Professional Documents
Culture Documents
Coagulation 1
Coagulation 1
Uploaded by
kriss WongCopyright:
Available Formats
You might also like
- Exchange TransfusionDocument35 pagesExchange Transfusionsobinjohnpkl100% (2)
- Basa, Gina Solon 2133027610Document3 pagesBasa, Gina Solon 2133027610ginaNo ratings yet
- A Study of Ampalaya Seeds As A Substitute For Coffee BeansDocument27 pagesA Study of Ampalaya Seeds As A Substitute For Coffee Beanskriss Wong0% (5)
- Blood Bank Case StudyDocument17 pagesBlood Bank Case StudyMelissa Harding33% (3)
- Blood Components Process FlowchartDocument1 pageBlood Components Process FlowchartCatherine Constantino BaintoNo ratings yet
- Cytology I - Techniques and Application: Peter NG Cyto Lab Ic, MT, PYNEHDocument201 pagesCytology I - Techniques and Application: Peter NG Cyto Lab Ic, MT, PYNEHbusiness onlyyouNo ratings yet
- Hematology Week 1 CBCDocument4 pagesHematology Week 1 CBCMICHELLE RAPELONo ratings yet
- Hematology II Notes - MagtalasDocument12 pagesHematology II Notes - MagtalasAbhugz VosotrosNo ratings yet
- Bone Marrow Pathology 2 PDFDocument69 pagesBone Marrow Pathology 2 PDFJorge VenturaNo ratings yet
- Reticulocyte CountDocument10 pagesReticulocyte CountNeo Mervyn MonahengNo ratings yet
- Chapter Blood: RBC Platelet HemostasisDocument89 pagesChapter Blood: RBC Platelet Hemostasisapi-19916399100% (1)
- Clinical Microscopy (Analysis of Urine and Other Body Fluids)Document14 pagesClinical Microscopy (Analysis of Urine and Other Body Fluids)Jeanly DoctorNo ratings yet
- Hematology BMLS 103Document88 pagesHematology BMLS 103harpreetNo ratings yet
- Chapter 1: Introduction To Urinalysis: Urine CompositionDocument74 pagesChapter 1: Introduction To Urinalysis: Urine CompositionMegumi TadokoroNo ratings yet
- Ethics in Blood TransfusionDocument1 pageEthics in Blood TransfusionGerardLumNo ratings yet
- Hematology Basics NewDocument32 pagesHematology Basics Newkimbo23No ratings yet
- Cerebrospinal Fluid: By: Raynhier G. Constantino, RMTDocument53 pagesCerebrospinal Fluid: By: Raynhier G. Constantino, RMTJaellah MatawaNo ratings yet
- LN Hematology MLT FinalDocument549 pagesLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Coag Made EasyDocument16 pagesCoag Made EasyBrian RobertsNo ratings yet
- 27kiran Body FluidsDocument33 pages27kiran Body FluidsABHINABA GUPTANo ratings yet
- Here, Only 1 Few Stages Undergo Subdivision (Sabi Ni Maam)Document6 pagesHere, Only 1 Few Stages Undergo Subdivision (Sabi Ni Maam)Jaenie Grace AliganNo ratings yet
- Coombs TestDocument11 pagesCoombs TestunilabreynosaNo ratings yet
- Methods of Studying Fungi: Dr. Alice Alma C. BungayDocument74 pagesMethods of Studying Fungi: Dr. Alice Alma C. BungayKaycee Gretz LorescaNo ratings yet
- Clinical MicrosDocument14 pagesClinical MicrosKRISTINE JOY PANGAHINNo ratings yet
- Renal BiopsyDocument53 pagesRenal Biopsybusiness onlyyouNo ratings yet
- Manual Platelet CountDocument14 pagesManual Platelet CountMiyo SobremisanaNo ratings yet
- Study Questions (Hematology)Document11 pagesStudy Questions (Hematology)tkanesNo ratings yet
- (6-7) PATH - Colonic Polyps and CarcinomaDocument11 pages(6-7) PATH - Colonic Polyps and Carcinomaaaron mbindyoNo ratings yet
- Microscopic Examination of UrineDocument4 pagesMicroscopic Examination of UrineGlaiza Erika Baes GudaNo ratings yet
- Coagulation NotesDocument14 pagesCoagulation NotesthrowawyNo ratings yet
- CrossmatchingDocument4 pagesCrossmatchingEl Marie SalungaNo ratings yet
- Analysis of Physical Properties of UrineDocument2 pagesAnalysis of Physical Properties of UrineameerabestNo ratings yet
- Chapter 14 - Routine and Point of Care Testing in HematologyDocument10 pagesChapter 14 - Routine and Point of Care Testing in HematologyNathaniel Sim100% (1)
- Bone Marrow ExaminationDocument31 pagesBone Marrow ExaminationMonique BorresNo ratings yet
