Professional Documents
Culture Documents
2 - PULPAL, Dental Pain
2 - PULPAL, Dental Pain
Uploaded by
Abod NaserOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 - PULPAL, Dental Pain
2 - PULPAL, Dental Pain
Uploaded by
Abod NaserCopyright:
Available Formats
Dr.
Tahani Abualteen
PULPAL & DENTAL PAIN
Dental pulp: It is a specialized connective tissue Dental pulp is a soft tissue unlike enamel and dentine which are hard tissues Dental pulp is similar to any connective tissue in the body (containing cells, fibers & ground substance) It is contained within the tooth Because of this property dental pulp is considered a specialized connective tissue Enclosed by dentine Dental pulp is the only connective tissue in body being surrounded by rigid walls (dentine walls) What happens if there's inflammation in any connective tissue? What are the signs of inflammation? - Redness, increased temperature, pain & swelling - Swelling is caused by vasodilatation - Vasodilatation is caused by different factors (histamine and other histamine-like factors) and also there is a role for the parasympathetic system that finally leads to exudate of fluids from inside of blood vessels to the outside (at extracellular matrix) - In any tissue of the body undergoing inflammation there is no problem with this fluid exudate because we have a space for the accompanying swelling to expand and the pain isn't going to be that much - But what happens if we dont have a space for that tissue to swell (as in the dental pulp due to the rigid walls surrounding it)?! The swelling will be at the expense of pressing the nerves & blood vessels and because of this the pain related to pulpitis (inflammation of dental pulp) is usually very severe and it is among the most severe pain that human can encounter (rated number two after delivery pain) It is continuous with the periodontal ligament through the apical foramen Dental pulp is a vital tissue (has blood supply & nerves) and thus it has to communicate with tissues surrounding the tooth (periodontal tissues) and this communication occurs through the apical foramen Pulpitis usually ends with pulp necrosis (death of dental pulp) unlike inflammation in other sites of the body because it is surrounded by rigid walls (as a result, the swelling expands on the expense of nerves & blood vessels and compress them) and it is nourished through a very small apical foramen (as a result, the blood supply is very limited) So that when nerves are compressed pain is elicited and when blood vessels are compressed pulp necrosis occurs
/101
Dr. Tahani Abualteen
Pulp necrosis contains millions of bacteria and so if pulp necrosis remains, these bacteria will move to the surrounding periodontal ligament and thats why one of the complications of pulpitis is inflammation of the periodontal tissue Apical foramen is narrow and only allows for passage of the neurovascular bundle It has a small volume (total volume in all teeth is 0.40 ml)
Pulpodentine complex: Functions of pulp & dentine are interlinked Dental pulp and dentine are categorized together because they embryologically originate from the same tissue which is the dental papilla (ectomesenchyme) Dental pulp and dentine are vital tissues unlike enamel which is a non-vital and because of this if we drill through enamel, this can be done without anesthesia since no pain will be elicited, But once we reach dentine, pain is felt and anesthesia is needed Functions of the pulp o Maintain dentinal health by supplying nutrients when pulp is lost, vitality of dentine is lost o Provide a pathway for sensory impulses from dentine o Initiate & govern repair of dentine in injury (tertiary dentine formation) Cells forming dentine still exist at the peripheral area of the dental pulp, and thus any injury to dentine, can be repaired (each 1.0 mm lost at enamel side is replaced by 1.0 mm at pulpal side) ** For dentine to be repaired, we need the rate of building to exceed the rate of destruction Cells forming enamel are lost, and thus any injury to enamel, can't be repaired Odontoblasts: They are the layer of specialized cells immediately adjacent to dentine They have processes that penetrate dentine for varying distances They are responsible for formation of dentine They are involved in sensory perception of dentine
