], then the half-life of 2c (S =Pro-Pro) was especially short (<10 min), suggesting the very quick release of DADLE in the brain. Interestingly, in case of Ala-Ala (2d), Pro-Ala (2e) or Ala-Pro (2f) combinations, the in vitro halflives were practically the same (around 20 min) that may imply that the affinity of POP to Pro is somewhat higher than to Ala, especially when Pro is the preceding amino acid. (Under our experimental conditions, t1/2 for DADLE was around 730 min). Nevertheless, these in vivo data clearly show that the metabolic stability and, thus, DADLE releasing rate of the putative metabolites (2a-f) of the corresponding BTCDSs can be manipulated by strategically selecting the spacer function.
Table 1. Metabolic Stability of T+-S-DADLE and T+-DADLE in Rat Brain Homogenate
Putative Metabolite T+-Pro-DADLE (2a) T+-Ala-DADLE (2b) T -Pro-Pro-DADLE (2c) T -Ala-Ala-DADLE (2d) T -Pro-Ala-DADLE (2e) T -Ala-Pro-DADLE (2f) T -DADLE (2g)
+ + + + +
measured very short in vitro half-lives in brain homogenate may also predict a quick onset of analgesia upon i.v. administration of the BTCDSs having dipeptidyl spacers. The distribution of POP activity within the brain was also investigated by incubating 100 M 2c (S=Pro-Pro) in homogenates of different brain sections (Table 2) analogously to the metabolic studies involving whole brain homogenate (Table 1). Among the studied brain sections, the highest metabolism was measured in the cortex, while 2c was quite stable (t1/2 > 1 h) in the medulla oblongata indicating low POP activity in this region of the brain. These observations are in agreement with findings about the uneven distribution of POP in the brain [20, 21]. Therefore, because POP is exclusively expressed by neurons and display region-specific distribution in the mouse brain, POP-activated prodrugs may be especially useful to target neurons in select regions (cortex, cerebellum, striatum and mid-brain) of the brain. ANALGESIC ACTIVITY In vivo substantiation of the in vitro metabolic stability studies (Table 1) and, thus, DADLE release in the brain from 1c and 1d as representative prodrugs having dipeptidyl spacer was done by monitoring CNS-mediated analgesia in rats upon i.v. injection of the BTCDSs (in 1:9 v/v DMSO : 20% w/v aqueous hydroxypropyl- -cyclodextrin) using the tail-flick model [11, 12, 22]. The latency of the tail-flick response to radiant heat (focused in the middle of the tail) was measured by using a Tail-Flick Analgesia Meter 0570001L (Columbus Instruments, Columbus, OH, USA). Baseline latencies (5-6 s) were collected for 15 min prior to prodrug administration, and tail-flick latency was measured at various times up to 6 h following BTCDS administration. Groups of 5-10 animals were treated with vehicle control or the prodrugs at 4.2 mol/kg of body weight dose. Data generated from the studies comparing treatment groups were subjected to analysis of variance (ANOVA) followed by Dunnetts post hoc procedure to detect significant differences (P> 0.05) between groups [23]. Administration of the dipeptidyl spacer-containing prodrugs (1c and 1d) produced analgesia significantly faster than prodrugs having single amino acid spacer (1a and 1b, respectively) as shown in Table 3. These data show excellent correlations with the measured in vitro half-lives (Table 1). The corresponding putative metabolites 2c and 2d were approximately 40-fold less stable in vitro than 2a and 2b, respectively, although more potent antinociception was observed with the use of single amino acid spacers where dipeptidyl aminopeptidase was the processing enzyme. In summary, our data clearly show that utilizing POP in brain-targeting prodrug design to transport peptides into the brain could be especially useful when the therapeutic objective calls for a very quick onset of action, thus, release of the parent peptide. We have also envisioned that, by optimizing the amino acid that precedes Pro or Ala in the dipeptidyl spacers shown here, the release of the biologically active peptide could further be controlled. These studies will be published separately.
t1/2 (min) 346 963 9 23 24 24 4620
Concentrationtime profiles were analyzed by exponential fitting assuming pseudofirst order degradation. In vitro half-lives (t1/2) were calculated from rate constant (k) as 0.693/k.
