Professional Documents
Culture Documents
Therapy Response in Malignant Limphoma
Therapy Response in Malignant Limphoma
Uploaded by
eddieshadowsOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Therapy Response in Malignant Limphoma
Therapy Response in Malignant Limphoma
Uploaded by
eddieshadowsCopyright:
Available Formats
Eur J Nucl Med Mol Imaging (2007) 34:17751782 DOI 10.
1007/s00259-007-0452-z
ORIGINAL ARTICLE
Early assessment of therapy response in malignant lymphoma with the thymidine analogue [18F]FLT
Andreas K. Buck & Clemens Kratochwil & Gerhard Glatting & Malik Juweid & Martin Bommer & Djurdja Tepsic & Andreas T. J. Vogg & Torsten Mattfeldt & Bernd Neumaier & Peter Mller & Sven N. Reske
Received: 4 November 2006 / Accepted: 5 April 2007 / Published online: 31 May 2007 # Springer-Verlag 2007
Abstract Purpose The aim of this study was to determine whether the thymidine analogue 3-deoxy-3-[18F]fluorothymidine ([18F]FLT) is adequate for early evaluation of the response of malignant lymphoma to antiproliferative treatment in a mouse xenotransplant model. Methods Immunodeficient mice bearing a follicular lymphoma xenotransplant were treated with high-dose chemotherapy (cyclophosphamide, n =10), immunotherapy (CD20 mAb, ibritumomab-tiuxetan, n =10) or radioimmunotherapy ([90Y]CD20 mAb, Zevalin, n =10). Forty-eight hours after
A. K. Buck : C. Kratochwil : G. Glatting : D. Tepsic : A. T. J. Vogg : B. Neumaier : S. N. Reske Department of Nuclear Medicine, University Hospital Ulm, Ulm, Germany M. Bommer Department of Haematology, University Hospital Ulm, Ulm, Germany T. Mattfeldt : P. Mller Institute of Pathology, University Hospital Ulm, Ulm, Germany A. K. Buck (*) Department of Nuclear Medicine, Technical University Munich, Ismaninger Strasse 22, 81675 Munich, Germany e-mail: andreas.buck@tum.de M. Juweid Department of Radiology and Holden Comprehensive Cancer Center, University of Iowa, Iowa City, IA, USA
treatment, antiproliferative effects were assessed with [18F] FLT. Ninety minutes after i.v. injection of 510 MBq [18F] FLT, mice were sacrificed and radioactivity within the tumour and normal organs was measured using a gamma counter and calculated as % ID/g. The proliferation fraction in tissue samples derived from treated and untreated tumours was evaluated by Ki-67 immunohistochemistry, which served as the reference for proliferative activity. Results In untreated lymphoma, the mean proliferation fraction was 83.6%. After chemotherapy, the mean proliferation fraction decreased to 39.3% (p =0.0001), after immunotherapy to 77.6% (p =0.0078) and after radioimmunotherapy to 78.8% (p =0.014). In none of the animals was a significant change in tumour size observed. In untreated lymphoma, tumoural [18F]FLT uptake was 5.4% ID/g, after chemotherapy it was 1.5% (p =0.0005), after immunotherapy, 3.9% (non-significant), and after radioimmunotherapy, 5.8% (non-significant). Conclusion In a lymphoma xenotransplant model, [18F] FLT detects early antiproliferative drug activity before changes in tumour size are visible. These findings further support the use of [18F]FLT-PET for imaging early response to treatment in malignant lymphoma. Keywords Lymphoma . Therapy control . Proliferation . Nucleosides
Introduction Deregulated cell cycle progression is a hallmark of malignant lymphoma and most human cancers. Therefore, the majority of anticancer drugs are designed to inhibit cell proliferation. Malignant lymphoma can be separated into
1776
Eur J Nucl Med Mol Imaging (2007) 34:17751782
subgroups with a low (<50%) and a high proliferation fraction (>50%), roughly overlapping with the histologically based definition of low- and high-grade tumours [1]. In general, lymphomas with low proliferative activity, such as follicular lymphoma grade I, mantle cell lymphoma or marginal zone lymphoma, are frequently associated with advanced clinical stage and low clinical aggressiveness. In contrast, lymphomas with a high proliferation fraction, such as large B-cell lymphoma or Burkitt lymphoma, are associated with higher biological aggressiveness and predominantly localised tumour manifestations [1]. In low-grade lymphomas, clinicopathological presentation is presumably related to alterations in apoptosis regulators, whereas in aggressive lymphoma alterations in cell cycle regulators such as c-myc are frequently observed. At present, assessment of response to therapy is based on morphological imaging modalities such as computed tomography, ultrasound or magnetic resonance imaging [2, 3]. However, changes in tumour volume may occur weeks or months after initiation of drug therapy, and reasonable treatment modification may be delayed in cases without a treatment response. Furthermore, morphologybased modalities have limited ability to discriminate between scar tissue and viable tumour in residual masses [4], and therapeutic effects of novel drugs that are cytostatic and do not directly lead to tumour shrinking cannot be visualised by morphological changes [5]. However, functional and metabolic alterations related to drug therapy can be non-invasively assessed with positron emission tomography (PET) and the glucose analogue [18F] fluorodeoxyglucose ([18F]FDG). [18F]FDG-PET has a high sensitivity regarding detection of malignant foci and is now widely used for diagnosis and staging of cancer. Nevertheless, tumoural accumulation of [18F]FDG is only in part related to proliferation [6], and specificity is reduced owing to non-specific accumulation in inflammatory lesions [7, 8]. Radiopharmaceuticals specifically addressing the cell cycle would be advantageous for assessment of therapy response and for development of tumour-targeted therapies. [11C] Thymidine was the first radiotracer successfully used for this purpose [9, 10]. However, the short half-life of 11C (20 min) and rapid metabolism in vivo limits its clinical application. The thymidine analogue 3-deoxy-3-[18F]fluorothymidine ([18F]FLT) offers a more suitable half-life of 110 min and is stable in vivo [11]. Like the native nucleoside thymidine, [18F]FLT is taken up by nucleoside transporters which are located in the cellular membrane. Within the cell, the cytosolic enzyme thymidine kinase 1 (TK1) phosphorylates FLT to FLTmonophosphate [12]. TK1 is a cell cycle-regulated enzyme of the thymidine salvage pathway [13] and is overexpressed in various tumour entities [14, 15]. Several studies have demonstrated a significant correlation of [18F]FLT uptake
