Professional Documents
Culture Documents
Hepatitis Virus E
Hepatitis Virus E
Uploaded by
Ngakan Ketut DarmawanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hepatitis Virus E
Hepatitis Virus E
Uploaded by
Ngakan Ketut DarmawanCopyright:
Available Formats
ISBT Science Series (2011) 6, 344349
STATE OF THE ART
3C-S6-01
2011 The Author(s). ISBT Science Series 2011 International Society of Blood Transfusion
Hepatitis E virus infection and blood transfusion in Japan
K. Matsubayashi, H. Sakata & H. Ikeda
Japanese Red Cross Hokkaido Blood Center, Osaka, Japan
Nearly 30 years ago, a volunteer immune to hepatitis A virus (HAV) developed acute hepatitis after experimental ingestion of faecal suspension collected from nine acute phase patients from a water-borne outbreak of non-A, nonB hepatitis in Afghanistan. The virus-like particles (VLPs) different from hepatitis A and B viruses were visualized in his stool [1,2]. Despite serological and morphological evidences for the novel enterically transmitted non-A, non-B hepatitis virus, it was very difcult to identify the sequence of this virus because the viral load in stool samples was extremely low and insufcient for cloning and sequencing [2]. It needs to be noted that PCR was not available at that time. Using the bile sample of the experimentally infected monkey, cDNA of this virus was nally cloned and sequenced. The nucleotides sequence was not homologous to any in the GenBank database at that time [3] and named hepatitis E virus (HEV) after enterically transmitted hepatitis virus. A few years later, full length HEV genome was sequenced and determined (GenBank accession no. M73218) [4]. The epidemic of enterically transmitted non-A, non-B hepatitis in New Delhi, India in 1955 through 1956 was described rst as an epidemic of hepatitis E [5]. Large epidemics of HEV have been reported from many countries in Central, East and South East Asia, Central America and North and West Africa. HEV is the major cause of acute hepatitis in developing countries with insufcient sanitary conditions and is transmitted mainly by water-borne route in association with contaminated drinking water and food [6]. In general, hepatitis E is a self-limited disease and asymptomatic HEV infection is common. Typical clinical manifestation of hepatitis E is similar to that of acute viral hepatitis; anorexia, dark coloured urine, vomiting, fever, epigastric pain and jaundice. Severe hepatic failure and high mortality rate of nearly 20% among pregnant women in hepatitis E are observed only in endemic area, which is a distinctive feature of this disease and most important issue to be solved in endemic area. Recently, persistent HEV infection and chronic hepatitis E along with progression of liver inammation and brosis with HEV-related cirrhosis
Correspondence: Keiji Matsubayashi, Japanese Red Cross Hokkaido Blood Center, 2-2 Yamanote, Nishi-ku, Sapporo 063-0002, Japan E-mail: kmatsu@hokkaido.bc.jrc.or.jp
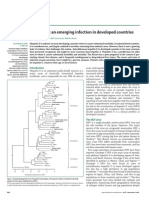
have been described in immunocompromised patients with lymphoma, recipients of organ transplant and patients with HIV infection [710]. HEV is a small spherical (2734 nm in diameter), nonenveloped virus with a single-stranded, positive-sense RNA genome of 72 kb which encodes three open reading frames (ORFs: ORF1, ORF2 and ORF3) between cap structure at 5end and poly-(A) tail at 3-end. The three ORFs encode for non-structural polyprotein, capsid protein and phosphorylated protein, respectively [11]. Although HEV has a single serotype, high genetic diversity of HEV genome is observed. HEV is classied into four major genotypes; genotype 1, 2, 3 and 4 [11]. Their features in epidemiology and virulence are different from each other (Table 1). Genotypes 1 and 2 are distributed in hyper endemic area in Asia, Central America and Africa and spread by water-borne route. In contrast, genotype 3 is found worldwide including Asia, North and South America, Europe and Oceania. Genotype 4 is restricted in East, South East Asia and rarely in Europe and seems to cause more severe hepatitis than genotype 3. Genotypes 3 and 4 are also isolated from sera, stool, liver and meat products of several animal species such as farmed pigs, wild boars and deer. Very recently, in addition to the four genotypes, other new genetic groups of HEV strain were isolated in wild boars in Japan [12,13]. Hepatitis E is diagnosed by detection of IgM, IgA, or IgG anti-HEV or HEV RNA. N-terminally truncated HEV capsid proteins can be efciently expressed and self-assembled as empty VLPs in insect cells infected with a recombinant baculovirus. The VLPs are used as immobilized antigens for the sensitive ELISA for HEV-specic antibodies [14]. Nested RT-PCR and real-time RT-PCR targeting ORF1 region or ORF2 3 overlapping region are used for detection of HEV RNA [1519]. Hepatitis E had been long considered as a disease of developing countries with poor sanitary conditions and recognized as an imported disease of travellers returned from the endemic area. However, recent evidences have indicated that autochthonous HEV infection occurs in developed countries including Japan, and appears to be more prevalent than previously thought. Hepatitis E patients without history of recent foreign travel were found in the USA and European countries and novel HEV strains of genotype 3, different from genotypes 1 and 2 in endemic area, were identied [2022]. At the same time, a novel
