Professional Documents
Culture Documents
Interaction Study Between Digoxin and A Preparation of Hawthorn (Crataegus Oxyacantha)
Interaction Study Between Digoxin and A Preparation of Hawthorn (Crataegus Oxyacantha)
Uploaded by
veeramaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Interaction Study Between Digoxin and A Preparation of Hawthorn (Crataegus Oxyacantha)
Interaction Study Between Digoxin and A Preparation of Hawthorn (Crataegus Oxyacantha)
Uploaded by
veeramaniCopyright:
Available Formats
HERBAL MEDICINE
ARTICLE
TANKANOW 10.1177/0091270003253417 DIGOXIN HERBAL MEDICINE AND ET HAWTHORN AL
Interaction Study between Digoxin and a Preparation of Hawthorn (Crataegus oxyacantha)
Roberta Tankanow, MS, Helen R. Tamer, PharmD, Daniel S. Streetman, PharmD, Scott G. Smith, Janice L. Welton, Thomas Annesley, PhD, Keith D. Aaronson, MD, and Barry E. Bleske, PharmD, FCCP
Hawthorn, an herbal supplement, is currently being evaluated for the treatment of heart failure. The flavonoid components of hawthorn may be responsible for hawthorns beneficial effects in the treatment of heart failure. However, these components may also affect P-glycoprotein function and cause interactions with drugs that are P-glycoprotein substrates, such as digoxin, which is also used to treat heart failure. Therefore, the purpose of this study was to determine the effect of hawthorn on digoxin pharmacokinetic parameters. A randomized, crossover trial with 8 healthy volunteers was performed evaluating digoxin 0.25 mg alone (D) for 10 days and digoxin 0.25 mg with Crataegus special extract WS 1442 (hawthorn leaves with flowers; Dr. Willmar Schwabe Pharmaceuticals) 450 mg twice daily (D + H) for 21 days. Pharmacokinetic studies were performed for 72 hours. There
were no statistically significant differences in any measured pharmacokinetic parameters. The AUC0-, Cmax-Cmin, Cmin, and renal clearance for the D group were 79 26 mcgh/L, 1.4 0.7 mcg/L, 0.84 0.2 mcg/L, and 74 10 mL/min versus 73 20 mcgh/L, 1.1 0.1 mcg/L, 0.65 0.2 mcg/L, and 81 22 mL/min for the D + H group, respectively (p > 0.05). Following 3 weeks of concomitant therapy, hawthorn did not significantly alter the pharmacokinetic parameters for digoxin. This suggests that both hawthorn and digoxin, in the doses and dosage form studied, may be coadministered safely. Keywords: Hawthorn; digoxin; pharmacokinetics; heart failure Journal of Clinical Pharmacology, 2003;43:637-642 2003 the American College of Clinical Pharmacology
rataegus oxyacantha, an extract of the herbal supplement hawthorn, has been used to treat a number of cardiovascular ailments, including heart failure, angina pectoris, and hypertension. Studies have shown that Crataegus extract may have positive inotropic, vasodilatory, and antioxidative properties.1-3 This compound also improves endothelial function.4,5 Based in part on these effects, Crataegus extract (hawFrom the University of Michigan College of Pharmacy and University of Michigan Health Systems, Ann Arbor, Michigan (Ms. Tankanow, Dr. Tamer, Dr. Streetman, Mr. Smith, Ms. Welton, Dr. Bleske) and the Department of Pathology (Dr. Annesley) and Department of Internal Medicine (Dr. Aaronson), University of Michigan Health Systems, Ann Arbor, Michigan. Supported in part by University of Michigan Health Systems Clinical Research Resource Committee and by General Clinical Research Center Grant No. M01-RR00042. Submitted for publication September 26, 2002; revised version accepted February 22, 2003. Address for reprints: Barry E. Bleske, PharmD, University of Michigan, College of Pharmacy, 428 Church Street, Ann Arbor, MI 48109-1065. DOI: 10.1177/0091270003253417
thorn) is currently being studied for the treatment of heart failure in a large mortality trial.6 Hawthorn is made up of a number of compounds, including flavonoids, which may be responsible for hawthorns cardiovascular effects.6 In addition, recent studies evaluating other natural compounds that contain flavonoids as well as flavonoids themselves have demonstrated alterations in P-glycoprotein activity.7-11 This may have important consequences in regard to drugs that are P-glycoprotein substrates. Since Pglycoprotein is found in high amounts in both the gut and kidney and is an efflux transporter, change in activity can lead to alterations in the absorption and clearance of drugs that are P-glycoprotein substrates. One drug that is a P-glycoprotein substrate is digoxin. Digoxin is indicated for the treatment of symptomatic heart failure due to systolic dysfunction.12 If hawthorn is shown to be beneficial in the treatment of heart failure, it is likely that it will be coadministered with digoxin. A hawthorn-digoxin interaction is
J Clin Pharmacol 2003;43:637-642
637
TANKANOW ET AL
