Professional Documents
Culture Documents
Fahmi
Fahmi
Uploaded by
Fahmiatul FununiCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Community Health Nursing Practice Questions With RationaleDocument16 pagesCommunity Health Nursing Practice Questions With RationaleBe Nj90% (21)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Statement of The ProblemDocument8 pagesStatement of The ProblemCarlo Arizabal100% (2)
- Clinical Pharmacy Pocket Companion 2nd EditionDocument567 pagesClinical Pharmacy Pocket Companion 2nd EditionA.M DiabNo ratings yet
- Paket Petronas Ame + Usg AbdomenDocument3 pagesPaket Petronas Ame + Usg AbdomenBayu HidayatNo ratings yet
- Eye HospitalDocument12 pagesEye HospitalMcguire ArtNo ratings yet
- S53 - Syed Kashif Ghani-Fpsc Zakir NagarDocument2 pagesS53 - Syed Kashif Ghani-Fpsc Zakir NagarFahad VaqarNo ratings yet
- DMMMSU-RETC-F013-Application For Ethics Review of A New ProtocolDocument4 pagesDMMMSU-RETC-F013-Application For Ethics Review of A New ProtocoluzamarknielconNo ratings yet
- Sepsis and Septic ShockDocument36 pagesSepsis and Septic ShockCarlos Emerson Rodriguez MalaverNo ratings yet
- MPU 3313 - V2 Kesihatan Dan Kesejahteraan 2Document13 pagesMPU 3313 - V2 Kesihatan Dan Kesejahteraan 2TAY JIUN HOANG MoeNo ratings yet
- Minutes of 290th Meeting of Registration BoardDocument1,286 pagesMinutes of 290th Meeting of Registration BoardUsman DarNo ratings yet
- Japanese Encephalitis Di Indonesia - JurnalDocument9 pagesJapanese Encephalitis Di Indonesia - JurnalMisyahHamisahSha'syahNo ratings yet
- Use of Restraint Form - Education Points For CompletionDocument2 pagesUse of Restraint Form - Education Points For Completionnostra83No ratings yet
- Medical AbbreviationsDocument31 pagesMedical AbbreviationsLailaNo ratings yet
- Twinkle Patel SynopsisDocument20 pagesTwinkle Patel Synopsissa867069No ratings yet
- COVID-19 mRNA Vaccine BNT162b2 UKPAR PFIZER BIONTECH 15dec2020Document51 pagesCOVID-19 mRNA Vaccine BNT162b2 UKPAR PFIZER BIONTECH 15dec2020gio malicoNo ratings yet
- FNCP 21 PDF FreeDocument9 pagesFNCP 21 PDF FreeAina HaravataNo ratings yet
- Management of Asherman's SyndromeDocument14 pagesManagement of Asherman's SyndromeEquipmed VenezuelaNo ratings yet
- ChennaiDocument14 pagesChennaiPatel VaghasiyaNo ratings yet
- Homeopathic Self-Care - The Quick and Easy Guide For The Whole Family (PDFDrive) PDFDocument452 pagesHomeopathic Self-Care - The Quick and Easy Guide For The Whole Family (PDFDrive) PDFNimesh Patel100% (4)
- Nemiliztli y Frias Epidemiologist ResumeDocument2 pagesNemiliztli y Frias Epidemiologist Resumeapi-520522903No ratings yet
- Final. Qcafi Guidelines On Face To Face Classes Sy 2022-2023Document4 pagesFinal. Qcafi Guidelines On Face To Face Classes Sy 2022-2023Benedicto IluminNo ratings yet
- A Comparison of International Profiles of Healthcare SystemsDocument5 pagesA Comparison of International Profiles of Healthcare SystemsJomahalemNo ratings yet
- A Review of Classification of Disease in AyurvedaDocument11 pagesA Review of Classification of Disease in AyurvedaEditor_IAIMNo ratings yet
- Contemporary Trends in The Treatment Modalities andDocument4 pagesContemporary Trends in The Treatment Modalities andProsthodontics DeptNo ratings yet
- Chronic Kidney DiseaseDocument283 pagesChronic Kidney DiseaseloisebadNo ratings yet
- Down SyndromeDocument28 pagesDown SyndromeChristine LohNo ratings yet
- Daftar Pustaka PDFDocument3 pagesDaftar Pustaka PDFPutu Ika WNo ratings yet
- 10 Common Superficial Tongue LesionsDocument9 pages10 Common Superficial Tongue LesionsAngga NNo ratings yet
- Crocus Sativus L. (Saffron) in The Treatment of Premenstrual Syndrome: A Double-Blind, Randomised and Placebo-Controlled TrialDocument5 pagesCrocus Sativus L. (Saffron) in The Treatment of Premenstrual Syndrome: A Double-Blind, Randomised and Placebo-Controlled TrialhanaNo ratings yet
- TH e Curr Icu Lum Ou Tli Ne of Le Mol Ogy: (Temporary Edition)Document36 pagesTH e Curr Icu Lum Ou Tli Ne of Le Mol Ogy: (Temporary Edition)api-3728690No ratings yet
Fahmi
Fahmi
Uploaded by
Fahmiatul FununiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fahmi
Fahmi
Uploaded by
Fahmiatul FununiCopyright:
Available Formats
the spine is most vulnerable to fracture.
