Professional Documents
Culture Documents
Case Report Ii.1 Identification Ii.3 Phisycal Examination
Case Report Ii.1 Identification Ii.3 Phisycal Examination
Uploaded by
Masayu Mutiara UtiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Report Ii.1 Identification Ii.3 Phisycal Examination
Case Report Ii.1 Identification Ii.3 Phisycal Examination
Uploaded by
Masayu Mutiara UtiCopyright:
Available Formats
CHAPTER II CASE REPORT II.1 IDENTIFICATION Name : Mrs.
. N Age : 60 years old Sex : female Address : Cempaka Dalam Status : married Occupation : housewive Hospitalized : October, 9th 2009 (12.40 a.m) II.2 ANAMNESIS Chief of complaint Bulging of the abdomen that became even larger since two weeks before admission History Of Illness 2 months before admission, the patient complained about bulging of her abdomen, her bulging abdomen seemed to spread evenly so she found some difficulty in wearing her outfits. The patient felt uncomfort, heavy, and full of stomach that caused the decrease in her appetite, there was no constant pain on her abdomen. There was no nausea, vomiting, or fever. Her body became weak. In addition, both of her legs were swollen too, but she neither had the swelling eyelids especially when she woke up in the morning nor itching on her skin. Because of her bulging abdomen, she sometimes felt shortness of her breath (dyspnea). Her dyspnea were not caused by her activities, emotional conditions, weathers, and never produced ngik sound. She still can sleep with one pillow, she never woke up in the middle of her night-time sleep because of short winded. She said sometimes she may had dark yellow or brown colored urine, but never passed black or bloody stools. Theres no others complaint in defecation and urination habits. She went to the local health care center and took some medicines (she didnt know name of drugs) but there was no improvement. 2 weeks before admission because of her abdomen seemed even more larger and tense, she had nausea and vomits, three times, containing all foods and fluids that she had been consumed that day. There was no blood in her vomit and no dark/bloody stools. Then, she was hospitalized in Moh. Hoesin Hospital in order to receive some better treatments. History of past illness No history of liver disease No history of blood tranfusion No history of consuming alcohol History of consuming herbal medicines homemade admitted History of hypertension History of familys diseases There is no patients family who have the same complaints of the disease
II.3 PHISYCAL EXAMINATION General condition (10, 9th 2009) General condition: sick Sickness condition : moderate sickness Conciousness : compos mentis Blood preassure : 180/100 mmHg Pulse rate : 108x/minute, regular, equal. Respiration rate : 20x/minute, regular (thoracal type) Temperature : 36,50C Nutrition state : normoweight (BW: 60 kgs; H: 150 cms, BMI: 19,53) Dehydration : (-) Spesific condition Skin The color of the skin is black-brown, eflorescency and scar (-), abnormal pigmentation (-), enough turgor, icteric (-), cyanosis (-), pale on palm of hands (-), pale on sole of feet (-), spider naevy (-), subcutaneous nodul (-), normal hair growth. Lymph nodes There are no enlargment of the lymph nodes on submandibular, neck, axilaries, and inguinal. Head Oval, symmetrical, alopecia (-), puffy face (-), deformity (-), malar rash (-). Eyes Exopthalmus (-), endopthalmus (-), edematous of superior palpebrae (-), pale of conjungtiva palpebrae (+), icteric sclera (+), pupils were isokor, Good light response on both of eyes, symmetrical eyes movements. Nose Epistaxis (-), normal nasal septum, normal mucous layer. Ear Normal both of meatus accusticus externus, decreasing hearing ability (-). Neck Jugular venous pressure (5-2) cmH 2O, lymph nodes enlargment (-), thyroid gland enlargement (-), hypertrophy sternocleidomastoideus (-), stiffness (-). Thorax Cor : ictus cordis was not seen : ictus cordis was not palpable : Normal shape, spider naevy (-)
Inspection Palpation
Percussion
: upper heart margin at 2nd intercostal space, right margin at linea sternalis, left margin at LMC sinistra Auscultation : HR 108x/menit, murmur (-), gallop (-) Pulmo Anterior Inspection : static: both hemithoraxs were symmetric, spider naevy (-). dynamic: same movement, no retraction Palpation : stemfremitus in both hemithoraxs were equal Percussion : sonorous in both of lungs, border of pulmo-liver at ICS V Auscultation : vesiculair (+) normal in both of lungs, rales (-), wheezing (-). Pulmo Posterior Inspection : static: symmetric and dynamic: same movement, no retraction Palpation : stemfremitus in both hemithoraxs were equal Percussion : sonorous in both of lungs Auscultation : vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection : dome shaped, umbilicus flattened, collateral vein (+) Palpation : tender, pressure pain(-), liver and spleen can not be examined. Percussion : stony dull, fluid wave test (+) Auscultation : normal bowel sound Genital : Vulva edema (-) Extremities :. Upper extremity Paint on joint (-), pale on finger (-), erythema of palm (+), pitting edema (-/-). Lower extremity Pain on joint (-), varices (-), pale on sole of foot (-), pretibial edema (+/+).
