Professional Documents
Culture Documents
People Registered With Drug Treatment Services Have Increased Risk of Drug-Related Death Following Discharge From Hospital
People Registered With Drug Treatment Services Have Increased Risk of Drug-Related Death Following Discharge From Hospital
Uploaded by
DheeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
People Registered With Drug Treatment Services Have Increased Risk of Drug-Related Death Following Discharge From Hospital
People Registered With Drug Treatment Services Have Increased Risk of Drug-Related Death Following Discharge From Hospital
Uploaded by
DheeCopyright:
Available Formats
Downloaded from ebmh.bmj.com on April 24, 2013 - Published by group.bmj.
com
Evidence-Based Mental Health Online First, published on April 17, 2013 as 10.1136/eb-2013-101305 Prognosis
People registered with drug treatment services have increased risk of drug-related death following discharge from hospital
doi:10.1136/eb-2013-101305
QUESTION Question: Are drug users at increased risk of drug-related death and non-drug-related suicide following discharge from hospital? Population: In total 69 457 individuals (69% men) were registered on the Scottish Drug Misuse Database (SDMD) over a 10-year period (April 1996March 2006). Deaths and hospital admissions were identied through linkage to national registers held by Scotlands Information Services Division, the General Register Ofce for Scotland and Health Protection Scotland. Setting: Scotland drug services; April 1996March 2006. Prognostic factors: Drug use as indicated by SDMD and hospital admission. Time-at-risk was calculated as date of rst attendance at drug treatment services to death or end of study (whichever came rst), and categorised according to time since most recent hospitalisation: during hospitalisation; within 28 days; 2990 days; 91 days to 1 year; and >1 year since discharge. The reference category was never admitted. Outcomes: Drug-related death (DRD), dened as main cause of death recorded with an ICD code indicating mental and behavioural disorders due to psychoactive substance misuse; accidental poisoning; intentional self-poisoning or assault by drugs, medicaments and biological substances; and poisoning events of undetermined intent. Non-DRD suicide, dened as any suicide excluding those with any ICD code corresponding to DRD. METHODS Design: Cohort study. Follow-up period: 10 years.
MAIN RESULTS There were 1383 DRDs during the study period, with a rate for the full cohort of 3.9/1000 person-years of follow-up (95% CI 3.7 to 4.2). Thirty-nine per cent of the cohort experienced at least one hospital stay. Those who never admitted had a DRD rate of 1.9/1000 person-years (95% CI 1.7 to 2.1). Those who admitted had higher DRD rates, with rates highest in the periods during and shortly following hospitalisation. The rate of DRD per 1000 person-years during hospitalisation was 87 (95% CI 72 to 103); within 28 days of hospitalisation it was 21 (95% CI 18 to 25); within 2990 days it was 12 (95% CI 10 to 15); within 91 days to 1 year it was 8.5 (95% CI 7.5 to 9.5); and >1 year since discharge it was 4.2 (95% CI 3.7 to 4.7). Following adjustment for demographic and behavioural factors (including age, sex, injecting history, substances used), compared to those who never admitted, people who admitted had an increased risk of DRD: hazard ratios 9.6 (95% CI 8 to 12) within 28 days of discharge; 5.6 (95% CI 4.6 to 6.8) within 2990 days; 4.0 (95% CI 3.5 to 4.7) within 91 days to 1 year; and 2.3 (95% CI 2.0 to 2.7) at >1 year since discharge. There were 269 non-DRD suicides during the study period. Non-DRD suicides showed a similar pattern to DRDs, with highest rate during hospitalisation (18/1000 person-years). The year following hospitalisation accounted for 38% of all non-DRD suicides. CONCLUSIONS People who are registered with drug treatment services have an increased rate of DRD and non-DRD suicide in the period following discharge from hospital. ABSTRACTED FROM
Merrall EL, Bird SM, Hutchinson SJ. A record-linkage study of drug-related death and suicide after hospital discharge among drug-treatment clients in Scotland, 19962006. Addiction. 2013;108:37784. Correspondence to: Elizabeth LC Merrall, MRC Biostatistics Unit, Robinson Way, Cambridge, CB2 OSR, UK; Elizabeth.merrall@mrc-bsu.cam.ac.uk Sources of funding: Medical Research Council and a grant from the Chief Scientist Ofce of the Scottish Executive. Additional reference is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/eb-2013-101305).
