Professional Documents
Culture Documents
General Tox Approach
General Tox Approach
Uploaded by
Anonymous 4txA8N8etCopyright:
Available Formats
You might also like
- FRCPath Mock 2014 Model AnswersDocument29 pagesFRCPath Mock 2014 Model Answersmonday125No ratings yet
- Ganong - Physiology Self - Assessment Questions - 03Document46 pagesGanong - Physiology Self - Assessment Questions - 03Anonymous 4txA8N8et100% (3)
- Chemistry of CannabisDocument52 pagesChemistry of Cannabisciborg1978No ratings yet
- Chromatography LabDocument9 pagesChromatography Labjtrumpeter224100% (1)
- Poisoning: Overview of Pediatric Poisoning, Diagnosis and Treatment Summary of The Most Encountered PoisoningDocument46 pagesPoisoning: Overview of Pediatric Poisoning, Diagnosis and Treatment Summary of The Most Encountered PoisoningSergey DukkNo ratings yet
- Poisoning Stage V - 2020Document96 pagesPoisoning Stage V - 2020Sarper Hikmet TAZENo ratings yet
- Poisoning PDFDocument124 pagesPoisoning PDFDawn WRein Legaspi67% (3)
- Alcohol ToxicityDocument81 pagesAlcohol ToxicityKarim RezaNo ratings yet
- Toxic Alcohols - High Yields NEJMDocument21 pagesToxic Alcohols - High Yields NEJMDr. Shanojan Thiyagalingam, FRCPC FACPNo ratings yet
- Approach To Poisoned PatientDocument90 pagesApproach To Poisoned PatientGopi KrishnanNo ratings yet
- UMBC CC-EMTP Class Notes, FLCC Class 2010Document93 pagesUMBC CC-EMTP Class Notes, FLCC Class 2010Marc LaBarberaNo ratings yet
- Toxic AlcoholsDocument4 pagesToxic AlcoholsKaran SandhuNo ratings yet
- Dyah Trifianingsih, S. Kep. Ners. M. KepDocument76 pagesDyah Trifianingsih, S. Kep. Ners. M. KepSiprianus S SNo ratings yet
- Alcohol & Glycols: Group # 5 Aranas, Roxette Louraine Ardivilla, Gazel Myrrh Hugo, KevinDocument30 pagesAlcohol & Glycols: Group # 5 Aranas, Roxette Louraine Ardivilla, Gazel Myrrh Hugo, KevinRoxette Louraine R. AranasNo ratings yet
- AlcoholsDocument23 pagesAlcoholsdhaineyNo ratings yet
- Tox CasesDocument7 pagesTox CasesNeo Mervyn Monaheng100% (1)
- Drug Toxicology: Agung Nova Mahendra Department of Pharmacology & Therapy Faculty of Medicine, Udayana UniversityDocument27 pagesDrug Toxicology: Agung Nova Mahendra Department of Pharmacology & Therapy Faculty of Medicine, Udayana Universitywayan lentaraNo ratings yet
- 41 Clinical Cases in Biochemistry UKDocument2 pages41 Clinical Cases in Biochemistry UKAlexandra Ioana MoatarNo ratings yet
- Toxicology Lecture 10 (Chapter 7 Volatiles)Document22 pagesToxicology Lecture 10 (Chapter 7 Volatiles)MowlidAbdirahman Ali madaaleNo ratings yet
- Respiratory Acidosis Is Characterized by An Increase in The pCODocument3 pagesRespiratory Acidosis Is Characterized by An Increase in The pCOMwanja MosesNo ratings yet
- 5 2015 Farmako-ToxicologyDocument71 pages5 2015 Farmako-ToxicologyIkhzan PriolaksanaNo ratings yet
- Chemical Pathology Practical ExamDocument46 pagesChemical Pathology Practical ExamAbdulsamad AfolabiNo ratings yet
- Michael Chansky Acid Base Made Easy HandoutDocument18 pagesMichael Chansky Acid Base Made Easy HandoutTeguh RamadhanNo ratings yet
- Alcohols Ethanol, MethanolDocument55 pagesAlcohols Ethanol, MethanoljayNo ratings yet
- Acid Base Disorders Peter SehaDocument29 pagesAcid Base Disorders Peter SehaPeter SehaNo ratings yet
- Respiratory Assessment FindingsDocument197 pagesRespiratory Assessment Findingsannatw100% (2)
- Adi - IntoxicationDocument52 pagesAdi - IntoxicationAdi WidanaNo ratings yet
- Questions To Consider:: Ethylene Glycol Poisoning. Ethylene Glycol Chemically Occupies A Position Between EthylDocument4 pagesQuestions To Consider:: Ethylene Glycol Poisoning. Ethylene Glycol Chemically Occupies A Position Between EthylJeanette Miña GrajoNo ratings yet
- Anion Gap Metabolic Acidosis: More Then Just A Mud PileDocument21 pagesAnion Gap Metabolic Acidosis: More Then Just A Mud PileFarah SyazanaNo ratings yet
- Management of Poisoned PatientsDocument56 pagesManagement of Poisoned PatientsAmmarah TaimurNo ratings yet
- Acid Base PhysiologyDocument4 pagesAcid Base PhysiologyGhadeer EbraheemNo ratings yet
- ABG Algorithm PDFDocument2 pagesABG Algorithm PDFamin2014No ratings yet
- Module Iii Lab Manual (2024)Document20 pagesModule Iii Lab Manual (2024)ur.yared21No ratings yet
- Rat PoisonDocument41 pagesRat Poisonkhizra mumtazNo ratings yet
- Approach To Acid-Base Problems: DR Frank DalyDocument57 pagesApproach To Acid-Base Problems: DR Frank DalyscanutdNo ratings yet
- Fluid and ElectrolytesDocument14 pagesFluid and Electrolytesstring44100% (2)
- Moderator: Dr. R. K. Yadav (MD) Presented By: Ashish JaisawalDocument47 pagesModerator: Dr. R. K. Yadav (MD) Presented By: Ashish Jaisawalimranqazi11No ratings yet
- Final Exam Focus SheetDocument9 pagesFinal Exam Focus SheetDane WrightNo ratings yet
- Acid-Base Interpretation: APRIL 4, 2017Document9 pagesAcid-Base Interpretation: APRIL 4, 2017mohamedsmnNo ratings yet
- General Principles and Management of PoisonsDocument5 pagesGeneral Principles and Management of PoisonsOkpetah Chioma christabelNo ratings yet
- Drug OverdoseDocument94 pagesDrug Overdosemicheal1960No ratings yet
- Student Tox LectureDocument49 pagesStudent Tox Lecturelenin_villaltaNo ratings yet
- ABG MMHG InterpretationDocument92 pagesABG MMHG InterpretationManmeet SNo ratings yet
- Acid Base Disorders DR Kwaifa - PPTX 1Document99 pagesAcid Base Disorders DR Kwaifa - PPTX 1DICKSONNo ratings yet
- Ethylene Glycol Toxicosis in Animals - Toxicology - MSD Veterinary ManualDocument6 pagesEthylene Glycol Toxicosis in Animals - Toxicology - MSD Veterinary ManualMuhammad AgussalimNo ratings yet
- Synthesis Final ReviewDocument20 pagesSynthesis Final ReviewSamNo ratings yet
