Professional Documents
Culture Documents
NCPs For Diabetes Mellitus
NCPs For Diabetes Mellitus
Uploaded by
Ejie Boy IsagaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCPs For Diabetes Mellitus
NCPs For Diabetes Mellitus
Uploaded by
Ejie Boy IsagaCopyright:
Available Formats
You may also want to check these updated NCPs for Diabetes Mellitus: 1. 2. 3. 4. 5.
Risk for Infection Risk for Disturbed Sensory Perception Fatigue Imbalanced Nutrition Less Than Body Requirements Deficient Fluid Volume
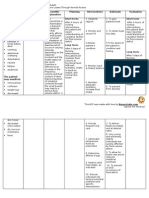
Deficient Fluid Volume Glucose appears in the urine (glycosuria) because the kidney excretes the excess glucose to make the blood glucose level normal. Glucose excreted in the urine acts as osmotic diuretic and causes excretion of increased amount of water, resulting in fluid volume deficit or polyuria. Nursing Diagnosis: Deficient Fluid Volume r/t intracellular DHN 2 the DM II Assessment Planning Nursing Interventions Rationale Evaluation
Short Term:After 3 of NI, patient shall have verbalized understanding of causative factors and purpose of Subjective: (none)Objective: individual therapeutic elevated temperature of interventions 38.4C/axilla and increased urine output. medications. sweating of the skin thirst Long Term: exhaustion weight loss After 2 days dry skin or mucous of NI, the membrane patient shall have maintained fluid volume at a functional level as evidenced by individual good skin turgor, moist
1. Establish rapport 2. Take and record vital signs 3. Monitor the temperature 4. Assess skin turgor and mucous membranes for signs of dehydration 5. Encourage the patient to increase fluid intake 6. Administer IVF as ordered by the Doctor 7. Administer anti-pyretic as prescribed by the Doctor.
1. Friendly Short relationship Term:After with patient 3 of NI, and to be patient will able to each have verbalized others understanding concern 2. To obtain of causative factors and baseline purpose of data 3. To monitor individual changes in therapeutic temperature interventions and 4. Dry skin and mucous medications. membranes are signs of Long Term: dehydration 5. To replace After 2 days fluid loss of NI, the and prevent patient will dehydration have 6. To replace maintained electrolytes fluid volume and fluid at a loss functional 7. To decrease level as body evidenced by temperature individual and will good skin have less turgor, moist
mucous membrane and stable vital signs.
occurrence mucous of membrane dehydration and stable . vital signs
Imbalanced Nutrition: Less Than Body Requirements Due to decrease of lack of insulin in the body, the glucose level continuously rises because glucose cannot be utilized without the presence of insulin. Glucose is the source of energy, while insulin is the vehicle to transport glucose to the body tissues. Because of decrease insulin level in the blood stream, the cells starved, leading to alteration of metabolism. The body needs glucose for metabolism; there will be a breakdown of energy reserved from adipose tissue, muscles and liver (glucagons). This will result to weight loss. But the energy breaks down, the glucose level continuously increase because there is less amount of insulin. The body tissues need to be fed, this will lead to polyphagia and polydipsia because the tissue are not being fed and need glucose for metabolism. NDx: Imbalanced Nutrition: less than body requirement r/t insulin deficiency Assessment Planning Nursing Interventions Rationale
Evaluation
Short Term:After 3 of NI, patient shall have verbalized understanding Subjective:Objective: of causative factors when poor muscle known and tone necessary generalized interventions weakness and identified increased thirst diabetic increased client. urination polyphagia Long Term: loss of weight After 1-4 months of NI, the patient shall have demonstrated weight gain toward goal.
1. Establish rapport 2. Ascertain understanding of individual nutritional needs 3. Discuss eating habits and encourage diabetic diet as prescribed by the Doctor 4. Document actual weight, do not estimate.Note total daily intake including patterns and time of eating. 5. Consult dietician/physician for further assessment and recommendation regarding food preferences and nutritional support
1. Friendly relationship Short with patient Term:After and to be 3 of NI, able to each patient will have others verbalized concern understandi 2. To determine of causative factors when what information known and necessary to be provided to intervention client/SO- and identifie 3. To achieve diabetic client. health needs of the patient with Long Term the proper food diet After 1-4 for is/her months of N diseasethe patient 4. Patient may will have be un aware demonstrate of their weight gain actual toward goal weight or
weight loss due to estimating weight. 5. To reveal changes that should be made in clients dietary intake- For greater understandi ng and further assessment of specific foods.