344
HEV infection and blood transfusion 345
swine HEV of genotype 3 was isolated from a pig in the USA which was closely related to human HEV of genotype 3 strains [23]. High prevalence of IgG anti-HEV was also observed in pig handlers in the USA [24]. These ndings suggested a possibility of autochthonous HEV infection as zoonosis in developed countries but it had been controversial whether HEV was a zoonotic agent or not. In Japan, a few years later, novel HEV strains of genotype 3 indigenous to Japan were isolated from a hepatitis patient with unknown aetiology and a farmed pig, respectively [15,16]. Following the discovery, many sporadic cases and several small outbreaks of HEV infection have been recognized in Japan and many Japan-indigenous HEV strains of genotype 3 and 4 have been identied in human as well as pigs, wild boars, deer, mongoose and bivalves Yamato-shijimi. Thus, HEV has a broad host range and pigs are recognized as an important reservoir of HEV. Furthermore, important studies on the route of transmission of HEV were reported from Japan. Members of two families developed hepatitis E after consumption of raw meat from Japanese Sika deer. HEV RNA sequences of genotype 3 isolated in their blood were identical to that in the leftover meat refrigerated in a freezer [25]. Although there had been several reports of the indirect evidences of HEV infection, this was the rst direct evidence of zoonotic infection of HEV from animal to human. Soon after the report by Tei S, et al. [25], Li TC et al. described another case report in which patients infected with HEV through consumption of wild boar meat contaminated with HEV of genotype 3 [26]. These ndings settled the debate over whether HEV is a zoonotic agent or not. Genotypes 3 and 4 of HEV are zoonotic agents. As many as 253 of incidents of HEV infection were extensively collected in Japan and analysed by a group led by Mishiro [27]. The status of HEV infection in Japan can be summarized briey as follows: (1) HEV infection spreads widely across Japan; (2) hepatitis E is a disease of middle-aged people with a predominance of male over female; (3) HEV strains of genotype 3 and 4 are autochthonous in Japan; (4) the older the age the severer the disease; (5) genotype 4 is associated with more obvious and severer clinical manifestations of hepatitis than genotype 3; (6) no seasonality in its incidence is observed; and (7) transmission routes remain unknown in approx. 60% cases, although about 30%, 8%, and 2% are ascribable to zoonotic food-borne transmission, imported infection, and bloodborne, respectively [27]. Thus, the status of HEV infection in Japan seems to be different from that in hyper endemic countries. Blood-borne transmission of HEV will be referred in more detail, next. As mentioned above, in hyper endemic area the route of transmission of HEV is extensively water-borne but a possibility of vertical transmission as well as blood-borne transmission has been suggested. In India, two cases of
transfusion-transmitted hepatitis E were reported by means of retrospective analyses [28]. However, they were unsuccessful in demonstrating the association of blood transfusion with hepatitis E infection by molecular approaches. We demonstrated for the rst time that transfusion-transmission hepatitis E existed even in a developed country by showing 100% sequence identity of HEV RNA genome both from a donor and a recipient in 2002 [29]. In this case, two blood products, fresh frozen plasma (FFP) and red cell concentrate (RCC) were derived from the HEV-positive blood. FFP was transfused to a patient and he developed hepatitis E. The nucleotide sequences of HEV isolated from the stored plasma and from the patient were identical and belonged to genotype 4 that was indigenous to Hokkaido, Japan. In contrast, the HEV-positive RCC that was transfused to another patient under immunosuppressed conditions did not cause any hepatitis symptoms. He was negative for any HEV markers on Day 130 after transfusion. The viral load of HEV in the RCC product could be too low to cause infection [29]. In Hokkaido, high prevalence of HEV RNA was observed in the donors with elevated ALT levels higher than 500 IU l (Fig. 1). Extensive epidemiological surveys for prevalence of anti-HEV antibodies were conducted in blood donors with elevated ALT levels higher than 200 IU l (n = 1389) and in qualied blood donors (n = 12 600) in Japan. The prevalence of IgG anti-HEV was 32% and 34% in these groups, respectively [30,31]. The studies revealed wide spread of autochthonous HEV infection among blood donors in Japan. HEV strains of
HAV (n = 1, 14%) HBV (n = 12, 162%) HCV (n = 9, 122%)
Negative (n = 36, 486%)
HEV (n = 11, 149%)
EBV (n = 3, 41%)
CMV (n = 3, 41%)
Fig. 1 Viruses determined among blood donors with elevated ALT levels higher than 500 IU l. Donated blood with ALT levels higher than 500 IU l were collected from April 2000 through March 2003 in Hokkaido, Japan (n = 74). In-house real-time PCR testing for HAV RNA, HBV DNA, HCV RNA, HEV RNA and EBV DNA and EIA (AxSYM CMV IgM; Abbott Laboratories, North Chicago, IL, US) for IgM anti-CMV were carried out.
