Professional Documents
Culture Documents
Bud 2
Bud 2
Uploaded by
phia29Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bud 2
Bud 2
Uploaded by
phia29Copyright:
Available Formats
UNIVERSITY OF KENTUCKY HOSPITAL CHANDLER MEDICAL CENTER
POLICY NUMBER: PH-06-07 FIRST ISSUED: 4/94 CURRENT AS OF: 1/12
Department of Pharmacy Policy
SUBJECT: PURPOSE: Beyond-Use Dating and Labeling
This policy is designed to ensure that all pharmacy prepared sterile products bear an appropriate beyond-use date.
1.
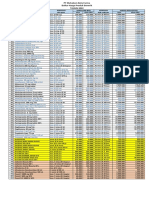
The beyond-use date assigned to sterile products should be based on currently available drug stability information and sterility considerations. Sources of drug stability information include references (e.g., Remingtons Pharmaceutical Sciences, Extended Stability for Parenteral Drugs, The Handbook on Injectable Drugs, Micromedex), manufacturer recommendations, and reliable, published research. When interpreting published drug stability information, the pharmacist should consider all aspects of the final sterile product being prepared (e.g., drug reservoir, drug concentration, storage conditions). 1.1. In the absence of passing additional sterility test (USP 71), the beyond use dates cannot exceed the following time periods before administration. Unless specified differently by the manufacturer or references, beyond-use dates are assigned according to the risk of contamination and storage conditions as outlined in the following table: Room Temp (15-30 degrees C) 1 hour 48 hours 12 hours 30 hours 24 hours Refrigerated Temp (2-8 degrees C) 1 hour 14 days 12 hours 7 days 3 days Frozen Solid-State (< -10 degrees C) N/A 45 days N/A 45 days 45 days
Immediate-Use Low Risk Low-Risk with 12-hour BUD Medium Risk High Risk 1.2.
Immediate-use compounding will: 1.2.1. Apply to any CSP for parenteral administration (IV, inhalation, IM, SQ, etc) prepared outside of an ISO Class 5 environment without terminal sterilization. Antineoplastic agents shall not be prepared outside of pharmacy. 1.2.2. Be reserved for emergent compounded sterile products only 1.2.3. Be compounded in an uncluttered environment free of bodily fluids with low traffic flow. Ideal aseptic technique shall be used to minimize contamination including the swiping of isopropyl alcohol on critical sites and the appropriate use of filter needles for ampules
1.2.4. Be labeled with the product, diluents, date and time prepared, concentration, and initials of compounder. 1.2.5. Shall be kept on the compounder or within close proximity until administered 1.2.6. Be appropriately disposed of if not used within 1 hour. 2. 2.1. Compounded sterile products (CSPs) prepared under all of the following conditions are at a LOW RISK of contamination 2.1.1. CSPs compounded from sterile commercial drugs using commercial sterile devices. 2.1.2. The CSPs are compounded with aseptic manipulations entirely within ISO Class 5 laminar airflow workbench, hood or barrier isolator using only sterile ingredients, products, components and devices. 2.1.3. Located in a ISO Class 7 buffer room with ISO class 8 ante area. 2.1.4. The compounding involves only transfer, measuring and mixing manipulations with closed or sealed packaging systems that are performed promptly and attentively, e.g., no prolonged interruptions. 2.1.5. Examples include reconstitution of single-dose vials of antibiotics or other small-volume parenterals, preparation of hydration solutions.
2.2.
Compounded sterile products (CSPs) prepared under all of the follwing conditions are at a MEDIUM RISK of contamination 2.2.1. Admixtures compounded using multiple additives and/or small volumes 2.2.2. Batch preparations (e.g., syringes) 2.2.3. Complex manipulations (e.g., TPNs or multiple ingredient CSPs) 2.2.4. Compounding occurs over a prolonged period of time (complex procedures). 2.2.5. No bacteriostatic agents are added to the preparation and it is administered over several days (e.g., chemotherapy or pain management administered via a infusion device. 2.2.6. The CSPs are compounded with aseptic manipulations entirely within ISO Class 5 laminar airflow workbench, hood or barrier isolator using only sterile ingredients, products, components and devices.
