Professional Documents
Culture Documents
Foot Drop: Section Anatomy Primer
Foot Drop: Section Anatomy Primer
Uploaded by
Ðr SalmaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Foot Drop: Section Anatomy Primer
Foot Drop: Section Anatomy Primer
Uploaded by
Ðr SalmaCopyright:
Available Formats
Anatomy Primer
Section
Foot drop
extbooks of neurology are just like cookery or gardening books. It is all so easy on paper. With a good working knowledge of neurological anatomy, it seems, almost any problem can be precisely localised. A couple of of hours yomping through a busy out patients leads to a rapid re-evaluation of that view. Foot drop, however, is a common neurological problem that is particularly amenable to an anatomical approach, so this month I will briefly outline the anatomy of peroneal nerve and discuss the clinical and neurophysiological approach to foot drop. The common peroneal nerve is a branch of the sciatic nerve. The sciatic nerve is formed in the pelvis by fibres from the lumbosacral trunk (L4,5) and by fibres from S1,2,3. The nerve immediately leaves the pelvis through the greater sciatic notch, below the piriformis muscle. The nerve may divide immediately, or may pass either above or through the piriformis. In the gluteal region the nerve lies deep to gluteus maximus, between the greater trochanter and the ischial tuberosity. The nerve then passes down the back of the thigh to the apex of the popliteal fossa. In the thigh the nerve divides into lateral common peroneal and medial tibial divisions. The common peroneal division supplies fibres to the short head of biceps femoris. The common peroneal nerve leaves the popliteal fossa between the tendon of biceps femoris and the lateral head of gastrocnemius. It crosses behind the head of the fibula and passes laterally around the neck of the fibula, where it is particularly vulnerable to compression or blunt trauma. The nerve gives off the sural communicating branch to the sural nerve, and the lateral cutaneous nerve of the calf. The nerve pierces the peroneus longus muscle to divide into deep and superficial branches. The deep peroneal nerve supplies the muscles of the anterior compartment (table 1). The superficial peroneal nerve supplies the muscles in the lateral compartment (table 1) and the skin over the anterior lower leg and dorsum of the foot. Clinical Evaluation of Foot Drop The manner in which the common peroneal nerve snakes around the fibular head exposes it to injury and external compression and this can sometimes occur in bizarre and quite unexpected ways (table 2). Common peroneal neuropathy presents with foot drop; foot drop is due to weakness of the muscles in the anterior and lateral compartments of the leg. Since it is these compartments that work against gravity, pathology in the spinal chord, lumbar
Figure 1
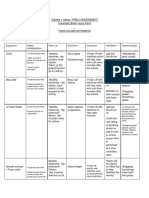
roots (L4 and L5), plexus, sciatic nerve, peroneal nerve and severe generalised neuropathies can all present in this way (Table 2). The first step in clinical evaluation is to exclude cord or other CNS pathology and examine for other peripheral nervous system involvement. In sciatic neuropathy there may also be weakness in a tibial nerve distribution also, however it is possible to have selective involvement of the common peroneal fasicles only. In L5 radiculopathy both ankle dosrsiflexion and inversion/eversion will be affected while in a pure common peroneal neuropathy inversion will be spared. There is a slight caveat however. If the foot is tested in the dropped position inversion may appear to be weak so inversion should be tested in a passively dorsiflexed position. In an isolated superficial peroneal neuropathy eversion will be weak and dorsiflexion spared while in an isolated deep peroneal neuropathy there will be weakness of dorsiflexion with sparing of eversion. In a common peroneal neuropathy sensation over the lateral foot (sural territory), sole of foot (plantar nerves) and medial calf and foot will be spared. Finally ankle jerks will be spared in a pure common peroneal neuropathy. Neurophysiological Evaluation The neurophysiological evaluation of foot drop nicely illustrates the old maxim that electrophsyiology is an extension of clinical assessment. The first step is to determine if the pathology is restricted to the common peroneal nerve only, so where possible it is worth studyingdoing the works in both lower limbs (Bilateral peroneal and tibial motor studies, bilateral superficial peroneal and sural sensory studies). If a common peroneal mono-neuropathy is confirmed, the next objective is to determine any site of injury or compression and give an estimate of severity. This can be achieved with a combination of nerve conduction studies and EMG. Segmental conduction studies around the fibular head should be performedfocal slowing or conduction block is a sign of compression or neuropraxia and also in an isolated deep peroneal neuropathy superficical peroneal sensory studies will be normal. EMG should be performed in one L4/L5 muscle not innervated by the common peroneal nerve (tibialis posterior is often used), one deep peroneal muscle (Tibialsis anterior) and one superficial (peroneus longus). The degree of dennervation and the presence or absence of voluntary activity will give pointers as to severity of the neuropathy.
