Professional Documents
Culture Documents
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Uploaded by
NafhyraJunetCopyright:
Available Formats
You might also like
- Ophthalmology-OSCE ReviewerDocument27 pagesOphthalmology-OSCE ReviewerGhia Villanueva Dijamco75% (4)
- Color Atlas and Synopsis of Clinical Ophthalmology - Retina 2012Document418 pagesColor Atlas and Synopsis of Clinical Ophthalmology - Retina 2012SALAH YOUNIS100% (1)
- Manual of Eye Emergencies Diagnosis and ManagementDocument221 pagesManual of Eye Emergencies Diagnosis and ManagementPhilip McNelson100% (2)
- Ocular AllergyDocument23 pagesOcular AllergyCecilia TorresNo ratings yet
- Clinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesDocument7 pagesClinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesRiza Haida WardhaniNo ratings yet
- Etiology of Proptosis in Children Sindhu 1998Document3 pagesEtiology of Proptosis in Children Sindhu 1998Putri Wulan SukmawatiNo ratings yet
- Jovr 6 3 192Document8 pagesJovr 6 3 192Felicia JesslynNo ratings yet
- BR J Ophthalmol 2005 BenEzra 444 8Document6 pagesBR J Ophthalmol 2005 BenEzra 444 8Gemilang KhusnurrokhmanNo ratings yet
- 9 Samuel EtalDocument4 pages9 Samuel EtaleditorijmrhsNo ratings yet
- Uveitis in Children and Adolescents: Extended ReportDocument5 pagesUveitis in Children and Adolescents: Extended ReportSelfima PratiwiNo ratings yet
- Eye Findings in Patients With Juvenile Dermatomyositis: Key Indexing TermsDocument6 pagesEye Findings in Patients With Juvenile Dermatomyositis: Key Indexing TermsOana BiancaNo ratings yet
- Childhood Glaucoma: An Overview: Parul Singh, Yogesh Kumar, Manoj Tyagi, Krishna Kuldeep, Parmeshwari Das SharmaDocument7 pagesChildhood Glaucoma: An Overview: Parul Singh, Yogesh Kumar, Manoj Tyagi, Krishna Kuldeep, Parmeshwari Das SharmaResa_G1A110068No ratings yet
- Phthisis Bulbi: Clinical and Pathologic Findings in RetinoblastomaDocument6 pagesPhthisis Bulbi: Clinical and Pathologic Findings in RetinoblastomaEstmar ValentinoNo ratings yet
- Javed and Kashif Split PDF 1674305144401Document4 pagesJaved and Kashif Split PDF 1674305144401criticseyeNo ratings yet
- Journal 3Document6 pagesJournal 3riskab123No ratings yet
- The New Zealand Medical JournalDocument7 pagesThe New Zealand Medical JournalNafhyraJunetNo ratings yet
- Jovr 6 3 192 PDFDocument7 pagesJovr 6 3 192 PDFShofura AzizahNo ratings yet
- Allergy: Vogt-Koyanagi-Harada Disease in An 8-Year-Old BoyDocument6 pagesAllergy: Vogt-Koyanagi-Harada Disease in An 8-Year-Old BoyErna HidayatNo ratings yet
- Retrospective Study of The Pattern of Eye Disorders Among Patients in Delta State University Teaching Hospital, OgharaDocument6 pagesRetrospective Study of The Pattern of Eye Disorders Among Patients in Delta State University Teaching Hospital, OgharaHello PtaiNo ratings yet
- Juvenile Myopia Progression, Risk Factors and Interventions: Pediatric Ophthalmology UpdateDocument5 pagesJuvenile Myopia Progression, Risk Factors and Interventions: Pediatric Ophthalmology UpdateZhakiAlAsrorNo ratings yet
- Congenital Glaucoma Epidemiological Clinical and Therapeutic Aspects About 414 EyesDocument5 pagesCongenital Glaucoma Epidemiological Clinical and Therapeutic Aspects About 414 Eyessiti rumaisaNo ratings yet
- Demography and Etiology of Congenital Cataract in A Tertiary Eye Centre of Kathmandu, NepalDocument8 pagesDemography and Etiology of Congenital Cataract in A Tertiary Eye Centre of Kathmandu, NepalasfwegereNo ratings yet
- Review: Ocular Toxoplasmosis II: Clinical Features, Pathology and ManagementDocument14 pagesReview: Ocular Toxoplasmosis II: Clinical Features, Pathology and Managementhidrisdmnk_747467972No ratings yet
- Jurnal MataDocument8 pagesJurnal MatamarinarizkiNo ratings yet
- PIIS1939455119301723Document5 pagesPIIS1939455119301723Yeol LoeyNo ratings yet
- Neonatal Cataract: Aetiology, Pathogenesis and ManagementDocument13 pagesNeonatal Cataract: Aetiology, Pathogenesis and ManagementLorenaNo ratings yet
- Conjunctivitis: Susana A. Alfonso,, Jonie D. Fawley,, Xiaoqin Alexa LuDocument21 pagesConjunctivitis: Susana A. Alfonso,, Jonie D. Fawley,, Xiaoqin Alexa LuMichi TristeNo ratings yet
- Dry Eye - WordDocument39 pagesDry Eye - WordJan IrishNo ratings yet
- IndianJPaediatrDermatol16142-3658051 100940Document3 pagesIndianJPaediatrDermatol16142-3658051 100940Fhie Fha RaraNo ratings yet
- Pediatrics 2008 Krakowski 812 24Document15 pagesPediatrics 2008 Krakowski 812 24Taqwa NindaNo ratings yet
- Atopicdermatitisisabarrier Issue, Notanallergyissue: Monica T. Kraft,, Benjamin T. PrinceDocument13 pagesAtopicdermatitisisabarrier Issue, Notanallergyissue: Monica T. Kraft,, Benjamin T. PrinceJesus MoralesNo ratings yet
- Jurnal 3Document6 pagesJurnal 3Adrianus NyomanNo ratings yet
- 10.1038@s41572 020 00231 4Document20 pages10.1038@s41572 020 00231 4Rasty AndrastyNo ratings yet