Components of pulpal tissue: Fibers o Collagen Confers rigidity Maintains 3D spatial relationship of cells, blood vessels & nerves o Elastin in blood vessel walls Cells o Odontoblasts o Fibroblasts o Undifferentiated mesenchymal cells o Macrophages, histiocytes & lymphocytes Amorphous matrix o Support Nerves & blood vessels
/102
Dr. Tahani Abualteen
Pulp nerves: They are sensory fibers (A & C fibers) and similar to general pain nerves in the body Types of nerve terminals near blood vessels o Large fibers Contain small vesicles (resemble cholinergic endings) o Medium fibers Numerous small dense-cored vesicles Found in pulp horns & pulp chamber o Small fibers Numerous large dense vesicles (purinergic or peptidergic endings) Plexus of Raschkow (subodontoblastic plexus) Odontoblasts, after building of dentine, remain in the pulp just below dentine forming the odontoblastic layer and beneath it we have a network of nerves called the Plexus of Raschkow Individual axons of A and C fibers divide into many branches in the plexus
Pulp nerves during tooth formation: Initial nerve fibers are always found near the base (NOT the tip) of dental papilla Dental papilla is found in the concavity of enamel organ and responsible for dentine & dental pulp formation At cap stage o Nerve fibers form a plexus (network of nerves) that get distributed to the dental follicle at first and then they spread into the dental papilla Dental follicle is found around the enamel organ and responsible for cementum, alveolar bone & PDL formation At bell stage o Nerve fibers are still un-Myelinated (and this means the Myelinated A fibers appear later) At eruption o Number of fibers & their average size increase due to transition towards myelination Initial nerve fibers are un-Myelinated C fibers (which are Unmyelinated) appear first then followed by A fibers (Which are Myelinated) Number & size of fibers continue to increase for a few years after eruption Dentine is then laid down throughout life pulp becomes reduced in size nerves decrease in size functionality decreases too Dentinogenesis is a continuous process that doesn't stop even after root completion and even without any stimulus Layers of dentine will continue to lay down very slowly from the inside "at pulpal side" at the expense of the pulp and because of that the volume of the pulp is decreased, along with it , the nerve plexuses also decrease in size and the functionality of the pulp decreases with time Young people have better dental pulps than elderly people because their dental pulps are bigger meaning better innervations and more blood vessels and so the ability of their dental pulp to respond to stimuli or to fight pathogens is stronger!
/103
Dr. Tahani Abualteen
Root canal treatment in elderly people is much more difficult than that in young people because canals would be very narrow, constricted, closed and different Ageing pulp o o o o Decrease in pulp volume Decrease in number of nerve axons entering pulp (so that, response of dental pulp is reduced) Reduction in Myelinated fiber size Plexus of Raschkow shows little change (less affected by aging)
Pulp nerves in primary teeth: Number of nerve axons in primary teeth is less than that in permanent teeth EXCEPT in primary canine There's no big difference in number of nerve axons between primary and permanent canines Number of nerve axons decrease with resorption until the tooth is shed (the whole root is lost) and get replaced by successor tooth