and TK1 activity, the latter being dependent on the presence of the cofactor ATP [16, 17]. [18F]FLT is not a direct measure of cell proliferation because [18F]FLT acts as chain terminator and therefore only a small amount of intracellular [18F]FLT is incorporated into DNA [16, 18]. In clinical studies, [18F]FLT-PET has already been successfully used for assessment of the proliferation rate in a variety of tumour entities, such as sarcoma, lung cancer, colorectal cancer and lymphoma [1929]. Recently, two independent studies have demonstrated that tumoural uptake of [18F]FLT significantly correlates with the proliferation rate of lung cancer, with a correlation coefficient of r =0.92 [27] or r = 0.84 [30]. In patients with non-Hodgkins lymphoma, we have reported a correlation coefficient of r =0.86 [31]. In malignant lymphoma, a surrogate marker of cellular proliferation would be highly desirable because low- and high-grade lymphomas differ significantly in terms of their proliferative activity. In the present study, we employed a mouse lymphoma xenotransplant model to evaluate the effect of different treatment modalities on proliferative activity early after the start of therapy and to investigate whether tumoural [18F] FLT uptake can be used as surrogate marker of the proliferation rate.
Materials and methods Induction of lymphoma xenotransplants in immunodeficient mice The human CD20-positive B-cell follicular lymphoma cell line DoHH2 was used for induction of lymphoma xenotransplants. DoHH2 is associated with a high proliferation rate of approximately 80% and expresses high levels of TK1, which is considered to be the key enzyme in the cellular trapping of [18F]FLT. Ten million (10106) lymphoma cells suspended in saline solution (0.9% NaCl, 100 l) were injected subcutaneously into the right shoulder region of female immunodeficient mice (CB-17 SCID). Six- to eight-week-old inbred mice were obtained from the central animal research facility (Tierforschungszentrum, University of Ulm, Ulm, Germany). Tumours reached diameters of 1.52.7 cm within 35 weeks, which were measured with a shifting calliper. Treatment was performed when the xenotransplants reached a size of approximately 10 mm10 mm. Therapeutic regimens Three groups of ten mice each underwent chemotherapy, immunotherapy or radioimmunotherapy. Response to
Eur J Nucl Med Mol Imaging (2007) 34:17751782
1777
therapy was evaluated 48 h after drug treatment. Immunotherapy consisted of a single intravenous (i.v.) injection (100 l) of the CD20 mAb ibritumomabtiuxetan (150 mg/kg, IDEC Pharmaceuticals, San Diego, CA). Chemotherapy was carried out by intraperitoneal injection of cyclophosphamide (Endoxan, 90 mg/kg, Baxter, Frankfurt, Germany). For radioimmunotherapy, 90 Y-labelled CD20 mAb (Zevalin, 5 MBq/mouse, IDEC Pharmaceuticals, San Diego, CA) was administered intravenously. The control group (ten mice) was treated with i.v. injection of NaCl solution (0.9%). Proliferative activity in lymphoma xenotransplants Formalin-fixed, paraffin-embedded sections (5 m) of resected tumour tissue were dewaxed, rehydrated and microwaved for 20 min in a 0.01 M citrate buffer. One hundred microlitres of the monoclonal Ki-67 specific antibody MIB-1 (IgG 1 kappa, DAKO, Hamburg, Germany) in a dilution of 1:500 was used as primary antibody. A peroxidase-complexed mAb was utilised as secondary antibody (EnVision, DAKO, Hamburg, Germany), and 3amino-9-ethylcarbazole (AEC, Sigma-Aldrich, Deisenhofen, Germany) served as chromogen. In each tumour xenotransplant, proliferative activity was calculated as percentage of MIB-1-stained nuclei per total number of nuclei in four representative cross-sections. Six hundred cells per cross-section and 2,400 cells per tumour were analysed for immunoreactivity. On control sections, the primary antibody was omitted. Further control sections were stained with a non-specific isotype-matched antibody. Figure 1 shows a typical cross-section of an untreated lymphoma xenotransplant and sections from tumours which were dissected 48 h after high-dose chemotherapy or 48 h after immuno- or radioimmunotherapy indicating antiproliferative drug activity. Radiosynthesis of [18F]FLT The synthesis of [18F]FLT is similar to that of the standard radiotracer for PET imaging, [18F]FDG. FLT was produced by the method of Machulla et al. [32] with minor modifications using an automated radiotracer synthesiser (General Electric Medical Systems, Uppsala, Sweden) [31]. Ex vivo [18F]FLT uptake
Fig. 1 Ki-67 immunohistochemistry of representative sections from lymphoma xenotransplants indicating proliferating cells (brownlabelled nuclei). A high proliferation fraction was observed in untreated lymphoma xenotransplants (a, 82% labelled nuclei). A significant but mild decrease was present 48 h after immunotherapy (b, 78% labelled nuclei) and 48 h after radioimmunotherapy with Zevalin (c, 76% labelled nuclei), while there was a more pronounced significant decrease after high-dose chemotherapy with cyclophosphamide (d, 34% labelled nuclei)
counter (Cobra II, Packard Instruments, Meriden, CT). Data were decay corrected and expressed as percent injected dose per gram (% ID/g). Activity in the tail was also measured to correct for potential subcutaneous depots of [18F] FLT. Additionally, tumour-to-muscle ratios were calculated. Statistical analysis GraphPad Prism software (version 4.03, GraphPad, San Diego, CA) was used for statistical analyses. Mean values, median and standard deviation of tumour size, tumoural [18F]FLT uptake, tumour-to-muscle ratios and proliferative activity in controls and mice treated with chemotherapy, immunotherapy or radioimmunotherapy were calculated. The non-parametric Mann-Whitney U test was used to test for statistical significance. A p value lower than 0.05 was considered statistically significant.