Table 2.
Metabolic Stability of T+-Pro-Pro-DADLE (2c) in Homogenates of Rat Brain Sections
Brain Section
t1/2 (min)
4 72 9 12 28 12 9
Cortex Medulla Oblongata Cerebellum Striatum Hypothalamus Mid-brain Whole brain
Concentration-time profiles were analyzed by exponential fitting assuming pseudo-first order degradation. In vitro half-lives (t1/2) were calculated from rate constant (k) as 0.693/k.
The in vitro release of DADLE and the concomitant loss of the T+-S moiety were unequivocally shown by ESI-MS analysis (data not shown) [12,17]. Altogether, it can be concluded that POP, indeed, can be utilized for the release of DADLE from the corresponding oxidized BTCDSs. The
100 The Open Medicinal Chemistry Journal, 2008, Volume 2
Prokai-Tatrai et al. [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16] [17] [18] [19] [20] [21] [22] [23] Miller, R.M.; Chang, K.J.; Cuatrecasas, P.; Wilkinson, S. Biochem. Biophys. Res. Commun., 1977, 4, 1311. Prokai-Tatrai, K.; Prokai, L. In Peptide Transport and Delivery into the Central Nervous System; Prokai and Prokai-Tatrai, Eds.; Birkhauser: Basel, 2003, Vol. 61, pp.157-188. Prokai, L. Exp. Opin. Ther. Patents, 1997, 7, 233. Prokai, L.; Prokai-Tatrai, K.; Bodor, N. Med. Res. Rev., 2000, 20, 367. Albert, A. Nature, 1958, 18, 421. Begley, D.J.; Brightman, M.W. In Peptide Transport and Delivery into the Central Nervous System; Prokai and Prokai-Tatrai, Eds.; Birkhauser: Basel, 2003, Vol. 61, pp. 41-78. Walter, R.; Simmons, W.H. Mol. Cell. Biochem., 1980, 30, 111. Bodor, N.; Prokai, L.; Wu, W.M.; Farag, S.; Jonalagadda, S.; Kawamura, M.; Simpkins, J.W. Science, 1992, 257, 1698. Prokai-Tatrai, K.; Prokai, L.; Bodor, N. J. Med. Chem., 1996, 39, 4775. Schwartz, J.C.; Malroy, B.; De LA Baume, S. Life Sci., 1981, 29, 1715. Prokai, L.; Prokai-Tatrai, K.; Ouyang, X.; Kim, H.-S.; Wu, W.M.; Zharikova, A. J. Med. Chem., 1999, 42, 4563. Stevens, S. Jr.; Prokai-Tatrai, K.; Prokai. L. Anal. Chem., 2005, 77, 698. Polgar, L. Curr. Med. Chem. CNS Agents, 2002, 2, 251. Kim, H. S. Thesis, University of Florida, 1997. Carelli, V.; Liberatore, F.; Scipione, L.; Musio, R.; Sciacovelli, O. Tetrahedron Lett., 2000, 8, 1235. Prokai-Tatrai, K.; Perjesi, P.; Rivera-Portalatin, N.M.; Prokai, L. Steroids, 2008, 73, 280. Rossner, S.; Schulz, I.; Zeitschel, U; Schliebs, R.; Bigl, V.; Demuth, H.U. Neurochem. Res., 2005, 30, 695. Myhnen, T.; Venlinen, J.; Garcia-Horsman, J.; Mnnist, P. Neuroscience, 2008, 2, 1177. All procedures were reviewed and approved by the Institutional Animal Care and Use Committee at the University of Florida, Gainesville, before initiation of the study. Glantz, S.A. Primer of Biostatistics, 5th ed.; McGraw-Hill: New York, 2002, pp. 99-103.
Table 3.