2011 The Author(s). ISBT Science Series 2011 International Society of Blood Transfusion, ISBT Science Series (2011) 6, 344349
346 K. Matsubayashi et al.
14 genotype 3 and 1 genotype 4 were identied in blood donors with elevated ALT and most of them were shown to be indigenous to Japan by phylogenetic analysis and closely related to swine HEV strains in Japan [30]. A higher prevalence of IgG anti-HEV was observed in male donors, older donors and in donors residing in eastern Japan [31] (Fig. 2). In 2004, we experienced the second case of transfusiontransmission hepatitis E which was associated with zoonotic food-borne infection of HEV [19] (Fig. 3). The causative donor donated blood and his blood was disqualied because of elevated ALT. By the subsequent PCR testing, the blood turned out to be HEV-positive. Look back study of the HEV-positive donor revealed that the PC donated from him 2 weeks previously also contained HEV RNA and were transfused to a patient. Three weeks before the donation, he had a barbecue party at a restaurant with his 12 family members and they cooked pig liver and intestines as well as beef and chicken. Of 13 participants, seven including the causative donor and his father, who consumed pig liver and or intestines, were positive for IgM and or IgG anti-HEV. The father died of fulminant hepatitis E 2 months after the dinner. However, other members were asymptomatic. HEV isolates from the donor showed 999% homology with that from his father and the recipient based on nearly entire HEV genome. The HEV isolates were genotype 4 that was indigenous to Hokkaido. In the recipient, the progress of HEV markers as well as liver function markers in the entire course were demonstrated; HEV RNA
was detected in serum on Day 22 and reached the peak of 72 log copies ml on Day 44 followed by the steep increase of ALT. AST and ALT increased at highest levels of 903 and 673 IU l on Day 59, respectively. IgG anti-HEV emerged on Day 67; subsequently, hepatitis was resolved. HEV RNA was detectable up to Day 97 in serum, Day 85 in faeces, and Day 71 in saliva. The results for saliva suggest that besides faecaloral route, oraloral transmission mode might be another route of human-to-human infection of HEV, although further studies are needed. Thereafter, nucleic acid-based screening for HEV was started experimentally, although limited in Hokkaido, (1) in order to exclude donors infected with HEV and (2) to nd out asymptomatic HEV carriers among blood donors. Since January 2005, in-house real-time RT-PCR system has been implemented and nearly 300 thousands of blood donors who passed the serological tests for HBV, HCV and HIV 1 2 and with ALT levels under 60 IU l are 20-pooled and tested for the presence of HEV RNA annually. The prevalence of HEV RNA among the blood donors in Hokkaido is approx. 0012%. Male dominance and no seasonality are observed throughout the years. Almost half of the HEVpositive donors cause ALT elevation but most of them are asymptomatic. Phylogenetic analyses indicated that HEV isolates from the positive donors belong to genotype 3 or 4, both of which seem to be indigenous to Hokkaido or its neighbouring area. Genotype 3 is more prevalent than genotype 4. More than half of the positive donors have an eating history of animal viscera before blood donation,
(a) Age group
n = 12 600; n = 1050 each of age group and gender 88
Positivity rate (%)
10 8 6 4 2 0
03 07 07 13
Male Female
28 20 45 41 41
67 53 4 0
P = 0002 39 29
1619
2029
3039
4049
5059
6069
Total
(b) Region
Hokkaido
n = 12 600; n = 900 each of region and gender 90 Fukuoka Osaka Okayama Aichi 09 Miyagi Tokyo 31 33 53 36 47 32 81
Positivity rate (%)
10 8 6 4 2 0 Fukuoka Okayama Osaka Aichi West/south Japan, 18%
23 10
18 02
13
Tokyo Miyagi Hokkaido East/north Japan, 56%
Fig. 2 Prevalence of IgG anti-HEV in qualied Japanese blood donors. Serum samples were collected from qualied Japanese blood donors with ALT level of 60 IU l or lower and tested negative for all the current blood screening tests for HBV, HCV, HIV-1 2, HTLV-1, syphilis and human parvovirus B19 at the seven JRC blood centres in Hokkaido, Miyagi, Tokyo, Aichi, Osaka, Okayama and Fukuoka from November 2005 through February 2006 (n = 12 600). The samples at each blood centre were collected separately by age group and by sex, resulting in 150 male and 150 female samples in each age group (a total of 1800 samples per centre). Positivity rate was summarized by age group (a) and by region (b) [31].
2011 The Author(s). ISBT Science Series 2011 International Society of Blood Transfusion, ISBT Science Series (2011) 6, 344349
HEV infection and blood transfusion 347
Fig. 3 Transfusion-transmitted hepatitis E in 2004 [19].