- Poisoning in ChildrenDocument11 pagesPoisoning in ChildrenAndriana HalfienNo ratings yet
- Body Fluids and ElectrolytesDocument42 pagesBody Fluids and ElectrolytesQusaiBadr100% (1)
- Tugas GinjalDocument22 pagesTugas GinjalAnastasia MargaretNo ratings yet
- Acid Base EquationsDocument21 pagesAcid Base EquationsBen JonesNo ratings yet
- Assignment: ToxicologyDocument8 pagesAssignment: ToxicologyAyesha LiaqatNo ratings yet
- Anion Gap Metabolic Acidemia Case BasedDocument4 pagesAnion Gap Metabolic Acidemia Case Basedspiros.a.markouNo ratings yet
- Case Report: An Unconscious Man With Profound Drug-Induced HypoglycaemiaDocument6 pagesCase Report: An Unconscious Man With Profound Drug-Induced Hypoglycaemiagevowo3277No ratings yet
- Acute Poisoning of Therapeutic Agents: by Alemayehu TomaDocument42 pagesAcute Poisoning of Therapeutic Agents: by Alemayehu TomaYohannis AsefaNo ratings yet
- Mnemonics: Do Not Adsorb To CharcoalDocument25 pagesMnemonics: Do Not Adsorb To CharcoalJiaYee GoNo ratings yet
- ABG Interpretation 1Document59 pagesABG Interpretation 1Sura KwakNo ratings yet
- Chapter Four: Chemical Analysis of UrineDocument174 pagesChapter Four: Chemical Analysis of UrineRebuma BeleteNo ratings yet
- AlcohoDocument32 pagesAlcohoVaibhav KaroliyaNo ratings yet
- Enzyme-summary (1)Document7 pagesEnzyme-summary (1)Aira Jane GamboaNo ratings yet
- ELECTROLYTES (Na & K)Document3 pagesELECTROLYTES (Na & K)Alondra SagarioNo ratings yet
- Alcohol Toxicity PDFDocument20 pagesAlcohol Toxicity PDFNabila Fatmayday UdiyahNo ratings yet
- The Impact Of Alcohol On The Brain - Based On The Teachings Of Dr. Andrew Huberman: Examining The Complex Interplay Between Alcohol And NeurobiologyFrom EverandThe Impact Of Alcohol On The Brain - Based On The Teachings Of Dr. Andrew Huberman: Examining The Complex Interplay Between Alcohol And NeurobiologyNo ratings yet
- Pass Paces EbDocument10 pagesPass Paces EbAnonymous 4txA8N8etNo ratings yet
- H IsselbacherDocument5 pagesH IsselbacherAnonymous 4txA8N8etNo ratings yet
- Topics Runtime: Subjects AnatomyDocument2 pagesTopics Runtime: Subjects AnatomyAnonymous 4txA8N8etNo ratings yet
- Hp165-02b-Nash (FF 050816v) ProtegidoDocument9 pagesHp165-02b-Nash (FF 050816v) ProtegidoAnonymous 4txA8N8etNo ratings yet
- Adpkd: Autosomal Dominant Polycystic Kidney DiseaseDocument7 pagesAdpkd: Autosomal Dominant Polycystic Kidney DiseaseAnonymous 4txA8N8etNo ratings yet
- Hanzi Pinyin English: HSK Level 2Document5 pagesHanzi Pinyin English: HSK Level 2Anonymous 4txA8N8etNo ratings yet
- Genetics 50qDocument62 pagesGenetics 50qAnonymous 4txA8N8etNo ratings yet
- Radiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedDocument1 pageRadiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedAnonymous 4txA8N8etNo ratings yet
- 6 Steps in Assisting in Cardiac Rhythm InterpretationDocument1 page6 Steps in Assisting in Cardiac Rhythm InterpretationAnonymous 4txA8N8etNo ratings yet
- EMQExample RacpDocument5 pagesEMQExample RacpAnonymous 4txA8N8etNo ratings yet
- Brunicardi-1996-Time Management - A RDocument7 pagesBrunicardi-1996-Time Management - A RAnonymous 4txA8N8etNo ratings yet
- Abdominal Exam DATEDocument3 pagesAbdominal Exam DATEAnonymous 4txA8N8etNo ratings yet
- Effective Feedback Skills: Sally Santen MD, PHDDocument9 pagesEffective Feedback Skills: Sally Santen MD, PHDAnonymous 4txA8N8etNo ratings yet
- Lymphoproliferative Disorders Part 2Document7 pagesLymphoproliferative Disorders Part 2Anonymous 4txA8N8etNo ratings yet
- Previous PLE QuestionsDocument3 pagesPrevious PLE QuestionsGrace Benero Pequero0% (1)
- Analytical Methods For Amino Acid Determination in OrganismsDocument18 pagesAnalytical Methods For Amino Acid Determination in OrganismsVeneta GizdakovaNo ratings yet
- A General Procedure For Mitsunobu Inversion of Sterically Hindered Alcohols - Inversion of Menthol. (1S, 2S, 5R) - 5-Methyl-2 - (1-Methylethyl) Cyclohexyl 4-Nitrobenzoate PDFDocument4 pagesA General Procedure For Mitsunobu Inversion of Sterically Hindered Alcohols - Inversion of Menthol. (1S, 2S, 5R) - 5-Methyl-2 - (1-Methylethyl) Cyclohexyl 4-Nitrobenzoate PDFthamtusieuquayNo ratings yet
- Oxford GR 10 Topic 1 Matter & ClassificationDocument54 pagesOxford GR 10 Topic 1 Matter & ClassificationkhotsoNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaAudry YuniarNo ratings yet
- Uncertainty Related To The Use Of: Relative Retention Times in Pharmaceutical AnalysisDocument7 pagesUncertainty Related To The Use Of: Relative Retention Times in Pharmaceutical AnalysisnmmMJKJNo ratings yet
- Gas Chromatography, GCDocument85 pagesGas Chromatography, GCShaise Jacob67% (3)
- Adenosine Injection: 2348 Adenosine / Official Monographs USP 39Document2 pagesAdenosine Injection: 2348 Adenosine / Official Monographs USP 39Luz De MarNo ratings yet
- Science7 Q1 WK5Document3 pagesScience7 Q1 WK5hannahsofiapreyesNo ratings yet
- PrefaceDocument566 pagesPrefaceNurlaini NasutionNo ratings yet
- Poster B12Document1 pagePoster B12Vikas GoyalNo ratings yet
- New Trends in Forced Degradation StudiesDocument10 pagesNew Trends in Forced Degradation StudiesLina SakellariouNo ratings yet
- HPLC Column Phenomenex LunaDocument34 pagesHPLC Column Phenomenex LunaShiraz Khan0% (1)
- Separation, Electroanalytical and Spectrometric TechniquesDocument115 pagesSeparation, Electroanalytical and Spectrometric TechniquesRicardo SimõesNo ratings yet
- Chromatography PharmacyDocument41 pagesChromatography PharmacyfarisaNo ratings yet
- Analytical Tasks - Efficiently Solved by HPTLC: Camag Bibliography ServiceDocument68 pagesAnalytical Tasks - Efficiently Solved by HPTLC: Camag Bibliography ServiceDarian HerascuNo ratings yet
