Professional Documents
Culture Documents
Injury To The Colon and Rectum
Injury To The Colon and Rectum
Uploaded by
Lilibeth Tenorio De LeonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Injury To The Colon and Rectum
Injury To The Colon and Rectum
Uploaded by
Lilibeth Tenorio De LeonCopyright:
Available Formats
Injury to the Colon and Rectum Karim Brohi, trauma.
org 8:7, July 2003 Case Presentation: Missed rectal injury A 22 year old man presented to the trauma centre 3 days following a stab wound to the right buttock. He had initially been seen at another hospital where a 1.5cm wound to the outer aspect of the right buttock had been cleaned and stitched. He represented due to pain in the buttock and appearance of a 4cm black patch around the buttock wound. He had never complained of any rectal pain or bleeding. Examination at the trauma centre included digital rectal examination and rigid sigmoidoscopy/proctoscopy, revealing some blood and pus and an injury to the lateral rectal wall. The patient was transferred immediately to the operating room for debridement of the buttock wound and defunctioning colostomy. On the operating table the nectroci patch on the buttock had expanded to approximately 8cm in diameter. Debridement was commenced but could not keep pace with the rapidly spreading necrotizinf fasciitis.
The patient eventually died on the operating table when it became apparent the sepsis had spread to include his upper and lower limbs.
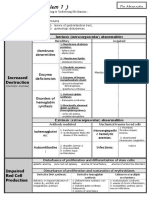
Guidelines for the management of Colon & Rectal Trauma Haemorrhagic Shock. Hypothermia - Coagulopathy - Acidosis Damage Control Procedure Control Haemorrhage Rapid primary suture of small wounds. Transect & close (stapler) more extensive injuries for later repair. Avoid colostomy. Colon: Primary repair. Consider colostomy if >24 hours post trauma. Rectum: Primary Repair if: Intra-peritoneal rectal injury. Extra-peritoneal rectal injury that can be mobilised intra-peritoneally or repaired trans-anally. No pre-sacral drainage No distal washout. Proximal diverting loop colostomy if: More extensive rectal injury. Position makes repair impossible. Pre-sacral drainage if high-energy, blunt trauma or delayed surgery No distal washout. Hartmann's Procedure if: Severe extra-peritoneal rectal injury.
Penetrating Abdominal Trauma Guidelines for Evaluation Immediate Laparotomy if: Shock Peritonitis (clinical examination) Evisceration
else: FAST Ultrasound Scan or Diagnostic Peritoneal Lavage
If either shows free intra-abdominal fluid proceed to laparotomy. With no evidence of free intra-peritoneal fluid, admit for close haemodynamic monitoring and serial physical examination. Proceed to laparotomy if develops signs of shock or peritonitis. At 24 hours / the next morning: Clinical exam abnormal but no obvious peritonitis: Consider laparoscopy. Consider CT scan. Clinical exam normal: Allow to eat & drink. If subsequently well - discharge.
Special scenarios 1. Stab wound to flank Problems: Retroperitoneal colon injury Renal / ureteric injury
Investigation of potential colon injury: There is no good radiological investigation for this injury. Serial physical examination is the most important. Consider CT scan with rectal contrast. Even if normal maintain a high index of suspicion. Continued management as for abdominal stab wound but will require longer period of observation, watching closely for signs of sepsis. Investigation of renal injury:
In the presence of haematuria proceed to CT scan with intravenous contrast. Absence of haematuria does not exclude an injury to the urinary tract. Maintain a high index of suspicion during observation. 2. Stab at Costal Margin If shocked - use FAST to exclude haemopericardium Haemothorax/pneumothorax and free fluid in abdomen implies a diaphragmatic injury. Consider next-day laparoscopy for all lower left chest stabs to exclude diaphragm injury. 3. Tangential Gunshot Wounds In general, most gunshot wounds will require laparotomy. However, if: Haemodynamically normal No clinical signs Possible tangential gunshot wound track
Consider CT scan or laparoscopy exclude/confirm peritoneal penetration.
Case Presentation 32yr old man admitted post Motor Vehicle Crash. On admission : Primary survey Airway : Maintaining own airway. Cervical collar & immobilisation in place Breathing : Respiratory rate 20, right sided chest bruising, clinically multiple right sided rib fractures. O2sats 96% Circulation : Pulse 120/min, BP 80/40 Disability : Glasgow Coma Score 14/15. Bilateral equal pupils. No gross peripheral motor or sensory deficit. Exposure : No other obvious injuries.
Introduction Case Presentation Initial Evaluation Radiology Grading Management Surgical Technique Conclusions
Chest X-Ray showed multiple right sided rib fractures and pneumohaemothorax. Right intercostal chest drain inserted Cervical spine and pelvis X-rays normal. Secondary Survey Showed distended abdomen, with pain and tenderness in the right flank. Macroscopic haematuria following urethral catheterisation. No other injuries detected. Resuscitation room intravenous urography was performed:
Demonstrating extravasation of contrast from the right kidney, and a functioning left kidney. Surgery Patient was taken for laparotomy, where he was found to have a 500mls of free blood in the peritoneum.
There was no injury to intraperitoneal organs, but a large, expanding retroperitoneal haematoma was present, which was leaking into the peritoneal cavity.
The retroperitoneum was opened, revealing an large laceration to the lower pole of the right kidney:
Devitalised tissue was debrided, and the kidney repaired with pledgeted mattress sutures across both ends of the laceration.
A drain was placed to the retroperitoneum and the abdomen closed. The patient had an uneventful postoperative course and was discharged home on day 8.
Intravenous Urography 90% accurracy under best of conditions Poor study in hypotensive patients Poor grading study Does not evaluate retroperitoneum One shot study may be important in unstable patients to identify a contralateral functioning kidney.
Introduction Case Presentation Initial Evaluation Radiology Grading Management Surgical Technique Conclusions
Extravasation of contrast from right kidney
Clot in collecting system
No filling of upper pole of right kidney
Computed Tomography Gold standard Delineates grade of injury Shows infarcted segments of kidney Images whole abdomen and retroperitoneum Not appropriate for haemodynamically unstable patients
Right perinephric haematoma. Renal vessels visible. Poor uptake of contrast Angiography Delineates vascular injury Where CT equivocal or unavailable Invasive Introduction Case Presentation Initial Evaluation Radiology Grading Management Surgical Technique Conclusions
Grading Classified according to the Organ Injury Scaling (OIS) Committee Scale
Minor
Contusion
Microscopic or gross haematuria, Urological studies normal
Haematoma Subcapsular, nonexapnding without parenchymal laceration. II Haematoma Nonexapnding perirenal haematoma confined to renal retroperitoneum. Laceration Major III Laceration <1cm parenchymal depth of renal cortex without urinary extravasation. >1cm depth of renal cortex, without collecting system rupture or urinary extravasation Parenchymal laceration extending through the renal cortex, medulla and collecting system. Main renal artery or vein injury with contained haemorrhage. Completely shattered kidney. Avulsion of renal hilum which devascularizes kidney.
