Professional Documents
Culture Documents
Hem 3
Hem 3
Uploaded by
Septian AndriantoCopyright:
Available Formats
You might also like
- Lesson01 FT125 Overview SiemensDocument10 pagesLesson01 FT125 Overview SiemensใบบอนสิชลNo ratings yet
- Fast Facts: Clinical Trials in Oncology: The fundamentals of design, conduct and interpretationFrom EverandFast Facts: Clinical Trials in Oncology: The fundamentals of design, conduct and interpretationNo ratings yet
- Introduction To GLFP On BPC NWDocument26 pagesIntroduction To GLFP On BPC NWSuyash PandeyNo ratings yet
- 106 Torque Settings PDFDocument5 pages106 Torque Settings PDFRicardo MatosNo ratings yet
- Bodansky-2017-Potential Cost Savings by MinimiDocument4 pagesBodansky-2017-Potential Cost Savings by MinimiGökhanNo ratings yet
- Kenny 2014Document5 pagesKenny 2014Ángel AranaNo ratings yet
- Critical Appraisal of The International Subarachnoid Aneurysm Trial (ISAT)Document7 pagesCritical Appraisal of The International Subarachnoid Aneurysm Trial (ISAT)Setiawan Arif WibowoNo ratings yet
- Guiding Goal-Directed TherapyDocument16 pagesGuiding Goal-Directed TherapyValeriy LevinNo ratings yet
- Anesthesiology 2015Document11 pagesAnesthesiology 2015The Vancouver SunNo ratings yet
- HHS Public Access: The Cost of Conversion in Robotic and Laparoscopic Colorectal SurgeryDocument16 pagesHHS Public Access: The Cost of Conversion in Robotic and Laparoscopic Colorectal SurgeryYassine BahrNo ratings yet
- Innovation Value and Reimbursement in Radiation AnDocument10 pagesInnovation Value and Reimbursement in Radiation AnGregorius HocevarNo ratings yet
- Robotic-Assisted Versus Laparoscopic Cholecystectomy: Outcome and Cost Analyses of A Case-Matched Control StudyDocument7 pagesRobotic-Assisted Versus Laparoscopic Cholecystectomy: Outcome and Cost Analyses of A Case-Matched Control StudyAndrei GheorghitaNo ratings yet
- Economics of Stem Cell Transplantation For Lymphoma: Counting The Cost of LivingDocument3 pagesEconomics of Stem Cell Transplantation For Lymphoma: Counting The Cost of LivingJNo ratings yet
- Hemodialise MBE CKJ 2021Document14 pagesHemodialise MBE CKJ 2021anderson roberto oliveira de sousaNo ratings yet
- tmp78F6 TMPDocument16 pagestmp78F6 TMPFrontiersNo ratings yet
- Lary24916 PDFDocument8 pagesLary24916 PDFDara SNo ratings yet
- Terapi CairanDocument5 pagesTerapi CairanZikry SitaniaNo ratings yet
- Does The Number of Operating Specialists Influence The Conversion Rate and Outcomes After Laparoscopic Colorectal Cancer Surgery?Document7 pagesDoes The Number of Operating Specialists Influence The Conversion Rate and Outcomes After Laparoscopic Colorectal Cancer Surgery?Yassine BahrNo ratings yet
- A Cost-Effectitveness Analysis of An In-Hospital Clinical Pharmacist ServiceDocument8 pagesA Cost-Effectitveness Analysis of An In-Hospital Clinical Pharmacist Servicetifanny carolinaNo ratings yet
- p2 - Patients and Carers Experiences of InteractingDocument12 pagesp2 - Patients and Carers Experiences of InteractingShruthi KrishnamoorthyNo ratings yet
- Cherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyDocument10 pagesCherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyShareDialysisNo ratings yet
- PIIS0748798322004966Document10 pagesPIIS0748798322004966grigmihNo ratings yet
- Critical Care - Full Text - Economic Analyses of Venous Thromboembolism Prevention Strategies in Hospitalized Patients - A Systematic ReviewDocument8 pagesCritical Care - Full Text - Economic Analyses of Venous Thromboembolism Prevention Strategies in Hospitalized Patients - A Systematic ReviewKathryn DunlapNo ratings yet
- CC 9070Document15 pagesCC 9070ossinNo ratings yet
- Healthcare 08 00077Document17 pagesHealthcare 08 00077gabriel-lNo ratings yet
- King's Research Portal: 10.12968/jowc.2020.29.12.751Document38 pagesKing's Research Portal: 10.12968/jowc.2020.29.12.751PaoloLansangNo ratings yet
- Mortality and Infectious Complications of Therapeutic Endovascular Interventional Radiology: A Systematic and Meta-Analysis ProtocolDocument8 pagesMortality and Infectious Complications of Therapeutic Endovascular Interventional Radiology: A Systematic and Meta-Analysis ProtocolgtNo ratings yet
- Noninvasive Monitoring 2016Document6 pagesNoninvasive Monitoring 2016Maria LaiaNo ratings yet
- Hepb y RTX PDFDocument3 pagesHepb y RTX PDFYeli VeMeNo ratings yet
- ArticleDocument9 pagesArticleAna Lazar IvanNo ratings yet
- Analysis of Blood Cross-Match Ordering Practice in Surgical Patients at Ndola Central HospitalDocument7 pagesAnalysis of Blood Cross-Match Ordering Practice in Surgical Patients at Ndola Central HospitalCandy CarlaNo ratings yet
- BEST Kidney StudyDocument10 pagesBEST Kidney StudyJoseph Zenas JungNo ratings yet
- LRB 2022 0029Document9 pagesLRB 2022 0029Dewa Gede Gangga KusumaNo ratings yet
- Critical Analysis of Quality of Life and Cost EfectivenessDocument19 pagesCritical Analysis of Quality of Life and Cost EfectivenessMarce SiuNo ratings yet
- Measure PDFDocument9 pagesMeasure PDFquirinalNo ratings yet
- Pi Is 0007091221007339Document18 pagesPi Is 0007091221007339Jeremy WongNo ratings yet
- Introduction To The Postanaesthetic Care Unit: Review Open AccessDocument7 pagesIntroduction To The Postanaesthetic Care Unit: Review Open AccessSamsul BahriNo ratings yet
- WFSA UpdateDocument60 pagesWFSA UpdateSyaiful FatahNo ratings yet
- PALMER2013Document19 pagesPALMER2013Andreyson SilvaNo ratings yet
- Bmri2021 6811373Document11 pagesBmri2021 68113738bnrzb5xpqNo ratings yet
- Economic Analysis and Budget Impact of Clostridial Collagenase Ointment Compared With Medicinal Honey For Treatment of Pressure Ulcers in The USDocument10 pagesEconomic Analysis and Budget Impact of Clostridial Collagenase Ointment Compared With Medicinal Honey For Treatment of Pressure Ulcers in The USItaloLozanoPalominoNo ratings yet
