Professional Documents
Culture Documents
Metoclopromide Reglan
Metoclopromide Reglan
Uploaded by
Nico TiuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metoclopromide Reglan
Metoclopromide Reglan
Uploaded by
Nico TiuCopyright:
Available Formats
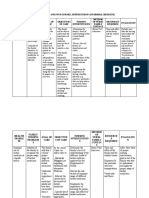
Mechanism of Action: The antiemetic properties of metoclopramide appear to be a result of its antagonism of central and peripheral dopamine receptors.
Dopamine produces nausea and vomiting by stimulation of the medullary chemoreceptor trigger zone (CTZ), and metoclopramide blocks stimulation of the CTZ by agents like l-dopa or apomorphine which are known to increase dopamine levels or to possess dopamine-like effects. Metoclopramide also abolishes the slowing of gastric emptying caused by apomorphine. Like the phenothiazines and related drugs, which are also dopamine antagonists, metoclopramide produces sedation and may produce extrapyramidal reactions, although these are comparatively rare. Metoclopramide inhibits the central and peripheral effects of apomorphine, induces release of prolactin and causes a transient increase in circulating aldosterone levels, which may be associated with transient fluid retention. The onset of pharmacological action of metoclopramide is 1 to 3 minutes following an intravenous dose, 10 to 15 minutes following intramuscular administration, and 30 to 60 minutes following an oral dose; pharmacological effects persist for 1 to 2 hours. Dosage - Children: Gastroesophageal reflux: Oral: 0.1-0.2 mg/kg/dose up to 4 times/day; efficacy of continuing metoclopramide beyond 12 weeks in reflux has not been determined; total daily dose should not exceed 0.5 mg/kg/day Gastrointestinal hypomotility (gastroparesis): Oral, I.M., I.V.: 0.1 mg/kg/dose up to 4 times/day, not to exceed 0.5 mg/kg/day Antiemetic (chemotherapy-induced emesis) (unlabeled): I.V.: 1-2 mg/kg 30 minutes before chemotherapy and every 2-4 hours, for a total of 5 doses (5-10 mg/kg) daily Post-pyloric feeding tube placement (unlabeled) : I.V.: <6 years: 0.1 mg/kg. 6-14 years: 2.5-5 mg. Dosage - Adults: Gastroesophageal reflux: Oral: 10-15 mg/dose up to 4 times/day 30 minutes before meals or food and at bedtime; single doses of 20 mg are occasionally needed for provoking situations Gastrointestinal hypomotility (gastroparesis): Oral: 10 mg 30 minutes before each meal and at bedtime for 2-8 weeks. I.V. (for severe symptoms): 10 mg over 1-2 minutes; 10 days of I.V. therapy may
be necessary for best response Antiemetic (chemotherapy-induced emesis) (unlabeled) : I.V.: 1-2 mg/kg 30 minutes before chemotherapy and every 2-4 hours, for a total of 5 doses (5-10 mg/kg) daily Postoperative nausea and vomiting (unlabeled) : I.M., I.V.: 10 mg near end of surgery; 20 mg doses may be used Post-pyloric feeding tube placement (unlabeled): I.M., I.V.: 10 mg Elderly: Gastroesophageal reflux: Oral: 5 mg 4 times/day (30 minutes before meals and at bedtime); increase dose to 10 mg 4 times/day if no response at lower dose Gastrointestinal hypomotility: Oral: Initial: 5 mg 30 minutes before meals and at bedtime for 2-8 weeks; increase if necessary to 10 mg doses. I.V.: Initiate at 5 mg over 1-2 minutes; increase to 10 mg if necessary Postoperative