- Basic Haematology Exercise 1 (MKEB2403)Document10 pagesBasic Haematology Exercise 1 (MKEB2403)kiedd_04100% (8)
- Cytopreparatory Technique: Ama AfrahDocument49 pagesCytopreparatory Technique: Ama Afrahreuben kwotaNo ratings yet
- Coombs Test - Principle, Types, Procedure and Result InterpretationDocument34 pagesCoombs Test - Principle, Types, Procedure and Result InterpretationABHINABA GUPTANo ratings yet
- Xi. Clotting Time Bleeding TimeDocument16 pagesXi. Clotting Time Bleeding TimeCookie MonsterNo ratings yet
- RBC AnomalyDocument38 pagesRBC AnomalyTorillo KimNo ratings yet
- Red Blood Cell AbnormalitiesDocument9 pagesRed Blood Cell AbnormalitiesIez FatihahNo ratings yet
- Hematology (Ferrokinetics HemoglobinometryDocument3 pagesHematology (Ferrokinetics HemoglobinometryAbby TorresNo ratings yet
- Blood Transfusion ReactionsDocument33 pagesBlood Transfusion Reactionsmarianne.bilaoen09100% (1)
- The Peripheral Blood FilmDocument5 pagesThe Peripheral Blood FilmanggaririnNo ratings yet
- CytologyDocument12 pagesCytologyEsther HutagalungNo ratings yet
- Chapter 15 - Examination of The Peripheral Blood Film and Correlation With The Complete Blood CountDocument7 pagesChapter 15 - Examination of The Peripheral Blood Film and Correlation With The Complete Blood CountNathaniel SimNo ratings yet
- Urine Specimen Collection: Ms. Sneha SehrawatDocument36 pagesUrine Specimen Collection: Ms. Sneha SehrawatRajaNo ratings yet
- Hematology 2 Lecture Notes Platelet Qualitative DisordersDocument4 pagesHematology 2 Lecture Notes Platelet Qualitative DisorderscccomayogNo ratings yet
- Blood DonationsDocument6 pagesBlood DonationsCHIPapiNo ratings yet
- Cytology II: Gynae and Non-Gynae CytologyDocument126 pagesCytology II: Gynae and Non-Gynae Cytologybusiness onlyyouNo ratings yet
- Anaerobe of Clinical ImportanceDocument43 pagesAnaerobe of Clinical ImportanceDayledaniel SorvetoNo ratings yet
- HEMOSTASIS Coagulation PathwayDocument3 pagesHEMOSTASIS Coagulation PathwayGianna SablanNo ratings yet
- Examination of UrineDocument7 pagesExamination of UrineDaniel LamasonNo ratings yet
- Routine UrinalysisDocument4 pagesRoutine UrinalysisDanica Joy Christelle L. PilarNo ratings yet
- Hematoxylin and Eosin StainingDocument6 pagesHematoxylin and Eosin StainingRaja Sharma100% (1)
- Serological TestsDocument2 pagesSerological TestsKimberly EspaldonNo ratings yet
- Relevance of Serum Tumor MarkersDocument25 pagesRelevance of Serum Tumor MarkersDrPawan KirtaniNo ratings yet
- FRCPath+picture-based+questions (1)Document39 pagesFRCPath+picture-based+questions (1)Marvi UmairNo ratings yet
- Polycythemia VeraDocument4 pagesPolycythemia VeraAllyson VillarNo ratings yet
- Laboratory Activity 10: Osmotic Fragility Test (Oft)Document27 pagesLaboratory Activity 10: Osmotic Fragility Test (Oft)Marie LlanesNo ratings yet
- 05 - Peripheral Blood Smear ExaminationDocument40 pages05 - Peripheral Blood Smear Examinationaustin_doc2rNo ratings yet
- Red Cell and White Cell Counting, BloodDocument89 pagesRed Cell and White Cell Counting, BloodJovel Gangcuangco100% (1)
- Quality in Laboratory Hemostasis and ThrombosisFrom EverandQuality in Laboratory Hemostasis and ThrombosisSteve KitchenNo ratings yet
- Exp 4&5 Post LabDocument4 pagesExp 4&5 Post Labkriss WongNo ratings yet
- Balancing Chemical Equations Student DirectionsDocument1 pageBalancing Chemical Equations Student Directionskriss Wong100% (1)
- Si UnitsDocument29 pagesSi Unitskriss WongNo ratings yet
- Microbiology 2013Document7 pagesMicrobiology 2013kriss Wong50% (2)
- Acetone: Common Name Chemical NameDocument7 pagesAcetone: Common Name Chemical Namekriss WongNo ratings yet
- 9) FruitsDocument18 pages9) Fruitskriss WongNo ratings yet
- Lectures 1 3 Handout For PrintingDocument43 pagesLectures 1 3 Handout For Printingkriss Wong100% (2)
- 0143 LabelDocument1 page0143 Labelkriss WongNo ratings yet