Results In controls and treated mice, [18F]FLT was administered via tail vein injection (100 l) at activity doses of 510 MBq per mouse. Ninety minutes after the injection, mice were sacrificed and dissected. Samples of lymphoma xenotransplants and muscle were weighed and the content of radioactivity was determined using an automated gamma Effects of various drug treatments on proliferation rate and tumour size In tissue specimens of untreated lymphoma xenotransplants (n =10), 83.6% of tumour cells exhibited Ki-67-positive
1778
Eur J Nucl Med Mol Imaging (2007) 34:17751782
immunostaining indicating high proliferative activity (median 82.5%, range 80.089.5%, SD 3.2%, Figs. 1 and 2). In the control group, lymphoma xenotransplants consisted mainly of tumour cells and only a minimal amount of stromal cells (<5%). Early antiproliferative effects of CD20 chemotherapy, immunotherapy and radioimmunotherapy were investigated and animals were examined 48 h after treatment. No significant change in the mean diameter of lymphoma xenotransplants was observed at 48 h after therapy, compared with prior to therapy (Mann-Whitney U test). In the control group, mean diameter of lymphoma xenotransplants was 2.3 cm (median 2.3, range 1.62.7, SD 0.4). Mean tumour diameter of mice undergoing chemotherapy, immunotherapy and radioimmunotherapy was 1.9 cm (median 2.0, SD 0.3), 2.3 cm (median 2.1, SD 0.4) and 2.1 cm (median 2.0, SD 0.3), respectively. Forty-eight hours after treatment with saline (control), the mean tumour diameter increased slightly (2.3 cm, median 2.4, range 1.82.7, SD 0.3). After treatment with chemotherapy, mean diameter was 2.0 cm (median 2.1, SD 0.3), after CD20 mAb, 2.1 cm (median 2.1, SD 0.4) and after radioimmunotherapy, 2.0 cm (median 2.0, SD 0.3). In mice treated with high-dose cyclophosphamide (Endoxan, 90 mg/kg, i.p.) a marked decrease in the proliferation rate was observed. The mean value was 39.3% (median 34%, range 2555%, SD 9%; p =0.0001, Fig. 2). Compared with the control group (n =10), immunohistochemistry also showed a mild but significant
reduction in the fraction of proliferating cells in lymphoma xenotransplants (n =10) after immunotherapy (ibritumomab-tiuxetan, 150 mg/ kg i.v.; Fig. 2). The mean value of Ki-67 positive cells was 77.6% (median 76%, range 70 86%, SD 4.8%; p =0.0078). Forty-eight hours after radioimmunotherapy (n =10) with 90Y-labelled CD20 mAb (Zevalin, 5 MBq/mouse, i.v.), the mean proliferation fraction slightly decreased to 78.8% (median 78%, range 6689%, SD 9.8%; p =0.014). Effect of drug treatment on [18F]FLT uptake in lymphoma xenotransplants Alterations in [18F]FLT uptake were assessed 48 h after chemotherapy or CD20 (radio-) immunotherapy (Fig. 2). Compared with controls (mean 5.4% ID/g, median 5.3, n = 10), a significant decrease in tumoural [18F]FLT uptake was observed in cyclophosphamide-treated animals (p =0.0005), the mean value in tumour xenotransplants being 1.5% ID/g (median 1.1%, range 0.13.6%, SD 1.6%). A slightly lower [18F]FLT uptake in lymphoma xenotransplants was observed 48 h after immunotherapy, with a mean value of 3.9% ID/g (median 3.3%, range 1.87.0%, SD 2.0%); however, the difference was not statistically significant. After radioimmunotherapy with 90Y-labelled CD20 mAb, no significant alteration in [18F]FLT uptake was detected (mean 5.8% ID/g, median 6.3%, range 3.27.1%, SD 2.5%). In cyclophosphamide-treated mice, tumour-to-muscle ratios (mean value 1.0, median 0.9, SD 0.7) were
a
p = 0.0001 p = 0.0078
proliferative activity (Ki-67 index)
100 80 60 40 20 0 control
90Y-CD20
b
ns
FLT uptake in lymphoma (%ID/g)
9 8 7 6 5 4 3 2 1 0 mAb CD20 mAb CTX control
p = 0.0005 ns
p = 0.014
90Y-CD20
mAb
CD20 mAb
CTX
Fig. 2 a The mean value of the proliferation fraction was 82% in untreated lymphoma (control, n =10). A significant but mild reduction in the proliferation rate was observed 48 h after radioimmunotherapy (mean 79%, [90Y]CD20 mAb (Zevalin), n =10) and immunotherapy (mean 78%, CD20 mAb). A more pronounced reduction in the proliferation fraction was seen 48 h after chemotherapy (CTX, mean
39%, n =10). b Mean [18F]FLT uptake in lymphoma 48 h after immuno- and radioimmunotherapy (n = 10 each) did not differ significantly from that in the control group. Forty-eight hours after chemotherapy, a significant decrease in [18F]FLT uptake was observed (p =0.0005)
Eur J Nucl Med Mol Imaging (2007) 34:17751782
1779
significantly lower compared with controls (mean value 2.4, median 3.2, SD 1.0). Tumour-to-muscle ratios did not show a significant difference between controls and CD20 mAb-treated animals (1.9, median 2.0, SD 0.7) or 90Y CD20 mAb-treated mice (2.2, median 2.8, SD 1.3). Correlation of proliferative activity and FLT uptake In treated and untreated tumours, linear regression analysis showed a significant correlation of Ki-67 index and [18F] FLT uptake (p =0.0002, r =0.56, Fig. 3a). There was also a significant correlation between tumour-to-muscle ratios and proliferative activity (p =0.0006, r =0.52, Fig. 3b). However, no significant correlations were found between proliferative activity and [18F]FLT uptake in individual groups (untreated controls, r =0.14, p =0.74; chemotherapy, r = 0.32, p =0.40; immunotherapy, r =0.25, p =0.50; radioimmunotherapy, r =0.64, p = 0.06). This is potentially related to the fact that FLT uptake reflects TK1 activity and is therefore only an indirect measure of proliferation whereas Ki-67 immunohistochemistry directly reflects the S-phase fraction of the cell cycle. Moreover, FLT uptake is affected by perfusion and heterogeneity of tumour tissue, whereas immunohistochemistry is unaffected or less affected by these two factors.