2.2.7. Located in a ISO Class 7 buffer room with ISO Class 8 ante area. 2.2.8. Examples include pooled admixtures (CSPs made from bulk vials), parenteral nutrition solutions using automated compounders, batch compounded preparations that dont contain bacteriostatic components. 2.3. Compounded sterile products (CSPs) prepared under all of the following conditions are at a HIGH RISK of contamination 2.3.1. Prepared from non-sterile (bulk powders) ingredients 2.3.2. Open system transfers 2.3.3. Non-sterile preparations that are exposed for at least 6hrs before being sterilized. 2.3.4. Preparation from sterile ingredients but exposed to less than ISO Class 5. 2.3.5. Located in a ISO Class 7 buffer room with separate ante area or . 2.3.6. Examples include CSPs prepared from bulk, nonsterile components (e.g., neomycin irrigation, concentrated morphine, alum irrigation) or final containers that are nonsterile and must be terminally-sterilized. 3. Sterile products should be labeled with at least the following information: 3.1. For patient specific products: the patients name and any other appropriate patient identification (e.g., location, identification number); for batch-prepared products: control or lot number; All solutions and ingredient names, amounts, strength, and concentrations (when applicable); Beyond-use date and time
3.2.
3.3.
3.4.
Prescribed administration regimen, when appropriate (including rate and route of administration); Appropriate auxiliary labeling (including precautions); 3.5.1. An overfill label stating 1ml syringes have 0.05ml overfill should be placed on the outside bag containing 1ml syringe doses to alert the nurse of the overfill.
3.5.
3.6. 3.7.
Storage requirements; Identification (e.g., assigned pharmacy identification, P#/ T#/R# of the responsible pharmacists, technician or resident, respectively); Device-specific instructions (when appropriate); and Any additional information, in accordance with state or federal requirements.
3.8. 3.9. 4.
Labels should be legible and affixed to the final container in a manner enabling it to be read while the sterile product is being administered (when possible).
Approved by:
Philip Schwieterman, PharmD Infusion Center/Sterile Products Manager
Rebecca Reagan, PharmD Associate Director, Center Pharmacy Services
Gary Johnson, MBA, PharmD Enterprise Pharmacy Director
You might also like
- Handbook of Microbiological Criteria for FoodsFrom EverandHandbook of Microbiological Criteria for FoodsNo ratings yet
- Good Manufacturing Practices (GMP) Modules for Pharmaceutical ProductsFrom EverandGood Manufacturing Practices (GMP) Modules for Pharmaceutical ProductsNo ratings yet
- Storage of MedicationsDocument8 pagesStorage of MedicationsRawan AlanaziNo ratings yet
- Internship Exercises 8-10Document25 pagesInternship Exercises 8-10JumelConingNo ratings yet
- Interpersonal Communication in Pharmaceutical CareDocument9 pagesInterpersonal Communication in Pharmaceutical Carephia29No ratings yet
- Metformin MetforminDocument6 pagesMetformin Metforminphia29No ratings yet
- Phil National Drug PolicyDocument32 pagesPhil National Drug Policyapi-374348390% (20)
- LVPDocument5 pagesLVPBüşra BaşoğluNo ratings yet
- Parenteral Preparations: Water For InjectionsDocument4 pagesParenteral Preparations: Water For InjectionsSonu SharmaNo ratings yet
- 15 Parenteral S ReportingDocument9 pages15 Parenteral S ReportingRastie CruzNo ratings yet
- NIP-MOP-Booklet 5Document22 pagesNIP-MOP-Booklet 5Kathryn Jan DomingoNo ratings yet
