Professional Documents
Culture Documents
Chapter 15 Key Terms
Chapter 15 Key Terms
Uploaded by
jenn1722Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 15 Key Terms
Chapter 15 Key Terms
Uploaded by
jenn1722Copyright:
Available Formats
CHAPTER 15 REVIEW/KEY TERMS
Digestion System: Nutrients are required for normal body function, Carbohydrates, proteins, lips, vitamins, minerals (derived from food). Obviously the food we ear is too big to be directly passed into blood, so the digestive system digests food into smaller molecules, absorb smaller molecules into the blood. Digestive system consists of Alimentary canal (GI tract, from mouth to anus) where the food passes through. Accessory Organs of the DS- Liver (make bile), Gallbladder (store bile), Pancreas (make pancreatic juice), Salivary glands (makes enzymes), Appendix. Essential Organs of the DS- Mouth, Esophagus, Stomach, Sm Intestine, Lg intestine, rectum, anal canal. Digestion- involves 2 parts: Mechanical digestion ( mastication-chewing, stomach churning, and peristalsis, physically breaking down food) and chemical digestion with the addition of hydrolysis (addition of water to the small absorbable nutrient molecules) ( enzymes in saliva, acid of stomach, bile from liver, chemically breaking down food into small parts). NONABSORBABLE FOOD MOLECULES + WATER digestive enzymes ABSORBABLE NUTRIENT MOLECULES Substrate- a number of different types of enzymes are involved in digestion. Each type of digestive enzyme acts on a specific substrate ( a particular type of food molecule and speeds up its breakdown into smaller molecules). A series of digestive reactions involving several digestive enzymes from different parts of the digestive system are usually required to break down complex food molecules into absorbable nutrients. Absorption The process by which nutrients pass from the digestive tract into the blood Accessory organs- Organs that have a digestive function but are not part of the alimentary canal
Alimentary canal also called the GI tract. the tube through which food passes from the mouth to the anus. Open at both ends. Various portions of the alimentary canal are specialized to perform different digestive functions. The hollow space within the GI tract through which food passes is called the lumen. - Mouth, stomach churning with acid, small intestine absorbing things, large intestine get water out. Happens in a certain process to obtain all needed nutrients. Structure of the Wall- 4 layers! Mucosa, Submucosa, muscularis, serosa. Lumen (hole)- mucosa- submucosa (blood vessels/nerves); 2 layers everywhere BUT stomach. - Mucosa- innermost layer, consists of a surface layer of columnar epithelial tissue supported by underlying connective tissue that contains a few smooth muscle cells. The epitheal cells produce digestive secretions and mucus. The epithelium is often folded to increase the surface area that is in contact with food. The mucosa has different functions in different parts of the digestive tract. In some regions it only secretes mucus, which protect underlying cells. In others, it secretes mucus and digestive fluids containing enzymes, and it absorbs nutrients. mucous membrane- secretes digestive enzymes and mucus) - Submucosa-lies between the muscular layer and the mucosa, contains nerves, lymphatic vessels, and blood vessels embedded in loose connective tissue. loose connective tissue, holds all mucosa in place, houses blood and lymph vessels- that are necessary for absorption. - Muscularis- lies just under the serosa,2 layers of smooth muscle for peristalsis. Smooth muscle x2 run parallel to each other to move food along. Circular muscle layer- going around, longitudinal layer-going length, their contractions constrict the tube. Contractions of these muscular layers mix food with digestive secretions and move food through the alimentary canal. - Serosa- outermost layer, serous membrane, secretes serous fluid to prevent sticking, connective tissue, keep everything moving properly.