- Fruithease Fruit ProductsDocument3 pagesFruithease Fruit Productskriss WongNo ratings yet
- Epidemiologicalmethods 150922085550 Lva1 App6892Document31 pagesEpidemiologicalmethods 150922085550 Lva1 App6892kriss WongNo ratings yet
- Zinc Oxide PasteDocument9 pagesZinc Oxide Pastekriss Wong100% (1)
- Quality Control Lab Manual AnswersDocument6 pagesQuality Control Lab Manual Answerskriss WongNo ratings yet
- The Ladmer SystemDocument12 pagesThe Ladmer Systemkriss WongNo ratings yet
- Sparkling Pineapple Wine: Krysmee DelightsDocument1 pageSparkling Pineapple Wine: Krysmee Delightskriss WongNo ratings yet
- Overview of Blood Components and Their PreparationDocument9 pagesOverview of Blood Components and Their PreparationaksinuNo ratings yet
- Clinical Hematology and Fundamentals of Hemostasis 5th Edition Harmening Test BankDocument7 pagesClinical Hematology and Fundamentals of Hemostasis 5th Edition Harmening Test Bankalbertchavezwbkafcgrns100% (33)
- Mechanism of Blood Clotting Extensic Pathway Factors Affecting Blood ClottingDocument18 pagesMechanism of Blood Clotting Extensic Pathway Factors Affecting Blood ClottingRaunak TripathiNo ratings yet
- Wwiy4300 PDF - PDF - Hematology - Blood PDFDocument10 pagesWwiy4300 PDF - PDF - Hematology - Blood PDFRam KumawatNo ratings yet
- MLS 123 MODULE 6 UNIT 5 Venipuncture Procedure Special Collection Procedure in POCTDocument16 pagesMLS 123 MODULE 6 UNIT 5 Venipuncture Procedure Special Collection Procedure in POCTVENUS LIRIA PANTINo ratings yet
- Finals Trans (Hema)Document16 pagesFinals Trans (Hema)Ayesha CaragNo ratings yet
- Blood - NotesDocument5 pagesBlood - NotesJenn Mamar CabayaoNo ratings yet
- Mechanisms of Transfusion-Related Acute Lung Injury (TRALI) : Anti-Leukocyte AntibodiesDocument6 pagesMechanisms of Transfusion-Related Acute Lung Injury (TRALI) : Anti-Leukocyte AntibodiesBladimir CentenoNo ratings yet
- Transfusion Checklist Poster June 2021 Ver 1.0 1Document1 pageTransfusion Checklist Poster June 2021 Ver 1.0 1Naresh SinghNo ratings yet
- Dr. Witra Irfan, SP.B (K) V - DVTDocument29 pagesDr. Witra Irfan, SP.B (K) V - DVTmuhammad azharanNo ratings yet
- Blood TypingDocument34 pagesBlood Typingaurezea100% (1)
- Lab DVTDocument20 pagesLab DVTLezard DomiNo ratings yet
- Blood TypesDocument2 pagesBlood TypesPRINTDESK by DanNo ratings yet
- BB Lab Manual 4Document2 pagesBB Lab Manual 4emmanuelNo ratings yet
- The Language of MedicineDocument9 pagesThe Language of MedicineErnesto SilveiraNo ratings yet
- CHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.Document2 pagesCHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.MAHESH GAUTAMNo ratings yet
- Review of Current Transfusion Therapy and Blood Banking PracticesDocument52 pagesReview of Current Transfusion Therapy and Blood Banking PracticesAmaranto SantosoNo ratings yet
- Pathophysiology of Protein S DeficiencyDocument5 pagesPathophysiology of Protein S DeficiencyRenz Ivan FuntilonNo ratings yet
- A Blood TypeDocument1 pageA Blood TypeDarwin CruzNo ratings yet
- MTAP ISBB - Sir JJ (Merged)Document9 pagesMTAP ISBB - Sir JJ (Merged)Nathan DrakeNo ratings yet
- Artikel Jurnal IbnuDocument4 pagesArtikel Jurnal Ibnuibnu rifaldiNo ratings yet
- Upper Gi BleedDocument12 pagesUpper Gi BleedTaha KamranNo ratings yet
- Cross MatchingDocument5 pagesCross MatchingMustafa KhandgawiNo ratings yet
- The Effect of 3.2% and 3.8% Sodium CitrateDocument6 pagesThe Effect of 3.2% and 3.8% Sodium CitrateBambang KurniawanNo ratings yet
- Finals FundaDocument82 pagesFinals FundaNecesario BanaagNo ratings yet
- Ficha Tecnica Factor ViiiDocument3 pagesFicha Tecnica Factor ViiiCaro ErazoNo ratings yet
Coagulation 1
Coagulation 1
Uploaded by
kriss WongOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Coagulation 1
Coagulation 1
Uploaded by
kriss WongCopyright:
Available Formats
Page |1 M.R.T.
