Professional Documents
Culture Documents
Chapter 12
Chapter 12
Uploaded by
newmexicoomfsCopyright:
Available Formats
You might also like
- Index Fund Investing 101Document100 pagesIndex Fund Investing 101newmexicoomfs100% (9)
- CCDM Manual PDFDocument715 pagesCCDM Manual PDFrehanaNo ratings yet
- Med Surg Test 4 Study GuideDocument29 pagesMed Surg Test 4 Study GuideJess100% (2)
- Dental SchoolDocument5 pagesDental SchoolnewmexicoomfsNo ratings yet
- 97Document79 pages97HATLERNo ratings yet
- 1 Path of The LiverDocument97 pages1 Path of The LiverLucas AresNo ratings yet
- Hepatobiliary Diseases 3Document28 pagesHepatobiliary Diseases 3AmirahNo ratings yet
- Askep SirosisDocument73 pagesAskep SirosisRisma Yuliana PratiwiNo ratings yet
- Cirrhosis 22008 Bajar Musica Gratis Descargar Musica Gratis Online Descargar Musica Gratis para CelularesDocument72 pagesCirrhosis 22008 Bajar Musica Gratis Descargar Musica Gratis Online Descargar Musica Gratis para CelularesYeni Chie Aneuk TuleutNo ratings yet
- With Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Document72 pagesWith Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Ainun JaariahNo ratings yet
- Approach To Cholestatic Jaundice: DR - Ram Raut - JR III (Medicine) Guide - Dr.D.B. Kadam Seminar Teacher-Dr - NitinDocument68 pagesApproach To Cholestatic Jaundice: DR - Ram Raut - JR III (Medicine) Guide - Dr.D.B. Kadam Seminar Teacher-Dr - NitinAnan JaiswalNo ratings yet
- 3 Liver CirrhosisDocument50 pages3 Liver CirrhosisKamal AhmedNo ratings yet
- With Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Document72 pagesWith Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Darin MonerNo ratings yet
- Lect. 8Document30 pagesLect. 8jayNo ratings yet
- 15 LivernDocument45 pages15 LivernDrAbdullrabAlmarwanyaNo ratings yet
- QUIBOD LiverDocument32 pagesQUIBOD LiverAileen Grace DelimaNo ratings yet
- Liver Cirrohsis (Lecture)Document87 pagesLiver Cirrohsis (Lecture)Rina Sundari Dels100% (1)
- Liver NotesDocument2 pagesLiver NotesAnne IsheeNo ratings yet
- Liver CirrhosisDocument16 pagesLiver CirrhosisBabesNo ratings yet
- Liver LecDocument107 pagesLiver LecNMD LIFESAVERNo ratings yet
- The Diseases of The Liver: Department of Pediatric Allergy, Gastroenterology and NutritionDocument125 pagesThe Diseases of The Liver: Department of Pediatric Allergy, Gastroenterology and NutritionlindaNo ratings yet
- Presented by Mr. Vinay Kumar M.Sc. Nursing 1 Year HCN, SrhuDocument66 pagesPresented by Mr. Vinay Kumar M.Sc. Nursing 1 Year HCN, SrhuVinay Kumar100% (2)
- Obstructive Jaundice: DR Nanteza SumayiyaDocument26 pagesObstructive Jaundice: DR Nanteza SumayiyaNinaNo ratings yet
- Hepatobiliary DiseaseDocument60 pagesHepatobiliary DiseaseFirdaus AslamNo ratings yet
- Liver CirrhosisDocument50 pagesLiver Cirrhosischai rinNo ratings yet
- Liver CirrohosisDocument157 pagesLiver CirrohosisSeema SachdevaNo ratings yet
- Hepatobiliary System: BY Pranjal Kulkarni Neha ManeDocument85 pagesHepatobiliary System: BY Pranjal Kulkarni Neha ManeGurneetNo ratings yet
- Pathology of The Liver, Biliary Tract andDocument64 pagesPathology of The Liver, Biliary Tract andembeoyabarareNo ratings yet
- 12.0 Care of Clients With Hepato Biliary and Pancreatic DisorderDocument68 pages12.0 Care of Clients With Hepato Biliary and Pancreatic DisorderJanna Niña ElementoNo ratings yet
- Gall Bladder and Bile DuctDocument18 pagesGall Bladder and Bile DuctClint MorrisonNo ratings yet
- Gallstone DiseaseDocument28 pagesGallstone DiseaseNurmalia PutriNo ratings yet
- Liver, Biliary Tract and Pancreas ProblemsDocument95 pagesLiver, Biliary Tract and Pancreas ProblemsBav VAansoqnuaetzNo ratings yet
- Pathology of The Liver: Systems Pathology II-PA5402 Dr. Khan T-W-RDocument78 pagesPathology of The Liver: Systems Pathology II-PA5402 Dr. Khan T-W-RCrystal Lynn Keener SciariniNo ratings yet
- Surgical Diseases of Liver1Document54 pagesSurgical Diseases of Liver1DR MOHAMED HEALTH CHANNELNo ratings yet
- Genitourinary ObjectivesDocument38 pagesGenitourinary Objectivescwumspa14No ratings yet
- Disorders of The Hepatobiliary System: Dr. Mehzabin AhmedDocument27 pagesDisorders of The Hepatobiliary System: Dr. Mehzabin Ahmedbpt2100% (1)
- Liver TransplantationDocument21 pagesLiver TransplantationRozi RamliNo ratings yet
- MetabolismDocument39 pagesMetabolismTiffany KnepperNo ratings yet
- Urea/ Ammonia Tests: Primary Liver Function TestsDocument6 pagesUrea/ Ammonia Tests: Primary Liver Function TestsMemory MahwendaNo ratings yet
- Liver Pathology PDFDocument7 pagesLiver Pathology PDFjohn smithNo ratings yet
- Etiologi Dan Patogenesis Ikterus,...Document103 pagesEtiologi Dan Patogenesis Ikterus,...Raditya PrimaNo ratings yet
- Hepatic CirrhosisDocument20 pagesHepatic CirrhosisAnifowose samsonNo ratings yet
- MedSurg NotesDocument21 pagesMedSurg NotesShanny BNo ratings yet
- NCM Lecture (Liver and Gallbladder)Document76 pagesNCM Lecture (Liver and Gallbladder)beer_ettaaNo ratings yet
- Urinary Symptoms - DR RashaDocument70 pagesUrinary Symptoms - DR RashaRasha TelebNo ratings yet
- 3.liver & Biliary TractDocument141 pages3.liver & Biliary TractBobi WijayaNo ratings yet