Discussion We have recently demonstrated that the thymidine analogue [18F]FLT can be used for non-invasive assessment of proliferative activity in a lymphoma xenotransplant model [28] and in the human disease [28, 31]. A close correlation between proliferation fraction and [18F]FLT uptake in lymphoma was described in the mouse model
12 10 8
(r =0.61) and in patients with low- and high-grade lymphoma (r =0.86). In the present study, we have shown that FLT can also be used for early assessment of the response to drug treatment in lymphoma-bearing mice. Currently, morphology-based imaging techniques such as CT or MRI are the mainstay diagnostic tests to assess response to therapy and to detect residual disease [2, 3]. Usually, imaging is performed weeks or months after initiation of therapy. Early assessment of therapy response would enable the oncologist to stop treatment in the absence of a response and to begin an alternative treatment, thereby preventing unnecessary toxicity and costs. It has already been demonstrated that PET using the glucose analogue [18F]FDG as tracer is a sensitive method for the assessment of cytostatic or cytotoxic effects early in the course of therapy [3335]. [18F]FDG has some limitations due to non-specific accumulation in nontumoural cells, resulting in overestimation of the proportion of viable tumour cells [7, 8, 36]. Compared with [18F]FDG, [18F]FLT and other thymidine analogues have been reported to be more specific for malignant tumours and to closely reflect tumour proliferation [37, 38, 39, 40]. Response assessment was performed as early as 48 h after drug treatment. For therapeutic regimens using monoclonal antibodies a delayed cytotoxic effect has been described [41, 42]. Using CD20 mAb radiolabelled with 90 Y ([90Y]ibritumomab-tiuxetan, Zevalin), treatment-related bone marrow toxicity was reported to occur no earlier than 4 weeks after treatment of lymphoma [40, 42]. Concomitantly, only a mild reduction in the proliferation fraction was detected in our animal model 48 h after treatment with Zevalin. This reduction in proliferation fraction was not associated with a significant decrease in tumoural FLT uptake, presumably owing to tumour heterogeneity.
12 10
R SD N P ----------------------------------------0.56 2.32 40 0.0002 -----------------------------------------
R SD N P ----------------------------------------0.52 1.72 40 0.0006 -----------------------------------------
Tumour / muscle ratio
20 30 40 50 60 70 80 90 100
8 6 4 2 0 20 30 40 50 60 70 80 90 100
% ID / g
6 4 2 0
proliferation fraction
proliferation fraction
Fig. 3 a Linear regression analysis indicates a significant correlation (r =0.56) between FLT uptake (% ID/g) and proliferative activity (Ki67 index, MIB-1 labelled nuclei per total number of nuclei) in treated
and untreated lymphoma xenotransplants. b Linear regression analysis of tumour-to-muscle ratios and proliferation fraction also shows a significant correlation (r =0.52)
1780
Eur J Nucl Med Mol Imaging (2007) 34:17751782
High-dose chemotherapy with cyclophosphamide (CTX, 90 mg/kg i.v.) was used to obtain a maximum therapeutic effect. CTX is an alkylating agent which directly interferes with DNA. The nucleotide salvage pathway and de novo synthesis of thymidine monophosphate are not directly affected [43]. In dissected tissue specimens, there was a decrease in the fraction of proliferating cells from 82% to 39%. Ex vivo gamma counting revealed a corresponding decrease in [18F]FLT uptake from 5.4 to 1.5% ID/g. These findings further support our hypothesis that antiproliferative effects of drug treatment can be detected early by [18F]FLT, before changes in tumour size become visible. A recent study by Leyton et al. also reported a rapid decrease in tumoural [18F]FLT uptake as early as 24 h after treatment of RIF-1 sarcoma-bearing mice with cisplatin [44]. In oesophageal carcinoma cells, Dittmann et al. showed a rapid decrease in [18F]FLT uptake 24 h after therapy with cisplatin [41]. A reduction in tumoural [18F] FLT uptake related to radiotherapy and androgen ablation therapy was demonstrated recently in animal models of prostate cancer [45, 46]. Using an epidermoid carcinoma xenotransplant model, Waldherr et al. demonstrated that [18F]FLT also reflects response to cytostatic therapies such as kinase inhibitors [47]. The rationale for use of [18F]FLT as a surrogate marker for cellular proliferation is based on its substrate specificity for the cell cycle-regulated protein TK1. Barthel et al. recently reported that in vivo uptake of [18F]FLT is closely related to TK1 activity and cellular concentration of ATP [17]. However, [18F]FLT acts as a chain terminator, and only a small amount of intracellular [18F]FLT is incorporated into DNA. [18F]FLT is therefore not a direct marker of proliferation [28, 48]. Other thymidine analogues such as 2 -[ 18 F]fluoro-5-methyl-1- - D -arabinofuranosyl-uracil (FMAU) or 