Professional Documents
Culture Documents
1
1
Uploaded by
Chethan KumarCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hayssen Training ElectricalDocument17 pagesHayssen Training ElectricalRoberto SanchezNo ratings yet
- Q3 G11 Physical Science Module 7Document19 pagesQ3 G11 Physical Science Module 7Lebz RicaramNo ratings yet
- Primarchs DatasheetsDocument24 pagesPrimarchs DatasheetsJosiah Young1100% (5)
- Selenium Interview Questions - CognizantDocument20 pagesSelenium Interview Questions - CognizantJessie SokhiNo ratings yet
- Ni Hms 467016Document163 pagesNi Hms 467016Chethan KumarNo ratings yet
- NAAC Guidelines For InstitutionsDocument4 pagesNAAC Guidelines For InstitutionsChethan KumarNo ratings yet
- SSC/ N 0501 Contribute To The Design of Software Products and ApplicationsDocument4 pagesSSC/ N 0501 Contribute To The Design of Software Products and ApplicationsChethan KumarNo ratings yet
- Chartreusis 5-095 and Its Inhibition Activity To RNA Helicase ofDocument6 pagesChartreusis 5-095 and Its Inhibition Activity To RNA Helicase ofChethan KumarNo ratings yet
- Rotational Dynamics: Points To RememberDocument9 pagesRotational Dynamics: Points To RememberJayashri Bhavsar 31No ratings yet
- Skills Test Unit 1 BDocument5 pagesSkills Test Unit 1 BOsama CanaanNo ratings yet
- 3 PBDocument11 pages3 PBSuci DwiNo ratings yet
- Peek - POLYETHER ETHER KETONEDocument58 pagesPeek - POLYETHER ETHER KETONEBryan Jesher Dela Cruz100% (1)
- Itcc Comm. Center Bms Io PGDocument3 pagesItcc Comm. Center Bms Io PGuddinnadeemNo ratings yet
- Mapping PEC 2021-Oct-20 Annex-D Courses Vs PLO Vs TaxonomyDocument2 pagesMapping PEC 2021-Oct-20 Annex-D Courses Vs PLO Vs TaxonomyEngr.Mohsin ShaikhNo ratings yet
- A 201Document1 pageA 201AnuranjanNo ratings yet
- Stamens PDFDocument10 pagesStamens PDFAmeya KannamwarNo ratings yet
- David RohlDocument3 pagesDavid RohlPhil CaudleNo ratings yet
- Freeplane User Guide PDFDocument31 pagesFreeplane User Guide PDFAlma_Valladare_719No ratings yet
- Scala AccesoriesDocument27 pagesScala AccesoriesZiggy BussyNo ratings yet
- Vitamin A & D: Chemistry, Biochemical Role, RDA & Deficiency DiseasesDocument20 pagesVitamin A & D: Chemistry, Biochemical Role, RDA & Deficiency DiseasesSELVI ANo ratings yet
- The EI SLP Therapy BundleDocument14 pagesThe EI SLP Therapy BundlelevyNo ratings yet
- Indonesian Sign Language Visualization Model (BISINDO) Website-Based Oral Health On Tooth Brushing Behavior in Deaf ChildrenDocument6 pagesIndonesian Sign Language Visualization Model (BISINDO) Website-Based Oral Health On Tooth Brushing Behavior in Deaf ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Kirk Summers Clinical Field Experience A Program Leader Interview Summary and ReflectionDocument4 pagesKirk Summers Clinical Field Experience A Program Leader Interview Summary and ReflectionKirk Summers100% (1)
- Detailed Report On Gwadar PortDocument4 pagesDetailed Report On Gwadar PortxeninNo ratings yet
- Chapter 11 Icse Midpoint TheoremDocument10 pagesChapter 11 Icse Midpoint TheoremDeepika MohanbabuNo ratings yet
- Crude Oil (Conversions)Document3 pagesCrude Oil (Conversions)Carolo DemoNo ratings yet
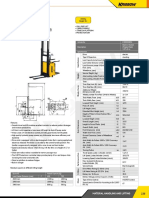
- Electric Stacker: Article No. KW0500894 Description Electric Stacker (Triplex Mast) 1.5T x3 M SpecificationDocument1 pageElectric Stacker: Article No. KW0500894 Description Electric Stacker (Triplex Mast) 1.5T x3 M SpecificationAsty RikyNo ratings yet
- Chapter 04Document37 pagesChapter 04BLESSEDNo ratings yet
- Glory To God Light From Light With LyricsDocument13 pagesGlory To God Light From Light With LyricsRodolfo DeriquitoNo ratings yet
- (THAAD) Five Failures and CountingDocument6 pages(THAAD) Five Failures and CountingGuilherme Da Silva CostaNo ratings yet
- MIET2407 - OENG1181 - Final Report 2018Document4 pagesMIET2407 - OENG1181 - Final Report 2018Trần TínNo ratings yet
- Advanced Management Accounting PDFDocument204 pagesAdvanced Management Accounting PDFptgo100% (1)
- Fxrate 06 06 2023Document2 pagesFxrate 06 06 2023ShohanNo ratings yet
- Gr11 Mock Exam Schedule 2024Document13 pagesGr11 Mock Exam Schedule 2024potrillo0330No ratings yet
1
1
Uploaded by
Chethan KumarOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1
1
Uploaded by
Chethan KumarCopyright:
Available Formats
Tokai J Exp Clin Med., Vol. 23, No. 3, pp.