Neurotrophic substances: They are growth factors important for the development of the nervous system inside the pulp Nerve growth factors (evidence for their important role in pulpal nervous system development): o Promote survival of neural crest cells in trigeminal ganglion o Produced in the maxillary process to maintain survival of nerve axons Maxillary process originates from the 1st brachial arch and it contains Neurotrophic substances that act on maintaining the survival of nerve axons o No role in directing spread of fibers Neurotrophic substances are important for growth of nerves but they don't determine the direction of this growth o Act on nearby nerves govern late invasion of pulp tissue by nerve fibers Initial nerve fibers are at first located at the base of dental papilla, and then they invade the dental papilla and this invasion is governed by the Neurotrophic substances o Allow permanent teeth to recruit their nerve supply from branches of axons previously supplying deciduous teeth (important!) The axons used to supply the deciduous teeth are not totally lost Some of these axons are recruited and chosen into the permanent successor tooth by the Neurotrophic substances (so that, some of the nervous elements inside the pulps of permanent teeth is actually originating from the primary nervous elements in the deciduous teeth) o Odontoblastic factors promote extension of new nerve fibers into the subodontoblastic layer & dentine in re-implanted teeth Re-implanted tooth = having the tooth out (by accident) and then putting it in back again If lost tooth is maintained in a material like milk or saliva re-implantation can be done After re-implantation is done, Neurotrophic substances allow the re-growth of the nervous elements inside the pulp of these amputated teeth
/104
Dr. Tahani Abualteen
Functions of A fibers: Myelinated Large diameter (1 4 m) Rapidly conducting (>2 m/s) Mediate sharp, piercing pain sensations Responsible for dentinal sensitivity Respond to any stimuli causing fluid movement in dentinal tubules These stimuli include: Drilling, drying & application of osmotic solutions Inside dentine we have tubules that contain fluids and these fluids move up and down inducing pain impulses in A fiber nerves Hydrodynamic theory = stimulation of nerve fibers caused by the movement of fluids up and down inside the dentinal tubules How can we explain the painful feeling when something sweet is eaten and the tooth is carious deep into dentine? - When something sweet is eaten, there will be a change in the osmotic pressure. Why? - Because of caries, dentine is exposed to the oral environment and when something sweet is eaten (and it is very concentrated) there will be movement of fluid from inside dentine toward the sweet area - This movement will activate the nerves; thats why pain is felt
Functions of C fibers: Unmyelinated Small diameter (< 0.5 m) Slowly conducting (< 2 m/s) Polymodal (activated by more than one type of stimulus) o Thermal o Mechanical o Chemical stimuli histamine (increase pain sensation) & bradykinin (decrease pain sensation) Mediate dull, longer standing & less well-localized
Neurotransmitters in dental pulp: Calcitonin gene-related peptide (CGRP) Substance P Neurokinin A
Autonomic nerve supply in the pulp: Autonomic nerve supply (sympathetic & parasympathetic) is needed in dental pulp to control contraction (vasoconstriction) & dilatation (vasodilatation) of smooth muscles found in wall of blood vessels Sympathetic: The majority of autonomic component is sympathetic Some are cholinergic (neurotransmitter found then is acetylcholine not adrenaline) o Removal of superior cervical ganglion (very important sympathetic ganglion in the head & neck region) results in some decrease in cholinesterase staining in the pulp
/105
Dr. Tahani Abualteen
In the mouse: o 1/2 of the sympathetic component is found in the pulp horn o 1/3 of the sympathetic component is found in pulp chamber (pulp inside the crown) o Rest in root canal "pulp inside the root" Functions:
/