widely noted in the herbal medicine literature, but neither case reports nor pharmacokinetic/ pharmacodynamic data have been reported. Since hawthorn may theoretically alter P-glycoprotein activity due to its flavonoid components, it therefore may also affect digoxin pharmacokinetic parameters. The purpose of this study was to determine if hawthorn, when coadministered with digoxin, would alter digoxin pharmacokinetic parameters. The findings from this study may have important implications regarding treatment of heart failure with hawthorn. METHODS A total of 8 healthy subjects completed an open-label, randomized crossover trial evaluating the effect of hawthorn on the pharmacokinetic parameters of digoxin. After approval from the human subject institutional review board and before study entry, informed consent was obtained from each subject. Inclusion criteria included the following: age > 18 years, serum creatinine < 1.2 mg/dL, and bilirubin < 1.5 mg/dL. Individuals taking concurrent scheduled medications (excluding oral contraceptives), those with significant medical histories, and smokers and pregnant females were excluded from the study. Subjects were also prohibited from taking vitamins, dietary supplementation, or herbal supplements during the study period. Grapefruit juice, grape juice, and red and white wine were also prohibited throughout the study period. Subjects were admitted as outpatients to the General Clinical Research Center, and after physical examination and baseline laboratory measurements were obtained, patients were randomized into one of two groups: digoxin 0.25 mg daily for a 10-day period (D) or digoxin 0.25 mg daily and Crataegus special extract WS 1442 twice daily (one tablet contained 450 mg dry extract of hawthorn leaves with flowers standardized to 84.3 mg of oligomeric procyanidines; Dr. Willmar Schwabe Pharmaceuticals, Karlsruhe, Germany) for a 21-day period (D + H). A 21-day period was employed for the D + H treatment group to allow for steady-state concentrations for both digoxin and hawthorn. Only a 10-day period was used for the D group since steadystate levels would be achieved by this time and would therefore decrease the exposure of healthy volunteers to digoxin. After each treatment period, there was a 21day washout period, and subjects were then crossed over to the opposite treatment. Compliance was determined by measuring digoxin trough levels after 5 days (also used as a safety measurement) and comparison
with trough digoxin levels on pharmacokinetic sampling days and by medication vial inspection. Digoxin was administered at 0900 h and hawthorn at 0900 h and 2100 h. Pharmacokinetic data were collected during 12hour clinic stays starting on digoxin-only day 10 and on digoxin + hawthorn day 21. Blood samples (7 mL, no anticoagulant) were drawn from each subject immediately before administration of digoxin and/or hawthorn (time 0) and then at 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, and 12 hours after administration of the medications; subjects were fitted with hep-lock catheters to facilitate the repeated blood draws. Catheters were removed after the 12-hour blood draw. Subjects were required to return to the clinic for blood draws at 24, 48, and 72 hours after the initial blood draw. Urine was also collected for a 24-hour time period, beginning at the baseline blood draw for determination of digoxin renal clearance. All patients were asked to void prior to the start of the collection period. For the D + H group, hawthorn administration continued throughout the 72-hour data collection period. Pharmacodynamic measurements included blood pressure (three measurements, 5 min apart, in seated position by automated blood pressure machine; Alaris Medical Systems IVAC Vitacheck Model 4415) and a standard 12-lead electrocardiogram (for heart rate and PR interval measurements), which was obtained prior to and after each treatment phase. All patients were required to be in a seated position for at least 15 minutes prior to pharmacodynamic assessment. Subjects were questioned about side effects or adverse reactions between days 5 and 7 in the D phase and between days 8 and 10 in the D + H phase. Digoxin Analysis Serum and urine samples were assayed for digoxin using the kinetic interaction of microparticles in solution (KIMS) immunoassay technique on a Roche Integra analyzer. The assay has a validated test range of 0.2 to 0.5 ng/mL. Any samples with an initial concentration above 5.0 ng/mL were diluted with a zero calibrator and reanalyzed. The interassay coefficients of variation were 9.6% at 0.85 ng/mL and 3.6% at 3.45 ng/mL. To determine if hawthorn interfered with the digoxin assay, 2 subjects were administered 450 mg of hawthorn twice a day for 7 days. After 7 days, blood samples were obtained and measured for digoxin concentrations. Both samples demonstrated serum digoxin concentrations below the detectable range of the assay (< 0.2 ng/ mL).