- Hepatic Disorders: R2 Thanaporn ChittipanichDocument42 pagesHepatic Disorders: R2 Thanaporn ChittipanichMimmey Yeniw100% (1)
- Hepatic and Biliary DisordersDocument103 pagesHepatic and Biliary Disordersramasalem1975No ratings yet
- Urine Dipstick Testing + Common Renal Problem 2012Document52 pagesUrine Dipstick Testing + Common Renal Problem 2012Ainul ArinaNo ratings yet
- Liver CirrhosisDocument83 pagesLiver CirrhosisRusiana NasilahNo ratings yet
- اليزيد UrinalysisDocument48 pagesاليزيد UrinalysisRa'aft Al-SamawiNo ratings yet
- Cirrhosis of LiverDocument106 pagesCirrhosis of LiveraahadNo ratings yet
- Sirosis Hepatis: Sigit Widyatmoko Fakultas Kedokteran UMSDocument66 pagesSirosis Hepatis: Sigit Widyatmoko Fakultas Kedokteran UMSArif Rahman DmNo ratings yet
- Obstructive Jaundice Group 6Document33 pagesObstructive Jaundice Group 6Qurbon AliNo ratings yet
- OUM Tutorial 1 SBNS3504 RenalDocument51 pagesOUM Tutorial 1 SBNS3504 RenalMashanimy HoneyNo ratings yet
- Case of Obstructive JaundiceDocument38 pagesCase of Obstructive JaundiceJay R Plogio100% (2)
- Liver Disorders-II Jaundice 3Document14 pagesLiver Disorders-II Jaundice 3Daksh SabharwalNo ratings yet
- Notes Liver CirrhosisDocument10 pagesNotes Liver CirrhosisSanthu Su100% (1)
- The Incidence of Esophageal Varices in Patients With CirrhosisDocument31 pagesThe Incidence of Esophageal Varices in Patients With CirrhosisDenata PrabhasiwiNo ratings yet
- Urinalysis and Body Fluids2020Document47 pagesUrinalysis and Body Fluids2020MONFOLA100% (2)
- Hepato-Biliary System and Their DisordersDocument131 pagesHepato-Biliary System and Their DisordersIton BumatayNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Obturation of The Root Canal: Capital EndodonticsDocument36 pagesObturation of The Root Canal: Capital EndodonticsnewmexicoomfsNo ratings yet
- Metallurgy & File Classification: Capital EndodonticsDocument26 pagesMetallurgy & File Classification: Capital EndodonticsnewmexicoomfsNo ratings yet
- Vortex Blue Instrumentation: Capital EndodonticsDocument16 pagesVortex Blue Instrumentation: Capital EndodonticsnewmexicoomfsNo ratings yet
- Entry Point I Entry Point II Entry Point IIIDocument1 pageEntry Point I Entry Point II Entry Point IIInewmexicoomfsNo ratings yet
- Trushape Instrumentation: Capital EndodonticsDocument5 pagesTrushape Instrumentation: Capital EndodonticsnewmexicoomfsNo ratings yet
- Locator Root AttachmentDocument8 pagesLocator Root AttachmentnewmexicoomfsNo ratings yet
- Valplast PDFDocument4 pagesValplast PDFnewmexicoomfs100% (1)
- Monitors at A GlanceDocument8 pagesMonitors at A GlancenewmexicoomfsNo ratings yet
- New Practice Checklist: Business Office QTY Model # Unit Cost Total Cost Comments EquipmentDocument10 pagesNew Practice Checklist: Business Office QTY Model # Unit Cost Total Cost Comments EquipmentnewmexicoomfsNo ratings yet
- Useful Medications For Oral Conditions: AnalgesicsDocument8 pagesUseful Medications For Oral Conditions: AnalgesicsnewmexicoomfsNo ratings yet
- Periodontal Reevaluation 2Document11 pagesPeriodontal Reevaluation 2newmexicoomfsNo ratings yet
- Musculoskeletal Pathology OutlineDocument4 pagesMusculoskeletal Pathology OutlinenewmexicoomfsNo ratings yet
- Vascular Pathology Vasculitis BasicsDocument6 pagesVascular Pathology Vasculitis BasicsnewmexicoomfsNo ratings yet
- 2015 WREB ClinicalCandidateGuideDocument86 pages2015 WREB ClinicalCandidateGuidenewmexicoomfsNo ratings yet
- Skin Pathology OutlineDocument4 pagesSkin Pathology OutlinenewmexicoomfsNo ratings yet
- "The Role of The Family in Crime and Delinquency": (An Essay)Document10 pages"The Role of The Family in Crime and Delinquency": (An Essay)Xia FermoNo ratings yet
- Overview of Singapore's Airfreight IndustryDocument14 pagesOverview of Singapore's Airfreight IndustryramanathanNo ratings yet
- Jan W. Gooch, Biosketch - Jan. 2015Document15 pagesJan W. Gooch, Biosketch - Jan. 2015jan w goochNo ratings yet
- PTR 38Document23 pagesPTR 38CyNo ratings yet
- Dissertation Conflit Israelo PalestinienDocument7 pagesDissertation Conflit Israelo PalestinienPaySomeoneToWriteAPaperForMeUK100% (2)
- Architectural Fasteners & Fittings - Stainless Steel - AnzorDocument18 pagesArchitectural Fasteners & Fittings - Stainless Steel - AnzorBhaiJan59No ratings yet
- Role of Mid-Day Meal SchemeDocument3 pagesRole of Mid-Day Meal SchemekishorebharathNo ratings yet
- B31.1 Vs B31.3Document18 pagesB31.1 Vs B31.3Muhammed Ali Noureddeen100% (2)
- Lecture 5 - The Dialog Between Business and ITDocument46 pagesLecture 5 - The Dialog Between Business and ITNegar ZamiriNo ratings yet
- Bidder Manual - Tender SubmissionDocument54 pagesBidder Manual - Tender SubmissionSDOT AshtaNo ratings yet
- Thomas ParallelsNewTestamentDocument3 pagesThomas ParallelsNewTestamentRebekka KingNo ratings yet
- Premature Fatigue Failure of A Spring Due To Quench CracksDocument8 pagesPremature Fatigue Failure of A Spring Due To Quench CracksCamilo Rojas GómezNo ratings yet
- What Is Seed and Angel FundingDocument2 pagesWhat Is Seed and Angel FundingQueen ValleNo ratings yet
- Audio Visual ChallengeDocument6 pagesAudio Visual ChallengeBogdan BasilescuNo ratings yet