147-151, 1998
Collagen production by Cultured Human Retinal Pigment Epithelial Cells
Kazuteru KIGASA 1), Hiroshi ISHIKA 1), Hajime OBAZA 1), WA WA WA Toshinari MINAMOTO2), Yutaka NAGAI2) and Yasuhiko TANAKA3)
1) Department of Ophthalmology, School of Medicine, Tokai University 2) Department of Tissue Physiology, Medical Research Institute, Tokyo Medical and Dental University 3) Department of Ophthalmology, School of Medicine, Keio University (Received April 30, 1998; Accepted May 11, 1998)
We investigated extracellular matrix produced by human retinal pigment epithelial cells (RPE) in vitro using electron microscopy and enzyme linked immunosorbent assay (ELISA). The thickness of the matrix under the cell layer was about 30 after 360 days of culture. It m consisted mainly of fibrous and granular components. Type IV and collagen were detected but type I and III were not detected by ELISA. It appeared that RPE can secrete type IV and V collagen and form a thick membrane which may cause proliferative vitreoretinopathy (PVR) by contraction. Control of RPE proliferation and secretion of extracellular matrix is indispensable for prevention of PVR. (Key words: collagen, human, proliferative vitreoretinopathy, retinal pigment epithelium)
INTRODUCTION The retinal pigment epithelium (RPE) is a single layer of cells around the outer circumference of the retina. The RPE cells play a vital role in providing anatomic, mechanical, and metabolic support for the photoreceptors and outer retina. Mitoses are extremely rare in adult cells, but they multiply and produce excessive amounts of extracellular matrix in certain pathological conditions. Proliferative vitreoretinopathy (PVR) is the most common cause of failure of rhegmatogenous retinal detachment surgery. PVR involves the uncontrolled proliferation of non-neoplastic cells capable of forming membranes, which may occur on either surface of the retina or along the detached surface of the vitreous gel. Contraction of these membranes creates tractional forces which can distort or detach the retina. Five major cellular constituents have been identified in vitreous and epiretinal membranes removed during vitrectomy : RPE cells, macrophages, fibroblast-like cells, fibrous astrocytes, and myofibroblast-like cells (3). The origin of these cells is controversial, but numerous
reports attribute the major role in PVR formation to RPE cells (2, 5, 7, 9, 15). A recent report (4) using immunohistochemical techniques stated that the membrane stroma was composed primarily of type I, II and III collagen and in discrete regions within the stroma, laminin, both heparan sulfate proteoglycans and type IV and V collagen were also present. The source of type I and III collagen was assumed to be fibroblast-like cells, glial cells, and RPE cells. Therefore, the role of extracellular matrix production by RPE cells is important in understanding the pathobiology of PVR. In this study we examined the extracellular matrix secreted by long-term cultured human RPE cells using electron microscopy and enzyme linked immunosorbent assay (ELISA) to clarify what kind of collagen was produced by the cells. MATERIALS AND METHODS Cell culture An eyeball was obtained from a 26-yearold male patient who underwent orbital excenteration secondary to a large facial hemangioma which had involved the right
Kazuteru KIGASAWA, Department of Ophthalmology, School of Medicine, Tokai University, Bohseidai, Isehara, Kanagawa 2591193 Japan