- MS Solutions: Tech TipDocument11 pagesMS Solutions: Tech TipKelumNo ratings yet
- Extension of The QuEChERS Method For Pesticide Residues Cereals, PeanutsDocument9 pagesExtension of The QuEChERS Method For Pesticide Residues Cereals, PeanutsrumitpashaNo ratings yet
- International Biodeterioration & Biodegradation: Daiyong Deng, Jun Guo, Guoqu Zeng, Guoping SunDocument7 pagesInternational Biodeterioration & Biodegradation: Daiyong Deng, Jun Guo, Guoqu Zeng, Guoping SunVenny SandjajaNo ratings yet
- ICW-3000 Water Purification System - MerckmilliporeDocument2 pagesICW-3000 Water Purification System - MerckmilliporeMerck IndiaNo ratings yet
- HPLC 2015Document102 pagesHPLC 2015Ojan FauzanNo ratings yet
- Applications of High Performance Liquid ChromatographyDocument3 pagesApplications of High Performance Liquid ChromatographyKavisa GhoshNo ratings yet
- Course Outline CEV444 (Sep 2017-Jan 2018)Document7 pagesCourse Outline CEV444 (Sep 2017-Jan 2018)Solehah OmarNo ratings yet
- Cbiescco 02Document7 pagesCbiescco 02Rishabh Bhati100% (1)
- pdf01 PDFDocument44 pagespdf01 PDFRafi IqbalNo ratings yet
- Kelebihan Kekurangan Kromatografi KolomDocument8 pagesKelebihan Kekurangan Kromatografi KolomFendy FendyNo ratings yet
- High Performance Liquid Chromatography (HPLC) : Presenter: Nandit P BDocument39 pagesHigh Performance Liquid Chromatography (HPLC) : Presenter: Nandit P BNandit BanawalikarNo ratings yet
- s00226 018 1057 3Document15 pagess00226 018 1057 3Aeric HalzNo ratings yet
General Tox Approach
General Tox Approach
Uploaded by
Anonymous 4txA8N8etCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
General Tox Approach
General Tox Approach
Uploaded by
Anonymous 4txA8N8etCopyright:
Available Formats
GENERAL APPROACH TO THE POISONED PATIENT
PRIMARY SURVEY AIRWAY: LOOK LISTEN FEEL MANAGE BREATHING: LOOK LISTEN FEEL MANAGE CIRCULATION: LOOK LISTEN FEEL MANAGE DISABILITY: PUPILS GCS MANAGE EXPOSURE: FULL VITALS: Check chemstrip and temperature ADJUNCTS TO PRIMARY SURVEY Universal antidotes (if indicated) Dextrose: 1g/Kg (D50W in adults, D25W in peds) Oxygen Narcan: 2mg bolus IV/IM/SL/SC/ETT then 10mg repeat if no effect (peds: 0.01mg/kg bolus then 0.1mg/Kg repeat) Thiamine: 100mg IV/IM (before glucose) Toxicologic Investigations Tox labs: CBC, urea, Cr, lytes, osmolarity, EtOH, glucose, ASA, APAP ECG Liver enzymes/function for hepatotoxins ABG if sick Serum Drug Levels prn Urine tox screen if indicated SECONDARY SURVEY Full head - to - toe examination Look for toxidromes Look for trauma Look for signs of medical illness ADJUNCTS TO SECONDARY SURVEY Decontamination Gastric Lavage Epicac Shower Irrigation Activated charcoal Multi-dose activated charcoal Whole Bowel Irrigation Elimination Alkalinization Forced Saline diuresis Dialysis Specific antidoses or adjuncts
CLINICAL FEATURES OF TOXICOLOGY
TOXICOLOGICAL HISTORY Overdose details: What, when, route, dose, co-ingestants, why EMS should bring all prescription bottles Get pharmacy printout Identify pills and make sure pills equal label Look through medications on old chart Ask family/friend about possible ingestants Ask what else is available in the house (INH example) Bring in containers Search the patient Have family or police search the patients house Consider body packing/stuffing if ingestant unknown Specifically ask about SLOW - RELEASE preparations TOXICOLOGICAL EXAMINATION Accurate vital signs essential Look for signs of trauma: head trauma important Look for signs of medical illness Look for body packing/stuffing Look for toxidromes = constellations of signs and symptoms associated with a class of drug or toxin Level of consciousness HR, BP, temp Pupils Skin Bowel sounds Reflexes, rigidity Odors in Overdoses Almonds Cyanide Carrots Water hemlock Fishy Zinc or aluminum Fruity EtOH, acetone, isopropanol, hydrocarbons Garlic Arsenic, etc Glue Toluene, solvents Pears Chloral hydrate, paraldehyde Rotten eggs H2S, NAC Shoe polish Nitro benzene Wintergreen Methyl salicylate
TOXINS CAUSING SEIZURES TOXINS AND CV CHANGES C Cyclic antidepressants Cholinergics:organophosphates Caffeine Camphor Amphetamines Antihistamines Amoxapine Phenothiazines Propranolol Phenylpropanolamine Piroxicam Isoniazid (think in aboriginals, refractory seizures, or anyone on TB Rx) Theophylline BRADYCARDIA TACHYCARDIA TCA Phenothiazine Theophylline Chloral Hydrate Any stimulant SSRIs SNRIs Cholinergics Beta Blockers CCBs Digoxin Na channel blockers Opiates Sedative/hypnotics Alpha agonists GHB Trazadone TCAs Antihistamines Cocaines Other stimulants BB CCB Digoxin Carbemazepine Quinine Chloroquine Phenothiazines
TOXINS CAUSING TEMP CHANGES Hyperthermia Anitcholinergics Sympathomimetics Seritonin syndrome Salicylates Methylxanthines Thyroxoine NMS Hypothermia CO Opiates Oral hypoglycemics Insulin Alcohol Sedatives Hypnotics Phenothiazines
WCT
TOXINS CAUSING PINPOINT PUPILS (MIOSIS) Clonidine Opiates (except demerol) Organophosphates PCP Phenothiazines Pilocarpine
TOXICOLOGY AND THE LAB
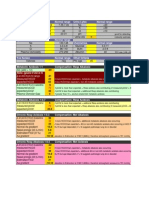