Fatigue Diabetes Mellitus is a group of metabolic diseases characterized by increased levels of glucose in the blood resulting from defects in insulin secretion, insulin action, or both. In type 2 diabetes, people have decreased sensitivity to insulin and impaired beta cell functioning resulting in decreased insulin production. Glucose derived from food cannot be stored in the liver thereby remaining into the bloodstream. The beta cells of the islets of Langerhans release glucagon which stimulates the liver to release the stored glucose. After 8 12 hours, the liver forms glucose from the breakdown of noncarboghydrate substances, including amino acids resulting to muscle wasting which results to weakness. Nursing Diagnosis: Fatigue RT decreased muscular strength Nursing Rationale Interventions Subjective:(none)Objective: 1. Assess 1. Response to an response to activity can be Short activity evaluated to generalized weakness Term:After 2. Assess muscle achieve desired increased respiratory 2-3 of nursing strength of level of rate of 25cpm interventions, patient and tolerance. presence of nonthe patient functional 2. To determine healing wound on will be able level of the level of both feet to identify activity. activity body weakness measures to 3. Discuss with 3. Education may wt. loss conserve and patient the provide fatigue increase need for motivation to limited ROM activity increase activity inability to perform body energy. 4. Alternate level even ADL Assessment Planning Evaluation The patient shall have been able to identify measures to conserve and increase body energyThe patient shall have been free from signs
altered VS altered sensorium
Long Term: After 3-5 days of nursing interventions, the patient will be free from signs of fatigue
activity with periods of rest/ uninterrupted sleep. 5. Monitor pulse, respiration rate and blood pressure before/after activity 6. Perform activity slowly with frequent rest periods 7. Promote energy conservation techniques by discussing ways of conserving energy while bathing, transferring and so on. 8. Provide adequate ventilation 9. Provide comfort and safety 10. Instruct patient to perform deep breathing exercises 11. Instruct client to increase Vitamins A, C and D and protein in her diet. 12. Instruct also patient to increase iron in diet 13. Administer oxygen as ordered.
though patient of fatigue may feel too weak initially 4. Prevents excessive fatigue-Indicates physiological levels of tolerance 5. Tolerance develops by adjusting frequency, duration and intensity until desired activity level is achieved. 6. Interventions should be directed at delaying the onset of fatigue and optimizing muscle efficiency. 7. Symptoms of fatigue are alleviated with rest. Also, patient will be able to accomplish more with a decreased expenditure of energy. 8. For proper oxygenation 9. To be free from injury 10. Promotes relaxation 11. For muscle strength and tissue repair 12. To prevent weakness and paleness 13. To provide
proper ventilation
Risk for Infection
Risks for infection is a increased probability of invasion of pathogenic organisms for a pt. with DM wound is possible in the furure. Clients with diabetes are susceptible to infections because of polymorphonuclear leukocyte function, diabetic neuropathies, and vascular insufficiency as a result is a poor glycemic control; thus making a wound to heal slowly because the damaged of the vascular system cannot carry sufficient oxygen, WBC, nutrients, and antibodies to the injured site. Thereby infections increase and enhance possibility of further complications.