BSS Total cholesterol HDL-cholesterol LDL-cholesterol Triglyceride Uric acid Ureum Creatinine Total protein Albumine Globulin Total bilirubin Direct bilirubin Indirect bilirubin SGOT SGPT Natrium Kalium Urine analysis Epitel Leukocite Erythrocite Protein Glucose
: 161 mg/dl : 170 mg/dl : 55 mg/dl : 110 mg/dl : 125 mg/dl : 5,4 mg/dl : 30 mg/dl : 1,3 mg/dl : 6,7 g/dl : 2,1 g/dl : 4,6 g/dl : 0,78 mg/dl : 0,19 : 0,49 : 32 U/l : 20 U/l : 137 mmol/L : 4,8 mmol/L : positive : 2-3/ HPF : 0-1/ HPF : negative : negative
(<200 mg/dl) (>55 mg/dl) (<130 mg dl) (<150 mg/dl) (F: 2,6-6,0 mg/dl) (15-39 mg/dl) (0,9-1,3 mg/dl) (6,0-7,8 mg/dl) (3,5-5 g/dl) (0,1-1,0 mg/dl) (<0,25 mg/dl) (<0,75 mg/dl) (<40 U/l) (<41 U/l) (135-150 mmol/L) (3,5-5 mmol/L) (0-5/HPF) (0-1/HPF)
II.4. SUPPORTIVE EXAMINATION LABORATORY FINDING Haematology (October, 9th, 2009) Haemoglobin : 8,6 g/dl (12-16 g/dl) Haematocrite : 26% (40-48 vol%) Leucocyte : 5900/mm3 (5000-10.000/mm3) ESR : 70 mm/h (<15 mm/h) Thrombocytes : 175.000/mm3 (200.000-500.000/mm3) Diff Count: Basofil : 0% (0-1%) Eosinofil Band : 0% (2-6%) Segment Limphocytes : 30% (20-40%) Monocytes Clinical Chemistry
: 0% (1-3%) : 67% (50-70%) : 3% (2-8%)
II.5 RESUME A sixty years old woman admitted to hospital on October 9th, 2009 with chief complaint bulging of the abdomen that became even larger since two weeks before admission. 2 months before admission, the patient complained about bulging of her abdomen, her bulging abdomen seemed to spread evenly so she found some difficulty in wearing her outfits. The patient felt uncomfort, heavy, and full of stomach that caused the decrease in her appetite, there was no constant pain on her abdomen. There was no nausea, vomiting, or fever. Her body became weak. In addition, both of her legs were swollen too, but she neither had the swelling eyelids especially when she woke up in the morning nor itching on her skin. Because of her bulging abdomen, she sometimes felt shortness of her breath (dyspnea). Her dyspnea were not caused by her activities, emotional conditions, weathers, and never produced ngik sound. She still can sleep with one pillow, she never woke up in the middle of her night-time sleep because of short winded. She said sometimes she may had dark yellow or brown colored urine, but never passed black or bloody stools. Theres no others complaint in defecation and urination habits. She went to the local health care center and took some medicines (she didnt know name of drugs) but there was no improvement. 2 weeks before admission because of her abdomen seemed even more larger and tense, she had nausea and vomits, three times, containing all foods and fluids that she had
been consumed that day. There was no blood in her vomit and no dark/bloody stools. Then, she was hospitalized in Moh. Hoesin Hospital in order to receive some better treatments. From physical examination we found: moderate sickness condition, vital sign within normal limit, nutrition state (in normal condition): IMT= 19,53 kgs/m2 (normoweight). There were pale of conjungtiva palpebrae (+), palmar erythema (+), icteric sclera (+), spider naevy (-), collateral vein (+), ascites (+). Laboratory findings show anemia (Hb: 8,6 g/dl), trombocitopenia (175.000/mm3), hypoalbuminenia (2,1 g/dl), decreasing in total bilirubin (direct and indirect; 0,78 mg/dl), HDL level (55mg/dl), and increasing of ESR 70mm/h, SGOT 32 U/L and SGPT 20 U/L. II.6 WORKING DIAGNOSIS Decompensated cirrhosis hepatis + anemia ec chronic disease+ hypertension stage II II.7 DIFFERENTIAL DIAGNOSIS Decompensated cirrhosis hepatis + anemia ec Fe deficiency.+ hypertension stage II II.8 TREATMENT Non-pharmacology: Bed rest Liver diet IIII (2000 calories, proteins 1 g/kgs body weight, low sodium diet) Pharmacology: IVFD RL gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x0,25 Ceftriaxon 1x1 gram II. 9 PLANNING EXAMINATION Abdominal USG Diagnostic paracentesis Liver biopsy Planning giving Human albumin 20% II.10 PROGNOSIS Quo ad vitam Quo and functionam : dubia ad malam : dubia ad malam FOLLOW UP October, 10th 2009 S O Bulging of abdomen General condition Conciousness : compos mentis Blood preassure : 140/80 mmHg Pulse rate : 80x/minute Respiration rate : 20x/minute Temperature : 36,5C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+), exopthalmus (-) Jugular venous pressure (5-2) cmH2O, lymph nodes enlargement (-), thyroid gland enlargement (-). Cor Inspection Palpation Percussion : ictus cordis was not seen : ictus cordis was not palpable : upper heart margin at 2nd intercostal space, right margin at linea sternalis dextra , left margin at linea midclavicularis sinistra Auscultation : HR 80 x/menit, murmur (-), gallop (-) Pulmo Inspection : static: both hemithoraxs were symmetric. dynamic: same movement, no retraction Palpation : stemfremitus in both hemithoraxs were equal Percussion : sonorous in both lungs, border of pulmo-liver at ICS V Auscultation : vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+
pretibial edema +/+ Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II DD/ Decompensated hepatic cirrhosis + anemia ec Fe deficiency + hypertension stage II Bed rest Liver diet III IVFD RL gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Nifedipine 4x1 Clonidine 3x0,25 Ceftriaxon 1x1 gram A
Extremities : eritema palmar +/+ pretibial edema +/+ Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II DD/ Decompensated hepatic cirrhosis + anemia ec Fe deficiency + hypertension stage II Bed rest Liver diet III IVFD RL gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x0,25 Ceftriaxon 1x1 gram
October, 12th 2009 S Bulging of abdomen, coughing General condition O Conciousness : compos mentis Blood preassure : 140/70 mmHg Pulse rate : 84x/minute Respiration rate : 20x/minute Temperature : 36,6C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+), Jugular venous pressure (5-2) cmH2O Cor: HR 84 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound
October, 13th 2009 S Dyspnea, no defecation for the last 4 days General condition O Conciousness : compos mentis Blood preassure : 140/70 mmHg Pulse rate : 84x/minute Respiration rate : 18x/minute Temperature : 36,1C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+), Jugular venous pressure (5-2) cmH2O Cor: HR 84 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound
Extremities : eritema palmar +/+ pretibial edema +/+ Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II DD/ Decompensated hepatic cirrhosis + anemia ec Fe deficiency + hypertension stage II Bed rest O2 3-5 l/minute Liver diet III IVFD RL gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x1 Ceftriaxon 1x1 gram Dulcolax sup ( night )
spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II DD/ Decompensated hepatic cirrhosis + anemia ec Fe deficiency + hypertension stage II Bed rest O2 3-5 l/minute Liver diet III IVFD RL gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x1 Ceftriaxon 1x1 gram Dulcolax sup ( night ) Laxadine 3x1c Planning : Check haematology and clinical chemistry Abdominal USG
October, 14th 2009 S O Dyspnea, BAB (-) General condition Conciousness : compos mentis Blood preassure : 180/90 mmHg Pulse rate : 82x/minute Respiration rate : 20x/minute Temperature : 36,4C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+). Jugular venous pressure (5-2) cmH2O Cor: HR 82x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and
October, 15st 2009 S General condition O Conciousness : compos mentis Blood preassure : 170/90 mmHg Pulse rate : 82x/minute Respiration rate : 20x/minute Temperature : 36C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+). Jugular venous pressure (5-2) cmH2O
Cor : HR 82 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation
Globulin SGOT SGPT TIBC Fe
: : : : :
3,4 g/dl 24 U/l 13 U/l 200 g/dl 31 g/dl
(<40 U/l) (<41 U/l) (274-385 g/dl) (32-145 g/dl)
: dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver/ spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ Laboratory finding: Haematology Haemoglobin Haematocrite Erythrocyte MCH MCV MCHC Leucocyte ESR Thrombocytes Reticulocyte Diff Count: Basofil Eosinofil Band Segment Limphocytes Monocytes Clinical Chemistry Total cholesterol HDL-cholesterol LDL-cholesterol Triglyceride Total protein Albumin
Abdominal USG: Liver: shape and size shrunken, regular border, blunt edge, coarse parenchyma Spleen: normal shape, size slightly enlarge, ascites (+) Impression: hepatic cirrhosis with portal hypertension. A Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II Bed rest Liver diet III IVFD D5% gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x1 Ceftriaxon 1x1 gram