Table 1 Characteristics of four HEV genotypes Genotype Geographical distribution 1 Asia Africa 2 Central America (Mexico) Africa (Nigeria and Chad) 3 Asia America Europe Oceania Zoonotic food-borne (from pig, wild boar and deer) Sporadic small outbreak Modest Chronic hepatitis in immunocompromised patients Middle-aged adults (men > women) 4 Asia (China, Japan, Korea, Vietnam, Taiwan, Indonesia and India) Europe (Germany, Belgium) Zoonotic food-borne (from pig and wild boar) Sporadic small outbreak Severe Acute Fulminant hepatitis in old-aged males Middle-aged adults (men > women)
Modes of transmission
Disease pattern Clinical features
Water-borne Vertical-transmission (?) Contact (?) Epidemic Modest Fulminant hepatitis in pregnant women Young adults
Water-borne
Epidemic Modest
Prevalent age group
Young adults
suggesting it may be associated with zoonotic HEV infection. Only in the rst year of HEV NAT screeninng, from January 2005 through February 2006, it took about 1 week until the results came out, therefore several HEV-positive blood products such as PC and RCC having short shelf life were occasionally released and transfused before the results were available. Seven cases of transfusion of HEV-positive blood occurred in the period and two patients developed hepatitis E after transfusion. Since March 2006, HEV NAT has been applied only to qualied donors and the results come out timely together with other NAT results for HBV, HCV and HIV. Thereafter, the blood products tested positive for HEV RNA have never been released so far.
In addition to our four cases in Hokkaido, two cases of HEV transmission via transfusion were reported in the different parts of Japan [7,32]. Furthermore, three bags of source plasma sent to a manufacturer of plasma-derived medicinal products from JRC were disqualied for the presence of HEV RNA. In response to the information, JRCs look-back surveys identied the causative donors and revealed that their blood products derived from the donations had been already transfused to three patients and they caused HEV infection. In Europe, two posttransfusion HEV infections were reported in UK [33] and France [34]. In summary, subclinical HEV infection spreads worldwide not only in endemic countries but also in developed
2011 The Author(s). ISBT Science Series 2011 International Society of Blood Transfusion, ISBT Science Series (2011) 6, 344349
348 K. Matsubayashi et al.
countries. Our HEV studies indicate that autochthonous HEV infection is constantly undergoing and that there was a small but signicant risk of blood-borne transmission of HEV at least in Hokkaido, Japan before implementation of NAT screening for HEV. Since the prevalence of IgG antibody to HEV in other non-endemic countries in Europe and North America is comparable to that of Japan, HEV infection may be undergoing there, too. In fact, approx. 10% (4 41) of plasma fractionation pools obtained from Europe and North America were positive for HEV RNA [35]. Hepatitis E is one of emerging infectious diseases and HEV infection should not be negligible even in non-endemic countries. Further epidemiological and clinical studies are necessary to be performed.
Disclosures
No potential conict of interests to declare.
References
1 Balayan MS, Andjar AG, Savinskaya SS, et al.: Evidence for a virus in non-A, non-B hepatitis transmitted via the fecal-oral route. Intervirology 1983; 20:2331 2 Khuroo MS: Discovery of hepatitis E: The epidemic non-A, non-B hepatitis 30 years down the memory lane. Virus Res 2011. (On-line published, in press). PMID: 21320558. 3 Reyes GR, Purdy MA, Kim JP, et al.: Isolation of a cDNA from the virus responsible for enterically transmitted non-A, non-B hepatitis. Science 1990; 247:13351339 4 Tam AW, Smith MM, Guerra ME, et al.: Hepatitis E virus (HEV): Molecular cloning and sequencing of the full-length viral genome. Virology 1991; 185:120131 5 Purcell RH: Hepatitis E virus; in Fields BN, Knipe DM, Howley PM (eds): Fields Virology, 3rd edn. Philadelphia: LippincottRaven, 1996:28312843 6 Panda SK, Thakral D, Rehman S: Hepatitis E virus. Rev Med Virol 2007; 17:151180 7 Tamura A, Shimizu YK, Tanaka T, et al.: Persistent infection of hepatitis E virus transmitted by blood transfusion in a patient with T-cell lymphoma. Hepatol Res 2007; 37:113120 8 Ollier L, Tieulie N, Sanderson F, et al.: Chronic hepatitis after hepatitis E virus infection in a patient with non-Hodgkin lymphoma taking rituximab. Ann Intern Med 2009; 150:430431 9 Kamar N, Selves J, Mansuy JM, et al.: Hepatitis E virus and chronic hepatitis in organ-transplant recipients. N Engl J Med 2008; 358:811817 10 Dalton HR, Bendall RP, Keane FE, et al.: Persistent carriage of hepatitis E virus in patients with HIV infection. N Engl J Med 2009; 361:10251027 11 Schlauder GG, Mushahwar IK: Genetic heterogeneity of hepatitis E virus. J Med Virol 2001; 65:282292 12 Takahashi K, Terada S, Kokuryu H, et al.: A wild boar-derived hepatitis E virus isolate presumably representing so far unidentied genotype 5. Kanzo 2010; 51:536538