4DMT
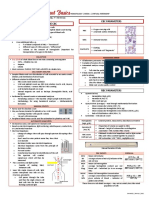
COAGULATION
Hemostasis cellular and biochemical events which function in harmony to keep blood with the veins and arteries. prevent blood loss from injuries. re-establish blood flow.
1. Primary Hemostasis involves platelets and endothelium. activated by small injuries. rapid, short-lived reponse. positive feedback: formation of platelet plug.
A. Platelets Production: Hemocytoblast Megakaryocyte Megakaryoblast Metamegakaryocyte Promegakaryocyte Platelets
Distribution: a. Peripheral blood 70% b. Spleen 30% RR: 150 400 x 10^9 / L Life Span: 8 11 days Size: 2.5 m in diameter Zones: a. Peripheral zone adhesion and aggregation. b. Sol Gel zone shape and contraction. c. Organelle zone metabolic activities. Function: a. Adhesion - platelets roll and cling to non - platelet surfaces. b. Activation - occurs when vWF and collagen binds to glycoprotein Ib receptor on the surface of the platelet. c. Aggregation - platelets adhere to each other. d. Secretion - platelets discharge the contents of their granules. e. Clot Retraction creates more bulk in the clot making it more resistant to stress. f. Cytokine signalling - platelets secrete platelet derived growth factor. B. Endothelial cells - assist in platelet activation. - limits coagulation mechanism. - clot dissolution.
Page |2 2. Secondary Hemostasis involve coagulation factors. activated by large wounds from trauma, surgery, dental procedures. delayed, long-term response. positive feedback: formation of fibrin clot.
A. Coagulation - mechanism whereby after injury to a blood vessel, plasma coagulation factors, tissue factors, and calcium work together on the surface of platelets to form a fibrin clot. B. Coagulation Factors - proteins engaged in formation of a fibrin clot from fibrinogen.
Factor I II III IV V VII VIII IX X XI XII Prekallikrein High Molecular Weight Kininogen XIII Platelet factor 3 Customary name Fibrinogen Prothrombin Tissue factor Ionic Calcium Labile factor Stable Factor Antihemophilic Factor (vWF) Christmas factor Stuart-Prower factor Plasma thromboplastin antecedent (PTA) Hageman factor Fletcher factor, PK Fitzgerald factor, HMWK Fibrin-stabilizing factor (FSF) Phospholipids, phosphatidyl serine PF3 Function Thrombin substrate, polymerizes to form fibrin Serine protease Cofactor Mineral Cofactor Serine protease Cofactor Factor VIII carrier and platelet adhesion Serine protease Serine protease Serine protease Serine protease Serine protease Cofactor Transamidase Assembly molecule
C. Coagulation Cascade - series of biochemical reactions and feedback mechanisms by means of intrinsic and extrinsic pathway, or both, leading to a common pathway forming a fibrin clot. C.1. Intrinsic pathway - utilization of plasma contact factors to initiate coagulation, beginning with the activation of factor XII; all necessary factors required are contained in the circulating blood. - activated partial thromboplastin time (aPTT) test monitors this pathway.
Page |3 - aPTT measures factors XII, XI, X, IX, VIII, V, II and I. C.2. Extrinsic pathway - coagulation pathway that is activated by tissue thromboplastin; necessary components are factor VII and calcium. - prothrombin time (PT) test monitors this pathway. - PT measures factors VII, X, V, II, I. C.3. Common pathway - final stage of the coagulation cascade, beginning with the convergence of the extrinsic and intrinsic pathways (factor X) ending with the formation of fibrin clot.
Page |4
3. Specimen Collection and Handling A. Anticoagulants - 3. 8 % or 3.2 % sodium citrate - normal ratio of blood to anticoagulant is 9:1 B. Holding sample - siliconized glassware (glass activates factor XII and platelets will adhere to glass). C. Collection of Blood Sample - venipuncture should be clean and quick with minimal stasis. - if drawing tubes for other tests, draw blue top last, except that if an EDTA tube is needed for a CBC, the purple top tube should be drawn after the blue top coagulation tube. If only drawing blood for coagulation testing, allow some blood to drip into vacutainer before collection. (The first blood drawn in a venipuncture is most likely to be contaminated with small amounts of tissue thromboplastin. This can activate the extrinsic pathway and lead to variable results). - prompt and gentle inversion must be done to bind all calcium immediately. D. Specimen Processing - transportation to the laboratory should be done as quickly because some changes can begin in vitro. - specimens should be centrifuged for 10 minutes to get the cell - free plasma - anticoagulant mixture. - always check for micro-clot formation, if present, specimen is unacceptable for testing. - hemolyzed specimens are also unacceptable for testing because of possible clotting factor activation. 4. Routine Test of Hemostatic Function A. Primary Hemostasis A.1. Bleeding Time - measures the time required for the cessation of bleeding after a standardized capillary puncture to a capillary bed. - the time required will depend on the capillary integrity, number of platelets and the platelet function. - types: a. Duke method: earlobe; RR: 0-6 minutes. b. Ivy method: forearm; RR: 1-6 minutes. c. Template method: forearm; RR: 2-9.5 minutes. - prolonged with aspirin.