Dr Brian McNamara is Consultant Neurophyisologist at Cork University Hospital. He was SHO and Registrar at Cork University Hospital, and SpR at Addenbrooke's Hospital in Cambridge. His interests include magnetic stimulation, cellular electrophysiology, and all aspects of clinical neurophysiology.
Table 1: Muscles supplied by the two divisions of the common peroneal nerve. Deep peroneal Tibialis Anterior Extensor Digitorum Longus Extensor Digitorum Brevis Peroneus Tertius Superficial Peroneal Peroneus Longus Peroneus Brevis
Figure 1: Course of the common, deep (blue) and superficial peroneal nerve, sites of stimulation for motor nerve conduction studies are shown by green discs.
24
ACNR VOLUME 3 NUMBER 1 MARCH/APRIL 2003
Anatomy Primer
Table 2: Some peripheral causes of foot drop
Generalised Neuropathy
Localised Neuropathy
Motor Neuronopathy Motor Neuropathy Motor and Sensory Polyneuropathy HMSN Mononeuritis Multiplex L4/L5 Radiculopathy Lumbosacral Plexopathy Sciatic Neuropathy eg. Buttock injection Trauma at fibular head Forcible stretch External Compression eg. Casts stockings etc. Prolonged immobility eg. During anaesthesia Occupational eg. gardening Habitual Leg crossing Weight loss
Figure 2: Normal peroneal motor study, note there is no slowing of conduction across the fibular head.
Common Peroneal Neuropathy
Figure 3: The same normal study superimposed on abnormal study (opposite leg). This study was taken from a patient who developed foot drop after having his leg in a plaster of Paris cast for 9 weeks, note the reduced amplitude and slowing across the fibular head.
P o w e r To R e n e w A L i f e
Clinically proven therapy for long-term seizure control and quality-of-life benefits
Daily Seizures Four Medications Lethargic Isolated Powerless Disoriented Inattentive
Seizure-Free Months One Medication Energetic Fun With Friends In Control Alert Achieving At School
EUROPEAN INDICATION FOR USE: The VNS Therapy System is indicated for use as an adjunctive therapy in reducing the frequency of seizures in patients whose epileptic disorder is dominated by partial seizures (with or without secondary generalisation) or generalised seizures, which are refractory to antiepileptic medications.