IV Laceration
Vascular V Laceration Vascular
Management Goals of management : minimize morbidity & mortality preserve renal function
Surgical vs Non-operative management: Most grade I - IV injuries can be treated conservatively, thus avoiding unnecessary surgery. Surgery is indicated for : Vascular (renal pedicle) injury Shattered kidney Expanding or pulsatile haematoma Shocked polytrauma patient
Introduction Case Presentation Initial Evaluation Radiology Grading Management Surgical Technique Conclusions
Relative indications for surgery include : A devitalized renal segment in the presence of other abdominal injuries Persistent extravasation Loculated collections Incomplete grading (CT or angiography)
9% of kidney injuries will require surgical exploration, and of these there is on average an 11% nephrectomy rate. Most nephrectomies are for haemorrhage, and 61% of nephrectomies are for renovascular injury. Patients underggoing nephrectomy tend to be more severely injured.
Surgical Technique Midline laparotomy Gain proximal control Debride Ligate bleeding vessels Repair collecting system Close capsule or use omental graft
Introduction Case Presentation Initial Evaluation Radiology Grading Management Surgical Technique Conclusions
Retroperitoneal drainage
Proximal control of the renal artery and vein before mobilisation of the colon and opening of Gerota's fascia results in an increased rate of renal salvage and hence lower nephrectomy rate. On the left, the vessels can be exposed through the posterior peritoneum, by dividing it vertically between the inferior mesenteric vein and the fourth part of the duodenum. The renal vein and artery can then be identified an controlled with vessel loops. On the right side, it is often easier to control the renal vein and artery after mobilisation of the colon. If bleeding occurs on mobilisation of the colon or opening of perinephric fascia, atraumatic vascular clamps may be placed on the renal artery and vein. Warm ischaemia is poorly tolerated, and acute tubular necrosis develops after 20 minutes, though this is usually transient. Partial nephrectomy is often possible. Preserving the capsule of the kidney if possible, devitalised tissue is debrided and bleeders controlled with diathermy or suture. The collecting system is closed with a running absorbable suture. Alternatively, pledgeted matress sutures may be placed across the capsule. If possible the capsule is closed, or an omental flap closed over the defect. Nephrectomy is inidicated in the shattered kidney or renal pedicle injury in an unstable patient. The pedicle vessels are ligated separately, to avoid later arteriovenous fistula formation. The ureter is tied and kidney removed. Retroperitoneal drainage is necessary post partial or total nephrectomy. This should not be in contact with the renal collecting system. If the collecting system has been reparied, a nephrostomy tube and/or double-J stent should be placed. Injuries to other abdominal organs should be drained separately.
Conclusions Blunt Trauma and Penetrating Trauma are different injuries CT scan gold standard for radiological investigation Always preserve renal tissue when possible
Exsanguinating Pelvic Trauma Case One We recently had a case of a pedestrian run over by her own car and suffered major pelvic fractures (anterior and posterior), a liver laceration and major chest injuries. The Surgical team decided that there was no major thoracic or abdominal souce of bleeding although a FAST (Focussed Abdominal Sonography for Trauma) or DPL (Diagnostic Peritoneal Lavage) was not done.
The Orthopaedic team decided that pelvic angiography and embolisation was the way to go for control of the major pelvic bleeding. The patient was initially stable after intubation, fluid and blood resuscitation, but became very unstable in the Angio suite and had a hypovolaemic arrest in radiology. She was resuscitated with fluids, blood and adrenaline and the radiologist was then able to complete the angio ( after about an hour) and successfully embolise 2 major arterial bleeders.
She then went to the OT and had external fixation appllied and eventually had a laparotomy which revealed a liver laceration, which the surgeons tell me was not a major source of blood loss. Unfortunately she had a further cardiac arrest on the operating table and was not able to be resuscitated.
Case Two 25 year old motorcyclist was brought to our unit via our Helicopter Emergency Medical Service. She was persistently hypotensive throughout her prehospital course and on arrival in the emergency department had a blood pressure of 70/50 and pulse rate of 130/min. She was alert, orientated and conversing normally. Her airway was clear and examination of the chest was normal. Her abdomen was obviously distended and pelvis very unstable to clinical examination. Blood pressure improved to 90/50 with infusion of 2 litres of crystalloid and 4 units warmed O-egative blood through a rapid infusion system. She was log-rolled to examine her back but immediately lost her blood pressure and only had a palpable carotid pulse. Blood pressure returned to around 80/40 after further fluid and blood transfusion. Pelvic X-ray showed pubic rami fractures and a left sacral fracture.
Ultrasound scan of her abdomen showed intraperitoneal free fluid in the hepatorenal space and pelvis.
She remained shocked and unresponsive to fluid resuscitation and was taken to the operating room. The decision was taken to place an external fixator prior to performing the laparotomy. Anaesthesia was induced and an incision made over the iliac crest. Unfortunately this entered the retroperitoneal haematoma and the patient began to haemorrhage from this wound. Packing was applied an the external fixator quickly completed. A laparotomy was carried out through a midline incision. The right lobe of the liver had a deep laceration not extending into the hepatic veins. There was a large pelvic retroperitoneal haematoma which was leaking into the intraperitoneal space. The haemorrhage from the liver laceration was controlled with ligation of bleeding arteries and packing. As the haematoma was expanding and leaking, attempts were made to control the retroperitoneal haemorrhage. The retroperitoneum was opened. This lead to significant haemorrhage from the general pelvic area. Both internal iliac arteries were identified and ligated. Further attempts were made to control venous haemorrhage by placing fogarty balloon catheters via the femoral veins. The patient became progressively cold, acidotic and coagulopathic despite administration of clotting factors and the use a rapid infuser go transfuse warmed fluids. All attempts to control haemorrhage were unsuccessful and the patient died on the table. Pelvic Injury Audit - 1994 Following this case we reviewed our management of pelvic injuries. We looked at all patients arriving with unstable pelvic fractures. Overall mortality was 6%. When there was a significant concomittant intra-abdominal injury (Abbreviated Injury Scale 3 or more) mortality rose to 50% (median injury severity score - ISS - for this group was 56). For those patients who arrived in hypovolaemic shock with a systolic blood pressure below 90mmHg, with combined intraperitoneal injury and unstable pelvic fracture the mortality was 100% (median ISS 63). Management of these patients was altered, based on the principles of protecting the primary clot, prevention of the hypothermia-acidosis-coagulopathy syndrome and early control of haemorrhage using damage control techniques.
Case Three 33yr old male driver of a car, lateral impact with another car and then head-on into a bus. At scene pulse 130, BP 80/40. GCS 14. Open pelvic fracture involving the rectum. At scene: Airway was clear, seat-belt mark to chest but lung fields appeared clear. No manual testing of pelvic stability. Pelvic splint applied. Minimal log-rolling. Scoop stretcher & vacuum mattress applied for transport. IV Access for
analgesia. A total of 100 mls of warmed Ringer's lactate given in prehospital phase. Emergency Department: Arrived with pulse of 130, BP 70/50, cool peripheries. Chest X-ray showed a large diaphragmatic tear with haemothorax.
Pelvic X-ray showed a complex unstable pelvic injury.