DRUG SCREENS NOT ROUTINELY INDICATED Lab doesnt screen for most drugs Initial screen may be negative if done soon after the ingestion Positive findings may not be the cause of the presentation (cocaine +ve in urine for days after use) Expensive Rarely change clinical managment ANION GAP The difference between measured cations and anions There truly is no difference b/c electrical neutrality is maintained but we dont measure all cations and anions thus a measured gap is evident Cations: Na+ is vast majority (Ca, Mg, K are minority) Anions: Cl-, HC03 Anion Gap made up mostly of albumin: thus hypoalbuminemic patients have a lower anion gap and increased AGMA may not be picked up (AG may go from 5 to 10 but is still within the normal range) Low anion gap (<3) can also be seen in Lithium toxicity and IgG myeloma Normal range is 10 - 15 (traditionally 12 +/- 3) Gain an ACID: if Cl- is the anion there will be NO increase in anion gap and the Cl- will increasethe same as the HC03 drops Gain an ACID: if Cl - is NOT the anion then there will be an increase in the anion gap and the increase will match the drop in the HC03 Delta Gap delta G = change in AG - change in HC03 delta G = (AG - 12) - (24 - HC03) elevated delta G > +6: simultaneous metabolic alkalosis or respiratory acidosis low delta G < -6: simultaneous respiratory alkalosis or low AG state Other CO/CN: oxidative phosphorylation inhibition EtOH: ethyl alcohol donates an H+ thus mild direct acidosis; also respiratory depression and dehydration thus mild indirect acidosis Paraldehyde: acetic and chloracetic acid Methanol: formic acid Ethylene glycol: oxalic acid Isoniazid: > 30 mg/kg causes lifethreatening acidosis, acidosis is secondary to lactate production during seizure; pyridoxine and dialysis as treatment Iron: inhibits oxidative phosphrylation, negative ionotrope, dehydrated, GI bleeding/hypovolemia, and Fe2+ > F3 + + H+ all contribute to acidosis ASA: acetylsalicylic acid, salicylic acid, also inhibits oxidative phosphorylation thus lactic acidosis (major mechanism), ketoacidosis, aminoacids (catabolic state due to inhibition of oxidative phosphyrlation); note combined A/B disorder b/c of stimulation of respiratory centers and respiratory alkalosis Toluene -inhaled hydrocarbon; often abused
-acrylic paints, glues, adhesives, paint, varnish, laquers -sniffing (breath over a container), huffing (sniff from a rag) or bagging (sniff from a bag) -rapid absorption to lungs, CNS intoxication for hours -CNS: stupor, intoxication, sz, ataxia, headache, hallucination -CVS: arrythmias and sudden death (SENSITIZED MYOCARDIUM to catecholamines); inhaled hydrocarbon then exertion > sudden death Toxins that increase AGMA independent of lactate ASA Methanol Ethylene glycol
DIFFERENTIAL DIAGNOSIS OF INCREASED AGMA
A M U D P I L E C A T O AKA, ASA, alcohol intoxication Methanol Uremia DKA Paradehyde, Phenformin (Metformin) Iron, Isoniazid, Ibuprofen (rare) Lactic acidosis (any cause) Ethylene glycol CO, CN ASA Toluene, Theophylline Other H2S Metformin
OSMOLAR GAP Osmolality = measured osmolality Lab measurement of moles of solute/kg of solvent Measured by freezing point depression Can also be measured by vapor pressure but this is less reliable b/c erroneously low results will occur with volatile substances (alcohols) Osmolarity = osmolarity calculated Calculated moles of solute/L of solution Different formulas exist Calgary lab uses: 1.86Na + BUN + glucose + 9 + EtOH (this assumes Na+ Cl- ionized forms which is more accurate)
Osmolar Gap
Edmonton lab uses: 2Na + BUN + glucose + EtOH (this assumes NaCl form which is less accurate) Osmolar Gap = Measure osmolality - Calculated osmolarity Normal osmolar gap = -15 up to + 10 (mean -2) Normal gap due to calcium, lipids, proteins Differential diagnosis of osmolar gap: see table Note that a wide range of osmolar gaps are possible with toxic alcohols; there may be no osmolar gap if converted to metabolites Indications for measuring toxic alcohols: (note: you can and should still measure toxic alcohol levels if indicated but you will have to specifically ask for them) Calgary lab: osmolar gap > 10 Edmonton lab: osmolar gap > 2; ethylene glycol level done osmoar gap > 5; methanol level done the Osmolar Gap Osmolarity formulas account for EtOH level New evidence that EtOH actually increases the osmolar gap more than expected from the EtOH level alone Purssell Ann Emerg Med 2001 Correlated osmolality with rising levels of EtOH Determined that EtOH X 1.25 should be used when calculating osmolarity EtOH results in higher osmolality than expected from simple EtOH level: why? Ethanol in solution has a nonideal osmotic behaviour (ie; they form bonds with each other when put in solution thus changing the osmotic effect). In other words, 1 mmol/L (osmolarity) leads to 1.25 mOsm/kg (osmolality)
Ethanol and
P A
Proteins Alcohols - Ethanol - Methanol - Isopropanol - Propylene glycol (plumming antifreeze, diluant for many drugs) - Diethylene glycol - Triethylene glycol Surgars - Mannitol - Glycerol - Sorbitol Contrast dye Acidosis - Lacticacidosis - Ketoacidosis (DKA, AKA) Lipids Acetone
C A L A
TOXICOLOGICAL TESTS Immunoassays Uses antibodies to detect drugs or metabolites Chromatography Analyte specificity is achieved by physical separation Major advantage: multiple substances can be detected in a single procedure Can look for many different compounds thus more useful for general screening Thin Layer Chromatography: substance put on thin layer plate, solvent is drawn up the plate by capillary action; compared to controls; slow and labor intensive High Performance Liquid Chromatography: similar idea but the mobile phase is pumped through under high pressure; peaks are detected depending on how far the substance moved down the plate and are compared to controls Gas Chromatography: similar idea but the moving phase is a gas Mass spectrometer: a highly sensitive detector to detect very small quantities; mas spec uses electromagnetic filtering to determine the mass of the ions; ultimately produces peaks on graph that are characteristic of certain drugs Urine Tox screens Vary with each lab Most urine screens use immunoassays Confirmatory Gas chromatography and mass spec is done if immunoassay is +ve