Antinociception in Sprague-Dawley Rats After i.v. Injection (4.2 mol/kg Body Weight Dose) of Prodrugs 1a-d of DADLE
Prodrug 1a S=Pro 1b S=Ala 1c S=Pro-Pro 1d S=Ala-Ala ~TMAX (min) 30 60 5 5-10 Anti-Nociceptiona 2.7 2.1 1.6 1.8
Antinociception was defined as (Maximum latency Baseline latency)/Baseline latency. TMAX was defined as time (min) to reach maximum tail-flick latency.
ACKNOWLEDGEMENTS The authors conducted the studies presented here while working at the Center for Drug Discovery, University of Florida. Technical assistance of Zoltan Szeiler with the tailflick latency measurements and support by Nicholas Bodor during these studies are acknowledged. REFERENCES
[1] [2] [3] Gentilucci, L. Curr. Top. Med. Chem., 2004, 4, 19. Roques, B.P.; Noble, F.; Daugie, V.; Fournie-Zaluski, M.C.; Beaumont, A. Pharmacol. Rev., 1993, 45, 87. Uchiyama, T.; Kotani, A.; Kishida, T.; Tatsumi, H.; Okamoto, A.; Fujita, T.; Murakami, M.; Muranishi, S.; Yamamoto, A. J. Pharm. Sci., 1998, 87, 448.
Received: August 27, 2008
Revised: September 19, 2008
Accepted: September 19, 2008
Prokai-Tatrai et al.; Licensee Bentham Open. This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/bync/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
You might also like
- Chaste - Resume RNDocument4 pagesChaste - Resume RNJohn Daniel BayanNo ratings yet
- Prodcution Quercetin PDFDocument8 pagesProdcution Quercetin PDFHamdin Kifahul MuhajirNo ratings yet
- Part 2. Tadalafil AnalogsDocument3 pagesPart 2. Tadalafil AnalogsAndrei StoicaNo ratings yet
- Molecules: Antiparkinson ProdrugsDocument23 pagesMolecules: Antiparkinson ProdrugsShasha elshaNo ratings yet
- Enfoque Ambiental Xu2014 Article DioxinAndDioxin-LikeCompoundsSDocument7 pagesEnfoque Ambiental Xu2014 Article DioxinAndDioxin-LikeCompoundsSJefersson TiqueNo ratings yet
- In Vitro Stability and in Vivo Pharmacokinetic Studies of A Model Opioid Peptide, H-Tyr - Ala-Gly-Phe - Leu-OH (DADLE), and Its Cyclic ProdrugsDocument9 pagesIn Vitro Stability and in Vivo Pharmacokinetic Studies of A Model Opioid Peptide, H-Tyr - Ala-Gly-Phe - Leu-OH (DADLE), and Its Cyclic ProdrugskhurramwmNo ratings yet
- Ijppp 0000020Document6 pagesIjppp 0000020ZevannayasmineNo ratings yet
- Nicotinamide Adenine Dinucleotide Phosphate - WikipediaDocument24 pagesNicotinamide Adenine Dinucleotide Phosphate - WikipediaBashiir NuurNo ratings yet
- Karimi 2020Document13 pagesKarimi 2020Nelson Daniel Marcano AguileraNo ratings yet
- DPI O'DonnellDocument9 pagesDPI O'DonnellNadia DivakovaNo ratings yet
- Reisser2002 Ic50Document4 pagesReisser2002 Ic50Jesús Rafael Méndez NateraNo ratings yet
- The Inhibitory Effects of Boldine, Glaucine, and Probucol On Tpa-Induced Down Regulation of Gap Junction FunctionDocument9 pagesThe Inhibitory Effects of Boldine, Glaucine, and Probucol On Tpa-Induced Down Regulation of Gap Junction Functionmonu kashyapNo ratings yet
- 3 PaperDocument10 pages3 PaperMehran BashirNo ratings yet
- Analytical Biochemistry: Liang-Jun Yan, Michael J. ForsterDocument7 pagesAnalytical Biochemistry: Liang-Jun Yan, Michael J. ForsterGadiezz Iy-ma NieaNo ratings yet