1-(2-deoxy-2-fluoro--D-arabinofuranosyl)-5[76Br]bromouracil (BFU) are incorporated into DNA (the fraction reaching up to 97% of total cell activity) and are therefore potentially more suitable proliferation markers [49, 50]. However, such radiopyrimidines have not yet been studied in vivo and it remains to be determined which radionucleoside is most appropriate for in vivo assessment of tumour proliferation. Several limitations have to be taken into account when extrapolating our findings to other tumour types and to the human disease. In this study we utilised the human lymphoma cell line DoHH2, which expresses high levels of TK1 and which is associated with high proliferative activity [28]. In tumours with low TK1 expression levels or a low proliferation fraction (e.g. low-grade lymphomas), [18F]FLT may be less useful for assessment of therapy response. Recent publications indicate that the metabolism of [18F]FLT is complex, especially in a post-therapy situation [5153]. Perumal et al. reported that [18F]FLT
uptake is related to the expression of equilibrative nucleoside transporters [51]. Kenny and co-workers have found a heterogeneous pattern of FLT uptake in primary tumours and metastases from breast cancer [52]. Heterogeneity of tumours potentially explains the relatively high variability of [18F]FLT uptake found in experimental tumours. A recent study by Muzi et al. indicates that metabolites of [18F]FLT, especially [18F]FLT-glucuronide, may account for up to 30% of the blood activity and can therefore contribute to tumoural [18F]FLT uptake [54]. Furthermore, therapyrelated activation of the thymidylate salvage pathway may increase the uptake of [18F]FLT [41, 51]. After treatment with inhibitors of thymidine monophosphate de novo synthesis [5-fluorouracil (5-FU), methotrexate], a sevento tenfold increase in [18F]FLT uptake in oesophageal carcinoma cells was observed. The authors speculated that this finding was caused by activation of the thymidylate salvage pathway and concomitant increase in TK1 activity [41]. In agreement with this in vitro study, Barthel et al. have found an increase in TK1 protein levels 48 h after 5FU treatment of fibrosarcoma-bearing mice [55]. However, treatment led to a reduction of proliferation fraction and decreased [18F]FLT uptake. This finding may be explained by a decrease in cytoplasmic ATP levels since ATP is an important cofactor of TK1 activity. In the presence of ATP, TK1 forms a tetramer which is 20-fold more effective than the dimer regarding phosphorylation of [18F]FLT. Changes in ATP levels therefore have a major impact on cellular uptake of [18F]FLT. In the latter study, the decrease in [18F] FLT uptake was also more pronounced than that in [18F] FDG uptake, suggesting [18F]FLT to be a promising radiotracer for monitoring drug treatment. However, the detailed uptake mechanism of FLT in various tumours remains to be determined. In conclusion, we have shown that in a mouse model of malignant lymphoma the thymidine analogue [18F]FLT is suitable for early assessment of drug-related cytotoxic effects even before tumour regression is physically detectable. This work suggests the potential use of [18F]FLT for imaging early response to anticancer drug treatment.
Acknowledgements This work was in part supported by grant Bu 1424/1 from Deutsche Forschungsgemeinschaft (DFG, KFO 120) and grant P.777 (Medical Faculty, University of Ulm). We thank Rolf Kunft for his assistance in digital microscopy. We also thank Gabi Ehmke for performing immunohistochemistry and Robert Stadler for his helpful comments on the manuscript.
References
1. Sanchez-Beato M, Sanchez-Aguilera A, Piris MA. Cell cycle deregulation in B-cell lymphomas. Blood 2003;101:122035.
Eur J Nucl Med Mol Imaging (2007) 34:17751782 2. Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkins lymphomas. NCI Sponsored International Working Group. J Clin Oncol 1999;17:124453. 3. Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, et al. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkins disease: Cotswolds meeting. J Clin Oncol 1989;7:16306. 4. Surbone A, Longo DL, DeVita VT Jr, Ihde DC, Duffey PL, Jaffe ES, et al. Residual abdominal masses in aggressive nonHodgkins lymphoma after combination chemotherapy: significance and management. J Clin Oncol 1988;6:18327. 5. Padhani AR, Husband JE. Are current tumor response criteria relevant for the 21st century? Br J Radiol 2000;73:10313. 6. Buck AK, Halter G, Schirrmeister H, Kotzerke J, Wurziger I, Glatting G, et al. Imaging proliferation in lung tumors with PET: [18F]FLT versus [18F]FDG. J Nucl Med 2003;44:142631. 7. Sandherr M, von Schilling C, Link T, Stock K, von Bubnoff N, Peschel C, et al. Pitfalls in imaging Hodgkins disease with computed tomography and positron emission tomography using fluorine-18-fluorodeoxyglucose. Ann Oncol 2001;12:71922. 8. Kazama T, Faria SC, Varavithya V, Phongkitkarun S, Ito H, Macapinlac HA. FDG PET in the evaluation of treatment for lymphoma: clinical usefulness and pitfalls. Radiographics 2005;25:191207. 