Fractures generally result from indirect trauma caused by excessive loading, sudden mus- cle contraction, or excessive motion beyond physiologic limits. Osteoporosis contributes to vertebral body collapse (compression fracture). Stable spinal fractures are caused by exion, extension, lateral bending, or vertical loading. The anterior structural column (ver- tebral bodies and dis s) or the posterior structural column (neural arch, articular processes, ligaments) has been disrupted. !nstable fractures occur "ith fracture-dislocations and exhibit disruption of both anterior and posterior structural columns. The potential for neural damage exists. The patient "ith a spinal fracture presents "ith acute tender- ness, s"elling, paravertebral muscle spasm, and change in the normal curves or in the gap bet"een spinous processes. #ain is greater "ith moving, coughing, or "eight bearing. $mmobili%a- tion is essential until initial assessments have determined "hether there is any spinal cord in&ury and "hether the fracture is stable or unstable. Fe" spinal fractures are associated "ith neurologic decits. $f spinal cord in&ury "ith neurologic decit does occur, it usually re'uires immediate surgery (laminectomy "ith spinal fusion) to decompress the spinal cord.
L e Amputation is the removal of a body part, v usually an extremity. *mputation of a lo"er extremity is often madee necessary by pro- gressive peripheral vascularl disease (often a se'uela of diabetes mellitus),s
*mputation
fulminating gas gangrene, trauma (crushing in&uries, burns, frostbite, electrical burns), congenital deformities, chronic osteomyelitis, oro malignant tumor. Of all these causes, peripheral vascular disease accounts for most amputationsf of lo"er extrem- ities. (See /hapter (1 for more information.) A *mputation is used to relieve symptoms, m improve function, and save or improve the patients 'uality of life. $f the health care team p communicates a positive attitude, the patient u ad&usts to the amputation more readily and actively participates in the rehabili- tative plan, t learning ho" to modify activities and ho" to use a as- sistive devices for *23s and mobility.
t i o n
Medical Management
Stable spinal fractures are treated conservatively "ith limited bed rest. The head of the bed is elevated less than () degrees until the acute pain subsides (several days). *nalgesics are prescribed for pain relief. The patient is monitored for a transient paralytic ileus caused by associated retroperitoneal hemorrhage. Sitting is avoided until the pain subsides. * spinal brace or plastic thoracolumbar orthosis may be applied for support during progressive ambulation and resumption of activities. The patient "ith an unstable fracture is treated "ith bed rest, possibly "ith the use of a special turning device (eg, Stry er frame) to maintain spinal alignment. +eurologic status is monitored closely during the preoperative and postoperative periods. ,ithin -. hours after fracture, open reduction, decompression, and xation "ith spinal fusion and instrument stabili%ation are usually accomplished. #ostoperatively, the patient may be cared for on the turning device or in a bed "ith a rm mattress. #rogressive ambulation is begun a fe" days after surgery, "ith the patient using a body brace orthosis. #atient teaching emphasi%es good posture, good body mechanics, and, after healing is sufcient, bac -strengthening exercises. (Spinal cord in&ury is discussed in /hapter 0(.)
2.
diagnostic a *ngiograph
* st a g e d a m p ut at io n m a y b e us e d " h e n g a n gr e n
e and infection exist. $nitially, a guillotine amputation is performed to remove the necrotic and infected tissue. The "ound is d4brided and al- lo"ed to drain. Sepsis is treated "ith systemic antibiotics. $n a fe" days, after the infection has been controlled and the patients con- dition has stabili%ed, a denitive amputation "ith s in closure is performed.