ADBF0802-11-1000-EC
Cyberonics Europe S.A./N.V. Belgicastraat 9, 1930 Zaventem Belgium Tel: +32 2 720 95 93 Fax: +32 2 720 60 53
w w w . v n s t h e r a p y. c o m / i n t e r n a t i o n a l
ACNR VOLUME 3 NUMBER 1 MARCH/APRIL 2003
25
You might also like
- Human Anatomy Physiology 11th Edition Marieb Test BankDocument15 pagesHuman Anatomy Physiology 11th Edition Marieb Test Banklaeliacaixpoyf100% (35)
- Savannah Prez - Pancake-x-BootyDocument73 pagesSavannah Prez - Pancake-x-BootyMauro AnticNo ratings yet
- Gluteal Tendinopathy - E3 RehabDocument24 pagesGluteal Tendinopathy - E3 RehabMahnaz ZiaNo ratings yet
- Types of Drug PreparationDocument5 pagesTypes of Drug PreparationZam Pamate100% (1)
- Muscle Flash CardsDocument127 pagesMuscle Flash Cardsjoelh9100% (3)
- Week 1 and 2 PCP Workbook QuestionsDocument4 pagesWeek 1 and 2 PCP Workbook Questionsapi-479717740100% (1)
- (New Procedures in Spinal Interventional Neuroradiology) Luigi Manfrà (Eds.) - Spinal Canal Stenosis-Springer International PublisDocument98 pages(New Procedures in Spinal Interventional Neuroradiology) Luigi Manfrà (Eds.) - Spinal Canal Stenosis-Springer International PublisThuyet Nguyen Phuoc100% (1)
- Manish Kumar Varshney's Practical Orthopedic Examination MADE EASY 2nd EdDocument577 pagesManish Kumar Varshney's Practical Orthopedic Examination MADE EASY 2nd Edankitkrgarg7100% (1)
- Water Fitness Lesson PlansDocument13 pagesWater Fitness Lesson Plansbashune0% (1)
- Peroneal Mononeuropathy MedscapeDocument13 pagesPeroneal Mononeuropathy MedscapeAnnisa Kinanti AstiNo ratings yet
- Foot DropDocument12 pagesFoot Dropmethmal subasingheNo ratings yet
- Disc HerniationDocument32 pagesDisc HerniationMadalina DragoiNo ratings yet
- Low Back PainDocument100 pagesLow Back Painchandrusai100% (1)
- Acute Flaccid ParalysisDocument19 pagesAcute Flaccid ParalysisAbdullah GadNo ratings yet
- Injuries To The Lumbosacral PlexusDocument8 pagesInjuries To The Lumbosacral PlexusKhriz Ann C ÜNo ratings yet
- Prolapse of Lumbar Intervertebral Disc: Li JieruoDocument36 pagesProlapse of Lumbar Intervertebral Disc: Li JieruoWai Kwong ChiuNo ratings yet
- 2 PDFDocument7 pages2 PDFDeei RizalNo ratings yet
- CLINICAL NEUROLOGY II Assignment 1Document8 pagesCLINICAL NEUROLOGY II Assignment 1Muskan AhujaNo ratings yet
- The Tibial Nerve and Tarsal Tunnel Syndrome: Section Anatomy PrimerDocument1 pageThe Tibial Nerve and Tarsal Tunnel Syndrome: Section Anatomy Primersatyagraha84No ratings yet
- Garosi 2012 Neurological Lameness in The Cat Common Causes and Clinical ApproachDocument9 pagesGarosi 2012 Neurological Lameness in The Cat Common Causes and Clinical Approachpetar.dzoicNo ratings yet
- Lumbar Disc HerniationDocument6 pagesLumbar Disc HerniationJosé Alberto RMNo ratings yet
- Ortho DR - RehabDocument44 pagesOrtho DR - RehabMohammed Saad NabhanNo ratings yet
- Gridrasi HDocument92 pagesGridrasi HramNo ratings yet
- 20-Common Peroneal NerveDocument29 pages20-Common Peroneal Nerverodrigocorcino899959No ratings yet
- 263 Lumbar Plexus Block - Psoas Compartment BlockDocument9 pages263 Lumbar Plexus Block - Psoas Compartment Blockarif AjiNo ratings yet
