Professional Documents
Culture Documents
Low 25-Hydroxyvitamin D and Risk of Type 2 Diabetes: A Prospective Cohort Study and Metaanalysis
Low 25-Hydroxyvitamin D and Risk of Type 2 Diabetes: A Prospective Cohort Study and Metaanalysis
Uploaded by
fniegas172Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Low 25-Hydroxyvitamin D and Risk of Type 2 Diabetes: A Prospective Cohort Study and Metaanalysis
Low 25-Hydroxyvitamin D and Risk of Type 2 Diabetes: A Prospective Cohort Study and Metaanalysis
Uploaded by
fniegas172Copyright:
Available Formats
Low 25-Hydroxyvitamin D and Risk of Type 2 Diabetes: A Prospective Cohort Study and Metaanalysis Shoaib Afzal1, Stig E.
Bojesen, and Brge G. Nordestgaard.
ABSTRACT: BACKGROUND: Vitamin D deficiency has been implicated in decreased insulin secretion and increased insulin resistance, hallmarks of type 2 diabetes mellitus. We tested the hypothesis that low plasma 25-hydroxyvitamin D [25(OH)D] is associated with increased risk of type 2 diabetes in the general population. METHODS: We measured 25(OH)D in 9841 participants from the general population, of whom 810 developed type 2 diabetes during 29 years of follow-up. Analyses were adjusted for sex, age, smoking status, body mass index, income, physical activity, HDL cholesterol, and calendar month of blood draw. RESULTS: Lower 25(OH)D concentrations, by clinical categories or seasonally adjusted quartiles, were associated with higher cumulative incidence of type 2 diabetes (trend, P = 2107 and P = 41010). Multivariable adjusted hazard ratios of type 2 diabetes were 1.22 (95% CI 0.851.74) for 25(OH)D <5 vs 20 g/L and 1.35 (1.09 1.66) for lowest vs highest quartile. Also, the multivariable adjusted hazard ratio of type 2 diabetes for a 50% lower concentration of 25(OH)D was 1.12 (1.03 1.21); the corresponding hazard ratio for those 58 years old was 1.26 (1.151.41). Finally, in a metaanalysis of 16 studies, the odds ratio for type 2 diabetes was 1.50 (1.33 1.70) for the bottom vs top quartile of 25(OH)D. CONCLUSIONS: We observed an association of low plasma 25(OH)D with increased risk of type 2 diabetes. This finding was substantiated in a metaanalysis.
Received for publication July 12, 2012. Accepted for publication October 31, 2012 2012 The American Association for Clinical Chemistry
Prognostic Utility of Secretory Phospholipase A2 in Patients with Stable Coronary Artery Disease
Michelle L. O'Donoghue, Ziad Mallat, David A. Morrow, Joelle Benessiano, Sarah Sloan, Torbjrn Omland, Scott D. Solomon, Eugene Braunwald, Alain Tedgui, and Marc S. Sabatine.
ABSTRACT:
BACKGROUND: Secretory phospholipase A2 (sPLA2) may contribute to atherogenesis. To date, few prospective studies have examined the utility of sPLA 2 for risk stratification in coronary artery disease (CAD). The phospholipase A2 enzymes are members of a large family that hydrolyze the sn-2 ester of glycerophospholipids to release free fatty acids and lysophospholipids. The secretory phospholipase A2 (sPLA2)7 family consists of 10 isoenzymes that are involved in a variety of biological processes that include hydrolysis of phospholipids, release of arachidonic acid, and eicosanoid generation (1). sPLA2 enzymes are distinct from lipoprotein-associated phospholipase A2 (Lp-PLA2), another biomarker that has been extensively studied for risk stratification and is now being evaluated as a potential therapeutic target (2). Growing evidence suggests that sPLA2 may play a causal role in the development of atherosclerosis. sPLA2-X has been shown to promote macrophage foam cell formation in murine models (3), and upregulated sPLA2-IIA or sPLA2-V expression has been shown to increase atherosclerotic lesion size in transgenic mice (4, 5). Additionally, genetic deletion of sPLA2-V or direct inhibition of sPLA2 activity has been shown to reduce atherosclerotic lesion progression in animals (5,,7). To date, a small number of studies have evaluated the utility of sPLA 2 for risk stratification in primary prevention populations and in patients with acute coronary syndrome (ACS) (1). However, the prognostic utility of sPLA2 activity has not been well established in a large population of patients with stable coronary artery disease (CAD). Determination of this association is particularly relevant given the interest in sPLA2 as a possible therapeutic target for helping to delay the progression of atherosclerosis (8). Furthermore, the relative prognostic utility of sPLA2 compared with other wellestablished markers of risk, including those measured using new high-sensitivity assays, remains unknown. We hypothesized that sPLA2 activity would provide incremental information for risk stratification beyond established clinical risk factors and biomarkers in a large cohort of subjects with stable CAD.