147
148 K. KIGASAWA et al.
orbit, resulting in blindness. The methods of RPE cell culture was described elsewhere (6). The harvested RPE cells were placed in 60mm plastic petri dishes (Corning ,NY, USA) containing 3 ml of Hams F12 medium supplemented with 16% fetal calf serum (GIBCO, Grand Island, NY, USA), 0.75% NaHCO3, penicillin (100 U/ml) and streptomycin (100 g/ml) (GIBCO). The medium was changed twice a week. Primary culture cells were incubated 360 days without passaging. Morphologic examination After 360 days of culture, the cells in the culture dish were used for morphologic examination. The cell layer with extracellular matrix was separated from the dish with forceps. The membrane was cut into two pieces with scissors. The first piece was fixed in buffered 10% formalin and embedded in paraffin for light microscopy. HematoxylinEosin, Mallory, PAS, Elastica and Alcianblue staining were performed. The second piece was fixed in 2% glutaraldehyde, postfixed in 1% osmium tetraoxide, dehydrated with graded ethanol and embedded in Epon for transmission electron microscopy. Ultrathin sections were stained with uranyl acetate and lead citrate and examined with a JEOL 100B transmission electron microscope (JEOL, Tokyo). Enzyme linked immunosorbent assay (ELISA) Another culture dish was used for preparation of collagens (11) and ELISA (14) as follows. The peeled membrane composed of the cell layer and the extracellular matrix was washed in cold 0.05M Tris-HCl buffer, pH 7.4, containing protease inhibitors (4 mM EDTA, 2 mM phenylmethylsulfonyl fluoride and 10 mM N-ethylmaleimide) and then homogenized. The homogenate was suspended in 0.5 M acetic acid and pepsin (Boehringer Mannheim, Manheim, Germany) was then added in an enzyme/substrate weight ratio of 1:40. The reaction mixture was stirred at 4 for 24 hours. The undigested residue was removed by centrifugation at 10,000 g for 1 hour and the supernatant was adjusted to 1.8 M NaCl by addition of crystalline NaCl to precipitate collagen. The solution was stirred for 24 hours at 4 and centrifuged for 1 hr at
100,000 g. The precipitate was dissolved in 0.15 M NaCl/0.05M Tris-HCl buffer, pH7.6, and 0.2 ml of a 20g/ml solution was dispensed into microtiter wells (Nunc-Immuno Plate II-96 U, Roskilde, Denmark) and incubated overnight at 4 . After washing with the same buffer, 0.2 ml of 1% BSA was added to each well and incubated for 1 hour at 37 for after coating. After washing with PBS-Tween, 0.2 ml of antibody solution (anti-human type I, III, IV and V collagen) (10) diluted at 1:10, 1:100, or 1:1000 with PBS-Tween-BSA was added to each well and incubated overnight at 4 . After washing with PBS-Tween, 0.2 ml of second antibody solution (alkaline-phosphatase labelled antirat IgG produced in rabbits) (DAKO, Copenhagen, Denmark) diluted to 1:500 with PBS-Tween was added and incubated for 1 hour at 37 . After washing with PBSTween, 0.15 ml of paranitrophenyl phosphate solution (5 mg/ 5 ml of 10% diethanol-amine buffer) (SIGMA, St. Louis, USA) was added to each well and incubated for 30 minutes at room temperature. The reaction was terminated by adding 0.1 ml of 3N NaOH, and the absorbance of the products of the enzyme reaction was measured at 405 nm. This study was carried out in accordance with the Declaration of Helsinki of the World Medical Association. RESULTS Light microscopic findings Primary culture cells retained epithelioid morphology even after 360 days of culture (Fig. 1). The membrane including the cell layer and extracellular matrix was separated from the dish easily with forceps (Fig. 2). The perpendicular sectional view of the membrane showed a monolayer of the cells and fibous materials under it. The fibrous extracellular matrix was stained positively with PAS and Alcian blue stain, and stained blue with Mallory stain, but was negative for Elastica stain. Electron microscopic findings The cultured RPE cells were flatter than those in vivo. Microvilli were seen on the free surface. Pigment granules, mitochondria and lysosomes were observed in the cytoplasm. The thickness of the extracellular matrix under the cell layer was about 30 m. It consisted of a fibrous component, granu-
Collagen Production by Retinal Pigment Epithelial Cells 149
Fig. 1 A phase contrast micrograph of longterm cultured RPE cells. There are large cells abundant in pigment granules and relatively small cells with few pigment granules.(original magnification 50)
Fig. 2 The membrane including cell layer and extracellular matrix is separated from the dish easily with forceps.
