Professional Documents
Culture Documents
Tracheoesophageal Fistula
Tracheoesophageal Fistula
Uploaded by
Pankaj SinghOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tracheoesophageal Fistula
Tracheoesophageal Fistula
Uploaded by
Pankaj SinghCopyright:
Available Formats
TRACHEOESOPHAGEAL FISTULA
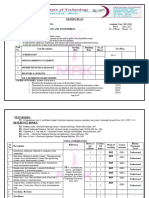
Successive stages in the development of the tracheoesophageal septum during embryologic development. (A) The laryngotracheal diverticulum forms as a ventral outpouching from the caudal part of the primitive pharynx. (B) Longitudinal tracheoesophageal folds begin to fuse toward the midline to eventually form the tracheoesophageal septum. (C) The
tracheoesophageal septum has completely formed. (D) If the tracheoesophageal septum deviates posteriorly, esophageal atresia with a tracheoesophageal fistula develops incidence of 1 in 3,000 to 4,000 live births. 10% cases may be associated with VACTREL polyhydramnios earliest,+/_ stomach bubble / neck pouch? Antenatal associated anomalies the neonate with esophageal atresia presents with copious, fine, white, frothy bubbles of mucus in the mouth and, sometimes, the nose. rattling respirations and episodes of coughing, choking and cyanosis.may be exaggerated by feeding abdominal distention develops as air builds up in the stomach i/c/o distal fistula Radiopaque 8 French (in preterm infants) or 10 French (in term infants) nasogastric or feeding tube should be passed through the nose to the stomach. In patients with atresia,
the tube typically stops at 10 to 12 cm. The normal distance to an infant's gastric cardia is approximately 17 cm. radiographs (posteroanterior and lateral views) should be obtained to confirm the position of the tube. The radiograph should include the entire abdomen. Contrast studies are seldom necessary to confirm the diagnosis. Such studies increase the risk of aspiration pneumonitis.
Waterson and Montreal classifications have been used to predict mortalit in patients with TOF. As per Watersons classification; Group A = bw >2500, no anomalies Group B = bw > 1800 moderate anomalies, moderate pneumoniis Group C = bw <1800 with svere anomalies / pneumoniis
As per Montreal class: Group I = No ventilator dependence with minor / major anomalies + ventilator dependence wih minor anomalies.
Group II = Ventilator dependence wih major anomalies/ life threatening anomalies regardless of pulmonary status. Unstable neonate with/without sepsis = stabilize, Gastrostomy with distal esophageal pouch foleys balloon occlusion of TOF done to minimize the air leak following ventilation therapy. Stable / mild pulmonary symptoms /minimal infiltrates taken for thoracotomy. Occasionally, urgent thoracotomy with ligation and division of the TEF, followed by delayed esophageal repair, may be necessary when respiratory support is required, and inspired air is lost via the fistula. Definitive esophageal repair is attempted when the infant's condition stabilizes. Before surgical correction, the infant must be evaluated thoroughly for other congenital anomalies with chest radiograph,renal ultrasound and echocardiogram. The goal of airway management in a patient with EA/TEF is to maintain adequate ventilation of the lungs without ventilating the fistula. The patient is positioned left side down for a right posterior lateral thoracotomy. If a previous gastrostomy was performed, it is opened and placed on straight drainage to avoid gastric distention during the procedure. A short posterolateral incision is made below the level of the tip of the scapula (Fig. 4), and hemostasis is obtained with electrocoagulation. The latissimus dorsi muscle is identified and retracted posteriorly, but occasionally is divided (Fig. 5). The auscultatory space of Korotkoff is identified, and the scapula is retracted superiorly and the serratus anterior muscle medially. It is usually unnecessary to divide the serratus muscle, thus avoiding the risk of developing a winged scapula. The fourth intercostal space is identified and entered. The intercostal muscles are carefully divided to avoid entering the pleura. An extrapleural dissection is carried out