9. Martiat P, Ferrant A, Labar D, Cogneau M, Bol A, Michel C, et al. In vivo measurement of carbon-11 thymidine uptake in nonHodgkins lymphoma using positron emission tomography. J Nucl Med 1988;29:16337. 10. Shields AF, Mankoff DA, Link JM, Graham MM, Eary JF, Kozawa SM, et al. Carbon-11-thymidine and FDG to measure therapy response. J Nucl Med 1998;39:175762. 11. Shields AF, Grierson JR, Dohmen BM, Machulla HJ, Stayanoff JC, Lawhorn-Crews JM, et al. Imaging proliferation in vivo with [18F]FLT and positron emission tomography. Nat Med 1998;4:13346. 12. Kong XB, Zhu QY, Vidal PM, Watanabe KA, Polsky B, Armstrong D, et al. Comparisons of anti-human immunodeficiency virus activities, cellular transport, and plasma and intracellular pharmacokinetics of 3-fluoro-3-deoxythymidine and 3-azido-3deoxythymidine. Antimicrob Agents Chemother 1992;36:80818. 13. Sherley JL, Kelly TJ. Regulation of human thymidine kinase during the cell cycle. J Biol Chem 1988;263:83508. 14. Eriksson S, Arner E, Spasokoukotskaja T, Wang L, Karlsson A, Brosjo O, et al. Properties and levels of deoxynucleoside kinases in normal and tumor cells; implications for chemotherapy. Adv Enzyme Regul 1994;34:1325. 15. Seitz U, Wagner M, Neumaier B, Wawra E, Glatting G, Leder G, et al. Evaluation of pyrimidine metabolising enzymes and in vitro uptake of 3-[18F]fluoro-3-deoxythymidine ([18F]FLT) in pancreatic cancer cell lines. Eur J Nucl Med Mol Imaging 2002; 29:117481. 16. Rasey JS, Grierson JR, Wiens LW, Kolb PD, Schwartz JL. Validation of FLT uptake as a measure of thymidine kinase-1 activity in A549 carcinoma cells. J Nucl Med 2002;43:12107. 17. Barthel H, Perumal M, Latigo J, He Q, Brady F, Luthra SK, et al. The uptake of 3-deoxy-3-[18F]fluorothymidine into L5178Y tumours in vivo is dependent on thymidine kinase 1 protein levels. Eur J Nucl Med Mol Imaging 2005;32:25763. 18. Lu L, Samuelsson L, Bergstrom M, Sato K, Fasth KJ, Langstrom B. Rat studies comparing 11C-FMAU, [18F]FLT, and [76Br]BFU as proliferation markers. J Nucl Med 2002;43:168898. 19. Francis DL, Freeman A, Visvikis D, Costa DC, Luthra SK, Novelli M, et al. In vivo imaging of cellular proliferation in
1781 colorectal cancer using positron emission tomography. Gut 2003;52:16026. Smyczek-Gargya B, Fersis N, Dittmann H, Vogel U, Reischl G, Machulla HJ, et al. PET with [18F]fluorothymidine for imaging of primary breast cancer: a pilot study. Eur J Nucl Med Mol Imaging 2004;31:7204. Cobben DC, van der Laan BF, Maas B, Vaalburg W, Suurmeijer AJ, Hoekstra HJ, et al. [18F]FLT PET for visualization of laryngeal cancer: comparison with [18F]FDG PET. J Nucl Med 2004;45:22631. Cobben DC, Elsinga PH, Suurmeijer AJ, Vaalburg W, Maas B, Jager PL, et al. Detection and grading of soft tissue sarcomas of the extremities with [18F]-3-fluoro-3-deoxy-L-thymidine. Clin Cancer Res 2004;10:168590. Choi SJ, Kim JS, Kim JH, Oh SJ, Lee JG, Kim CJ, et al. [18F]3deoxy-3-fluorothymidine PET for the diagnosis and grading of brain tumors. Eur J Nucl Med Mol Imaging 2005;32:6539. Chen W, Cloughesy T, Kamdar N, Satyamurthy N, Bergsneider M, Liau L, et al. Imaging proliferation in brain tumors with [18F]-FLT PET: comparison with [18F]-FDG. J Nucl Med 2005;46:94552. van Westreenen HL, Cobben DC, Jager PL, van Dullemen HM, Wesseling J, Elsinga PH. Comparison of 18F-FLT PET and 18FFDG PET in esophageal cancer. J Nucl Med 2005;46:4004. Dittmann H, Dohmen BM, Paulsen F, Eichhorn K, Eschmann SM, Horger M, et al. [18F]FLT PET for diagnosis and staging of thoracic tumours. Eur J Nucl Med Mol Imaging 2003;30: 140712. Buck AK, Schirrmeister H, Hetzel M, Von Der Heide M, Halter G, Glatting G, et al. 3-deoxy-3-[18F]fluorothymidine-positron emission tomography for noninvasive assessment of proliferation in pulmonary nodules. Cancer Res 2002;62:33314. Wagner M, Seitz U, Buck A, Neumaier B, Schultheiss S, Bangerter M, et al. 3-[18F]fluoro-3-deoxythymidine ([18F]FLT) as positron emission tomography tracer for imaging proliferation in a murine B-cell lymphoma model and in the human disease. Cancer Res 2003;63:26817. Buchmann I, Neumaier B, Schreckenberger M, Reske S. [18F]3deoxy-3-fluorothymidine-PET in NHL patients: whole-body biodistribution and imaging of lymphoma manifestationsa pilot study. Cancer Biother Radiopharm 2004;19:43642. Vesselle H, Grierson J, Muzi M, Pugsley JM, Schmidt RA, Rabinowitz P, et al. In vivo validation of 3deoxy-3-[18F] fluorothymidine ([18F]FLT) as a proliferation imaging tracer in humans: correlation of [18F]FLT uptake by positron emission tomography with Ki-67 immunohistochemistry and flow cytometry in human lung tumors. Clin Cancer Res 2002;8:331523. Buck AK, Bommer M, Stilgenbauer S, Juweid M, Glatting G, Schirrmeister H, et al. Molecular imaging of proliferation in malignant lymphoma. Cancer Res 2006;66:1105561. Machulla HJ, Blocher A, Kuntzsch M. Simplified labeling approach for synthesizing 