- Content ServerDocument20 pagesContent ServerAnatha ChrisciliaNo ratings yet
- Military NursingDocument6 pagesMilitary Nursingdwirinanti90215No ratings yet
- Safety ChecklistDocument8 pagesSafety ChecklistdharmaNo ratings yet
- Nguyen 2019Document6 pagesNguyen 2019ClintonNo ratings yet
- Surgery: SciencedirectDocument7 pagesSurgery: SciencedirectAriska Nur FitrianaNo ratings yet
- Effect of Gap Length and Position On Results of Treatment of Cancer of The Larynx in Scotland by Radiotherapy.. A Linear Quadratic AnalysisDocument9 pagesEffect of Gap Length and Position On Results of Treatment of Cancer of The Larynx in Scotland by Radiotherapy.. A Linear Quadratic AnalysisrgergerNo ratings yet
- Drummonds Checklist ExerciseDocument6 pagesDrummonds Checklist Exerciseknamrata0657No ratings yet
- Research ArticleDocument7 pagesResearch ArticleYosia KevinNo ratings yet
- Laboratory QADocument8 pagesLaboratory QAAnkush SinghalNo ratings yet
- AmbulasiDocument12 pagesAmbulasiRafii KhairuddinNo ratings yet
- Anesth Analg-2012-Corcoran-640-51 PDFDocument12 pagesAnesth Analg-2012-Corcoran-640-51 PDFBijay KC100% (1)
- Optimizing Red Blood Cell Transfusion Practice: S. D. Surgenor, M. Hampers, and H. L. CorwinDocument10 pagesOptimizing Red Blood Cell Transfusion Practice: S. D. Surgenor, M. Hampers, and H. L. CorwinnadaNo ratings yet
- Acute Appendicitis: Position Paper, WSES, 2013: Review Open AccessDocument4 pagesAcute Appendicitis: Position Paper, WSES, 2013: Review Open AccessgamhaelNo ratings yet
- Robotics in General Surgery - A Systematic Cost Assessment - PMCDocument13 pagesRobotics in General Surgery - A Systematic Cost Assessment - PMCÁgoston János Csigi100% (1)
- s13643 022 02135 8 PDFDocument9 pagess13643 022 02135 8 PDFdeaalifiahNo ratings yet
- 2016 Article 284Document7 pages2016 Article 284NungkyNo ratings yet
- Catheter Related Infxts JANDocument20 pagesCatheter Related Infxts JANyvettejzNo ratings yet
- Y. AL HashmiDocument11 pagesY. AL HashmiAzam alausyNo ratings yet
- Delirium and Associated Length of Stay and Costs in Critically Ill PatientsDocument8 pagesDelirium and Associated Length of Stay and Costs in Critically Ill PatientsedavioNo ratings yet
- Correlation of Serum C-Reactive Protein, White Blood Count and Neutrophil Percentage With Histopathology Findings in Acute AppendicitisDocument6 pagesCorrelation of Serum C-Reactive Protein, White Blood Count and Neutrophil Percentage With Histopathology Findings in Acute Appendicitisyosep andrianu lorenNo ratings yet
- SLED Vs CRRT PDFDocument9 pagesSLED Vs CRRT PDFquilino2012No ratings yet
- Revised OCRA Checklist BookDocument60 pagesRevised OCRA Checklist BookAndré100% (1)
- Sales Salise BelgiraDocument30 pagesSales Salise BelgiraManilyn Villarey100% (1)
- Gas LawsDocument20 pagesGas LawsDavidNo ratings yet
- Presented by Luciano Jerez ChavesDocument42 pagesPresented by Luciano Jerez ChavesMahmoud BersaliNo ratings yet
- Switch Machines m23Document2 pagesSwitch Machines m23Salvatore JimenoNo ratings yet
- Synopsis of Pharmacy Management System 2-1Document16 pagesSynopsis of Pharmacy Management System 2-1parv saxenaNo ratings yet
- CRC Handbook of Chemistry and Physics 95th EditionDocument2 pagesCRC Handbook of Chemistry and Physics 95th EditionCARLOSNo ratings yet
- TOE80 (Good Quality)Document30 pagesTOE80 (Good Quality)tomaszNo ratings yet
- Midea MSV1 07 09 12HRN1 CRN1Document37 pagesMidea MSV1 07 09 12HRN1 CRN1Giselma ZéoNo ratings yet
- A 12-Bit Multichannel ADC For Pixel Detectors in ParticleDocument7 pagesA 12-Bit Multichannel ADC For Pixel Detectors in ParticleY chenNo ratings yet
- Preparation and Properties of Compounds-03 - Assignments (New)Document12 pagesPreparation and Properties of Compounds-03 - Assignments (New)Raju SinghNo ratings yet
- Iocl ReportDocument51 pagesIocl ReportChandanKumarSinghNo ratings yet
- Design of Parking SystemDocument59 pagesDesign of Parking SystemvnitceNo ratings yet
- Quants For Mba ExamsDocument56 pagesQuants For Mba ExamsVallankan100% (10)
- Physical Chemistry IIDocument22 pagesPhysical Chemistry IIJamaica FielNo ratings yet
- 8051 Vs Motorola 68HC11Document19 pages8051 Vs Motorola 68HC11zuanne83No ratings yet
- List of Algorithms - Wikipedia, The Free EncyclopediaDocument34 pagesList of Algorithms - Wikipedia, The Free EncyclopediaPollen AhmedNo ratings yet
- MiCOM P341Document8 pagesMiCOM P341AsadAliAwan100% (1)
- EMX - 00 - 008b - 007 - TP - 001-A - En-Grid CodeTest Procedure Plant CapabilityDocument56 pagesEMX - 00 - 008b - 007 - TP - 001-A - En-Grid CodeTest Procedure Plant CapabilityRichardLemusNo ratings yet
- Work, Power and Energy: JeeprogressDocument46 pagesWork, Power and Energy: JeeprogressRahul KumarNo ratings yet
- Mathematics Scheme of Learning For JHS 1Document3 pagesMathematics Scheme of Learning For JHS 1Ransford Agyenim BoatengNo ratings yet
- FALCENTDocument2 pagesFALCENTJhea VelascoNo ratings yet
- Homework 6 Induction Motor 1 - de La CruzDocument3 pagesHomework 6 Induction Motor 1 - de La CruzAlvaro De La CruzNo ratings yet
- Shri Vaishnav Institute of Technology & ScienceDocument7 pagesShri Vaishnav Institute of Technology & ScienceSaijal SharmaNo ratings yet
- Bearing Gard™: Distributor 101Document46 pagesBearing Gard™: Distributor 101riinNo ratings yet
- Oe 23 7 9052Document22 pagesOe 23 7 9052محمد امین نیشابوریNo ratings yet
- SAIS MPS q4-SY2022-2023Document31 pagesSAIS MPS q4-SY2022-2023ilyn dutadoNo ratings yet
Hem 3
Hem 3
Uploaded by
Septian AndriantoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hem 3
Hem 3
Uploaded by
Septian AndriantoCopyright:
Available Formats
Original article
doi:10.1111/j.1463-1318.2009.01889.x
Economic evaluation of the treatment of grade II haemorrhoids: a comparison of stapled haemorrhoidopexy and rubber band ligation