- 1st Sem Mid Term PYQs 2018&2019Document20 pages1st Sem Mid Term PYQs 2018&2019Sujeet RaiNo ratings yet
- PragyaResume PDFDocument1 pagePragyaResume PDFVarsha GurbaniNo ratings yet
- CinemaDocument9 pagesCinemaAlexNo ratings yet
- Explained: Choosing Representation, Mutation, and Crossover in Genetic AlgorithmsDocument2 pagesExplained: Choosing Representation, Mutation, and Crossover in Genetic AlgorithmsJosephNo ratings yet
- Biography of Gabriela SilangDocument2 pagesBiography of Gabriela SilangAngel MonjasNo ratings yet
- Fomulation of Best Fit Hydrophile - Lipophile Balance Dielectric Permitivity DemulsifierDocument10 pagesFomulation of Best Fit Hydrophile - Lipophile Balance Dielectric Permitivity DemulsifierNgo Hong AnhNo ratings yet
- Mipi-Tutorial PDF CompressedDocument13 pagesMipi-Tutorial PDF CompressedGeorgeNo ratings yet
- Medieval Book ListDocument43 pagesMedieval Book Listapi-242642581100% (2)
- LeadershipDocument4 pagesLeadershipDestyarsah Nusrati100% (1)
- Watchtower: 1941 Convention Report - St. Louis, MissouriDocument75 pagesWatchtower: 1941 Convention Report - St. Louis, MissourisirjsslutNo ratings yet
- Pre Repair and Post Repair Inspection ReportDocument4 pagesPre Repair and Post Repair Inspection ReportHoneyza NarzabalNo ratings yet
- AUTOSAR EXP NVDataHandling 2Document52 pagesAUTOSAR EXP NVDataHandling 2afraNo ratings yet
- Resume-Gmb 1Document3 pagesResume-Gmb 1api-353827251No ratings yet
- Why You Should Make Time For Self-ReflectionDocument3 pagesWhy You Should Make Time For Self-Reflectionjasbir.iitdNo ratings yet
- 9280810391Document382 pages9280810391text2fake5720No ratings yet
Chapter 12
Chapter 12
Uploaded by
newmexicoomfsOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 12
Chapter 12
Uploaded by
newmexicoomfsCopyright:
Available Formats
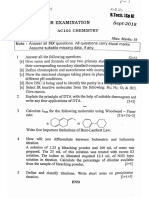
Pathology Exam 3
Chapter 12
Chapter 12 Diseases of the Liver, Biliary Tract, & Pancreas Bilirubin Metabolism Bilirubin tetrapyrrole pigment derived from Hb breakdown; appears yellow in body fluids Hemoglobin (Hb) iron-containing red pigment found in erythrocytes o 15g Hb/dl of blood o Composed of globin (colorless protein) + 4 heme molecules Each heme molecule has 4 pyrrole rings Each pyrrole ring = 4 carbon atoms + 1 nitrogen atom Linked by methene bridges to form a ring around a ferrous iron Ferrous iron combines reversibly w/oxygen molecule o Broken down in macrophages Hb breakdown o Heme ring opened to form tetrapyrrole chain green biliverdinglobin o Iron atoms removed to be reused by the body yellow bilirubinglobin o Globin removed 4 yellow bilirubin molecules o Bilirubin moves into ECF taken up by blood & bound to plasma proteins taken up by liver cells o Each bilirubin is conjugated to 2 molecules of glucuronic acid bilirubin diglucuronide excreted into bile o Bilirubin diglucuronide is deconjugated & reduced by bacteria urobilinogen (UBG) o UBG oxidized orange urobilin excreted as feces urobilin or urinary urobilin o Bilifuscins dark brown dipyrrole substances derived from stages of heme synthesis in bone marrow; responsible for color of feces Jaundice (AKA Icterus) Features o Yellow discoloration of skin, mucous membranes, & sclerae o Due to serum bilirubin & binding of bilirubin to tissue elements (esp. elastic fibers) Causes o Hemolytic jaundice - excessive bilirubin production o Hepatocellular jaundice injury of liver cells (associated w/hypoalbuminemia) o Obstructive jaundice obstruction of bile ducts Differentiation (Tests of Liver Function) Serum bilirubin Measured by van den Bergh rxn (normal is <1mg/dl, jaundice is >3mg/dl) Tests conjugated bilirubin (directly) & unconjugated bilirubin (indirect rxn) Bilirubinuria Significant of conjugated bilirubin in the blood Urine w/ bilirubin is dark yellow-brown & is foamy when shaken; use color tests Serum alkaline Retained bile salts (obstructive jaundice) detergent action on cell membranes of liver cells phosphatase & bile duct epithelium release of hepatic alkaline phosphatase into blood Also occurs w/ hepatocellular jaundice Serum aspartate AST levels when AST enzyme is released from dying cells (esp. liver & heart cells) aminotransferase Measure of extent of hepatocellular necrosis (hepatocellular jaundice) (AST) Slight also seen in obstructive & hemolytic jaundice Hypoalbuminemia Accompanies hepatocellular jaundice (liver synthesizes albumin)
Pathology Exam 3
Chapter 12
Predisposing factors Cause Mechanism
Severity Liver Function Tests
Hemolytic Jaundice Hemolytic anemia w/ anoxic injury of liver Large internal hemorrhage Augmented destruction of Hb bilirubin production Liver doesnt conjugate/excrete excessive bilirubin Unconjugated bilirubin in blood indirect reacting hyperbilirubinemia Mild No bilirubinuria serum bilirubin (indirect) slight in serum AST
Hepatocellular Jaundice
Obstructive Jaundice
Rupture of bile canaliculi hepatocyte necrosis Degeneration of some hepatocytes (dont conjugate bilirubin well) Others allow conjugated bilirubin to escape into blood
Distended bile canaliculi Conjugated bilirubin escapes into hepatic lymph & blood Bile pigments dont reach intestine in normal amounts Pale stools - fecal pyrrole pigments serum bilirubin (direct) Bilirubinuria (dark urine) Marked serum alkaline phosphatase