638 J Clin Pharmacol 2003;43:637-642
DIGOXIN AND HAWTHORN
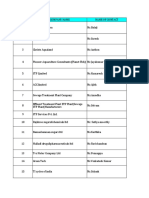
Data Analysis Pharmacokinetic parameters were determined by noncompartmental methods and inspection of the data, when appropriate. Specifically, the area under the serum concentration-time curve (AUC) to 24 hours (AUC0-24) and to the last measured time point (AUC0-72) was determined by the linear trapezoidal method with extrapolation to infinity (AUC0-). The elimination halflife (t1/2) was determined by linear regression analysis of the terminal phase of the log concentration-time profile. The minimal serum concentrations (Cmin), maximal serum concentration (Cmax), and time to Cmax (tmax) were determined by inspection of the available data points. Renal clearance (CLR) was calculated as the total amount of unchanged drug excreted into the urine (Ae) over 24 hours divided by the AUC0-24. Statistical comparison between the two phases was performed by a paired t-test. A p 0.05 was considered the critical probability level. The reported data are represented as the mean and standard deviation. RESULTS There were 11 subjects screened with a total of 8 patients completing the study, 4 male and 4 female. The subjects ranged in age from 19 to 43 years old (mean = 28 6) with a mean weight of 69 13 kg. One subject did not complete the study due to palpitations that were thought to be secondary to digoxin, and 1 patient was not able to complete the study due to a family emergency. One volunteer withdrew from the study for personal reasons before beginning the protocol. In regard to compliance, inspection of subject medication vials indicated that no doses were missed. In addition, there was no difference in digoxin trough concentrations at the mid-phase safety check and at the start of pharmacokinetic sampling (0.69 0.4 mcg/L vs. 0.84 0.2 mcg/L for the D group and 0.63 0.1 vs. 0.65 0.2 mcg/L for the D + H group, p > 0.05, respectively). Mean pharmacokinetic parameters for serum concentrations of digoxin are shown in Table I, and the mean serum concentration-time profiles are displayed in Figure 1. Overall, digoxin concentrations are slightly lower in the D + H group. However, there were no statistical differences between the two groups. For Cmin, the difference approached significance (p = 0.054), with 6 of 8 patients in the D + H group having lower concentrations as compared to the D group. Overall, there were no significant differences in the pharmacodynamic parameters measured from baseline values for either group. The baseline PR interval for the
Table I Pharmacokinetic Parameters
Parameter D D+H % Change
AUC0-24 (ngh/mL) AUC0-72 (ngh/mL) AUC0- (ngh/mL) Cmax (ng/mL) Cmin (ng/mL) Cmax-Cmin (ng/mL) tmax (h) t1/2 (h) CLR (mL/min)
23 4 49 9 79 26 2.1 0.6 0.84 0.2 1.4 0.7 1.3 0.5 50 15 74 10
22 4 46 11 73 20 1.8 0.2 0.65 0.2 1.1 0.1 1.0 0.5 48 6 81 22
6 7 8 14 23 17 23 4 +9
Results expressed as mean standard deviation. D, digoxin-alone group; D + H, digoxin and hawthorn group; AUC, area under the concentration-time curve; Cmax, maximum concentration; Cmin, minimum concentration; tmax, time to maximum concentration; t1/2, half-life; CLR, renal clearance.
Figure 1. Mean serum concentration-time curve for digoxin. D, digoxin alone; D + H, digoxin + hawthorn.
D and D + H phases was 149 20 msec and 150 16 msec (p > 0.05), respectively. Following each phase, the PR interval increased to 156 24 msec and 152 14 msec for D and D + H, respectively. The mean change in PR interval for D and D + H was 6.5 11 msec versus 1.0 13 msec (p > 0.05), respectively. Baseline heart rate (HR) during the D and D + H phases was 65 6 beats/min and 64 6 beats/min (p > 0.05), respectively. Following each phase, the HR was 62 4 and 65 7 for D and D + H, respectively. The mean change in HR for D and D + H was 2.5 8 beats/min and 1 6 beats/min (p > 0.05), respectively. The hawthorn and digoxin were well tolerated. In the digoxin-only group, 1 patient noted nausea, which
HERBAL MEDICINE
639
TANKANOW ET AL
lasted for 1 to 2 days, and in the D + H group, 2 patients complained of mild nausea, which resolved in 1 day. In the combination group, 1 subject complained of flatulence and insomnia, and 1 subject complained of headache and dizziness. These effects were mild and resolved in a day. DISCUSSION This study demonstrated no statistically significant difference in digoxin pharmacokinetic or pharmacodynamic parameters when coadministered with hawthorn over a 3-week time period. These findings are in contrast with those that have demonstrated significant reductions in digoxin AUC, Cmax, and Cmin when digoxin was given together with St. Johns wort, a compound containing many of the same constituents as hawthorn.7 These differences were at least partly attributed to induction of the P-glycoprotein transporter.7 In particular, both are rich in various flavonols, including rutin, quercetin, isoquercitrin, and hyperoside, all of which are present in both products.13-15 These similarities are of significance as prior publications have suggested that compounds such as rutin, quercetin, and hyperoside may be capable of altering the activity of various drug-metabolizing enzymes.16 Even more significant in relation to effects on digoxin is the mounting evidence that quercetin, present in both St. Johns wort and hawthorn, is capable of altering Pglycoprotein-mediated drug transport.10,11,17 It could also be hypothesized that rutin and isoquercitrin, both quercetin glycosides, have similar abilities to alter Pglycoprotein activity. Erlund et al18 demonstrated that quercetin was present in plasma following oral administration of both quercetin aglycone and rutin and that both quercetin and rutin are mainly present in the plasma as quercetin glucuronides and/or sulfates. Despite the similarities between hawthorn and St. Johns wort, important differences in their constituents may contribute to their disparate effects on digoxin pharmacokinetics. In addition to its flavonol content, hawthorn contains numerous other compounds, including chlorogenic acid, epicatechin, ursolic acid, and proticatecholic acid, none of which have been shown to alter drug metabolism or transport. Conversely, some additional compounds in St. Johns wort include hyperforin, adhyperforin, and hypericin. Perloff et al19 have shown that hypericin strongly induces P-glycoprotein in vitro and may be the principle component responsible for the P-glycoprotein induction observed with St. Johns wort in vivo. Thus, it is likely that these differences explain why hawthorn did