13 Takahashi M, Nishizawa T, Sato H, et al.: Analysis of the fulllength genome of a hepatitis E virus isolate obtained from a wild boar in Japan that is classiable into a novel genotype. J Gen Virol 2011; 92:902908 14 Li TC, Suzuki K, Yamakawa Y, et al.: Expression and selfassembly of empty virus-like particles of hepatitis E virus. J Virol 1997; 71:72077213 15 Takahashi K, Iwata K, Watanabe N, et al.: Full genome nucleotide sequence of a hepatitis E virus strain that may be indigenous to Japan. Virology 2001; 287:912 16 Okamoto H, Takahashi M, Nishizawa T, et al.: Analysis of the complete genome of indigenous swine hepatitis E virus isolated in Japan. Biochem Biophys Res Commun 2001; 289:929 936 17 Mizuo H, Suzuki K, Tokikawa Y, et al.: Polyphyletic strains of hepatitisEvirus are responsible for sporadic cases of acute hepatitis in Japan. J Clin Microbiol 2002; 40:32093218 18 Jothikumar N, Cromeans TL, Robertson BH, et al.: A broadly reactive one-step real-time RT-PCR assay for rapid and sensitive detection of hepatitis E virus. J Virol Methods 2006; 131:6571 19 Matsubayashi K, Kang JH, Sakata H, et al.: A case of transfusion-transmitted hepatitis E caused by blood from a donor infected with hepatitis E virus via zoonotic food-borne route. Transfusion 2008; 48:13681375 20 Kwo PY, Schlauder GG, Carpenter HA, et al.: Acute hepatitis E by a new isolate acquired in the United States. Mayo Clin Proc 1997; 72:11331136 21 Schlauder GG, Dawson GJ, Erker JC, et al.: The sequence and phylogenetic analysis of a novel hepatitis E virus isolated from a patient with acute hepatitis reported in the United States. J Gen Virol 1998; 79:447456 22 Schlauder GG, Desai SM, Zanetti AR, et al.: Novel hepatitis E virus (HEV) isolated from Europe: evidence for additional genotypes of HEV. J Med Virol 1999; 57:243251 23 Meng XJ, Purcell RH, Halbur PG, et al.: A novel virus in swine is closely related to the human hepatitis E virus. Proc Natl Acad Sci USA 1997; 94:98609865 24 Meng XJ, Wiseman B, Elvinger F, et al.: Prevalence of antibodies to hepatitis E virus in veterinarians working with swine and in normal blood donors in the United States and other countries. J Clin Microbiol 2002; 40:117122 25 Tei S, Kitajima N, Takahashi K, et al.: Zoonotic transmission of hepatitis E virus from deer to human beings. Lancet 2003; 362:371373 26 Li TC, Chijiwa K, Sera N, et al.: Hepatitis E virus transmission from wild boar meat. Emerg Infect Dis 2005; 11:1958 1960 27 Abe T, Aikawa T, Akahane Y, et al.: Demographic, epidemiological and virological characteristics of hepatitis E virus infections in Japan based on 254 human cases collected nationwide. Kanzo 2006; 47:384391 28 Arankalle VA, Chobe MS: Retrospective analysis of blood transfusion recipients: evidence for post-transfusion hepatitis E. Vox Sang 2000; 79:7274 29 Matsubayashi K, Nagaoka Y, Sakata H, et al.: Transfusiontransmitted hepatitis E caused by apparently indigenous
2011 The Author(s). ISBT Science Series 2011 International Society of Blood Transfusion, ISBT Science Series (2011) 6, 344349
HEV infection and blood transfusion 349
hepatitis E virus strain in Hokkaido, Japan. Transfusion 2004; 44:934940 30 Sakata H, Matsubayashi K, Takeda H, et al.: A nationwide survey for hepatitis E virus prevalence in Japanese blood donors with elevated alanine aminotransferase. Transfusion 2008; 48:25682576 31 Takeda H, Matsubayashi K, Sakata H, et al.: A nationwide survey for prevalence of hepatitis E virus antibody in qualied blood donors in Japan. Vox Sang 2010; 99:307313 32 Mitsui T, Tsukamoto Y, Yamazaki C, et al.: Prevalence of hepatitis E virus infection among hemodialysis patients in Japan:
evidence for infection with a genotype 3 HEV by blood transfusion. J Med Virol 2004; 74:56372 33 Boxall E, Herborn A, Kochethu G, et al.: Transfusion-transmitted hepatitis E in a nonhyperendemic country. Transfus Med 2006; 16:7983 34 Colson P, Coze C, Gallian P, et al.: Transfusion-associated hepatitis E, France. Emerg Infect Dis 2007; 13:6486499 , Nick S, et al.: Widespread distribution of 35 Baylis SA, Koc O hepatitis E virus in plasma fractionation pools. Vox Sang 2011 (In press). doi: 10.1111/j.1423-0410.2011.01527.x. PMID: 21806631.