DECONTAMINATION GENERAL Definition Decontamination is the prevention of absorption into the bloodstream Factors to consider Is this a dangerous toxin? Is there likely to be further absorption? How long from the time of ingestion? Is there an effective antidote? Has the clinical course excluded the posibility of toxicity? Gastric Emptying Most studies show that minimal drug is in stomach after 2-4 hours Time in stomach varies with drug Drugs that SLOW gastric emptying and increase the possible time for gastric empyting to be effective Anticholinergics Opiates Sedative/hypnotics Gastric concretions: ASA, iron, phenobarbital Vomiting Self induced vomiting and ipecac are never indicated Unlikely to removed significant amount of toxin Risk of aspiration Ipecac hinds administration of charcoal Risk of MWTs, esophageal rupture GASTRIC LAVAGE Technique of Gastric Lavage Large gastric tube (36 french) Left lateral position Tap water or saline 300 cc in, clamp, drain by gravity Continue until clear; follow lavage with activated charcoal Potential Complications Injury to pharynx Esophageal tears Gastric perforation Aspiration Evidence Behind and Controversies Shown to decrease drug absorption in volunteers Only (limited) clinical benefit has been shown if done LESS than one hour Has been trends toward clinical improvements in serious overdoses Some people advocate never using gastric lavage, BUT!! ACEP policy statement: little to indicate value; selective use only Study limitations Small sample sizes thus not powered to exclude clinically important differences
Include multiple different overdoses Exclude critically ill patients (where it is really needed!!) Poor controls, poor randomization Hasnt been specifically studied where it makes more sense (enteric coated, pylorospasms, gastric concretions, etc)
Indications for gastric lavage No universal indications can be given Case-by-case consideration is appropriate Considerations FOR gastric lavage Potentially lethal overdose NO effective antidote Patient currently symptomatic Time since ingestions < 1-2 hours Charcoal ineffective (Li, Fe) Gastric concretions (ASA, Fe, enteric coated, phenobarb) Pylorospasm (ASA) No antecedant vomiting Delayed gastric absorption (anticholinergics, narcotics, enteric coated preparations) Contraindications Inability to protect airway (ie; must intubate)
ACTIVATED CHARCOAL Dose No universal correct dose; no maximum dose known Ideal charcoal:drug ratio is 10:1 Most common initial doses: 0.5 - 1.0 g/kg (Adults = 50 gm) Use larger doses (1.5 - 2.0 g/kg) for dangerous large ingestions of agents well absorbed by charcoal: ASA, theophylline, verapamil SR How beneficial is activated charcoal? Lowers absorption, lower peak serum levels, decreased area under the curve Beneficial only if substance still present in the GI tract and binds to charcoal Many animal studies showing benefit Many human studies showing decreased absorption Limited studies to show clinical benefit Indications Should be administered in virtually all cases of potentially toxic overdoses More effective earlier but history is so inaccurate, reasonable to give even with later presentations Consider using for overdose of toxin that doesnt bind charcoal b/c of possibility of co-ingestant Drugs NOT absorbed by charcoal C Caustics H Hydrocarbons
I Iron L Lithium, Lead E Ethanol Multidose Activated Charcoal (MDAC) Doses and frequency varies with indication Can be given by continuous NG infusion Massive ingestion: one dose wont be enough Sustained release: delayed release of drug Gastric concretions Enhanced elimination: prevents enterohepatic reabsorption of active drug or metabolites? Contraindications Caustic ingestions: doesnt bind, obscures endoscopy Unprotected airway Hydrocarbons: increased risk of aspiration and ARDS Complications Very safe GI upset Bowel obstruction: case reports with MDAC Aspiration is biggest risk Trivial aspiration very common Significant aspiration rare -
CATHARTICS Purpose = increase GI transit speed, decrease transit time No proven benefit Effect on activated charcoal: occasionally benefitial, usually no effect, occasionally harmful Only three used with any frequency: sorbital, magnesium sulfate, magnesium citrate Sorbital: 1 gm/kg; repeat dose X 1 only at 0.5 mg/kg with MDAC if no ileus/obstruction No evidence of harm for single use if no contraindications Complications: dehydration, electrolyte changes, GI upset, abdominal distension Children have more problems with fluid and electrolyte shifts Relative contraindications: Bowel obstruction Ileus (absent bowel sounds) Diarrhea (uneccessary) Infants and young children WHOLE BOWEL IRRIGATION General More effective than clearing bowel than cathartic PEG-ELS solution is electrolyte and osmolarity balanced thus no fluid/electrolyte shifts (isotonic components); huge volumes are not dangerous Components are not absorbed Mechanical washout of bowel (doesnt draw in fluid or stimulate motility) Indications for WBI: serious overdoses, poor binding to charcoal, sustained release
Iron Lithium Body packers Body stuffers Slow release preparations ASA CCBs Valproic acid
OTHER GI DECONTAMINATION Endoscopic removal: difficult to remove concretions and body packs; complications of procedure usually outweigh potential benefit; rarely indicated (very durable packs with body packers) Surgical removal: rarely body packs causing bowel obstruction or intestinal ischemia Surgery post GI perforation after caustic ingestions