- Involvement of the γ Isoform of cPLA in the Biosynthesis of Bioactive N-AcylethanolaminesDocument14 pagesInvolvement of the γ Isoform of cPLA in the Biosynthesis of Bioactive N-AcylethanolaminesRobert MargineanNo ratings yet
- De Novo Biosynthesis and Radiolabeling ofDocument9 pagesDe Novo Biosynthesis and Radiolabeling ofElizabeth Parral HerreraNo ratings yet
- tmp5B01 TMPDocument14 pagestmp5B01 TMPFrontiersNo ratings yet
- Bioorganic & Medicinal Chemistry LettersDocument5 pagesBioorganic & Medicinal Chemistry Lettersneha bhatiaNo ratings yet
- Structure and Regulation of Human Phospholipase DDocument10 pagesStructure and Regulation of Human Phospholipase Dxtang2No ratings yet
- Anti Tubercular ActivityDocument34 pagesAnti Tubercular ActivityRamya Gopala KrishnanNo ratings yet
- J. Biol. Chem.-2011-Okumoto-44367-79Document14 pagesJ. Biol. Chem.-2011-Okumoto-44367-79Romana MasnikosaNo ratings yet
- Effect of A Cordless Retraction Paste Material On Implant Surfaces: An in Vitro StudyDocument11 pagesEffect of A Cordless Retraction Paste Material On Implant Surfaces: An in Vitro StudyPaul BudionganNo ratings yet
- Van Rooy 2012Document6 pagesVan Rooy 2012It's RohanNo ratings yet
- Diketopiperazines RevDocument27 pagesDiketopiperazines RevIsaí MillánNo ratings yet
- Molecules 16 04104Document18 pagesMolecules 16 04104Josué VelázquezNo ratings yet
- Cell-Specific mRNA Alterations in Na+, K+-ATPase α and β Isoforms and FXYD in Mice Treated Chronically with Carbamazepine, an Anti-Bipolar DrugDocument8 pagesCell-Specific mRNA Alterations in Na+, K+-ATPase α and β Isoforms and FXYD in Mice Treated Chronically with Carbamazepine, an Anti-Bipolar DrugGading AuroraNo ratings yet
- Metode NADPHDocument16 pagesMetode NADPHYovi AviantoNo ratings yet
- Adrenergic Agents: Shengquan LiuDocument36 pagesAdrenergic Agents: Shengquan LiuAnaliza Kitongan LantayanNo ratings yet
- Vit e Loaded PLGADocument14 pagesVit e Loaded PLGACătălina RădulescuNo ratings yet
- Thermodynamic Study of Cu - Binding To The DAHK and GHK Peptides by Isothermal Titration Calorimetry (ITC) With The Weaker Competitor GlycineDocument28 pagesThermodynamic Study of Cu - Binding To The DAHK and GHK Peptides by Isothermal Titration Calorimetry (ITC) With The Weaker Competitor Glycinemazinasi53No ratings yet
- Bioorganic & Medicinal ChemistryDocument8 pagesBioorganic & Medicinal ChemistryEdgar AponteNo ratings yet
- Journal of Drug Delivery Science and TechnologyDocument5 pagesJournal of Drug Delivery Science and TechnologyFaizhal Dimas LeksonoNo ratings yet
- Stability and Enzymatic Studies With Omeprazole:Hydroxypropyl - CyclodextrinDocument10 pagesStability and Enzymatic Studies With Omeprazole:Hydroxypropyl - CyclodextrinPharma StpNo ratings yet
- Dib Sample PaperDocument6 pagesDib Sample Papervenkatesab DNo ratings yet
- Optimización Estructural y Evaluación Biológica de Derivados Sustituidos de BisfenolDocument18 pagesOptimización Estructural y Evaluación Biológica de Derivados Sustituidos de Bisfenolmaria joseNo ratings yet
- Hepatotoxicity in Rats Treated With Dimethylformamide or Toluene or BothDocument7 pagesHepatotoxicity in Rats Treated With Dimethylformamide or Toluene or BothmuammarNo ratings yet
- BIO 120 Exer 7Document4 pagesBIO 120 Exer 7Asi Jen100% (1)
