Professional Documents
Culture Documents
Bupivacaine
Bupivacaine
Uploaded by
Krystel Joy AuroOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bupivacaine
Bupivacaine
Uploaded by
Krystel Joy AuroCopyright:
Available Formats
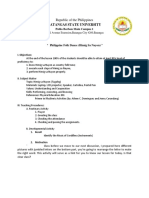
West Visayas State University COLLEGE OF NURSING La Paz, Iloilo City DRUG STUDY Attending Physician: Dr. B.L.J.
Impression / Diagnosis: Diabetes Mellitus Foot Wagner IV Right; S/P Below Knee Amputation Right Indication Local or regional anesthesia or analgesia for surgical, obstetric, or diagnostic procedures Contraindications Hypersensitivity; cross sensitivity with other amide local anesthetics may occur; Bupivacaine contains bisulfites and should be avoided in patients with known Adverse Reactions Seizure, Cardiovascular collapse, Respiratory arrest, Special Nursing Responsibilities Precautions concurrent use of Assessment other local 1. Systemic Toxicity: anesthetics; Liver Assess for systemic disease; toxicity Concurrent use of (circumoral anticoagulants tingling and (including lownumbness, ringing dose heparin and in ears, metallic anesthetics; Liver taste, dizziness, disease; blurred vision, Concurrent use of tremors, slow anticoagulants speech, irritability, (including lowtwitching, seizures, dose heparin/ cardiac heprinoids) dysrhythmias) each shift. Report to physician or other health care professional. 2. Orthostatic Hypotension:
Name of Patient: N.E.P Age: 46 years old Ward/Bed Number: Room 408
Name of Drug Generic: Bupivacaine Hydrochloride Brand:
Dosage, Route, Frequency, and Timing Dosage:
Mechanism of Action Local anesthetics inhibit initiation and conduction of sensory nerve impulses by altering the influx of sodium and efflux of potassium in neurons, slowing or stopping pain transmission. Epidural administration allows action to take place at the level of the spinal nerve roots immediately adjacent to the site of administration. The catheter is placed as close as possible to the dermatomes (skin surface areas innervated by a single spinal nerve or group of spinal nerves)
Route:
Frequency: Sensorcaine Timing: Classification Functional: Epidural local anesthetics Chemical:
Side Effects BP, bradycardia, dizziness, anxiety,
restlessness,
that, when blocked, will produce effective spread of analgesia for the site of injury. Therapeutic Effects: Decreased pain or induction of anesthesia; low doses have minimal effect on sensory or motor function; higher doses may produce complete motor blockade Source: Deglin J.H., Vallerand A.H (2008) ; Drug Guide for Nurses 11th Edition; F.A. Davis Company; Pages 478480
intolerance. Decreased BP, shock & arrhythmias, local infections at anesthesia site,
3.
Monitor blood pressure, heart rate, and respiratory rate continuously while patient is receiving this medication. Mild hypotension is common because of the effect of local anesthetic block of nerve fibers on the sympathetic nervous system, causing vasodilation. Significant hypo tension and bradycardia may occur, especially when rising from a prone position or following large dose increases or boluses. Treatment of unresolved hypotension may include hydration, decreasing the epidural rate, and/or removal of local anesthetic from analgesic solution. Unwanted Motor and Sensory
Deficit: The goal of adding low-dose local anesthetics to epidural opioids for pain management is to provide analgesia, not to produce anesthesia. Patients should be able to ambulate if their condition allows, and epidural analgesic should not hamper this important recovery activity. However, many factors, including location of the epidural catheter, local anesthetic dose, and variability in patient response, can result in patients experiencing unwanted motor and sensory deficits. Pain is the first sensation lost, followed by temperature, touch, proprioception, and skeletal muscle tone
4.
5.
Assess for sensory deficit every shift. Ask pa tient to point to numb and tingling skin areas (numbness and tingling at the incision site is common and usually normal). Notify physician or other health care professional of un wanted motor and sensory deficits. Unwanted motor and sensory deficits often can be corrected with simple treatment. For example, a change in position may relieve nor extremity muscle weakness is often treated by decreasing the epidural infusion rate and keeping the patient in bed until the weakness resolves. Sometimes removing the local anesthetic from the analgesic solution
6.
is necessary, such as when signs of local anesthetic toxicity are detected or when simple treatment of motor and sensory deficits has been unsuccessful. Advise patient to request assistance during ambulation until orthostatic hypotension and motor deficits are ruled out.
7.
8.
9.
Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendation
s should not be exceeded
10.