serum bilirubin (direct reacting) Bilirubinuria (dark urine) Marked in serum AST
Hepatic Failure Normal Liver o Large reserve of function o Cells have great regenerative capacity Hepatic failure o Injury must be severe &/or chronic to cause liver failure o Clinical features more frequent/prominent in chronic liver failure o Chronic liver failure often proceeds to cirrhosis (portal venous hypertension) Cirrhosis (portal venous hypertension) Features o Chronic liver diseases in which widespread hepatocytic necrosis results in fibrosis of liver o Liver has enormous regenerative capacity regeneration from remaining viable liver cells, return of normal hepatic function & structure o Hepatic necrosis hepatic fibrosis when injury is chronic/recurrent Regeneration still occurs as nodules of regenerating cells w/ sinusoids surrounded by septa of fibrous tissue Causes Characteristics Appearance Changes Chronic Most common cause of cirrhosis Large, soft, yellow Fatty degeneration w/ alcoholism Ethanol = hepatotoxin Hepatitis: enlarge, hepatomegaly & abnormal function yellowish green (bile Acute alcoholic hepatitis w/ Can lead to chronic/repetitive staining) coagulative necrosis, Acute attacks of acute alcoholic Mallory body = meshwork inflammation, & focal fibrosis hepatitis & micronodular of hyaline cytoplasmic cirrhosis material Viral Macronodular cirrhosis Irregular, large nodules Cryptogenic cirrhosis = hepatitis (postnecrotic, posthepatitic) asymptomatic Autoimmune Circulating Abs of unknown Inflammatory infiltrate w/ many hepatitis cause plasma cells Young-middle aged women Hyperglobulinemia Responds to immunosuppressive therapy Hepatotoxic Often an unpredictable rxn drugs & Removal of drug often prevents poisons cirrhosis
Pathology Exam 3
Chapter 12
Biliary tract obstruction
Due to carcinomas of head of pancreas or biliary tract, chronic pancreatitis, gallstones, bile duct suture, cystic fibrosis of pancreas
Relieved surgically
Pathologic Anatomy o Cirrhotic liver enlarged (fatty degeneration) or shrunken (hepatocytic necrosis, retraction of fibrous tissue); firm & nodular o Nodules bulging; plates of regenerating liver cells w/ sinusoids; 1mm-many cm; o Septa shrunken & firm; b/t nodules; gray-white fibrous tissue scar; contain small blood vessels & bile ducts o Intraportohepatic shunt small blood vessels in septa; portal venous blood can reach hepatic vein tributaries w/out traversing intralobular sinusoids; causes liver cells to become ischemic Portal Venous Hypertension o Occurs in most cases of cirrhosis o Causes: Abnormal transmission of hepatic arterial pressure to portal vein branches, due to alterations of intrahepatic vascular bed Pressure on intrahepatic veins by expanding nodules of regenerating liver tissue Fibrous obliteration of small intrahepatic blood vessels in septa o Effects Chronic passive congestion of spleen enlarged, firm; excessive function shortens lifespan of formed elements of blood Ascites due to transudation of fluid from congested capillaries in portal venous bed; causes abdominal protuberance & edema of legs Establishment of collateral circulation b/t portal vein tributaries & systemic veins Esophageal varices large, dilated, thin-walled submucosal veins; bulge into lower esophagus; rupture = massive hemorrhage into alimentary tract Hemorrhoids Caput Medusae enlarged subcutaneous paraumbilical veins Portocaval shunt - Portal blood bypasses the liver Leads to hepatic ischemia & hyperammonemia Clinical Features o Manifestations of causative condition o Manifestations of chronic hepatic failure o Manifestations of portal venous hypertension o Progressive & irreversible o Cause of death hepatic failure &/or complications of portal venous hypertension
Viral Hepatitis Features o Part of several systemic viral infections (yellow fever, congential rubella, infectious mono) o Viral infection in which hepatic lesion is dominant clinical/anatomic feature Pathologic Anatomy o Major lesion hepatocellular degeneration & necrosis w/ round cell infiltrate o Hepatocyte injury due to cytotoxic T-cells cellular immune rxn to viral Ags on cell membrane of liver cells Course o Most cases resolve spontaneously regeneration, return of normal structure & function o May become chronic hepatitis can still resolve completely o Progression to cirrhosis o Death from hepatic failure may occur w/in days-weeks due to necrosis of most hepatocytes Clinical Features
Pathology Exam 3
Chapter 12
o o o o o o o
Incubation period weeks-months; onset abrupt or insiduous Manifestations of acute infection fever, headache, malaise, lassitude Prominent GI symptoms anorexia, nausea, vomiting Tender hepatomegably Hepatocellular jaundice Manifestations of hypersensitivity due to circulating viral Ag-Ab complexes; rash, arthralgia Leukocyte count normal or ed; relative lymphocytosis Severity of clinical features varies by patient & different type of VH Many are mild few symptoms, no jaundice