nausea and vomiting (unlabeled): I.M.: 5 mg near end of surgery; may repeat dose if necessary Dosing adjustment in renal impairment: Clcr 10-40 mL/minute: Administer at 50% of normal dose Clcr<10 mL/minute: Administer at 25% of normal dose Hemodialysis: Not dialyzable (0% to 5%); supplemental dose is not necessary Supplied Injection, solution, as hydrochloride (Reglan): 5 mg/mL (2 mL, 10 mL, 30 mL). Syrup, as hydrochloride: 5 mg/5 mL (10 mL, 480 mL) [some products contain sodium benzoate; sugar free] Tablet, as hydrochloride (Reglan): 5 mg, 10 mg
You might also like
- Sample Ultrasound ReportDocument3 pagesSample Ultrasound ReportPapadove0% (1)
- Becoming Cancer-Free ManuscriptDocument149 pagesBecoming Cancer-Free ManuscriptD100% (1)
- Autonomic Nervous System Drugs Simple Complement Type QuestionsDocument11 pagesAutonomic Nervous System Drugs Simple Complement Type QuestionsIrina Panciu Stefan100% (1)
- Safety Injectables WorkbookDocument110 pagesSafety Injectables Workbookgeraffe94% (18)
- MetoclopramideDocument3 pagesMetoclopramideapi-3797941100% (1)
- Metoclopramide DiclofenacDocument7 pagesMetoclopramide DiclofenacRasco, Allen jayNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- V. Phenothiazines (ALIPHATIC)Document3 pagesV. Phenothiazines (ALIPHATIC)Christine Pialan SalimbagatNo ratings yet
- Phenytoin Dosage: Usual Adult Dose For SeizuresDocument4 pagesPhenytoin Dosage: Usual Adult Dose For SeizuresHarish Ayu LNo ratings yet
- PP ObatDocument7 pagesPP ObatSaifan AbdurrohmanNo ratings yet
- Drug CardsDocument3 pagesDrug CardsDave HillNo ratings yet
- Metformin Hydrochloride PDFDocument4 pagesMetformin Hydrochloride PDFHannaNo ratings yet
- Metoclopramide HCL Metoclopramide Inj 10mg-2ml IreDocument7 pagesMetoclopramide HCL Metoclopramide Inj 10mg-2ml IresiripNo ratings yet
- Mot Ilium TabDocument11 pagesMot Ilium TabChandra FatmaNo ratings yet
- Prokinin Tablet & Susp Patient Information LeafletDocument1 pageProkinin Tablet & Susp Patient Information Leafletpharmacia1.comNo ratings yet
- Antiemetic Drugs: Dr. Jatin DhananiDocument31 pagesAntiemetic Drugs: Dr. Jatin DhananiRiddhi JainNo ratings yet
- For Drug Recitation 1Document33 pagesFor Drug Recitation 1Abigail LonoganNo ratings yet
- Keterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugDocument7 pagesKeterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugEm Hernandez AranaNo ratings yet
- Emestop PDFDocument6 pagesEmestop PDFDr.2020No ratings yet
- MetoclopramideDocument1 pageMetoclopramideMichael Kuzbyt100% (1)
- Morphine SulfateDocument4 pagesMorphine SulfateWAQAS AHMADNo ratings yet
- ANTIEMETICSDocument26 pagesANTIEMETICSkhurshidghorihumaNo ratings yet
- 07 Miscellaneous Drugs Group ADocument64 pages07 Miscellaneous Drugs Group AKamal GhimireNo ratings yet
- ImipramineDocument6 pagesImipramineMuhammed Faruk JambazNo ratings yet
- Morphine IV Neomedv2.0 Full 20170518Document5 pagesMorphine IV Neomedv2.0 Full 20170518RanggaDyantoNo ratings yet
- RBCH - PHT Aminophylline Loading Dose GuidelinesDocument2 pagesRBCH - PHT Aminophylline Loading Dose GuidelinesAdrian PrasetioNo ratings yet
- REGLAN Injection (Metoclopramide Injection, USP) RX OnlyDocument15 pagesREGLAN Injection (Metoclopramide Injection, USP) RX OnlydpkkrsterNo ratings yet