Students Name: _______________________________ Clinical Instructor: ______________________________
You might also like
- BupivacaineDocument6 pagesBupivacaineAngelica Dalit MendozaNo ratings yet
- BUPIVACAINEDocument1 pageBUPIVACAINEVoid Less0% (2)
- Lidocaine Drug StudyDocument1 pageLidocaine Drug StudyMichael Baylon Dueñas100% (2)
- Drug Study (Lidocaine HCL) - TorresDocument6 pagesDrug Study (Lidocaine HCL) - TorresbabiNo ratings yet
- Drug Study (Epinephrine, Lidocaine, Diazepam)Document6 pagesDrug Study (Epinephrine, Lidocaine, Diazepam)Abigaile Operiano100% (2)
- Lesson Plan Mapeh 4a'sDocument3 pagesLesson Plan Mapeh 4a'sJhayzki Asuncion100% (3)
- Advanced Corporate Finance Quiz 2 SolutionsDocument3 pagesAdvanced Corporate Finance Quiz 2 SolutionslaurenNo ratings yet
- ORDocument7 pagesORMay EvelynNo ratings yet
- Isoflurane ThiopentalDocument13 pagesIsoflurane ThiopentalMr rawr100% (1)
- Drug StudyDocument8 pagesDrug StudyAnne Lorraine RodriguezNo ratings yet
- Drug StudyDocument2 pagesDrug Studyluvbel100% (2)
- Drug Study - MidazolamDocument8 pagesDrug Study - MidazolamKian HerreraNo ratings yet
- Sevoflurane 2Document2 pagesSevoflurane 2Tasha_Caballer_379100% (1)
- KetamineDocument2 pagesKetamineyanti anggrenie100% (1)
- Drug Study: Lidocaine Hydrochloride XylocaineDocument2 pagesDrug Study: Lidocaine Hydrochloride XylocaineJoevence Gazo CuaresmaNo ratings yet
- Drug Study Nov. 12Document6 pagesDrug Study Nov. 12Jenny Ajoc100% (4)
- Atropine Sulfate (Drug Study)Document3 pagesAtropine Sulfate (Drug Study)Franz.thenurse6888100% (1)
- Drug StudyDocument3 pagesDrug StudyROCHELLE DALIWAN100% (1)
- Midazolam Drug Study SaclotDocument1 pageMidazolam Drug Study SaclotMaybelle Cababat Saclot100% (1)
- Casilan, Ynalie Drug Study (Morphine)Document5 pagesCasilan, Ynalie Drug Study (Morphine)Ynalie CasilanNo ratings yet
- Drug Mode of Action Indication Adverse Effects Nursing Responsibilities Generic NameDocument3 pagesDrug Mode of Action Indication Adverse Effects Nursing Responsibilities Generic NameJinky Nacar DomingoNo ratings yet
- DRUG STUDY LidocaineDocument1 pageDRUG STUDY Lidocainejulesubayubay542860% (5)
- Drug Classification Action of Drug Indication and Contraindication Side Effect Nursing ConsiderationDocument2 pagesDrug Classification Action of Drug Indication and Contraindication Side Effect Nursing ConsiderationDanica Kate GalleonNo ratings yet
- Succunylcholine (Anectine) : University of San Carlos College of Nursing Drug StudyDocument1 pageSuccunylcholine (Anectine) : University of San Carlos College of Nursing Drug StudyFederico AndalesNo ratings yet
- Drug Study - Anesthestics....Document43 pagesDrug Study - Anesthestics....Edward Baes67% (3)
- DRUG STUDY - FurosemideDocument2 pagesDRUG STUDY - FurosemideKian HerreraNo ratings yet
- Drug Study Potassium ChlorideDocument5 pagesDrug Study Potassium ChlorideKenneth Mark B. TevesNo ratings yet
- 9 PropofolDocument2 pages9 PropofolAbdelhafiz Susmiran100% (3)
- DRUG STUDY-LidocaineDocument3 pagesDRUG STUDY-LidocaineCarissa Mae Tapec Estrada100% (1)
- Heparin InjectionDocument2 pagesHeparin InjectiongagandipkSNo ratings yet
- Dopamine HCLDocument1 pageDopamine HCLIvanne Hisoler100% (3)
- Drug StudyDocument3 pagesDrug Studyunkown userNo ratings yet
- Drug Study: Midazolam: RecommendedDocument5 pagesDrug Study: Midazolam: RecommendedShara Lailanie A. AzisNo ratings yet
- XylocaineDocument1 pageXylocaineRozanne BanzaliNo ratings yet
- Atropine Sulfate Drug STudyDocument2 pagesAtropine Sulfate Drug STudyLiway100% (1)
- Ritalin LA: Initial, 20 MG PO qAM May Adjust Dose in Weekly 10-mg Incremen TS, Not To Exceed 60 Mg/day (Patients Requiring A Lower InitialDocument2 pagesRitalin LA: Initial, 20 MG PO qAM May Adjust Dose in Weekly 10-mg Incremen TS, Not To Exceed 60 Mg/day (Patients Requiring A Lower InitialKwin SaludaresNo ratings yet