COMMENTARY
errall and colleagues report the ndings of a notably signicant, meaningful and relevant study of postdischarge death or suicide among drug treatment clients in Scotland. While people experiencing substance and/or alcohol misuse seldom evoke the same or similar societal response than those with heart disease, diabetes or oncology do, for many occidental countries, alcohol and substance misuse are signicant public health problems. According to the data provided by the WHO, drug and alcohol-related problems account for as much as 5.4% of the global burden of disease.1 Yet it can be argued that the corresponding body of research activity (and funding) dedicated to this area does not correspond to the associated burden of disease; as a result, Merrall and colleagues study can be considered to be timely.
The use of electronic administrative records as the primary source of data is a most welcome development, the limitations of epidemiological research notwithstanding. For instance, in this case, the validity of ndings is determined, at least in part, by the methodological rigour of the original classication, and the problems of determining when a suicide is a suicide as a matter of public record. Accordingly, perhaps a brief acknowledgment here of such limitations may have been useful. The authors ndings are in keeping with the limited, related extant body of literature, wherein evidence indicates the period of time immediately following discharge has been found to be a particularly high-risk time for suicide. Accordingly, the recommendation for an additional support at the time of discharge echoes the exhortations of related studies. However, the
authors could have extended this argument to illustrate how the need to provide care for substance and/or alcohol users merely changes (rather than stops) after discharge. Perhaps some specic postdischarge follow-up interventions or strategies could have been identied. While the authors should be commended for including some suggestions for further statistically focused studies, a deeper insight into the particular lived experiences that contribute to these elevated postdischarge death rates would better inform the service responses to these needs.
John R Cutcliffe Adjunct Professor: University of Ottawa, Canada; School of Nursing, University of Coimbra, Portugal; and University of Malta, Malta Competing interests None.
EBMH Month 2013 Vol 00 No 00 Copyright Article author
(or their employer) 2013. Produced by BMJ Publishing Group Ltd under licence.
Downloaded from ebmh.bmj.com on April 24, 2013 - Published by group.bmj.com
People registered with drug treatment services have increased risk of drug-related death following discharge from hospital
Evid Based Mental Health published online April 17, 2013
doi: 10.1136/eb-2013-101305
Updated information and services can be found at:
http://ebmh.bmj.com/content/early/2013/04/16/eb-2013-101305.full.html
These include:
Data Supplement References P<P Email alerting service
"Supplementary Data"
http://ebmh.bmj.com/content/suppl/2013/04/16/eb-2013-101305.DC1.html
This article cites 1 articles
http://ebmh.bmj.com/content/early/2013/04/16/eb-2013-101305.full.html#ref-list-1
Published online April 17, 2013 in advance of the print journal. Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article.
Topic Collections
Articles on similar topics can be found in the following collections Suicide (psychiatry) (191 articles) Alcohol dependence (105 articles) Substance dependence (380 articles) Epidemiologic studies (521 articles) Epidemiology (1371 articles)
Advance online articles have been peer reviewed, accepted for publication, edited and typeset, but have not not yet appeared in the paper journal. Advance online articles are citable and establish publication priority; they are indexed by PubMed from initial publication. Citations to Advance online articles must include the digital object identifier (DOIs) and date of initial publication.
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Downloaded from ebmh.bmj.com on April 24, 2013 - Published by group.bmj.com
Notes
Advance online articles have been peer reviewed, accepted for publication, edited and typeset, but have not not yet appeared in the paper journal. Advance online articles are citable and establish publication priority; they are indexed by PubMed from initial publication. Citations to Advance online articles must include the digital object identifier (DOIs) and date of initial publication.