: : : : : : : : : : : : : : :
7,2 g/dl 21% 2.420.000/mm3 29 picogram 78 gram 30% 4.800/mm3 88 mm/h 125.000/mm3 : 0,4% 0% 3% 2% 53% 38% 4% (0-1%) (1-3%) (2-6%) (50-70%) (20-40%) (2-8%)
(14-18, 12-16 g/dl) (40-48 vol%) (2.500.000-4.500.000/mm3) (27-31 picogram) (82-92 gram) (32-36%) (5000-10.000/mm3) (<15 mm/h) (200.000-500.000/mm3) (0,5-1,5%)
Planning : Human albumin 20% 50cc / day diagnostic Paracentesis ascites liquid
: 151 mg/dl (<200 mg/dl) : 14 mg/dl (>55 mg/dl) : 102 mgdl (<130 mg/dl) : 175 mg/dl (<150 mg/dl) : 4,8 g/dl (6,0-7,8 g/dl) : 1,4 g/dl (3,5-5 g/dl)
October, 16th 2009 S Headache O General condition Conciousness : compos mentis Blood preassure : 150/90 mmHg Pulse rate : 80x/minute Respiration rate : 20x/minute Temperature : 36,5C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+). Jugular venous pressure (5-2) cmH2O
Cor: HR 80 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ parasintesis ascites liquid 1800 cc A Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II Bed rest Liver diet III IVFD RL gtt X/m (micro) Furosemid 1x40mg Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x1 Ceftriaxon 1x1 gram Albumin 20% 50 cc day 1 A
Pale of conjunctiva palpebra (+), icteric sclera (+), Jugular venous pressure (5-2) Cor: HR 84 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II Bed rest Liver diet III IVFD RL gtt X/m (micro) Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x1 Albumin 20% 50 cc day 2
October, 17th 2009 S General condition O Conciousness : compos mentis Blood preassure : 140/80 mmHg Pulse rate : 84x/minute Respiration rate : 20x/minute Temperature : 36,6C Spesific condition
October, 19th 2009 S Dyspnea, coughing General condition O Conciousness : compos mentis Blood preassure : 190/90 mmHg Pulse rate : 86x/minute Respiration rate : 24x/minute Temperature : 36,5C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+), Jugular venous pressure (5-2) cmH2O
Cor: HR 86 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ A Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II Bed rest O2 3-5 l/minute Liver diet III IVFD RL gtt X/m (micro) Spironolacton 2x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonodine 3x1 Nifedipine 4x1 A
Pale of conjunctiva palpebra (+), icteric sclera (+), Jugular venous pressure (5-2) cmH2O Cor: HR 80 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II Bed rest O2 3-5 l/minute Liver diet III IVFD D5% gtt X/m (micro) Furosemide 2x40 mg Spironolacton 3x100mg Vit Bcomplex 3x1tab Curcuma 3x1tab Clonidine 3x0,25
October, 20th 2009 S Epigastic pain, dyspnea, coughing General condition O Conciousness : compos mentis Blood preassure : 140/60 mmHg Pulse rate : 80x/minute Respiration rate : 20x/minute Temperature : 37,1C
Spesific condition
October, 21st 2009 S dyspnea General condition O Conciousness : compos mentis Blood preassure : 130/80 mmHg Pulse rate : 76x/minute Respiration rate : 22x/minute Temperature : 37,1C Spesific condition Pale of conjunctiva palpebra (+), icteric sclera (+), Jugular venous pressure (5-2) cmH2O
Cor: HR 84 x/menit, murmur (-), gallop (-) Pulmo: vesiculair (+) normal, rales (-), wheezing (-) Abdomen Inspection Palpation : dome-shaped, collateral vein (+) : tender, borderline of pulmo-liver at ICS V, pressure pain (-), liver and spleen couldnt be examined. Percussion : stony-dull, fluid wave test (+) Auscultation : normal bowel sound Extremities : eritema palmar +/+ pretibial edema +/+ A Decompensated hepatic cirrhosis + anemia ec chronic disease + hypertension stage II Bed rest O2 3-5 l/minute Liver diet III IVFD D5% gtt X/m (micro) Furosemide 2x40 mg Spironolacton 3x100mg Vit Bcomplex 3x1tab Ceftriaxon 1x1 gram Curcuma 3x1tab Clonidine 3x0,25