The intact pleura and underlying lung are retracted medially with moistened sponges under a soft malleable retractor. The dissection continues with the use of a moist peanut sponge until the azygos is fully mobilized and the mediastinal pleura over the vein is opened. The azygos vein is divided between two 4-0 suture ties. This vein is often the marker for the site of the TEF as it enters the trachea. A branch of the vagus nerve usually passes over the area as well. the TEF is identified and carefully dissected free near the trachea preserving the small vessels to the midesophagus that arise directly from the aorta. A.The tracheoesophageal fistula site is mobilized circumferentially distal to the fistula, and the area is encircled with a vessel loop. B: Traction sutures are placed, with great care taken not to encroach on the lumen of the trachea, which can result in narrowing with closure. Division of the fistula is then performed using a tenotomy scissors. C: The tracheal end is closed with a 5-0 continuous or interrupted suture. The closure is tested with positive-pressure ventilation to rule out a leak. The tracheal suture line is covered with mediastinal pleura to reduce the risk of recurrent tracheoesophageal fistula should an anastomotic leak occur. While the proximal esophageal pouch is mobilized, a proximal fistula should be excluded. The proximal esophagus is mobilized to the thoracic inlet within the neck. When opening the proximal esophagus, care should be taken to ensure that the opening is at the lowermost point recognized with the feeding tube tip. The distal esophagus is freed only as much as necessary to approximate the ends of the esophagus. A single-layer anastomosis is performed with full-thickness, interrupted 4-0 sutures, involving mucosa and muscularis. The posterior sutures are placed with the suture knots on the outside. B: After the posterior suture line is completed, a feeding tube is advanced into the distal esophagus and stomach. The anterior sutures are inserted to complete the single-layer anastomosis.
Circular myotomy of the proximal esophageal pouch is useful to gain 1.0 cm of esophageal length for a tension-free anastomosis.
No. 12 French chest tube is placed, entering the posterior mediastinal space below the incision, being careful to avoid injury to the intact pleura during insertion. The tip of the tube is situated superiorly, near, but not on, the anastomosis, and is kept in place with a 4-0 PDS or Vicryl suture Post op & complications: The nasogastric tube that was placed in the stomach at the time of the procedure should be fixed and not moved. If it slips out, replacement should not be attempted. Head of bed elevation and enteral drip feedings are often initiated through the nasogastric tube on postoperative day 3 in an effort to minimize GERD. The chest tube is left in place and usually on water seal until postoperative day 6, when a contrast barium swallow confirms that no anastomotic leak is present. Oral feedings may be initiated after a negative contrast study. Care should be exercised during oral feedings
because of the high incidence of esophageal dysmotility problems (>30%) and the risk of GERD, which is observed in 50% of cases. When GERD is noted, the patient should be placed on reflux precautions, along with the administration of H2-blockers and prokinetic agents (metoclopramide). If an anastomotic leak is noted, it is usually minimal and closes spontaneously over the course of the next week. Rarely, a major anastomotic disruption may require reoperation. Most anastomotic strictures respond to esophageal dilatation using either a balloon dilator or a more traditional dilator of the Tucker, Maloney type with fluoroscopic guidance or Savory dilators passed over a guidewire when needed. Failure of an anastomotic stricture to respond to dilatation is often caused by GERD; which can be treated wih floppy nissens or toupets fundoplication. Recurrent TEF is an uncommon complication.; requiring surgical repair. In c/o type A TOF; gap between the two ends of the esophagus can be measured by placing a radiopaque dilator in the proximal esophagus, refluxing contrast material into the lower esophagus through the gastrostomy, and obtaining a radiograph (Fig. 18). When the gap is less than 2.0 cm a thoracotomy and primary repair can be attempted. Delayed anastomosis is possible in the majority of cases (4 to 5 months); however, a proximal esophageal myotomy to bridge the gap frequently may be necessary. Staged stretching of the proximal esophagus by formation of an esophagostomy that is periodically advanced inferiorly onto the anterior chest wall, as described by Kimura and Soper, is an alternative method of achieving additional length A reversed gastric tube is fashioned along the greater curvature of the stomach, incising both anterior and posterior walls to conform to the size of No. 18 to 24 French catheter.alternatively gastric pullup may be done/ colon interposition may be done.