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Hypertension Protocol JeannineDocument53 pagesHypertension Protocol JeannineAleile DRNo ratings yet
- What The Python Spirit Really WantsDocument2 pagesWhat The Python Spirit Really WantsNOWHERE-MANNo ratings yet
- Ancients D6 RulebookDocument29 pagesAncients D6 RulebookRandy Miller100% (6)
- A Police-Led Addiction Treatment Referral Program in MassachusettsDocument2 pagesA Police-Led Addiction Treatment Referral Program in MassachusettsKeegan HamiltonNo ratings yet
- Original ResearchDocument23 pagesOriginal ResearchDhilah Harfadhilah FakhirahNo ratings yet
- Angelina Alphonce JohoDocument80 pagesAngelina Alphonce JohoMerlina WijayawatiNo ratings yet
- Geriatrics: Roger E. ThomasDocument44 pagesGeriatrics: Roger E. ThomasSubhash SharmaNo ratings yet
- Chapter 7. Longitudinal Studies: Nama: Sofia Marcelina NPM: A1E017005 PRODI: Pendidikan FisikaDocument4 pagesChapter 7. Longitudinal Studies: Nama: Sofia Marcelina NPM: A1E017005 PRODI: Pendidikan FisikaSofia MarcelinaNo ratings yet
- Health Services and Suicide PreventionDocument7 pagesHealth Services and Suicide Preventionfajat abdul fatahNo ratings yet
- Reduces Mortality in High-Risk Smokers Intensive Smoking Cessation InterventionDocument9 pagesReduces Mortality in High-Risk Smokers Intensive Smoking Cessation InterventionAnonymous Hc8CYEf9WKNo ratings yet
- IkhsanDocument14 pagesIkhsanSilvia Icha RiskiNo ratings yet
- 1471 Adasaasdasdas2458 2 9Document6 pages1471 Adasaasdasdas2458 2 9kennydimitraNo ratings yet
- A Systematic Review of What Barriers and Facilitators Prevent and Enable Physical Healthcare Services Access For Autistic AdultsDocument14 pagesA Systematic Review of What Barriers and Facilitators Prevent and Enable Physical Healthcare Services Access For Autistic AdultsLoreto Opazo RojasNo ratings yet
- End of Life Care For Lung CancerDocument7 pagesEnd of Life Care For Lung CancerPhilip R. MarallagNo ratings yet
- Disorders Transition To Schizophrenia in Acute and Transient PsychoticDocument8 pagesDisorders Transition To Schizophrenia in Acute and Transient PsychoticMuhammad Habibul IhsanNo ratings yet
- Piis 0749379716305177Document8 pagesPiis 0749379716305177api-341254870No ratings yet
- Annals of General PsychiatryDocument9 pagesAnnals of General PsychiatryPutu Agus GrantikaNo ratings yet
- Diabetes ComparativosDocument9 pagesDiabetes ComparativosMarlon Salguedo MadridNo ratings yet
- Reviews: Smoking and Survival of Colorectal Cancer Patients: Systematic Review and Meta-AnalysisDocument9 pagesReviews: Smoking and Survival of Colorectal Cancer Patients: Systematic Review and Meta-AnalysisMudhi'afaturrochmah Silviana PutriNo ratings yet
- Annotated Bibliography For Obesity and SmokingDocument5 pagesAnnotated Bibliography For Obesity and Smokingapi-240254375No ratings yet
- Telemedicine and Asthma: An innovative approach to improve morbidity and mortality rates for active adults.: Effects of Telemedicine in Asthma care for remote and inner-city underserved populations.From EverandTelemedicine and Asthma: An innovative approach to improve morbidity and mortality rates for active adults.: Effects of Telemedicine in Asthma care for remote and inner-city underserved populations.No ratings yet