o Control pulp blood flow Since they cause vasoconstriction (to decrease amount of blood supply) & when sympathetic nerves aren't working, blood vessels are opened (to increase amount of blood supply) and this is important for: o Regulation of odontogenesis o Afferent transmission of impulses associated with pain sensation Evidences of functions: o Anatomical evidence nerve fibers are located near blood vessels & odontoblasts (because they need to control the contraction of smooth muscles and regulate dentinogenesis) o Sympathectomy (removal of one of the sympathetic ganglia or the whole sympathetic system) lead to vasodilatation & changed in dentine apposition Parasympathetic: The minority of autonomic component is parasympathetic Majority are cholinergic (neurotransmitter found then is acetylcholine not adrenaline) o Removal of inferior alveolar nerve Results in abolishing cholinesterase staining in the pulp Results in increased rate f tooth eruption (due to increased intrapulpal pressure)
Nociceptive response - substance P: Pulp reacts initially if dentine is stimulated: o Electrically or o Mechanically or o Chemically C fibers are stimulated first, and this leads to Retrograde impulses in C branches (those impulses aren't running in normal direction (from peripheral nerves to cerebral cortex) but in the opposite direction) and this causes the Release of substance P at nerve terminals and this leads to o Vasodilatation tissue edema o Release of histamine increase capillary permeability & fluid Extravasation inflammation & conduction of pain
Nociceptive response bradykinin: Noxious stimulation of the pulp (any injury to the dental pulp) leads to Bradykinin formation which leads to o Contribution to vasodilatation o May stimulate release of encephalins from pulpal cells
/106
Dr. Tahani Abualteen
Encephalins are protective anti-inflammatory agents that inhibit bradykinin release by means of negative feedback mechanism (Upon the release of certain or adequate concentration of bradykinin, bradykinin itself activates pulpal cells to release encephalins that inhibit synthesis and release of bradykinin and this is a protective negative feedback mechanism)
Nociceptive response ecosanoid group: They are metabolites of arachidonic acid o Arachidonic acids = group of molecules formed by a cascade of reactions by the aid of cyclooxygenase enzyme o Action of cyclo-oxygenase enzyme is blocked by Aspirin leading to deactivation of the arachnoid acid derivatives and this actually stops pain conduction o The most important metabolites of arachnoid acid are Prostaglandins & Leucotrienes PG I2 is produced by endothelial cells o Inhibits platelet aggregation o Vasodilator Thromboxane A2 produced by platelets & fibroblasts o Stimulate platelet aggregation In the pulp o PG I2, PG F2 , PG E2 o Thromboxane A2 o Leucotrience 12-HETE, LTC4
Nociceptive response prostaglandins: Bacterial/mechanical/chemical irritation cause Increase in prostaglandin F2 & E2 (found in high concentrations in inflamed pulp) which cause o Vasodilatation o Increase pain-producing properties of: Histamine Bradykinin Serotonin
Pain relieving drugs: Aspirin: Inhibitor of cyclo-oxygenase enzyme Inhibitor of PG synthesis Root canal medicaments: o o o o Placed in between visits of root canal treatment to reduce pain Include: Phenol, Chlorophenol, cresol, Thymol, guaiacol Inhibitors of PG & Leucotrienes synthesis Have antibacterial activity
Eugenol More effective than phenols in inhibition of prostaglandin synthesis Mainly used in temporary fillings (zinc oxide and eugenol)
/107
Dr. Tahani Abualteen
Pulpitis & pulp necrosis: Injury to dentine (through cavity preparation for example) will cause: o Nerve fibers & odontoblastic processes to be pulled by a hydrodynamic force (which is the movement of fluids in the dentinal tubules, and which is important to initiate the pain) and this causes them to be o Separated from pulpal tissue and this leads to o Damaging nerve fibers & killing of odontoblasts and so that o Pain in dentine is initiated When injury is small (low intensity stimulus): o Damaged areas are very small odontoblastic layer damage is slight o Reparative dentine may seal off small damaged areas (rate of building exceeds rate of destruction) Blocks re-innervation Innervation of adjacent areas is increased o CGRP (Calcitonin gene-related peptide) from reactive axons promote growth of new fibers o When the lesion heals new fibers disappear When cavity reaches the pulp