ELIMINATION
GENERAL Elimination = removal of toxin after it has been absorbed Indications Patients who fail supportive care Patients in whom the normal route of elimination is impaired (renal failure) Patients in whom the toxin is expected to be very significant Patients that are not expected to tolerate the physiologic effects Methods of Elimination MDAC Hemodialysis Urine alkalinization Peritoneal dialysis Charcoal hemoperfusion Hemofiltration Plasmapheresis Exchange transfusion Diuresis Chelation Ion Trapping = Urine Alkalinization ASA Barbituates Formic acid (methanol): minor role Methotrexate Chlorpropamide (Diabenese - oral hypoglycemic) HEMODIALYSIS What are features of dialyzable drugs? Low Vd Low protein binding Small molecular weights Water soluble
Single compartment kinetics Low endogenous clearance Adv of hemodialysis over other extracorporeal techniques Corrects acid - base abnormalities Corrects electrolyte abnormalities Removes MORE drug than CRRT (continous hemofiltration) Toxins well removed by HEMODIALYSIS Methanol Ethylene Glycol Isopropranol ASA Lithium Valproic acid Theophyllin
DIALYZABLE OVERDOSES M Methanol E Ethylene Glycol T Theophylline I Isopropranol V Valproic Acid A ASA L Lithium
Possibly effective dialysis Amanita mushroom toxin Tegretol BB: atenolol, sotalol Paraquat Phenytoin Phenobarbital Procainamide Methotrexate
DIAGNOSTIC IMAGING AND TOXICOLOGY
RADIOPAQUE INGESTIONS C Chloral hydrate, Calcium carbonate H Heavy metals (iron, lead, arsenic, lithium, zinc), barium, bisthmus I Iron P Play-doh P Phenothiazines, Potassium chloride E Enteric coated pills D Dental amalgam
ED MANAGEMENT Approach: see ToNotes Decontamination
Ipecac: NO role in ED b/c emesis will only dec absp by 30%. May be indicated for use at the home (2) Gastric Lavage orogastric hose 30 - 40 F infuse 300ml until fluid is clear adv: immediate recovery of gastric material, control lavage duration, direct access for instillation of charcol disadv: invasive, efficacy is questionable a/f 1-2h postingestion, aspiration risk (decreased by trendelenberg) (3) Shower Decrease Absorption (1) Activated Charcol agent of choice for gastrointestinal decontamination in acute may reduce absorption by 50% alone dose: 1g/Kg disadv: poor pt acceptance, messy (5) Cathartics theory: speed up GI motility :. shortening time for absorption but: not shown to improve pt outcome and may increase absortpion disadv: frequent liquid stools, dehydration and lyte imbalances esp in children (6) Whole Bowel Irrigation used in body stuffers and sustained-release or enteridccoated medication overdoses NG tube then goGo-Litely @ 1-2 L/hr until objects
(1)
removed or effluent clear Increased Elimination (1) Dialysis (2) Forced Diuresis (3) Alkalinization of serum TCA example: changing pH from 7.45 to 7.50 increases albumin binding from 95 - 96% of drug :. free drug (which is active) goes from 5% to 4% which is a 20% reduction in the amount of free drug. Alkalinization also changes the intracellular pH and allows the open of H/M ? gates of the Na+ channel and release of the TCA (4) Alkalinization of the urine Ion Trapping of ASA in the urine b/c the alkalinized form is not reabsorbed as well. Supportive Care (1) Oxygen, IV, Monitor (2) Management of Respiratory Complications Airway protection: intubation if necessary Ventilation may be necessary ARDS: high-flow oxygen, +ve pressure ventilation, consider PEEP (3) CV Complications arrythmias as per ACLS hypotension: fluids only (vassopressors rare) hypertension: nitroprusside, CCBs (4) Neuro Complications coma: airway etc seizures: very dangerours, standard tx w/ benzos and phenobarb, paralyzing agents may be needed initially to control prolonged sz (pancuronium) behavioural abnormailities: chemical sedation is dangerous b/c of cardioresp compromise :. use physical restraints if possible: ativan and haloperidol are effective if necessary Diagnostic Studies Drug Screens: urine and blood Routine labs ABGs important Definitive Care Antagonists: see table 129-2, pp740 All poisoned pts should get oxygen, glucose, and naloxozone (narcan) Elimination: example is alkalinization of urine in ASA od
You might also like
- FRCPath Mock 2014 Model AnswersDocument29 pagesFRCPath Mock 2014 Model Answersmonday125No ratings yet
- Ganong - Physiology Self - Assessment Questions - 03Document46 pagesGanong - Physiology Self - Assessment Questions - 03Anonymous 4txA8N8et100% (3)
- Chemistry of CannabisDocument52 pagesChemistry of Cannabisciborg1978No ratings yet
- Chromatography LabDocument9 pagesChromatography Labjtrumpeter224100% (1)
- Poisoning: Overview of Pediatric Poisoning, Diagnosis and Treatment Summary of The Most Encountered PoisoningDocument46 pagesPoisoning: Overview of Pediatric Poisoning, Diagnosis and Treatment Summary of The Most Encountered PoisoningSergey DukkNo ratings yet
- Poisoning Stage V - 2020Document96 pagesPoisoning Stage V - 2020Sarper Hikmet TAZENo ratings yet
- Poisoning PDFDocument124 pagesPoisoning PDFDawn WRein Legaspi67% (3)
- Alcohol ToxicityDocument81 pagesAlcohol ToxicityKarim RezaNo ratings yet
- Toxic Alcohols - High Yields NEJMDocument21 pagesToxic Alcohols - High Yields NEJMDr. Shanojan Thiyagalingam, FRCPC FACPNo ratings yet
- Approach To Poisoned PatientDocument90 pagesApproach To Poisoned PatientGopi KrishnanNo ratings yet
- UMBC CC-EMTP Class Notes, FLCC Class 2010Document93 pagesUMBC CC-EMTP Class Notes, FLCC Class 2010Marc LaBarberaNo ratings yet
- Toxic AlcoholsDocument4 pagesToxic AlcoholsKaran SandhuNo ratings yet