Fig. 3 (A) Electron micrographs of long-term cultured RPE cells and extracellular matrix. Cultured cells have microvilli on the free surface. Pigment granules, mitochondria and lysosomes are seen in the cytoplasm. The thickness of the extracellular matrix under the cell layer is about 30 It consists of fibrous compom. nents, granular material and fragments of the cells.(bar5
Fig. 3 (B) Electron micrographs of long-term cultured RPE cells and extracellular matrix. Basal infolding of the cells and basal lamina are observed.(bar1 m)
150 K. KIGASAWA et al.
Table 1 ELISA Results dilution antibody anti-type anti-type anti-type anti-type I III IV V 1:10 0.078 0.072 0.340 0.627 1:100 0.033 0.056 0.279 0.508 1:1000 0.035 0.043 0.238 0.397
(Absorbance : 405nm)
Fig. 3 (C) Electron micrographs of long-term cultured RPE cells and extracellular matrix. The maximum diameter of the fibrils in the extracellular matrix is 30 nm and they have an indistinct banded pattern. They form bundles and pass through the granular matrix at random.(bar1 m)
lar material and fragments of the cells (Fig. 3-A). Basal infolding and basal lamina were recognized (Fig. 3-B). The maximum diameter of the fibrils in the extracellular matrix was about 30 nm and they had an indistinct banded pattern. They formed bundles and passed through the granular matrix at random (Fig. 3-C). ELISA As show in Table 1, dilution-dependent positive reactions were observed with type IV and V collagen. With type I and III collagen, the reactions were very low in background levels (0.020.09). Therefore the major types of collagen produced by cultured human RPE in this study were type IV and V, and type I and III were very minor components or not secreted. DISCUSSION There are several reports on collagen production by cultured RPE. Newsome and Kenyon (12) reported that cultured RPE of the chick embryo produced basement-mem-
brane material and striated collagen fibrils as extracellular deposits beneath the basal surface of the cells. The fibrils were oriented randomly and had a diameter of 15-45 nm. Although longitudinal macroperiodicity was not clearly discernible in fibrils of small diameter, a definite macroperiod ranging from 55 to 60 nm could be found in larger fibers. These extracellular deposits were not examined biochemically in the report. Li et al. (8) noted that feline RPE produced an extracellular matrix in vitro which was located between the basal surface of the RPE and the culture plate. The matrix had three morphological components: bundles, granules and fibrils. Basal membrane formation was not evident. The bundles exhibited a macroperiodicity of 11823 nm. Some of the fibrils showed a periodicity but a periodic band pattern of about 67 nm which is usually seen in interstitial collagen fibrils was not observed. Type IV collagen was detected biochemically but type I collagen was not detected. Campochiaro et al. (1) reported that human cultured RPE was found to produce collagen types I, II, III, and IV, but not type V using immunohistochemical staining techniques. Newsome et al. (13) reported using the same technique that cultured RPE of humans and monkeys produced collagen types I, III, IV and V, but not type II. In our study, a basal lamina, a fibrous component and a granular component were produced by lomg-term cultured human RPE. The maximum diameter of the fibrils was about 30 nm and they had an indistinct banded pattern. With ELISA, type IV and V collagen were detected but type I and III were not apparent. There are some discrepancies among these results in morphological and biochemical findings, probably due to differences in culture conditions. RPE cells behave as an epithelial cell line under normal conditions, but under abnor-
Collagen Production by Retinal Pigment Epithelial Cells 151
mal conditions they may be transformed into mesenchymal cell-like cells. Many pathological reports on PVR note that fibrils are assumed to be synthesized by metaplastic RPE cells, but it is not clear what kind of cell synthesizes each extracellular matrix component in PVR membranes. In this study, it was found that cultured human RPE cells formed a thick membrane including a large number of fibrils and consisting of type IV and/or V collagen. This membrane may cause PVR by contraction. It is indispensable for prevention of PVR to control RPE proliferation and secretion of extracellular matrix.