Intraperitoneal free fluid on abdominal ultrasound (FAST) . The pelvic splint was left on. A further 300 mls warmed RInger's given in emergency department. Right chest tube placed. 700 mls blood evacuated. Blood, platelets, fresh frozen plasma and cryoprecipitate was ordered. Operating Room: At laparotomy there was a large right diaphragmatic tear with liver herniation and a laceration to the right lobe of the liver extending into the retrohepatic inferior vena cava. There was a laceration to the upper pole of the spleen. There was a large retroperitoneal haematoma centrally in the upper abdomen and in the pelvis. The liver and vena cava were packed, a splenectomy performed and the pelvis packed (pelvic splint remains in place). The right diaphragm was repaired. The abdomen was closed and angiography was then performed on the table in the operating room. Obturator and internal pudendal arteries were embolized. Branches of the hepatic artery were also embolized. Once the major haemorrhage had been controlled, crystalloid, blood and clotting factors were administered to correct the base deficit. The patient was transferred to the intensive care unit and warmed. The following morning he developed an abdominal compartment syndrome and the abdomen was opened and the packs removed. The caval
injury was re-packed. 48 hours later all packs were removed and the abdomen closed primarily.
The Case Presentation Algorithms
Prehospital On Impact: A 28 year old male motorcyclist traveling approx 60 mph intercepts an automobile which ignores a stoplight.
On Scene: pulse 120, systolic blood pressure 90, Resp 16, GCS 8. PreHospital Questions: This patient is obviously in shock. How do you define haemodynamically instability? Adam Starr Age, fracture pattern, RTS, base deficit, GCS, systolic blood pressure and (according to Wolfgang Ertel) lactate - these are available quickly.
How do you diagnose an unstable pelvic fracture in the street? Is clinical examination valuable? Is it harmful? Clinical Examination of the pelvis is used to assess for mechanical instability. However the sensitivity and specificity of this test have been called into question. In addition, opening and closing the pelvis may destabilise clot that has formed and provoke fresh haemorrhage:
Preserve clot - minimal movement, gentle handling, minimum of rolling. Punch anyone who tries to 'spring' the pelvis. Fit pelvic belt on basis of mechanism of injury. Minimal iv fluid to preserve systolic of 70 (90 mmHg if associated head injury). Take to a hospital that understands the condition! The Right iliac wing is mobile to exam. Do you stabilize this on scene? (e.g. London splint, Geneva belt, Dallas binder, Kendrick extrication device, PASG, etc) The nearest community hospital is 30 minutes away. The nearest Level II Trauma Center is 60 min. Level I Trauma Center is 90 min. To which hospital should this patient be transported? Both the Kellam and the Routt algorithms address thetransfer question.
If the patient is taken first to a community hospital, what should be done there prior to transfer?
Most algorithms (e.g. Agolini ) call for fluid resuscitation. (NotBrohi) How much fluid should this patient receive? Ken MattoxWe are focusing on the WRONG thesis, the WRONG argument, and are bound to reach the WRONG conclusions. Remember the days of "flail" chest. The patients did not look bad until AFTER they arrived at the hospital and had a lot of fluids. The issue in pelvic fracture is similar. AGGRESSIVE cyclic hyperresuscitation results in a predictable coagulopathy and a rise in venous pressure. This leads to venous bleeding from the pelvic veins, requiring repeat cyclic hyperresuscitation and a viscous cycle requiring still other therapy. The studies of immediate external fixators are virtually ALL WAG [Wild Assed Guess] data and a lot of "expert opinion" expressed. Emergency Room On Arrival - Level I trauma center Intubated and ventilated, saturations 99% Pulse 160, blood pressure 70/40, Patient immobilized to long backboard.
2 large bore iv's running LR. Chest Xray - Left hemopneumothorax. Lt Chest tube placed. AP pelvic Xray obtained.
Emergency Room Questions: Is the AP pelvic X-rays as a priority? Do you order them on everybody? The American College of Surgeons Advanced Trauma Life Support advocates the routine use of the antero-posterior pelvic X-ray as an adjunct to the primary survey. Some authors suggest that this is not cost effective and that clinical criteria may be used to screen for the presence of a pelvic injury. Examination of the pelvis is notoriously unreliable, especially in obtunded, intoxicated or obese patients. In addition, repeated 'springing' of the pelvis may result in disruption of any clot that has formed and lead to further exsanguination. The antero-posterior pelvic X-ray should still be routinely used to determine the presence of pelvic injury in multiply injured trauma patients. Clinical examination, especially repeated 'springing' of the pelvis, should be kept to an absolute minimum. Is there anything wrong with this pelvic X-ray? Are the orthopaedic Tile and Burgess-Young pelvic injury classifications useful in this situation?
A sheet was immediately wrapped around the pelvis in the emergency room. Blood pressure improved to 90/60 with tachycardia of 130/min.
Can the haemodynamic response response to non-invasive stabilisation be used to predict the need for further interventions (external fixation / angiography etc.) Where is this patient bleeding from?
How do you want to investigate this further and where? (Evers and Pohlemann have already taken the patient to the OR.)
The patient has received 3L crystalloid, the 4 units of PRBC's and 4 units of FFP . Abdominal ultrasound shows hypoechoic stripe in the hepatorenal space. (positive for free intraperitoneal fluid).
FAST vs DPL Questions: Is this a positive FAST? If so, do you trust it? Is FAST accurate in the presence of a pelvic fracture / retroperitoneal haematoma? 'Ultrasonography has been shown to be as accurate as DPL and CT in the detection of hemoperitoneum following abdominal trauma.'
Is there still a place for Diagnostic Peritoneal Lavage? 'Because of the high incidence of hemoperitoneum associated with retroperitoneal hematoma, peritoneal lavage is less useful in the setting of of pelvic fracture than in other settings of suspected intra-abdominal trauma.' 'Nine of 27 patients initially stable patients underwent laparotomy on the day of admission because of the development of hemodynamic instability, and all had retroperitoneal hematoma as the source of the increasing transfusion requirements.' 'It is likely that CT scanning of patients with pelvic fractures and suspected intra-abdominal injuries to solid organs will result in the lowering of the negative laparotomy rate and morbidity in that group.' What if this patient were FAST Negative? - there's no intraperitoneal injury. What do you want to do now?
Prior to laparotomy, the sheet & towel clip were replaced with a pelvic clamp. Application time was 35 minutes.
Ex Fix Questions: Is there any point in applying an external fixation device over and above the non-invasive belts? The surgeons (e.g. Scalea, Brohi, Agolini) want to perform an immediate laparotomy. It appears that pelvic external fixation o does not significantly tamponade retroperitoneal hemorrhage, o does not significantly reduce intrapelvic volume, and o frequently increases posterior pelvic displacement - in the vicinity of major sources of venous and arterial hemorrhage. Is there any evidence to support the use of the external fixator? Which method of external stabilization is best? When should it be applied?
Operating Room On OR Arrival: BP 90/50 pulse 140. At laparotomy - an extensive liver laceration is found and is controlled with packing. A large pelvic retroperitoneal haematoma is present.