- Dyah Trifianingsih, S. Kep. Ners. M. KepDocument76 pagesDyah Trifianingsih, S. Kep. Ners. M. KepSiprianus S SNo ratings yet
- Alcohol & Glycols: Group # 5 Aranas, Roxette Louraine Ardivilla, Gazel Myrrh Hugo, KevinDocument30 pagesAlcohol & Glycols: Group # 5 Aranas, Roxette Louraine Ardivilla, Gazel Myrrh Hugo, KevinRoxette Louraine R. AranasNo ratings yet
- AlcoholsDocument23 pagesAlcoholsdhaineyNo ratings yet
- Tox CasesDocument7 pagesTox CasesNeo Mervyn Monaheng100% (1)
- Drug Toxicology: Agung Nova Mahendra Department of Pharmacology & Therapy Faculty of Medicine, Udayana UniversityDocument27 pagesDrug Toxicology: Agung Nova Mahendra Department of Pharmacology & Therapy Faculty of Medicine, Udayana Universitywayan lentaraNo ratings yet
- 41 Clinical Cases in Biochemistry UKDocument2 pages41 Clinical Cases in Biochemistry UKAlexandra Ioana MoatarNo ratings yet
- Toxicology Lecture 10 (Chapter 7 Volatiles)Document22 pagesToxicology Lecture 10 (Chapter 7 Volatiles)MowlidAbdirahman Ali madaaleNo ratings yet
- Respiratory Acidosis Is Characterized by An Increase in The pCODocument3 pagesRespiratory Acidosis Is Characterized by An Increase in The pCOMwanja MosesNo ratings yet
- 5 2015 Farmako-ToxicologyDocument71 pages5 2015 Farmako-ToxicologyIkhzan PriolaksanaNo ratings yet
- Chemical Pathology Practical ExamDocument46 pagesChemical Pathology Practical ExamAbdulsamad AfolabiNo ratings yet
- Michael Chansky Acid Base Made Easy HandoutDocument18 pagesMichael Chansky Acid Base Made Easy HandoutTeguh RamadhanNo ratings yet
- Alcohols Ethanol, MethanolDocument55 pagesAlcohols Ethanol, MethanoljayNo ratings yet
- Acid Base Disorders Peter SehaDocument29 pagesAcid Base Disorders Peter SehaPeter SehaNo ratings yet
- Respiratory Assessment FindingsDocument197 pagesRespiratory Assessment Findingsannatw100% (2)
- Adi - IntoxicationDocument52 pagesAdi - IntoxicationAdi WidanaNo ratings yet
- Questions To Consider:: Ethylene Glycol Poisoning. Ethylene Glycol Chemically Occupies A Position Between EthylDocument4 pagesQuestions To Consider:: Ethylene Glycol Poisoning. Ethylene Glycol Chemically Occupies A Position Between EthylJeanette Miña GrajoNo ratings yet
- Anion Gap Metabolic Acidosis: More Then Just A Mud PileDocument21 pagesAnion Gap Metabolic Acidosis: More Then Just A Mud PileFarah SyazanaNo ratings yet
- Management of Poisoned PatientsDocument56 pagesManagement of Poisoned PatientsAmmarah TaimurNo ratings yet
- Acid Base PhysiologyDocument4 pagesAcid Base PhysiologyGhadeer EbraheemNo ratings yet
- ABG Algorithm PDFDocument2 pagesABG Algorithm PDFamin2014No ratings yet
- Module Iii Lab Manual (2024)Document20 pagesModule Iii Lab Manual (2024)ur.yared21No ratings yet
- Rat PoisonDocument41 pagesRat Poisonkhizra mumtazNo ratings yet
- Approach To Acid-Base Problems: DR Frank DalyDocument57 pagesApproach To Acid-Base Problems: DR Frank DalyscanutdNo ratings yet
- Fluid and ElectrolytesDocument14 pagesFluid and Electrolytesstring44100% (2)
- Moderator: Dr. R. K. Yadav (MD) Presented By: Ashish JaisawalDocument47 pagesModerator: Dr. R. K. Yadav (MD) Presented By: Ashish Jaisawalimranqazi11No ratings yet
- Final Exam Focus SheetDocument9 pagesFinal Exam Focus SheetDane WrightNo ratings yet
- Acid-Base Interpretation: APRIL 4, 2017Document9 pagesAcid-Base Interpretation: APRIL 4, 2017mohamedsmnNo ratings yet
- General Principles and Management of PoisonsDocument5 pagesGeneral Principles and Management of PoisonsOkpetah Chioma christabelNo ratings yet
- Drug OverdoseDocument94 pagesDrug Overdosemicheal1960No ratings yet
- Student Tox LectureDocument49 pagesStudent Tox Lecturelenin_villaltaNo ratings yet
- ABG MMHG InterpretationDocument92 pagesABG MMHG InterpretationManmeet SNo ratings yet
- Acid Base Disorders DR Kwaifa - PPTX 1Document99 pagesAcid Base Disorders DR Kwaifa - PPTX 1DICKSONNo ratings yet
- Ethylene Glycol Toxicosis in Animals - Toxicology - MSD Veterinary ManualDocument6 pagesEthylene Glycol Toxicosis in Animals - Toxicology - MSD Veterinary ManualMuhammad AgussalimNo ratings yet
- Synthesis Final ReviewDocument20 pagesSynthesis Final ReviewSamNo ratings yet
- Poisoning in ChildrenDocument11 pagesPoisoning in ChildrenAndriana HalfienNo ratings yet
- Body Fluids and ElectrolytesDocument42 pagesBody Fluids and ElectrolytesQusaiBadr100% (1)
- Tugas GinjalDocument22 pagesTugas GinjalAnastasia MargaretNo ratings yet
- Acid Base EquationsDocument21 pagesAcid Base EquationsBen JonesNo ratings yet
- Assignment: ToxicologyDocument8 pagesAssignment: ToxicologyAyesha LiaqatNo ratings yet
- Anion Gap Metabolic Acidemia Case BasedDocument4 pagesAnion Gap Metabolic Acidemia Case Basedspiros.a.markouNo ratings yet
- Case Report: An Unconscious Man With Profound Drug-Induced HypoglycaemiaDocument6 pagesCase Report: An Unconscious Man With Profound Drug-Induced Hypoglycaemiagevowo3277No ratings yet
- Acute Poisoning of Therapeutic Agents: by Alemayehu TomaDocument42 pagesAcute Poisoning of Therapeutic Agents: by Alemayehu TomaYohannis AsefaNo ratings yet
- Mnemonics: Do Not Adsorb To CharcoalDocument25 pagesMnemonics: Do Not Adsorb To CharcoalJiaYee GoNo ratings yet
- ABG Interpretation 1Document59 pagesABG Interpretation 1Sura KwakNo ratings yet
- Chapter Four: Chemical Analysis of UrineDocument174 pagesChapter Four: Chemical Analysis of UrineRebuma BeleteNo ratings yet
- AlcohoDocument32 pagesAlcohoVaibhav KaroliyaNo ratings yet
- Enzyme-summary (1)Document7 pagesEnzyme-summary (1)Aira Jane GamboaNo ratings yet
- ELECTROLYTES (Na & K)Document3 pagesELECTROLYTES (Na & K)Alondra SagarioNo ratings yet
- Alcohol Toxicity PDFDocument20 pagesAlcohol Toxicity PDFNabila Fatmayday UdiyahNo ratings yet