Movements- Smooth muscle layers produce two types of movement, mixing, and peristalsis. - Mixing movements (segmentation) alternating rhythmic contractions in short sections of the tube. Mix food in lumen with secretions - Peristalsis: propels food along the canal. Circular muscle fibers produce ring-like constrictions that move along tube in wavelike manner. Pushes food in front of it by a pinching motion Mouth- Functions: intake of food, mechanical breaking during mastication of food into small pieces, mixing it with saliva to start chemical digestion, swallowing it. It is surrounded by cheeks, palate (hard palate-front, soft palate-back), and tongue, teeth. Mixing the food with salvia. - Soft palate ends with ulvula - Bumps on tongue are called papilla not taste buds or taste hairs - Frenulum is whats under tongue to hold it in place (what some kids have to get snipped) - Mechanical breaking food into small pieces during mastication Teeth- accessory structures involved in mastication. Humans form 2 sets of teeth. Deciduous teeth (first set, baby teeth, fall out 6-7) Permanent teeth (32 teeth, second set of teeth, adult teeth) - 32 permanent teeth, four types: incisors (biting off food) cuspids (canine, grasp and tear food) bicuspids ( 4, used for chewing/crushing) Molars (3 sets, used for chewing/crushing) - BOTH bicuspids and molars crush and grind food
Tooth Anatomy- Crown (visible, portion above gingiva) root (below gumline, embedded in socket in alveolar bone of jaw) ; Attachment of root to jaw: Cementum-attaching to bone, Peridontal membrane- keeping tooth in bone.
Composition of a tooth- Dentin (below enamel, bulk of tooth, bone-like, with a cavity you can start to see dif color here) Enamel ( hardest surface of the body, resists abrasion caused by chewing) Pulp Cavity- central portion, blood vessels, and nerves enter cavity through root canal, and with a really bad cavity you can start to see the pulp cavity. Chime- liquefied food entering the small intestine from the stomach. Food is mixed with gastric juice and as digestion occurs, it is converted into a semi liquid substance called chime. Small amounts are released intermittently into the duodenum by the opening of the pyloric sphincter. Digestion mechanical and chemical processes that convert non-absorbable foods into absorbable nutrients Duodenum- The first part of the small intestine, which receives bile and pancreatic juice Peristalsis- wave like contractions that move food through the alimentary canal Sphincter- circular muscle that closes an opening Substrate- A chemical that is acted upon and changed by an enzyme Segmentation- mixing movements that involve ring-like contractions at multiple places along the alimentary canal followed by relaxation as the contractions form at other locations. Papillae- a small nipple like projection Mastication- the chewing of food Deciduous teeth- The first set of teeth, which are lost and replaced by permanent teeth. 20 deciduous teeth, 10 in each jaw, all are in place by age 3. Gradually shed starting at about 6 yrs of age and are lost in the same order as their emergence. The loss of a deciduous tooth occurs because the growth of a permanent tooth underneath it causes reabsorption of the root. Later, the emerging permanent tooth pushes out the deciduous tooth.
Permanent teeth- begin appearing at about six years of age when the first molats erupt. All of the permanent teeth, except the third molars, are in place by age 16. The third molars (wisdom teeth) erupt between 17-21 years of age, or they may never emerge. In many persons there is insufficient room for the third molars so they become impacted and often must be surgically removed. The 32 permanent teeth, 16 in each jaw, consist of four different types: incisors, cuspids, bicuspids, and molars. Crown- The portion that protrudes above the gingiva (or gum) covering the alveolar bone. Root- embedded in a socket in the alveolar cementum attaches the root to the tough periodontal membrane whose fibers penetrate into the bone. Dentin- a hard bone like substance, under the enamel and cementum and around the pulp cavity. Enamel- part of the crown, overlaying the dentin. Hardest substance in the body, and is located to resist the abrasion caused by chewing hard foods. Pulp cavity- root canal a central space in the interior of a tooth. In a molar, the pulp cavity is relatively large and roughly box-shaped. But in a cuspid, the pulp cavity is an elongated enlargement of the root canal. Pulp is a soft connective tissue that supports the blood vessels and nerves.