Laparotomy Questions: Do you open the retroperitoneal haematoma? Is there are role for ligation of the internal iliacs? Pohlemann and Ertel recommend extraperitoneal packing. Should you pack intra- or extra-peritoneally? Is internal fixation of the symphysis pubis indicated at laparotomy? Where do you want to send the patient now?
A symphysis pubis plate was used to close the anterior diastasis. Bilateral extraperitoneal paravesical pelvic packing is performed after the evacuation of approximately 3000ml of clot from this region. The abdomen is closed. The pelvic C-Clamp is removed. 70 minute operative procedure BP 90/60, pulse 140, urine output 300 ml. The patient is transferred to the angiography suite.
Angiography Suite Angiography: Haemorrhage from the left obturator artery is identified and embolized. BP 100/70, pulse 100
Angiography Questions: In retrospect should angiography have been performed first?
Physicians are often reluctant, for no valid reason, to transport hemodynamically unstable patients to the angiography suite. We urge them to abandon this attitude. Patients in hemorrhagic shock, with surgically correctable injuries, should be transported to the operating theatre, regardless of shock. By the same token, patients in hemorrhagic shock, with unknown sources of hemorrhage - as well as those with hemorrhage best treated by embolization - should be transported to the angiographic suite, regardless of shock. Left where they are, be it the emergency department of intensive care unit, they may die of exsanguination.'
'Three basic principles should guide the angiographer in performing embolization. The purpose is to slow the bleeding to the extent that the body will control its own hemorrhage, rather than create large areas of ischemia or necrosis. If ischemia and necrosis must be created it should be limited to the smallest area possible. The procedure must be done expidetiously.'
Overall 7-11% of pelvic fractures will require embolization. Only 2% of lateral compression fractures have demonstrable arterial haemorrhage, compared to 20% of anteroposterio compression, vertical shear or combined
mechanism injuries. Can angiography control intraperitoneal haemorrhage avoiding the need for laparotomy? Should the operating room and angiography be the same place?
After sustained hemodynamic improvement in angiography, iliosacral screws are placed under fluoroscopy to supplement the pelvic internal fixation.
Definitive Fixation Questions: How and when should definitive fixation be instituted? Would you do this without a CT scan?
Intensive Care Unit The patient was transferred to the Intensive Care Unit where he was warmed and his acidosis and coagulopathy corrected. The patient subsequently underwent a CT scan of his head which revealed a small left subdural hematoma and diffuse brain injury with tight basal cisterns. Initial intracranial pressures of approximately 35 mm Hg increased relentlessly over the ensuing 48 hours despite aggressive management. Eventually ICP topped 100 mm Hg pressure. Pupils became fixed and dilated. A day later life support was withdrawn.
Traumatic Brain Injury Questions: Does management of the pelvic injury affect neurological outcome?
Management of traumatic brain injury focuses on stabilisation of the patient and prevention of secondary neuronal injury to avoid further loss of neurons. Full neuromonitoring including intracranial pressure measurement are rarely available prior to the patients arrival in the intensive care unit. Significant neurological damage can occur between the time of injury and CT scanning, accurate measurement of ICP and other parameters. The acute management of these patients is therefore directed towards assuming there is significant intracranial pathology and instituting measures to protect living brain tissue.
Non-operative management of thoracic vascular Injury Case Presentation This was a 34 year old male who suffered a low velocity gunshot wound to the left upper chest, presenting with a 1cm wound just under the left midclavicle as a sucking chest wound. This wound was sutured close and a left tube thoracostomy placed, which initially put out 300cc blood. There was an apparent exit wound on the upper right back over the mid right scapula. Physical exam showed complete sensorimotor loss below the nipples and no rectal tone, consistent with a spinal cord injury at T4. Distal pulses were all present and equal in all 4 extremities. Patient's vital signs initially were BP 110/70, Pulse 120, RR 30, O2 sat 97% room air. CXR showed bullet fragments across the upper right chest posteriorly, and a left pulmonary contusion.
After the chest tube was placed, BP intermittently dropped into the 80's, and over the course of the next 4 hours a total of 1000cc blood came out the left chest tube. Patient was intubated. An arteriogram was performed showing a nonocclusive and non-extravasating intimal injury of the right innominate artery at the takeoff of the right subclavian and carotid arteries. Left great vessels were not injured. A flexible esophagoscopy showed no injury. It was decided to observe the patient nonoperatively. A right chest tube was placed which did not put out any blood. Over the next 5 days the blood from the left chest stopped, vital signs stabilized, and the patient was extubated. A repeat arteriogram showed complete resolution of the innominate artery intimal defect. The patient never required surgery. He was transferred to a spinal cord injury rehab center 10 days post injury.
Initial Angiogram
Repeat Angiogram
Discussion It was clear that the innominate artery injury was not responsible for the left chest bleeding (which was probably from the parenchymal injury of the lung), or the hemodynamic instability, and was an essentially incidental finding. Such nonocclusive "minimal" arterial injuries are well documented to have a benign natural history, and should be followed rather than being immediately operated upon when they are asymptomatic (i.e. no hard signs of vascular injury) with a vessel that is not occluded and has no gross extravasation, as the majority never require surgery. A patient such as this does not need unnecessary surgery, especially surgery as extensive as this procedure would have to have been. His bleeding from the left chest tube was borderline in terms of an indication to operate, which is generally suggested when output exceeds 200cc/hour for more than 4 hours. Fortunately it tapered off.
CLASSIC CASES Tension Haemothorax Case Presentation A 31 year old man is transferred from another hospital following a kick to the left chest. Initial chest X-ray showed a large haemothorax.
The patient was taken to the CT scanner, by which time the whole chest had filled with blood and there was radiological evidence of tension.
CTs show a left hemithorax full of blood, with the lung compressed down to a very small volume. The heart, trachea and mediastinal structures are shifted to the right. By this time the patient was in respiratory distress with a respiratory rate of 40 with shallow, painful respiration. Pulse was 105 and blood pressure 110/60. A left sided chest drain was placed and the patient transferred to our institution. Over the next 12 hours the patient drained 4000mls of venous blood from the left chest, but the patient remained haemodynamically stable. The bleeding slowed and stopped. Thoracoscopic washout was performed to evacuate approximately 1000mls of retained clot on day 3 and the patient was discharged home on day 7. Discussion Massive haemothorax is a well-recognised condition and may often produce radiological evidence of tension. Aprat from tracheal & mediastinal deviation, the other signs are not present. The affected hemithorax is dull to percussion and there is no distension of neck veins or raised jugular venous pressure due to the hypovolaemic state. This patient should have had a chest drain placed following the initial chest X-ray. While most venous bleeding will stop eventually there is no credence to the myth that the build-up of tension in the left chest will tamponade the bleeding - as evidenced by the dramatic collapse of the left lung and shift of the mediastinum visible on the CT scan. There is little indication for a CT scan in the emergent management of this patient, though a scan of the abdomen did rule out associated splenic trauma.