Nursing Diagnosis: Risk for Infection Nursing Rationale Evaluation Interventions 1. Establish 1. to obtain rapport patients Short 2. Take and trust and Short Term:After record vital cooperation Term:The 4 hours of pt. shall signs 2. To obtain NPI the 3. Encourage baseline data have risks factors identified expression of 3. facilitates of feelings and grieving the risks occurrence factors of anxieties loss of infection 4. Observe non 4. non verbal occurrence will be verbal cues cues is more of infection reduce or 5. Encourage accurate than shall have control to a Subjective: client to look verbal cues- reduced or manageable (none)Objective: at/touch to begin to controlled level by a affected body incorporate to a clean bed 1. purulent discharge part changes into manageable and 2. hyperthermia 6. Encourage body image level by a maintain 3. altered circulation verbalization 5. to enhance clean bed skin intact 4. immunological of and role handling of and skin intact. deficit play potential Long anticipated problems Term: conflicts 6. to prevent Long 7. Encourage to dehydration Term: After 1-2 increase fluid 7. to boost weeks of intakeimmune The patient NPI, pt will increase Vit. system and shall be be free of C in the dietpromote free of purulent increase collagen purulent drainage or CHON intake formation- damage or erythema 8. Change for tissue erythema and be dressing repair and be febri afebrile 9. Provide a safe 8. to promote and quiet healing and Assessment Planning
environment 10. Take Due meds on time
prevent contaminatio n of the wound 9. To promote pts comfort 10. To met the bodys requirements
You might also like
- ENACb 1Document166 pagesENACb 1DarrylpnzNo ratings yet
- Diabetes Mellitus NCPDocument7 pagesDiabetes Mellitus NCPjfgnzls182892% (12)
- CA - Amniotic Fluid EmbolismDocument13 pagesCA - Amniotic Fluid EmbolismRodelen Maraño100% (2)
- Risk For Unstable Blood GlucoseDocument4 pagesRisk For Unstable Blood GlucosehallegendNo ratings yet
- Fluid Volume ExcessDocument4 pagesFluid Volume ExcessTamil Villardo100% (2)
- 8NCP's For ColostomyDocument23 pages8NCP's For ColostomyCzarina Porciuncula79% (14)
- A Requiem To Mother EarthDocument5 pagesA Requiem To Mother EarthSandra SabuNo ratings yet
- 3 Nursing Care Plan Diabetes MellitusDocument5 pages3 Nursing Care Plan Diabetes MellitusAnnisa Silvera II50% (2)
- Nursing Care Plans For Diabetes MellitusDocument12 pagesNursing Care Plans For Diabetes MellitusRaveen mayi85% (59)
- Nursing Care Plan For Diabetes Mellitus Type 2 (Kenneth Regida)Document3 pagesNursing Care Plan For Diabetes Mellitus Type 2 (Kenneth Regida)Kenneth Anthony Tiu Regida100% (8)
- Nursing Care Plan Diabetes 2Document3 pagesNursing Care Plan Diabetes 2inagasi83% (12)
- Diabetes Mellitus Nursing Care PlanDocument7 pagesDiabetes Mellitus Nursing Care PlanjamieboyRN91% (32)
- NCPDocument3 pagesNCPGimcy Dela Fuente100% (6)
- Tachycardia NCPDocument2 pagesTachycardia NCPRemita Hutagalung50% (4)
- Activity Intolerance Related To Decrease Blood FlowDocument3 pagesActivity Intolerance Related To Decrease Blood FlowDarkCeades100% (3)
- Hypothyroidism Nursing Care PlanDocument2 pagesHypothyroidism Nursing Care Planmrhammer1957100% (3)
- NCP - DMDocument4 pagesNCP - DMMonica Garcia88% (8)
- Accurately Measure The Patient's Weight and Height. For Baseline DataDocument2 pagesAccurately Measure The Patient's Weight and Height. For Baseline DataMonica RiveraNo ratings yet