Complications
/omplications that may occur "ith amputation include hemorrhage, infection, skin breakdown, phantom limb pain, and joint contracture. 5ecause ma&or blood vessels have been severed, massive bleeding may occur. $nfection is a ris "ith all surgical procedures. The ris for infection increases "ith contaminated "ounds after traumatic amputation. S in irritation caused by the prosthesis may result in s in brea do"n. Phantom limb pain is caused by the severing of peripheral nerves. 6oint contracture is caused by positioning and a protective exion "ithdra"al pattern associated "ith pain and muscle imbalance.
Medical Management
The ob&ective of treatment is to achieve healing of the amputa- tion "ound, the result being a nontender residual limb (stump) "ith healthy s in for prosthesis use. 7ealing is enhanced by gentle handling of the residual limb, control of residual limb edema through rigid or soft compression dressings, and use of aseptic techni'ue in "ound care to avoid infection.
2104
Unit 15
8!S/!3OS9:3:T*3 F!+/T$O+
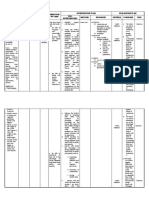
Above knee (AK)
Above elbow (AE) Below elbow (BE)
Knee disarticulation Below knee (BK)
Syme
F !U"# $%&1$
3evels of amputation are determined by circulatory ade'uacy, type of prosthesis,
function of the part, and muscle balance. (A) 3evels of amputation of upper extremity. ( ') 3evels of amputation of lo"er extremity.
* closed rigid cast dressing used to provide uniform
is fre'uently
porated in the dressing. Stump ("ound) hematomas are controlled
compression, to support soft tissues, to control pain, and to pre- vent &oint contractures. $mmediately after surgery, a sterili%ed residual limb soc is applied to the residual limb. Felt pads are placed over pressure-sensitive areas. The residual limb is "rapped "ith elastic plaster-ofparis bandages "hile rm, even pressure is maintained. /are is ta en not to constrict circulation. For the patient "ith a lo"er extremity amputation, the plaster cast may be e'uipped to attach a temporary prosthetic extension (pylon) and an articial foot. This rigid dressing techni'ue is used as a means of creating a soc et for immediate postoperative pros- thetic tting. The length of the prosthesis is tailored to the indi- vidual patient. :arly minimal "eight bearing on the residual limb "ith a rigid cast dressing and a pylon attached produces little dis- comfort. The cast is changed in about 1) to 1. days. :levated body temperature, severe pain, or a loose-tting cast may neces- sitate earlier replacement. * removable rigid dressingmay be placed over a soft dressing to control edema, to prevent &oint exion contracture, and to pro- tect the residual limb from unintentional trauma during transfer activities. This rigid dressing is removed several days after surgery for "ound inspection and is then replaced to control edema. The dressing facilitates residual limb shaping. * soft dressing"ith or "ithout compression may be used if there is signicant "ound drainage and fre'uent inspection of the resid- ual limb (stump) is desired. *n immobili%ing splint may be incor-
"ith "ound drainage devices to minimi%e infection.
"ehabilitation
#atients "ho re'uire amputation because of severe trauma are usu- ally, but not al"ays, young and healthy, heal rapidly, and partici- pate in a vigorous rehabilitation program. 5ecause the amputation is the result of an in&ury, the patient needs psychological support in accepting the sudden change in body image and in dealing "ith the stresses of hospitali%ation, long-term rehabilitation, and mod- ication of lifestyle. #atients "ho undergo amputation need sup- port as they grieve the loss, and they need time to "or through their feelings about their permanent loss and change in body image. Their reactions are unpredictable and can include anger, bitterness, and hostility. The multidisciplinary rehabilitation team (patient, nurse, phy- sician, social "or er, psychologist, prosthetist, vocational rehabil- itation "or er) helps the patient achieve the highest possible level of function and participation in life activities (Fig. 0;-1<). #ros- thetic clinics and amputee support groups facilitate this rehabi- litation process. =ocational counseling and &ob retraining may be necessary to help patients return to "or . #sychological problems (eg, denial, "ithdra"al) may be in- uenced by the type of support the patient receives from the re- habilitation team and by ho" 'uic ly *23s and use of the
5ased on the assessment data, the patients ma&or nursing diag- noses may include the follo"ing> ? *cute pain related to amputation ? ?is for disturbed sensory perception> phantom limb pain related to amputation ? $mpaired s in integrity related to surgical amputation ? 2isturbed body image related to amputation of body part ? $neffective coping, related to failure to accept loss of body part ? ?is for anticipatory and@or dysfunctional grieving related to loss of body part ? Self-care decit> feeding, bathing@hygiene, dressing@grooming, or toileting, related to loss of extremity ? $mpaired physical mobility related to loss of extremity /O33*5O?*T$=: #?O53:8S@ #OT:+T$*3 /O8#3$/*T$O+S 5ased on the assessment data, potential complications that may develop include the follo"ing>
F !U"# $%&1(
8any amputees receive prostheses
soon after surgery and begin learning ho" to use them "ith the help and support of the rehabilita- tion team, "hich includes nurses, physicians, physical therapists, and others.