L. McKenzie*, R. de Verteuil*, J. Cook, V. Shanmugam, M. Loudon, A. J. M. Watson and L. Vale*
*Health Economics Research Unit, Health Services Research Unit, University of Aberdeen, Aberdeen, UK, Department of Surgery, Aberdeen Royal Inrmary, Aberdeen, UK and Department of Surgery, Manchester Royal Inrmary, Manchester, UK Received 23 December 2008; accepted 3 March 2009; Accepted Article online 13 April 2009
Abstract
Objectives Haemorrhoidal disease is a common condition causing considerable distress to individuals and signicant cost to healthcare services. This paper explored the cost-effectiveness of stapled haemorrhoidopexy (SH) compared with the non-surgical intervention, rubber band ligation (RBL), for grade II symptomatic circumferential haemorrhoids. Method An economic evaluation alongside a randomized controlled trial conducted between October 2002 and February 2005. Adults were recruited and randomized to either SH or RBL. The same surgeon performed all procedures and investigators were blinded until analyses were completed. Primary outcomes measured at 52 weeks were cumulative costs to the NHS, clinical diagnosis of recurrence and quality adjusted life years (QALYs). Results Sixty symptomatic men and women with conrmed clinical diagnosis of grade II symptomatic haemorrhoids were randomized. Loss to follow-up was up to 10% at 52 weeks. The mean cost for SH was greater than RBL (mean difference: 1483, 95% CI: 13391676); disease recurrence was lower (OR = 0.18, 95% CI: 0.03 0.86); and there was no evidence of a statistically signicant difference in QALYs ()0.014, 95% CI: 0.076 to 0.051). SH was associated with a modest incremental cost per recurrence avoided at 12 months follow-up (4945). Based on current data, it was considered highly unlikely to be cost-effective in terms of incremental cost per QALY. Conclusions There is insufcient evidence about the cost-effectiveness of SH for grade II haemorrhoids to recommend its routine use in place of RBL. Further information is needed from larger trials with a longer-term follow-up to inform subsequent economic evaluation. Keywords Cost-effectiveness analysis, haemorrhoids, randomised controlled trial, rubber band ligation, stapled haemorrhoidopexy.
Introduction
Haemorrhoidal disease is one of the commonest benign ano-rectal conditions and is associated with relapsing and remitting symptoms. The majority of patients (75%) diagnosed with second-degree haemorrhoids require treatment within a few years [1]. Early intervention may avoid advanced disease and its associated complications. The current standard treatment for symptomatic grade II haemorrhoids, rubber band ligation (RBL), is readily available, can be performed as an out-patient
Correspondence to: Luke Vale, Health Economics Research Unit, University of Aberdeen, Foresterhill, Aberdeen, AB25 2ZD, UK. E-mail: l.vale@abdn.ac.uk
procedure, is tolerated well and does not require general anaesthesia [1]. As a consequence, the cost per procedure is relatively low. This technique, however, is associated with a treatment failure rate of more than 40% [2,3] and the return of symptoms will reduce quality of life and require lead to further costly treatment. Excisional haemorrhoidectomy (EH) is considered the gold standard treatment for advanced (grades III and IV) haemorrhoids and remains the most commonly performed surgical intervention [4]. A systematic review comparing EH with RBL has shown no signicant difference in the clinical effectiveness for grade II haemorrhoids. Furthermore, EH was shown to be associated with increased incidence of complications [5].
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
587
Economic evaluation of the treatment of grade II haemorrhoidsf
L. McKenzie et al.
Stapled haemorrhoidopexy (SH) is an alternative surgical intervention accepted and performed widely because of its clinical success [68]. It shares a similar mechanism of action to RBL by addressing haemorrhoidal prolapse and bleeding while maintaining the presence of the anal cushions. It acts by relocating the haemorrhoidal cushions cranially into their original position by excising a strip of lower rectal mucosa (pain insensitive mucosa) and by interrupting the blood supply to the haemorrhoids. It is, however, more costly than RBL. There is very limited literature evidence available comparing SH with RBL for grades III and IV haemorrhoids [9] and there is no data available for grade II haemorrhoids. In view of the relatively high recurrence rate for symptoms following RBL and the lack of comparative studies against SH and the difference in treatment cost, we conducted a pilot study to compare these two techniques in a randomized controlled setting. This economic evaluation, conducted alongside the randomized controlled trial (RCT), sought to assess the costeffectiveness of SH compared with RBL for grade II symptomatic haemorrhoids.
follow-up events, both for secondary care and primary care. As detailed below, resource usage was recorded as part of the trial for each individual patient and wherever possible, unit costs for these resources were identied at the individual patient level. At initial treatment visits and all scheduled follow-up visits at 6, 26 and 52 weeks hospital resource use was recorded using data collection forms for each patient. Information recorded included the anaesthetic time (for SH), length of time for the procedures, recovery time and postprocedure stay in ward, duration of any inpatient stay and medications. Details of any unscheduled hospital visits, primary care contacts, over the counter medications and prescriptions were obtained from a self-reported patient questionnaire completed at 6, 26 and 52 weeks postrandomization. Details of the methods used to derive resource used to provide the two procedures are described below.