CLASSIC CASES Tension Gastrothorax Case Presentation A 40 year old man is the unrestrained driver in a front-impact motor vehicle collision. He arrives with a respiratory rate of approximately 20/minute but haemodynamically stable. Initial chest X-ray showed an elevtaed and slightly thickened left hemidiaphragm, suggesting a diaphragm injury. The patient was transferred, self-ventilating, to the CT scanner. He gradually became more and more dyspneoic, with rising respiratory rate.
CTs show a left hemithorax almost full of the stomach, with shift of mediastinal structures to the right. Towards the end of the scan the patient became progressively tachycardic and then hypotensive at 80/60. Further scanning was terminated and the patient anaesthetised, intubated and ventilated. Positive pressure ventilation caused re-expansion of the left lung and partial return of the stomach into the abdomen. The patient was transferred to the operating room for laparotomy, which identified a large circumferential laceration of the diaphragm approximately 2cm from the costal margin. The stomach and spleen were reduced into the abdomen and the diaphragm injury repaired primarily. Discussion Tension gastrothorax has previously been described. In the spontaneously ventilating patient the negative pressure generated in the thoracic cavity progressively sucks the stomach into the chest with each breath. Eventually, respiratory and haemodynamic compromise ensue, as with a classic tension pneumothorax. Various methods have been used to treat the condition acutely. Nasogastric trubes can be placed to decompress the stomach - although placement may be difficult due to kinking at the level of the diaphragm. Needle decompression of the stomach has also been suggested but this may theoretically lead to contamination of the thoracic cavity. Positive pressure ventilation allows immediate re-expansion of the lung and forces intraperitoneal contents back into the abdomen. As the patient will require operative repair, ventilation is already indicated.
CLASSIC CASES Late presentation of diaphragm rupture following blunt thoracic trauma Case Presentation A 67 year old woman was admitted via the emergency department complaining of nausea, vomiting and abdominal pain after meals. Chest X-ray on admission:
The Chest X-ray showed rupture of the left hemi-diaphragm with associated collapse of the left lung. On questioning, the patient admitted to having fallen 3 months previously and having sustained two broken ribs on the left chest. She was seen in the emergency department of another hospital and discharged after an overnight stay with analgesia. A chest X-ray was taken at the time, which presumably showed no evidence of diaphragmatic rupture. A CT scan showed the stomach in the left thoracic cavity, and the rib fractures responsible for the diaphragmatic laceration:
The patient was prepared for operation and underwent a scheduled procedure the following day. Operating room At operation approximately two-thirds of the stomach and the spleen had herniated through a 10cm diaphragm laceration into the chest. The stomach and spleen were reduced into the abdomen by extending the laceration laterally.
A band-like constriction of the stomach by the diaphragm can be seen in the marks on the stomach:
The chest was washed out and the diaphragmatic laceration was repaired with a continuous nylon suture. Stay sutures on either side of the laceration allow the diaphragm to be tented downwards to aid closure.
The abdomen was closed and the patient made an uneventful post-operative recovery. Discussion Blunt injury to the diaphragm occur in approximately 1% of all trauma adminssions. The diaphragm is most commonly injured by a direct blow to the abdomen, causing a sudden increase in intra-abdominal pressure, or by direct laceration from rib fractures. Rupture of the diaphragm rarely occurs in isolation, and associated injuries to the thoracic aorta, liver & spleen and pelvis are often present. Diagnosis is often difficult or missed, as the above case shows. A high index of suspicion is vital. Chest X-ray may reveal the injury if abdominal contents have herniated into the chest, may reveal a thickening or fuzziness of the diaphragmatic outline, an elevated hemidiaphragm or be completely normal - especially if the patient is intubated &
ventilated. Haemopneumothoraces are a common associated finding. Overall the plain Chest X-ray has a 50% accurracy. Diaphragmatic injury may be detected on ultrasound - but rarely. CT scanning has a sensitivity of only around 7080%. MRI may be the best non-invasive examination for blunt diaphragmatic injury. Laparoscopy or thoracoscopy have become the primary means of diagnosing diaphragmatic injury - though the are more frequently employed for penetrating trauma. As with CT and MRI scanning, the patient must be haemodynamically stable for these procedures. Delay in detecting and repairing diaphragmatic injury increased both morbidity and mortality. Operative repair is also technically more difficult, the longer the delay to surgery. Diaphragmatic injuries are usually repaired via a laparotomy incision.Abdominal contents are reduced and the diaphragm can usually be repaired simply with a large monofilament non-absorbably suture, placed as locked stitches or horizontal mattress sutures. Care should be taken if the laceration extends into the central tendon of the diaphragm, where the myocardium is easily caught in poorly placed sutures. It is important to adequately wash out the thoracic cavity prior to closure, to remove any clot or contamination. In cases where the diaphragmatic hernia has been present for a long time (years) simple closure may be difficult or impossible, and non-absorbably mesh may be required.
Transfusion for Massive Blood Loss Presented below is a description of massive blood loss and the inherent problems associated with large volume blood transfusions. Following this is a suggested protocol for guiding management of the patient receiving a massive transfusion for haemorrhage. Definition Massive transfusion is arbitrarily definied as the replacement of a patient's total blood volume in less than 24 hours, or as the acute administration of more than half the patient's estimated blood volume per hour. Aim of Treatment The aim of treatment is the rapid and effective restoration of an adequate blood volume and to maintain blood composition within safe limits with regard to haemostasis, oxygen carrying capacity, oncotic pressure and biochemistry. Complications of Massive Transfusion The complications of massive transfusion are those of any blood transfusion plus : Blood Volume Replacement The complications of massive transfusion are exacerbated by inadequate or excessive transfusion. Traditionally transfusion of hypovolaemic patients has been directed towards maintaining a haemoglobin concentration of 10g/dl. The use of haemoglobin as the only indicator (or 'transfusion trigger') may result in unnecessary administration of blood products, with their concommittant risks. Transfusion requirements should be based on the patient's physiologic needs, defined by their oxygen demand (consumption). Oxygen consumption is given by :
Where CO = Cardiac Output, CaO2 and CvO2 are arterial and venous oxygen content respectively. Oxygen delivery is :
The extraction ratio (ER) is the ratio of oxygen consumption to oxygen delivery, normally around 25%.
The most appropriate monitor of tissue oxygen supply is the tissue oxygen tension, reflected by the PvO2, or mixed venous partial pressure of oxygen (normally 6 kPa, 45mmHg). Patients with a low PvO2 can be classed as stable or unstable depending on haemodynamics, ventilation, acid base status and urine output. If
they are stable, no therapy is indicated until a true critical level is reached (PvO2 around 3 kPa, 23mmHg). If unstable, treatment must be intituted. Thus transfusion should be guided by haemodynamic stability, PvO2 and ER. Obviously during trauma resuscitation, haemodynamic stability is the key indicator. In summary : o o o If Hb > 10g/dl transfusion is rarely indicated. If Hb < 7g/dl transfusion is usually necessary. With Hbs between 7 and 10 g/dl, clinical status, PvO2 and ER are helpful in defining transfusion requirements.