Because of her bulging abdomen, she sometimes felt shortness of her breath (dyspnea). Her dyspnea were not caused by her activities, emotional conditions, weathers, and never produced ngik sound. She still can sleep with one pillow, she never woke up in the middle of her night-time sleep because of short winded. She said sometimes she may had dark yellow or brown colored urine, but never passed black or bloody stools. Theres no others complaint in defecation and urination habits. She went to the local health care center and took some medicines (she didnt know name of drugs) but there was no improvement. 2 weeks before admission because of her abdomen seemed even more larger and tense, she had nausea and vomits, three times, containing all foods and fluids that she had been consumed that day. There was no blood in her vomit and no dark/bloody stools. Then, she was hospitalized in Moh. Hoesin Hospital in order to receive some better treatments. From physical examination we found: moderate sickness condition, vital sign within normal limit, nutrition state (in normal condition): IMT= 19,53 kgs/m2 (normoweight). There were pale of conjungtiva palpebrae (+), palmar erythema (+), icteric sclera (+), collateral vein (+), ascites (+).. The bulging of the abdomen in this patient was more specifically due to fluid accumulation in the peritoneal cavity. Because from physical examination we could see the bulging seemed to spread evenly in all region of the abdomen (frogs belly), tender in palpation, and had stony-dull sound. There was no palpable mass or tense and defans muscular in abdominal wall which is usually because of perforation/ peritonitis . The ascites because of kidneys diseases was stepped aside because there were no symptoms and signs being found. The patient were not experienced palpebrae edema when she woke up in the morning, nausea or vomit, itchs on skin, or any changed in urination habits (lessen in urines volume or frequency). On the other hands, fluid accumulation in patient with cardiovascular disorder usually observed at patients feet and ankle. The dyspnea is more severe, influenced by activities and better if patient take some rest (dyspnea on effort), orthopnea, paroxysmal nocturnal dyspnea can occur. So ascites in this case is more specific due to pathologic process in liver which is cirrhosis hepatic. Cirrhosis may cause no symptoms for long periods. The onset of symptoms may be insidious or, less often, abrupt. From anamnesis we knew that patient complain about felt weakness of her body, losing appetite, nausea, vomit (non-specific symptoms of compensated cirrhosis) and she had dark-yellow or brown coloured urine. In advanced cirrhosis, anorexia is usually present and may be extreme, with associated nausea and occasional vomiting. Abdominal pain may be present and is related either to hepatic enlargement and stretching of Glisson's capsule or to the presence of ascites.5 Physical examination, laboratory findings, and abdominal USG are very important in diagnosing cirrhosis hepatic.4 The stigmata of cirrhosis hepatic including erythema of palm, collateral vein, ascites, splenomegaly, icterus, and hypoalbuminemia are fulfilled in this patient. The single best test for diagnosing cirrhosis is biopsy of the liver. Liver biopsies, however, carry a small risk for serious complications, and, therefore, biopsy often is reserved for those patients in whom the diagnosis of the type of liver disease or the presence of cirrhosis is not clear.
CHAPTER III CASE ANALYSIS A sixty years old woman admitted to hospital on October 9th, 2009 with chief complaint bulging of the abdomen that became even larger since two weeks before admission. 2 months before admission, the patient complained about bulging of her abdomen, her bulging abdomen seemed to spread evenly so she found some difficulty in wearing her outfits. The patient felt uncomfort, heavy, and full of stomach that caused the decrease in her appetite, there was no constant pain on her abdomen. There was no nausea, vomiting, or fever. Her body became weak. In addition, both of her legs were swollen too, but she neither had the swelling eyelids especially when she woke up in the morning nor itching on her skin.
10