- MIDAZOLAM Drug StudyDocument3 pagesMIDAZOLAM Drug StudyEur Miole60% (5)
- Nursing Responsibility Adverse Effects Machanism of Action Drug NameDocument2 pagesNursing Responsibility Adverse Effects Machanism of Action Drug NameSalwa ZeinNo ratings yet
- Clonidine Hydrochloride (Drug Study)Document2 pagesClonidine Hydrochloride (Drug Study)Franz.thenurse688875% (4)
- Drug Study: Morphine SulfateDocument8 pagesDrug Study: Morphine SulfateShara Lailanie A. Azis100% (1)
- DRUG STUDY AdenosineDocument1 pageDRUG STUDY Adenosinejulesubayubay5428100% (1)
- Epinephrine Drug StudyDocument2 pagesEpinephrine Drug StudyAbigail De Leon80% (5)
- EsmololDocument2 pagesEsmololtherock316_995149No ratings yet
- DRUG+STUDY PropofolDocument2 pagesDRUG+STUDY PropofolJoevence Gazo Cuaresma100% (2)
- FamotidineDocument1 pageFamotidineMäc LäntinNo ratings yet
- AcarboseDocument1 pageAcarboseHanna SeNo ratings yet
- Dopamine HydrochlorideDocument2 pagesDopamine HydrochlorideNasrah N. MusaNo ratings yet
- BNP (C)Document2 pagesBNP (C)Mae Ann Bueno CastillonNo ratings yet
- Midazolam Drug Study SaclotDocument1 pageMidazolam Drug Study SaclotMaybelle Cababat SaclotNo ratings yet
- DRUG-STUDY-Lidocaine RyreyDocument1 pageDRUG-STUDY-Lidocaine RyreyJanelle Cabida SupnadNo ratings yet
- Drug Study - FluconazoleDocument2 pagesDrug Study - Fluconazoleryan100% (1)
- Drug Study CardinalDocument21 pagesDrug Study CardinalDrei LanuzoNo ratings yet
- ZonisamideDocument2 pagesZonisamideRo-anne AkuNo ratings yet
- Phenytoin and Protamine SulfateDocument2 pagesPhenytoin and Protamine SulfateTintin Ponciano100% (1)
- NeostigmineDocument4 pagesNeostigmineDonna Lyn B. DizonNo ratings yet
- Drug StudyDocument6 pagesDrug StudyBrix John PortellanoNo ratings yet
- MirasolDocument7 pagesMirasolJan Chrispian MirasolNo ratings yet
- RLE OR - Drug StudyDocument6 pagesRLE OR - Drug Studyelijahdale.guillergan-05No ratings yet
- Anestesia 1Document22 pagesAnestesia 1Carlos MNo ratings yet
- Indication Specific Action Side Effects/ Adverse Effects Nursing Consideration/ Patient TeachingDocument6 pagesIndication Specific Action Side Effects/ Adverse Effects Nursing Consideration/ Patient TeachingKrista Madranca CastroNo ratings yet
- Extra Pyramidal Side EffectsDocument27 pagesExtra Pyramidal Side EffectsChisco OKabsNo ratings yet
- Basics of Anesthesia: Karolina Doskocz gr2BDocument6 pagesBasics of Anesthesia: Karolina Doskocz gr2BKarolina DoskoczNo ratings yet
- Organizational Chart: Health StaffDocument8 pagesOrganizational Chart: Health StaffKrystel Joy AuroNo ratings yet
- Translation LabelDocument1 pageTranslation LabelKrystel Joy AuroNo ratings yet
- Uedc Form 5 West Visayas State UniversityDocument2 pagesUedc Form 5 West Visayas State UniversityKrystel Joy AuroNo ratings yet
- Edited Instrument HFJJDocument9 pagesEdited Instrument HFJJKrystel Joy AuroNo ratings yet
- National Tuberculosis ProgramDocument2 pagesNational Tuberculosis ProgramKrystel Joy AuroNo ratings yet
- National Tuberculosis ProgramDocument2 pagesNational Tuberculosis ProgramKrystel Joy AuroNo ratings yet
- Home VisitDocument17 pagesHome VisitKrystel Joy AuroNo ratings yet
- Molo District Health Center: AP (Pre-Natal)Document2 pagesMolo District Health Center: AP (Pre-Natal)Krystel Joy AuroNo ratings yet
- Table of Contents (Dec 25, 2013)Document12 pagesTable of Contents (Dec 25, 2013)Krystel Joy AuroNo ratings yet
- Goal:: Nursing Interventions For SchizophreniaDocument3 pagesGoal:: Nursing Interventions For SchizophreniaKrystel Joy AuroNo ratings yet
- West Visayas State University College of Nursing Iloilo CityDocument5 pagesWest Visayas State University College of Nursing Iloilo CityKrystel Joy AuroNo ratings yet