- Allergic ConjunctivitisDocument16 pagesAllergic ConjunctivitisJose Antonio Fuentes VegaNo ratings yet
- Dhaiban 2021Document7 pagesDhaiban 2021Eric PavónNo ratings yet
- Rematoid AtritisDocument9 pagesRematoid AtritisNovelis TriwikarnoNo ratings yet
- Perilimbal Conjunctival Pigmentation in Chinese Patients With Vernal KeratoconjunctivitisDocument4 pagesPerilimbal Conjunctival Pigmentation in Chinese Patients With Vernal KeratoconjunctivitisDwi HardiyantiNo ratings yet
- Steriod Cataract PDFDocument4 pagesSteriod Cataract PDFLisa IskandarNo ratings yet
- 34tupe EtalDocument5 pages34tupe EtaleditorijmrhsNo ratings yet
- Cong GlaucomaDocument20 pagesCong GlaucomapratikandpNo ratings yet
- Ankyloblepharon Filiforme Adnatum: A Case ReportDocument4 pagesAnkyloblepharon Filiforme Adnatum: A Case ReportGheavita Chandra DewiNo ratings yet
- Clinical and Laboratory Study of Ocular Rosacea in Northern GreeceDocument5 pagesClinical and Laboratory Study of Ocular Rosacea in Northern GreeceBambang AdiNo ratings yet
- ButajiraDocument6 pagesButajirahenok birukNo ratings yet
- Jurnal MataDocument7 pagesJurnal MatatrianaamaliaNo ratings yet
- Diagnosis of HyperIgE Syndromes HIES On Black Phenotype Patients With Atopic Dermatitis Followed in Dakar SenegalDocument10 pagesDiagnosis of HyperIgE Syndromes HIES On Black Phenotype Patients With Atopic Dermatitis Followed in Dakar SenegalAthenaeum Scientific PublishersNo ratings yet
- Ophthalmological Findings in Children With EncephalitisDocument8 pagesOphthalmological Findings in Children With EncephalitisSabila TasyakurNo ratings yet
- JournalDocument20 pagesJournalBetrix MelindaNo ratings yet
- 2014 Article 6Document12 pages2014 Article 6RizkiNo ratings yet
- Atopic Dermatitis: Skin-Directed Management: Clinical ReportDocument12 pagesAtopic Dermatitis: Skin-Directed Management: Clinical ReportDenia Haritsa AprilianiNo ratings yet
- En Editorial 1Document2 pagesEn Editorial 1Suci FirmanNo ratings yet
- Demographic and Clinical Characteristics of Patients With Glaucoma in A Tertiary Eye Facility in GhanaDocument6 pagesDemographic and Clinical Characteristics of Patients With Glaucoma in A Tertiary Eye Facility in GhanaAldhi Putra PradanaNo ratings yet
- Javadneg A 10 28 4 63c47c3 PDFDocument18 pagesJavadneg A 10 28 4 63c47c3 PDFLhia PrisciliiaNo ratings yet
- Neonatal Cataract: Aetiology, Pathogenesis and ManagementDocument13 pagesNeonatal Cataract: Aetiology, Pathogenesis and ManagementSonyaSellyHNo ratings yet
- Ophthalmic Physiologic Optic - 2020 - Brandt - Impaired Visual Acuity Caused by Uncorrected Refractive Errors and AmblyopiaDocument11 pagesOphthalmic Physiologic Optic - 2020 - Brandt - Impaired Visual Acuity Caused by Uncorrected Refractive Errors and Amblyopia2017079621No ratings yet
- Intraocular Lenses and Clinical Treatment in Paediatric CataractDocument5 pagesIntraocular Lenses and Clinical Treatment in Paediatric CataractLinna LetoNo ratings yet
- Atopic Dermatitis in Infants and Children in IndiaDocument11 pagesAtopic Dermatitis in Infants and Children in IndiaMaris JessicaNo ratings yet
- Endogenous Endophthalmitis: A 9-Year Retrospective Study at A Tertiary Referral Hospital in MalaysiaDocument17 pagesEndogenous Endophthalmitis: A 9-Year Retrospective Study at A Tertiary Referral Hospital in MalaysiaWahyudi Bambang SukocoNo ratings yet
- Allergic Conjunctivitis in NigeriaDocument5 pagesAllergic Conjunctivitis in NigeriaStephen OguntoyeNo ratings yet
- An Objective Approach To DED Severity Sullivan Et Al IOVS 12-2010Document6 pagesAn Objective Approach To DED Severity Sullivan Et Al IOVS 12-2010Meyva HannaNo ratings yet
- Associations of Anisometropia With Unilateral Amblyopia, Interocular Acuity Difference, and Stereoacuity in PreschoolersDocument9 pagesAssociations of Anisometropia With Unilateral Amblyopia, Interocular Acuity Difference, and Stereoacuity in PreschoolersCalvin NugrahaNo ratings yet
- Eye Infections PDFDocument10 pagesEye Infections PDFDara Agusti MaulidyaNo ratings yet
- Epidemiologia Miopia UsaDocument7 pagesEpidemiologia Miopia Usabrenda elielNo ratings yet
- Lapsus MufidahDocument19 pagesLapsus MufidahNafhyraJunetNo ratings yet
- Lapsus MufidahDocument19 pagesLapsus MufidahNafhyraJunetNo ratings yet
- Column1: Komp Masuk Keluar Tarif KetDocument9 pagesColumn1: Komp Masuk Keluar Tarif KetNafhyraJunetNo ratings yet
- The New Zealand Medical JournalDocument7 pagesThe New Zealand Medical JournalNafhyraJunetNo ratings yet
- The Clinical Significance of Perilimbal Conjunctival Pigmentation in Vernal ConjunctivitisDocument4 pagesThe Clinical Significance of Perilimbal Conjunctival Pigmentation in Vernal ConjunctivitisNafhyraJunetNo ratings yet
- 11-Review On Some Plants of Indian Traditional Medicine WithDocument21 pages11-Review On Some Plants of Indian Traditional Medicine WithNafhyraJunetNo ratings yet
- Research TraditionDocument52 pagesResearch TraditionNafhyraJunetNo ratings yet