Laboratory findings show anemia (Hb: 8,6 g/dl), trombocitopenia (175.000/mm3) due to both congestive splenomegaly as well as decreased thrombopoietin from the liver, hypoalbuminenia (2,1 g/dl): advanced cirrhosis leads to a reduced level of albumin in the blood and reduced blood clotting factors due to the loss of the liver's ability to produce these proteins. Bed rest: it is shown to inhibit the neurohomural system (RAAS and SNS) activated chronically in upright position in cirrhotic patients that impairs renal blood perfusion and causes sodium retention. Bed rest reduces the plasma aldosterone level and improves the response to diuretic therapy in cirrhotic patients. However, bed rest is not recommended routinely as it is often unpractical and could cause decubitus ulcers and muscle atrophy in malnourished cirrhotic patients6. Management of patients with cirrhosis and ascites. Generally, reduction of sodium intake is beneficial in patients with ascites. A low-sodium diet (60 to 90 mEq per day, equivalent to approximately 1500 to 2000 mg of salt per day) may facilitate the elimination of ascites and delay the reaccumulation of fluid.7,8 Two different schedules of diuretic treatment are used in cirrhotic patients with ascites. The most conservative schedule stars with spironolactone 100/mg day. If there is no response the dose is increased progressively to 200 mg/day and 400 mg/day. Furosemide is added at increasing doses (40, 80, and 160 mg/day) in patients not responding to 400 mg/day of spironolactone. In this patient we use the second strategy consists in the simultaneous administration of spironolactone and furosemide starting with 100 mg/day and 40 mg/day, respectively. If there is no response the dosages are increased to 200 mg/day and 80 mg/day and to 400 mg/day and 160 mg/day. Respectively there is a general agreement that these are the highest doses of diuretic to be used in cirrhotics. Weight loss should not go over 0.5 kg/day in the absence of edema and more than 1 kg/day in edematous state. 7,8 Clonidine (central agonist beta2 ) is used to decrease blood pressure and usually used to the resistance hypertension. The small dose of clonidine can used to treat hypertension without using a diuretic. All patients with ascites should be evaluated for transplantation, since the presence of ascites is associated with poor long-term survival (survival rate at five years, 30 to 40% vs. 70 to 80% among patients who have undergone transplantation).7 Fluid retention is the most frequent complication of End Stage of Liver Disease which is occurring in about 50% of patients within 10 years of the diagnosis of cirrhosis. It is associated with poor prognosis and 1-year and 5-year survivals of 85% and 56%, respectively.9
11
You might also like
- 01 - Lineberry - Propulsion Fundamentals - 2019Document95 pages01 - Lineberry - Propulsion Fundamentals - 2019Николай СидоренкоNo ratings yet
- MCQ NeuroDocument21 pagesMCQ NeuroMasayu Mutiara UtiNo ratings yet
- The Cygnus MysteryDocument25 pagesThe Cygnus MysteryGraham Harris100% (3)
- P1 - The Particulate Nature of Matter PDFDocument17 pagesP1 - The Particulate Nature of Matter PDFEdgardo LeysaNo ratings yet
- Presentasi Kasus Dokter Arif Cynthia NataliaDocument26 pagesPresentasi Kasus Dokter Arif Cynthia NataliaIntan SorayaNo ratings yet
- AR Kelompok G - ADB+ HemoroidDocument22 pagesAR Kelompok G - ADB+ HemoroidSagung Ari DipratariNo ratings yet
- AR Kelompok G - ADB+ HemoroidDocument22 pagesAR Kelompok G - ADB+ HemoroidChindy SarindraNo ratings yet
- CR Piopneumothoraks Nicky FIXdDocument62 pagesCR Piopneumothoraks Nicky FIXdPutri RahmawatiNo ratings yet
- Sirosis HepatisDocument29 pagesSirosis HepatisXaverius da CunhaNo ratings yet
- Caseeeee Egaaa IrbasssDocument27 pagesCaseeeee Egaaa IrbasssIrbasMantiniSyaifulNo ratings yet
- Revisi - Case Sirosis Hepatis PDLDocument24 pagesRevisi - Case Sirosis Hepatis PDLDebby TamaraNo ratings yet
- Duty Report July, 26 2017: Coass: Nodya Melinda Noori Succi IslamDocument22 pagesDuty Report July, 26 2017: Coass: Nodya Melinda Noori Succi IslamRahadian MalikNo ratings yet
- Systemic Lupus Erithematosus & Marfan's SyndromeDocument74 pagesSystemic Lupus Erithematosus & Marfan's SyndromeFitriYani SimangunsoNgNo ratings yet
- Case Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaDocument39 pagesCase Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaFarella KartikaNo ratings yet
- Case Report: TH NDDocument10 pagesCase Report: TH NDyan hidayatNo ratings yet
- Case TitleDocument5 pagesCase TitleMaulidianaIndahNo ratings yet
- DMDFDocument22 pagesDMDFsujal177402100% (1)
- Presentasi Kasus Gizi Buruk FixDocument78 pagesPresentasi Kasus Gizi Buruk FixZahra AfifahNo ratings yet
- Anamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoDocument25 pagesAnamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoTebeNo ratings yet
- Case ReportDocument22 pagesCase ReportAgus MahendraNo ratings yet