- USP General Frequently Asked QuestionsDocument14 pagesUSP General Frequently Asked QuestionsPraveen KumarNo ratings yet
- Chemotherapy and Other Hazardous Drugs Safe Use Guidelines: I. II. Iii. IV. V. VI. Vii. Viii. IX. XDocument13 pagesChemotherapy and Other Hazardous Drugs Safe Use Guidelines: I. II. Iii. IV. V. VI. Vii. Viii. IX. XVette Angelikka Dela CruzNo ratings yet
- Usp 797GCDocument61 pagesUsp 797GCAwni1989No ratings yet
- 4 Module 3 - Improving Patient Safety and ComplianceDocument6 pages4 Module 3 - Improving Patient Safety and ComplianceSaman VithanageNo ratings yet
- Antimicrobial Effectiveness Testing GoodDocument3 pagesAntimicrobial Effectiveness Testing Goodmingsu1156No ratings yet
- %USP 32%-51.mETODO DE EFECTIVIDAD DE ANTIMICROBIANOSDocument5 pages%USP 32%-51.mETODO DE EFECTIVIDAD DE ANTIMICROBIANOScolve87No ratings yet
- 17 - Sterile ProductsDocument28 pages17 - Sterile Productsygaber13No ratings yet
- Aseptic RichDocument82 pagesAseptic RichMohammedNo ratings yet
- Compounding ExtemperaneousDocument48 pagesCompounding Extemperaneousedunation024No ratings yet
- Assisting Small Scale CompoundingDocument55 pagesAssisting Small Scale CompoundingAberaNo ratings yet
- Open Vial Policy - 15th Feb 2013Document4 pagesOpen Vial Policy - 15th Feb 2013drnareshchauhanNo ratings yet
- Martin de Rosales DiaposDocument32 pagesMartin de Rosales DiaposFlorentina yohana ngeluNo ratings yet
- Ampicillin 30 G: IndustryDocument2 pagesAmpicillin 30 G: IndustryKATHENo ratings yet
- Pharmacy Prepared Ophthalmic Products 1Document2 pagesPharmacy Prepared Ophthalmic Products 1Upik MoritaNo ratings yet
- Paed - Group Work 1 For BMSEDocument27 pagesPaed - Group Work 1 For BMSERwapembe StephenNo ratings yet
- Standards For The Establishement and Practice of Pharmaceutical Compounding LaboratoryDocument12 pagesStandards For The Establishement and Practice of Pharmaceutical Compounding LaboratorydaritiNo ratings yet
- Preservative Efficacy TestingDocument3 pagesPreservative Efficacy TestingrambhadesiNo ratings yet
- Research - Handling Anti Cancer DrugsDocument43 pagesResearch - Handling Anti Cancer DrugsSunshine BNo ratings yet
- Software For Chemistry Water Device Testing: Biologics 1041Document6 pagesSoftware For Chemistry Water Device Testing: Biologics 1041Naveen KusumaNo ratings yet
- 〈797〉 Pharmaceutical Compounding-Sterile PreparationsDocument33 pages〈797〉 Pharmaceutical Compounding-Sterile PreparationsTri Wahyuni Iskandar PutriNo ratings yet
- Manufacture of Non-Sterile ProductsDocument15 pagesManufacture of Non-Sterile ProductsDev SudersanNo ratings yet
- Us P 797 Pharmaceutical Compounding Sterile CompoundingDocument61 pagesUs P 797 Pharmaceutical Compounding Sterile Compoundingdeepa_ragu5695No ratings yet
- WHO Policy Statement - The Use of Opened Multi-Dose Vials of Vaccine in Subsequent Immunization SessionsDocument13 pagesWHO Policy Statement - The Use of Opened Multi-Dose Vials of Vaccine in Subsequent Immunization SessionscristineNo ratings yet
- Microbial Contamination and GMP-Second LectureDocument22 pagesMicrobial Contamination and GMP-Second Lecturenadesansudhakar100% (1)
- Ways of Protecting Yourself From Acquiring InfectionDocument3 pagesWays of Protecting Yourself From Acquiring InfectionYan CancinoNo ratings yet
- Package Insert - COMIRNATYDocument21 pagesPackage Insert - COMIRNATYChase O'SeaNo ratings yet
- WHO IVB 14.07 EngDocument14 pagesWHO IVB 14.07 EnggineNo ratings yet
- 〈51〉 ANTIMICROBIAL EFFECTIVENESS TESTINGDocument3 pages〈51〉 ANTIMICROBIAL EFFECTIVENESS TESTINGevct1989No ratings yet