REFERENCES 1) Campochiaro PA, Jerdan JA, Glaser BA: The extracellular matrix of human retinal pigment epithelial cells in vivo and its synthesis in vitro. Invest Ophthalmol Vis Sci 27: 1615-1621, 1986 2) Clarkson JG, Green WR, Massof D: A histopathological review of 168 cases of preretinal membrane. Am J Ophthalmol 84: 1-17, 1977 3) Glaser MG: Pathology of PVR. In Freeman HM, Tolentino FI (eds.): Proliferative Vitreoretinopathy (PVR). New York, Springer-Verlag, 1988, 12-21 pp. 4) Jerdan JA, Pepose JS, Glaser BM, et al: Proliferative vitreoretinopathy membranes. An immunohistochemical study. Ophthal-mology 96: 801-810, 1989 5) Kampik A, Kenyon kR, Michels RG, et al: Epiretinal and vitreous membranes: Comparative study of 56 cases. Arch Ophthalmol 99: 1445-1454, 1981 6) Kigasawa K, Soushi S, Tanaka Y, Obazawa H: Morphologic and chromosomal study of a human
7)
8)
9)
10)
11)
12)
13)
14)
15)
16)
retinal pigment epithelial cell line. Jap J Ophthalmol 38: 10-15, 1994 Laqua H, Machemer R: Clinical-pathological correlation in massive periretinal proliferation. Am J Ophthalmol 80 : 913-929, 1975 Li W, Stram LE, Agurre GD, Rocky JH: Extracellular matrix production by cat retinal pigment epithelium in vitro: Characterization of type IV collagen synthesis. Exp Eye Res 38: 291-304, 1984 Machemer R and Laqua H: Pigment epithelium proliferation in retinal detachment (massive periretinal proliferation). Am J Ophthalmol 80: 1-23, 1975 Minamoto T, Ooi A, Okada Y et al: Desmoplastic reaction of gastric carcinoma: A light- and electronmicroscopic immunohistochemical analysis using collagen type-specific antibodies. Human Pathology 19: 815-821, 1988 Miller EJ, Rhodes RK: Preparation and characterization of collagens. Methods in Enzymol 82: 33-64, 1982 Newsome DA, Kenyon KR: Collagen production in vitro by the retinal pigment epithelium of the chick embryo. Dev Viol 32: 387-400, 1973 Newsome DA, Pfeffer BA, Hassel JR, et al: Detection of extracellular matrix molecules synthesized in vitro by monkey and human retinal pigment epithelium: Infuluence of donor age and multiple passages. Exp Eye Res 46: 305-321, 1988 Rennard SI, Berg R, Martin GR et al: Enzyme-linked immunoassays (ELISA) for connective tissue components. Anal Biochem 104: 205-214, 1980 Smith RS, van Heuven WAJ, Streeten B: Vitreous membranes: A light and electron microscopical study. Arch Ophthalmol 95: 1556-1560, 1976 Wallow IHL, Miller SA: Preretinal membrane by retinal pigment epithelium. Arch Ophthalmol 96: 16431646, 1978
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hayssen Training ElectricalDocument17 pagesHayssen Training ElectricalRoberto SanchezNo ratings yet
- Q3 G11 Physical Science Module 7Document19 pagesQ3 G11 Physical Science Module 7Lebz RicaramNo ratings yet
- Primarchs DatasheetsDocument24 pagesPrimarchs DatasheetsJosiah Young1100% (5)
- Selenium Interview Questions - CognizantDocument20 pagesSelenium Interview Questions - CognizantJessie SokhiNo ratings yet
- Ni Hms 467016Document163 pagesNi Hms 467016Chethan KumarNo ratings yet
- NAAC Guidelines For InstitutionsDocument4 pagesNAAC Guidelines For InstitutionsChethan KumarNo ratings yet
- SSC/ N 0501 Contribute To The Design of Software Products and ApplicationsDocument4 pagesSSC/ N 0501 Contribute To The Design of Software Products and ApplicationsChethan KumarNo ratings yet