- Lapkas Marasmus JadiDocument48 pagesLapkas Marasmus JadiRivhan FauzanNo ratings yet
- CC 10 NOv 2017 ITPDocument32 pagesCC 10 NOv 2017 ITPLilik NatasubrataNo ratings yet
- Morning Report: Disusun Oleh: Noermawati DewiDocument34 pagesMorning Report: Disusun Oleh: Noermawati DewidevyNo ratings yet
- Duty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemDocument15 pagesDuty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemGiovina FajarNo ratings yet
- Apriyanto Lifandy Desmy FadillahDocument38 pagesApriyanto Lifandy Desmy FadillahdesmyyNo ratings yet
- Case Based Discussion: Pembimbing: Dr. Minidian Fasitasari, M.SC, SP - GKDocument28 pagesCase Based Discussion: Pembimbing: Dr. Minidian Fasitasari, M.SC, SP - GKArieph PatrianaNo ratings yet
- MR GoutyDocument25 pagesMR GoutyArvindan SubramaniamNo ratings yet
- Morning Report: Disusun Oleh: Noermawati DewiDocument38 pagesMorning Report: Disusun Oleh: Noermawati DewidevyNo ratings yet
- Case Report Typhoid Fever (A01.0)Document32 pagesCase Report Typhoid Fever (A01.0)Alvin PratamaNo ratings yet
- Morning Report: Disusun Oleh: Noermawati DewiDocument37 pagesMorning Report: Disusun Oleh: Noermawati DewidevyNo ratings yet
- Morning Report: Disusun Oleh: Devy Puspo WardoyoDocument36 pagesMorning Report: Disusun Oleh: Devy Puspo WardoyodevyNo ratings yet
- MR 10 Mei CMLDocument12 pagesMR 10 Mei CMLWenNy RupiNaNo ratings yet
- Morning Report: Disusun Oleh: Devy Puspo WardoyoDocument43 pagesMorning Report: Disusun Oleh: Devy Puspo WardoyodevyNo ratings yet
- Morning Report Case: Februari 19, 2010Document17 pagesMorning Report Case: Februari 19, 2010Felicia adeline ChristianNo ratings yet
- +CBD ANEMIA, ABDOMINAL PAIN DR Saugi - MuznaDocument36 pages+CBD ANEMIA, ABDOMINAL PAIN DR Saugi - MuznaAlmira PratiwiNo ratings yet
- Peads - Diamond Blackfan AnemiaDocument40 pagesPeads - Diamond Blackfan AnemiaBaran PalanimuthuNo ratings yet
- PR CBD DR LusitoDocument66 pagesPR CBD DR LusitoFebry Hw PratamaNo ratings yet
- AnasarcaDocument54 pagesAnasarcaSulaiman TahsinNo ratings yet
- Morning Report RakaDocument19 pagesMorning Report Rakaraka widhiartaNo ratings yet
- AR 28 April ACKDDocument17 pagesAR 28 April ACKDShaastieNo ratings yet
- Laporan 3-10-2019 Tumor Colorectal (DR Alders, SP.B)Document10 pagesLaporan 3-10-2019 Tumor Colorectal (DR Alders, SP.B)Astrid CarolineNo ratings yet
- A Woman 55 Years Old With: Grade Ii Decubitus Ulcer Glutea Dextra RegionDocument41 pagesA Woman 55 Years Old With: Grade Ii Decubitus Ulcer Glutea Dextra RegionHananiKusumasariNo ratings yet
- Acute PancreatitisDocument9 pagesAcute PancreatitisAlvin Germo PasuquinNo ratings yet
- Final CaseDocument45 pagesFinal Case_carido_No ratings yet
- Lapsus - Asrarudin - BPHDocument18 pagesLapsus - Asrarudin - BPHAsrarudin HamidNo ratings yet
- Fulqy Case ReportDocument7 pagesFulqy Case ReportZulkifli SalimNo ratings yet
- Gastroenteritis With Severe DehydrationDocument11 pagesGastroenteritis With Severe DehydrationdianarahimmNo ratings yet
- Case CHF, Cap, DM Tipe 2 - Dr. Ruddy, SP - PDDocument34 pagesCase CHF, Cap, DM Tipe 2 - Dr. Ruddy, SP - PDMelisaNo ratings yet
- Laporan Kasus: Gout ArthritisDocument55 pagesLaporan Kasus: Gout ArthritisikaNo ratings yet
- Case Report Priska Pramuji and Sugianto MukminDocument17 pagesCase Report Priska Pramuji and Sugianto Mukmingiggs_libraNo ratings yet
- CC 4 Nov 2017 SeizureDocument44 pagesCC 4 Nov 2017 SeizurenisaNo ratings yet
- Case Report Typhoid Fever (A01.0)Document32 pagesCase Report Typhoid Fever (A01.0)Alvin PratamaNo ratings yet
- CR Destroyed LungDocument42 pagesCR Destroyed LungAndre Prasetyo MahesyaNo ratings yet
- Morning Report: Disusun Oleh: Noermawati DewiDocument37 pagesMorning Report: Disusun Oleh: Noermawati DewidevyNo ratings yet
- Nilawati. GEA With Severe Dehydration, Duty HannaDocument19 pagesNilawati. GEA With Severe Dehydration, Duty HannaHanna GustinNo ratings yet
- CC HCU Ped AnemiaDocument42 pagesCC HCU Ped AnemialatifahNo ratings yet
- CholelitiasisDocument42 pagesCholelitiasisEdwin YosuaNo ratings yet
- Protocol - IM DyspneaDocument7 pagesProtocol - IM DyspneaTrisNo ratings yet
- Sri Pertiwi, Syok Sepsis CAPDocument14 pagesSri Pertiwi, Syok Sepsis CAPLukman NurhakimNo ratings yet