Salivary glands- secrete saliva into the mouth (which is full of enzymes) where it is mixed with food during chewing. The presence of food (or nonfood objects) in the mouth activated neural reflexes that stimulate the flow of saliva. Activated by the presence of food in the mouth or thoughts of food. The mere thought of appetizing food can stimulate the slow of saliva. The functions of saliva include binding food particles together, dissolving certain foods, cleansing and lubricating the mouth, and starting carbohydrate digestion. The sense of taste is dependent upon saliva because only dissolved food molecules can stimulate taste buds. There are 3 pairs of major salivary glands: the parotid, submandibular, and sublingual salivary glands. Parotid gland- opening side of mouth, cheek. largest salivary gland located in front of each ear over the masseter muscle. Parotid glands secrete saliva that is rich in amylase. Parotid secretions are emptied through a duct into the vestibule of the mouth near the upper second molars. Submandibular gland- found in the floor of the mouth, and produces a watery saliva that contains relatively little mucus. 2 under your tounge on both sides of the frenulum. gleeker. Secretions of the subman glands are emptied through ducts into the anterior part of the mouth at the base of the lingual frenulum. Sublingual gland- lie on the floor of the mouth under the tongue. Under tongue, row of bumps. They are the smallest of the major salivary glands. Their secretions consist mostly of mucus, and are emptied by several ducts into the floor of the mouth under the tongue. Saliva- consists mostly of water (99.5%), which helps to dissolve food substances, plus a small amount of other substances. Mucus helps to hold food particles together during chewing and swallowing. Saliva contains 2 enzymes salivary amylase, lysozyme (enzyme that kills certain bacteria). Mucus binds food during chewing and swallowing.
Salivary amylase- digestive enzyme that speeds up the breakdown of starch and glycogen. Acts on starch and glycogen (polysaccharides) and speeds up their breakdown into maltose, a disaccharide sugar. The action of salivary amylase continues for a few minutes after food enters the stomach, but it soon stops because it is inactivated by the strong acidity of gastric juice. Lysozyme- Enzyme that kills bacteria. Digestion in the mouth- Both mechanical and chemical digestion take place in the mouth. Mechanical digestion in the mouth consists of breaking food into smaller pieces and mixing it with saliva during chewing. This improves chemical digestion because the smaller pieces have an increased surface area upon which digestive secretions may act. Chemical digestion starts in the mouth with the breakdown of certain complex carbs. Digestion of starch and glycogen into maltase by salivary amylase. Action of enzyme ends with acidity of gastric juice in the stomach. Chemical digestion continues until it reaches stomach. Makes food into bolus to move down into pharynx. Pharynx- the passageway that connects the nasal and oral cavities with the larynx and esophagus. It is part of both the respiratory and digestive systems. Its digestive function is the transport of food from the mouth to the esophagus during swallowing. Transports food from mouth to esophagus during swallowing, followed by the swallowing reflex. Swallowing Reflex- the reflex is activated when food is pushed into the pharynx by the tongue. The soft palate contracts upward, preventing food from entering the nasal cavity, and directs food downward into the pharynx, and this causes the epiglottis to flop over and cover the opening into the larynx. This action prevents food from entering the larynx and directs it into the esophagus. Food pushed into pharynx by tongue. Soft palate contracts upward, larynx moves upward.