- Bioorganic & Medicinal Chemistry Letters: Sciverse SciencedirectDocument7 pagesBioorganic & Medicinal Chemistry Letters: Sciverse SciencedirectHM BelphegorNo ratings yet
- Anti 10 PDFDocument5 pagesAnti 10 PDFTetteh JudeNo ratings yet
- Li BerkeleyoneDocument6 pagesLi BerkeleyoneVõ Quốc CườngNo ratings yet
- Nitric Oxide, CGMP, and Hormone Regulation of Active Sodium TransportDocument6 pagesNitric Oxide, CGMP, and Hormone Regulation of Active Sodium TransportMichael Daley100% (1)
- Discovery of A Highly Selective and Efficient Reagent For Formation of Intramolecular Disulfide Bonds in PeptidesDocument7 pagesDiscovery of A Highly Selective and Efficient Reagent For Formation of Intramolecular Disulfide Bonds in PeptidesSveti JeronimNo ratings yet
- Ijms 21 01505Document37 pagesIjms 21 01505Ary MfNo ratings yet
- Blanckaert 2009Document8 pagesBlanckaert 2009Peter BlanckaertNo ratings yet
- Life Sciences Assignment: The Sodium-Potassium PumpDocument6 pagesLife Sciences Assignment: The Sodium-Potassium PumpShivam MishraNo ratings yet
- Docosahexaenoic AcidDocument10 pagesDocosahexaenoic AcidCrina LupuNo ratings yet
- Articulo Quimica Medicinal 3Document16 pagesArticulo Quimica Medicinal 3Jose Antonio Espinosa TorresNo ratings yet
- Characterization of A Theme C Glycoside Hydrolase Family 9 Endo-Beta-Glucanase From A Biogas Reactor MetagenomeDocument7 pagesCharacterization of A Theme C Glycoside Hydrolase Family 9 Endo-Beta-Glucanase From A Biogas Reactor MetagenomeKhairul NasrizalNo ratings yet
- Asher Kalir Et Al - N - Allyl Analogues of Phencyclidine: Chemical Synthesis and Pharmacological PropertiesDocument5 pagesAsher Kalir Et Al - N - Allyl Analogues of Phencyclidine: Chemical Synthesis and Pharmacological PropertiesBic0000No ratings yet
- Paper Gen PBP4Document4 pagesPaper Gen PBP4Leo FigueroaNo ratings yet
- Nicotinamide Adenine Dinucleotide - WikipediaDocument116 pagesNicotinamide Adenine Dinucleotide - WikipediaBashiir NuurNo ratings yet
- Zns 9173Document9 pagesZns 9173JuanokNo ratings yet
- Angelo BanaresDocument11 pagesAngelo BanaresNathan Russel PangilinanNo ratings yet
- EugeniPIller PNAS 11Document12 pagesEugeniPIller PNAS 11Felix Ernst KesslerNo ratings yet
- Blei 2018Document4 pagesBlei 2018luke100% (1)
- Polygala TenuifoliaDocument5 pagesPolygala TenuifoliaTuấn Nguyen AnhNo ratings yet
- Dopamine Receptor SignalingDocument42 pagesDopamine Receptor SignalingHir SavaNo ratings yet
- Redox Biology: John B. Hibbs JR., Zdenek Vavrin, James E. CoxDocument14 pagesRedox Biology: John B. Hibbs JR., Zdenek Vavrin, James E. CoxNidya Aryanda KNo ratings yet
- Zhao Et Al. - 2009 - Decreased TK Activity Contributes To Impaired Hippocampal Neurogenesis in TDDocument10 pagesZhao Et Al. - 2009 - Decreased TK Activity Contributes To Impaired Hippocampal Neurogenesis in TDmarej312No ratings yet
- An Electroporation Protocol For Efficient DNA Transfection in PC12 CellsDocument11 pagesAn Electroporation Protocol For Efficient DNA Transfection in PC12 CellsnaganathNo ratings yet
- Thesis Statement - Louis DavidDocument3 pagesThesis Statement - Louis DavidLoushitNo ratings yet