Operative costs
Method
Description of trial
The trial was a pragmatic, randomized, controlled trial comparing SH with RBL for grade II haemorrhoids. Further details of the trial are reported elsewhere [9], but in brief 60 participants were recruited from one centre in Aberdeen Scotland, between October 2002 and February 2005, and randomized to either SH (n = 30) or RBL (n = 30). Patients with associated colonic malignancy, symptomatic anal sphincter damage or ano-rectal sepsis were excluded from the trial. Written informed consent was obtained from all eligible participants and the Grampian Research Ethics Committee approved the study (Ethics committee approval code GREC 01 0297). Participants who were randomized to SH would, if symptoms had not resolved, be eligible for two repeat procedures. This was assessed at a 6-week, 26week or 52-week follow-up or at a re-presentation. RBL patients were eligible for a maximum of four repeat procedures. Longer-term recurrence rates for both the treatments were assessed at 40.7 ( 6.3) months. All analyses were conducted on an intention to treat basis.
Measurement of costs
Costs included healthcare resource costs (from the perspective of the NHS) for initial treatment and
The resources required for RBL were based on the procedure being performed in an outpatient setting. Details of the staff involved were recorded on a case report form completed at the time of surgery. Also included on this form were details of the postdischarge medication and the use of consumables (disposable rubber band applicator, disposable proctoscope) required for the procedure. Resource costs for SH included theatre running costs, assumed to include an element for recovery facilities, were derived from the published sources [10] to establish a theatre cost. The cost of staff involved in theatre was based upon the number and grade-specic healthcare professionals necessary for each procedure. Operative costs relating to surgical repair of haemorrhoids (including consumables, drugs, equipment and sterilization) for the two interventions studied were sourced from the hospital pharmacy and measured prospectively. The cost of reusable items were converted into annual costs (when it was believed, the equipment would last more than 1 year using a discount rate of 3.5% [11]). This value was divided by the amount of time the equipment would be used in a year to give a cost per patient. In the instance that a patient experienced a recurrence, the overall resource use of the repeat surgery was assumed to be the mean value of the original surgical procedure across all the patients. A summary of the costs used in the analysis is provided in Table 1. All costs are at calculated in 2004 prices and inated to 2006 2007 prices using the hospital pay and prices ination index [12].
588
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
L. McKenzie et al.
Economic evaluation of the treatment of grade II haemorrhoids
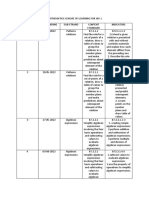
Table 1 Unit costs.
Unit cost ()
Source
Operative event: stapled haemorrhoidopexy procedure Operative event Equipment and drugs 389.32 Hospital pharmacy Cost per min in pre-op (anaesthetic room) 1.47 10 Cost per min in theatre 3.37 10 Cost per min in recovery 0.29 10 Cost per min for theatre overheads 9.74 10 Hospital stay Day case 28.19 10 In-patient 138.12 10 Operative event: rubber band ligation procedure Operative event Equipment and drugs 26.97 Hospital pharmacy Hospital stay Out-patient 74.82 10 Post discharge events (for both rubber band ligation and stapled haemorrhoidopexy) Contact with health professionals GP visit 17.35 16 Visits by nurse 11.93 16 Out-patient visits 74.82 16 Telephone consultation 20.60 16 GP home visit out of hours visits 54.22 16 Sanitary pad 2.05 Chemist and druggist 0.00 Discharge medication Laxative 2.64 17 Antibiotic 0.67 17 haemorrhoidal cream 7.32 17 Analgesic 1.84 17 Anaesthetic 1.52 17 17 Prescriptions Antihistamine 0.34 17 Analgesic 1.03 17 Laxative 2.52 17 Antibiotics 0.67 17 Anti-inammatory 2.85 17 haemorrhoidal cream 5.81 17 Anti-fungal cream 2.58 17 Repeat RBL Mean RBL Repeat stapled haemorrhoidopexy Mean stapling Hospital stay Day-case 28.19 10 In-patient 138.12 10
Effectiveness
Clinical effectiveness was measured in terms of whether or not the treatment had failed over the 52 weeks following initial treatment. At the 52-week follow-up, a clinical assessment was made using proctoscopy and symptom enquiry. This was performed by an experienced consultant colorectal surgeon who was blinded to the
original intervention. Further assessment of clinical effectiveness was undertaken at a mean follow-up of 40.7 ( 6.3) months. Quality of life was measured using the EQ-5D questionnaire. Each patient was asked to complete the EQ-5D at baseline, 3, 6, 26 and 52 weeks. Quality adjusted life years (QALYs) were calculated from the EQ-5D responses using UK population tariffs [13].
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
589
Economic evaluation of the treatment of grade II haemorrhoidsf
L. McKenzie et al.
Differences between three groups were based on linear regression adjusting for the EQ-5D score at baseline [14].
Cost-effectiveness
The incremental cost per recurrence avoided was estimated by combining the estimates of incremental costs and the difference in recurrence rates. Similarly, using the estimates of incremental cost and QALYs, the incremental cost per QALY was estimated. No discounting of costs and effects was performed, as the time horizon was only 1 year. Non-parametric Bootstrap methods were used for statistical inference on total costs, QALYs and cost per QALY because of skewed distributions [15].
Sensitivity analysis
base case analysis, the mean difference in QALYs was estimated using information from those trial participants who had utility scores available at each time point. The drawback of this approach is that a participant would be excluded if data for that participant were available only for three of the four time points, approximately 10% of responses were missing. A second approach was therefore adopted. In this, the missing data were imputed from the most recent previous score that was available.
Results
A total of 69 patients were identied from clinic or direct access endoscopy, of which two patients were subsequently deemed unsuitable (one recent RBL and another unsuitable for anaesthesia). Details of the trial were presented to the remaining 67 patients, 66 of whom chose to participate. Of these, 64 were considered suitable for randomization. Four patients were then excluded (one could not attend hospital due to personal commitment and three were not recruited for want of base line data due to technical reasons) leaving a total of 60 eligible patients who were randomized (by computer) to either RBL or SH. Complete data were available for 54 patients at the end of the trial period (two withdrew early, four moved and forwarding addresses were not obtainable before the nal follow-up). The baseline characteristics and clinical outcomes for this trial are reported elsewhere [9].