- Calidad de Vida 03Document7 pagesCalidad de Vida 03RosarioBengocheaSecoNo ratings yet
- Physicians and Substance AbuseDocument9 pagesPhysicians and Substance AbuseTabatha DuranNo ratings yet
- Gut 2011 Morris 806 13Document9 pagesGut 2011 Morris 806 13568563No ratings yet
- Mercury Exposure and Risk of Cardiovascular Disease in Two U.S. CohortsDocument17 pagesMercury Exposure and Risk of Cardiovascular Disease in Two U.S. CohortsKiky JatiningrumNo ratings yet
- Hypothetical Case Study Physicians' Labelling of End-Of-Life Practices: ADocument7 pagesHypothetical Case Study Physicians' Labelling of End-Of-Life Practices: Apenikek603No ratings yet
- Annals EpocDocument16 pagesAnnals EpocewbNo ratings yet
- Patient Survival Report 1Document5 pagesPatient Survival Report 1Rabeya Bibi 193-15-13510No ratings yet
- Health Affairs September, 2001 - October, 2001 LENGTH: 3352 Words TITLE: Are The Benefits of Newer Drugs Worth Their Cost? Evidence From TheDocument9 pagesHealth Affairs September, 2001 - October, 2001 LENGTH: 3352 Words TITLE: Are The Benefits of Newer Drugs Worth Their Cost? Evidence From Theapi-3711225No ratings yet
- Open Letter The Statistical Analysis and Data Integrity of Mehra Et Al - FinalDocument4 pagesOpen Letter The Statistical Analysis and Data Integrity of Mehra Et Al - FinalInvictus InmoralisNo ratings yet
- 1-s2.0-S1525505013004186 TUGAS INDAH-mainDocument5 pages1-s2.0-S1525505013004186 TUGAS INDAH-mainRendi Er PratamaNo ratings yet
- Future ImplicationsDocument2 pagesFuture ImplicationsConsuelo MolinaNo ratings yet
- Jurnal CHF 3 PDFDocument9 pagesJurnal CHF 3 PDFmuthia octavianaNo ratings yet
- Farmacos en AncianosDocument12 pagesFarmacos en AncianosKarina Alexandra Vera-Pinto EstacioNo ratings yet
- Adherence To Cardiovascular Therapy: A Meta-Analysis of Prevalence and Clinical ConsequencesDocument9 pagesAdherence To Cardiovascular Therapy: A Meta-Analysis of Prevalence and Clinical Consequencesdaniela NeculmanNo ratings yet
- Consumption of Alcohol, Cigarettes and Illegal Substances Among Physicians and Medical Students in Brandenburg ...Document8 pagesConsumption of Alcohol, Cigarettes and Illegal Substances Among Physicians and Medical Students in Brandenburg ...Marcelo Valenzuela DíazNo ratings yet
- Epidemiology ReviewDocument10 pagesEpidemiology ReviewSaurabhNo ratings yet
- Alok A. Khorana - Incidence and Predictors of Venous Thromboembolism (VTE) Among Ambulatory High-RiskDocument8 pagesAlok A. Khorana - Incidence and Predictors of Venous Thromboembolism (VTE) Among Ambulatory High-RiskFarid RakhmanNo ratings yet
- Encyclopedia of Public Health - Cohort StudyDocument3 pagesEncyclopedia of Public Health - Cohort StudyPhanindra Vasu KottiNo ratings yet
- Association Between Serum Lipids and Survival in Hemodialysis Patients and Impact of RaceDocument11 pagesAssociation Between Serum Lipids and Survival in Hemodialysis Patients and Impact of RaceJuanCarlosGonzalezNo ratings yet
- Title:: Long-Term Determinants of Death After Stroke in Ghana: Analysis by Stroke Types & SubtypesDocument23 pagesTitle:: Long-Term Determinants of Death After Stroke in Ghana: Analysis by Stroke Types & SubtypesanafolorisgreatNo ratings yet
