Professional Documents
Culture Documents
Functional Reach Test
Functional Reach Test
Uploaded by
scribdmelwinOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Functional Reach Test
Functional Reach Test
Uploaded by
scribdmelwinCopyright:
Available Formats
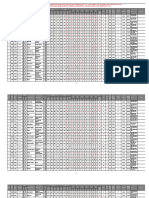
Name of Instrument: Functional Reach Test Author: Pamela W. Duncan, Debra K.
Weiner, Julie Chandler and Stephanie Studenski
Contact Info: Name: Address: Pamela W. Duncan Graduate Program in Physical Therapy P.O. Box 3965, Duke University Medical Center Durham, NC 27710
Phone: Fax: E-mail: Privacy Use Cost: $ Public Use Cost: $ Year Developed: 1990 Where to obtain Instrument: Contact author Other: www.arom.com Description of the Instrument Functional Reach test is a measure of balance and is the difference, in inches, between arm's length and maximal forward reach, using a fixed base of support. This test can be used to detect balance impairment, change in balance performance over time, and in the design of modified environments for impaired older persons. The test utilizes a force platform, an electronic system for measuring functional reach or a 48-inch measuring device or "yardstick". A reach of less than or equal to 6 inches predicted fall Form of instrument: Risk/Hazard Assessment Tool Method of delivery: In-person interview/assessment Relevance to injury/ Percentage of the instrument specific to injury To assess balance that may contribute to risk of falling among the elderly. Time to administer or complete the instrument 1-2 minutes Methods of data analyses: Quantitative
Setting/sample instrument used in: Volunteers, age 21-87 years, were recruited from 3 resources: a) employees at the Duke University Medical Center and the Durham Veterans Administration Hospital; b) students of the Duke University Physical Therapy Program; and c) the Duke Aging Center registry of community-dwelling elderly. Was it pilot tested? No Pilot test sample: Reliability Measures Test-retest reliability r = .89 Interrater agreement on reach measurement = .98 Validity Measures Functional Reach Test was strongly associated with measurements of centre of pressure excursion r = .71 and the R2 using linear regression was .51. Additional testing completed by Eagle et al. (1999) on a sample of elderly inpatients indicated the following: Sensitivity (ability to detect falls when they are present) = 76% Specificity (ability to identify correctly the absence of falls) = 34% Positive Predictive Value (how well test predicted compared to actual number of falls) = 33% Negative Predictive Value (how well negative test correctly predicts absence of falls) = 77% Accuracy (overall rate of agreement between the test and the actual number of falls) = 46% Prevalence (ratio of the number of people who have fallen divided by the total number of people at risk for falling) = 30% Reference Duncan, P.W., Weiner, D.K., Chandler, J. & Studenski, S. (1990). Functional reach: a new clinical measure of balance. Journal of Gerontology: MEDICAL SCIENCES, 45(6), M192-M197. Other References Eagle, J., Salamara, S., Whitman, D., Evans, L.A., Ho, E., & Olde, J. (1999). Comparison of Three Instruments in Predicting Accidental Falls in Selected Inpatients in a General Teaching Hospital. Journal of Gerontological Nursing, 25(7), 40-45. Whitney, S.L., Poole, J.L., & Cass, S.P. (1999). A Review of Balance Instruments for Older Adults. The American Journal of Occupational Therapy, 52(8), 666-671. Keywords: falls, fall prevention, elderly, seniors, asssessment.