- Uveitis: Anatomy Classification Clinical Features TreatmentDocument10 pagesUveitis: Anatomy Classification Clinical Features Treatmenthenok birukNo ratings yet
- Navya Krishna-National Programme For Control of BlindnessDocument41 pagesNavya Krishna-National Programme For Control of BlindnessAnmol KudalNo ratings yet
- Mehrdad Mohammadpour MD Resume: OphthalmologyDocument15 pagesMehrdad Mohammadpour MD Resume: OphthalmologyHamed NazariNo ratings yet
- Funduscopy of Retinal PathologiesDocument4 pagesFunduscopy of Retinal PathologiesAvinindita Nura LestariNo ratings yet
- Exotropia in AdultsDocument3 pagesExotropia in AdultsTlati AmineNo ratings yet
- Strabismus 10Document25 pagesStrabismus 10william williamNo ratings yet
- Hubungan Tingkat Pengetahuan Dengan Upaya Pencegahan Penyakit Glaukoma Pada Klien Berisiko Di Wilayah Kerja Puskesmas Jenggawah Kabupaten Jember (Correlation Between Knowledge Level and Prevention ofDocument7 pagesHubungan Tingkat Pengetahuan Dengan Upaya Pencegahan Penyakit Glaukoma Pada Klien Berisiko Di Wilayah Kerja Puskesmas Jenggawah Kabupaten Jember (Correlation Between Knowledge Level and Prevention ofSri WidyaNo ratings yet
- Color BlindnessDocument3 pagesColor BlindnessRainZZaKNo ratings yet
- LeukocoriaDocument5 pagesLeukocoriabahaashakirNo ratings yet
- Metabolic and Complicated Cataract: DR - Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, RishikeshDocument31 pagesMetabolic and Complicated Cataract: DR - Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, Rishikeshsai shantanu100% (1)
- 17corneal DystrophiesDocument15 pages17corneal Dystrophies2begeniusNo ratings yet
- Morning Report MataDocument14 pagesMorning Report MataYoungky PutraNo ratings yet
- Differential Diagnosis: Hallows Around LightDocument10 pagesDifferential Diagnosis: Hallows Around LightfeedodeedoNo ratings yet
- Understanding Strabismus PDFDocument143 pagesUnderstanding Strabismus PDFhenok birukNo ratings yet
- 9 Retinal DetachmentDocument6 pages9 Retinal DetachmentNinin Erdininsih ArNo ratings yet
- OpthalDocument15 pagesOpthalWaiwit KritayakiranaNo ratings yet
- Eye ExaminationDocument9 pagesEye ExaminationFilbert KunardiNo ratings yet
- Emteaz OphthalmologyDocument16 pagesEmteaz OphthalmologyRaouf Ra'fat SolimanNo ratings yet
- Icd X BayiDocument11 pagesIcd X BayiArifin YusufNo ratings yet
- White Dot Syndromes: Presented by Yasmine Sameh El Sharnouby Ophthalmology SpecialistDocument43 pagesWhite Dot Syndromes: Presented by Yasmine Sameh El Sharnouby Ophthalmology SpecialistJasmine MinoNo ratings yet
- 1.2 Asst EngineerDocument21 pages1.2 Asst Engineercoep05No ratings yet
- Referensi 9 PDFDocument4 pagesReferensi 9 PDFDzulkifli SukriNo ratings yet
- Dispensing AnisometropiaDocument28 pagesDispensing Anisometropiahenok biruk100% (2)
- A Consideration of Binocular Parameters in The Spectacle PDFDocument5 pagesA Consideration of Binocular Parameters in The Spectacle PDFPierre A. RodulfoNo ratings yet
- ReferatDocument14 pagesReferatJeanne d'Arc DyanchanaNo ratings yet
- Eidon - Atlas Catalog WebDocument51 pagesEidon - Atlas Catalog Webefze71No ratings yet
- Strabismus Quick GuideDocument4 pagesStrabismus Quick Guideghitza80100% (1)
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Uploaded by
NafhyraJunetOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Uploaded by
NafhyraJunetCopyright:
Available Formats
Original Article
Allergic Conjunctivitis at Sheikh Zayed Regional Eye Care Center, Gambia
Patricia D Wade, MD, FMCOph; Anthonia N Iwuora, MD, FMCOph, FWASC; Laritza Lopez, DO; Mustapha A Muhammad, DO
Sheikh Zayed Regional Eye Care Center, Gambia
Purpose: To assess the prevalence of allergic conjunctivitis in Gambia and to determine its epidemiologic features, seasonal variations and associated ocular and systemic conditions. Methods: Records of patients clinically diagnosed with allergic conjunctivitis between April 2007 and March 2008 were reviewed. Variables including age, sex, date of presentation, and systemic and ocular findings were recorded. Results: A total of 7,912 patients were visited within the study period, out of which 624 (7.9%) were diagnosed with allergic conjunctivitis. The disease was equally distributed in male and female subjects, with high preponderance in children (54.5%). Most patients (60.7%) presented during the dry season as compared to the rainy season. Refractive error was the most common ocular condition associated with the condition present in 7.4% of patients while the most common systemic association was asthma, reported in 1.4% of cases. Conclusion: Allergic conjunctivitis in Gambia is more common in children than in adults and has seasonal variation with more patients presenting during dry seasons. Refractive errors are the most common ocular problem associated with the disease and asthma is a systemic association.