- BSI - Case Report Form Design IssuesDocument19 pagesBSI - Case Report Form Design IssuesKatti VenkataramanaNo ratings yet
- Provisional RestorationsDocument9 pagesProvisional RestorationsshivaprasadmNo ratings yet
- Sampleresponseletters PDFDocument4 pagesSampleresponseletters PDFlevanah87369No ratings yet
- HyperthermiaDocument2 pagesHyperthermiapamgee100% (11)
- Waterleau - Ebrochure Lucas - EngDocument10 pagesWaterleau - Ebrochure Lucas - EngAlaa SalemNo ratings yet
- Review ArticleDocument18 pagesReview Articlenasution hariNo ratings yet
- Assessment and Management of The Unconscious PatientDocument6 pagesAssessment and Management of The Unconscious PatientRed DevilNo ratings yet
- The Mind's Own Physician: A Scientific Dialogue With The Dalai Lama On The Healing Power of MeditationDocument20 pagesThe Mind's Own Physician: A Scientific Dialogue With The Dalai Lama On The Healing Power of MeditationNew Harbinger Publications75% (4)
- Country Paper IndiaDocument63 pagesCountry Paper IndiaShashank16No ratings yet
- CG252 2012-07 Common Ground MagazineDocument40 pagesCG252 2012-07 Common Ground MagazineCommonGroundBCNo ratings yet
- Dr. Ayushi Verma, BDS: Professtional SummaryDocument2 pagesDr. Ayushi Verma, BDS: Professtional SummaryAyushi VermaNo ratings yet
- PsycoanalyticDocument55 pagesPsycoanalyticAdarsh S MelparampilNo ratings yet
- SPGDT Hospital: DR I Ketut Wiargitha, SPB (K) Trauma, FinacsDocument68 pagesSPGDT Hospital: DR I Ketut Wiargitha, SPB (K) Trauma, FinacsOgizWaraNo ratings yet
- Osteotomy The BasicsDocument13 pagesOsteotomy The BasicsHari25885No ratings yet
- Suturing TechniquesDocument5 pagesSuturing TechniquesAndikaPurbaNo ratings yet
- Animal BitesDocument5 pagesAnimal BitesvyalylaNo ratings yet
- Goodman & Snyder: Differential Diagnosis For Physical Therapists, 5th EditionDocument2 pagesGoodman & Snyder: Differential Diagnosis For Physical Therapists, 5th EditionZainab WaqarNo ratings yet
- Allergy Skin TestsDocument6 pagesAllergy Skin TestsAnindya Putri KusumajatiNo ratings yet
- Careersguide Medical WritingDocument40 pagesCareersguide Medical Writingbeiza1979100% (1)
- Role Play DiareDocument7 pagesRole Play DiareNi Putu aristaNo ratings yet
- DiureticsDocument29 pagesDiureticsSaravanan RajagopalNo ratings yet
- Ultra Month 12Document8 pagesUltra Month 12Milton JuniorNo ratings yet
- Dual DiagnosisDocument4 pagesDual DiagnosisKaroll Martinez DiazNo ratings yet
- 01 Ultra Violet SterilizationDocument14 pages01 Ultra Violet SterilizationNur Sayyid UmarNo ratings yet
- CareplanDocument2 pagesCareplanapi-381090302No ratings yet
- Lysine: An Effective Adjunct Treatment For Herpes Simplex Virus OutbreaksDocument3 pagesLysine: An Effective Adjunct Treatment For Herpes Simplex Virus OutbreaksHerpesSimplexVirus100% (9)
- Public Health Needs Assessment Profile and Health Promotion Proposal by Theresa Lowry Lehnen Specialist Nurse Practitioner in Conjunction With Surrey University 2005Document46 pagesPublic Health Needs Assessment Profile and Health Promotion Proposal by Theresa Lowry Lehnen Specialist Nurse Practitioner in Conjunction With Surrey University 2005Theresa Lowry-LehnenNo ratings yet
- NCP Activity NavidasDocument2 pagesNCP Activity NavidasFran LanNo ratings yet