- The Impact Of Alcohol On The Brain - Based On The Teachings Of Dr. Andrew Huberman: Examining The Complex Interplay Between Alcohol And NeurobiologyFrom EverandThe Impact Of Alcohol On The Brain - Based On The Teachings Of Dr. Andrew Huberman: Examining The Complex Interplay Between Alcohol And NeurobiologyNo ratings yet
- Pass Paces EbDocument10 pagesPass Paces EbAnonymous 4txA8N8etNo ratings yet
- H IsselbacherDocument5 pagesH IsselbacherAnonymous 4txA8N8etNo ratings yet
- Topics Runtime: Subjects AnatomyDocument2 pagesTopics Runtime: Subjects AnatomyAnonymous 4txA8N8etNo ratings yet
- Hp165-02b-Nash (FF 050816v) ProtegidoDocument9 pagesHp165-02b-Nash (FF 050816v) ProtegidoAnonymous 4txA8N8etNo ratings yet
- Adpkd: Autosomal Dominant Polycystic Kidney DiseaseDocument7 pagesAdpkd: Autosomal Dominant Polycystic Kidney DiseaseAnonymous 4txA8N8etNo ratings yet
- Hanzi Pinyin English: HSK Level 2Document5 pagesHanzi Pinyin English: HSK Level 2Anonymous 4txA8N8etNo ratings yet
- Genetics 50qDocument62 pagesGenetics 50qAnonymous 4txA8N8etNo ratings yet
- Radiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedDocument1 pageRadiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedAnonymous 4txA8N8etNo ratings yet
- 6 Steps in Assisting in Cardiac Rhythm InterpretationDocument1 page6 Steps in Assisting in Cardiac Rhythm InterpretationAnonymous 4txA8N8etNo ratings yet
- EMQExample RacpDocument5 pagesEMQExample RacpAnonymous 4txA8N8etNo ratings yet
- Brunicardi-1996-Time Management - A RDocument7 pagesBrunicardi-1996-Time Management - A RAnonymous 4txA8N8etNo ratings yet
- Abdominal Exam DATEDocument3 pagesAbdominal Exam DATEAnonymous 4txA8N8etNo ratings yet
- Effective Feedback Skills: Sally Santen MD, PHDDocument9 pagesEffective Feedback Skills: Sally Santen MD, PHDAnonymous 4txA8N8etNo ratings yet
- Lymphoproliferative Disorders Part 2Document7 pagesLymphoproliferative Disorders Part 2Anonymous 4txA8N8etNo ratings yet
- Previous PLE QuestionsDocument3 pagesPrevious PLE QuestionsGrace Benero Pequero0% (1)
- Analytical Methods For Amino Acid Determination in OrganismsDocument18 pagesAnalytical Methods For Amino Acid Determination in OrganismsVeneta GizdakovaNo ratings yet
- A General Procedure For Mitsunobu Inversion of Sterically Hindered Alcohols - Inversion of Menthol. (1S, 2S, 5R) - 5-Methyl-2 - (1-Methylethyl) Cyclohexyl 4-Nitrobenzoate PDFDocument4 pagesA General Procedure For Mitsunobu Inversion of Sterically Hindered Alcohols - Inversion of Menthol. (1S, 2S, 5R) - 5-Methyl-2 - (1-Methylethyl) Cyclohexyl 4-Nitrobenzoate PDFthamtusieuquayNo ratings yet
- Oxford GR 10 Topic 1 Matter & ClassificationDocument54 pagesOxford GR 10 Topic 1 Matter & ClassificationkhotsoNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaAudry YuniarNo ratings yet
- Uncertainty Related To The Use Of: Relative Retention Times in Pharmaceutical AnalysisDocument7 pagesUncertainty Related To The Use Of: Relative Retention Times in Pharmaceutical AnalysisnmmMJKJNo ratings yet
- Gas Chromatography, GCDocument85 pagesGas Chromatography, GCShaise Jacob67% (3)
- Adenosine Injection: 2348 Adenosine / Official Monographs USP 39Document2 pagesAdenosine Injection: 2348 Adenosine / Official Monographs USP 39Luz De MarNo ratings yet
- Science7 Q1 WK5Document3 pagesScience7 Q1 WK5hannahsofiapreyesNo ratings yet
- PrefaceDocument566 pagesPrefaceNurlaini NasutionNo ratings yet
- Poster B12Document1 pagePoster B12Vikas GoyalNo ratings yet
- New Trends in Forced Degradation StudiesDocument10 pagesNew Trends in Forced Degradation StudiesLina SakellariouNo ratings yet
- HPLC Column Phenomenex LunaDocument34 pagesHPLC Column Phenomenex LunaShiraz Khan0% (1)
- Separation, Electroanalytical and Spectrometric TechniquesDocument115 pagesSeparation, Electroanalytical and Spectrometric TechniquesRicardo SimõesNo ratings yet
- Chromatography PharmacyDocument41 pagesChromatography PharmacyfarisaNo ratings yet
- Analytical Tasks - Efficiently Solved by HPTLC: Camag Bibliography ServiceDocument68 pagesAnalytical Tasks - Efficiently Solved by HPTLC: Camag Bibliography ServiceDarian HerascuNo ratings yet
- MS Solutions: Tech TipDocument11 pagesMS Solutions: Tech TipKelumNo ratings yet
- Extension of The QuEChERS Method For Pesticide Residues Cereals, PeanutsDocument9 pagesExtension of The QuEChERS Method For Pesticide Residues Cereals, PeanutsrumitpashaNo ratings yet
- International Biodeterioration & Biodegradation: Daiyong Deng, Jun Guo, Guoqu Zeng, Guoping SunDocument7 pagesInternational Biodeterioration & Biodegradation: Daiyong Deng, Jun Guo, Guoqu Zeng, Guoping SunVenny SandjajaNo ratings yet
- ICW-3000 Water Purification System - MerckmilliporeDocument2 pagesICW-3000 Water Purification System - MerckmilliporeMerck IndiaNo ratings yet
- HPLC 2015Document102 pagesHPLC 2015Ojan FauzanNo ratings yet
- Applications of High Performance Liquid ChromatographyDocument3 pagesApplications of High Performance Liquid ChromatographyKavisa GhoshNo ratings yet
- Course Outline CEV444 (Sep 2017-Jan 2018)Document7 pagesCourse Outline CEV444 (Sep 2017-Jan 2018)Solehah OmarNo ratings yet
- Cbiescco 02Document7 pagesCbiescco 02Rishabh Bhati100% (1)
- pdf01 PDFDocument44 pagespdf01 PDFRafi IqbalNo ratings yet
- Kelebihan Kekurangan Kromatografi KolomDocument8 pagesKelebihan Kekurangan Kromatografi KolomFendy FendyNo ratings yet
- High Performance Liquid Chromatography (HPLC) : Presenter: Nandit P BDocument39 pagesHigh Performance Liquid Chromatography (HPLC) : Presenter: Nandit P BNandit BanawalikarNo ratings yet
- s00226 018 1057 3Document15 pagess00226 018 1057 3Aeric HalzNo ratings yet