METHODS: We measured plasma sPLA2 activity at baseline in 3708 subjects in the PEACE randomized trial of trandolapril vs placebo in stable CAD. Median follow-up was 4.8 years. We used Cox regression to adjust for demographics, clinical risk factors, apolipoprotein B, apolipoprotein A1, and medications.
RESULTS: After multivariable adjustment, sPLA2 was associated with an increased risk of cardiovascular death, myocardial infarction, or stroke (adjusted hazard ratio Q4:Q1 1.55, 95% CI 1.132.14) and cardiovascular death or heart failure (1.91, 1.203.03). In further multivariable assessment, increased activity levels of sPLA2 were associated with the risk of cardiovascular death, myocardial infarction, or stroke (adjusted hazard ratio 1.47, 95% CI 1.062.04), independent of lipoprotein-associated phospholipase A2 mass and C-reactive protein, and modestly improved the area under the curve (AUC) beyond established clinical risk factors (AUC 0.6680.675, P = 0.01). sPLA2, N-terminal pro-B-type natriuretic peptide, and high-sensitivity cardiac troponin T all were independently associated with cardiovascular death or heart failure, and each improved risk discrimination (P = 0.02, P < 0.001, P < 0.001, respectively). CONCLUSIONS: sPLA2 activity provides independent prognostic information beyond established risk markers in patients with stable CAD. These data are encouraging for studies designed to evaluate the role of sPLA2 as a therapeutic target. Received for publication March 31, 2011. Accepted for publication June 29, 2011. 2011 The American Association for Clinical Chemistry
Determination of Antimicrobial Resistance Pattern and Production of ExtendedSpectrum -Lactamases amongst Esche-richia coli and Klebsiella pneumoniae from Clinical Isolates Anand Kalaskar, Kandi Vramana ABSTRACT: Background: The prevalence of antibiotic resistance among extended-spectrum lactamase (ESBL) producing Escherichia coliand Klebsiella pneumoniae has been increased markedly in recent years. The present study was done to know the prevalence of ESBL production among isolates of E. coli and K. pneumoniae and to study the susceptibility pattern of isolates against different antibiotics. Methods: Extended-spectrum -lactamase producing E. coli and K. pneumoniae were isolated from various samples obtained from outdoor and indoor patients of the Prathima Institute of medical sciences, Andhra Pradesh, India. They were tested for ESBL production by double disc synergy test and resistance to various antibiotics like fluoroquinolones, cephalosporins, aminoglycosides and -lactamase inhibitor combinations and susceptibility to carbapenems were determined by Kirby-Bauer disc diffusion method. Results: A total of 94 ESBL producing isolates were obtained. Of them 60 were E. coli and 34 K. pneumoniae. They were obtained from urine, sputum, pus, wound swabs blood & tracheal aspirates. Urine (38.29%) was the main source of ESBL-producing isolates from all patients, followed by sputum (34.04%). About 37.23% of these isolates were collected from medical wards and 27.65% were collected from outdoor. All isolates were susceptible to imipenem. The resistance to cephalosporins (1-4 generations) was almost 100%. Resistance to Aztreonam, Ampicillin and Co-amoxyclav was also 100%. A high degree of resistance was observed to other antibiotics. Conclusion: The highest prevalence of resistance to ESBL in E. coli and K. pneumonia is associated with a multitude of infections in hospitalized patients with a significant longer duration of hospital stay, increased morbidity and greater hospital charges. Advanced drug resistance surveillance and molecular characteristics of ESBL isolates is necessary to guide the proper and judicious antibiotic use.