3-deoxy-3[18F]fluorothymidine ([18F] FLT). J Radioanal Nucl Chem 2000;24:8436. Mikhaeel NG, Timothy AR, ODoherty MJ, Hain S, Maisey MN. [18F]FDG-PET as a prognostic indicator in the treatment of aggressive non-Hodgkins lymphomacomparison with CT. Leuk Lymphoma 2000;39:54353. Kostakoglu L, Goldsmith SJ. 18F-FDG PET evaluation of the response to therapy for lymphoma and for breast, lung, and colorectal carcinoma. J Nucl Med 2003;44:22439. Romer W, Hanauske AR, Ziegler S, Thodtmann R, Weber W, Fuchs C, et al. Positron emission tomography in non-Hodgkins lymphoma: assessment of chemotherapy with fluorodeoxyglucose. Blood 1998;91:446471. Spaepen K, Stroobants S, Dupont P, Bormans G, Balzarini J, Verhoef G, et al. [18F]FDG PET monitoring of tumor response to
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
1782 chemotherapy: does [18F]FDG uptake correlate with the viable tumor cell fraction? Eur J Nucl Med Mol Imaging 2003;30:6828. van Waarde A, Cobben DC, Suurmeijer AJ, Maas B, Vaalburg W, de Vries EF, et al. Selectivity of [18F]FLT and [18F]FDG for differentiating tumor from inflammation in a rodent model. J Nucl Med 2004;45:695700. Buck AK, Hetzel M, Schirrmeister H, Halter G, Moller P, Kratochwil C, et al. Clinical relevance of imaging proliferative activity in lung nodules. Eur J Nucl Med Mol Imaging 2005;32:52533. Rose AL, Smith BE, Maloney DG. Glucocorticoids and rituximab in vitro: synergistic direct antiproliferative and apoptotic effects. Blood 2002;100:176573. Hainsworth JD. Monoclonal antibody therapy in lymphoid malignancies. Oncologist 2000;5:37684. Dittmann H, Dohmen BM, Kehlbach R, Bartusek G, Pritzkow M, Sarbia M, et al. Early changes in [18F]FLT uptake after chemotherapy: an experimental study. Eur J Nucl Med Mol Imaging 2002;29:14629. Wiseman GA, Gordon LI, Multani PS, Witzig TE, Spies S, Bartlett NL, et al. Ibritumomab tiuxetan radioimmunotherapy for patients with relapsed or refractory non-Hodgkin lymphoma and mild thrombocytopenia: a phase II multicenter trial. Blood 2002;99:433642. Kano Y, Akutsu M, Tsunoda S, Mano H, Sato Y, Honma Y, et al. In vitro cytotoxic effects of a tyrosine kinase inhibitor STI571 in combination with commonly used antileukemic agents. Blood 2001;97:19992007. Leyton J, Latigo JR, Perumal M, Dhaliwal H, He Q, Aboagye EO. Early detection of tumor response to chemotherapy by 3-deoxy3-[18F]fluorothymidine positron emission tomography: the effect of cisplatin on a fibrosarcoma tumor model in vivo. Cancer Res 2005;65:420210. Oyama N, Ponde DE, Dence C, Kim J, Tai YC, Welch MJ. Monitoring of therapy in androgen-dependent prostate tumor model by measuring tumor proliferation. J Nucl Med 2004;45:51925. Sugiyama M, Sakahara H, Sato K, Harada N, Fukumoto D, Kakiuchi T, et al. Evaluation of 3-deoxy-3-[18F]-fluorothymidine
Eur J Nucl Med Mol Imaging (2007) 34:17751782 for monitoring tumor response to radiotherapy and photodynamic therapy in mice. J Nucl Med 2004;45:17548. Waldherr C, Mellinghoff IK, Tran C, Halpern BS, Rozengurt N, Safaei A, et al. Monitoring antiproliferative responses to kinase inhibitor therapy in mice with 3-deoxy-3-18F-fluorothymidine PET. J Nucl Med 2005;46:11420. Shields AF, Briston DA, Chandupatla S, Douglas KA, LawhornCrews J, Collins JM, et al. A simplified analysis of [18F]3-deoxy3-fluorothymidine metabolism and retention. Eur J Nucl Med Mol Imaging 2005;259:126975. Bading JR, Shahinian AH, Vail A, Bathija P, Koszalka GW, Koda RT, et al. Pharmacokinetics of the thymidine analogue 2-fluoro5-methyl-1-beta-D-arabinofuranosyluracil (FMAU) in tumorbearing rats. Nucl Med Biol 2004;31:40718. Lu L, Samuelsson L, Bergstrom M, Sato K, Fasth KJ, Langstrom B. Rat studies comparing [11C]FMAU, [18F]FLT, and [76Br]BFU as proliferation markers. J Nucl Med 2002;43:168898. Perumal M, Pillai RG, Barthel H, Leyton J, Latigo JR, Forster M, et al. Redistribution of nucleoside transporters to the cell membrane provides a novel approach for imaging thymidylate synthase inhibition by positron emission tomography. Cancer Res 2006;66:855864. Kenny LM, Vigushin DM, Al-Nahhas A, Osman S, Luthra SK, Shousha S, et al. Quantification of cellular proliferation in tumor and normal tissues of patients with breast cancer by [18F] fluorothymidine-positron emission tomography imaging: evaluation of analytical methods. Cancer Res 2005;65:1010412. Muzi M, Mankoff DA, Grierson JR, Wells JM, Vesselle H, Krohn KA. Kinetic modeling of 3-deoxy-3-fluorothymidine in somatic tumors: mathematical studies. J Nucl Med 2005;46:37180. Muzi M, Vesselle H, Grierson JR, Mankoff DA, Schmidt RA, Peterson L, et al. Kinetic analysis of 3-deoxy-3-fluorothymidine PET studies: validation studies in patients with lung cancer. J Nucl Med 2005;46:27482. Barthel H, Cleij MC, Collingridge DR, Hutchinson OC, Osman S, He Q, et al. 3-deoxy-3-[18F]fluorothymidine as a new marker for monitoring tumor response to antiproliferative therapy in vivo with positron emission tomography. Cancer Res 2003;63:37918.