You might also like
- Epidemiology Cheat SheetDocument4 pagesEpidemiology Cheat SheetElizabeth100% (2)
- Role Play Script EnglishDocument7 pagesRole Play Script EnglishLilii Duii Asharii100% (1)
- Fall Prevention PosterDocument1 pageFall Prevention Posterapi-241173284No ratings yet
- 3 Chapter 3. MethodologyDocument41 pages3 Chapter 3. MethodologyJerome Alvarez100% (2)
- Tutorial 9 PDFDocument6 pagesTutorial 9 PDFPututWisnuNugrohoNo ratings yet
- Annual Medical ReportDocument6 pagesAnnual Medical ReportMarvin Joseph AndalNo ratings yet
- The Global Pharmaceutical Industry Case Study Scenario PlanningDocument4 pagesThe Global Pharmaceutical Industry Case Study Scenario PlanningIke Ten100% (1)
- Ecg in Emergency Medicine and Acute Care-2005Document420 pagesEcg in Emergency Medicine and Acute Care-2005Ioana Nicoleta Dinu91% (22)
- Critiquing Assessment Tool FRTDocument3 pagesCritiquing Assessment Tool FRTJustine RamosNo ratings yet
- Quality Assurance in Hematology Group 11Document51 pagesQuality Assurance in Hematology Group 11Mandy A. DelfinNo ratings yet
- Validity and ReliabilityDocument7 pagesValidity and ReliabilityKelsey WrightNo ratings yet
- Reliability and ValidityDocument22 pagesReliability and Validityreza.ws1No ratings yet
- Epi-Lessons 5Document44 pagesEpi-Lessons 5Najeeb haiderNo ratings yet
- Quality ControlDocument19 pagesQuality ControlFrankenstein MelancholyNo ratings yet
- Dementia and Effort Test PerformanceDocument21 pagesDementia and Effort Test PerformanceIcaroNo ratings yet
- 2014 Article 752Document5 pages2014 Article 752AntenehNo ratings yet
- Sample Size For Pre-Tests of Questionnaires: Quality of Life Research July 2014Document6 pagesSample Size For Pre-Tests of Questionnaires: Quality of Life Research July 2014dianafauziyyahNo ratings yet
- Grip Strength in Children Test-Retest Reliability Using GrippitDocument6 pagesGrip Strength in Children Test-Retest Reliability Using GrippitJosariaFerrazNo ratings yet
- Prognostic TestsDocument3 pagesPrognostic TestsHANS BENNo ratings yet
- Most Frequently Used Terms in Biostatistics: Your LogoDocument44 pagesMost Frequently Used Terms in Biostatistics: Your LogocainbelzebubNo ratings yet
- Data Presentation in The ALARM International Program: DefinitionsDocument5 pagesData Presentation in The ALARM International Program: DefinitionsgirezaNo ratings yet
- Diagnostic Test DesignDocument30 pagesDiagnostic Test DesignDika Gita PratamaNo ratings yet
- Quality Control in Clinical Biochemistry BMLTDocument56 pagesQuality Control in Clinical Biochemistry BMLTSelim JaforNo ratings yet
- Ultrasound Guided Vascular AccessDocument19 pagesUltrasound Guided Vascular Accessdragon_hubo100% (2)
- A Guide To Validation in HPLC: R.A. Van Iterson Drenthe College Emmen HollandDocument15 pagesA Guide To Validation in HPLC: R.A. Van Iterson Drenthe College Emmen HollandBHASKARNo ratings yet
- HPLC ValidationDocument15 pagesHPLC ValidationRambabu komati - QA100% (5)
- The Norton ScaleDocument4 pagesThe Norton ScaleFadityo PrihantoroNo ratings yet
- Clinical Measurement (Pgs 24) : Normal Skewed Kurtosis KurtosisDocument15 pagesClinical Measurement (Pgs 24) : Normal Skewed Kurtosis KurtosisConnorNo ratings yet
- Characteristics of Research ToolsDocument3 pagesCharacteristics of Research ToolsLalrinchhani SailoNo ratings yet
- Kajal Srivastava SPM Deptt. S.N.Medical College,: Determining The Size of A SampleDocument38 pagesKajal Srivastava SPM Deptt. S.N.Medical College,: Determining The Size of A SampleAnkit TomarNo ratings yet
- Critical AppraisalDocument3 pagesCritical Appraisalumar asadullahNo ratings yet
- Chapter No. 08 Fundamental Sampling Distributions and Data Descriptions - 02 (Presentation)Document91 pagesChapter No. 08 Fundamental Sampling Distributions and Data Descriptions - 02 (Presentation)Sahib Ullah MukhlisNo ratings yet