- Chartreusis 5-095 and Its Inhibition Activity To RNA Helicase ofDocument6 pagesChartreusis 5-095 and Its Inhibition Activity To RNA Helicase ofChethan KumarNo ratings yet
- Rotational Dynamics: Points To RememberDocument9 pagesRotational Dynamics: Points To RememberJayashri Bhavsar 31No ratings yet
- Skills Test Unit 1 BDocument5 pagesSkills Test Unit 1 BOsama CanaanNo ratings yet
- 3 PBDocument11 pages3 PBSuci DwiNo ratings yet
- Peek - POLYETHER ETHER KETONEDocument58 pagesPeek - POLYETHER ETHER KETONEBryan Jesher Dela Cruz100% (1)
- Itcc Comm. Center Bms Io PGDocument3 pagesItcc Comm. Center Bms Io PGuddinnadeemNo ratings yet
- Mapping PEC 2021-Oct-20 Annex-D Courses Vs PLO Vs TaxonomyDocument2 pagesMapping PEC 2021-Oct-20 Annex-D Courses Vs PLO Vs TaxonomyEngr.Mohsin ShaikhNo ratings yet
- A 201Document1 pageA 201AnuranjanNo ratings yet
- Stamens PDFDocument10 pagesStamens PDFAmeya KannamwarNo ratings yet
- David RohlDocument3 pagesDavid RohlPhil CaudleNo ratings yet
- Freeplane User Guide PDFDocument31 pagesFreeplane User Guide PDFAlma_Valladare_719No ratings yet
- Scala AccesoriesDocument27 pagesScala AccesoriesZiggy BussyNo ratings yet
- Vitamin A & D: Chemistry, Biochemical Role, RDA & Deficiency DiseasesDocument20 pagesVitamin A & D: Chemistry, Biochemical Role, RDA & Deficiency DiseasesSELVI ANo ratings yet
- The EI SLP Therapy BundleDocument14 pagesThe EI SLP Therapy BundlelevyNo ratings yet
- Indonesian Sign Language Visualization Model (BISINDO) Website-Based Oral Health On Tooth Brushing Behavior in Deaf ChildrenDocument6 pagesIndonesian Sign Language Visualization Model (BISINDO) Website-Based Oral Health On Tooth Brushing Behavior in Deaf ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Kirk Summers Clinical Field Experience A Program Leader Interview Summary and ReflectionDocument4 pagesKirk Summers Clinical Field Experience A Program Leader Interview Summary and ReflectionKirk Summers100% (1)
- Detailed Report On Gwadar PortDocument4 pagesDetailed Report On Gwadar PortxeninNo ratings yet
- Chapter 11 Icse Midpoint TheoremDocument10 pagesChapter 11 Icse Midpoint TheoremDeepika MohanbabuNo ratings yet
- Crude Oil (Conversions)Document3 pagesCrude Oil (Conversions)Carolo DemoNo ratings yet
- Electric Stacker: Article No. KW0500894 Description Electric Stacker (Triplex Mast) 1.5T x3 M SpecificationDocument1 pageElectric Stacker: Article No. KW0500894 Description Electric Stacker (Triplex Mast) 1.5T x3 M SpecificationAsty RikyNo ratings yet
- Chapter 04Document37 pagesChapter 04BLESSEDNo ratings yet
- Glory To God Light From Light With LyricsDocument13 pagesGlory To God Light From Light With LyricsRodolfo DeriquitoNo ratings yet
- (THAAD) Five Failures and CountingDocument6 pages(THAAD) Five Failures and CountingGuilherme Da Silva CostaNo ratings yet
- MIET2407 - OENG1181 - Final Report 2018Document4 pagesMIET2407 - OENG1181 - Final Report 2018Trần TínNo ratings yet
- Advanced Management Accounting PDFDocument204 pagesAdvanced Management Accounting PDFptgo100% (1)
- Fxrate 06 06 2023Document2 pagesFxrate 06 06 2023ShohanNo ratings yet
- Gr11 Mock Exam Schedule 2024Document13 pagesGr11 Mock Exam Schedule 2024potrillo0330No ratings yet