Thrombocytopenia Dilutional thrombocytopenia is inevitable following massive transfusion as platelet function declines to zero after only a few days of storage. It has been shown that at least 1.5 times blood volume must be replaced for this to become a clinical problem. However, thrombocytopenia can occur following smaller transfusions if disseminated intravascular coagulation (DIC) occurs or there is pre-existing thrombocytopenia. Coagulation Factor Depletion Stored blood contains all coagulation factors except V and VIII. Production of these factos is increased by the stress response to trauma. Therefore only mild changes in coagulation are due to the transfusion per se, and supervening DIC is more likely to be responsible for disordered haemostasis. DIC is a consequence of delayed or inadequate resuscitation, and the usual explanation for abnormal coagulation indices out of proportion to the volume of blood transfused. Oxygen Affinity Changes Massive transfusion of stored blood with high oxygen affinity adversely affects oxygen delivery to the tissues. Evidence for this is as yet not forthcoming, but it would seem wise to use fairly fresh red cell transfusions (<1 week old). Use of fresh (<24 hours) blood is not indicated. 2,3 DPG levels rise rapidly following transfusion and normal oxygen affinity is usually restored in a few hours. Hypocalcaemia Each unit of blood contains approximately 3g citrate, which binds ionized calcium. The healthy adult liver will metabolise 3g citrate every 5 minutes. Transfusion at rates higher than one unit every five minutes or impaired liver function may thus lead to citrate toxicity and hypocalcaemia. Hypocalcaemia does not have a clinically apparent effect on coagulation, but patients may exhibit transient tetany and hypotension. Calcium should only be given if there is biochemical, clinical or electrocardiographic evidence of hypocalcaemia. Hyperkalaemia The plasma potassium concentration of stored blood increases during storage and may be over 30mmol/l. Hyperkalaemia is generally not a problem unless very large amounts of blood are given quickly. On the contrary, hypokalaemia is more common as red cells begin active metabolism and intracellular uptake of potassium restarts. Acid/Base Disturbances Lactic acid levels in the blood pack give stored blood an acid load of up to 30-40mmol/l. This, along with citric acid is usually metabolised rapidly. Indeed, citrate is metabolised to bicarbonate, and a profound metabolic alkalosis may ensue. The acid-base status of the recipient is usually of more importance, final acid/base status being dependent on tissue perfusion, rate of administration amd citrate metabolism. Hypothermia Hypothermia leads to reduction in citrate and lactate metabolism (leading to hypocalcaemia and metabolic acidosis), increase in affinity of haemoglobin for oxygen, impairment of red cell deformability, platelet dysfunction and an increased tendency to cardiac dysrhythmias. Acute Respiratory Distress Syndrome (ARDS) The aetiology of ARDS is as yet not fully understood, but various risk factors have been identified. Both under- and over-transfusion are associated with an increased risk of ARDS, as is albumin < 30g/l.
Microaggregate filters should be used during massive transfusion except when giving fresh whole blood or platelets.
Protocol for Management of Massive Transfusion
Sequence of Components Profound hypotension should be treated speedily. Administer crystalloid or colloid infusions rather than delay fluid administration. Initial red cell replacement is in the form of packed red cells. Laboratory Samples At the start of resuscitation, blood should be taken for group and crossmatch, coagulation tests, full blood count and biochemistry. These must be properly labelled and identified in all situations. Blood Bank Arrangements Routine procedures should be followed until it becomes obvious that massive transfusion is likely. The blood bank should be informed as soon as possible that a major trauma is arriving or in the building. For extreme emergencies group O blood should be supplied first. Rhesus D negative blood should be supplied to all women of childbearing age. Type specific (ABO Rh D matched) blood should be available in 5 minutes and the switch should be made promptly so as not to deplete stores of group O blood. Continue transfusing blood on this basis until time is available to crossmatch on the original serum sample. If an antibody screen is negative and more than one blood volume has been administered there is no point attempting compatibility tests except to exclude ABO mismatches. Monitoring During massive transfusion, regular monitoring of haemoglobin, platelet count, prothrombin time (PT), partial thromboplastin time(PTT) and fibrinogen levels should take place and be used to guide component replacement. Components Component replacement should occur only in the presence of active bleeding or if interventional procedures are to be undertaken. Platelet concentrates (1 pack/10kg) are given if platelet count falls below 50. Each platelet concentrate also provides around 50ml of fresh plasma. Fresh frozen plasma (12ml/kg)is administered if PT or PTT are running higher than 1.5 times control levels. Cryoprecipitate (1-1.5 packs/10kg) is given for Fibrinogen levels < 0.8g/l. For massive uncontrolled traumative haemorrhage, maintenance of full haeostatic ability is usually unrealistic. The priority is for definitive surgical arrest of haemorrhage from major vessels. Combinations of stored whole blood, packed cells, colloids & crystalloids are given to maintain blood volume or pressure at adequate levels and haemoglobin at around 7g/dl or haematocrit at 0.25. Conserve limited supplies of fresh blood, plasma or platelets until the bleeding is controlled. When blood loss has lessened (0.5l/hour) and major vessels have been controlled, it becomes worthwhile correcting haemostasis.
CLASSIC CASES Infrahepatic Inferior Vena Cava injury Lateral repair Case Presentation Woman, 30 y old, sustained a gunshot wound to the right upper quadrant. She was and remained hemodynamically normal since the admitance in the emergency room. At laparotomy, the bullet was found to have penetrated the anterior and posterior surfaces of the stomach. There was minimal intraperitoneal blood but there was a right retroduodenal haematoma. The head of the pancreas was injurede (without injury to the main pancreatic duct) and the inferior vena cava was injured just below the junction with the right renal vein.
Gunshot entry wound, right upper quadrant
Anterior stomach injury (repaired)
A medial visceral rotation was performed to obtain control the infrarenal vena cava with a vascular clamp. The cephalad control was performed by compression of the reno-caval junction.
Right medial visceral rotation
A lateral wall repair was completed with a simple running suture.
Lateral wall of IVC injury (repaired)
The culprit The gastric wounds were repaired by simple suture. Total intraoperative blood loss was 400ml, and she had no postoperative complications. Discussion & References For discussion and references on the management of IVC injuries see the entry in the Open Library of Trauma Inferior Vena Cava Injuries
CLASSIC CASES Superficial Femoral Artery Injury Staged repair with arterial shunt Case Presentation A case of a young male, restrained passenger who was involved in a rollover motor vehicle crash. A metal road sign pole was impaled through and through his right lower extremity.
Impalement through right thigh He was taken to OR with a shattered femur and transected superficial femoral artery and vein. After removing the sign post, we ligated his superficial femoval vein and placed a temporary shunt in the artery between the superficial femoral and popliteal arteries. Orthopaedics then plated his femur. and we then performed a bypass of his superficial femoral artery with contralateral greater saphenous vein.