- Protocol and AbstractDocument16 pagesProtocol and Abstractmaijosh0314No ratings yet
- Perpectiva Publica CancerDocument8 pagesPerpectiva Publica CancerDaniela Millan AngelNo ratings yet
- Capsule ProposalDocument6 pagesCapsule Proposaltho2793No ratings yet
- Screening Elders For Risk of Hospital Admission (1993)Document7 pagesScreening Elders For Risk of Hospital Admission (1993)Timothy TanNo ratings yet
- NHS Waiting List: The ExpressDocument5 pagesNHS Waiting List: The Expressfashuanmi ibukunNo ratings yet
- Briefly Summarize The Study You FoundDocument7 pagesBriefly Summarize The Study You FoundvevalyneoyooNo ratings yet
- Physical Health Assessment and Cardiometabolic Monitoring Practices Across Three Adult Mental Health Inpatient Units - A Retrospective Cohort StudyDocument13 pagesPhysical Health Assessment and Cardiometabolic Monitoring Practices Across Three Adult Mental Health Inpatient Units - A Retrospective Cohort StudyEshetu WondimuNo ratings yet
- An Increased Risk of Stroke Among Panic Disorder Patients: A 3-Year Follow-Up StudyDocument7 pagesAn Increased Risk of Stroke Among Panic Disorder Patients: A 3-Year Follow-Up StudyMade Priska RusmanaNo ratings yet
- Back To Cardiology ArticlesDocument10 pagesBack To Cardiology ArticlesmrezasyahliNo ratings yet
- Radiation Safety Paper Week 2Document4 pagesRadiation Safety Paper Week 2api-313040758No ratings yet
- Literature Review On Tobacco ConsumptionDocument7 pagesLiterature Review On Tobacco Consumptionafmzwflmdnxfeb100% (1)
- Rss Abstracts Booklet 2019 A4 PDFDocument324 pagesRss Abstracts Booklet 2019 A4 PDFSlice LeNo ratings yet
- Antithrombic Medications Vs Antithrombic DevicesDocument7 pagesAntithrombic Medications Vs Antithrombic Devicesapi-240398244No ratings yet
- Vital Signs: Awareness and Treatment of Uncontrolled Hypertension Among Adults - United States, 2003-2010Document8 pagesVital Signs: Awareness and Treatment of Uncontrolled Hypertension Among Adults - United States, 2003-2010Widya Setiabudi AseliNo ratings yet
- Vital Signs HTNDocument10 pagesVital Signs HTNAnuthat HongprapatNo ratings yet
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocument19 pagesWorld's Largest Science, Technology & Medicine Open Access Book PublisherMuhammad KhubaibNo ratings yet
- Preventable Adverse Drug ReactionsDocument54 pagesPreventable Adverse Drug ReactionsÇağla K.No ratings yet
- Cigarrette Smoking and Lung CancerDocument14 pagesCigarrette Smoking and Lung CancerJaicé AlalunaNo ratings yet
- ANNALS HIV ManegementDocument16 pagesANNALS HIV ManegementewbNo ratings yet
- Precision Medicine Oncology: A PrimerFrom EverandPrecision Medicine Oncology: A PrimerLorna Rodriguez-RodriguezNo ratings yet
- Laporan Penjualan Bulan Maret 2013': Area:MagelangDocument4 pagesLaporan Penjualan Bulan Maret 2013': Area:MagelangDheeNo ratings yet
- Worksheet in LAP MART 13'Document4 pagesWorksheet in LAP MART 13'DheeNo ratings yet
- What Makes You BeautifulDocument8 pagesWhat Makes You BeautifulDheeNo ratings yet
- The Internet and Mental Health Practice: EBMH NotebookDocument7 pagesThe Internet and Mental Health Practice: EBMH NotebookDheeNo ratings yet
- BTLS GratisDocument1 pageBTLS GratisDheeNo ratings yet