- USP 43 - Chapter 51 ANTIMICROBIAL EFFECTIVENESS TESTINGDocument3 pagesUSP 43 - Chapter 51 ANTIMICROBIAL EFFECTIVENESS TESTINGChetalee NaikNo ratings yet
- Musango2015: ST NDDocument9 pagesMusango2015: ST NDKeith OmwoyoNo ratings yet
- USP General Chapter : Pharmaceutical Compounding - Sterile PreparationsDocument37 pagesUSP General Chapter : Pharmaceutical Compounding - Sterile PreparationsMutiara Hasanah100% (1)
- Chapter 17 Sterile ProductsDocument28 pagesChapter 17 Sterile ProductsM Imran SajidNo ratings yet
- Chapter 17Document21 pagesChapter 17Kena SamuelNo ratings yet
- Asean Stability Guideline 2013Document42 pagesAsean Stability Guideline 2013Ani Andriani75% (4)
- Opthalmic PreparationsDocument8 pagesOpthalmic PreparationsprasanthiNo ratings yet
- Chemo Drugs HandlingDocument26 pagesChemo Drugs HandlingSooraj ThomasNo ratings yet
- Parenteral Preparations, Challenges in Formulations Pharmaceutical Outsourcing - The Journal of Pharmaceutical & BiopharmaceutDocument1 pageParenteral Preparations, Challenges in Formulations Pharmaceutical Outsourcing - The Journal of Pharmaceutical & BiopharmaceutCRYSTAL A. ARIETANo ratings yet
- Official: Á51Ñ Antimicrobial Effectiveness TestingDocument3 pagesOfficial: Á51Ñ Antimicrobial Effectiveness TestingKaren Rojas LópezNo ratings yet
- Startvac Epar Product Information enDocument20 pagesStartvac Epar Product Information enVo Thanh ThinNo ratings yet
- 7blm2a enDocument18 pages7blm2a enShaheen AlamNo ratings yet
- USP General Chapter : Pharmaceutical Compounding - Sterile PreparationsDocument37 pagesUSP General Chapter : Pharmaceutical Compounding - Sterile PreparationsRRR1No ratings yet
- Suppositories and Pessaries - Siti Amirah Hakimah Binti Mohd Fairuz (2062191008)Document7 pagesSuppositories and Pessaries - Siti Amirah Hakimah Binti Mohd Fairuz (2062191008)amrhkmhNo ratings yet
- Containers Within The Section Volume in Container. The Text, Which Is Being Published in This Issue of PFDocument11 pagesContainers Within The Section Volume in Container. The Text, Which Is Being Published in This Issue of PFYuzark GumintangNo ratings yet
- 8 - Sterile PreparationsDocument102 pages8 - Sterile PreparationsAlma Grace MenianoNo ratings yet
- IQA QW 200511 The Pharmaceutical ProcessDocument7 pagesIQA QW 200511 The Pharmaceutical ProcessDavide MoggeNo ratings yet
- Vaccine Preparation and-Administration-Workflow-PfizerDocument4 pagesVaccine Preparation and-Administration-Workflow-PfizerChona LopezNo ratings yet
- 4 - Extemporanous CompoundingDocument21 pages4 - Extemporanous Compoundingygaber13No ratings yet
- Open Vial Policy - MoHFW - Sep2015Document6 pagesOpen Vial Policy - MoHFW - Sep2015SaumyaNo ratings yet
- Bud - Labeling PrescriptionsDocument15 pagesBud - Labeling PrescriptionsUsna AprilianaNo ratings yet
- Development and Manufacturing of Injectable (Parenteral) Drug Products UnitDocument10 pagesDevelopment and Manufacturing of Injectable (Parenteral) Drug Products UnitParul SrivastavaNo ratings yet
- Manual for the Implementation of Environmental, Health, and Safety Standards for the Control of Locusts: December 2021From EverandManual for the Implementation of Environmental, Health, and Safety Standards for the Control of Locusts: December 2021No ratings yet
- Frame Formulation NumberDocument2 pagesFrame Formulation Numberphia29No ratings yet
- Spesiasi Logam Berat Di Sediimen Muara KarangDocument1 pageSpesiasi Logam Berat Di Sediimen Muara Karangphia29No ratings yet
- Is Doa 10 Cup TestDocument1 pageIs Doa 10 Cup TestUqi.No ratings yet