- Chapter 18: NeurologyDocument22 pagesChapter 18: NeurologypoddataNo ratings yet
- Comprehensive Review in Clinical (0753-1506)Document754 pagesComprehensive Review in Clinical (0753-1506)Abdurrahman HasanuddinNo ratings yet
- 41-Article Text-59-1-10-20190211Document3 pages41-Article Text-59-1-10-20190211Faishol Reza AdiyaksaNo ratings yet
- Spinal cord lesion 2 د.رشاد عبدالغنيDocument58 pagesSpinal cord lesion 2 د.رشاد عبدالغنيMohammad BelbahaithNo ratings yet
- Lumbar Radicular Pain: PathophysiologyDocument4 pagesLumbar Radicular Pain: PathophysiologynetifarhatiiNo ratings yet
- Low BackDocument7 pagesLow BackMuhammad FahmyNo ratings yet
- Back Pain Printable VersionDocument43 pagesBack Pain Printable VersionSabin ParajuliNo ratings yet
- Lees Testing The ReflexesDocument6 pagesLees Testing The ReflexesIsnan AnshariNo ratings yet
- LO - Sudden Paralysis, Spinal Cord InjuryDocument14 pagesLO - Sudden Paralysis, Spinal Cord InjuryMaureen ArethaNo ratings yet
- The Saphenous Nerve Is A Cutaneous Branch of The: Sport Related Injuries of The Nerves in The Knee RegionDocument4 pagesThe Saphenous Nerve Is A Cutaneous Branch of The: Sport Related Injuries of The Nerves in The Knee RegioncostinNo ratings yet
- Common Peroneal Neuropathy in Patients After First-Time StrokeDocument4 pagesCommon Peroneal Neuropathy in Patients After First-Time StrokeMarina GincuNo ratings yet
- Patella Dislocation Association With Drop Foot: Case ReportDocument2 pagesPatella Dislocation Association With Drop Foot: Case ReportekaNo ratings yet
- 2015 - 03 - 26 NEJM SciaticaDocument9 pages2015 - 03 - 26 NEJM SciaticaShaun TylerNo ratings yet
- Tarsal Tunnel Syndrome-A New Way To Diagnose An Old ProblemDocument12 pagesTarsal Tunnel Syndrome-A New Way To Diagnose An Old ProblemRianti NuranisaNo ratings yet
- 2008 - Article - 9023 ArtikeDocument7 pages2008 - Article - 9023 ArtikewilmarstrNo ratings yet
- Back and Nexk PainDocument7 pagesBack and Nexk PainDenise MathreNo ratings yet
- Electrodiagnostic in Sciatica NeuropathyDocument37 pagesElectrodiagnostic in Sciatica NeuropathyRizka_aprilNo ratings yet
- Axonotmesis, and Neurotmesis) and by SunderlandDocument24 pagesAxonotmesis, and Neurotmesis) and by SunderlandSakanadeNo ratings yet
- Review of Literature: Presenting By: Monika S. Kulkarni 1 Year MPT Department of Orthopaedic Manual TherapyDocument44 pagesReview of Literature: Presenting By: Monika S. Kulkarni 1 Year MPT Department of Orthopaedic Manual TherapyANKITA SHETTYNo ratings yet
- Lumbar Disc HerniationDocument19 pagesLumbar Disc HerniationPutri WulandariNo ratings yet
- Aritculo 3 Neuropatías Por Atrapamiento Miembro SuperiorDocument14 pagesAritculo 3 Neuropatías Por Atrapamiento Miembro SuperiorCesar AlvarezNo ratings yet
- HPNDocument3 pagesHPNFerdyNo ratings yet
- Lumbar Spinal Stenosis: Pathophysiology, Clinical Features, and DiagnosisDocument14 pagesLumbar Spinal Stenosis: Pathophysiology, Clinical Features, and DiagnosisAnastasia TjanNo ratings yet
- 2017 Spine ExaminationDocument7 pages2017 Spine Examinationradhika thapaNo ratings yet