not alter digoxin pharmacokinetics to a similar extent as previous studies of St. Johns wort. These findings have important implications not only for the concomitant use of digoxin and hawthorn but also for the likely impact of hawthorn on other Pglycoprotein substrates. Digoxin is well recognized as a P-glycoprotein substrate20 and is only minimally metabolized in humans.21 As a result, digoxin has been widely used as a model P-glycoprotein substrate. The relatively weak effects of hawthorn on digoxin observed herein suggest that, at similar doses, hawthorn is unlikely to alter the P-glycoprotein-mediated transport of other compounds. The lack of a pharmacokinetic interaction between hawthorn and digoxin does not, however, rule out a pharmacodynamic interaction, which is particularly concerning given their potential for use in similar patient populations. As a result, we evaluated ECG, heart rate, and blood pressure parameters and found no evidence of any such interaction. However, there is still a distinct possibility that hawthorn may increase digoxins effect on contractility. As more is learned about the mechanism(s) by which hawthorn works in heart failure, it is becoming increasingly clear that it is unique from that of digoxin. Although, like digoxin, there is some evidence of positive inotropic effects associated with hawthorn, hawthorn is associated with a slight increase in heart rate, opposite of what would be expected with digoxin.2 Furthermore, one of the main effects of hawthorn seems to be its ability to produce endothelium-dependent vasodilation, an effect not seen with digoxin.2,5,22 In the interpretation of both the pharmacokinetic and the pharmacodynamic results, particular aspects of the study design and study limitations warrant additional consideration. First, as part of the study design, hawthorn was administered simultaneously with digoxin. Coadministration in this manner allowed for inference regarding both P-glycoprotein activity and other factors, such as physiochemical effects, that may alter digoxin absorption. Our results indicate no significant differences in absorption as determined by CmaxCmin and tmax values, suggesting that simultaneous administration is unlikely to affect digoxin absorption. Furthermore, since we did not administer intravenous digoxin, the actual effect on digoxin bioavailability is unknown. Along this line, our results may also be explained if hawthorn blocked P-glycoprotein in the gut and at the same time reduced the amount of digoxin available for absorption through a physical or chemical interaction. It should also be emphasized that this only applies to digoxin, as it is not known whether haw-
640 J Clin Pharmacol 2003;43:637-642
DIGOXIN AND HAWTHORN
thorn absorption is affected. While we did not measure hawthorns individual components, we did use a standardized product made by a reputable manufacturer, making lack of hawthorn absorption highly unlikely. Second, although no statistically significant pharmacokinetic interaction was observed, close inspection of the data suggests that hawthorn coadministration does result in a quantitatively small decrease in absorption and increase in the clearance of digoxin, presumably related to the mild induction of Pglycoprotein activity. This interpretation is based on the finding that AUC, Cmax, Cmax-Cmin, and Cmin were lower and renal clearance was higher in the digoxin plus hawthorn group. In fact, Cmin was approximately 22% lower in this group, a difference that approached our a priori threshold level (p 0.05) for statistical significance (p = 0.054). The reason that these more modest differences were not considered statistically significant is that the study was only adequately powered to detect differences of 25%. Even though our findings suggest that hawthorn causes mild induction (< 25% change) of P-glycoprotein activity, the clinical significance of this is anticipated to be minor in most patients. Certainly, the concern expressed in the clinical herbal medicine literature that hawthorn could increase the risk of digoxin toxicity is not supported by this study. A third consideration is that the true half-life for many of the hawthorn constituents is unknown. In the absence of definitive pharmacokinetic studies of hawthorn, we assumed that 21 days would be sufficient time to reach hawthorn steady state. Whether a longer study period would yield significant results is unknown. It should be mentioned that the study time period for the St. Johns wort study was 15 days and that other studies have shown alterations in P-glycoprotein activity (inhibition or induction) over a much shorter time period than 21 days.11,17 Finally, this study was done in normal subjects and used only one dosage of hawthorn. Whether differences would be seen in patients with heart failure, the likely setting for coadministration, or with higher hawthorn doses is unknown. However, the dosage investigated herein is identical to that being used in a largescale clinical trial of hawthorn6 and is similar to or higher than doses from numerous studies cited in a recent review of hawthorn pharmacology.23 In conclusion, coadministration of hawthorn with digoxin resulted in only modest changes in digoxin pharmacokinetics, differences that did not achieve statistical significance. We hypothesize that these differences are a result of mild P-glycoprotein induction likely due to the presence of quercetin and various
quercetin glycosides in the hawthorn extract. In addition, there was no evidence of any pharmacodynamic interaction, as measured by ECG, heart rate, and blood pressure. In total, these findings suggest that both drugs may be given together safely in the clinical setting in the doses studied.
The authors would like to acknowledge the support of the General Clinical Research Staff. Their assistance was invaluable and appreciated.