- Aboy1 Y.O With Bronchopneumonia, Iron Deficiency, Leukocytosis and Hepatomegaly Suspected Hematological MalignanciesDocument28 pagesAboy1 Y.O With Bronchopneumonia, Iron Deficiency, Leukocytosis and Hepatomegaly Suspected Hematological Malignanciesayu_gultom29No ratings yet
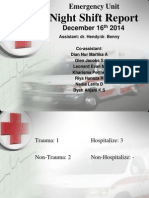
- Night Shift Report: Emergency UnitDocument43 pagesNight Shift Report: Emergency UnitDian Nur Martika AnggrainiNo ratings yet
- Case Report Session (CRS)Document9 pagesCase Report Session (CRS)revininNo ratings yet
- Pleurak EffusionDocument16 pagesPleurak EffusionElfriska SihombingNo ratings yet
- Dafftar Singkatan C-DDocument10 pagesDafftar Singkatan C-DMasayu Mutiara UtiNo ratings yet
- SOTK September 2019Document3 pagesSOTK September 2019Masayu Mutiara UtiNo ratings yet
- Laporan Harian Neuropediatri: Lantai 1Document6 pagesLaporan Harian Neuropediatri: Lantai 1Masayu Mutiara UtiNo ratings yet
- Laporan Harian Neuropediatri: Lantai 1Document7 pagesLaporan Harian Neuropediatri: Lantai 1Masayu Mutiara UtiNo ratings yet
- Laporan Harian Neuropediatri: Lantai 1Document7 pagesLaporan Harian Neuropediatri: Lantai 1Masayu Mutiara UtiNo ratings yet
- 19 Juli 2017 (Hari Rawat Ke-1)Document12 pages19 Juli 2017 (Hari Rawat Ke-1)Masayu Mutiara UtiNo ratings yet
- Daftar Pustaka: Acute Poststreptococcal GlomerulonephritisDocument2 pagesDaftar Pustaka: Acute Poststreptococcal GlomerulonephritisMasayu Mutiara UtiNo ratings yet
- Electro Cardiograph yDocument1 pageElectro Cardiograph yMasayu Mutiara UtiNo ratings yet
- Halaman DepanDocument1 pageHalaman DepanMasayu Mutiara UtiNo ratings yet
- What Is Diabetes MellitusDocument2 pagesWhat Is Diabetes MellitusMasayu Mutiara UtiNo ratings yet
- Pretest and PosttestDocument3 pagesPretest and PosttestMarissa FontanilNo ratings yet
- Bhel Training ReportDocument32 pagesBhel Training ReportVivek PrasadNo ratings yet
- AtropineDocument4 pagesAtropineAnung RespatiNo ratings yet
- Rohit Data Analyst Professional SummaryDocument10 pagesRohit Data Analyst Professional SummaryKritika ShuklaNo ratings yet
- Bloques de Distribución de PotenciaDocument6 pagesBloques de Distribución de PotenciaRaul HernandezNo ratings yet
- By Group 7: Maintenance of CNC MachinesDocument27 pagesBy Group 7: Maintenance of CNC MachinesFerdian Gamalea DelastaNo ratings yet
- Infections PDFDocument29 pagesInfections PDFLoudry ElfaNo ratings yet
- Pidato Bahasa InggrisDocument3 pagesPidato Bahasa InggrisMarta SaputraNo ratings yet
- MAN-10150-05 GeoMx DSP Manual Slide Prep User ManualDocument69 pagesMAN-10150-05 GeoMx DSP Manual Slide Prep User ManualNati Martin MoralesNo ratings yet
- Gabisan Let Scheck1 PDFDocument3 pagesGabisan Let Scheck1 PDFEdrick Paras100% (1)
- Doc-20240210-Wa0005 240508 203425Document110 pagesDoc-20240210-Wa0005 240508 203425cristina silvaNo ratings yet
- Poster PresentationDocument1 pagePoster PresentationPilla SatishNo ratings yet
- The Dangers of CrammingDocument2 pagesThe Dangers of CrammingIntan Shafira RachmadhiniNo ratings yet
- North American Rated Devices: Pin & SleeveDocument3 pagesNorth American Rated Devices: Pin & Sleevesmsm280No ratings yet
- PPT01-Introduction To Big DataDocument34 pagesPPT01-Introduction To Big DataTsabitAlaykRidhollahNo ratings yet
- ProcartaPlex Human Combinable Simplex UGDocument24 pagesProcartaPlex Human Combinable Simplex UGMonika MittalNo ratings yet
- Concept Note - C Financing MechanismsDocument17 pagesConcept Note - C Financing Mechanismst.ahmadzadeNo ratings yet
- Summary ReportDocument24 pagesSummary ReportRonniNo ratings yet
- MG500 Service Training PDFDocument22 pagesMG500 Service Training PDFJav SeNo ratings yet
- Ruby Village TemplateDocument2 pagesRuby Village Templatekomal sharmaNo ratings yet
- Report FormatDocument3 pagesReport FormatAditya BorborahNo ratings yet
- Funnel Bulk SMS-GVNDocument6 pagesFunnel Bulk SMS-GVNJamie JordanNo ratings yet
- Acustica Ruby EbonyDocument1 pageAcustica Ruby EbonyZizja TurtleNo ratings yet
- 03 Vision 2020 The Right To SightDocument9 pages03 Vision 2020 The Right To SightMwanja MosesNo ratings yet
- G7 1Q SETS Activity-WorksheetDocument2 pagesG7 1Q SETS Activity-WorksheetluiNo ratings yet
- Eleven Rack User GuideDocument130 pagesEleven Rack User GuideGeocasta AbaddonNo ratings yet
- Glossary CambridgeDocument14 pagesGlossary CambridgeAlexey PetrovNo ratings yet