Healthcare costs
In economic evaluation, sensitivity analysis is used to address concerns which might relate to such issues as whether the methods of estimating data inuence the conclusions or whether data are generalizable to other settings. In this analysis, there is uncertainty about the magnitude of any difference in cost. The total cost per patient was recalculated using alternative values for the procedure cost. This was done separately for SH and RBL. For SH, the initial procedure cost (and similarly the cost per re-treatment) was reduced by 25% and by 50%. For RBL, initial procedure cost (and cost per retreatment) was increased by 50% and by 100%. With respect to the precision surrounding estimates of the incremental cost per recurrence avoided the cost effectiveness results were re-estimated using the extreme values of the 95% condence intervals for the difference in total costs and recurrence rates. This was done using best case and worst case scenarios for the SH procedure. A further area addressed in the sensitivity analysis was the impact of imputing missing quality-of-life data. In the
The mean total cost per patient, both in aggregate and separately for each element of healthcare is presented in Table 2. These are rounded to the nearest pound. The mean cost per patient treated using SH was signicantly higher than that for RBL (1757 compared to 273). Much of this difference can be attributed to the initial
Table 2 Mean healthcare costs per patient (costs rounded to nearest ) over a 12 month period. Stapled haemorrhoidopexy (SD) 30 30 1647 ()227) 31 ()174) 18 ()2) 3 ()5) 15 ()30.36) 41 ()121) 1,757 ()346) Mean difference* 95% condence interval
Mean cost per case* n Valid n Procedure cost Re-treatment cost Discharge medication Prescription costs Primary care contacts Secondary care contacts Total cost per case
RBL (SD) 30 30 102 (0) 64 ()105) 14 ()2) 1 ()3) 4 ()11) 91 ()152) 273 ()246)
P-value
)1545 33 )4 )2 )12 50 )1483
< 0.000 0.380 < 0.000 0.122 0.053 0.165 < 0.000
)1630 to1461 )42 to 107 )5 to)3 )4 to 0 )24 to 0 )22 to 123 )1676 to1339
*Costs are rounded to nearest pound. Summation errors may be attributed to rounding. Based on the 2.5 and 97.5 percentile from the bootstrapping.
590
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
L. McKenzie et al.
Economic evaluation of the treatment of grade II haemorrhoids
procedure cost which is relatively high for SH (1647 vs 102 for RBL) due to the cost of the disposable stapling gun (336) along with drugs and staff costs incurred in theatre, plus the hospital stay requirement.
Incremental cost per recurrence
Incremental cost per QALY
Recurrence rate at 52 weeks was signicantly higher in the RBL treatment group than the stapling group [11 (41%), n = 27, compared to 3 (11%), n = 27; OR = 0.18 (95% CI: 0.030.86), P = 0.028). This gave an incremental cost per recurrence avoided from SH of 4945. At a mean follow-up of 40.7 ( 6.3) months the recurrence rates were 12 out of 22 patients for whom data were available in the RBL group and 4 out of 24 patients in the stapling group, OR = 0.22 (95% CI: 0.040.92). This gives an incremental cost per recurrence of 3917. This estimate excludes treatment costs incurred after the rst year.
Table 3 EQ-5D and estimated quality adjusted life years. EQ-5D score Scenario Available data only Treatment SH RBL Difference SH RBL Difference Baseline 0.75 0.79 0.041 0.73 0.80 0.065 6 weeks 0.87 0.85 0.027 0.84 0.85 0.011
Quality Adjusted Life Years and the EQ-5D scores at baseline and at 52 weeks are reported in Table 3. Four patients in each treatment group had missing values for EQ-5D data at one or more time points. The mean value for QALYs was higher for the RBL patients than those treated with SH, although the condence intervals were wide. In terms of mean incremental cost per QALY, RBL dominated SH (RBL was associated with lower mean cost and greater mean QALYs than the SH group).
Sensitivity analysis
The results of the sensitivity analyses described in the methods are presented in Table 4. Under each scenario for procedure costs and also for the best case scenario based on condence intervals for costs, RBL was the
26 weeks 0.88 0.90 0.038 0.86 0.91 0.026
52 Weeks 0.85 0.88 0.059 0.83 0.89 0.026
QALYs (95% CI)* 0.863 0.876 )0.0135 ()0.067 to 0.066) 0.866 0.880 )0.014 ()0.076 to 0.051)
Imputed data
QALYs based on adjustment for baseline EQ-5D score. *95% CI based on results of bootstrapping exercise. Based on cases with complete data for all EQ-5D scores. RBL (n = 26) and Stapled haemorrhoidopexy (n = 26). Table 4 Sensitivity analysis on increment al cost per recurrence avoided. Incremental cost per recurrence avoided () 3595 922 4732 4451 1210 26 008
Sensitivity analysis Adjustment to procedure cost
Scenario Cost of Stapled haemorrhoidopexy 25% lower; Base case value for RBL Cost of Stapled haemorrhoidopexy 50% lower; Base case value for RBL Cost of RBL 50% higher; Base case value for stapled haemorrhoidopexy Cost of RBL 100% higher; Base case value for Stapled haemorrhoidopexy Best case scenario for Stapled haemorrhoidopexy Worst case scenario for SH
RBL () 273 273 356 439 439 273
Stapled haemorrhoidopexy () 1337 917 1757 1757 917 1757
Incremental cost () 1064 644 1401 1318 478 1483
Incremental recurrence avoided 0.296 0.296 0.296 0.296 0.395* 0.057
Extreme value of condence interval
All costs rounded to nearest pound. *Based on extreme values from condence intervals.
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
591
Economic evaluation of the treatment of grade II haemorrhoidsf
L. McKenzie et al.
Table 5 Incremental cost per QALY for the base case and sensitivity analyses. Probability cost-effectiveness for different threshold values for societys willingness to pay for a QALY 10 000 0.0% 100.0% 0.0% 100.0% 0.1% 99.9% 1.3% 97.7% 20 000 1.2% 98.8% 0.5% 99.5% 2.4% 97.6% 9.8% 91.2% 30 000 7.0% 93.0% 2.7% 97.3% 7.6% 92.4% 16.6% 83.4% 50 000 17.8% 82.2% 9.9% 90.1% 16.6% 83.4% 23.9% 76.1%
Scenario QALYs based on cases with complete EQ-5D data QALYs where missing EQ-5D data has been imputed Costs of haemorrhoidopexy 75% of base case Costs of haemorrhoidopexy 50% of base case
Surgery SH RBL SH RBL SH RBL SH RBL
Cost () 1757 273 1757 273 1318 273 878 273
QALYs 0.863 0.876 0.866* 0.880 0.866* 0.880 0.866* 0.880
Incremental cost per QALY Dominated Dominated Dominated Dominated
SH, stapled haemorrhoidopexy; RBL, rubber band ligation. *Based on the mean value for RBL and the adjusted difference reported in Table 3.
dominant procedure in terms of the incremental cost per recurrence avoided. Table 5 shows that the base case results for incremental cost per QALY were also robust in terms of RBL being the dominant intervention for variations in procedure costs.