REFERENCES
1. Munch G, Brixius K, Frank K, Erdmann E: WS 1442 (extract of Crataegus species) increases force of contraction in human failing + + myocardium by inhibition of the Na /K -ATPase. Circulation 1997; 96(Suppl.):4090. 2. Schussler M, Holzl J, Fricke W: Myocardial effects of flavonoids from Crataegus species. Arzneimittelforschung 1995;45:842-845. 3. Bahorun T, Gressier B, Trotin F, Brunet C, Dine T, Luyckx M, et al: Oxygen species scavenging activity of phenolic extracts from hawthorn fresh plant organs and pharmaceutical preparations. Arzneimittelforschung 1996;46:1086-1089. 4. Chen ZY, Zhang ZS, Kwan KY, Zhu M, Ho WKK, Huang Y: Endothelium-dependent relaxation induced by hawthorn extract in rat mesenteric artery. Life Sci 1998;63:1983-1991. 5. Kim SH, Kang KW, Kim KW, Kim ND: Procyanidins in Crataegus extract evoke endothelium-dependent vasorelaxation in rat aorta. Life Sci 2000;67:121-131. 6. Holubarsch CJF, Colucci WS, Meinertz T, Gaus W, Tendera M: Survival and prognosis: investigations of Crataegus extract WS 1442 in congestive heart failure (SPICE): rationale, study design, and study protocol. Eur J Heart Failure 2000;2:431-437. 7. Johne A, Brockmoller J, Bauer S, Agathe M, Langheinrich M, Roots I: Pharmacokinetic interaction of digoxin with an herbal extract from St. Johns wort (Hypericum perforatum). Clin Pharmacol Ther 1999;66:338-345. 8. Critchfield JW, Welsh CJ, Phang JM, Yeh GC: Modulation of adriamycin accumulation and efflux by flavonoids in HCT-15 colon cells. Biochem Pharmacol 1994;48:1437-1445. 9. Conseil G, Cortay HB, Dayan G, Jault JM, Barron D, Di Pietro A: Flavonoids: a class of modulators with bifunctional interactions at vicinal ATP- and steroid-binding sites on mouse P-glycoprotein. Proc Natl Acad Sci USA 1998;95:9831-9836. 10. Shapiro AB, Ling V: Effect of quercetin on hoechst 33342 transport by purified and reconstituted P-glycoprotein. Biochem Pharmacol 1997;53:587-596. 11. Phang JM, Poore CM, Lopaczynska J, Yeh GC: Flavonol-stimulated efflux of 7,12-dimethylbenz(a)anthracene in multidrug-resistant breast cancer cells. Cancer Res 1993;53:5977-5981. 12. Heart Failure Society of America: Guidelines for management of patients with heart failure caused by left ventricular systolic dysfunction-pharmacological approaches. J Cardiac Failure 1999; 5:357-382. 13. Nahrstedt A, Butterweck V: Biologically active and other chemical constituents of the herb of Hypericum perforatum L. Pharmacopsychiatry 1997;30(Suppl.):129-134.
HERBAL MEDICINE
641
TANKANOW ET AL
14. Chang Q, Zhu M, Zuo Z, Chow M, Ho WK: High-performance liquid chromatographic method for simultaneous determination of hawthorn active components in rat plasma. J Chromatogr B Biomed Sci Appl 2001;760:227-235. 15. Zhang Z, Chang Q, Zhu M, Huang Y, Ho WK, Chen Z: Characterization of antioxidants present in hawthorn fruits. J Nutr Biochem 2001;12:144-152. 16. Obermeier MT, White RE, Yang CS: Effects of bioflavonoids on hepatic P450 activities. Xenobiotica 1995;25:575-584. 17. Scambia G, Ranelletti FO, Panici PB, De Vincenzo R, Bonanno G, Ferrandina G, et al: Quercetin potentiates the effect of adriamycin in a multidrug-resistant MCF-7 human breast-cancer cell line: Pglycoprotein as a possible target. Cancer Chemother Pharmacol 1994;34:459-464. 18. Erlund I, Kosonen T, Alfthan G, Maenpaa J, Perttunen K, Kenraali J, et al: Pharmacokinetics of quercetin aglycone and rutin in healthy volunteers. Eur J Clin Pharmacol 2000;56:545-553.
19. Perloff MD, von Moltke LL, Stormer E, Shader RI, Greenblatt DJ: Saint Johns wort: an in vitro analysis of P-glycoprotein induction due to extended exposure. Br J Pharmacol 2001;134:1601-1608. 20. Greiner B, Eichelbaum M, Fritz P, Kreichgauer HP, von Richter O, Zundler J, et al: The role of intestinal P-glycoprotein in the interaction of digoxin and rifampin. J Clin Invest 1999;104:147-153. 21. Lacarelle B, Rahmani R, de Sousa G, Durand A, Placidi M, Cano JP: Metabolism of digoxin, digoxigenin digitoxosides and digoxigenin in human hepatocytes and liver microsomes. Fundam Clin Pharmacol 1991;5:567-582. 22. Schussler M, Holzl J, Rump AFE, Fricke U: Functional and antiischemic effects of monoacetyl-vitexinrhamnoside in different in vitro models. Gen Pharmacol 1995;26:1565-1570. 23. Rigelsky JM, Sweet BV: Hawthorn: pharmacology and therapeutic uses. Am J Health-Syst Pharm 2002;59:417-422.