Page |5 A.2. Clot Retraction - evaluates platelet function, fibrinogen, red cell volume and fibrinolytic activity. - whole blood is allowed to clot and observed for retraction. - platelets of adequate number and viability are required for clot retraction to occur. - normal value: evidence of retraction within 2 hours (varies with methodology). B. Secondary Hemostasis B.1. Coagulation time/ Clotting Time - measures the period required for the free flowing blood to clot or solidify after it has been removed to the body. - types: a. Drop or Slide method: capillary blood; NV: 2-4 minutes b. Lee and White method (tube method): venous blood: NV: 7-15 minutes B.2. Prothrombin Time (PT) - test for extrinsic and common pathway. - measures factors I, II, V, VII and X. - monitors oral anticoagulants (warfarin, coumarin, dicoumarol). - reagent: tissue thromboplastin and CaCl2. - sensitive to vitamin K factors. - International normalized ratio (INR)
INR = (patient result)ISI
(mean of the reference range) *ISI = International Sensitivity Index from manufacturer
- reference range: < 14 seconds a. Therapeutic goal: INR 2.0 3.5 B.3. Activated Partial Thromboplastin Time - test for intrinsic and common pathway. - measures all factors except factor VII and XII. - monitors heparin therapy. - reagents: activator (kaolin, celite or ellagic acid), platelet phospholipid (PF3) and CaCl2. - reference range: 20 40 seconds
Page |6 OTHER TESTS: Laboratory Tests for Primary Hemostasis 1. Capillary Resistance / Fragility/ Tourniquet /Rumpel Leedes or Hess Test 2. 3. 4. 5. Platelet Adhesiveness Test Platelet Aggregation Test Platelet Count Platelet Morphology and MPV Laboratory Tests for Secondary Hemostasis 1. 2. 3. 4. Plasma Recalcification Time Activated Clotting Time Stypven Time Thrombin Time / Thrombin Clotting Time 5. Reptilase Time 6. Substitution Test (Mixing Studies) 7. Prothrombin Consumption/Serum Prothrombin Test 8. Thromboplastin Generation Test 9. Specific Factor Assay 10. Assay of vWR:Ag and vWR:Reo Rockett/Laurel 11. Duckerts or Clot Solubility Test 12. Tests for Circulating Inhibitors of Coagulation Laboratory Tests for Fibrinolysis 1. Determination of Fibrinolytic Products 2. Lysis Time 3. Proteins involved in Fibrinolysis
5. Bleeding Disorders
Page |7
Disorder of Primary Hemostasis
Platelet Disorders Vascular Disorders
Qualitative
Quantitative
Disorders of Platelet Secretion Disorders of Platelet Adhesion Disorders of Platelet Aggregation Glanzmanns thrombasthenia Acquired von Willebrand Disease
Thrombocytopenia
Thrombocytosis primary
Hereditary Hereditary Hemorrhagic Telangiectasia/ Rendu-WeberOsler, HemangiomaThrombocytopenia
Disorders related to distribution or dilution /big spleen
reactive
Acquired
Bernard Soullier/ Giant Platelet Syndrome
Increased platelet destruction/ utilization Impaired/ decreased platelet production BM failure Thromboxane Pathway Disorders TTP, drug induced, non immune mechanisms, DIC Kasabach-Merit, Ehler-Danlos, Marfan, Osteogenesis imperfect, Pseudoxanthoma elasticum
von Willebrand Disease Storage Pool Diseases Primary granule deficiency Hemmeler anomaly
Congenital hypoplasia, MHA, WAS, BS, Fanconi, TAR
Anaphylactoid purpura, Henoch Schonlein, Senile purpura, Scurvy, Purpura simplex, Infectious purpura, Drug induced purpuras associated with paraprotenemiea s, Amyloidosis, Idiopathic purpuras
Electron dense/ delta granules deficiency
Neonatal hypoplasia - drugs, infections Acquired Acquired hypoplasia ionizing radiation, drugs -
Hereditary
Pudlak, Wiskott Aldrich, Chediak Higashi, TAR
aspirin like defects
Alpha granules deficiency
due to inhibitors of prostaglandin pathway (chronic aspirin intake or inhibitors of thromboxane or cyclooxegenase pathway
Gray Platelet Syndrome, Quebec Platelet Disorder
Page |8
Page |9
P a g e | 10
P a g e | 11
References:
McPherson, R. & Pincus, M. (2006). Henrys Clinical Diagnosis and Management by Laboratory Methods. US: Saunders Elsevier Linne, J. & Ringsrud, K. (1999). Clinical Laboratory Science The Basics and Routine Techniques Harmening DM: Clinical Hematology and Fundamentals of Hemostasis, ed 3. Philadelphia, FA Davis Co, 1997. Turgeon ML: Clinical Hematology: Theory and Procedures, ed 3. Philadelphia, Lippincott-Raven Publishers, 1998.