You might also like
- Intentional Interviewing and Counseling Facilitating Client Development in A Multicultural Society 9th Edition Ebook PDF VersionDocument62 pagesIntentional Interviewing and Counseling Facilitating Client Development in A Multicultural Society 9th Edition Ebook PDF Versionteresa.vanhorn90798% (55)
- Hkls SurveyquestDocument2 pagesHkls SurveyquestRuben AntonioNo ratings yet
- Philippine Health Care Delivery SystemDocument42 pagesPhilippine Health Care Delivery Systemfniegas172100% (5)
- Legal Foundations of Philippine EducationDocument2 pagesLegal Foundations of Philippine Educationfniegas17275% (4)
- Leaders On LeadershipDocument189 pagesLeaders On Leadershipfniegas172No ratings yet
- Intercession - A ManualDocument40 pagesIntercession - A Manualfniegas172100% (8)
- Serum Concentrations of Adiponectin and Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease in Apparently Healthy Middle-Aged MenDocument15 pagesSerum Concentrations of Adiponectin and Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease in Apparently Healthy Middle-Aged MenEcha MagungNo ratings yet
- Ijms-22-00287Document10 pagesIjms-22-00287vidhi parekhNo ratings yet
- Jrip 3 31Document4 pagesJrip 3 31Shivpartap SinghNo ratings yet
- DM Nefro3Document10 pagesDM Nefro3Teddy Alexander MorinNo ratings yet
- Lpa ReclassificationDocument10 pagesLpa ReclassificationersilvermanNo ratings yet
- Dia Care-1992-Ganda-1245-50Document6 pagesDia Care-1992-Ganda-1245-50Heru MurdiantoNo ratings yet
- Diabetes Obesity Metabolism - 2023 - McGuire - Effects of Oral Semaglutide On Cardiovascular Outcomes in Individuals WithDocument10 pagesDiabetes Obesity Metabolism - 2023 - McGuire - Effects of Oral Semaglutide On Cardiovascular Outcomes in Individuals Withivan dario hernandez erazoNo ratings yet
- Aceves Ramirez2022Document8 pagesAceves Ramirez2022Diana MartinezNo ratings yet
- 4 - 2015serum Lipoprotein (A) Concentrations Are Inversely Associated With T2D, Prediabetes, and Insulin ResDocument10 pages4 - 2015serum Lipoprotein (A) Concentrations Are Inversely Associated With T2D, Prediabetes, and Insulin Resjef5525No ratings yet
- 2015 Takeuchi BMCPediatricsDocument9 pages2015 Takeuchi BMCPediatricsEduardo PasteneNo ratings yet
- Artículo Dislipemia ESCDocument12 pagesArtículo Dislipemia ESCSMIBA MedicinaNo ratings yet
- Cardiovascular Benefit of Empagliflozin Across The Spectrum of Cardiovascular Risk Factor Control in The Empa-Reg Outcome TrialDocument11 pagesCardiovascular Benefit of Empagliflozin Across The Spectrum of Cardiovascular Risk Factor Control in The Empa-Reg Outcome TrialBaginda Yusuf SiregarNo ratings yet
- ,content, 31,2,361 FullDocument2 pages,content, 31,2,361 FullMilka MimingNo ratings yet
- Vitamin D Levels Predict All-Cause and Cardiovascular Disease Mortality in Subjects With The Metabolic SyndromeDocument7 pagesVitamin D Levels Predict All-Cause and Cardiovascular Disease Mortality in Subjects With The Metabolic SyndromeAgafioNo ratings yet
- Research ArticleDocument9 pagesResearch Articleinterna unpadNo ratings yet
- Cardiovascular Outcomes StudiesDocument5 pagesCardiovascular Outcomes StudiesAnonymous LOeICSOqNo ratings yet
- SUultima EvidenciaDocument8 pagesSUultima Evidenciasalvado moyanoNo ratings yet
- Ao - FR CV Les Arp2010Document8 pagesAo - FR CV Les Arp2010Taskina Akhter TomaNo ratings yet
- Association Between Serum Interleukin (IL) - 12 Level and Severity of Non-Alcoholic Fatty Liver Disease (NAFLD)Document16 pagesAssociation Between Serum Interleukin (IL) - 12 Level and Severity of Non-Alcoholic Fatty Liver Disease (NAFLD)Samuel SimanjuntakNo ratings yet