Primary Carcinoma of Liver Features o Uncommon in US o Less common than metastatic carcinoma of liver o Liver cell carcinomas (malignant hepatomas) - Occur in cirrhotic livers, regenerative hyperplasia composed of atypical hepatocytes; associated w/ chronic hepatitis B & C o Bile duct carcinomas arise from bile duct epithelium w/ noncirrhotic liver Pathologic Anatomy o Usu. starts in right lobe of severely cirrhotic liver o Soft, bulky intrahepatic mass o Numerous satellite nodules due to extensive spread w/in intrahepatic portal & hepatic veins o Metastases lungs, regional lymph nodes (peribiliary, lower mediastinal) Clinical Features o Abdominal pain, weight loss o Fever o Weakness o Rapid swelling of abdomen o Jaundice, large fixed liver & ascites o Brief course, death w/in 6 months due to hemorrhage for esophageal varices, rupture of liver, hepatic coma, or general debility Cholelithiasis Features o Gallbladder stones o Symptomatic or asymptomatic o Twice as common in women estrogen s hepatic secretion of cholesterol & s secretion of bile salts into the bile o Other predisposing factors: American Indian women, obesity, diabetes mellitus, chronic hemolytic anemia Types of Gallstones o Components: cholesterol, bile pigments, calcium, & small amount of protein Type Composition Characteristics Associated w/: Mixed Cholesterol Most common Chronic Bile pigments (bilirubin & Otherwise normal gallbladder cholecystitis biliverdin) Multiple Calcium Smooth, faceted, green or yellow Protein matrix 2-20mm diameter Pure Cholesterol Uncommon Cholesterol Traces of other substances Otherwise normal gallbladder Solitary Large, ellipsoid, pebbled, colorlessyellow, translucent surface Pure Calcium Uncommon
Pathology Exam 3
Chapter 12
Calcium
Bile pigments
Otherwise normal gallbladder Small, irregular, hard, brittle, black Multiple
Pathogenesis o Cause unknown Chronic cholecystitis is RESULT, not cause of cholelithiasis o Secretion of abnormal (lithogenic) bile amount of cholesterol or bile pigments &/or amount of bile salts or phospholipids o normal gallbladder concentrated biles bile salts & phospholipids (lecithin) prevent precipitation of cholesterol o Rarely dissolve in situ o May be related to inadequate adaptation to cholesterol-rich diet (meats) Effects o Irritation of the gallbladder Mechanical & chemical irritation of mucosa Chronic cholecytitis wall becomes thick, fibrotic w/ loss of mucosal folds o Obstruction of biliary tract Obstruction of cystic duct Distention of gallbladder pain (biliary colic) If obstruction persists, distention compresses intramural blood vessels ischemic damage hemorrhage & necrosis of gallbladder (acute cholecystitis) Obstruction of common bile duct Occurs where duct narrows to enter duodenum Pain (biliary colic) Obstructive jaundice Acute ascending cholangitis bacteria ascend bile duct bile stained abscesses in liver Acute pancreatitis If persistant, Biliary cirrhosis Clinical Features o Chronic cholecystitis or slight distention of biliary tract Belching, nausea, vomiting, constipation Nonspecific symptoms of indigestion aggravated by large meals o Biliary colic Sharp pain in upper right quadrant (right subscapular area) Begins suddenly - @ night or after heavy meal; lasts 1-several hours Constant pain, nausea, vomiting, tenderness o Treatment cholecystectomy; exploration of common bile duct & stone removal
Carcinoma of Extrahepatic Biliary Tract Features o Adenocarcinomas o Cause: unknown o Sites of predilection: Gallbladder complications of longstanding cholelithiasis & chronic cholecystitis Distal communal bile duct & duodenal papilla
Pathology Exam 3
Chapter 12
Confluence of common hepatic & cystic ducts Pathologic Anatomy o Primary adenocarcinoma hard & infiltrative OR soft & papillary o Obstructive jaundice primary tumor or metastases restrict bile ducts o Metastases occur early liver, duodenum, etc. Clinical Features o Obstructive jaundice, upper abdominal pain, hepatomegaly o Palpable primary tumor o Previous confirmation of symptomatic cholelithiasis o Most incurable death w/in months-years due to biliary obstruction
Acute Pancreatitis Features o Due to escape of large amounts of pancreatic enzymes from the pancreatic ducts autocatalytic activation of enzymes by contact w/ ISF enzymatic autodigestion of pancreas Occurs due to structural or functional duct obstruction & active pancreatic secretion occurring simultaneously (ex: after a meal) o Enzymes Enzyme Effect Results Trypsin Necrosis & digestion of pancreatic Release of more pancreatic enzymes more Chymotrypsin ducts & acini necrosis Phospholipase Elastase Digestion of blood vessel walls Hemorrhage by rhexis Lipase Splits triglycerides of fat cells Fat necrosis FFAs combine w/ cations in in/around pancreas ECF Ca-salts precipitate soapy, yellowwhite nodules Hypocalcemia Amylase Minor role in pancreatitis Hyperamylasemia (amylase in blood) Causes (Predisposing Factors:) o Chronic alcoholism Ethanol induces: Direct chemical irritation of duodenum, spasm of sphincter of Oddi, & pancreatic duct obstruction Gastrin release from stomach, secondary stimulation of pancreatic secretion o Gallstones May obstruct main pancreatic duct or small interlobular ducts or cause spasm in sphincter of Oddi (surrounds common bile & main pancreatic ducts) o Obesity Obese person eats large meals - s pancreatic secretions & duct pressure o Trauma Ex: surgery in area near pancreas Ex: blunt abdominal trauma w/ pancreatic damage Pathologic Anatomy o Pancreas is swollen peritoneal cavity contains serous/seroanguineous fluid Mushy, grayish-yellow Hemorrhage o Nodules 2-5 mm, soft, opaque yellowish-white, & soapy (fat necrosis) Scattered in adipose tissue around pancreas o Bacterial infection may occur o Necrotic tissue replaced by fibrous scar OR a cyst filled w/ opaque yellowish-brown fluid (pseudocyst)