Esophagus- a muscular tube that extends from the pharynx down through the thoracic cavity and the diaphragm to join with the stomach. Food is carried to the stomach by peristalsis. The esophageal mucosa produces mucus that lubricates the esophagus and aids in the passage of food. Esophagus does a lot of peristalsis. Uses peristalsis to move food into the stomach. Lower esophageal sphincter- the junction of the esophagus and stomach there is a thickened ring of circular muscle fibers known as the lower esophageal or cardiac, sphincter muscle. Located at the end of the esophagus. Guards the junction of stomach and esophagus. Normally constricted to prevent regurgitation/backflow of stomach contents into the esophagus, but it opens only to allow food to enter the stomach from the esophagus. Stomach- Lies in the upper left abdominal cavity, contains rugae. Structure of the stomach: May be subdivided into four regions: cardiac, fundic, pyloric regions, and body. - Cardiac: closest to heart, relatively small, receives food from esophagus. - Fundic: expands above the level of the cardiac region and serves as a temporary storage area. - Pyloric: narrow portion located near the junction wit the duodenum - Body: largest region of the stomach, located between the fundic and pyloric regions
Pyloric sphincter- thickened ring of circular muscle fibers that is located at the junction of the stomach and duodenum. This muscle usually is contracted, closing the stomach outlet, but it relaxes to let food pass into the small intestine. Rugae- the mucus membrane lining the stomach is quite thick and, in an empty stomach, is organized into numerous folds called rugae, which allow the mucosa to stretch as the stomach fills with food. The mucosa is dotted with numerous pores called gastric pits. Gastric Pits- The mucosa is dotted with numerous pores called gastric pits. These gastric pits are openings of the gastric glands that extend deep into the mucosa.
Gastric juice- the secretion of the gastric glands. Cells near the opening of the gastric glands secrete mucus that coats and protects the mucosa from the action of digestive secretions. Chief cells, located at the bottom of the glands, secrete digestive enzymes. Parietal cells, located in the midportion of the glands, secrete hydrochloric acid. Very acidic pH2 due to an abundance of hydrochloric acid. Gastric juice converts food into chyme (what food in stomach is called) Heartburn- sometimes the lower esophageal sphincter inadvertently allows a small amount of gastric juice to regurgitate into the base of the esophagus. When this occurs, the acidic gastric juice irritates the esophageal lining and produces a burning sensation called heartburn. Control of Gastric Secretions- rate of gastric secretions is controlled by both neural and hormonal means. Gastric juice is produced continuously, but its secretion is greatly increased when food is on the way to, or already in, the stomach. The sight, smell, or thought of appetizing food, food in the mouth, or good in the stomach stimulate the transmission of parasympathetic impulses that increase the secretion of gastric juice. These impulses also stimulate certain stomach cells to secrete a hormone called gastrin. As stomach contents are gradually emptied into the small intestine, there is a decrease in the frequency of parasympathetic impulses to the stomach, which reduces the secretion of gastric juice. When chime passes from the stomach into the small intestine, it stimulates the intestinal mucosa to release two hormones: cholecystokinin, and secretin, which reduce the secretion of gastric juice. Parasympathetic impulses decrease in frequency as stomach empties, decrease in gastric juice secretion. Intestinal mucosa secretes two hormones in response to chyme- cholecystokinin, secretinwhich both help decrease gastric juice secretion. 1. Parasympathetic preganglionic nerve fiber (vagus) parasympathetic postganglionic nerve fiber 2. Impulses stimulate the release of gastric juice from gastric glands 3. Impulses stimulate the release of gastrin 4. Gastrin stimulates glands to release more gastric juice
Gastrin- absorbed into the blood and is carried to stomach mucosal cells, increasing their secretions. Stimulates gastric glands to increase their rate of secretion. Source: gastric mucosa, food in the stomach stimulates release of gastrin Cholecytokinin- a hormone secreted by the mucosa of the small intestine that stimulates secretion of pancreatic juice and contraction of the gallbladder. Secreted by intestines in response to fat-laden chyme. Stimulates secretions rich in digestive enzymes. Reduces secretion of gastric glands; stimulates secretion of pancreatic juice that is rich in digestive enzymes; stimulates contraction of gallbladder, causing release of bile. Source: intestinal mucosa; fatty chyme stimulates the release of cholecystokinin. Secretin- a hormone secreted by the intestinal mucosa that stimulates the pancreas to secrete pancreatic juice. Released by intestines in response of acid chyme. Causes pancreas to produce juice rich in carbonates, neutralize acidity of chyme. Stimulates secretion of pancreatic juice that is rich in carbonates; inhibits gastric secretion. Source- intestinal mucosa; acid chyme stimulates the release of secretin. Digestion and absorption: Hydrochloric acid pH2-activates enzyme pepsin, denatures proteins, inhibits most bacterial growth, should probably kill all bacteria. Pepsin- most important digestive enzyme in the gastric juice and it is secreted in an inactive form that prevents digestion of calls secreting it. Once released into the stomach, pepsin is activated by the strong acidity of gastric juice. Pepsin acts on proteins and breaks these complexes into smaller molecules called peptides. However, peptides are still much too large to be absorbed. Rennin- an enzyme in the gastric juice of infants. It curdles milk proteins which keeps them in the stomach longer and makes them more easily digestible by pepsin.