? ? ?
#ostoperative hemorrhage $nfection S in brea do"n
Planning and !oals
The ma&or goals of the patient may include relief of pain, absence of altered sensory perceptions, "ound healing, acceptance of al- tered body image, resolution of the grieving process, independence in self-care, restoration of physical mobility, and absence of complications.
prosthesis are learned. 9no"ing the full options and capabilities available "ith the various prosthetic devices can give the patient a sense of control over the disability.
)U"* )! P"+C#**, -.# PA- #)- U)/#"!+ )! A) AMPU-A- +)
Assessment
5efore surgery, the nurse must evaluate the neurovascular and func- tional status of the extremity through history and physical assessment. $f the patient has experienced a traumatic amputation, the nurse assesses the function and condition of the residual limb. The nurse also assesses the circulatory status and function of the unaf- fected extremity. $f infection or gangrene develops, the patient may have associated enlarged lymph nodes, fever, and purulent drainage. * culture is ta en to determine the appropriate antibiotic therapy. The nurse evaluates the patients nutritional status and creates a plan for nutritional care, if indicated. For "ound healing, a bal- anced diet "ith ade'uate protein and vitamins is essential. *ny concurrent health problems (eg, dehydration, anemia, car- diac insufciency, chronic respiratory problems, diabetes mellitus) need to be identied and treated so that the patient is in the best possible condition to "ithstand the trauma of surgery. The use of corticosteroids, anticoagulants, vasoconstrictors, or vasodilators may inuence management and "ound healing. The nurse assesses the patients psychological status. 2eter- mination of the patients emotional reaction to amputation is es- sential for nursing care. Arief response to a permanent alteration in body image is normal. *n ade'uate support system and pro- fessional counseling can help the patient cope in the aftermath of amputation surgery.
)u0sing nte0ventions
?:3$:=$+A #*$+ Surgical pain can be effectively controlled "ith opioid analgesics, nonpharmaceutical interventions, or evacuation of the hematoma or accumulated fluid. #ain may be incisional or may be caused by inammation, infection, pressure on a bony prominence, or hematoma. 8uscle spasms may add to the patients discomfort. /hanging the patients position or placing a light sandbag on the residual limb to counteract the muscle spasm may improve the pa- tients level of comfort. :valuation of the patients pain and re- sponses to interventions is an important part of the nurses role in pain management. The pain may be an expression of grief and alteration of body image. 8$+$8$B$+A *3T:?:2 S:+SO?C #:?/:#T$O+S *mputees may experience phantom limb pain soon after surgery or - to ( months after amputation. $t occurs more fre'uently may in above- nee amputations. The patient describes pain or unusual sensations, such as numbness, tingling, or muscle cramps, as "ell as a feeling that the extremity is present, crushed, cramped, or t"isted in an abnormal position. ,hen a patient describes phantom pains or sensations, the nurse ac no"ledges these feel- ings and helps the patient modify these perceptions. #hantom sensations diminish over time. The pathogenesis of the phantom limb phenomenon is un no"n. 9eeping the patient active helps decrease the occurrence of phantom limb pain. :arly
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Community Health Nursing Practice Questions With RationaleDocument16 pagesCommunity Health Nursing Practice Questions With RationaleBe Nj90% (21)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Statement of The ProblemDocument8 pagesStatement of The ProblemCarlo Arizabal100% (2)