2011 The Author(s). ISBT Science Series 2011 International Society of Blood Transfusion, ISBT Science Series (2011) 6, 344349
You might also like
- Handbook of Bird BiologyDocument659 pagesHandbook of Bird BiologyNoriane RhouyNo ratings yet
- Horse Racing System - Turf Anaylist The Indicator Handicapping MethodDocument24 pagesHorse Racing System - Turf Anaylist The Indicator Handicapping Methodartus1480% (10)
- Boericke Materia MédicaDocument597 pagesBoericke Materia MédicaJarib Mervich Jiménez100% (17)
- Hepatitis E Springer Nature 2020 1Document11 pagesHepatitis E Springer Nature 2020 1azael11071991No ratings yet
- HEV StudyDocument12 pagesHEV StudyjackalackaNo ratings yet
- Hepatite EDocument22 pagesHepatite EYmirNo ratings yet
- Acute HEV Hepatitis: Clinical and Laboratory DiagnosisDocument7 pagesAcute HEV Hepatitis: Clinical and Laboratory Diagnosissouth streamNo ratings yet
- Grabow, Taylor - 1996 - Hepatitis E Virus in South AfricaDocument6 pagesGrabow, Taylor - 1996 - Hepatitis E Virus in South AfricaStephen KorsmanNo ratings yet
- Hepatitis Infection: An UpdateDocument48 pagesHepatitis Infection: An UpdateManuel CastilloNo ratings yet
- Article in Press: Hepatitis A Related Acute Liver Failure by Consumption of Contaminated FoodDocument3 pagesArticle in Press: Hepatitis A Related Acute Liver Failure by Consumption of Contaminated Foodeclipse1712No ratings yet
- Donor-Derived Genotype 4 Hepatitis E Virus Infection, Hong Kong, China, 2018Document9 pagesDonor-Derived Genotype 4 Hepatitis E Virus Infection, Hong Kong, China, 2018south streamNo ratings yet
- Hepatitis E Virus: A Review: P. Vasickova, I. Psikal, P. Kralik, F. Widen, Z. Hubalek, I. PavlikDocument20 pagesHepatitis E Virus: A Review: P. Vasickova, I. Psikal, P. Kralik, F. Widen, Z. Hubalek, I. Pavlikyo4nutzNo ratings yet
- Zoonotic and Foodborne Trnasmition of Hepatitis EDocument9 pagesZoonotic and Foodborne Trnasmition of Hepatitis Ejulma1306No ratings yet
- Hepatitis E Virus Songtanin 2023Document22 pagesHepatitis E Virus Songtanin 2023rootscriptureNo ratings yet
- 2017.08.10 - Prof. Suwandhi - Hepatitis EDocument32 pages2017.08.10 - Prof. Suwandhi - Hepatitis EAdelaTeresaNo ratings yet
- Keane Et Al-2012-HIV MedicineDocument6 pagesKeane Et Al-2012-HIV Medicinejulma1306No ratings yet
- First Clinical Case of Equine Parvovirus-Hepatitis-Related Theiler's Disease in AsiaDocument9 pagesFirst Clinical Case of Equine Parvovirus-Hepatitis-Related Theiler's Disease in AsiaMaría F. Naranjo OrtízNo ratings yet
- Viral Hepatitis: Juliana Chan, Pharm.DDocument26 pagesViral Hepatitis: Juliana Chan, Pharm.DSuneil R AlsNo ratings yet
- Abo/Rh Blood Groups and Risk of Hiv Infection and Hepatitis B Among Blood Donors of Abidjan, Côte D'IvoireDocument5 pagesAbo/Rh Blood Groups and Risk of Hiv Infection and Hepatitis B Among Blood Donors of Abidjan, Côte D'Ivoirehusain albaqaliNo ratings yet
- 2020 Viral Hepatitis - StatPearls - NCBI BookshelfDocument7 pages2020 Viral Hepatitis - StatPearls - NCBI BookshelfamyNo ratings yet
- Hep E DR. SOMNATH MUKHERJEEDocument38 pagesHep E DR. SOMNATH MUKHERJEESuprnatrlNo ratings yet
- 2020-Vol 3Document14 pages2020-Vol 3BSRNo ratings yet
- High Mortality Associated With An Outbreak of Hepatitis E Among Displaced Persons in Darfur, SudanDocument6 pagesHigh Mortality Associated With An Outbreak of Hepatitis E Among Displaced Persons in Darfur, SudanKatrina ManurungNo ratings yet
- Viral Hepatitis - Pragmatic Approach To Its Challenge in IndiaDocument3 pagesViral Hepatitis - Pragmatic Approach To Its Challenge in IndiabagusNo ratings yet
- Acute Viral HepatitisDocument66 pagesAcute Viral HepatitisIfabiyi OlaniyiNo ratings yet