- Assessment Inferen CE Plannin G Interve Ntion Rationa LE Evalua TionDocument4 pagesAssessment Inferen CE Plannin G Interve Ntion Rationa LE Evalua TionBg Celo33% (3)
- NCP Pleural EffusionDocument7 pagesNCP Pleural EffusionEjie Boy Isaga100% (2)
- DM NCPDocument7 pagesDM NCPMichael Anthony Cardenas Macaballug67% (3)
- Lanjutan NCP DMDocument14 pagesLanjutan NCP DMVera Andri YaniNo ratings yet
- Diabetes Mellitus NCPDocument5 pagesDiabetes Mellitus NCPCazze SunioNo ratings yet
- Nursing Care Plan For DM PatientDocument10 pagesNursing Care Plan For DM PatientRainier Rhett Concha100% (5)
- NCP For DM1Document2 pagesNCP For DM1Pau Hipol MadriagaNo ratings yet
- NCP - Diabetes Mellitus Type IIDocument10 pagesNCP - Diabetes Mellitus Type IIChristine Karen Ang SuarezNo ratings yet
- NCP - Excess Fluid Volume (Aortic Stenosis)Document3 pagesNCP - Excess Fluid Volume (Aortic Stenosis)Daniel Vergara Arce100% (3)
- Assessment Using Functional Health Patterns: AppendixDocument16 pagesAssessment Using Functional Health Patterns: AppendixNalzaro Emyril89% (19)
- NCP DiabetesDocument4 pagesNCP Diabeteskyshb67% (3)
- NCP DiabetesDocument3 pagesNCP DiabetesKartika MilaningrumNo ratings yet
- NCP Ineffective Tissue PerfusionDocument7 pagesNCP Ineffective Tissue Perfusionapi-283753722100% (3)
- Risk For Unstable Blood GlucoseDocument24 pagesRisk For Unstable Blood GlucoseFerreze Ann100% (1)
- NCP Imbalanced Nutrition Less Than Body RequirementsDocument5 pagesNCP Imbalanced Nutrition Less Than Body Requirementsrusnani100% (1)
- XI. Nursing Care Plan Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation SubjectiveDocument4 pagesXI. Nursing Care Plan Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation SubjectiveMartin Allen ClaudioNo ratings yet
- CRF Fluid Volume Excess NCPDocument3 pagesCRF Fluid Volume Excess NCPchubbielitaNo ratings yet
- NCP: Diabetes Mellitus Prepregnancy/GestationalDocument11 pagesNCP: Diabetes Mellitus Prepregnancy/GestationalJavie85% (13)
- NCP FVDDocument2 pagesNCP FVDMarlon AnryNo ratings yet
- NCP For Diabetes MellitusDocument2 pagesNCP For Diabetes MellitusNanes Tan75% (12)
- Ineffective Tissue PerfusionDocument1 pageIneffective Tissue PerfusionRhae RaynogNo ratings yet
- Assessment Diagnosis Rationale Expected Outcome Implementation Rationale EvaluationDocument5 pagesAssessment Diagnosis Rationale Expected Outcome Implementation Rationale EvaluationRazzel Daza100% (1)
- NCP For DMDocument14 pagesNCP For DMLynzzky Virtudes AbranNo ratings yet
- Nursing Care Plan DiabetesDocument2 pagesNursing Care Plan DiabetesJen Faye Orpilla100% (9)
- Anemia NCPDocument20 pagesAnemia NCPNursidar Pascual Mukattil80% (5)
- Deficient Fluid Volume (AGEDocument2 pagesDeficient Fluid Volume (AGENursesLabs.com83% (6)
- NCP Imbalanced Nutrition Less Than Body Requirements DIARRHEADocument2 pagesNCP Imbalanced Nutrition Less Than Body Requirements DIARRHEAMa. Elaine Carla TatingNo ratings yet
- NCP Hypertension 2Document3 pagesNCP Hypertension 2Roseben Somido50% (2)
- Short Term: Independent: Independent: Short TermDocument2 pagesShort Term: Independent: Independent: Short TermAndre ImperialNo ratings yet
- NCP EsrdDocument9 pagesNCP EsrdMarisol Dizon100% (1)
- NCPDocument4 pagesNCPAndrea BroccoliNo ratings yet
- Casestudy PTB2 Hemoptysis NCPDocument2 pagesCasestudy PTB2 Hemoptysis NCPSusie PadaoanNo ratings yet
- Diabetes Mellitus (DM) 2Document1 pageDiabetes Mellitus (DM) 2Bheru Lal100% (1)