Shunt in superficial femoral artery He was able to ambulate with a functional limb post operatively and did surprisingly well! Discussion & References For discussion and references on the management see the articles on Peripheral Vascular Trauma and Damage Control Surgery
Revised Trauma Score The Revised Trauma Score is a physiological scoring system, with high inter-rater reliability and demonstrated accurracy in predictng death. It is scored from the first set of data obtained on the patient, and consists of Glasgow Coma Scale, Systolic Blood Pressure and Respiratory Rate. Glasgow Coma Scale Systolic Blood Pressure Respiratory Rate Coded Value (GCS) (SBP) (RR) 13-15 9-12 6-8 4-5 3 >89 76-89 50-75 1-49 0 10-29 >29 6-9 1-5 0 4 3 2 1 0
RTS = 0.9368 GCS + 0.7326 SBP + 0.2908 RR Values for the RTS are in the range 0 to 7.8408. The RTS is heavily weighted towards the Glasgow Coma Scale to compensate for major head injury without multisystem injury or major physiological changes. A threshold of RTS < 4 has been proposed to identify those patients who should be treated in a trauma centre, although this value may be somewhat low. The RTS correlates well with the probability of survival :
The RTS Calculator will sit as a standalone window on your desktop.
You might also like
- Leon Chaitow - Fascial Dysfunction 2ed PDFDocument407 pagesLeon Chaitow - Fascial Dysfunction 2ed PDFRukaphuong100% (14)
- 100 Item Exam On Fundamentals of NursingDocument58 pages100 Item Exam On Fundamentals of Nursingjacnpoy96% (54)
- Regulation - Lactase - Gene - Click - Learn - WorksheetDocument3 pagesRegulation - Lactase - Gene - Click - Learn - WorksheetSophia BrannemanNo ratings yet
- Endocrine: Portal Vascular SystemDocument9 pagesEndocrine: Portal Vascular SystemhoatbuiNo ratings yet
- Lovenox (Enoxaparin)Document1 pageLovenox (Enoxaparin)E100% (5)
- Pnle Course OutlineDocument11 pagesPnle Course Outlinestuffednurse100% (2)
- Muraqaba of Colored Lights - MeditationDocument3 pagesMuraqaba of Colored Lights - Meditationapi-3749476No ratings yet
- Videbeck - Psychiatric Mental Health Nursing - NewDocument27 pagesVidebeck - Psychiatric Mental Health Nursing - NewJohnrey Tesoro0% (1)
- Case Study 9 - Simon (Chronic Schizophrenia)Document6 pagesCase Study 9 - Simon (Chronic Schizophrenia)Vonn GalangNo ratings yet
- Liver Trauma: DR Tarik El Batrawy Specialist General SurgeryDocument50 pagesLiver Trauma: DR Tarik El Batrawy Specialist General Surgerykata61No ratings yet
- Uveit FosterDocument954 pagesUveit FosterEdmond IsufajNo ratings yet
- 1.a Superior Orbital Fissure SyndromeDocument2 pages1.a Superior Orbital Fissure SyndromeDr Sumant SharmaNo ratings yet
- PD QuestionsDocument8 pagesPD QuestionsYuvraj ChauhanNo ratings yet
- Echs Guide BookDocument33 pagesEchs Guide Bookesmchennai100% (1)
- Pulmonary FibrosisDocument4 pagesPulmonary FibrosisDimpal Choudhary67% (3)
- Intestinal Obstruction PDFDocument7 pagesIntestinal Obstruction PDFmist73No ratings yet
- Acyanotic Congenital Heart DiseaseDocument7 pagesAcyanotic Congenital Heart DiseaseSam Raj100% (1)
- Acute PericarditisDocument8 pagesAcute Pericarditisalina abu rumiNo ratings yet
- The ABC of Weaning Failure - A Structured ApproachDocument9 pagesThe ABC of Weaning Failure - A Structured ApproachArul ShanmugamNo ratings yet
- MCQ's With KEY Medicine - BDocument8 pagesMCQ's With KEY Medicine - BSiraj Ul IslamNo ratings yet
- Corneal DystrophyDocument5 pagesCorneal DystrophyDejan JanevNo ratings yet
- Acanthamoeba KeratitisDocument2 pagesAcanthamoeba KeratitisHitesh SharmaNo ratings yet
- Antibiotic 4 SurgicalDocument3 pagesAntibiotic 4 SurgicalNanaDinaWahyuniNo ratings yet
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument4 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- Cleviprex® (Clevidipine) Injectable Emulsion (eMC)Document7 pagesCleviprex® (Clevidipine) Injectable Emulsion (eMC)raju1559405No ratings yet
- Pediatrics - Neonatal ICUDocument2 pagesPediatrics - Neonatal ICUJasmine KangNo ratings yet
- Diagnosis and Management of Diabetic Amyotrophy: EndocrinologyDocument3 pagesDiagnosis and Management of Diabetic Amyotrophy: EndocrinologyDavis G. OctaviusNo ratings yet
- Basic Life Support DefinitionDocument2 pagesBasic Life Support DefinitionThomas KristiantoNo ratings yet
- Textbook of Introduction To EnvironmentaDocument134 pagesTextbook of Introduction To EnvironmentayadvinderNo ratings yet
- Splenomegaly Treatment & Management - Approach Considerations, Activity, Pharmacologic TherapyDocument7 pagesSplenomegaly Treatment & Management - Approach Considerations, Activity, Pharmacologic TherapyAndri Feisal NasutionNo ratings yet
- Cushing Syndrome GuidelineDocument3 pagesCushing Syndrome Guidelinediaga081100% (1)
- Systemic Lupus Erythematosus PDFDocument4 pagesSystemic Lupus Erythematosus PDFsazaki224No ratings yet
- Red EyeDocument6 pagesRed EyeafatNo ratings yet
- Cardiac Tamponade, Also Known As Pericardial Tamponade, Is AnDocument7 pagesCardiac Tamponade, Also Known As Pericardial Tamponade, Is AnSimran Josan100% (1)
- Mitral Stenosis Summary Notes PDFDocument5 pagesMitral Stenosis Summary Notes PDFCristina Georgiana CoticăNo ratings yet
- Glomerulonephritis PDFDocument5 pagesGlomerulonephritis PDFmist73No ratings yet
- Uterine Lipoleioma FulltextDocument3 pagesUterine Lipoleioma FulltextmylonasophiaNo ratings yet
- Atrioventricular Septal DefectDocument3 pagesAtrioventricular Septal DefectManishta Menaka DhuromsinghNo ratings yet
- CANCER (1) HandoutDocument50 pagesCANCER (1) HandoutLiza Noble-RoaNo ratings yet
- Amaurosis FugaxDocument11 pagesAmaurosis FugaxRexArtem100% (1)
- Membranes for Life SciencesFrom EverandMembranes for Life SciencesKlaus-Viktor PeinemannNo ratings yet
- Physiology Quiz CardiologyDocument5 pagesPhysiology Quiz CardiologySaad JalalNo ratings yet
- Soal MCQ 10 April 2014Document12 pagesSoal MCQ 10 April 2014Domiko Widyanto100% (1)