- Hepatitis E Virus (HEV) - Specific T-Cell Responses Are Associated With Control of HEV InfectionDocument14 pagesHepatitis E Virus (HEV) - Specific T-Cell Responses Are Associated With Control of HEV Infectionchanchalv_678018469No ratings yet
- 1 HEV Burden Paper Final 03 Oct 14 Yellow BookDocument20 pages1 HEV Burden Paper Final 03 Oct 14 Yellow BookTippu NawazNo ratings yet
- 17akinbolaji EtalDocument5 pages17akinbolaji EtaleditorijmrhsNo ratings yet
- Hepatitis E - ArticleDocument3 pagesHepatitis E - ArticleMichelle A. DegrandezNo ratings yet
- Hepatitis EDocument7 pagesHepatitis EmdNo ratings yet
- Arboviruses in ChinaDocument21 pagesArboviruses in ChinaChris LicínioNo ratings yet
- Hepatitis A-PrintDocument17 pagesHepatitis A-PrintVirginia EchoNo ratings yet
- Hep BDocument5 pagesHep BPolichonNo ratings yet
- Background: Cirrhosis Hepatocellular Carcinoma (HCC)Document24 pagesBackground: Cirrhosis Hepatocellular Carcinoma (HCC)Ignatius Rheza SetiawanNo ratings yet
- Hepatitis E InfectionDocument27 pagesHepatitis E Infectiontummalapalli venkateswara raoNo ratings yet
- Jana-2018-ABO & RH Blood Groups' DistributionDocument6 pagesJana-2018-ABO & RH Blood Groups' DistributionKemo JakNo ratings yet
- Acute Hepatitis A Virus Infection Presenting With Multiorgan Dysfunction: A Case ReportDocument3 pagesAcute Hepatitis A Virus Infection Presenting With Multiorgan Dysfunction: A Case ReportHananti AhhadiyahNo ratings yet
- Hel 12514Document6 pagesHel 12514perisici4_535458722No ratings yet
- Investigation of An Epidemic of Hepatitis E in Nellore in South IndiaDocument7 pagesInvestigation of An Epidemic of Hepatitis E in Nellore in South IndiaShaileshNo ratings yet
- TMPCFBF TMPDocument3 pagesTMPCFBF TMPFrontiersNo ratings yet
- Hep E DR. SOMNATH MUKHERJEEDocument38 pagesHep E DR. SOMNATH MUKHERJEESuprnatrlNo ratings yet
- WHO - Ebola Virus Disease (Evd) Key FactsDocument6 pagesWHO - Ebola Virus Disease (Evd) Key FactsBeatrice IoanaNo ratings yet
- Hepatitis A and E Virus Infections Among Children in MongoliaDocument4 pagesHepatitis A and E Virus Infections Among Children in MongoliaGunbilig DisanNo ratings yet
- (Part 2) Potential Zoonotic Bat-Borne Disease in Indonesia - Yan Newsletter Feb 2022Document7 pages(Part 2) Potential Zoonotic Bat-Borne Disease in Indonesia - Yan Newsletter Feb 2022YanMardianNo ratings yet
- HashmatDocument9 pagesHashmatSHAFIQNo ratings yet
- 2019 Article 1119Document11 pages2019 Article 1119south streamNo ratings yet
- Schistosomiasis Case StudyDocument5 pagesSchistosomiasis Case Studyapi-318749549No ratings yet
- Case Report: Acute Hepatitis E in A Pediatric Traveler Presenting With Features of Autoimmune Hepatitis: A Diagnostic and Therapeutic ChallengeDocument4 pagesCase Report: Acute Hepatitis E in A Pediatric Traveler Presenting With Features of Autoimmune Hepatitis: A Diagnostic and Therapeutic Challengeanjingbasah 24No ratings yet
- SumberDocument50 pagesSumberahmad munifNo ratings yet
- Elena HepDocument2 pagesElena HepMirela IoanaNo ratings yet
- Hepatitis e IDocument11 pagesHepatitis e IJenny Granados ChávezNo ratings yet
- The Biology and Pathogenesis of Hepatitis Viruses: Current Science February 2010Document15 pagesThe Biology and Pathogenesis of Hepatitis Viruses: Current Science February 2010AyaNo ratings yet
- Bo Kazha NovaDocument8 pagesBo Kazha NovaYudha Baskara ArdhaputraNo ratings yet
- Viral Hepatitis A eDocument6 pagesViral Hepatitis A eSokheng ThyNo ratings yet
- Perio2000 2007 MTYinDocument27 pagesPerio2000 2007 MTYinmin moongNo ratings yet
- Hepatitis E Virus Seropositivity in An Ethnically Diverse Community Blood Donor PopulationDocument7 pagesHepatitis E Virus Seropositivity in An Ethnically Diverse Community Blood Donor Populationadmir4No ratings yet