- Spinal Cord InjuryDocument24 pagesSpinal Cord InjuryGayzel Dela CruzNo ratings yet
- Back PainDocument18 pagesBack PainCabdiladif Ahmed McrfNo ratings yet
- Motor FunctionDocument47 pagesMotor FunctionDinaNo ratings yet
- Lumbar Spine: A Guide For Neurologists Surgical Disorders of The Thoracic andDocument8 pagesLumbar Spine: A Guide For Neurologists Surgical Disorders of The Thoracic andchristian_dyrNo ratings yet
- REFLEXESDocument24 pagesREFLEXESKen Angelo JavierNo ratings yet
- Lateral Tendon Disorders Peroneal Tendinopathy Differential DiagnosisDocument5 pagesLateral Tendon Disorders Peroneal Tendinopathy Differential Diagnosischu_chiang_3No ratings yet
- Entrapment Neuropathies Conversion-GateDocument76 pagesEntrapment Neuropathies Conversion-GateRam ReddyNo ratings yet
- 242 FullDocument7 pages242 FullParaschiva PîțuNo ratings yet
- Foot & Ankle OBDocument229 pagesFoot & Ankle OBAhmed ShehataNo ratings yet
- Boehnke - Dorsal Scapular Nerve SyndromeDocument7 pagesBoehnke - Dorsal Scapular Nerve Syndromekeeley_holderNo ratings yet
- P9 Disorders of The CerebellumDocument29 pagesP9 Disorders of The CerebellumHomeground entertainmentNo ratings yet
- 1 s2.0 S0749073922000219 MainDocument15 pages1 s2.0 S0749073922000219 Mainbdjxk95cyhNo ratings yet
- Divine Intervention Episode 44 Usmle Anatomy Series Part 1Document11 pagesDivine Intervention Episode 44 Usmle Anatomy Series Part 1Swisskelly1No ratings yet
- Emg Notes: Sunday, April 22, 2007Document11 pagesEmg Notes: Sunday, April 22, 2007Shauki AliNo ratings yet
- Low Back Pain Low Back Pain: Aldsr B Aldy S. RambeDocument40 pagesLow Back Pain Low Back Pain: Aldsr B Aldy S. RambeSantri Sasmita DewiNo ratings yet
- Lumbar Disc Herniation: Prof - Dr.Hidayet Sarı Physical Medicine and Rehabilitation DepartmentDocument20 pagesLumbar Disc Herniation: Prof - Dr.Hidayet Sarı Physical Medicine and Rehabilitation DepartmentraraNo ratings yet
- Spinal Stenosis And Pinched Nerve A Simple Guide to These conditionsFrom EverandSpinal Stenosis And Pinched Nerve A Simple Guide to These conditionsRating: 5 out of 5 stars5/5 (1)
- Pinyin ChartDocument2 pagesPinyin ChartJunu LadakhiNo ratings yet
- Pinyin. RomanisationDocument19 pagesPinyin. RomanisationÐr SalmaNo ratings yet
- Intro To SSDocument81 pagesIntro To SSÐr SalmaNo ratings yet
- Asmaaul Husna - Dayof WeekDocument38 pagesAsmaaul Husna - Dayof WeekÐr SalmaNo ratings yet
- Tips 2 Success Usmle Study PlanDocument8 pagesTips 2 Success Usmle Study PlanÐr SalmaNo ratings yet
- WHO Guidelines Hand Hygiene in Health CareDocument270 pagesWHO Guidelines Hand Hygiene in Health CareÐr Salma100% (1)
- Anesthesia For The Trauma PatientDocument48 pagesAnesthesia For The Trauma PatientÐr SalmaNo ratings yet
- Triads in MedicineDocument4 pagesTriads in MedicineÐr SalmaNo ratings yet
- WHO Guidelines Hand Hygiene in Health CareDocument270 pagesWHO Guidelines Hand Hygiene in Health CareÐr Salma100% (1)
- Ent SignsDocument2 pagesEnt SignsÐr SalmaNo ratings yet
- Health and Medicine Based On Kitab Al TibbDocument13 pagesHealth and Medicine Based On Kitab Al TibbÐr SalmaNo ratings yet