642 J Clin Pharmacol 2003;43:637-642
You might also like
- DSCE High Yield GoodDocument23 pagesDSCE High Yield GoodManNo ratings yet
- General Practitioner Sample Resume WWW - Careerfaqs.com - AuDocument3 pagesGeneral Practitioner Sample Resume WWW - Careerfaqs.com - AuSubhash RitwalNo ratings yet
- Indikasi, Teknik Pembuatan Stoma, ReanastomosispptDocument43 pagesIndikasi, Teknik Pembuatan Stoma, ReanastomosispptErwin Aritama Ismail100% (1)
- Antidiabetic Activity of Plants ThesisDocument8 pagesAntidiabetic Activity of Plants Thesisygsyoeikd100% (1)
- Assessment of Digoxin Serum Concentration in Continuous and Interrupted Digoxin RegimensDocument7 pagesAssessment of Digoxin Serum Concentration in Continuous and Interrupted Digoxin RegimensLuh Putu Santi AgustiniNo ratings yet
- Reasearch Publication - RJPSDocument4 pagesReasearch Publication - RJPSHamza Muhammad ShethNo ratings yet
- Capparis Spinosa L. (Caper) Fruit Extract inDocument6 pagesCapparis Spinosa L. (Caper) Fruit Extract inyunitia anjaniNo ratings yet
- Effectiveness and Metabolic Effects of Perindopril and Diuretics Combination in Primary HypertensionDocument5 pagesEffectiveness and Metabolic Effects of Perindopril and Diuretics Combination in Primary Hypertensionguugle gogleNo ratings yet
- Sulodexide For Kidney Protection in Type 2 Diabetes PatientsDocument8 pagesSulodexide For Kidney Protection in Type 2 Diabetes PatientsFerdinand YuzonNo ratings yet
- Pomegranate Juice HealingDocument23 pagesPomegranate Juice HealingKingNo ratings yet
- Bazedoxifane Dan IbuprofenDocument7 pagesBazedoxifane Dan Ibuprofendita novia maharaniNo ratings yet
- Adverse Drug Effects Observed With VildagliptinDocument10 pagesAdverse Drug Effects Observed With Vildagliptin吴善统No ratings yet
- ManuscriptDocument7 pagesManuscriptndumanyachisom23No ratings yet
- Hormone Therapy in Postmenopausal WomenDocument8 pagesHormone Therapy in Postmenopausal WomenChyntia Pramita SariNo ratings yet
- Drug Interaction HT and DMDocument6 pagesDrug Interaction HT and DMAfief Izuddin MhsNo ratings yet
- Nutrient ProfileDocument25 pagesNutrient ProfileJeemCarloFagelaPulaNo ratings yet
- Metabolic StressDocument3 pagesMetabolic StressRoberto MartineNo ratings yet
- Jrip 3 31Document4 pagesJrip 3 31Shivpartap SinghNo ratings yet
- Poster Template 1Document1 pagePoster Template 1Jose Angel Valdez Jr.No ratings yet
- Panax GinsengDocument9 pagesPanax GinsengDevi MelissaNo ratings yet
- Potkin2002 QTP+ Hal Risp Thiridazine RCTDocument10 pagesPotkin2002 QTP+ Hal Risp Thiridazine RCTIulia CiocotisanNo ratings yet
- Markovitz2002 Risp+Probenecid RCTDocument9 pagesMarkovitz2002 Risp+Probenecid RCTIulia CiocotisanNo ratings yet
- ARTIKEL1 Uji Klinik Green TeaDocument6 pagesARTIKEL1 Uji Klinik Green TeaTitiSulistiowatiNo ratings yet
- Anti Diabetic HerbsDocument25 pagesAnti Diabetic HerbsSmritaPradhan PNo ratings yet
- Anethum Graveolens and Hyperlipidemia: A Randomized Clinical TrialDocument13 pagesAnethum Graveolens and Hyperlipidemia: A Randomized Clinical TrialYuliantikha Nurul QomariahNo ratings yet
- Use of Digoxin For Heart Failure and Atrial FibrillationDocument9 pagesUse of Digoxin For Heart Failure and Atrial FibrillationeeleeNo ratings yet
- Choi2014 231128 194257Document13 pagesChoi2014 231128 194257TaraaNo ratings yet
- The Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsDocument9 pagesThe Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsLucky PratamaNo ratings yet
- Desmopressin Clinical PREADocument15 pagesDesmopressin Clinical PREAjoelrequenaNo ratings yet
- SKDI Perkonsil, 11 Maret 13Document8 pagesSKDI Perkonsil, 11 Maret 13Zulfah Zamzami PutriNo ratings yet
- Morinda Citrifolia: Research ArticleDocument5 pagesMorinda Citrifolia: Research ArticleMayara MeloNo ratings yet
- NIH Public Access: Author ManuscriptDocument14 pagesNIH Public Access: Author ManuscriptPutri Septiana PratiwiNo ratings yet
- Inggris - SaponinDocument6 pagesInggris - SaponinrifaniNo ratings yet
- Glenmark Remo+Teneli MS D1 (17082021)Document13 pagesGlenmark Remo+Teneli MS D1 (17082021)Bhavani KirthiNo ratings yet
- Nihms 333002Document16 pagesNihms 333002German FloresNo ratings yet