37.
47.
38.
48.
39.
49.
40. 41.
50.
51.
42.
52.
43.
44.
53.
54.
45.
55.
46.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 5.4 SCADA System Functional RequirementsDocument85 pages5.4 SCADA System Functional RequirementsYinwu ZhaoNo ratings yet
- Geothermal Energy Poster 2Document1 pageGeothermal Energy Poster 2api-298575301100% (2)
- Run-On and FregmentsDocument29 pagesRun-On and FregmentsMushtaq AhmadNo ratings yet
- Surrogacy Contract Sample 070215 PDFDocument26 pagesSurrogacy Contract Sample 070215 PDFBalbir DhimanNo ratings yet
- CACR21 January 2015Document19 pagesCACR21 January 2015maikaNo ratings yet
- 48 Weeks To Total M-Powerment!Document18 pages48 Weeks To Total M-Powerment!sundevil2010usa4605No ratings yet
- NYJC Prelim 2006 P2Document12 pagesNYJC Prelim 2006 P2miiewNo ratings yet
- F1.4 - Marine Sediment Treatment and ReuseDocument14 pagesF1.4 - Marine Sediment Treatment and ReuseKwan Chun SingNo ratings yet
- Experiment 13 Ultrafiltration UnitDocument13 pagesExperiment 13 Ultrafiltration UnitKishen NaniNo ratings yet
- Salvador Sanchez Complaint SignedDocument2 pagesSalvador Sanchez Complaint SignedStephen LoiaconiNo ratings yet
- A Review On The Enhancement of Figure of MeritDocument23 pagesA Review On The Enhancement of Figure of Meritsasa_22No ratings yet
- 5 ElementosDocument3 pages5 ElementosHectorNo ratings yet
- Unit 5. PHCDocument24 pagesUnit 5. PHCFenembar MekonnenNo ratings yet
- Golis University: Faculty of Business and Economics Chapter Four (Part Two) Accounting Information SystemDocument32 pagesGolis University: Faculty of Business and Economics Chapter Four (Part Two) Accounting Information Systemsaed cabdiNo ratings yet
- RS 232 Repeater KFD2-FF-Ex2.RS232: FunctionDocument4 pagesRS 232 Repeater KFD2-FF-Ex2.RS232: FunctionEder AlexandreNo ratings yet
- Dermatology: Professional Certificate inDocument4 pagesDermatology: Professional Certificate inmadimadi11No ratings yet
- Winsem2014-15 Cp0670 17-Apr-2015 Rm01 U4 l4 Rainwater-HarvestingDocument12 pagesWinsem2014-15 Cp0670 17-Apr-2015 Rm01 U4 l4 Rainwater-HarvestingShiv ShivNo ratings yet
- Unfuck Your Anilingus - How To Keep Your Oral Butt Sex Classy - Faith G Harper - 2022 - Microcosm Publishing - 9781648411618 - Anna's ArchiveDocument28 pagesUnfuck Your Anilingus - How To Keep Your Oral Butt Sex Classy - Faith G Harper - 2022 - Microcosm Publishing - 9781648411618 - Anna's Archiverhy4kjgqx6No ratings yet
- Petroleum Refining Notes 1Document5 pagesPetroleum Refining Notes 1api-304149645No ratings yet
- Oxidation of N-Acetyl Alanine by Chloramine-T in Presence of Hydrochloric Acid: A Kinetic and Mechanistic StudyDocument10 pagesOxidation of N-Acetyl Alanine by Chloramine-T in Presence of Hydrochloric Acid: A Kinetic and Mechanistic StudyCentral Asian StudiesNo ratings yet
- Significant Risk RegisterDocument8 pagesSignificant Risk RegisterswestyNo ratings yet
- Upda-Multiple Choice QuestionsDocument39 pagesUpda-Multiple Choice QuestionsAnonymous GllSJsUNo ratings yet
- CP SYSTEM - DESIGN DOCUMENT (Rev.01)Document46 pagesCP SYSTEM - DESIGN DOCUMENT (Rev.01)suman ghosh100% (1)
- Manual Usuario Smart LGDocument36 pagesManual Usuario Smart LGkarl CgcNo ratings yet
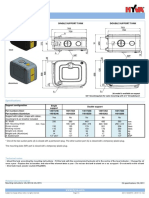
- Hyva Oil Tank: Single Support Tank Double Support TankDocument4 pagesHyva Oil Tank: Single Support Tank Double Support TankPutera Bumi NusantaraNo ratings yet
- Alexandra Marchuk V Faruqi and Faruqi AnswerDocument52 pagesAlexandra Marchuk V Faruqi and Faruqi Answerdavid_latNo ratings yet
- Snowball SamplingDocument3 pagesSnowball SamplingHamza ChNo ratings yet
- AaaaaaaaaaaaaaDocument6 pagesAaaaaaaaaaaaaaCarlos CBNo ratings yet
- UD150L-40E Ope M501-E053GDocument164 pagesUD150L-40E Ope M501-E053GMahmoud Mady100% (3)
- Biology Paper Ib: Maple Leaf International SchoolDocument22 pagesBiology Paper Ib: Maple Leaf International SchoolFcgfht ghkhkujk100% (1)