pulpitis: o Odontoblastic layer is destroyed o Inflammation occurs locally o In small lesions dentine bridge forms inflammation resolves & pulp heals (reversible pulpitis) Mild inflammation (inflammation area demarcated by fibrous tissue) o In large lesions (due to more severe stimuli) no dentine bridge forms inflammation doesn't resolve & pulp doesnt heal and root canal treatment has to be done (irreversible pulpitis) Severe inflammation (inflammation area demarcated by fibrous tissue) Lack of pain at a later stage of pulpitis Patients with irreversible pulpitis may complain of pain for 2-3 days maximum & after this, the pain will disappear and this leads some people to think that the problems is solved, but actually the pulp here is transferring from irreversibly inflamed one into necrotic one
o CGRP (Calcitonin gene-related peptide) mediates growth of new nerve fibers outside inflammation area and this causes Hypersensitivity in early pulpitis Difficulty in achieving anesthesia in a tooth with an inflamed pulp (all signs of anesthesia are perfect but there is still some pain and that's because of the growth of new fibers surrounding the inflamed area so patient needs to bear a little bit of pain just to enter the pulp &eradicates it)
When there is more severe pulpal exposure pulp necrosis: o o o o Irreversible pulpitis (severe inflammation) lead to pulp necrosis if left untreated Necrosis area is demarcated by fibrous tissue CGRP (Calcitonin gene-related peptide) mediates growth of new nerve fibers outside necrosis area Lesion extends to root apex (because pulp and PDL are continuous through apical foramen): Nerve growth in periapical tissue New fibers appear to be involved in pain sensation
/108
Dr. Tahani Abualteen
Pain of dental origin: Exposure of dentine leads to sensitivity initiates pain o Dental caries or cavity preparation o Coronal fractures o Cemental layer wears away Any sensation through exposed dentine will be perceived as pain Heat and cold may be perceived as separate sensations? Because it is found that all sensations felt inside the tooth are perceived only as pain and so, if high or low temperatures are applied on the tooth, temperature won't be felt but pain instead! Temperatures are felt by soft tissues surrounding teeth (e.g. gums, tongue, cheeks, lips) Most sensitive areas in dentine as at o EDJ o Exposed dentine in cervical root areas ** Teeth sensitivity might be treated by fluoride gel application or Sensodyne toothpaste regular use to seal the opened dentinal tubules Nerve fibers to dentine are limited to coronal dentine Nerve fibers are numerous under cusps Nerve fibers extend for a short distance within dentine Odontoblastic processes vary in extension through dentine o Function as receptors
Three theories of dentinal hypersensitivity: 1. Odontoblastic processes as receptors o Odontoblasts are neural crest in origin and function as receptors 2. Nerve fibers extend through dentine a. b. c. d. Direct stimulation of these nerve fibers leads to Deformation of odontoblasts by fluid movement and this Promotes potassium release and this initiates Action potential in neighboring nerve fibers
3. Hydrodynamic theory (the most acceptable) a. Movement of fluids through dentinal tubules inward & outward b. Distortion of nerve endings in Raschkows plexus Referred pain: Referred pain = Pain felt distal to the origin site (and not feeling the pain at site of origin anymore) Sensation of pain resulting from a deep organ peripherally in areas derived from the same somite o Referred pain can't cross the midline o E.g. Pain of cardiac origin may be perceived in the arm o E.g. Toothache may be perceived as headache Convergence of somatic & visceral sensory impulses at one or more of 3 levels o Pre-spinal o Spinal
/109
Dr. Tahani Abualteen