- Effects of The Proton Pump Inhibitor Lansoprazole On The Pharmacokinetics and Pharmacodynamics ofDocument11 pagesEffects of The Proton Pump Inhibitor Lansoprazole On The Pharmacokinetics and Pharmacodynamics ofLuciana OliveiraNo ratings yet
- V37-4 Art 3 pp186-193Document8 pagesV37-4 Art 3 pp186-193wikka94No ratings yet
- Original Article Randomized Placebo-Controlled Dose-Ranging and Pharmacodynamics Study of Roxadustat (FG-4592) To Treat Anemia in Nondialysis-Dependent Chronic Kidney Disease (NDD-CKD) PatientsDocument9 pagesOriginal Article Randomized Placebo-Controlled Dose-Ranging and Pharmacodynamics Study of Roxadustat (FG-4592) To Treat Anemia in Nondialysis-Dependent Chronic Kidney Disease (NDD-CKD) PatientsNurul MaulidaNo ratings yet
- The Effect of Cinnamon On Glucose of Type II DiabeDocument4 pagesThe Effect of Cinnamon On Glucose of Type II Diabeغاز الشمالNo ratings yet
- Effect of Salvia Officinalis On Diabetic Patients: Journal of Renal Injury PreventionDocument4 pagesEffect of Salvia Officinalis On Diabetic Patients: Journal of Renal Injury PreventionAna Raíza OliveiraNo ratings yet
- Aerius Syrup PIDocument9 pagesAerius Syrup PITerrence LiNo ratings yet
- Jahe 7 Shidfar2015Document6 pagesJahe 7 Shidfar2015irmaNo ratings yet
- Update of Green Tea Interactions With Cardiovascular Drugs and Putative MechanismsDocument6 pagesUpdate of Green Tea Interactions With Cardiovascular Drugs and Putative MechanismsSiscaNo ratings yet
- Comparative Bioavailability Study of Phenytoin inDocument4 pagesComparative Bioavailability Study of Phenytoin inHuydiNo ratings yet
- Kanukula 2019Document7 pagesKanukula 2019Dianne GalangNo ratings yet
- The Effects of Andrographis Paniculata (Burm.f.) Nees On The Pharmacokinetics and Pharmacodynamics of Midazolam in Healthy VolunteersDocument7 pagesThe Effects of Andrographis Paniculata (Burm.f.) Nees On The Pharmacokinetics and Pharmacodynamics of Midazolam in Healthy VolunteersAdquinta Wulandini PutriNo ratings yet
- Terlipressin in Hepatorenal SyndromeDocument9 pagesTerlipressin in Hepatorenal SyndromeMehtab AlamNo ratings yet
- Efficacy of Supplementary Vitamin D On Improvement of Glycemic Parameters in Patients With Type 2 Diabetes Mellitus A..Document5 pagesEfficacy of Supplementary Vitamin D On Improvement of Glycemic Parameters in Patients With Type 2 Diabetes Mellitus A..ariahenkusNo ratings yet
- Groenendaal Vandemeent2016Document11 pagesGroenendaal Vandemeent2016Soshi DaysNo ratings yet
- Interaccion Alimento - FarmacoDocument8 pagesInteraccion Alimento - FarmacoNATALIA TOVAR ORTIZNo ratings yet
- 2 51 1624856559 Ijmpsdec20213Document10 pages2 51 1624856559 Ijmpsdec20213TJPRC PublicationsNo ratings yet
- (2019) Pharmaceutics IVIVC MircioiuDocument15 pages(2019) Pharmaceutics IVIVC MircioiuValentina AnutaNo ratings yet
- International Journal of Ayurveda and Pharma ResearchDocument6 pagesInternational Journal of Ayurveda and Pharma ResearchrinNo ratings yet
- Pediatric PharmacotherapyDocument4 pagesPediatric Pharmacotherapyvk89.naharNo ratings yet
- Analise CORTISOL Salivar Jung Et Al. (2014)Document10 pagesAnalise CORTISOL Salivar Jung Et Al. (2014)sandro kanzlerNo ratings yet
- Effect OF Chlorpromazine AND Haloperidol Combination ON Lipid Profile IN Nigeria Schizophrenic PatientsDocument10 pagesEffect OF Chlorpromazine AND Haloperidol Combination ON Lipid Profile IN Nigeria Schizophrenic PatientstrianaamaliaNo ratings yet
- PHD Thesis On Antidiabetic Activity of PlantsDocument7 pagesPHD Thesis On Antidiabetic Activity of PlantsBuyCheapPapersMiramar100% (2)
- Huang 2018Document11 pagesHuang 2018Savitri IndrasariNo ratings yet
- Interaction of Coadministered Amlodipine and Atorvastatin in 1660 Patients With ConcomitantDocument16 pagesInteraction of Coadministered Amlodipine and Atorvastatin in 1660 Patients With ConcomitantLuciana OliveiraNo ratings yet
- Postnatal Hydrocortisone For Preventing or Treating Bronchopulmonary Dysplasia in Preterm Infants: A Systematic ReviewDocument7 pagesPostnatal Hydrocortisone For Preventing or Treating Bronchopulmonary Dysplasia in Preterm Infants: A Systematic ReviewAldy RinaldiNo ratings yet