- Lower Heart Rate Variability Is Associated With Higher Plasma Concentrations of IL-6 in Type 1 DiabetesDocument8 pagesLower Heart Rate Variability Is Associated With Higher Plasma Concentrations of IL-6 in Type 1 DiabetesVanathy KarunamoorthyNo ratings yet
- Dia Care-2005-Sever-1151-7Document7 pagesDia Care-2005-Sever-1151-7Barbara Sakura RiawanNo ratings yet
- Semaglutide and Cardiovascular Outcomes in Patients With Type 2 DiabetesDocument11 pagesSemaglutide and Cardiovascular Outcomes in Patients With Type 2 DiabetesFhirastika AnnishaNo ratings yet
- Efficacy of Supplementary Vitamin D On Improvement of Glycemic Parameters in Patients With Type 2 Diabetes Mellitus A..Document5 pagesEfficacy of Supplementary Vitamin D On Improvement of Glycemic Parameters in Patients With Type 2 Diabetes Mellitus A..ariahenkusNo ratings yet
- MGvol81.2011 25Document8 pagesMGvol81.2011 25eminacengic5851No ratings yet
- Emailing Expression of KGF-1 and KGF-2 in Skin Wounds ADocument12 pagesEmailing Expression of KGF-1 and KGF-2 in Skin Wounds ARimaWulansariNo ratings yet
- Predicting and Preventing Autoimmunity, Myth or Reality?: Michal Harel and Yehuda ShoenfeldDocument24 pagesPredicting and Preventing Autoimmunity, Myth or Reality?: Michal Harel and Yehuda ShoenfeldPollyanna MenezesNo ratings yet
- 302 Cardiovascular Risk: AssessmentDocument1 page302 Cardiovascular Risk: AssessmentLêHữuHoàiNo ratings yet
- LeaderDocument12 pagesLeaderMoeez AkramNo ratings yet
- R230C But Not 565C - T VariantDocument11 pagesR230C But Not 565C - T VariantRogelio MoscosoNo ratings yet
- 1 s2.0 S2213177917305358 MainDocument10 pages1 s2.0 S2213177917305358 MainMayar HassanNo ratings yet
- 2015 Article 215Document15 pages2015 Article 215alerta.bfcmNo ratings yet
- Correlation of Dyslipidemia and Type 2 Diabetes Mellitus Amongst The People of Vidarbha Region of IndiaDocument6 pagesCorrelation of Dyslipidemia and Type 2 Diabetes Mellitus Amongst The People of Vidarbha Region of IndiaKiki FatmawatyNo ratings yet
- 1956.full 2Document9 pages1956.full 2Jauhar FirdausNo ratings yet
- Risk Factors, Mortality, and Cardiovascular Outcomes in Patients With Type 2 DiabetesDocument12 pagesRisk Factors, Mortality, and Cardiovascular Outcomes in Patients With Type 2 DiabetesAnnisa FujiantiNo ratings yet
- Paper13 PDFDocument6 pagesPaper13 PDFSekar MentariNo ratings yet
- DM Tipe 2Document5 pagesDM Tipe 2Septian PutraNo ratings yet
- Marina Eloi, Daniela Vargas Horvath, João Carlos Ortega, Monica Simon Prado, Luis Eduardo Coelho Andrade, Et AlDocument2 pagesMarina Eloi, Daniela Vargas Horvath, João Carlos Ortega, Monica Simon Prado, Luis Eduardo Coelho Andrade, Et AlSitha WisesaNo ratings yet
- New and Emerging Biomarkers in Cardiovascular DiseaseDocument15 pagesNew and Emerging Biomarkers in Cardiovascular DiseaseSerendipity21No ratings yet
- Using The EQ-5D Index Score As A Predictor of Outcomes in Patients With Type 2 Diabetes - Clarke May08Document20 pagesUsing The EQ-5D Index Score As A Predictor of Outcomes in Patients With Type 2 Diabetes - Clarke May08Haneesha MuddasaniNo ratings yet
- 02.2012 ADA LB Abstracts - CovDocument55 pages02.2012 ADA LB Abstracts - CovEndang SetiawatiNo ratings yet
- Lixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeDocument11 pagesLixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeMoeez AkramNo ratings yet
- 51-Article Text-179-1-10-20100404Document6 pages51-Article Text-179-1-10-20100404MUHAMMAD FARHABNo ratings yet
- Hyperbilirubinemia: A Risk Factor For Infection in The Surgical Intensive Care UnitDocument14 pagesHyperbilirubinemia: A Risk Factor For Infection in The Surgical Intensive Care UnitChristian Karl B. LlanesNo ratings yet
- 2.5 Overview of Cardiovascular SafetyDocument3 pages2.5 Overview of Cardiovascular SafetyKamalia LayalNo ratings yet