You might also like
- Executive Coaching Workbook PDFDocument19 pagesExecutive Coaching Workbook PDFDiego Fortes100% (4)
- ConstipationDocument33 pagesConstipationsalmawalidNo ratings yet
- Esophageal AtresiaDocument21 pagesEsophageal AtresiaOktania Putri Kusnawan100% (2)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Intestinal Obstruction in Paediatrics - James GathogoDocument21 pagesIntestinal Obstruction in Paediatrics - James GathogoMalueth Angui100% (1)
- Complete Intestinal ObstructionDocument8 pagesComplete Intestinal ObstructionThuganamix100% (2)
- DyspepsiaDocument7 pagesDyspepsiaFa'iz HeryotoNo ratings yet
- Acute Cholecystitis SeminarDocument42 pagesAcute Cholecystitis SeminarNatnaelNo ratings yet
- Gastric Outlet Obstruction: Its Surgical ManagementDocument40 pagesGastric Outlet Obstruction: Its Surgical ManagementGudeta shegerNo ratings yet
- Intestinal ObstructionDocument12 pagesIntestinal ObstructionNurul Nurnita100% (1)
- Pneumonperitoneum A Review of Nonsurgical Causes PDFDocument7 pagesPneumonperitoneum A Review of Nonsurgical Causes PDFDellysa Eka Nugraha TNo ratings yet
- Pancreatic CancerDocument25 pagesPancreatic CancerAatir JavaidNo ratings yet
- Agis Mira Dewi, S.kedDocument35 pagesAgis Mira Dewi, S.kedAgiish EMdeNo ratings yet
- Esophageal Atresia and Tracheoesophageal FistulaDocument28 pagesEsophageal Atresia and Tracheoesophageal FistulaarifNo ratings yet
- Child's HerniaDocument13 pagesChild's HerniaKreshnik HAJDARINo ratings yet
- Philippine Urological Association, Inc.: Executive Committee and Board Members 1997Document12 pagesPhilippine Urological Association, Inc.: Executive Committee and Board Members 1997mits98No ratings yet
- BRONCHITIS Case PresentationDocument28 pagesBRONCHITIS Case PresentationJoshua DulayNo ratings yet
- Palliative Care Case Study: Qamar Abbas Deputy Medical Director ST Clare HospiceDocument12 pagesPalliative Care Case Study: Qamar Abbas Deputy Medical Director ST Clare HospicePraba KaranNo ratings yet
- GastroenteritisDocument24 pagesGastroenteritisMomogi ForeverhappyNo ratings yet
- Bowel ObstructionDocument6 pagesBowel ObstructionKryza Dale Bunado BaticanNo ratings yet
- SplenectomyDocument7 pagesSplenectomynessajoanNo ratings yet
- Acute TonsillitisDocument34 pagesAcute TonsillitisArvindhan100% (1)
- Ulcerative Colitis: DR Syed Ubaid Associate Professor of SurgeryDocument71 pagesUlcerative Colitis: DR Syed Ubaid Associate Professor of SurgeryFachry Al RafiqiNo ratings yet
- Hirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshDocument48 pagesHirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshArchana Mahata100% (1)
- Esophageal CarcinomaDocument11 pagesEsophageal CarcinomaFRM2012No ratings yet
- Biliary AtresiaDocument8 pagesBiliary AtresiaBrooke MauriNo ratings yet
- Pyloric StenosisDocument11 pagesPyloric StenosisJustin CharlesNo ratings yet
- COVID-19: Brian, Fernando, Jason, FelitaDocument8 pagesCOVID-19: Brian, Fernando, Jason, FelitaCharson ChenNo ratings yet
- Pneumothorax: DR G.B.L Samarasekera Consultant Respiratory Physician DGH - GampahaDocument50 pagesPneumothorax: DR G.B.L Samarasekera Consultant Respiratory Physician DGH - GampahappgpcsNo ratings yet