- Activity Intolerance Related To AmeniaDocument1 pageActivity Intolerance Related To AmeniaSiti Syazana Mohamad MogriNo ratings yet
- NCP Deficient KnowledgeDocument1 pageNCP Deficient KnowledgeLouie Siazon Vasquez100% (1)
- NCP For UtiDocument3 pagesNCP For UtiAaron Sanchez100% (1)
- Risk For Impaired Skin Integrity and Readiness For Enhanced PowerDocument3 pagesRisk For Impaired Skin Integrity and Readiness For Enhanced PowerdanaNo ratings yet
- Nursing Care PlansDocument6 pagesNursing Care PlansTwobee Kriz LeghidNo ratings yet
- DM Care PlanDocument9 pagesDM Care PlanHarish Kumar KumawatNo ratings yet
- GastroenteritisDocument8 pagesGastroenteritistanlimdania100% (3)
- NCPGDMDocument8 pagesNCPGDMChristopher LontocNo ratings yet
- NCP CKDDocument9 pagesNCP CKDDanica Salinas100% (1)
- Deficit Vo. NCPDocument4 pagesDeficit Vo. NCPThessabelles Ebuen-PeñaNo ratings yet
- New Born NCPDocument8 pagesNew Born NCPCarl Vincent Marrion Rejuso100% (1)
- Lethargic Weakness Decreased Performance: Nursing Care PlanDocument2 pagesLethargic Weakness Decreased Performance: Nursing Care PlanZhayree R.No ratings yet
- Cues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale EvaluationDocument4 pagesCues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale EvaluationEjie Boy Isaga100% (1)
- Trait TheoryDocument6 pagesTrait TheoryEjie Boy Isaga100% (1)
- Drug StudyDocument5 pagesDrug StudyEjie Boy IsagaNo ratings yet
- Patient - S Load FormDocument2 pagesPatient - S Load FormEjie Boy IsagaNo ratings yet
- NCP SviDocument4 pagesNCP SviEjie Boy IsagaNo ratings yet
- I. Physical Exam: Poor Skin TurgorDocument8 pagesI. Physical Exam: Poor Skin TurgorEjie Boy IsagaNo ratings yet
- Perpetual Succour Hospital 3A-Floor PlanDocument1 pagePerpetual Succour Hospital 3A-Floor PlanEjie Boy IsagaNo ratings yet
- Philippine Nurses Licensure Examination Failure: A Lived ExperienceDocument16 pagesPhilippine Nurses Licensure Examination Failure: A Lived ExperienceEjie Boy IsagaNo ratings yet
- TPR Monitoring Sheet: University of San Jose-Recoletos College of NursingDocument1 pageTPR Monitoring Sheet: University of San Jose-Recoletos College of NursingEjie Boy IsagaNo ratings yet
- Nursing Care PlanDocument6 pagesNursing Care PlanEjie Boy IsagaNo ratings yet
- Trait TheoryDocument6 pagesTrait TheoryEjie Boy Isaga100% (1)
- Informed ConsentDocument1 pageInformed ConsentEjie Boy IsagaNo ratings yet
- Treatment Guidelines For Tuberculosis (RIPE) : Preventive TherapyDocument4 pagesTreatment Guidelines For Tuberculosis (RIPE) : Preventive TherapyEjie Boy IsagaNo ratings yet
- CHN ActivitiesDocument11 pagesCHN ActivitiesEjie Boy IsagaNo ratings yet
- Discharge Plan FormDocument2 pagesDischarge Plan FormEjie Boy IsagaNo ratings yet
- Physical AssessmentDocument3 pagesPhysical AssessmentEjie Boy IsagaNo ratings yet
- NCP'SDocument10 pagesNCP'SEjie Boy IsagaNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanEjie Boy IsagaNo ratings yet
- Inhaled SteriodsDocument7 pagesInhaled SteriodsEjie Boy IsagaNo ratings yet
- Functional Anatomy of The Respiratory System NoseDocument5 pagesFunctional Anatomy of The Respiratory System NoseEjie Boy IsagaNo ratings yet
- Battles Fought On The Great Wall of China Qin DynastyDocument2 pagesBattles Fought On The Great Wall of China Qin DynastySachin NagmotiNo ratings yet
- EVM TechmaxDocument96 pagesEVM Techmaxnikhileshdhuri97No ratings yet
- SR-36-01-01 HAZOP TOR Rehman Production FacilityDocument30 pagesSR-36-01-01 HAZOP TOR Rehman Production FacilityMuhammad.Saim100% (1)