o Supra-spinal Pain Neurons have 3 levels: primary, secondary, tertiary and these neurons have junctions in between them at the pre-spinal, spinal and supra-spinal levels E.g. Heart nerves cross with left shoulder nerves thats why infracted people feel pain in left shoulder Referred oro-facial pain: In trigeminal, levels are o Pre-pontine o Ponto-medullary o Supra-pontine No convergence within brain Pain within the oral cavity is referred o Within the distribution of the specific divisions of the trigeminal nerve o Doesnt cross midline except in ramifications of nerve terminals (at incisor region) Migrainous headache may be due to dental conditions o Not referred pain because it is vascular in origin and it is NOT nerve-related
/1010
You might also like
- Anatomy Physiology and Disease Foundations For The Health Professions 1st Edition Roiger Solutions Manual Full Chapter PDFDocument58 pagesAnatomy Physiology and Disease Foundations For The Health Professions 1st Edition Roiger Solutions Manual Full Chapter PDFrelatermotifef4oq100% (13)
- Reflexology Entire Course in PDFDocument73 pagesReflexology Entire Course in PDFRadu Moglan75% (8)
- Paramahansa Yogananda - Christian Yoga - Supe Advanced Course Number 1 - Lessons 1-12 (163p) (Anomolous)Document163 pagesParamahansa Yogananda - Christian Yoga - Supe Advanced Course Number 1 - Lessons 1-12 (163p) (Anomolous)alvaro93% (15)
- Final - Daphnia Heart Rate ReportDocument15 pagesFinal - Daphnia Heart Rate ReportWill Perkins100% (1)
- Fixed Orthodontic Appliances: A Practical GuideFrom EverandFixed Orthodontic Appliances: A Practical GuideRating: 1 out of 5 stars1/5 (1)
- Morphology of Permanent Molars Class Traits: in Order To Call A Tooth As A Molar It Needs To HaveDocument10 pagesMorphology of Permanent Molars Class Traits: in Order To Call A Tooth As A Molar It Needs To HaveAbod NaserNo ratings yet
- The Nervous System (BDS)Document27 pagesThe Nervous System (BDS)leeminhoangrybirdNo ratings yet
- Beyond Telepathy Andrija PuharichDocument292 pagesBeyond Telepathy Andrija PuharichWild Card100% (1)
- (Personal Note) RPD & FPDDocument2 pages(Personal Note) RPD & FPDAmniAzmi0% (1)
- Hand Out 2021 Restoration of Endodontically Treated TeethDocument40 pagesHand Out 2021 Restoration of Endodontically Treated TeethpriyaNo ratings yet
- My 3rd Seminar - DentinDocument25 pagesMy 3rd Seminar - DentinJon YorkNo ratings yet
- Fixed Partial Denture Cementation and Maintainence: Presented by DR Shubhangi Agrawal Iind Year PGDocument269 pagesFixed Partial Denture Cementation and Maintainence: Presented by DR Shubhangi Agrawal Iind Year PGShubhangi AgrawalNo ratings yet
- A Study On Flexible Dentures PDFDocument9 pagesA Study On Flexible Dentures PDFAnonymous NFiQTb1No ratings yet
- Minor Connector PDFDocument24 pagesMinor Connector PDFghanim alubeidiNo ratings yet
- Gunning SplintsDocument2 pagesGunning Splintsmoondreamerm2No ratings yet
- Pontics: Vaishakhi .Y. Baisane (Ivth Year B.D.S)Document47 pagesPontics: Vaishakhi .Y. Baisane (Ivth Year B.D.S)Vaishakhi BaisaneNo ratings yet
- Restoration of Endodontically Treated TeethDocument17 pagesRestoration of Endodontically Treated TeethAfaf MagedNo ratings yet
- Prognosis of Initial Endodontic Therapy PDFDocument30 pagesPrognosis of Initial Endodontic Therapy PDFRamona MateiNo ratings yet
- Maxillofacial Prosthetics Part-1 A Revie PDFDocument10 pagesMaxillofacial Prosthetics Part-1 A Revie PDFmehak malhotraNo ratings yet
- CPD DesignDocument8 pagesCPD DesignMayuri PatilNo ratings yet
- Provisional RestorationsDocument9 pagesProvisional RestorationsMukhtar AndrabiNo ratings yet
- Occlusion in Implant Prosthodontics: Radhika B Parekh, Omkar Shetty, Rubina TabassumDocument4 pagesOcclusion in Implant Prosthodontics: Radhika B Parekh, Omkar Shetty, Rubina TabassumTung Thanh NguyenNo ratings yet
- Cementation of Indirect Restorations - An Overview of Resin CementsDocument6 pagesCementation of Indirect Restorations - An Overview of Resin CementsNaoki MezarinaNo ratings yet
- 5 - Calcium Hydroxide Vs Mineral Trioxide Aggregates For Partial Pulpotomy of Permanent Molars With Deep Caries PDFDocument6 pages5 - Calcium Hydroxide Vs Mineral Trioxide Aggregates For Partial Pulpotomy of Permanent Molars With Deep Caries PDFAbdul Rahman AlmishhdanyNo ratings yet
- Prosthodontic Stents: March 2019Document28 pagesProsthodontic Stents: March 2019Ahmad WahabNo ratings yet