- 31 Uro Hydrocele 111211112520 Phpapp02Document6 pages31 Uro Hydrocele 111211112520 Phpapp02ppc_20No ratings yet
- Malabsorption Syndrome: By:-Ms. Sarungbam Sarju Devi Asst. Professor RinpsDocument27 pagesMalabsorption Syndrome: By:-Ms. Sarungbam Sarju Devi Asst. Professor RinpsShitaljit IromNo ratings yet
- Colostomy CareDocument15 pagesColostomy CareMahmoud Sherif100% (1)
- Diarrhea: WHO and IMCI GuidelinesDocument37 pagesDiarrhea: WHO and IMCI GuidelinesJohn Christopher LucesNo ratings yet
- Acute PyelonephritisDocument16 pagesAcute PyelonephritisDilshan WickramanayakaNo ratings yet
- Case Report Esophageal AtresiaDocument3 pagesCase Report Esophageal Atresiaadriani lawrenciaNo ratings yet
- PeritonitisDocument19 pagesPeritonitisAditya SahidNo ratings yet
- NCP GeDocument14 pagesNCP GeSuluhTriUtomoNo ratings yet
- Congestive Heart FailureDocument37 pagesCongestive Heart FailurePierre Aseron ManuelNo ratings yet
- Colostomy and Nursing CareDocument63 pagesColostomy and Nursing CareSangeeta BSRNo ratings yet
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- Hirschprung DiseaseDocument9 pagesHirschprung DiseaseRajeev JhaNo ratings yet
- Anal FissureDocument8 pagesAnal Fissurenisya1982_hasibuanNo ratings yet
- Diverticular Disease RingkasanDocument20 pagesDiverticular Disease RingkasanSuardimanAchoNo ratings yet
- GoutDocument26 pagesGoutRifki AlfikriNo ratings yet
- Clinical Review: Acute CholecystitisDocument5 pagesClinical Review: Acute CholecystitisElsa SimangunsongNo ratings yet
- Inguinal HerniaDocument9 pagesInguinal HerniaAmanda RapaNo ratings yet
- Large Bowel Obstruction by Nic MDocument42 pagesLarge Bowel Obstruction by Nic MRisky OpponentNo ratings yet
- Duodenal UlcerDocument1 pageDuodenal UlcerNeferterieManguinaoVillanueva100% (1)
- Peptic UlcerDocument5 pagesPeptic UlcermerobabuNo ratings yet
- Mastitis: By: Hj. Fatimah Usman, OBGYN (C)Document12 pagesMastitis: By: Hj. Fatimah Usman, OBGYN (C)David TurnerNo ratings yet
- Bowel IncontinenceDocument4 pagesBowel IncontinenceprashanthNo ratings yet
- Inguinal Hernia: Karen Brasel, MD, MPH Medical College of WisconsinDocument39 pagesInguinal Hernia: Karen Brasel, MD, MPH Medical College of WisconsinGbotemi AlaladeNo ratings yet
- Updated Nurses Role in Organ DonationDocument7 pagesUpdated Nurses Role in Organ Donationapi-401168581No ratings yet
- Coass 17205 - Case Report Otitis Externa Diffuse (Revisi 31.12) 2Document53 pagesCoass 17205 - Case Report Otitis Externa Diffuse (Revisi 31.12) 2atikahanifahNo ratings yet
- TetanusDocument3 pagesTetanusRoma Nova Pascual CabarrubiasNo ratings yet
- Leg UlcersDocument22 pagesLeg UlcersMarera DomnicNo ratings yet
- How Low Can You Endure The Pain, Mr. Bond?Document70 pagesHow Low Can You Endure The Pain, Mr. Bond?Venny VeronicaNo ratings yet
- Management of Patients With Intestinal and Rectal DisordersDocument33 pagesManagement of Patients With Intestinal and Rectal DisordersDoneva Lyn MedinaNo ratings yet
- Interstitial CystitisDocument8 pagesInterstitial CystitisAhmad SyaifudinNo ratings yet
- Intestinal Obstruction: EpidemiologyDocument11 pagesIntestinal Obstruction: EpidemiologyBereket temesgenNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Walther Handgun Comparison ChartDocument1 pageWalther Handgun Comparison ChartSasaki KyoukaNo ratings yet