Pathology Exam 3
Chapter 12
Clinical Features o Major features: epigastric pain, hyperamylasemia o Acute interstitial pancreatitis (mild case) spontaneous recovery in 24-48 hours o Acute pancreatic necrosis (severe case) constant epigastric pain, nausea, vomiting, tenderness, shock, marked in serum amylase & lipase o Treatment conservative o 1/3 pts die w/in 10 days of onset
Chronic Pancreatitis occurs after multiple attacks of acute interstitial pancreatitis scarring of pancreas due to recovery cause: usu. chronic alcoholism appearance: small, pale, irregular, hard (sometimes calcified), dilated ducts w/ thick gray fluid or calcium carbonate stones clinical features: early attacks of abdominal pain (1-2 days long), late pancreatic insufficiency w/ steatorrhea & secondary diabetes mellitus, cause of death: attach of acute pancreatic necrosis Carcinoma of Pancreas Features o Cause: unknown o Classification: Head of pancreas more common Body & Tail of pancreas Pathologic Anatomy o Primary lesion large infiltrative mass of hard, grayish-white tissue Often invades adjacent organs/tissues biliary tract, duodenum, retroperitoneum o Microscopic appearance adenocarcinoma; invasion of lymph vessels, veins, & perineural spaces o Metastases early; regional lymph nodes, peritoneum, lungs; more massive/frequent/widespread from body & tail of pancreas Clinical Features o carcinoma of the head of pancreas early obstruction of common bile duct obstructive jaundice, epigastric or right hypochondriac pain o carcinoma of the body & tail of pancreas constant dull epigastric or left hypochondriac pain (radiate thru back, worse at night & in supine position), depression, wt. loss ascites due to peritoneal implantation metastases o treatment surgery; often fatal death 6 months after onset Cystic Fibrosis of Pancreas (systemic mucoviscidosis) Features o Generalized disease children, adolescents, young adults o Dysfunction of exocrine glands Abnormally viscid secretion duct obstruction atrophy of secretory element & fibrosis of glands o CFP is inherited autosomal recessive trait Long arm of chromosome 7 Codes for a cell membrane protein that regulates chloride transport by epithelial cells Heterozygotes are normal o Basic metabolic abnormality defect in chloride (& water) transport by epithelium of small exocrine gland ducts Secretions of pancreas & mucous glands become scant & viscid Pathologic Anatomy
Pathology Exam 3
Chapter 12
Histologic lesion smallest ducts/glands of all viscera are plugged by inspissated secretory material; glandular tissue atrophy & fibrosis o Secondary bacterial infection in resp. tract o Lesions & organ dysfunction pancreas, lungs, intestine, liver, & male genital tract (aspermia & sterility) Clinical Features o Intestinal obstruction @ birth (10%) most die as neonates o Pancreatic insufficiency, failure to gain weight, chronic/recurrent infections of bronchi & lungs, chronic paranasal sinusitis o Leads to resp. failure, hypoxemia, cor pulmonale o Diagnosis trypsin in duodenal fluid & high [Cl-] in sweat o Death pulmonary infection & resp. failure in childhood/adolescence o Possible to screen early in pregnancy o
You might also like
- Index Fund Investing 101Document100 pagesIndex Fund Investing 101newmexicoomfs100% (9)
- CCDM Manual PDFDocument715 pagesCCDM Manual PDFrehanaNo ratings yet
- Med Surg Test 4 Study GuideDocument29 pagesMed Surg Test 4 Study GuideJess100% (2)
- Dental SchoolDocument5 pagesDental SchoolnewmexicoomfsNo ratings yet
- 97Document79 pages97HATLERNo ratings yet
- 1 Path of The LiverDocument97 pages1 Path of The LiverLucas AresNo ratings yet
- Hepatobiliary Diseases 3Document28 pagesHepatobiliary Diseases 3AmirahNo ratings yet
- Askep SirosisDocument73 pagesAskep SirosisRisma Yuliana PratiwiNo ratings yet
- Cirrhosis 22008 Bajar Musica Gratis Descargar Musica Gratis Online Descargar Musica Gratis para CelularesDocument72 pagesCirrhosis 22008 Bajar Musica Gratis Descargar Musica Gratis Online Descargar Musica Gratis para CelularesYeni Chie Aneuk TuleutNo ratings yet
- With Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Document72 pagesWith Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Ainun JaariahNo ratings yet
- Approach To Cholestatic Jaundice: DR - Ram Raut - JR III (Medicine) Guide - Dr.D.B. Kadam Seminar Teacher-Dr - NitinDocument68 pagesApproach To Cholestatic Jaundice: DR - Ram Raut - JR III (Medicine) Guide - Dr.D.B. Kadam Seminar Teacher-Dr - NitinAnan JaiswalNo ratings yet
- 3 Liver CirrhosisDocument50 pages3 Liver CirrhosisKamal AhmedNo ratings yet