Keywords: Prevalence; Allergy; Conjunctivitis J Ophthalmic Vis Res 2012; 7 (1): 24-28. Correspondence to: Patricia D Wade, MD, FMCOph. Sheikh Zayed Regional Eye Care Center, Kanifing Layout, Banjul, Gambia, West Africa; Tel: +23 48037 053350; e-mail: delsatpwade@yahoo.com Received: February 26, 2011 Accepted: July 27, 2011
INTRODUCTION Allergic conjunctivitis refers to a group of disorders affecting the ocular surface usually associ ated w i t h t y p e 1 h y p ersen si t i v i t y reactions.1,2 It comprises a spectrum of disorders from non-sight threatening conditions such as seasonal allergic conjunctivitis (SAC), p e r e n n i a l a l l e r g i c co n j u n ct i v i t i s ( P A C ) , giant papillary conjunctivitis (GPC), to less common but sight threatening diseases such as vernal keratoconjunctivitis (VKC), and atopic keratoconjunctivitis (AKC).3 Along with
an IgE mediated reaction, complex chronic inflammation is involved in the pathogenesis of many ocular allergies.4 Allergic conjunctivitis is a typically mast cell mediated hypersensitivity reaction. Exposure of sensitized, IgE coated mast cells to airborne allergens is the primary irritating stimulus. Chain reactions in the plasma membrane of mast cells lead to membrane rupture and extrusion of the contents of the cell into surrounding tissues. These contents act as mediators and together with many other cell mediators stimulate the proliferation of fibroblasts and recruitment of various cell
24
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2012; Vol. 7, No. 1
Allergic Conjunctivitis in Gambia; Wade et al
types to the conjunctiva, all of which result in development of papillae as seen in patients with vernal keratoconjunctivitis. 5 Topical antihistamines have been employed for many years to provide fast relief for patients. These include mast cell stabilizers such as sodium cromoglicate, nedocromil and lodoxamide which also have anti-inflammatory effects.6 Allergic conjunctivitis has a global distribution with a widely varying incidence. It is less common in Northern Europe and North America, but more common in Africa, Mediterranean countries, Central and South America and in the Indian subcontinent.7 METHODS This retrospective study was conducted at Sheikh Zayed Regional Eye Care Center and was approved by the ethical committee of this institution. This center is the only tertiary eye care facility in Gambia overseeing the activities of seven secondary centers from where patients are referred. Patients may also come directly to the center without referral. Records of patients visited from April 2007 to March 2008 and diagnosed with allergic conjunctivitis were retrieved for the purpose of the study. Follow-up cases were not included in the study. Patient information including age, sex and address were recorded. Other data included
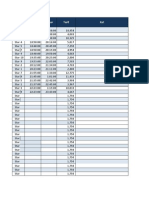
presenting complaints and their duration, drug and family history, and previous allergies or history of asthma. Findings on slit lamp and fundus examination were noted. Patients with tarsal papillae, pigmented conjunctiva, limbal papillae associated with follicles, conjunctival scarring, trichiasis or corneal scarring were diagnosed with allergic conjunctivitis concomitant with trachoma. Obtained information was recorded into data sheets and entered into Epi-info software version 3.0. Frequency values were tested using the Chi-square test. Significance level was set at 0.05. RESULTS A total of 1,248 eyes of 624 patients were diagnosed with allergic conjunctivitis within the study period. Figure 1 shows the age and gender distribution; 340 patients (54.5%) were children aged 0-15 years. The child to adult ratio was 1:1.2 (P=0.002). There were 296 (47.4%) male and 328 (52%) female subjects with 1:1.1 female/male ratio reflecting no statistically significant difference by gender (P=0.07). Figure 2 demonstrates the ocular associations of allergic conjunctivitis. Refractive errors were present in 92 (7.4%) eyes while trachoma was diagnosed in 16 (1.3%) eyes. Corneal opacities were present in 14 (1.1%) eyes and cataracts were
Figure 1. Age-sex distribution of cases
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2012; Vol. 7, No. 1
25
Allergic Conjunctivitis in Gambia; Wade et al
Figure 2. Concomitant ocular conditions
observed in 12 (1.0%) eyes; 11 eyes (0.9%) had keratoconus while 7 eyes (0.6%) had pinguecula. Pterygia were noted in 6 (0.5%) eyes while chalazia and ptosis were present in 2 eyes (0.2%) each. Stye and glaucoma were diagnosed in one eye (0.1%) each. Figure 3, shows the monthly distribution of
cases; 379 patients (60.7%) were visited during the dry season, November to May, while 245 patients (39.3%) were seen during the rainy season, June to October, providing a ratio of 1:1.5 (P=0.01). Table 1, shows patients with concomitant systemic diseases. Some patients had other
Figure 3. Monthly distribution of cases
26
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2012; Vol. 7, No. 1
Allergic Conjunctivitis in Gambia; Wade et al
Table 1. Patients diagnosed with systemic diseases
Systemic diseases Asthma Atopic dermatitis Epilepsy Hypertension Diabetes Number 9 1 1 1 1 Percent 1.4 0.2 0.2 0.2 0.2