Intrinsic factor- gastric juice also contains a substance known as intrinsic factor that is essential for the absorption of vitamin b12 by the small intestine. - Except for a few substances such as water, minerals, some drugs, and alcohol, little absorption occurs in the stomach. Pancreas- small pennant-shaped gland located posterior to the pyloric portion of the stomach. It is connected by a duct to the inner curve of the duodenum, the first part of the small intestine. The pancreas has both endocrine and exocrine functions. The digestive function of the pancreas is the secretion of pancreatic juice, and the cells that produce it compose most of the pancreas. Pancreatic juice is collected by tiny ducts that enter the pancreatic duct, which leaves the pancreas and joins the common bile duct just before the bile duct enters the duodenum. - Digestive function (exocrine function) is to secrete pancreatic juice - Neural control- parasymp impulses stimulate pancreas to secrete pancreatic juice - Hormonal control- secretin, cholecystokinin Digestion by Pancreatic enzymes- Pancreatic amylase (pancreatic enzyme that breaks down starch and glycogen to maltose.) - Pancreatic lipase ( pancreatic enzyme that breaks fats into monoglycerides and fatty acids. These molecules are absorbable.) - Trypsin (pancreatic enzyme that breaks proteins into peptides, activated by intestinal secretions)
Trypsin- Major pancreatic enzyme in pancreatic juice. Trypsin splits proteins into shorter amino acid chains called peptides. Like pepsin in the stomach, it is secreted in an inactive form and is activated only when mixed with intestinal secretions within the small intestine. This mode of secretion prevents the pancreatic cells from being digested by their own enzymatic secretions.
Lipase- pancreatic lipase, pancreatic enzyme, acts on fats (triglycerides) and splits them into monoglycerides and fatty acids that are absorbable. Control of Pancreatic Secretions: Controlled by both neural and hormonal mechanisms. Neural control is via parasymp fibers. When parasymp impulses active the stomach mucosa, they also stimulate the pancreas to secrete pancreatic juice. Hormonal control of pancreatic secretion results from two hormones that stimulate different types of pancreatic cells. Acid chyme entering the duodenum stimulates the intestinal mucosa to release the hormone secretin, which is carried by the blood to the pancreas, where it stimulates secretion of pancreatic juice that is rich in carbonates. Carbonates neutralize the acidity of the chyme entering the small intestine. Fat-laden chyme stimulates the production of cholecystokinin CKK by the intestinal mucosa. CCK stimulates secretion of pancreatic juice that is rich in digestive enzymes. 1. 2. 3. 4. 5. Acid chyme enters duodenum Secretin released into bloodstream from intestinal mucosa Secretin stimulates pancreas Pancreas secretes pancreatic juice Pancreatic juice, high in bicarbonate ions, neutralizes acidic chyme
Hepatic duct- As noted, the production of bile is the only digestive function of the liver. Bile is collected in tiny ducts that merge to form the bile ducts of the hepatic triads, which in turn, join to form the hepatic duct, which carries bile from the liver. Cystic duct- a short duct that extends from the gallbladder. Carries bile to and from the gallbladder. Common bile duct- the hepatic duct and the cystic duct, merge to form the common bild duct. Carries bile to the duodenum. Gallbladder- a small, pear-shaped sac that stores bile temporarily between meals