- Hyperemesis Gravidarum: DefinitionDocument3 pagesHyperemesis Gravidarum: DefinitiondrpinnakavamsiNo ratings yet
- Levofloxacin-1Document31 pagesLevofloxacin-1Fallen AngelNo ratings yet
- Antidiarrhoeal DrugsDocument15 pagesAntidiarrhoeal DrugsJyoti SidhuNo ratings yet
- 03 Tocolytics Group ADocument39 pages03 Tocolytics Group AKamal GhimireNo ratings yet
- Hemostan, Methergine CA Gluconate2Document4 pagesHemostan, Methergine CA Gluconate2Stacy MC PelitoNo ratings yet
- HaloperidolDocument2 pagesHaloperidolJordhy ReynaldNo ratings yet
- jbsnisdfbefbeijnfefDocument20 pagesjbsnisdfbefbeijnfefdewi khurmiNo ratings yet
- Preanesthetic Medication JasminaDocument44 pagesPreanesthetic Medication Jasminaanjali sNo ratings yet
- Preanesthetic Medication JasminaDocument44 pagesPreanesthetic Medication Jasminaanjali s100% (1)
- Preanesthetic Medication JasminaDocument44 pagesPreanesthetic Medication Jasminaanjali sNo ratings yet
- AntifungalDocument7 pagesAntifungalKhor Chin PooNo ratings yet
- Management of Severe Ulcerative Colitis: DR - Siddharth SinghDocument21 pagesManagement of Severe Ulcerative Colitis: DR - Siddharth SinghLohith VakacherlaNo ratings yet
- PCM PoisonDocument23 pagesPCM PoisonPrabhat KcNo ratings yet
- Theophylline PDFDocument3 pagesTheophylline PDFWindy Gigiers SeptianiNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs (Nsaids)Document46 pagesNonsteroidal Anti-Inflammatory Drugs (Nsaids)b3djo_76No ratings yet
- Paracetamol Poisoning: G. Rajapandi 521625111 Final MbbsDocument18 pagesParacetamol Poisoning: G. Rajapandi 521625111 Final MbbsAntony PrakashNo ratings yet
- Pain Pocket GuideDocument2 pagesPain Pocket Guidebtalera100% (2)
- Obat AnestesiDocument9 pagesObat AnestesiNatanael SusantoNo ratings yet
- AcetylcystineDocument2 pagesAcetylcystineJoevith FalabiNo ratings yet
- Less 2 Hrs After Meal: Goals For Blood Glucose Levels During Pregnany: 95 MG/DL or Less Before Meals and 120 MG/DL orDocument6 pagesLess 2 Hrs After Meal: Goals For Blood Glucose Levels During Pregnany: 95 MG/DL or Less Before Meals and 120 MG/DL orspain michaelisNo ratings yet
- Magnesium Sulfate - Drug InformationDocument10 pagesMagnesium Sulfate - Drug InformationLuisEnriqueDeLaCruzSolanoNo ratings yet
- TheophyllineDocument6 pagesTheophyllineapi-3797941100% (1)
- Clostridium Difficile Guideline - UMMCDocument5 pagesClostridium Difficile Guideline - UMMCdamondouglas100% (3)
- HTAR FormularyDocument204 pagesHTAR FormularyMay TanNo ratings yet
- Cloxacillin and inDocument6 pagesCloxacillin and inGabb CabigtingNo ratings yet
- Enalapril (Vasotec ®) :: Dosing (Adults)Document9 pagesEnalapril (Vasotec ®) :: Dosing (Adults)Ica Joy ArandiaNo ratings yet
- Mefenamic AcidDocument3 pagesMefenamic AcidVaibhav MehtaNo ratings yet
- GIT DrugsDocument180 pagesGIT DrugsMaria Linevel Balderamos Dalida100% (1)
- Drug StudyDocument10 pagesDrug StudybaniniycsebNo ratings yet
- To Control Nausea and Vomiting: Drug StudyDocument2 pagesTo Control Nausea and Vomiting: Drug StudyPeace Andong PerochoNo ratings yet
- Azathioprine: Class: IndicationsDocument3 pagesAzathioprine: Class: IndicationsAnna GozaliNo ratings yet
- Valproic AcidDocument5 pagesValproic AcidMark PradsNo ratings yet