systemic disorders that may or may not be associated with allergic conjunctivitis. Nine patients (1.4%) were asthmatic, while atopic dermatitis, epilepsy, hypertension and diabetes mellitus were diagnosed in one patient (0.2%) each. DISCUSSION Allergic conjunctivitis is one of the most common ocular conditions encountered by pediatricians, internists, and family practitioners. 8-10 Of the 7,912 patients visited within the study period, 624 (7.9%) were diagnosed with various forms of ocular allergies making it one of the most common disorders at our clinic. Although more female subjects were seen with allergy, the gender difference failed to reach statistical significance. This is in line with a similar study performed by Uchio et al who reported female predominance11 in ocular allergy but in contrast to the study by Marback et al in which male preponderance was observed.12 Gambia has a sandy environment. Children playing outdoors in the sand use their dusty hands to wipe their eyes, introducing foreign substances which affect the conjunctiva, resulting in allergic conjunctivitis.13 Allergic conjunctivitis has been noted as one of the most frequent reasons for a child visiting an ophthalmologist.14 Gambia has a subtropical climate with distinct cold and hot seasons. From November to May the weather is cold, dry and dusty while the rainy season is from June to October. The majority of patients (60.7%) with allergic conjunctivitis were seen during the dry season, while 39.3% were seen during the rainy season; a finding which can be attributed to the presence of dust and pollen in the air during the dry seasons. The diagnosis of allergic conjunctivitis at
this center was similar to other eye centers in African countries, i.e. by meticulous questioning, emphasizing on the existence of ocular itching and looking for tarsal papillae, follicles and conjunctival pigmentation.16 We lacked facilities for specific IgE and skin tests as recommended in other studies.9,13 There were other ocular conditions coexisting with allergic conjunctivitis; refractive errors were found to be the most common. Mimura et al17 in their study on the relationship between refractive errors and allergic conjunctivitis noted a significant number of allergic conjunctivitis patients with refractive errors (22.1%) and concluded that refractive error may be a risk factor for allergic conjunctivitis. Another coexisting condition was trachoma. Based on the 1987 national survey in Gambia, trachoma was one of the leading causes of treatable and avoidable blindness in the country, accounting for 17% of cases. With adequate intervention, the disease has now been reduced to less than 5% in endemic communities. Few cases of trachoma are sometimes seen concomitant with allergic conjunctivitis as in the present study. This confirms the study of Bezerra et al18 in Brazil in which in about 5.8% of cases, trachoma coexisted with allergic conjunctivitis. The use of traditional medicines is quite common in our community as in most other African settings. Harmful eye medications are known to cause irreversible damage to the cornea; 1.1% of our cases were diagnosed with corneal opacities. It is unknown if these opacities were due to traditional eye remedies or because patients with vernal conjunctivitis may also develop central corneal changes known as vernal plaques. These plaques consist of mucin and epithelial cells and can cause scarring and visual loss. 8 Videokeratography is a useful technique in detecting mild keratoconus, which is a complication of vernal keratoconjunctivitis. In the absence of videokeratography, patients in our study were diagnosed clinically; thereby mild cases were missed. This accounts for a low prevalence (0.9%) of the condition in our series as compared to the study by Totan et al19 in which a complementary device was used for diagnosis and reported a prevalence of 26.8% for keratoconus.
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2012; Vol. 7, No. 1
27
Allergic Conjunctivitis in Gambia; Wade et al
Allergic conjunctivitis is a frequent disorder and often associated with other manifestations of atopy such as rhinitis or asthma.20 In a study on children with allergic conjunctivitis at an outpatient clinic in Denmark, 24% were found to have asthma concomitant with allergic conjunctivitis while 30% had eczema and 42% had rhinitis.21 In our study 1.4% of cases had asthma while only 0.2% had atopic dermatitis. No patient was diagnosed with rhinitis which seems to be a more common association with allergic conjunctivitis. It can be concluded that there is a need to ask patients or look for associated conditions for quick intervention so patients can be managed with other specialties. This may reduce frequent clinic visits and avoid seeking alternative treatment. Conflicts of Interest None. REFERENCES
1. Ono SJ, Abelson MB. Allergic conjunctivitis: update on pathophysiology and prospects for future treatment. J Allergy Clin Immunol 2005;115:118-122. 2. Zepeda Otega B, Rosas Vargas MA, Ito Tsuchiya FM, del Rio Navarro BE, Sienra Monge JJ. Allergic conjunctivitis in children. Rev Alerg Mex 2007;54:4153. 3. Fonacier L, Luchs J, Udell I. Ocular allergies. Curr Allergy Asthma Rep 2001;1:389-396. 4. Messmer EM. Ocular allergies. Ophthalmologe 2005;102:527-543. 5. Dutta LC, Dutta NK. Allergic conjunctivitis and allied conditions. In: Dutta LC (ed). Modern Ophthalmology. 3rd ed. New Delhi: Jaypee Brothers; 2005: 90-98. 6. Bielory L, Lien KW, Bigelsen S. Efficacy and tolerability of newer antihistamines in the treatment of allergic conjunctivitis. Drugs 2005;65:215-228. 7. Medi K. The clinical picture of vernal keratoconjunctivitis in Uganda. Community Eye Health 2001;14:66-67.