- (HMI-LP-RT30 + R131-A - User Manual) A06 - ENDocument110 pages(HMI-LP-RT30 + R131-A - User Manual) A06 - ENrehanNo ratings yet
- UVU Jungle Marathon 2012 BookDocument41 pagesUVU Jungle Marathon 2012 BookGerhard FlatzNo ratings yet
- The Normal DistributionDocument30 pagesThe Normal DistributionJohn Rich CaidicNo ratings yet
- FlapDocument100 pagesFlapRicha Agrawal100% (2)
- Structural and Literary DevicesDocument40 pagesStructural and Literary Devicesapi-237159930No ratings yet
- Describe Physical and Chemical Change OperationallyDocument2 pagesDescribe Physical and Chemical Change OperationallyMaria Anna GraciaNo ratings yet
- Sample Ale ExamDocument37 pagesSample Ale ExamMarian Lim100% (1)
- Relative Color Pickup of Three Different Knits and Predictive Dyeing Recipe FormulationDocument17 pagesRelative Color Pickup of Three Different Knits and Predictive Dyeing Recipe FormulationNguyễn Huy CườngNo ratings yet
- Textbook Pediatric Behavioral Nutrition Factors Environment Education and Self Regulation 1St Edition Areej Hassan Ebook All Chapter PDFDocument39 pagesTextbook Pediatric Behavioral Nutrition Factors Environment Education and Self Regulation 1St Edition Areej Hassan Ebook All Chapter PDFjanet.galloway812100% (8)
- Quarter 3 - Las No. 1 (Week 5-7) Active Recreation (Street and Hip-Hop Dances) (Pe10Pf-Iiia-H-39, Pe10Pf-Lllc-H-45)Document11 pagesQuarter 3 - Las No. 1 (Week 5-7) Active Recreation (Street and Hip-Hop Dances) (Pe10Pf-Iiia-H-39, Pe10Pf-Lllc-H-45)hakkensNo ratings yet
- MGje 6 Fix GX PK Yp RBJ LBRDocument9 pagesMGje 6 Fix GX PK Yp RBJ LBRBANOTH KUMARNo ratings yet
- Business Presentation YAKULTDocument12 pagesBusiness Presentation YAKULTJosuaNo ratings yet
- Ciarrochi Fisher and Lane Link Between Values and Well-Being Among People With Cancer 2010 Psycho OncologyDocument9 pagesCiarrochi Fisher and Lane Link Between Values and Well-Being Among People With Cancer 2010 Psycho OncologyJuan C. VargasNo ratings yet
- Hybrid Vehicle A Study On Technology IJERTV3IS120917 PDFDocument8 pagesHybrid Vehicle A Study On Technology IJERTV3IS120917 PDFAshish MathurNo ratings yet
- Ex 4Document4 pagesEx 420-MCE-63 SYED HASSAN KUMAILNo ratings yet
- Geometry - Olympiad Material BY DR SHYAM SUNDAR AGRAWALDocument67 pagesGeometry - Olympiad Material BY DR SHYAM SUNDAR AGRAWALdrssagrawalNo ratings yet
- AM1000 Modbus Protocol en VA0Document4 pagesAM1000 Modbus Protocol en VA0Pedro José Arjona GonzálezNo ratings yet
- Asma G.SDocument5 pagesAsma G.SAfia FaheemNo ratings yet
- Price List 2018Document20 pagesPrice List 2018Imml TasbiNo ratings yet
- KONAN Emmanuel Sales Technical Engineer 16 Juin 23Document1 pageKONAN Emmanuel Sales Technical Engineer 16 Juin 23EMMANUEL KONANNo ratings yet
- Credit Card Fraud Detection Using Improved Deep Learning ModelsDocument22 pagesCredit Card Fraud Detection Using Improved Deep Learning ModelsrauhNo ratings yet
- Synchronous Generators: Instructional ObjectivesDocument18 pagesSynchronous Generators: Instructional Objectivessanthosh2009No ratings yet
- EQUILIBRIUMDocument1 pageEQUILIBRIUMMohammed IliasNo ratings yet
- Bored Piles - Bilfinger Spezialtiefbau GMBHDocument4 pagesBored Piles - Bilfinger Spezialtiefbau GMBHOga MeoNo ratings yet
- Autonomous University of Baja California: Faculty of Engineering Aerospace EngineeringDocument18 pagesAutonomous University of Baja California: Faculty of Engineering Aerospace EngineeringOscar Oreste Salvador CarlosNo ratings yet