- Salbutamol AcidosisDocument3 pagesSalbutamol AcidosisAccounts OfficerNo ratings yet
- SEED No 1 - COAG - Principles of HaemostasisDocument4 pagesSEED No 1 - COAG - Principles of HaemostasisM Yusuf Ali RNo ratings yet
- CMB Lab Exp 9Document9 pagesCMB Lab Exp 9Elizabeth Jade ViceraNo ratings yet
- Acute Respiratory Distress SyndromeDocument20 pagesAcute Respiratory Distress SyndromeAngel Cauilan100% (1)
- Answer All The Following Short Essay Questions: (3 Questions)Document4 pagesAnswer All The Following Short Essay Questions: (3 Questions)Soad ShedeedNo ratings yet
- Cell (Biology) : Navigation SearchDocument14 pagesCell (Biology) : Navigation Searchsamz95100% (1)
- Apasi Yg Ga Buat NisaDocument20 pagesApasi Yg Ga Buat Nisamuhammad iqbal mahfuzhNo ratings yet
- Perioperative CareDocument18 pagesPerioperative CareCo Pablico EricNo ratings yet
- NorovirusDocument16 pagesNorovirusapi-509861377No ratings yet
- Minnesota Hospital Association's Lown Institute ResponseDocument3 pagesMinnesota Hospital Association's Lown Institute ResponseinforumdocsNo ratings yet
- GP1 Introduction To PathologyDocument74 pagesGP1 Introduction To PathologyAh ZhangNo ratings yet
- What Is Cancer? What Causes Cancer?: Discovered An Important Clue As To Why Cancer Cells SpreadDocument8 pagesWhat Is Cancer? What Causes Cancer?: Discovered An Important Clue As To Why Cancer Cells SpreadAlfred Melvin SolivaNo ratings yet
- Anemia of Prematurity UpToDate PDFDocument13 pagesAnemia of Prematurity UpToDate PDFАлександар ТасићNo ratings yet
- Optic Atrophy :major Review March 2010, Kerala Journal of Ophthalmology, Devendra V. Venkatramani Et AlDocument6 pagesOptic Atrophy :major Review March 2010, Kerala Journal of Ophthalmology, Devendra V. Venkatramani Et AlNavojit ChowdhuryNo ratings yet
- SepticemiaDocument2 pagesSepticemiaJennah Ricci TuazonNo ratings yet
- Rotation: Medical Intensive Care Unit (South Campus) For Interns and ResidentsDocument6 pagesRotation: Medical Intensive Care Unit (South Campus) For Interns and ResidentsHashimIdreesNo ratings yet
- Know About Pediatric Cardiac SurgeryDocument8 pagesKnow About Pediatric Cardiac SurgeryAshish DolasNo ratings yet
- SURGERYDocument20 pagesSURGERYManoj KumarNo ratings yet
- Pathology of AnemiaDocument3 pagesPathology of AnemiaNesma AdelNo ratings yet
- Acute Glomerular NephritisDocument5 pagesAcute Glomerular NephritisRoh JitenNo ratings yet
- Patients Safety - Key Issues and ChallengesDocument4 pagesPatients Safety - Key Issues and ChallengeskabirNo ratings yet
- Pulmonary HypertensionDocument8 pagesPulmonary Hypertensionmerin sunilNo ratings yet
- CH 15 PT 1Document28 pagesCH 15 PT 1Kathleen Anne JoreNo ratings yet
- Growth and DevelopmentDocument53 pagesGrowth and Developmentjennywatsurproblem100% (2)
- EXECUTIVE Branch of GovernmentDocument17 pagesEXECUTIVE Branch of GovernmentLilibeth Tenorio De LeonNo ratings yet
- Tips FengshuiDocument47 pagesTips FengshuiLilibeth Tenorio De LeonNo ratings yet
- Surgical Nutritions: Prepared By: Lilibeth C.Tenorio, M.DDocument33 pagesSurgical Nutritions: Prepared By: Lilibeth C.Tenorio, M.DLilibeth Tenorio De Leon100% (1)
- A Farmer Uses A Hand Tractor or Power Tiller Which Is Commonly Used For Land Preparation in Wetland RiceDocument5 pagesA Farmer Uses A Hand Tractor or Power Tiller Which Is Commonly Used For Land Preparation in Wetland RiceLilibeth Tenorio De LeonNo ratings yet
- Vestibular Handout FinalDocument2 pagesVestibular Handout Finalapi-414170492No ratings yet
- Caring For The Inner Child - AlchemyinstituteDocument6 pagesCaring For The Inner Child - AlchemyinstitutesalmazzNo ratings yet
- Dangerous DrugsDocument3 pagesDangerous DrugsTakisha Mcphee100% (2)
- Day in The Life of A Pharmacist PDFDocument3 pagesDay in The Life of A Pharmacist PDFjoanne_rawksNo ratings yet
- Bronchopulmonary DysplasiaDocument3 pagesBronchopulmonary Dysplasiabun_yulianaNo ratings yet
- Bhu 1Document10 pagesBhu 1Sriramvikas AthaluriNo ratings yet
- Multiple Atrophy System (MSA) Trust Caregiver's GuideDocument11 pagesMultiple Atrophy System (MSA) Trust Caregiver's GuideThe Multiple System Atrophy CoalitionNo ratings yet
- Cancer TerminatorDocument282 pagesCancer Terminatorandystark8100% (7)
- DipiroDocument38 pagesDipiroPetrick Ariska Pratama50% (2)
- CBT For Front Line Medical Professionals Using The Socratic MethodDocument44 pagesCBT For Front Line Medical Professionals Using The Socratic MethodNaya KatsaragakiNo ratings yet
- Bilastine ExpertOpinion JureguiDocument10 pagesBilastine ExpertOpinion JureguiAnisoara AvonNo ratings yet
- Control The Crazy by Vinny Guadagnino - ExcerptDocument10 pagesControl The Crazy by Vinny Guadagnino - ExcerptCrown Publishing Group0% (1)
- Divertikel - WehrmannDocument36 pagesDivertikel - WehrmannSake Cinema21No ratings yet
- NCP Anorexia NervosaDocument5 pagesNCP Anorexia NervosaJohn Ver Tolentino AdaoNo ratings yet
- Breastcrawl PDFDocument41 pagesBreastcrawl PDFRyan AndarestaNo ratings yet
- Cardiac TamponadeDocument6 pagesCardiac TamponadeJara Maris Moreno BudionganNo ratings yet
- Position Document Local Management Diabetic Foot UlcersDocument28 pagesPosition Document Local Management Diabetic Foot Ulcerspolin timiselaNo ratings yet
- FP Human Systems As Linguistic SystemsDocument15 pagesFP Human Systems As Linguistic SystemsEmilia MorosanNo ratings yet
- Atlas of PET:CT in Pediatric PatientsDocument248 pagesAtlas of PET:CT in Pediatric PatientsEmilija JanevikNo ratings yet
- 327overviewonthalassemias AreviewDocument14 pages327overviewonthalassemias AreviewAnonymous 8w9QEGNo ratings yet
- NNR2007 81 SfpassDocument11 pagesNNR2007 81 SfpassAyuNo ratings yet
- Theory and Research FrameworksDocument27 pagesTheory and Research FrameworkseroimperialNo ratings yet
- Attention Deficit Hyperactivity DisorderDocument4 pagesAttention Deficit Hyperactivity DisorderThata Thata100% (1)