- Kitab Al Qanun Fi Al-TibbDocument5 pagesKitab Al Qanun Fi Al-TibbÐr Salma100% (1)
- Neisseria Meningitidis Strep Pneumoniae E. ColiDocument3 pagesNeisseria Meningitidis Strep Pneumoniae E. ColiÐr SalmaNo ratings yet
- Sunan Abu Dawud Medicine (Kitab Al Tibb)Document6 pagesSunan Abu Dawud Medicine (Kitab Al Tibb)Ðr SalmaNo ratings yet
- Female Muscle DiagramDocument1 pageFemale Muscle DiagrammakukikiNo ratings yet
- Thigh Mcqs ExplainedDocument9 pagesThigh Mcqs ExplainedRobert EdwardsNo ratings yet
- Sacroiliac Joint Exercises For Back Pain ReliefDocument13 pagesSacroiliac Joint Exercises For Back Pain ReliefSam Visnic100% (1)
- AnatomyDocument8 pagesAnatomyRobbie WoelkersNo ratings yet
- Nsca Personal TrainerDocument180 pagesNsca Personal TrainerMaria castillo100% (1)
- Sacroilliac JointDocument37 pagesSacroilliac JointMfxMazprofxNo ratings yet
- Functional Anatomy HandoutDocument10 pagesFunctional Anatomy HandoutpowerliftermiloNo ratings yet
- Jill Miller Cue Clinic WorkbookDocument8 pagesJill Miller Cue Clinic WorkbookKati SolNo ratings yet
- Kettlebell Swing AlternativesDocument4 pagesKettlebell Swing AlternativesCeline Kyla MalloNo ratings yet
- An Electromyographic Analysis of Sumo And.19Document7 pagesAn Electromyographic Analysis of Sumo And.19JulianoEscudeiroNo ratings yet
- Intro To Diagnostic Imaging - 2 - Prof - Dr.i̇smet TAMERDocument37 pagesIntro To Diagnostic Imaging - 2 - Prof - Dr.i̇smet TAMERAly MssreNo ratings yet
- TzUpdated Low Back and Core PDFDocument8 pagesTzUpdated Low Back and Core PDFStephanie JonesNo ratings yet
- A Three-Dimensional Biomechanical Analysis of The Squat During Varying Stance WidthsDocument16 pagesA Three-Dimensional Biomechanical Analysis of The Squat During Varying Stance WidthsRafael Escamilla100% (1)
- 1.12 Gluteal Region and Posterior Thigh Compartment PDFDocument5 pages1.12 Gluteal Region and Posterior Thigh Compartment PDFJuliaNo ratings yet
- Jenevieve Cortes Advincula - Muscular Laboratory Sheet 1Document5 pagesJenevieve Cortes Advincula - Muscular Laboratory Sheet 1Jenevieve AdvinculaNo ratings yet
- Anatomy MCQDocument23 pagesAnatomy MCQPirabakar Mahendran100% (3)
- Anatomy High Yield From Usmleworld ForumDocument9 pagesAnatomy High Yield From Usmleworld Forumabe8284No ratings yet
- Workout Plan Tab and AlanaDocument9 pagesWorkout Plan Tab and Alanaapi-658308760No ratings yet
- Openings in The Skull Bone of The Skull Structures TransmittedDocument19 pagesOpenings in The Skull Bone of The Skull Structures TransmittedMacy Peralta100% (1)
- Model Answer of Formative Written OSCADocument6 pagesModel Answer of Formative Written OSCAAhmed SamahaNo ratings yet
- The Biomechanics of The Modern Golf Swing - Implications For Lower Back InjuriesDocument13 pagesThe Biomechanics of The Modern Golf Swing - Implications For Lower Back Injuries杨钦杰No ratings yet
- Anatomy HWDocument4 pagesAnatomy HWTassnime SebaeiNo ratings yet
- Evaluation of The Patient With Hip PainDocument12 pagesEvaluation of The Patient With Hip PainannisaNo ratings yet