8. Friedlaender M. Overview of ocular allergy treatment. Curr Allergy Asthma Rep 2001;1:375-379. 9. Martn A, Gomez Demel E, Gagliardi J, Berra A, Mariani AL, Baena Cagnani CE, et al. Clinical signs and symptoms are not enough for correct diagnosis of allergic conjunctivitis. J Investig Allergol Clin Immunol 2003;13:232-237. 10. Marmouz F, Raffard M. Allergic conjunctivitis: diagnosis and treatment. Eur Ann Allergy Clin Immunol 2004;36:25-29. 11. Uchio E, Kimura R, Migita H, Kozawa M, Kadonoso K. Demographic aspects of allergic ocular disease and evaluation of new criteria for clinical assessment of ocular allergy. Graefes Arch Clin Exp Ophthalmol 2008;246:291-296. 12. Marback PM, de Freitas D, Paranhos Junior A, Belfort Junior R. Epidemiology and clinical features of allergic conjunctivitis in a reference center. Arq Bras Oftalmol 2007;70:312-316. 13. Del Rio-Navarro BE, Sienna-Monge JJ, Castellanos A, Williams-Gotti MJ. Allergic conjunctivitis. Bol Med Hosp Infant Mex 1992;49:201-204. 14. Fauquert JL. Childhood allergic conjunctivitis: the allergists point of view. J Fr Ophthalmol 2007;30:292299. 15. http://www.africanguide.com/country/gambia/ info.htm(Accessed 26th/02/2010). 16. Ndoye PA, Ba EA, Wane AM, Sow A, Ndiaye MR, Wade A. A systematic approach to the diagnosis and treatment of allergic conjunctivitis. Dakar Med 2007;52:13-16. 17. Mimura T, Mimura Y, Arimoto A, Amano S, Yamagmi S, Funatsu H, et al. Relationship between refraction and allergic conjunctivitis. Eye (Lond) 2009;23:63-66. 18. Bezerra Hde L, Santos GI. Trachoma in patients with allergic conjunctivitis. Arq Bras Oftalmol 2010;73:235239. 19. Totan Y, Hepen IF, Ceki O, Gndz A, Aydin E. Incidence of Keratoconus in subjects with vernal keratoconjunctivitis: a videokeratographic study. Ophthalmology 2001;108:824-827. 20. Creuzot-Garcher C. Different clinical forms of conjunctival allergy. J Fr Ophtalmol 2007;30:288-291. 21. Gradman J, Wolthers OD. Allergic conjunctivitis in children with asthma, rhinitis and eczema in a secondary outpatient clinic. Pediatr Allergy Immunol 2006;17:524-526.
28
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2012; Vol. 7, No. 1
You might also like
- Ophthalmology-OSCE ReviewerDocument27 pagesOphthalmology-OSCE ReviewerGhia Villanueva Dijamco75% (4)
- Color Atlas and Synopsis of Clinical Ophthalmology - Retina 2012Document418 pagesColor Atlas and Synopsis of Clinical Ophthalmology - Retina 2012SALAH YOUNIS100% (1)
- Manual of Eye Emergencies Diagnosis and ManagementDocument221 pagesManual of Eye Emergencies Diagnosis and ManagementPhilip McNelson100% (2)
- Ocular AllergyDocument23 pagesOcular AllergyCecilia TorresNo ratings yet
- Clinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesDocument7 pagesClinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesRiza Haida WardhaniNo ratings yet
- Etiology of Proptosis in Children Sindhu 1998Document3 pagesEtiology of Proptosis in Children Sindhu 1998Putri Wulan SukmawatiNo ratings yet
- Jovr 6 3 192Document8 pagesJovr 6 3 192Felicia JesslynNo ratings yet
- BR J Ophthalmol 2005 BenEzra 444 8Document6 pagesBR J Ophthalmol 2005 BenEzra 444 8Gemilang KhusnurrokhmanNo ratings yet
- 9 Samuel EtalDocument4 pages9 Samuel EtaleditorijmrhsNo ratings yet
- Uveitis in Children and Adolescents: Extended ReportDocument5 pagesUveitis in Children and Adolescents: Extended ReportSelfima PratiwiNo ratings yet
- Eye Findings in Patients With Juvenile Dermatomyositis: Key Indexing TermsDocument6 pagesEye Findings in Patients With Juvenile Dermatomyositis: Key Indexing TermsOana BiancaNo ratings yet
- Childhood Glaucoma: An Overview: Parul Singh, Yogesh Kumar, Manoj Tyagi, Krishna Kuldeep, Parmeshwari Das SharmaDocument7 pagesChildhood Glaucoma: An Overview: Parul Singh, Yogesh Kumar, Manoj Tyagi, Krishna Kuldeep, Parmeshwari Das SharmaResa_G1A110068No ratings yet
- Phthisis Bulbi: Clinical and Pathologic Findings in RetinoblastomaDocument6 pagesPhthisis Bulbi: Clinical and Pathologic Findings in RetinoblastomaEstmar ValentinoNo ratings yet
- Javed and Kashif Split PDF 1674305144401Document4 pagesJaved and Kashif Split PDF 1674305144401criticseyeNo ratings yet
- Journal 3Document6 pagesJournal 3riskab123No ratings yet
- The New Zealand Medical JournalDocument7 pagesThe New Zealand Medical JournalNafhyraJunetNo ratings yet
- Jovr 6 3 192 PDFDocument7 pagesJovr 6 3 192 PDFShofura AzizahNo ratings yet
- Allergy: Vogt-Koyanagi-Harada Disease in An 8-Year-Old BoyDocument6 pagesAllergy: Vogt-Koyanagi-Harada Disease in An 8-Year-Old BoyErna HidayatNo ratings yet
- Retrospective Study of The Pattern of Eye Disorders Among Patients in Delta State University Teaching Hospital, OgharaDocument6 pagesRetrospective Study of The Pattern of Eye Disorders Among Patients in Delta State University Teaching Hospital, OgharaHello PtaiNo ratings yet
- Juvenile Myopia Progression, Risk Factors and Interventions: Pediatric Ophthalmology UpdateDocument5 pagesJuvenile Myopia Progression, Risk Factors and Interventions: Pediatric Ophthalmology UpdateZhakiAlAsrorNo ratings yet