- Bend TestDocument38 pagesBend TestAzan Safril100% (1)
- CASO 2 - Guia EstudianteDocument5 pagesCASO 2 - Guia EstudianteMishe MontenegroNo ratings yet
- HRM Section A and C Case HHUPD-1-3Document3 pagesHRM Section A and C Case HHUPD-1-3vijay kumarNo ratings yet
- Structural Developments: Inland Waterway Towboats and BargesDocument8 pagesStructural Developments: Inland Waterway Towboats and BargesEd UrquizaNo ratings yet
- CURVESDocument30 pagesCURVESPHULARAM PEGUNo ratings yet
- How Index Fossils Help Define Geologic TimeDocument2 pagesHow Index Fossils Help Define Geologic Timelasxdkasdas sdadwdacNo ratings yet
- Pairing Scheme 1st Year 2024 BY PHYSICS INN ACDEMIA M.A. JAVEDDocument1 pagePairing Scheme 1st Year 2024 BY PHYSICS INN ACDEMIA M.A. JAVEDabdull phyNo ratings yet
- Emily Demjanenko ResumeDocument1 pageEmily Demjanenko Resumeapi-354589335No ratings yet
- The Cost of Goods Sold For The Month of December: Excel Professional Services, IncDocument4 pagesThe Cost of Goods Sold For The Month of December: Excel Professional Services, IncmatildaNo ratings yet
- Market Structure and Market PerformanceDocument22 pagesMarket Structure and Market PerformanceAishwarya SudhirNo ratings yet
- ManufuckingscriptDocument13 pagesManufuckingscript가푸타No ratings yet
- SQL Database Interview QuestionsDocument29 pagesSQL Database Interview Questionstest caseNo ratings yet
- Deep Nightly FathomsDocument44 pagesDeep Nightly FathomsMaria Guarneri67% (3)
- 2 Method of Statement For RC Wall Between Feature Wall and Ramp - Rev 01 PDFDocument3 pages2 Method of Statement For RC Wall Between Feature Wall and Ramp - Rev 01 PDFJoe LeeNo ratings yet
- Introductory Entomology: Third Semester Lamjung CampusDocument206 pagesIntroductory Entomology: Third Semester Lamjung Campusnishan khatriNo ratings yet
- Combiflam Tablets PI - 08072019Document13 pagesCombiflam Tablets PI - 08072019ArunNo ratings yet
- Answers For Exercises On Topic 8 1Document7 pagesAnswers For Exercises On Topic 8 1Mark John Paul CablingNo ratings yet
- Kilmarnock To ArdrossanDocument2 pagesKilmarnock To Ardrossanadamdon89100% (1)
- Dangase Group - Research FinalDocument59 pagesDangase Group - Research FinalGlenda PapelleroNo ratings yet
- Maxey Mark Pauline 1965 JapanDocument28 pagesMaxey Mark Pauline 1965 Japanthe missions networkNo ratings yet
- Lesson Plan Ds 8603Document7 pagesLesson Plan Ds 8603sramalingam288953No ratings yet
- EQ 5D 5L Index Value Calculator V1.1Document146 pagesEQ 5D 5L Index Value Calculator V1.1mmmaw mmNo ratings yet
- Chapter 4 - Braking System 4.1 Brake LinesDocument14 pagesChapter 4 - Braking System 4.1 Brake LinesEmanuel VidalNo ratings yet
- STD 5 Unit 7 Simple Machines Study MaterialDocument6 pagesSTD 5 Unit 7 Simple Machines Study MaterialCool WritzNo ratings yet
- 02 - Virtualisation and NetworkingDocument63 pages02 - Virtualisation and Networkingvecanoc954No ratings yet
- Typical Details of Switchyard RequirementDocument364 pagesTypical Details of Switchyard RequirementEspro100% (1)
- Cobol 1.0Document43 pagesCobol 1.0sarathNo ratings yet
- Pond Based Tilapia Hatchery ManagementDocument50 pagesPond Based Tilapia Hatchery ManagementAlvin Javier PeranteNo ratings yet