Discussion
With SH for grade II haemorrhoids, we found that at 52 weeks there was a statistically signicant reduction in recurrences which was associated with a relatively modest incremental cost per recurrence avoided, although it is a matter of judgement as to this additional benet is worth the extra cost. However, there was no evidence that this difference in the risk of recurrence translated into differences in quality of life. Furthermore, it was unlikely that SH would be considered cost-effective at threshold values for societys willingness to pay for a QALY based upon the 12-month data. The population in the trial was representative of those seen in practice and were all treated by a single surgeon with considerable experience in performing both procedures. Therefore, it might be expected that if there were benets to SH in terms of quality of life than these would be seen within this study. However, the relatively small size of the RCT on which this economic evaluation was based would render the results imprecise. Furthermore, the time horizon over which costs and effects were considered was only 52 weeks, although further information of recurrence rates was available for a mean follow-up of 40.7 months. Given the nding of increased recurrences in the RBL arm, the difference in cost might fall over a longer time horizon and that the quality of life
associated with the RBL arm would be reduced. Given that the benets from SH may persist into the future, it is possible to consider under what circumstances SH might be considered worthwhile. For example, if societys maximum value willingness to pay for a QALY was 20 000 [11] and the difference in cost was unchanged, then SH would need be associated with an average gain of 0.07 QALYs compared with RBL over the expected life time of a patient. This might occur if, on an average, patients who initially received RBL spent at least 0.6 years more with a recurrence (and patients with a recurrence returned to their pre-treatment quality of life). Numerous factors, including the long-term performance of both procedures, will affect estimates of cost-effectiveness but should differences in recurrence rates persist, then it is possible that the cost-effectiveness of SH might improve but further long-term data would need to incorporated into a well-designed economic model to explore this fully. The results of the analysis were sensitive to the costs associated with SH. Changes in management as well as in equipment can result in improvements in the costeffectiveness of this procedure. In terms of future research, a further larger scale RCT would be required. The design of this study might be informed by a modelling exercise in which value of information methods are used to determine an optimal design and sample size.
Conclusions
Based upon the data presented in this paper, it is unlikely that SH would be considered a cost-effectiveness treatment for grade II haemorrhoids and hence there is no
592
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
L. McKenzie et al.
Economic evaluation of the treatment of grade II haemorrhoids
basis to recommend its use in place of RBL. However, the risk of recurrence at 52 weeks and at a mean follow-up of 40.7 months following surgery is lower. Further information is needed from larger trials with a longer term follow-up before this conclusion should be revisited.
Acknowledgements
The authors are thankful to Gladys McPherson, computer programmer for her help with randomization. The authors also thank all the participants for their help with this study and the staff at Aberdeen Royal Inrmary. The authors are very grateful to Ethicon Endosurgery, A Johnson & Johnson Company for funding this trial and economic evaluation (ISRCTN registration number 23585705). The Health Services Research Unit and Health Economics Research Unit are funded by the Chief Scientist Ofce of the Scottish Governments Health Directorates. The views expressed are those of the authors.
References
1 Nisar PJ, Scholeeld JH. Managing haemorrhoids. Br Med J 2003; 327: 84751. 2 Komborozos VA, Skrekas GJ, Pissiotis CA. Rubber band ligation of symptomatic internal hemorrhoids: results of 500 cases. Dig Surg 2000; 17: 716. 3 Konings M, Debets JM, Baeten CG. Rubber band ligation of haemorrhoids: symptoms almost gone after 6-weeks, but many patients need re-treatment in the long run. Ned Tijdscdr Geneeskd 1999; 143: 12658. (abstract). 4 MacRae HM, McLeod SR. Comparison of haemorrhoidal treatment modalities: a meta-analysis. Dis Colon Rectum 1995; 38: 68794. 5 Shanmugam V, Thaha MA, Rabindranath KS, Campbell KL, Steele RJ, Loudon MA. Systematic review of randomized trials comparing rubber band ligation with excisional haemorrhoidectomy. Br J Surg 2005; 92: 14817.
6 Roswell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: a randomised controlled trial. Lancet 2000; 355: 7825. 7 Ho Y-H, Chong WK, Tsang C, Ho EUKW, Tsang CL, Seow-Cheon F. Stapled haemorrhoidal cost and effectiveness randomised controlled trial including incontinence scoring, anorectal manometry and endoanal ultrasound assessments up to three months. Dis Colon Rectum 2000; 34: 166675. 8 Mehigan BJ, Monson JRT, Hartley JE. Stapling procedure for haemorrhoids versus milligan morgan haemorrhoidectomy: a randomised controlled trial. Lancet 2000; 355: 7825. 9 Shanmugam V, Muthukumarasamy G, Cook JA, Vale L, Watson AJ, Loudon MA. Randomised controlled trial comparing rubber band ligation with stapled haemorrhoidopexy for grade II circumferential haemorrhoids longterm results. Colorectal Dis [Epub ahead of print 26 March 2009]. 10 Anonymous. (2004) Scottish Health Service Costs 2004. Information and Statistics Division, NHS Scotland, Edinburgh. 11 National Institute for Clinical Excellence. Guide to the Methods of Technology Appraisal (reference N0515). http:// www.nice.org.uk. (2004). 12 Curtis L. (2008) Unit Costs of Health and Social Care 2008. University of Kent, Canterbury. 13 Kind P, Hardman G, Macran S. (1999) UK population norms for EQ-5D. Discussion paper 172, Centre for Health Economics. York: University of York. 14 Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005; 14: 48796. 15 Briggs A, Gray A. Handling uncertainty when performing economic evaluation of healthcare interventions. Health Technol Assess 1999; 3: 1134. 16 Netten A, Curtis L. (2004) Unit Costs of Health and Social Care 2004. University of Kent, Canterbury. 17 British Medical Association Royal Pharmaceutical Society of Great Britain. 2005.