- With Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Document72 pagesWith Ordinary Talent and Extraordinary Perseverance, All Things Are Attainable.Darin MonerNo ratings yet
- Lect. 8Document30 pagesLect. 8jayNo ratings yet
- 15 LivernDocument45 pages15 LivernDrAbdullrabAlmarwanyaNo ratings yet
- QUIBOD LiverDocument32 pagesQUIBOD LiverAileen Grace DelimaNo ratings yet
- Liver Cirrohsis (Lecture)Document87 pagesLiver Cirrohsis (Lecture)Rina Sundari Dels100% (1)
- Liver NotesDocument2 pagesLiver NotesAnne IsheeNo ratings yet
- Liver CirrhosisDocument16 pagesLiver CirrhosisBabesNo ratings yet
- Liver LecDocument107 pagesLiver LecNMD LIFESAVERNo ratings yet
- The Diseases of The Liver: Department of Pediatric Allergy, Gastroenterology and NutritionDocument125 pagesThe Diseases of The Liver: Department of Pediatric Allergy, Gastroenterology and NutritionlindaNo ratings yet
- Presented by Mr. Vinay Kumar M.Sc. Nursing 1 Year HCN, SrhuDocument66 pagesPresented by Mr. Vinay Kumar M.Sc. Nursing 1 Year HCN, SrhuVinay Kumar100% (2)
- Obstructive Jaundice: DR Nanteza SumayiyaDocument26 pagesObstructive Jaundice: DR Nanteza SumayiyaNinaNo ratings yet
- Hepatobiliary DiseaseDocument60 pagesHepatobiliary DiseaseFirdaus AslamNo ratings yet
- Liver CirrhosisDocument50 pagesLiver Cirrhosischai rinNo ratings yet
- Liver CirrohosisDocument157 pagesLiver CirrohosisSeema SachdevaNo ratings yet
- Hepatobiliary System: BY Pranjal Kulkarni Neha ManeDocument85 pagesHepatobiliary System: BY Pranjal Kulkarni Neha ManeGurneetNo ratings yet
- Pathology of The Liver, Biliary Tract andDocument64 pagesPathology of The Liver, Biliary Tract andembeoyabarareNo ratings yet
- 12.0 Care of Clients With Hepato Biliary and Pancreatic DisorderDocument68 pages12.0 Care of Clients With Hepato Biliary and Pancreatic DisorderJanna Niña ElementoNo ratings yet
- Gall Bladder and Bile DuctDocument18 pagesGall Bladder and Bile DuctClint MorrisonNo ratings yet
- Gallstone DiseaseDocument28 pagesGallstone DiseaseNurmalia PutriNo ratings yet
- Liver, Biliary Tract and Pancreas ProblemsDocument95 pagesLiver, Biliary Tract and Pancreas ProblemsBav VAansoqnuaetzNo ratings yet
- Pathology of The Liver: Systems Pathology II-PA5402 Dr. Khan T-W-RDocument78 pagesPathology of The Liver: Systems Pathology II-PA5402 Dr. Khan T-W-RCrystal Lynn Keener SciariniNo ratings yet
- Surgical Diseases of Liver1Document54 pagesSurgical Diseases of Liver1DR MOHAMED HEALTH CHANNELNo ratings yet
- Genitourinary ObjectivesDocument38 pagesGenitourinary Objectivescwumspa14No ratings yet
- Disorders of The Hepatobiliary System: Dr. Mehzabin AhmedDocument27 pagesDisorders of The Hepatobiliary System: Dr. Mehzabin Ahmedbpt2100% (1)
- Liver TransplantationDocument21 pagesLiver TransplantationRozi RamliNo ratings yet
- MetabolismDocument39 pagesMetabolismTiffany KnepperNo ratings yet
- Urea/ Ammonia Tests: Primary Liver Function TestsDocument6 pagesUrea/ Ammonia Tests: Primary Liver Function TestsMemory MahwendaNo ratings yet
- Liver Pathology PDFDocument7 pagesLiver Pathology PDFjohn smithNo ratings yet
- Etiologi Dan Patogenesis Ikterus,...Document103 pagesEtiologi Dan Patogenesis Ikterus,...Raditya PrimaNo ratings yet
- Hepatic CirrhosisDocument20 pagesHepatic CirrhosisAnifowose samsonNo ratings yet
- MedSurg NotesDocument21 pagesMedSurg NotesShanny BNo ratings yet
- NCM Lecture (Liver and Gallbladder)Document76 pagesNCM Lecture (Liver and Gallbladder)beer_ettaaNo ratings yet
- Urinary Symptoms - DR RashaDocument70 pagesUrinary Symptoms - DR RashaRasha TelebNo ratings yet
- 3.liver & Biliary TractDocument141 pages3.liver & Biliary TractBobi WijayaNo ratings yet
- Hepatic Disorders: R2 Thanaporn ChittipanichDocument42 pagesHepatic Disorders: R2 Thanaporn ChittipanichMimmey Yeniw100% (1)
- Hepatic and Biliary DisordersDocument103 pagesHepatic and Biliary Disordersramasalem1975No ratings yet
- Urine Dipstick Testing + Common Renal Problem 2012Document52 pagesUrine Dipstick Testing + Common Renal Problem 2012Ainul ArinaNo ratings yet
- Liver CirrhosisDocument83 pagesLiver CirrhosisRusiana NasilahNo ratings yet
- اليزيد UrinalysisDocument48 pagesاليزيد UrinalysisRa'aft Al-SamawiNo ratings yet
- Cirrhosis of LiverDocument106 pagesCirrhosis of LiveraahadNo ratings yet
- Sirosis Hepatis: Sigit Widyatmoko Fakultas Kedokteran UMSDocument66 pagesSirosis Hepatis: Sigit Widyatmoko Fakultas Kedokteran UMSArif Rahman DmNo ratings yet
- Obstructive Jaundice Group 6Document33 pagesObstructive Jaundice Group 6Qurbon AliNo ratings yet
- OUM Tutorial 1 SBNS3504 RenalDocument51 pagesOUM Tutorial 1 SBNS3504 RenalMashanimy HoneyNo ratings yet
- Case of Obstructive JaundiceDocument38 pagesCase of Obstructive JaundiceJay R Plogio100% (2)
- Liver Disorders-II Jaundice 3Document14 pagesLiver Disorders-II Jaundice 3Daksh SabharwalNo ratings yet
- Notes Liver CirrhosisDocument10 pagesNotes Liver CirrhosisSanthu Su100% (1)
- The Incidence of Esophageal Varices in Patients With CirrhosisDocument31 pagesThe Incidence of Esophageal Varices in Patients With CirrhosisDenata PrabhasiwiNo ratings yet
- Urinalysis and Body Fluids2020Document47 pagesUrinalysis and Body Fluids2020MONFOLA100% (2)