P a g e | 12
You might also like
- Exchange TransfusionDocument35 pagesExchange Transfusionsobinjohnpkl100% (2)
- Basa, Gina Solon 2133027610Document3 pagesBasa, Gina Solon 2133027610ginaNo ratings yet
- A Study of Ampalaya Seeds As A Substitute For Coffee BeansDocument27 pagesA Study of Ampalaya Seeds As A Substitute For Coffee Beanskriss Wong0% (5)
- Blood Bank Case StudyDocument17 pagesBlood Bank Case StudyMelissa Harding33% (3)
- Blood Components Process FlowchartDocument1 pageBlood Components Process FlowchartCatherine Constantino BaintoNo ratings yet
- Cytology I - Techniques and Application: Peter NG Cyto Lab Ic, MT, PYNEHDocument201 pagesCytology I - Techniques and Application: Peter NG Cyto Lab Ic, MT, PYNEHbusiness onlyyouNo ratings yet
- Hematology Week 1 CBCDocument4 pagesHematology Week 1 CBCMICHELLE RAPELONo ratings yet
- Hematology II Notes - MagtalasDocument12 pagesHematology II Notes - MagtalasAbhugz VosotrosNo ratings yet
- Bone Marrow Pathology 2 PDFDocument69 pagesBone Marrow Pathology 2 PDFJorge VenturaNo ratings yet
- Reticulocyte CountDocument10 pagesReticulocyte CountNeo Mervyn MonahengNo ratings yet
- Chapter Blood: RBC Platelet HemostasisDocument89 pagesChapter Blood: RBC Platelet Hemostasisapi-19916399100% (1)
- Clinical Microscopy (Analysis of Urine and Other Body Fluids)Document14 pagesClinical Microscopy (Analysis of Urine and Other Body Fluids)Jeanly DoctorNo ratings yet
- Hematology BMLS 103Document88 pagesHematology BMLS 103harpreetNo ratings yet
- Chapter 1: Introduction To Urinalysis: Urine CompositionDocument74 pagesChapter 1: Introduction To Urinalysis: Urine CompositionMegumi TadokoroNo ratings yet
- Ethics in Blood TransfusionDocument1 pageEthics in Blood TransfusionGerardLumNo ratings yet
- Hematology Basics NewDocument32 pagesHematology Basics Newkimbo23No ratings yet
- Cerebrospinal Fluid: By: Raynhier G. Constantino, RMTDocument53 pagesCerebrospinal Fluid: By: Raynhier G. Constantino, RMTJaellah MatawaNo ratings yet
- LN Hematology MLT FinalDocument549 pagesLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Coag Made EasyDocument16 pagesCoag Made EasyBrian RobertsNo ratings yet
- 27kiran Body FluidsDocument33 pages27kiran Body FluidsABHINABA GUPTANo ratings yet
- Here, Only 1 Few Stages Undergo Subdivision (Sabi Ni Maam)Document6 pagesHere, Only 1 Few Stages Undergo Subdivision (Sabi Ni Maam)Jaenie Grace AliganNo ratings yet
- Coombs TestDocument11 pagesCoombs TestunilabreynosaNo ratings yet
- Methods of Studying Fungi: Dr. Alice Alma C. BungayDocument74 pagesMethods of Studying Fungi: Dr. Alice Alma C. BungayKaycee Gretz LorescaNo ratings yet
- Clinical MicrosDocument14 pagesClinical MicrosKRISTINE JOY PANGAHINNo ratings yet
- Renal BiopsyDocument53 pagesRenal Biopsybusiness onlyyouNo ratings yet
- Manual Platelet CountDocument14 pagesManual Platelet CountMiyo SobremisanaNo ratings yet
- Study Questions (Hematology)Document11 pagesStudy Questions (Hematology)tkanesNo ratings yet
- (6-7) PATH - Colonic Polyps and CarcinomaDocument11 pages(6-7) PATH - Colonic Polyps and Carcinomaaaron mbindyoNo ratings yet
- Microscopic Examination of UrineDocument4 pagesMicroscopic Examination of UrineGlaiza Erika Baes GudaNo ratings yet
- Coagulation NotesDocument14 pagesCoagulation NotesthrowawyNo ratings yet
- CrossmatchingDocument4 pagesCrossmatchingEl Marie SalungaNo ratings yet
- Analysis of Physical Properties of UrineDocument2 pagesAnalysis of Physical Properties of UrineameerabestNo ratings yet
- Chapter 14 - Routine and Point of Care Testing in HematologyDocument10 pagesChapter 14 - Routine and Point of Care Testing in HematologyNathaniel Sim100% (1)
- Bone Marrow ExaminationDocument31 pagesBone Marrow ExaminationMonique BorresNo ratings yet