- Tarnish & CorrosionDocument11 pagesTarnish & CorrosionShahzadi SamanaNo ratings yet
- Recent Advances in DentistryDocument2 pagesRecent Advances in DentistrySudarsan SangeethaNo ratings yet
- Impression Making in CDDocument8 pagesImpression Making in CDAMAN RAJPUTNo ratings yet
- Bonded Composites Versus Ceramic Veneers PDFDocument7 pagesBonded Composites Versus Ceramic Veneers PDFAnnaAffandieNo ratings yet
- 22 Maxillary Posterior Edentulism - Pocket DentistryDocument8 pages22 Maxillary Posterior Edentulism - Pocket DentistryrezaalfessiNo ratings yet
- Insertion Appointment of Complete Dentures: Lec 17 4 GradeDocument15 pagesInsertion Appointment of Complete Dentures: Lec 17 4 GradeSaif Hashim100% (1)
- Management of Alveolar Ridge ResorptionDocument29 pagesManagement of Alveolar Ridge Resorptionفواز نميرNo ratings yet
- Restoration of THE Endodonticall Y Treated Tooth: Amith Babu Amrita Dora Ganesh O.R Praveen J Ourvind SinghDocument100 pagesRestoration of THE Endodonticall Y Treated Tooth: Amith Babu Amrita Dora Ganesh O.R Praveen J Ourvind SinghCahyani CahyaniNo ratings yet
- Centric RelationDocument21 pagesCentric RelationAatish Dilip ShahNo ratings yet
- MNGMNT Gingival TissueDocument7 pagesMNGMNT Gingival TissueHRNo ratings yet
- Cds With and Without FacebowDocument6 pagesCds With and Without FacebowAdarsh varmaNo ratings yet
- Streamline Introduction of PonticsDocument0 pagesStreamline Introduction of PonticsAmar BhochhibhoyaNo ratings yet
- Selection and Arrangement of Teeth For Complete Dentures: By: Dr. Rohan BhoilDocument84 pagesSelection and Arrangement of Teeth For Complete Dentures: By: Dr. Rohan BhoilMaqbul AlamNo ratings yet
- DentinDocument43 pagesDentinHari PriyaNo ratings yet
- Pontic SeminarDocument40 pagesPontic Seminarankita sethiNo ratings yet
- 17 Fracture MechanicsDocument16 pages17 Fracture MechanicsRevathy M NairNo ratings yet
- Osseointegration of Dental ImplantsDocument164 pagesOsseointegration of Dental ImplantsjubinNo ratings yet
- Denture Cleaners (Materi Kuliah)Document13 pagesDenture Cleaners (Materi Kuliah)karinagitakNo ratings yet
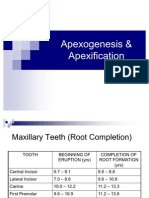
- Apexogenesis & ApexificationDocument35 pagesApexogenesis & ApexificationFaizan Ahmed50% (2)
- Impression Techniques: For Implant ProsthesesDocument38 pagesImpression Techniques: For Implant Prosthesesbaqer hussain0% (1)
- Group Function OcclusionDocument6 pagesGroup Function OcclusionHamad KayaniNo ratings yet
- Anomalies of The Orofacial RegionDocument118 pagesAnomalies of The Orofacial RegionAhmed Barakat100% (1)
- Temporomandibular Disorders and ManagementDocument79 pagesTemporomandibular Disorders and ManagementVijay ChinthaNo ratings yet
- 304 Review ArticleDocument4 pages304 Review ArticleDr Raj Jain100% (1)
- Endodontically - Treated Post& Core System IMPTDocument29 pagesEndodontically - Treated Post& Core System IMPTnoreenmyanmarNo ratings yet
- Stresses Induced by CPD-FinalDocument26 pagesStresses Induced by CPD-FinalNikita AggarwalNo ratings yet
- BiocompatibilityDocument50 pagesBiocompatibilityAysha MohammedaliNo ratings yet
- Residual Ridge ResorptionDocument147 pagesResidual Ridge ResorptionMithileshwari PatilNo ratings yet
- Biocompatible Dental MaterialsDocument12 pagesBiocompatible Dental MaterialsAryant Dentia RNo ratings yet
- Saliva and Its Prosthodontic Implications / Orthodontic Courses by Indian Dental AcademyDocument38 pagesSaliva and Its Prosthodontic Implications / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Muscle DeprogrammerDocument17 pagesMuscle DeprogrammerDilesh PradhanNo ratings yet
- PulpDocument54 pagesPulpAnsh DuttaNo ratings yet
- Post and Core Orthodontic Courses by Indian Dental AcademyDocument46 pagesPost and Core Orthodontic Courses by Indian Dental AcademyPadmini Reddy100% (1)
- Traumatic Injuries Notes 22nk8pfDocument16 pagesTraumatic Injuries Notes 22nk8pfAmee PatelNo ratings yet
- Denture CharacterizationDocument3 pagesDenture CharacterizationDapinder BrarNo ratings yet