- Hepato-Biliary System and Their DisordersDocument131 pagesHepato-Biliary System and Their DisordersIton BumatayNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Obturation of The Root Canal: Capital EndodonticsDocument36 pagesObturation of The Root Canal: Capital EndodonticsnewmexicoomfsNo ratings yet
- Metallurgy & File Classification: Capital EndodonticsDocument26 pagesMetallurgy & File Classification: Capital EndodonticsnewmexicoomfsNo ratings yet
- Vortex Blue Instrumentation: Capital EndodonticsDocument16 pagesVortex Blue Instrumentation: Capital EndodonticsnewmexicoomfsNo ratings yet
- Entry Point I Entry Point II Entry Point IIIDocument1 pageEntry Point I Entry Point II Entry Point IIInewmexicoomfsNo ratings yet
- Trushape Instrumentation: Capital EndodonticsDocument5 pagesTrushape Instrumentation: Capital EndodonticsnewmexicoomfsNo ratings yet
- Locator Root AttachmentDocument8 pagesLocator Root AttachmentnewmexicoomfsNo ratings yet
- Valplast PDFDocument4 pagesValplast PDFnewmexicoomfs100% (1)
- Monitors at A GlanceDocument8 pagesMonitors at A GlancenewmexicoomfsNo ratings yet
- New Practice Checklist: Business Office QTY Model # Unit Cost Total Cost Comments EquipmentDocument10 pagesNew Practice Checklist: Business Office QTY Model # Unit Cost Total Cost Comments EquipmentnewmexicoomfsNo ratings yet
- Useful Medications For Oral Conditions: AnalgesicsDocument8 pagesUseful Medications For Oral Conditions: AnalgesicsnewmexicoomfsNo ratings yet
- Periodontal Reevaluation 2Document11 pagesPeriodontal Reevaluation 2newmexicoomfsNo ratings yet
- Musculoskeletal Pathology OutlineDocument4 pagesMusculoskeletal Pathology OutlinenewmexicoomfsNo ratings yet
- Vascular Pathology Vasculitis BasicsDocument6 pagesVascular Pathology Vasculitis BasicsnewmexicoomfsNo ratings yet
- 2015 WREB ClinicalCandidateGuideDocument86 pages2015 WREB ClinicalCandidateGuidenewmexicoomfsNo ratings yet
- Skin Pathology OutlineDocument4 pagesSkin Pathology OutlinenewmexicoomfsNo ratings yet
- "The Role of The Family in Crime and Delinquency": (An Essay)Document10 pages"The Role of The Family in Crime and Delinquency": (An Essay)Xia FermoNo ratings yet
- Overview of Singapore's Airfreight IndustryDocument14 pagesOverview of Singapore's Airfreight IndustryramanathanNo ratings yet
- Jan W. Gooch, Biosketch - Jan. 2015Document15 pagesJan W. Gooch, Biosketch - Jan. 2015jan w goochNo ratings yet
- PTR 38Document23 pagesPTR 38CyNo ratings yet
- Dissertation Conflit Israelo PalestinienDocument7 pagesDissertation Conflit Israelo PalestinienPaySomeoneToWriteAPaperForMeUK100% (2)
- Architectural Fasteners & Fittings - Stainless Steel - AnzorDocument18 pagesArchitectural Fasteners & Fittings - Stainless Steel - AnzorBhaiJan59No ratings yet
- Role of Mid-Day Meal SchemeDocument3 pagesRole of Mid-Day Meal SchemekishorebharathNo ratings yet
- B31.1 Vs B31.3Document18 pagesB31.1 Vs B31.3Muhammed Ali Noureddeen100% (2)
- Lecture 5 - The Dialog Between Business and ITDocument46 pagesLecture 5 - The Dialog Between Business and ITNegar ZamiriNo ratings yet
- Bidder Manual - Tender SubmissionDocument54 pagesBidder Manual - Tender SubmissionSDOT AshtaNo ratings yet
- Thomas ParallelsNewTestamentDocument3 pagesThomas ParallelsNewTestamentRebekka KingNo ratings yet
- Premature Fatigue Failure of A Spring Due To Quench CracksDocument8 pagesPremature Fatigue Failure of A Spring Due To Quench CracksCamilo Rojas GómezNo ratings yet
- What Is Seed and Angel FundingDocument2 pagesWhat Is Seed and Angel FundingQueen ValleNo ratings yet
- Audio Visual ChallengeDocument6 pagesAudio Visual ChallengeBogdan BasilescuNo ratings yet
- 1st Sem Mid Term PYQs 2018&2019Document20 pages1st Sem Mid Term PYQs 2018&2019Sujeet RaiNo ratings yet
- PragyaResume PDFDocument1 pagePragyaResume PDFVarsha GurbaniNo ratings yet
- CinemaDocument9 pagesCinemaAlexNo ratings yet
- Explained: Choosing Representation, Mutation, and Crossover in Genetic AlgorithmsDocument2 pagesExplained: Choosing Representation, Mutation, and Crossover in Genetic AlgorithmsJosephNo ratings yet
- Biography of Gabriela SilangDocument2 pagesBiography of Gabriela SilangAngel MonjasNo ratings yet
- Fomulation of Best Fit Hydrophile - Lipophile Balance Dielectric Permitivity DemulsifierDocument10 pagesFomulation of Best Fit Hydrophile - Lipophile Balance Dielectric Permitivity DemulsifierNgo Hong AnhNo ratings yet
- Mipi-Tutorial PDF CompressedDocument13 pagesMipi-Tutorial PDF CompressedGeorgeNo ratings yet
- Medieval Book ListDocument43 pagesMedieval Book Listapi-242642581100% (2)
- LeadershipDocument4 pagesLeadershipDestyarsah Nusrati100% (1)
- Watchtower: 1941 Convention Report - St. Louis, MissouriDocument75 pagesWatchtower: 1941 Convention Report - St. Louis, MissourisirjsslutNo ratings yet
- Pre Repair and Post Repair Inspection ReportDocument4 pagesPre Repair and Post Repair Inspection ReportHoneyza NarzabalNo ratings yet
- AUTOSAR EXP NVDataHandling 2Document52 pagesAUTOSAR EXP NVDataHandling 2afraNo ratings yet
- Resume-Gmb 1Document3 pagesResume-Gmb 1api-353827251No ratings yet
- Why You Should Make Time For Self-ReflectionDocument3 pagesWhy You Should Make Time For Self-Reflectionjasbir.iitdNo ratings yet
- 9280810391Document382 pages9280810391text2fake5720No ratings yet