- JSS College of Pharmacy: Training and Placement CellDocument3 pagesJSS College of Pharmacy: Training and Placement CellMeghan MamillapalliNo ratings yet
- NCM 106 Quiz 1Document4 pagesNCM 106 Quiz 1poleene de leonNo ratings yet
- Dangerous DrugsDocument9 pagesDangerous DrugsEarvin Recel GuidangenNo ratings yet
- Pharmacology Paper-Ii: Final Exam National Board of Examinations December 2017Document2 pagesPharmacology Paper-Ii: Final Exam National Board of Examinations December 2017Ashok JainNo ratings yet
- Clinical Pharmacology of The Antihelminthic Drugs: Katzung, Bertram G. Basic & Clinical Pharmacology. New York: LangeDocument16 pagesClinical Pharmacology of The Antihelminthic Drugs: Katzung, Bertram G. Basic & Clinical Pharmacology. New York: LangeGrant Wynn ArnucoNo ratings yet
- Anti Emetic DrugsDocument3 pagesAnti Emetic Drugs033-Akanksha KishoreNo ratings yet
- 13 Chapter 5Document64 pages13 Chapter 5yoganaNo ratings yet
- Drug Interactions-Principles Examples and ClinicalDocument13 pagesDrug Interactions-Principles Examples and ClinicalRaudhatul JannahNo ratings yet
- Stock 310122Document24 pagesStock 310122AfifahNo ratings yet
- Project NewDocument31 pagesProject NewDrGajanan VaishnavNo ratings yet
- Recent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A ReviewDocument18 pagesRecent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A Reviewmalik003No ratings yet
- ADMEDocument10 pagesADMEdhavalNo ratings yet
- Additional Information Form - Real Active CureDocument4 pagesAdditional Information Form - Real Active Curekhaleel HasanNo ratings yet
- Appendix 14 - Guideline On MIV Applications For Chemical DrugsDocument0 pagesAppendix 14 - Guideline On MIV Applications For Chemical DrugsWilliam ChandraNo ratings yet
- B. Pharmacy Project List 2020-2021: Sl. No Project Supervisor Reg. No Students Title of The Project DepartmentDocument3 pagesB. Pharmacy Project List 2020-2021: Sl. No Project Supervisor Reg. No Students Title of The Project DepartmentanandNo ratings yet
- DrugsDocument5 pagesDrugsErkzNo ratings yet
- Formulation Development and Evaluation of Sustained Release Tablet Chlorpromazine HCLDocument7 pagesFormulation Development and Evaluation of Sustained Release Tablet Chlorpromazine HCLWJPSR JournalNo ratings yet
- PCPDocument19 pagesPCPJafer DetamoNo ratings yet
- AGUSTUSDocument35 pagesAGUSTUSYogie 1290No ratings yet
- Daftar Harga Produk Generik 2022 New (DITEMPEL)Document1 pageDaftar Harga Produk Generik 2022 New (DITEMPEL)Ade IrawanNo ratings yet
- Clinical PharmacokineticsDocument36 pagesClinical PharmacokineticsDr.U.P.Rathnakar.MD.DIH.PGDHM80% (5)
- General Pharmacology 1Document59 pagesGeneral Pharmacology 1Ramadi PrameelaNo ratings yet
- MEIDocument45 pagesMEIFebri FernandoNo ratings yet
- Retriksi BPJS KronisDocument3 pagesRetriksi BPJS KronisRevi GustriniNo ratings yet
- NCM 212 - Drug Approval ProcessDocument8 pagesNCM 212 - Drug Approval ProcessLYRIZZA LEA BHEA DESIATANo ratings yet
- Antibiotic Cross-Sensitivity ChartDocument1 pageAntibiotic Cross-Sensitivity ChartChing JuNo ratings yet
- Approved Moh Guidelines On Submission of Documentation For Registration of Human Pharmaceutical Products RwandaDocument436 pagesApproved Moh Guidelines On Submission of Documentation For Registration of Human Pharmaceutical Products RwandaAry Bima WinardoNo ratings yet
- Evaluation of Quality of A Drug Product: Prepared and Presented byDocument22 pagesEvaluation of Quality of A Drug Product: Prepared and Presented byAlekhya GuntupalliNo ratings yet