- Keto LogDocument7 pagesKeto LogKim Justin InfantadoNo ratings yet
- Drug StudyDocument10 pagesDrug StudyFranco ObedozaNo ratings yet
- PhenytoinDocument6 pagesPhenytoinapi-3797941100% (1)
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Deborah Stover RN ResumeDocument2 pagesDeborah Stover RN Resumeapi-479158a34fNo ratings yet
- New Possibilities On The Application of Violet Light in Dentistry Combining Aesthetics and Microbiological Control Report of Two Clinical CasesDocument10 pagesNew Possibilities On The Application of Violet Light in Dentistry Combining Aesthetics and Microbiological Control Report of Two Clinical CasesAthenaeum Scientific PublishersNo ratings yet
- Lecture 8 Expectorants and Emetics, IntroductionDocument6 pagesLecture 8 Expectorants and Emetics, IntroductionAmrit Sareen100% (3)
- Apf Clinic Aftercare InstructionsDocument4 pagesApf Clinic Aftercare InstructionsapNo ratings yet
- Hematenics Vitamins How To ChooseDocument27 pagesHematenics Vitamins How To ChooseRohit BharadwajNo ratings yet
- Reflection'brain On FireDocument2 pagesReflection'brain On FireJevelyn AgdolNo ratings yet
- Ocular Prosthesis Case HistoryDocument5 pagesOcular Prosthesis Case HistorydrsmritiNo ratings yet
- Summary of The Scientific Literature For Pain and Anxiety Control DentistryDocument10 pagesSummary of The Scientific Literature For Pain and Anxiety Control DentistrySri Ram Kumar スリランカラムクマーNo ratings yet
- Community HealthDocument4 pagesCommunity HealthwhitNo ratings yet
- Adult ImmunizationDocument2 pagesAdult ImmunizationSMRNo ratings yet
- Men, Women, and Depression - Undoing DepressionDocument3 pagesMen, Women, and Depression - Undoing DepressionlabebuNo ratings yet
- Oral Pathology, Lecture 1Document64 pagesOral Pathology, Lecture 1ameer mousaNo ratings yet
- Necrotizing Soft Tissue InfectionsDocument29 pagesNecrotizing Soft Tissue InfectionsMoritz SolivenNo ratings yet
- Case Study Intestinal ParasitismDocument16 pagesCase Study Intestinal Parasitismjean therese100% (3)
- ARTIC MouldChart 2017 220623 162138Document8 pagesARTIC MouldChart 2017 220623 162138adellya tasya sukmaNo ratings yet
- Spesifikasi KALTECH KUC-2D + Probe ConvexDocument3 pagesSpesifikasi KALTECH KUC-2D + Probe Convexspip meranginNo ratings yet
- Gallblad DER: ImagingDocument45 pagesGallblad DER: ImagingBohna FranciscoNo ratings yet
- Ertapenem Package Insert PDFDocument2 pagesErtapenem Package Insert PDFDavidNo ratings yet
- Acute Nerve InjuryDocument28 pagesAcute Nerve InjuryEdgar RobledoNo ratings yet
- Medication Errors in The ElderlyDocument7 pagesMedication Errors in The Elderlysalaheldin elabiadNo ratings yet
- Sports-Related InjuriesDocument2 pagesSports-Related Injurieslil trxshNo ratings yet
- Computation and FNCPDocument3 pagesComputation and FNCPWinnie AriolaNo ratings yet
- Condylar HyperplasiaDocument20 pagesCondylar HyperplasiaSamuel Flores CalderonNo ratings yet
- Gen Bio 2 LAW Q4 Week 3 4 (AutoRecovered)Document12 pagesGen Bio 2 LAW Q4 Week 3 4 (AutoRecovered)Samantha DomileNo ratings yet
- Impetigo and CHMDocument2 pagesImpetigo and CHMcbrammah9357No ratings yet
- Printout - Fever and Abd Pain - Causes and DiagnosisDocument7 pagesPrintout - Fever and Abd Pain - Causes and DiagnosisgianneNo ratings yet