- Untitled 1Document17 pagesUntitled 1bennyNo ratings yet
- Renal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysFrom EverandRenal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 13: DermatologyFrom EverandComplementary and Alternative Medical Lab Testing Part 13: DermatologyRating: 5 out of 5 stars5/5 (4)
- Human Body SystemsDocument21 pagesHuman Body Systemsveeramani100% (3)
- BIO-Zoology PracticalDocument38 pagesBIO-Zoology PracticalveeramaniNo ratings yet
- Cell Organelles ReviewDocument21 pagesCell Organelles ReviewveeramaniNo ratings yet
- Cell Biology Standard 1EDocument15 pagesCell Biology Standard 1EveeramaniNo ratings yet
- Guess My Name Identifying AnimalsDocument1 pageGuess My Name Identifying AnimalsveeramaniNo ratings yet
- Cell Structure FunctionDocument26 pagesCell Structure Functionveeramani0% (1)
- (Please Fill in All The Details in BLOCK Letters) : Staff Resume FormatDocument1 page(Please Fill in All The Details in BLOCK Letters) : Staff Resume FormatveeramaniNo ratings yet
- Protein DatabaseDocument1 pageProtein DatabaseveeramaniNo ratings yet
- Nadine Ayouch Part 1 AssigmentDocument9 pagesNadine Ayouch Part 1 AssigmentNadine AyouchNo ratings yet
- Cytotoxicity Test of Binjai Leaf Mangifera Caesia PDFDocument6 pagesCytotoxicity Test of Binjai Leaf Mangifera Caesia PDFAnonymous QF5aauTNo ratings yet
- Aspartame As An Artificial SweetenerDocument16 pagesAspartame As An Artificial SweetenerIsmi Arinal HaqNo ratings yet
- Nottingham Hip Fracture Score As A Predictor of One Year PDFDocument4 pagesNottingham Hip Fracture Score As A Predictor of One Year PDFjavieccrNo ratings yet
- Sexual Dysfunction 4Document53 pagesSexual Dysfunction 4CJ AngelesNo ratings yet
- Clinical ReflectionDocument4 pagesClinical Reflectionapi-316342033No ratings yet
- Crede'S and Ritgen'S Manuever Episiorrhapy Care: University of Northern PhilippinesDocument9 pagesCrede'S and Ritgen'S Manuever Episiorrhapy Care: University of Northern PhilippinesJewel Ramos GalinatoNo ratings yet
- Post Modern CounselingDocument27 pagesPost Modern CounselingIvanNo ratings yet
- Anchorage Loss - A Multifactorial Response: The Angle Orthodontist January 2004Document9 pagesAnchorage Loss - A Multifactorial Response: The Angle Orthodontist January 2004Thomas Karl QuilangNo ratings yet
- Self Healing With Qi Gong ContentDocument9 pagesSelf Healing With Qi Gong ContentSteven RendinaNo ratings yet
- Drugs and TeensDocument13 pagesDrugs and Teenstony_petriNo ratings yet
- Nutrition For Exercise and Sport Exam PDFDocument6 pagesNutrition For Exercise and Sport Exam PDFAngela BrownNo ratings yet
- Asugal Albi 90 MsdsDocument6 pagesAsugal Albi 90 MsdsMuhammad Aasim HassanNo ratings yet
- A Review On Needle Free Injection SystemDocument11 pagesA Review On Needle Free Injection SystemShiji DanielNo ratings yet
- Bank Question For DiscussDocument7 pagesBank Question For Discusssaepulloh bin amingNo ratings yet
- Ankle Disarticulation Prosthetics: Course Work ManualDocument52 pagesAnkle Disarticulation Prosthetics: Course Work ManualJananthan Thavarajah67% (3)
- Neuromodulation For Addiction 082209Document9 pagesNeuromodulation For Addiction 082209hellno1234100% (1)
- Are We Ready For CannabisDocument15 pagesAre We Ready For CannabisBeatta RamirezNo ratings yet
- ماتريال المراكز والوحدات كاملة-3Document33 pagesماتريال المراكز والوحدات كاملة-3Sanaa SbdelghanyNo ratings yet
- Dos 523 ProjectDocument13 pagesDos 523 Projectapi-375157618No ratings yet
- Analytical Customer UpdationDocument16 pagesAnalytical Customer UpdationSathish SmartNo ratings yet
- Waste Disposal of Each Family MemberDocument4 pagesWaste Disposal of Each Family MemberLemuel Glenn BautistaNo ratings yet
- Internet Case For Supplement 7Document3 pagesInternet Case For Supplement 7johnmia20No ratings yet
- Industrial Report ON The Dabur CompanyDocument71 pagesIndustrial Report ON The Dabur CompanyAmit JaiswalNo ratings yet
- Carvedilol (Drug Study)Document3 pagesCarvedilol (Drug Study)Franz.thenurse688890% (10)
- The Glivec PrecedentDocument20 pagesThe Glivec PrecedentSoham MukherjeeNo ratings yet
- Blood ProductDocument89 pagesBlood ProductSam0% (1)