- Clinical Pharmacy Pocket Companion 2nd EditionDocument567 pagesClinical Pharmacy Pocket Companion 2nd EditionA.M DiabNo ratings yet
- Paket Petronas Ame + Usg AbdomenDocument3 pagesPaket Petronas Ame + Usg AbdomenBayu HidayatNo ratings yet
- Eye HospitalDocument12 pagesEye HospitalMcguire ArtNo ratings yet
- S53 - Syed Kashif Ghani-Fpsc Zakir NagarDocument2 pagesS53 - Syed Kashif Ghani-Fpsc Zakir NagarFahad VaqarNo ratings yet
- DMMMSU-RETC-F013-Application For Ethics Review of A New ProtocolDocument4 pagesDMMMSU-RETC-F013-Application For Ethics Review of A New ProtocoluzamarknielconNo ratings yet
- Sepsis and Septic ShockDocument36 pagesSepsis and Septic ShockCarlos Emerson Rodriguez MalaverNo ratings yet
- MPU 3313 - V2 Kesihatan Dan Kesejahteraan 2Document13 pagesMPU 3313 - V2 Kesihatan Dan Kesejahteraan 2TAY JIUN HOANG MoeNo ratings yet
- Minutes of 290th Meeting of Registration BoardDocument1,286 pagesMinutes of 290th Meeting of Registration BoardUsman DarNo ratings yet
- Japanese Encephalitis Di Indonesia - JurnalDocument9 pagesJapanese Encephalitis Di Indonesia - JurnalMisyahHamisahSha'syahNo ratings yet
- Use of Restraint Form - Education Points For CompletionDocument2 pagesUse of Restraint Form - Education Points For Completionnostra83No ratings yet
- Medical AbbreviationsDocument31 pagesMedical AbbreviationsLailaNo ratings yet
- Twinkle Patel SynopsisDocument20 pagesTwinkle Patel Synopsissa867069No ratings yet
- COVID-19 mRNA Vaccine BNT162b2 UKPAR PFIZER BIONTECH 15dec2020Document51 pagesCOVID-19 mRNA Vaccine BNT162b2 UKPAR PFIZER BIONTECH 15dec2020gio malicoNo ratings yet
- FNCP 21 PDF FreeDocument9 pagesFNCP 21 PDF FreeAina HaravataNo ratings yet
- Management of Asherman's SyndromeDocument14 pagesManagement of Asherman's SyndromeEquipmed VenezuelaNo ratings yet
- ChennaiDocument14 pagesChennaiPatel VaghasiyaNo ratings yet
- Homeopathic Self-Care - The Quick and Easy Guide For The Whole Family (PDFDrive) PDFDocument452 pagesHomeopathic Self-Care - The Quick and Easy Guide For The Whole Family (PDFDrive) PDFNimesh Patel100% (4)
- Nemiliztli y Frias Epidemiologist ResumeDocument2 pagesNemiliztli y Frias Epidemiologist Resumeapi-520522903No ratings yet
- Final. Qcafi Guidelines On Face To Face Classes Sy 2022-2023Document4 pagesFinal. Qcafi Guidelines On Face To Face Classes Sy 2022-2023Benedicto IluminNo ratings yet
- A Comparison of International Profiles of Healthcare SystemsDocument5 pagesA Comparison of International Profiles of Healthcare SystemsJomahalemNo ratings yet
- A Review of Classification of Disease in AyurvedaDocument11 pagesA Review of Classification of Disease in AyurvedaEditor_IAIMNo ratings yet
- Contemporary Trends in The Treatment Modalities andDocument4 pagesContemporary Trends in The Treatment Modalities andProsthodontics DeptNo ratings yet
- Chronic Kidney DiseaseDocument283 pagesChronic Kidney DiseaseloisebadNo ratings yet
- Down SyndromeDocument28 pagesDown SyndromeChristine LohNo ratings yet
- Daftar Pustaka PDFDocument3 pagesDaftar Pustaka PDFPutu Ika WNo ratings yet
- 10 Common Superficial Tongue LesionsDocument9 pages10 Common Superficial Tongue LesionsAngga NNo ratings yet
- Crocus Sativus L. (Saffron) in The Treatment of Premenstrual Syndrome: A Double-Blind, Randomised and Placebo-Controlled TrialDocument5 pagesCrocus Sativus L. (Saffron) in The Treatment of Premenstrual Syndrome: A Double-Blind, Randomised and Placebo-Controlled TrialhanaNo ratings yet
- TH e Curr Icu Lum Ou Tli Ne of Le Mol Ogy: (Temporary Edition)Document36 pagesTH e Curr Icu Lum Ou Tli Ne of Le Mol Ogy: (Temporary Edition)api-3728690No ratings yet