- Basic Haematology Exercise 1 (MKEB2403)Document10 pagesBasic Haematology Exercise 1 (MKEB2403)kiedd_04100% (8)
- Cytopreparatory Technique: Ama AfrahDocument49 pagesCytopreparatory Technique: Ama Afrahreuben kwotaNo ratings yet
- Coombs Test - Principle, Types, Procedure and Result InterpretationDocument34 pagesCoombs Test - Principle, Types, Procedure and Result InterpretationABHINABA GUPTANo ratings yet
- Xi. Clotting Time Bleeding TimeDocument16 pagesXi. Clotting Time Bleeding TimeCookie MonsterNo ratings yet
- RBC AnomalyDocument38 pagesRBC AnomalyTorillo KimNo ratings yet
- Red Blood Cell AbnormalitiesDocument9 pagesRed Blood Cell AbnormalitiesIez FatihahNo ratings yet
- Hematology (Ferrokinetics HemoglobinometryDocument3 pagesHematology (Ferrokinetics HemoglobinometryAbby TorresNo ratings yet
- Blood Transfusion ReactionsDocument33 pagesBlood Transfusion Reactionsmarianne.bilaoen09100% (1)
- The Peripheral Blood FilmDocument5 pagesThe Peripheral Blood FilmanggaririnNo ratings yet
- CytologyDocument12 pagesCytologyEsther HutagalungNo ratings yet
- Chapter 15 - Examination of The Peripheral Blood Film and Correlation With The Complete Blood CountDocument7 pagesChapter 15 - Examination of The Peripheral Blood Film and Correlation With The Complete Blood CountNathaniel SimNo ratings yet
- Urine Specimen Collection: Ms. Sneha SehrawatDocument36 pagesUrine Specimen Collection: Ms. Sneha SehrawatRajaNo ratings yet
- Hematology 2 Lecture Notes Platelet Qualitative DisordersDocument4 pagesHematology 2 Lecture Notes Platelet Qualitative DisorderscccomayogNo ratings yet
- Blood DonationsDocument6 pagesBlood DonationsCHIPapiNo ratings yet
- Cytology II: Gynae and Non-Gynae CytologyDocument126 pagesCytology II: Gynae and Non-Gynae Cytologybusiness onlyyouNo ratings yet
- Anaerobe of Clinical ImportanceDocument43 pagesAnaerobe of Clinical ImportanceDayledaniel SorvetoNo ratings yet
- HEMOSTASIS Coagulation PathwayDocument3 pagesHEMOSTASIS Coagulation PathwayGianna SablanNo ratings yet
- Examination of UrineDocument7 pagesExamination of UrineDaniel LamasonNo ratings yet
- Routine UrinalysisDocument4 pagesRoutine UrinalysisDanica Joy Christelle L. PilarNo ratings yet
- Hematoxylin and Eosin StainingDocument6 pagesHematoxylin and Eosin StainingRaja Sharma100% (1)
- Serological TestsDocument2 pagesSerological TestsKimberly EspaldonNo ratings yet
- Relevance of Serum Tumor MarkersDocument25 pagesRelevance of Serum Tumor MarkersDrPawan KirtaniNo ratings yet
- FRCPath+picture-based+questions (1)Document39 pagesFRCPath+picture-based+questions (1)Marvi UmairNo ratings yet
- Polycythemia VeraDocument4 pagesPolycythemia VeraAllyson VillarNo ratings yet
- Laboratory Activity 10: Osmotic Fragility Test (Oft)Document27 pagesLaboratory Activity 10: Osmotic Fragility Test (Oft)Marie LlanesNo ratings yet
- 05 - Peripheral Blood Smear ExaminationDocument40 pages05 - Peripheral Blood Smear Examinationaustin_doc2rNo ratings yet
- Red Cell and White Cell Counting, BloodDocument89 pagesRed Cell and White Cell Counting, BloodJovel Gangcuangco100% (1)
- Quality in Laboratory Hemostasis and ThrombosisFrom EverandQuality in Laboratory Hemostasis and ThrombosisSteve KitchenNo ratings yet
- Exp 4&5 Post LabDocument4 pagesExp 4&5 Post Labkriss WongNo ratings yet
- Balancing Chemical Equations Student DirectionsDocument1 pageBalancing Chemical Equations Student Directionskriss Wong100% (1)
- Si UnitsDocument29 pagesSi Unitskriss WongNo ratings yet
- Microbiology 2013Document7 pagesMicrobiology 2013kriss Wong50% (2)
- Acetone: Common Name Chemical NameDocument7 pagesAcetone: Common Name Chemical Namekriss WongNo ratings yet
- 9) FruitsDocument18 pages9) Fruitskriss WongNo ratings yet
- Lectures 1 3 Handout For PrintingDocument43 pagesLectures 1 3 Handout For Printingkriss Wong100% (2)