- Congenital Glaucoma Epidemiological Clinical and Therapeutic Aspects About 414 EyesDocument5 pagesCongenital Glaucoma Epidemiological Clinical and Therapeutic Aspects About 414 Eyessiti rumaisaNo ratings yet
- Demography and Etiology of Congenital Cataract in A Tertiary Eye Centre of Kathmandu, NepalDocument8 pagesDemography and Etiology of Congenital Cataract in A Tertiary Eye Centre of Kathmandu, NepalasfwegereNo ratings yet
- Review: Ocular Toxoplasmosis II: Clinical Features, Pathology and ManagementDocument14 pagesReview: Ocular Toxoplasmosis II: Clinical Features, Pathology and Managementhidrisdmnk_747467972No ratings yet
- Jurnal MataDocument8 pagesJurnal MatamarinarizkiNo ratings yet
- PIIS1939455119301723Document5 pagesPIIS1939455119301723Yeol LoeyNo ratings yet
- Neonatal Cataract: Aetiology, Pathogenesis and ManagementDocument13 pagesNeonatal Cataract: Aetiology, Pathogenesis and ManagementLorenaNo ratings yet
- Conjunctivitis: Susana A. Alfonso,, Jonie D. Fawley,, Xiaoqin Alexa LuDocument21 pagesConjunctivitis: Susana A. Alfonso,, Jonie D. Fawley,, Xiaoqin Alexa LuMichi TristeNo ratings yet
- Dry Eye - WordDocument39 pagesDry Eye - WordJan IrishNo ratings yet
- IndianJPaediatrDermatol16142-3658051 100940Document3 pagesIndianJPaediatrDermatol16142-3658051 100940Fhie Fha RaraNo ratings yet
- Pediatrics 2008 Krakowski 812 24Document15 pagesPediatrics 2008 Krakowski 812 24Taqwa NindaNo ratings yet
- Atopicdermatitisisabarrier Issue, Notanallergyissue: Monica T. Kraft,, Benjamin T. PrinceDocument13 pagesAtopicdermatitisisabarrier Issue, Notanallergyissue: Monica T. Kraft,, Benjamin T. PrinceJesus MoralesNo ratings yet
- Jurnal 3Document6 pagesJurnal 3Adrianus NyomanNo ratings yet
- 10.1038@s41572 020 00231 4Document20 pages10.1038@s41572 020 00231 4Rasty AndrastyNo ratings yet
- Allergic ConjunctivitisDocument16 pagesAllergic ConjunctivitisJose Antonio Fuentes VegaNo ratings yet
- Dhaiban 2021Document7 pagesDhaiban 2021Eric PavónNo ratings yet
- Rematoid AtritisDocument9 pagesRematoid AtritisNovelis TriwikarnoNo ratings yet
- Perilimbal Conjunctival Pigmentation in Chinese Patients With Vernal KeratoconjunctivitisDocument4 pagesPerilimbal Conjunctival Pigmentation in Chinese Patients With Vernal KeratoconjunctivitisDwi HardiyantiNo ratings yet
- Steriod Cataract PDFDocument4 pagesSteriod Cataract PDFLisa IskandarNo ratings yet
- 34tupe EtalDocument5 pages34tupe EtaleditorijmrhsNo ratings yet
- Cong GlaucomaDocument20 pagesCong GlaucomapratikandpNo ratings yet
- Ankyloblepharon Filiforme Adnatum: A Case ReportDocument4 pagesAnkyloblepharon Filiforme Adnatum: A Case ReportGheavita Chandra DewiNo ratings yet
- Clinical and Laboratory Study of Ocular Rosacea in Northern GreeceDocument5 pagesClinical and Laboratory Study of Ocular Rosacea in Northern GreeceBambang AdiNo ratings yet
- ButajiraDocument6 pagesButajirahenok birukNo ratings yet
- Jurnal MataDocument7 pagesJurnal MatatrianaamaliaNo ratings yet
- Diagnosis of HyperIgE Syndromes HIES On Black Phenotype Patients With Atopic Dermatitis Followed in Dakar SenegalDocument10 pagesDiagnosis of HyperIgE Syndromes HIES On Black Phenotype Patients With Atopic Dermatitis Followed in Dakar SenegalAthenaeum Scientific PublishersNo ratings yet
- Ophthalmological Findings in Children With EncephalitisDocument8 pagesOphthalmological Findings in Children With EncephalitisSabila TasyakurNo ratings yet
- JournalDocument20 pagesJournalBetrix MelindaNo ratings yet
- 2014 Article 6Document12 pages2014 Article 6RizkiNo ratings yet
- Atopic Dermatitis: Skin-Directed Management: Clinical ReportDocument12 pagesAtopic Dermatitis: Skin-Directed Management: Clinical ReportDenia Haritsa AprilianiNo ratings yet
- En Editorial 1Document2 pagesEn Editorial 1Suci FirmanNo ratings yet
- Demographic and Clinical Characteristics of Patients With Glaucoma in A Tertiary Eye Facility in GhanaDocument6 pagesDemographic and Clinical Characteristics of Patients With Glaucoma in A Tertiary Eye Facility in GhanaAldhi Putra PradanaNo ratings yet
- Javadneg A 10 28 4 63c47c3 PDFDocument18 pagesJavadneg A 10 28 4 63c47c3 PDFLhia PrisciliiaNo ratings yet
- Neonatal Cataract: Aetiology, Pathogenesis and ManagementDocument13 pagesNeonatal Cataract: Aetiology, Pathogenesis and ManagementSonyaSellyHNo ratings yet
- Ophthalmic Physiologic Optic - 2020 - Brandt - Impaired Visual Acuity Caused by Uncorrected Refractive Errors and AmblyopiaDocument11 pagesOphthalmic Physiologic Optic - 2020 - Brandt - Impaired Visual Acuity Caused by Uncorrected Refractive Errors and Amblyopia2017079621No ratings yet
- Intraocular Lenses and Clinical Treatment in Paediatric CataractDocument5 pagesIntraocular Lenses and Clinical Treatment in Paediatric CataractLinna LetoNo ratings yet
- Atopic Dermatitis in Infants and Children in IndiaDocument11 pagesAtopic Dermatitis in Infants and Children in IndiaMaris JessicaNo ratings yet