- Eriatric Nutrition: A Prosthodontic Review: AsssaasasasssDocument5 pagesEriatric Nutrition: A Prosthodontic Review: AsssaasasasssMaqbul AlamNo ratings yet
- Full Mouth Rehabilitation of A Patient With Ra PDFDocument3 pagesFull Mouth Rehabilitation of A Patient With Ra PDFdehaaNo ratings yet
- Basic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionFrom EverandBasic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionNo ratings yet
- Orthodontic Biomechanics: Treatment Of Complex Cases Using Clear AlignerFrom EverandOrthodontic Biomechanics: Treatment Of Complex Cases Using Clear AlignerNo ratings yet
- InstrumentsDocument21 pagesInstrumentsAbod NaserNo ratings yet
- 2 - Dental PulpDocument9 pages2 - Dental PulpAbod NaserNo ratings yet
- 1 - Introduction To Oral PhysiologyDocument7 pages1 - Introduction To Oral PhysiologyAbod NaserNo ratings yet
- 3 - Development of The RootDocument11 pages3 - Development of The RootAbod NaserNo ratings yet
- Early Embryological Development: Oral Histology Dent 206 DR Ashraf ShaweeshDocument26 pagesEarly Embryological Development: Oral Histology Dent 206 DR Ashraf ShaweeshAbod NaserNo ratings yet
- Sci 10 Week 3 Nervous SystemDocument17 pagesSci 10 Week 3 Nervous SystemNikkha elle Teleron100% (1)
- Unit-Two Biological Bases of BehaviorDocument27 pagesUnit-Two Biological Bases of Behaviorरोशन सिग्देलNo ratings yet
- Adrenergic and Cholinergic Receptors in The HeartDocument2 pagesAdrenergic and Cholinergic Receptors in The HeartRuth CaldwellNo ratings yet
- Male Seadxual Disfunction PDFDocument1,013 pagesMale Seadxual Disfunction PDFAlexandr TrotskyNo ratings yet
- Ultrasound-Guided Nerve Blocks in The Head and Neck For Chronic Pain Management - The Anatomy, Sonoanatomy, and ProcedureDocument16 pagesUltrasound-Guided Nerve Blocks in The Head and Neck For Chronic Pain Management - The Anatomy, Sonoanatomy, and Proceduremarcus moraisNo ratings yet
- 7 - CholinergicsDocument10 pages7 - CholinergicsRaunaq Singh RatraNo ratings yet
- K5 - Disorders of Autonomic Nervous SystemDocument47 pagesK5 - Disorders of Autonomic Nervous SystemDenis Harli SiregarNo ratings yet
- Enteric Nervous System: Physiology 1103Document11 pagesEnteric Nervous System: Physiology 1103Rheum RaponticumNo ratings yet
- Plant and Animal Chemical and Nervous ControlDocument27 pagesPlant and Animal Chemical and Nervous ControlAlnedKirby Carijutan Mendiola100% (1)
- Physiology of ANS Lecture 1 by Dr. Mudassar Ali RoomiDocument19 pagesPhysiology of ANS Lecture 1 by Dr. Mudassar Ali RoomiMudassar RoomiNo ratings yet
- The Nervous System and Reflex Arc (GCSE)Document35 pagesThe Nervous System and Reflex Arc (GCSE)Raja UsamaNo ratings yet
- Several" and Graph Which Means "Writings." Hence, Literally, Polygraph Means ManyDocument34 pagesSeveral" and Graph Which Means "Writings." Hence, Literally, Polygraph Means Manykim ryan uchiNo ratings yet
- 2 2 2 Year 10 Psychology Lesson PlansDocument54 pages2 2 2 Year 10 Psychology Lesson Plansapi-264819644100% (1)
- Science10 Q3 SLM7Document17 pagesScience10 Q3 SLM7PiaNo ratings yet
- Sympathomimetics and SympatholyticsDocument3 pagesSympathomimetics and Sympatholyticsbunso padillaNo ratings yet
- Psychology and Life 20th Edition Gerrig Test BankDocument50 pagesPsychology and Life 20th Edition Gerrig Test BankquwirNo ratings yet
- The Neurophysiology of Acupuncture A ViewpointDocument11 pagesThe Neurophysiology of Acupuncture A ViewpointpedroNo ratings yet
- Endo Lect Adrenal Androgens and Medullary HormonesDocument38 pagesEndo Lect Adrenal Androgens and Medullary HormonesdoctorrfarrukhNo ratings yet
- Psychology 114 Completed PDFDocument80 pagesPsychology 114 Completed PDFGrace AndersonNo ratings yet
- 4TH QUARTER FORMATIVE TEST in SCIENCE 10Document4 pages4TH QUARTER FORMATIVE TEST in SCIENCE 10Wayne GodioNo ratings yet
- Spinal CordDocument38 pagesSpinal CordAsad OsmanNo ratings yet
- Ana NervDocument5 pagesAna NervBrent ValdespinaNo ratings yet
- Chapter 7Document15 pagesChapter 7Bea SeloterioNo ratings yet
- Nervous System ESSENTIAL QUESTIONSDocument8 pagesNervous System ESSENTIAL QUESTIONSAmanuelNo ratings yet