- 0143 LabelDocument1 page0143 Labelkriss WongNo ratings yet
- Fruithease Fruit ProductsDocument3 pagesFruithease Fruit Productskriss WongNo ratings yet
- Epidemiologicalmethods 150922085550 Lva1 App6892Document31 pagesEpidemiologicalmethods 150922085550 Lva1 App6892kriss WongNo ratings yet
- Zinc Oxide PasteDocument9 pagesZinc Oxide Pastekriss Wong100% (1)
- Quality Control Lab Manual AnswersDocument6 pagesQuality Control Lab Manual Answerskriss WongNo ratings yet
- The Ladmer SystemDocument12 pagesThe Ladmer Systemkriss WongNo ratings yet
- Sparkling Pineapple Wine: Krysmee DelightsDocument1 pageSparkling Pineapple Wine: Krysmee Delightskriss WongNo ratings yet
- Overview of Blood Components and Their PreparationDocument9 pagesOverview of Blood Components and Their PreparationaksinuNo ratings yet
- Clinical Hematology and Fundamentals of Hemostasis 5th Edition Harmening Test BankDocument7 pagesClinical Hematology and Fundamentals of Hemostasis 5th Edition Harmening Test Bankalbertchavezwbkafcgrns100% (33)
- Mechanism of Blood Clotting Extensic Pathway Factors Affecting Blood ClottingDocument18 pagesMechanism of Blood Clotting Extensic Pathway Factors Affecting Blood ClottingRaunak TripathiNo ratings yet
- Wwiy4300 PDF - PDF - Hematology - Blood PDFDocument10 pagesWwiy4300 PDF - PDF - Hematology - Blood PDFRam KumawatNo ratings yet
- MLS 123 MODULE 6 UNIT 5 Venipuncture Procedure Special Collection Procedure in POCTDocument16 pagesMLS 123 MODULE 6 UNIT 5 Venipuncture Procedure Special Collection Procedure in POCTVENUS LIRIA PANTINo ratings yet
- Finals Trans (Hema)Document16 pagesFinals Trans (Hema)Ayesha CaragNo ratings yet
- Blood - NotesDocument5 pagesBlood - NotesJenn Mamar CabayaoNo ratings yet
- Mechanisms of Transfusion-Related Acute Lung Injury (TRALI) : Anti-Leukocyte AntibodiesDocument6 pagesMechanisms of Transfusion-Related Acute Lung Injury (TRALI) : Anti-Leukocyte AntibodiesBladimir CentenoNo ratings yet
- Transfusion Checklist Poster June 2021 Ver 1.0 1Document1 pageTransfusion Checklist Poster June 2021 Ver 1.0 1Naresh SinghNo ratings yet
- Dr. Witra Irfan, SP.B (K) V - DVTDocument29 pagesDr. Witra Irfan, SP.B (K) V - DVTmuhammad azharanNo ratings yet
- Blood TypingDocument34 pagesBlood Typingaurezea100% (1)
- Lab DVTDocument20 pagesLab DVTLezard DomiNo ratings yet
- Blood TypesDocument2 pagesBlood TypesPRINTDESK by DanNo ratings yet
- BB Lab Manual 4Document2 pagesBB Lab Manual 4emmanuelNo ratings yet
- The Language of MedicineDocument9 pagesThe Language of MedicineErnesto SilveiraNo ratings yet
- CHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.Document2 pagesCHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.MAHESH GAUTAMNo ratings yet
- Review of Current Transfusion Therapy and Blood Banking PracticesDocument52 pagesReview of Current Transfusion Therapy and Blood Banking PracticesAmaranto SantosoNo ratings yet
- Pathophysiology of Protein S DeficiencyDocument5 pagesPathophysiology of Protein S DeficiencyRenz Ivan FuntilonNo ratings yet
- A Blood TypeDocument1 pageA Blood TypeDarwin CruzNo ratings yet
- MTAP ISBB - Sir JJ (Merged)Document9 pagesMTAP ISBB - Sir JJ (Merged)Nathan DrakeNo ratings yet
- Artikel Jurnal IbnuDocument4 pagesArtikel Jurnal Ibnuibnu rifaldiNo ratings yet
- Upper Gi BleedDocument12 pagesUpper Gi BleedTaha KamranNo ratings yet
- Cross MatchingDocument5 pagesCross MatchingMustafa KhandgawiNo ratings yet
- The Effect of 3.2% and 3.8% Sodium CitrateDocument6 pagesThe Effect of 3.2% and 3.8% Sodium CitrateBambang KurniawanNo ratings yet
- Finals FundaDocument82 pagesFinals FundaNecesario BanaagNo ratings yet
- Ficha Tecnica Factor ViiiDocument3 pagesFicha Tecnica Factor ViiiCaro ErazoNo ratings yet