- M2M - The Day You Went AwayDocument11 pagesM2M - The Day You Went AwayDheeNo ratings yet
- Essay of MacbethDocument9 pagesEssay of MacbethMaria Ximena Romero GaravitoNo ratings yet
- Haryana SDO Exam Answer KeyDocument4 pagesHaryana SDO Exam Answer KeyPankaj SardanaNo ratings yet
- IR Repeated UestionsDocument9 pagesIR Repeated UestionssarasultanNo ratings yet
- 2240A10 v9 0417 CarmenSandiego IM BleedCMDocument2 pages2240A10 v9 0417 CarmenSandiego IM BleedCMCesar Zambrano MarazoNo ratings yet
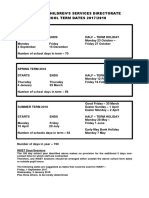
- Cumbria County Council Term Dates 2017-2018Document1 pageCumbria County Council Term Dates 2017-2018Samuel Kings SchoolNo ratings yet
- Ali Garah PDFDocument6 pagesAli Garah PDFMubashir MalikNo ratings yet
- Atty Ogena PDFDocument7 pagesAtty Ogena PDFNotario PrivadoNo ratings yet
- NSTP002 Proposal of Bom13Document2 pagesNSTP002 Proposal of Bom13Hazel Joy UgatesNo ratings yet
- 01Document38 pages01jessiewyattNo ratings yet
- Corporate AccountingDocument79 pagesCorporate Accountingakshrajput2005No ratings yet
- EN 1011-1 - 1998-A2 - 2003 (NBN) (E) - VervallenDocument5 pagesEN 1011-1 - 1998-A2 - 2003 (NBN) (E) - Vervallenjihu1170100% (1)
- AIR PHILIPPINES vs. PENNSWELL, INC.Document1 pageAIR PHILIPPINES vs. PENNSWELL, INC.Jayson Gabriel Soriano100% (4)
- Doctrine of Harmonious ConstructionDocument13 pagesDoctrine of Harmonious ConstructionVicky VermaNo ratings yet
- Ads 2223 485683 PDFDocument3 pagesAds 2223 485683 PDFHarsh PatelNo ratings yet
- Sharda TilakDocument135 pagesSharda TilakAayushi TayalNo ratings yet
- Dhaka Tribune Print Edition: December 06, 2013Document26 pagesDhaka Tribune Print Edition: December 06, 2013Dhaka TribuneNo ratings yet
- Jody Wilson-Raybould's Full Written Submission To The Justice CommitteeDocument43 pagesJody Wilson-Raybould's Full Written Submission To The Justice CommitteeNational Post93% (14)
- para Aque Kings Enterprises, Inc. vs. Court of Appeals 268 SCRA 727, February 26, 1997Document22 pagespara Aque Kings Enterprises, Inc. vs. Court of Appeals 268 SCRA 727, February 26, 1997Shieremell DiazNo ratings yet
- Omnibus CertificationDocument1 pageOmnibus CertificationGertrude GamonnacNo ratings yet
- Against The Passage of The Rizal BillDocument10 pagesAgainst The Passage of The Rizal BillJennifer AdvientoNo ratings yet
- Garg JJ400276 - 9045101903Document2 pagesGarg JJ400276 - 9045101903Sanju DhatwaliaNo ratings yet
- Donaldfox Exposingthenucleartruthof9 11andotherthingsifindinteresting Dickcheney Aclearandpresentdan 140929152401 Phpapp02Document289 pagesDonaldfox Exposingthenucleartruthof9 11andotherthingsifindinteresting Dickcheney Aclearandpresentdan 140929152401 Phpapp02Ashley Diane HenryNo ratings yet
- GarletDocument1 pageGarletGertrude ArquilloNo ratings yet
- Non Fatal OffencesDocument5 pagesNon Fatal OffencesAimi AzemiNo ratings yet
- Winfield Plaintiff DepoDocument32 pagesWinfield Plaintiff Depothe kingfish100% (1)
- Lukas 23 33-43Document2 pagesLukas 23 33-43MCTC LuponNo ratings yet
- C.P.C Case Analysis Order 7 Rlue 11Document21 pagesC.P.C Case Analysis Order 7 Rlue 11Uday ReddyNo ratings yet
- 02 Reyes v. CaDocument2 pages02 Reyes v. CaMikhel BeltranNo ratings yet