2010 The Authors. Journal Compilation 2010 The Association of Coloproctology of Great Britain and Ireland. Colorectal Disease, 12, 587593
593
Copyright of Colorectal Disease is the property of Wiley-Blackwell and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
You might also like
- Lesson01 FT125 Overview SiemensDocument10 pagesLesson01 FT125 Overview SiemensใบบอนสิชลNo ratings yet
- Fast Facts: Clinical Trials in Oncology: The fundamentals of design, conduct and interpretationFrom EverandFast Facts: Clinical Trials in Oncology: The fundamentals of design, conduct and interpretationNo ratings yet
- Introduction To GLFP On BPC NWDocument26 pagesIntroduction To GLFP On BPC NWSuyash PandeyNo ratings yet
- 106 Torque Settings PDFDocument5 pages106 Torque Settings PDFRicardo MatosNo ratings yet
- Bodansky-2017-Potential Cost Savings by MinimiDocument4 pagesBodansky-2017-Potential Cost Savings by MinimiGökhanNo ratings yet
- Kenny 2014Document5 pagesKenny 2014Ángel AranaNo ratings yet
- Critical Appraisal of The International Subarachnoid Aneurysm Trial (ISAT)Document7 pagesCritical Appraisal of The International Subarachnoid Aneurysm Trial (ISAT)Setiawan Arif WibowoNo ratings yet
- Guiding Goal-Directed TherapyDocument16 pagesGuiding Goal-Directed TherapyValeriy LevinNo ratings yet
- Anesthesiology 2015Document11 pagesAnesthesiology 2015The Vancouver SunNo ratings yet
- HHS Public Access: The Cost of Conversion in Robotic and Laparoscopic Colorectal SurgeryDocument16 pagesHHS Public Access: The Cost of Conversion in Robotic and Laparoscopic Colorectal SurgeryYassine BahrNo ratings yet
- Innovation Value and Reimbursement in Radiation AnDocument10 pagesInnovation Value and Reimbursement in Radiation AnGregorius HocevarNo ratings yet
- Robotic-Assisted Versus Laparoscopic Cholecystectomy: Outcome and Cost Analyses of A Case-Matched Control StudyDocument7 pagesRobotic-Assisted Versus Laparoscopic Cholecystectomy: Outcome and Cost Analyses of A Case-Matched Control StudyAndrei GheorghitaNo ratings yet
- Economics of Stem Cell Transplantation For Lymphoma: Counting The Cost of LivingDocument3 pagesEconomics of Stem Cell Transplantation For Lymphoma: Counting The Cost of LivingJNo ratings yet
- Hemodialise MBE CKJ 2021Document14 pagesHemodialise MBE CKJ 2021anderson roberto oliveira de sousaNo ratings yet
- tmp78F6 TMPDocument16 pagestmp78F6 TMPFrontiersNo ratings yet
- Lary24916 PDFDocument8 pagesLary24916 PDFDara SNo ratings yet
- Terapi CairanDocument5 pagesTerapi CairanZikry SitaniaNo ratings yet
- Does The Number of Operating Specialists Influence The Conversion Rate and Outcomes After Laparoscopic Colorectal Cancer Surgery?Document7 pagesDoes The Number of Operating Specialists Influence The Conversion Rate and Outcomes After Laparoscopic Colorectal Cancer Surgery?Yassine BahrNo ratings yet
- A Cost-Effectitveness Analysis of An In-Hospital Clinical Pharmacist ServiceDocument8 pagesA Cost-Effectitveness Analysis of An In-Hospital Clinical Pharmacist Servicetifanny carolinaNo ratings yet
- p2 - Patients and Carers Experiences of InteractingDocument12 pagesp2 - Patients and Carers Experiences of InteractingShruthi KrishnamoorthyNo ratings yet
- Cherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyDocument10 pagesCherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyShareDialysisNo ratings yet
- PIIS0748798322004966Document10 pagesPIIS0748798322004966grigmihNo ratings yet
- Critical Care - Full Text - Economic Analyses of Venous Thromboembolism Prevention Strategies in Hospitalized Patients - A Systematic ReviewDocument8 pagesCritical Care - Full Text - Economic Analyses of Venous Thromboembolism Prevention Strategies in Hospitalized Patients - A Systematic ReviewKathryn DunlapNo ratings yet
- CC 9070Document15 pagesCC 9070ossinNo ratings yet
- Healthcare 08 00077Document17 pagesHealthcare 08 00077gabriel-lNo ratings yet
- King's Research Portal: 10.12968/jowc.2020.29.12.751Document38 pagesKing's Research Portal: 10.12968/jowc.2020.29.12.751PaoloLansangNo ratings yet
- Mortality and Infectious Complications of Therapeutic Endovascular Interventional Radiology: A Systematic and Meta-Analysis ProtocolDocument8 pagesMortality and Infectious Complications of Therapeutic Endovascular Interventional Radiology: A Systematic and Meta-Analysis ProtocolgtNo ratings yet
- Noninvasive Monitoring 2016Document6 pagesNoninvasive Monitoring 2016Maria LaiaNo ratings yet
- Hepb y RTX PDFDocument3 pagesHepb y RTX PDFYeli VeMeNo ratings yet
- ArticleDocument9 pagesArticleAna Lazar IvanNo ratings yet
- Analysis of Blood Cross-Match Ordering Practice in Surgical Patients at Ndola Central HospitalDocument7 pagesAnalysis of Blood Cross-Match Ordering Practice in Surgical Patients at Ndola Central HospitalCandy CarlaNo ratings yet
- BEST Kidney StudyDocument10 pagesBEST Kidney StudyJoseph Zenas JungNo ratings yet
- LRB 2022 0029Document9 pagesLRB 2022 0029Dewa Gede Gangga KusumaNo ratings yet
- Critical Analysis of Quality of Life and Cost EfectivenessDocument19 pagesCritical Analysis of Quality of Life and Cost EfectivenessMarce SiuNo ratings yet
- Measure PDFDocument9 pagesMeasure PDFquirinalNo ratings yet
- Pi Is 0007091221007339Document18 pagesPi Is 0007091221007339Jeremy WongNo ratings yet
- Introduction To The Postanaesthetic Care Unit: Review Open AccessDocument7 pagesIntroduction To The Postanaesthetic Care Unit: Review Open AccessSamsul BahriNo ratings yet
- WFSA UpdateDocument60 pagesWFSA UpdateSyaiful FatahNo ratings yet
- PALMER2013Document19 pagesPALMER2013Andreyson SilvaNo ratings yet
- Bmri2021 6811373Document11 pagesBmri2021 68113738bnrzb5xpqNo ratings yet