- Notes Physician's Orders: College of NursingDocument1 pageNotes Physician's Orders: College of NursingKrystel Joy AuroNo ratings yet
- West Visayas State University College of Nursing Iloilo CityDocument8 pagesWest Visayas State University College of Nursing Iloilo CityKrystel Joy AuroNo ratings yet
- Quotes About Friendship: C.S. Lewis Friendship 57,509 People Liked ItDocument19 pagesQuotes About Friendship: C.S. Lewis Friendship 57,509 People Liked ItKrystel Joy AuroNo ratings yet
- Acute Cholecystitis: From ER To Surgery: Riginal RticleDocument5 pagesAcute Cholecystitis: From ER To Surgery: Riginal RticleKrystel Joy AuroNo ratings yet
- Metaphysics of AristotleDocument60 pagesMetaphysics of AristotleJaimon Thadathil100% (4)
- Cooling Tower FundamentalDocument64 pagesCooling Tower FundamentaltienNo ratings yet
- Famous Letters of Mahatma GandhiDocument146 pagesFamous Letters of Mahatma Gandhivishalnaidu2010No ratings yet
- Venteo de Emergencia 94200-3FDocument3 pagesVenteo de Emergencia 94200-3FSantiago PeñuelaNo ratings yet
- Handbook 2022-2023Document120 pagesHandbook 2022-2023pranseiyarNo ratings yet
- The Nigeria of My DreamsDocument2 pagesThe Nigeria of My DreamsifelakojaofinNo ratings yet
- Equity EssayDocument8 pagesEquity EssayTeeruVarasuNo ratings yet
- Ga Hong Mei's DiaryDocument5 pagesGa Hong Mei's DiaryZefroudeille MartiniNo ratings yet
- Christmas DollDocument20 pagesChristmas Dollcraftycow62No ratings yet
- A Management Information SystemDocument15 pagesA Management Information SystemFRAkfurdNo ratings yet
- Enrichment Student Proposals Clinical Research PDFDocument2 pagesEnrichment Student Proposals Clinical Research PDFSethNo ratings yet
- Heck Vs SantosDocument3 pagesHeck Vs SantosMasterboleroNo ratings yet
- 02 - The Concept of Professionalism in Relation To ItqanDocument40 pages02 - The Concept of Professionalism in Relation To Itqanhappy100% (1)
- Gligoric - I Play Against Pieces (2003) PDFDocument144 pagesGligoric - I Play Against Pieces (2003) PDFArdelean Lorela100% (3)
- Ayobami Kehinde An Aesthetics of Realism The Image of Postcolonial Africa in Meja Mwangis Going Down River Road An EssayDocument31 pagesAyobami Kehinde An Aesthetics of Realism The Image of Postcolonial Africa in Meja Mwangis Going Down River Road An EssayMedara MosesNo ratings yet
- HAZOP STUDY-Madu PDFDocument21 pagesHAZOP STUDY-Madu PDFTirupati JalnilNo ratings yet
- 09 Samss 107Document11 pages09 Samss 107YOUSUF KHANNo ratings yet
- Production Planning and Control (Uninterruptable Power Supply)Document6 pagesProduction Planning and Control (Uninterruptable Power Supply)zesleyNo ratings yet
- Change The Verbs To Adverbs AidDocument2 pagesChange The Verbs To Adverbs Aidarnel0% (1)
- Classroom Ppa MathDocument2 pagesClassroom Ppa MathJaime DailegNo ratings yet
- Application of Geomatry in BusinessDocument23 pagesApplication of Geomatry in BusinessSoummo ChakmaNo ratings yet
- Bombastic Words For SPM EssayDocument11 pagesBombastic Words For SPM EssayAmirul Zaki100% (3)
- RS125 Workshop ManualDocument290 pagesRS125 Workshop ManualJuan José Cázares RamírezNo ratings yet
- Ebook An Introduction To Contemporary Islamic Philosophy 3Rd Edition Mohammad Fana I Eshkevari Online PDF All ChapterDocument69 pagesEbook An Introduction To Contemporary Islamic Philosophy 3Rd Edition Mohammad Fana I Eshkevari Online PDF All Chaptercarl.rojas572100% (9)
- Paradise Mislaid: How We Lost Heaven and How We Can Regain ItDocument223 pagesParadise Mislaid: How We Lost Heaven and How We Can Regain Itlemonslover100% (2)
- LUN Provisioning FormDocument4 pagesLUN Provisioning FormluckysrvstvNo ratings yet
- Compounding Self AssessmentDocument15 pagesCompounding Self AssessmentLara LaiNo ratings yet
- Course Handout Spreadsheet For ManagersDocument8 pagesCourse Handout Spreadsheet For ManagersSunil ChinnuNo ratings yet