- Anti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsDocument5 pagesAnti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsBarbara Sakura RiawanNo ratings yet
- Terjemahan JurnalDocument13 pagesTerjemahan JurnalIqhe Harsono SyastrowinotoNo ratings yet
- 2015 Article 244Document8 pages2015 Article 244nasar adenNo ratings yet
- Cushing SubDocument7 pagesCushing SubClaudia IrimieNo ratings yet
- Lixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeDocument11 pagesLixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeAndi Soraya PurnamandaNo ratings yet
- Bahan Semiloka LitbangDocument15 pagesBahan Semiloka LitbangArumrukmasariNo ratings yet
- Glycosylated Haemoglobin and Lipid Profile Pattern For Hypertensive-Diabetics in Port HarcourtDocument8 pagesGlycosylated Haemoglobin and Lipid Profile Pattern For Hypertensive-Diabetics in Port Harcourtijmb333No ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofAlina PirtacNo ratings yet
- Oup Accepted Manuscript 2020Document11 pagesOup Accepted Manuscript 2020Luis Bonino SanchezNo ratings yet
- UKPDS36Document8 pagesUKPDS36Siskawati SuparminNo ratings yet
- Original Article Evaluation of Dyslipidaemia in Type 2 Diabetes Mellitus PatientsDocument6 pagesOriginal Article Evaluation of Dyslipidaemia in Type 2 Diabetes Mellitus PatientsEnvhy AmaliaNo ratings yet
- Cardiovascular Risk in Clopidogrel-Treated Patients According To Cytochrome P450 2C19 2 Loss-of-Function Allele or Proton Pump Inhibitor CoadministrationDocument10 pagesCardiovascular Risk in Clopidogrel-Treated Patients According To Cytochrome P450 2C19 2 Loss-of-Function Allele or Proton Pump Inhibitor CoadministrationVenansius ReinaldiNo ratings yet
- Genetically Elevated LDL Associates With Lower Risk of Intracerebral HemorrhageDocument11 pagesGenetically Elevated LDL Associates With Lower Risk of Intracerebral HemorrhageRachtipatPitiwararomNo ratings yet
- 25-Hydroxyvitamin D Is Associated With Adiposity andDocument23 pages25-Hydroxyvitamin D Is Associated With Adiposity andRenata NunanNo ratings yet
- Therapeutic LipidologyFrom EverandTherapeutic LipidologyMichael H. DavidsonNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- Lg. Washing Machine - Mfl39760206 - Cube - 7 - Pro-T65Document68 pagesLg. Washing Machine - Mfl39760206 - Cube - 7 - Pro-T65fniegas172No ratings yet
- 30 Consistent Traits of The JezebelDocument7 pages30 Consistent Traits of The Jezebelfniegas172No ratings yet
- Giving Testimonies: Making God-Glorifying TestimoniesDocument6 pagesGiving Testimonies: Making God-Glorifying Testimoniesfniegas172No ratings yet
- Unless The LORD Builds The House: Heritage RewardDocument6 pagesUnless The LORD Builds The House: Heritage Rewardfniegas172No ratings yet
- Our Heart, Our Desire Is To See The Nations Worship. Our Cry, Our Prayer Is To Sing Your Praise To The Ends of The EarthDocument2 pagesOur Heart, Our Desire Is To See The Nations Worship. Our Cry, Our Prayer Is To Sing Your Praise To The Ends of The Earthfniegas172No ratings yet
- Claps: 1. Wow 2. Pacquiao 3. Rainbow 4. Raise The Roof 5Document1 pageClaps: 1. Wow 2. Pacquiao 3. Rainbow 4. Raise The Roof 5fniegas172No ratings yet
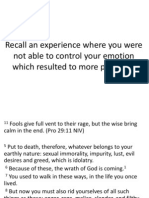
- Recall An Experience Where You Were Not Able To Control Your Emotion Which Resulted To More ProblemsDocument3 pagesRecall An Experience Where You Were Not Able To Control Your Emotion Which Resulted To More Problemsfniegas172No ratings yet
- Bless Our Cops Servant Leaders SurveyDocument4 pagesBless Our Cops Servant Leaders Surveyfniegas172No ratings yet
- RICE. Becoming The Fat GirlDocument288 pagesRICE. Becoming The Fat GirlNina NavajasNo ratings yet
- Soal Persiapan Ulangan Bersama Semester 2 Kelas Xi 2021Document7 pagesSoal Persiapan Ulangan Bersama Semester 2 Kelas Xi 2021Fauzan NaufalNo ratings yet