- Analytical Chemistry - Errors in Chemical AnalysesDocument20 pagesAnalytical Chemistry - Errors in Chemical AnalysesAdilla Rizka YonitaNo ratings yet
- Pilot Study ReportDocument3 pagesPilot Study ReportAkshata BansodeNo ratings yet
- Meta-Analysis: Montarat Thavorncharoensap, Ph.D. Faculty of Pharmacy, Mahidol UniversityDocument44 pagesMeta-Analysis: Montarat Thavorncharoensap, Ph.D. Faculty of Pharmacy, Mahidol UniversityNanangNo ratings yet
- Psycass ReviewerDocument19 pagesPsycass ReviewerHeidi BrionesNo ratings yet
- Tinetti Balance Scale InstrumentDocument2 pagesTinetti Balance Scale InstrumentInilah Namanya WestaNo ratings yet
- Week Systematic Errors and Random Errors in AnalysisDocument9 pagesWeek Systematic Errors and Random Errors in AnalysisVijay Kumar VishvakarmaNo ratings yet
- Cross Sectional Studies 1Document49 pagesCross Sectional Studies 1Noha SalehNo ratings yet
- Study Desien - by Tahani AlghamdiDocument41 pagesStudy Desien - by Tahani AlghamdiMian. Shoaib.No ratings yet
- A Randomized Trial of Urodynamic Testing Before Stress-Incontinence SurgeryDocument11 pagesA Randomized Trial of Urodynamic Testing Before Stress-Incontinence SurgeryHerlin Ajeng NurrahmaNo ratings yet
- Module 3 - MeasurementDocument10 pagesModule 3 - MeasurementCaleb KimNo ratings yet
- EBM, Design Study, Quantifying RiskDocument71 pagesEBM, Design Study, Quantifying Riskseptian kristyanaNo ratings yet
- Improving The Healthcare Quality Measurement System Using Attribute Agreement Analysis Assessing The Presence and Stage of Pressure UlcersDocument13 pagesImproving The Healthcare Quality Measurement System Using Attribute Agreement Analysis Assessing The Presence and Stage of Pressure UlcersAyman AlhalfawyNo ratings yet
- Screening TestDocument22 pagesScreening TestRabea DiaNo ratings yet
- Evaluation of Textile Materials: Practical StatisticsDocument23 pagesEvaluation of Textile Materials: Practical StatisticsSam DNo ratings yet
- Evaluating Clinical Rating Scales For Evidence Based Derm - 2005 - DermatologicDocument4 pagesEvaluating Clinical Rating Scales For Evidence Based Derm - 2005 - DermatologicMilena MonteiroNo ratings yet
- ENG - Epidemiology Biostatistics IMGDocument8 pagesENG - Epidemiology Biostatistics IMGManivanh AvalosNo ratings yet
- Uts WPS OfficeDocument7 pagesUts WPS OfficeSintia DeviNo ratings yet
- 1 BasicDocument21 pages1 Basicmahir faisalNo ratings yet
- Aea2014 Ps MetaDocument24 pagesAea2014 Ps Metascrib@pym.clNo ratings yet
- WINSEM2022-23 BBIT206L TH VL2022230501238 Reference Material I 20-12-2022 Accuracy and PrecisionDocument21 pagesWINSEM2022-23 BBIT206L TH VL2022230501238 Reference Material I 20-12-2022 Accuracy and PrecisionGravity JaiNo ratings yet
- Research Question (Truth in The Universe) Study Plan (Truth in The Study)Document7 pagesResearch Question (Truth in The Universe) Study Plan (Truth in The Study)natrix029No ratings yet
- Journal ClubDocument6 pagesJournal ClubRoselineTiggaNo ratings yet
- Evaluating Agreement - Conducting A Reliability Study 2009Document8 pagesEvaluating Agreement - Conducting A Reliability Study 2009CarlosNo ratings yet
- Errors of Research: Fajar Awalia YuliantoDocument22 pagesErrors of Research: Fajar Awalia YuliantoaureliNo ratings yet
- Event-And Interval-Based Measurement of Stuttering: A ReviewDocument17 pagesEvent-And Interval-Based Measurement of Stuttering: A ReviewMarjorie TovarNo ratings yet
- Diagnostic Accuracy Measures: Methodological NotesDocument6 pagesDiagnostic Accuracy Measures: Methodological NotesFrontiersNo ratings yet
- Evidence Based Medicine: Kiki Lukman, Bagian Bedah Fakultas Kedokteran UNPAD/ RS DR Hasan Sadikin BandungDocument70 pagesEvidence Based Medicine: Kiki Lukman, Bagian Bedah Fakultas Kedokteran UNPAD/ RS DR Hasan Sadikin BandungOby BedahNo ratings yet