- Endogenous Endophthalmitis: A 9-Year Retrospective Study at A Tertiary Referral Hospital in MalaysiaDocument17 pagesEndogenous Endophthalmitis: A 9-Year Retrospective Study at A Tertiary Referral Hospital in MalaysiaWahyudi Bambang SukocoNo ratings yet
- Allergic Conjunctivitis in NigeriaDocument5 pagesAllergic Conjunctivitis in NigeriaStephen OguntoyeNo ratings yet
- An Objective Approach To DED Severity Sullivan Et Al IOVS 12-2010Document6 pagesAn Objective Approach To DED Severity Sullivan Et Al IOVS 12-2010Meyva HannaNo ratings yet
- Associations of Anisometropia With Unilateral Amblyopia, Interocular Acuity Difference, and Stereoacuity in PreschoolersDocument9 pagesAssociations of Anisometropia With Unilateral Amblyopia, Interocular Acuity Difference, and Stereoacuity in PreschoolersCalvin NugrahaNo ratings yet
- Eye Infections PDFDocument10 pagesEye Infections PDFDara Agusti MaulidyaNo ratings yet
- Epidemiologia Miopia UsaDocument7 pagesEpidemiologia Miopia Usabrenda elielNo ratings yet
- Lapsus MufidahDocument19 pagesLapsus MufidahNafhyraJunetNo ratings yet
- Lapsus MufidahDocument19 pagesLapsus MufidahNafhyraJunetNo ratings yet
- Column1: Komp Masuk Keluar Tarif KetDocument9 pagesColumn1: Komp Masuk Keluar Tarif KetNafhyraJunetNo ratings yet
- The New Zealand Medical JournalDocument7 pagesThe New Zealand Medical JournalNafhyraJunetNo ratings yet
- The Clinical Significance of Perilimbal Conjunctival Pigmentation in Vernal ConjunctivitisDocument4 pagesThe Clinical Significance of Perilimbal Conjunctival Pigmentation in Vernal ConjunctivitisNafhyraJunetNo ratings yet
- 11-Review On Some Plants of Indian Traditional Medicine WithDocument21 pages11-Review On Some Plants of Indian Traditional Medicine WithNafhyraJunetNo ratings yet
- Research TraditionDocument52 pagesResearch TraditionNafhyraJunetNo ratings yet
- Uveitis: Anatomy Classification Clinical Features TreatmentDocument10 pagesUveitis: Anatomy Classification Clinical Features Treatmenthenok birukNo ratings yet
- Navya Krishna-National Programme For Control of BlindnessDocument41 pagesNavya Krishna-National Programme For Control of BlindnessAnmol KudalNo ratings yet
- Mehrdad Mohammadpour MD Resume: OphthalmologyDocument15 pagesMehrdad Mohammadpour MD Resume: OphthalmologyHamed NazariNo ratings yet
- Funduscopy of Retinal PathologiesDocument4 pagesFunduscopy of Retinal PathologiesAvinindita Nura LestariNo ratings yet
- Exotropia in AdultsDocument3 pagesExotropia in AdultsTlati AmineNo ratings yet
- Strabismus 10Document25 pagesStrabismus 10william williamNo ratings yet
- Hubungan Tingkat Pengetahuan Dengan Upaya Pencegahan Penyakit Glaukoma Pada Klien Berisiko Di Wilayah Kerja Puskesmas Jenggawah Kabupaten Jember (Correlation Between Knowledge Level and Prevention ofDocument7 pagesHubungan Tingkat Pengetahuan Dengan Upaya Pencegahan Penyakit Glaukoma Pada Klien Berisiko Di Wilayah Kerja Puskesmas Jenggawah Kabupaten Jember (Correlation Between Knowledge Level and Prevention ofSri WidyaNo ratings yet
- Color BlindnessDocument3 pagesColor BlindnessRainZZaKNo ratings yet
- LeukocoriaDocument5 pagesLeukocoriabahaashakirNo ratings yet
- Metabolic and Complicated Cataract: DR - Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, RishikeshDocument31 pagesMetabolic and Complicated Cataract: DR - Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, Rishikeshsai shantanu100% (1)
- 17corneal DystrophiesDocument15 pages17corneal Dystrophies2begeniusNo ratings yet
- Morning Report MataDocument14 pagesMorning Report MataYoungky PutraNo ratings yet
- Differential Diagnosis: Hallows Around LightDocument10 pagesDifferential Diagnosis: Hallows Around LightfeedodeedoNo ratings yet
- Understanding Strabismus PDFDocument143 pagesUnderstanding Strabismus PDFhenok birukNo ratings yet
- 9 Retinal DetachmentDocument6 pages9 Retinal DetachmentNinin Erdininsih ArNo ratings yet
- OpthalDocument15 pagesOpthalWaiwit KritayakiranaNo ratings yet
- Eye ExaminationDocument9 pagesEye ExaminationFilbert KunardiNo ratings yet
- Emteaz OphthalmologyDocument16 pagesEmteaz OphthalmologyRaouf Ra'fat SolimanNo ratings yet
- Icd X BayiDocument11 pagesIcd X BayiArifin YusufNo ratings yet
- White Dot Syndromes: Presented by Yasmine Sameh El Sharnouby Ophthalmology SpecialistDocument43 pagesWhite Dot Syndromes: Presented by Yasmine Sameh El Sharnouby Ophthalmology SpecialistJasmine MinoNo ratings yet
- 1.2 Asst EngineerDocument21 pages1.2 Asst Engineercoep05No ratings yet
- Referensi 9 PDFDocument4 pagesReferensi 9 PDFDzulkifli SukriNo ratings yet
- Dispensing AnisometropiaDocument28 pagesDispensing Anisometropiahenok biruk100% (2)
- A Consideration of Binocular Parameters in The Spectacle PDFDocument5 pagesA Consideration of Binocular Parameters in The Spectacle PDFPierre A. RodulfoNo ratings yet
- ReferatDocument14 pagesReferatJeanne d'Arc DyanchanaNo ratings yet
- Eidon - Atlas Catalog WebDocument51 pagesEidon - Atlas Catalog Webefze71No ratings yet
- Strabismus Quick GuideDocument4 pagesStrabismus Quick Guideghitza80100% (1)