- Jurnal Keperawatan Muhammadiyah: Pipit Festi Wiliyanarti, Lusinta Dwi Kurniawati, Gita MariniDocument7 pagesJurnal Keperawatan Muhammadiyah: Pipit Festi Wiliyanarti, Lusinta Dwi Kurniawati, Gita Marinihepi nopita sariNo ratings yet
- Coronavirus Pandemic PEST AnalysisDocument2 pagesCoronavirus Pandemic PEST AnalysisAneliya ShterevaNo ratings yet
- What Philippine Law Was Created To Include in It The Code of Ethics of Filipino Nurses?Document3 pagesWhat Philippine Law Was Created To Include in It The Code of Ethics of Filipino Nurses?Shirlene Benigra GorospeNo ratings yet
- TeleHealth Lecture NotesDocument40 pagesTeleHealth Lecture NotesKarthik100% (3)
- SDS PAC LiquidDocument4 pagesSDS PAC LiquidQuality AssuranceNo ratings yet
- Important Questions Answers Why This Matters:: (G4056/P2509) (G4057/P2509)Document8 pagesImportant Questions Answers Why This Matters:: (G4056/P2509) (G4057/P2509)JskNo ratings yet
- NCM 107Document7 pagesNCM 107FERNANDEZ, RELLY ANDREWNo ratings yet
- The Given Charts Give Information About The Number of Students at University in The UK From 1991 To 2001Document5 pagesThe Given Charts Give Information About The Number of Students at University in The UK From 1991 To 2001vldhhdvdNo ratings yet
- Complex Regional Pain SyndromeDocument24 pagesComplex Regional Pain SyndromeJanine RustNo ratings yet
- Formato de GlosarioDocument19 pagesFormato de GlosarioArturo Saavedra VargasNo ratings yet
- AIDS Foundation of Chicago - Annual Report 2015Document24 pagesAIDS Foundation of Chicago - Annual Report 2015AdamAce VelasquezNo ratings yet
- OsteoarthritisDocument37 pagesOsteoarthritisChikezie Onwukwe100% (1)
- Natural ResourcesDocument5 pagesNatural ResourcessandeepNo ratings yet
- Assessment of Adolescent Self-HarmDocument7 pagesAssessment of Adolescent Self-HarmWilson Javier Dominguez PerezNo ratings yet
- 19 Disaster SurgeryDocument45 pages19 Disaster SurgeryAhmed noor Ahmed noorNo ratings yet
- Tripping Over The Truth: How The Metabolic Theory of Cancer Is Overturning One of Medicine's Most Entrenched Paradigms - Travis ChristoffersonDocument5 pagesTripping Over The Truth: How The Metabolic Theory of Cancer Is Overturning One of Medicine's Most Entrenched Paradigms - Travis Christoffersonwehyryji0% (1)
- Alyssa TriageDocument2 pagesAlyssa TriageJim Claude Battad JovenNo ratings yet
- General Medicine: Open AccessDocument3 pagesGeneral Medicine: Open AccessPeter jörgNo ratings yet
- Prevalence of Rifampicin Resistance Tuberculosis and Associated Factors Among Presumptive TB or MDRDocument3 pagesPrevalence of Rifampicin Resistance Tuberculosis and Associated Factors Among Presumptive TB or MDRTigray OutlookNo ratings yet
- Chapter IiDocument8 pagesChapter IiWorld LyricsNo ratings yet
- Guideline For Community-Based Treatment and Care Services For People Affected by Drug Use and Dependence in Southeast AsiaDocument23 pagesGuideline For Community-Based Treatment and Care Services For People Affected by Drug Use and Dependence in Southeast AsiaAgZawNo ratings yet
- Assessing-the-Impact-of-a-Community 3Document18 pagesAssessing-the-Impact-of-a-Community 3harfridzkhail.haddaraniNo ratings yet
- Republic of The Philippines Professional Regulation Commission ManilaDocument2 pagesRepublic of The Philippines Professional Regulation Commission ManilaNOr JOeNo ratings yet
- Book - OT Manager - Chap 57 Organizational EthicsDocument9 pagesBook - OT Manager - Chap 57 Organizational EthicsWhitney JosephNo ratings yet
- Self-Declaration Form - STUDIODocument2 pagesSelf-Declaration Form - STUDIOLeticia BikaerNo ratings yet
- USOR Annual Report 2011Document54 pagesUSOR Annual Report 2011State of UtahNo ratings yet