- Reviewer in Practical Research 2Document12 pagesReviewer in Practical Research 2theadominiquecruz3018No ratings yet
- Concise Biostatistical Principles & Concepts: Guidelines for Clinical and Biomedical ResearchersFrom EverandConcise Biostatistical Principles & Concepts: Guidelines for Clinical and Biomedical ResearchersNo ratings yet
- Sample Size for Analytical Surveys, Using a Pretest-Posttest-Comparison-Group DesignFrom EverandSample Size for Analytical Surveys, Using a Pretest-Posttest-Comparison-Group DesignNo ratings yet
- Diagnostic Tests of Placenta Accreta Index Score PDocument6 pagesDiagnostic Tests of Placenta Accreta Index Score PBogdan CăpățînăNo ratings yet
- Medicine Blue Book: Sixth EditionDocument12 pagesMedicine Blue Book: Sixth EditionFlorence MarzanNo ratings yet
- HELLP Syndrome: The State of The Art: Secondary Logo Journal LogoDocument3 pagesHELLP Syndrome: The State of The Art: Secondary Logo Journal LogoFaheem AshrafNo ratings yet
- List of Equipment and Supplies For Pediatric Units.Document11 pagesList of Equipment and Supplies For Pediatric Units.vruttika parmar0% (1)
- M7872 - Novartis-GSK OncologyDocument10 pagesM7872 - Novartis-GSK OncologycgmenesesNo ratings yet
- Pharma IndustriesDocument21 pagesPharma IndustriesNamratha. N100% (1)
- File No Seat No.: OptionsDocument41 pagesFile No Seat No.: OptionsShujat AbroNo ratings yet
- Health Report SWG 16.11.18 Final PDFDocument248 pagesHealth Report SWG 16.11.18 Final PDFFrancis Mwangi ChegeNo ratings yet
- OCR BlueprintsSeries PediatricInfectiousDiseases2004ShahDocument237 pagesOCR BlueprintsSeries PediatricInfectiousDiseases2004ShahAnthonyJohanNo ratings yet
- Brosur DIAREDocument3 pagesBrosur DIAREHumaira AzzahraNo ratings yet
- Nabh Entry Level StandardsDocument46 pagesNabh Entry Level StandardsDr. Suhas SodalNo ratings yet
- INBDE Day 2Document11 pagesINBDE Day 2Mirza Hammad Ul-HaqNo ratings yet
- Ear, Nose and Throat EmergenciesDocument3 pagesEar, Nose and Throat Emergenciesfmta100% (1)
- Dr. Steevens' Hospital Dublin 8: Nurses and Midwives With The Nursing and Midwifery Board of IrelandDocument2 pagesDr. Steevens' Hospital Dublin 8: Nurses and Midwives With The Nursing and Midwifery Board of IrelandLexNo ratings yet
- Final Round Case PDFDocument20 pagesFinal Round Case PDFTahiratul ElmaNo ratings yet
- Covid-19 Vaccine and The Abortion IssueDocument4 pagesCovid-19 Vaccine and The Abortion IssuerickyNo ratings yet
- Stunting Goudet Et Al-2019-Cochrane Database of Systematic ReviewsDocument4 pagesStunting Goudet Et Al-2019-Cochrane Database of Systematic ReviewsWienta DiarsvitriNo ratings yet
- Iso Ca1 Prelimexam With RatioDocument15 pagesIso Ca1 Prelimexam With RatioJenny Yen100% (1)
- Data SDM Klinik Graha MedikaDocument1 pageData SDM Klinik Graha MedikaSuryasana EkaputraNo ratings yet
- A Retrospective Analysis of Fourniers Gangrene at A TertiaryGovernment Hospital in The PhilippinesDocument3 pagesA Retrospective Analysis of Fourniers Gangrene at A TertiaryGovernment Hospital in The PhilippinesGian PagadduNo ratings yet
- Assignment InternsDocument8 pagesAssignment Internssai revanthNo ratings yet
- Rabies CaseDocument3 pagesRabies CaseanastasiaNo ratings yet
- Operative Delivery: Presenters: Yonas Gudeta (RMHS/402/09)Document71 pagesOperative Delivery: Presenters: Yonas Gudeta (RMHS/402/09)Jhon Negesse100% (1)
- Grainger & Allison's Diagnostic Radiology SadrzajDocument8 pagesGrainger & Allison's Diagnostic Radiology SadrzajAleksandar MilosavljevicNo ratings yet
- Fitness To Work - 9 NovDocument2 pagesFitness To Work - 9 NovWilson Ong Ying FaNo ratings yet
- Gda AnswersDocument15 pagesGda AnswersSameer Gulhane100% (1)