- Khairunisa SQ Et Al Text Rev mk2 MF Ayu Cleared MIDocument26 pagesKhairunisa SQ Et Al Text Rev mk2 MF Ayu Cleared MILuqman HakimNo ratings yet
- Oropouche Virus As An Emerging Cause of Acute Febrile Illness in ColombiaDocument14 pagesOropouche Virus As An Emerging Cause of Acute Febrile Illness in Colombiajuliana22004No ratings yet
- Discuss The Microbial Threats To Transfusion Safety and The Procedures That The Transfusion Service Takes To Avoid Their TransmissionDocument3 pagesDiscuss The Microbial Threats To Transfusion Safety and The Procedures That The Transfusion Service Takes To Avoid Their TransmissionAlison HinesNo ratings yet
- Lec 9Document26 pagesLec 9Ghadi AbdalazizNo ratings yet
- HepeDocument6 pagesHepegmustafaNo ratings yet
- Seasonality of Hepatitis ADocument5 pagesSeasonality of Hepatitis AHaydas ChannelNo ratings yet
- Viral Hepatitis: Acute HepatitisFrom EverandViral Hepatitis: Acute HepatitisResat OzarasNo ratings yet
- G3 (Lesson 1-12)Document4 pagesG3 (Lesson 1-12)Nhung HoangNo ratings yet
- DFTR 4 OiDocument28 pagesDFTR 4 OiJoshua LindseyNo ratings yet
- Idoc - Pub - Dental Anatomy Questions PDFDocument16 pagesIdoc - Pub - Dental Anatomy Questions PDFhieulee84No ratings yet
- Sample Proposal 1 - DengueDocument8 pagesSample Proposal 1 - Dengueazliothman100% (1)
- Anr 0135Document44 pagesAnr 0135amokhtaNo ratings yet
- MCQ FMS4 2009 FixDocument18 pagesMCQ FMS4 2009 Fixdanielgunawan92No ratings yet
- Confusing Pairs...Document6 pagesConfusing Pairs...Nathan HudsonNo ratings yet
- "Pratff (1T-I Rti I) WR - : OrderDocument1 page"Pratff (1T-I Rti I) WR - : OrderKishore Kumar ShahNo ratings yet
- USDF 2015 TrainingLevelTest3Document2 pagesUSDF 2015 TrainingLevelTest3PuertoRicoEcuestreNo ratings yet
- Ruth ReportDocument51 pagesRuth ReportJhoy GongobNo ratings yet
- Introduction To ZoologyDocument4 pagesIntroduction To Zoologymarketing dvcNo ratings yet
- Repaso Examen Laboratorio ZOOLOGIADocument12 pagesRepaso Examen Laboratorio ZOOLOGIAcaripukisNo ratings yet
- APKC Dog Show Entry FormDocument1 pageAPKC Dog Show Entry Formrana-atheya-1338No ratings yet
- Contractor Injury Report FormDocument2 pagesContractor Injury Report Formmohamed11111981100% (1)
- CH 11Document66 pagesCH 11Vincents Genesius EvansNo ratings yet
- Useful Informations CancelledRC PanipatDocument57 pagesUseful Informations CancelledRC PanipatRavi KumarNo ratings yet
- Past SimpleDocument3 pagesPast SimpleInês Margarida PereiraNo ratings yet
- Toradora! Volume 04Document134 pagesToradora! Volume 04rmhwindNo ratings yet
- Cambridge Primary Progression Test: English Question Paper 1 InsertDocument4 pagesCambridge Primary Progression Test: English Question Paper 1 InsertHossam100% (1)
- Kisi Kisi Bahasa Inggris Kls 8Document3 pagesKisi Kisi Bahasa Inggris Kls 8Ayin KatiliNo ratings yet
- Pet MockDocument18 pagesPet MockRob101010No ratings yet
- Sedalia Bazoo84Document1 pageSedalia Bazoo84CarterHintzNo ratings yet
- Q. 1 - Q. 5 Carry One Mark Each.: GATE 2016 General Aptitude - GA Set-8Document6 pagesQ. 1 - Q. 5 Carry One Mark Each.: GATE 2016 General Aptitude - GA Set-8RavikanthNo ratings yet
- Programme Ipvs2024Document45 pagesProgramme Ipvs2024Gabriela Piovesan ZaninNo ratings yet
- Skeletal System Lesson PlanDocument10 pagesSkeletal System Lesson PlanNicketa AndersonNo ratings yet
- Reading Comprehension Exercise Read The Text Below and Answer The Questions ! Blue WhaleDocument3 pagesReading Comprehension Exercise Read The Text Below and Answer The Questions ! Blue WhaleMuhammad GemmaNo ratings yet
- Nervous System LessonDocument18 pagesNervous System Lessonapi-270448768No ratings yet