- Economic Analysis and Budget Impact of Clostridial Collagenase Ointment Compared With Medicinal Honey For Treatment of Pressure Ulcers in The USDocument10 pagesEconomic Analysis and Budget Impact of Clostridial Collagenase Ointment Compared With Medicinal Honey For Treatment of Pressure Ulcers in The USItaloLozanoPalominoNo ratings yet
- Content ServerDocument20 pagesContent ServerAnatha ChrisciliaNo ratings yet
- Military NursingDocument6 pagesMilitary Nursingdwirinanti90215No ratings yet
- Safety ChecklistDocument8 pagesSafety ChecklistdharmaNo ratings yet
- Nguyen 2019Document6 pagesNguyen 2019ClintonNo ratings yet
- Surgery: SciencedirectDocument7 pagesSurgery: SciencedirectAriska Nur FitrianaNo ratings yet
- Effect of Gap Length and Position On Results of Treatment of Cancer of The Larynx in Scotland by Radiotherapy.. A Linear Quadratic AnalysisDocument9 pagesEffect of Gap Length and Position On Results of Treatment of Cancer of The Larynx in Scotland by Radiotherapy.. A Linear Quadratic AnalysisrgergerNo ratings yet
- Drummonds Checklist ExerciseDocument6 pagesDrummonds Checklist Exerciseknamrata0657No ratings yet
- Research ArticleDocument7 pagesResearch ArticleYosia KevinNo ratings yet
- Laboratory QADocument8 pagesLaboratory QAAnkush SinghalNo ratings yet
- AmbulasiDocument12 pagesAmbulasiRafii KhairuddinNo ratings yet
- Anesth Analg-2012-Corcoran-640-51 PDFDocument12 pagesAnesth Analg-2012-Corcoran-640-51 PDFBijay KC100% (1)
- Optimizing Red Blood Cell Transfusion Practice: S. D. Surgenor, M. Hampers, and H. L. CorwinDocument10 pagesOptimizing Red Blood Cell Transfusion Practice: S. D. Surgenor, M. Hampers, and H. L. CorwinnadaNo ratings yet
- Acute Appendicitis: Position Paper, WSES, 2013: Review Open AccessDocument4 pagesAcute Appendicitis: Position Paper, WSES, 2013: Review Open AccessgamhaelNo ratings yet
- Robotics in General Surgery - A Systematic Cost Assessment - PMCDocument13 pagesRobotics in General Surgery - A Systematic Cost Assessment - PMCÁgoston János Csigi100% (1)
- s13643 022 02135 8 PDFDocument9 pagess13643 022 02135 8 PDFdeaalifiahNo ratings yet
- 2016 Article 284Document7 pages2016 Article 284NungkyNo ratings yet
- Catheter Related Infxts JANDocument20 pagesCatheter Related Infxts JANyvettejzNo ratings yet
- Y. AL HashmiDocument11 pagesY. AL HashmiAzam alausyNo ratings yet
- Delirium and Associated Length of Stay and Costs in Critically Ill PatientsDocument8 pagesDelirium and Associated Length of Stay and Costs in Critically Ill PatientsedavioNo ratings yet
- Correlation of Serum C-Reactive Protein, White Blood Count and Neutrophil Percentage With Histopathology Findings in Acute AppendicitisDocument6 pagesCorrelation of Serum C-Reactive Protein, White Blood Count and Neutrophil Percentage With Histopathology Findings in Acute Appendicitisyosep andrianu lorenNo ratings yet
- SLED Vs CRRT PDFDocument9 pagesSLED Vs CRRT PDFquilino2012No ratings yet
- Revised OCRA Checklist BookDocument60 pagesRevised OCRA Checklist BookAndré100% (1)
- Sales Salise BelgiraDocument30 pagesSales Salise BelgiraManilyn Villarey100% (1)
- Gas LawsDocument20 pagesGas LawsDavidNo ratings yet
- Presented by Luciano Jerez ChavesDocument42 pagesPresented by Luciano Jerez ChavesMahmoud BersaliNo ratings yet
- Switch Machines m23Document2 pagesSwitch Machines m23Salvatore JimenoNo ratings yet
- Synopsis of Pharmacy Management System 2-1Document16 pagesSynopsis of Pharmacy Management System 2-1parv saxenaNo ratings yet
- CRC Handbook of Chemistry and Physics 95th EditionDocument2 pagesCRC Handbook of Chemistry and Physics 95th EditionCARLOSNo ratings yet
- TOE80 (Good Quality)Document30 pagesTOE80 (Good Quality)tomaszNo ratings yet
- Midea MSV1 07 09 12HRN1 CRN1Document37 pagesMidea MSV1 07 09 12HRN1 CRN1Giselma ZéoNo ratings yet
- A 12-Bit Multichannel ADC For Pixel Detectors in ParticleDocument7 pagesA 12-Bit Multichannel ADC For Pixel Detectors in ParticleY chenNo ratings yet
- Preparation and Properties of Compounds-03 - Assignments (New)Document12 pagesPreparation and Properties of Compounds-03 - Assignments (New)Raju SinghNo ratings yet
- Iocl ReportDocument51 pagesIocl ReportChandanKumarSinghNo ratings yet
- Design of Parking SystemDocument59 pagesDesign of Parking SystemvnitceNo ratings yet
- Quants For Mba ExamsDocument56 pagesQuants For Mba ExamsVallankan100% (10)
- Physical Chemistry IIDocument22 pagesPhysical Chemistry IIJamaica FielNo ratings yet
- 8051 Vs Motorola 68HC11Document19 pages8051 Vs Motorola 68HC11zuanne83No ratings yet
- List of Algorithms - Wikipedia, The Free EncyclopediaDocument34 pagesList of Algorithms - Wikipedia, The Free EncyclopediaPollen AhmedNo ratings yet
- MiCOM P341Document8 pagesMiCOM P341AsadAliAwan100% (1)
- EMX - 00 - 008b - 007 - TP - 001-A - En-Grid CodeTest Procedure Plant CapabilityDocument56 pagesEMX - 00 - 008b - 007 - TP - 001-A - En-Grid CodeTest Procedure Plant CapabilityRichardLemusNo ratings yet
- Work, Power and Energy: JeeprogressDocument46 pagesWork, Power and Energy: JeeprogressRahul KumarNo ratings yet
- Mathematics Scheme of Learning For JHS 1Document3 pagesMathematics Scheme of Learning For JHS 1Ransford Agyenim BoatengNo ratings yet
- FALCENTDocument2 pagesFALCENTJhea VelascoNo ratings yet
- Homework 6 Induction Motor 1 - de La CruzDocument3 pagesHomework 6 Induction Motor 1 - de La CruzAlvaro De La CruzNo ratings yet
- Shri Vaishnav Institute of Technology & ScienceDocument7 pagesShri Vaishnav Institute of Technology & ScienceSaijal SharmaNo ratings yet
- Bearing Gard™: Distributor 101Document46 pagesBearing Gard™: Distributor 101riinNo ratings yet
- Oe 23 7 9052Document22 pagesOe 23 7 9052محمد امین نیشابوریNo ratings yet
- SAIS MPS q4-SY2022-2023Document31 pagesSAIS MPS q4-SY2022-2023ilyn dutadoNo ratings yet