Liver- Largest gland in the body at 1.4 kg. Located in upper right quadrant, protected by ribs, dark reddish color, 4 lobes. Functions: secretion of bile, role in carbohydrate, lipid, protein digestion. Detoxifies poisons and harmful chemicals, removes worn out blood cells, stores fat, glycogen, iron, and several vitamins, synthesis of blood proteins, nutrient inter-converstion. Bile- continuously produced by liver cells. A yellowish green liquid. Consists of water, bile salts, bile pigments, cholesterol, and minerals. Bile pigments, mostly bilirubin, are a break-down waste products of hemoglobin breakdown. Bile salts are the only bile components that play a digestive role. When in contact with fatty substances they break up the lipid globules into very small droplets, called emulsification. Bile salts aid the digestion of lipids, also aid in the absorption of fatty acids, cholesterol, and fat-soluble vitamins by the sm intestine. Emulsification- greatly increases the surface area of the lipid substance exposed to water and lipid-digesting enzymes. Release of Bile- bile normally enters the duodenum only when food is present. When the intestine is empty, the hepatopancreatic sphincter at the base of the common bile duct is closed, and this forces bile to enter the gallbladder, where it is stored temporarily. When fat-laden chyme enters the duodenum, it stimulates the release of CKK from the intestinal mucosa. CKK is carried by the blood to the gallbladder, where it stimulates contraction of muscles in the gallbladder into the common bile duct. CKK relaxes the hp sphincter muscle so bile is injected into the sm intestine. This hormone control releases bile only when it is needed in the sm intestine. Small intestine- 2.5 cm wide, 6.4m long. Site of most digestion and absorption of nutrients. Three segments- Duodenum (1st and shortest) Jejunum (middle) Ileum (last and longest joins up with the large intestine, joins by ileocecal sphincter). Suspended by mesentery (curtain-like) from body wall. Goals of sm intestine, neutralize nutrients the chyme, absorb nutrients. Jejunum- middle section of sm intestine. Ileum- longest segment, joins with the large intestine to make ileocecal sphincter
Mesentery- suspends the sm intestine from the posterior abd wall. Provide support, but allow movement. Supports blood vessels, lymp vess, and nerves Villi- increase surface area, contain, lacteal, blood capillaries, micro villi on surface. Tiny projections from the mucosa that are extremely abundant. Microvilli- microscopic, formed by folds of plasma membranes that form the exposed surfaces of epithelial cells. Lacteal- centrally located lymphatic capillary, located on each villi. Surrounded by a blood capillary network. Intestinal juice- fluid secreted by intestinal glands. Slightly alkaline and contains abundant water and mucus. Provides an appropriate environment for the action of bile salts and pancreatic digestive enzymes within the small intestine. Recall that trypsin in pancreatic juice is activated only after being mixed with intestinal secretions. - Make in response to the chyme - Slightly alkaline with abundant water and mucus. - Forms appropriate environment for actions of bile salts and pancreatic digestive enzymes - Regulation of intestinal secretion - Mechanical stimulation due to presence of chyme - Activates secretion of intestinal juice and enzymes - Neural reflex due to intestinal wall stretch - Parasymp impulses increase the rate of intestinal secretions
Digestion and absorption, general events: vigorous contractions mix chyme with bile, pancreatic juice, and intestinal juice. Emulsification of fats with bile so you can digest fats, digestion of carbs, proteins, and lipids occur due to pancreatic and intestinal enzymes. Absorption of nutrients into the blood stream. Absorption of carbs: simple sugars (glucose, fructose, galactose) occurs primarily by active transport
Absorption of fats: Monocylcerides and fatty acids diffuse into epithelial cells, molecules recombine into fat molecules. Passively transported. 1. 2. 3. 4. 5. 6. Fatty acids in lumen of intestine Fatty acids from fat digestion enter epithelial cell Fatty acids are used to synthesize fats in endoplasmic reticulum Fats collect in clusters encased in protein to form chylomicrons Chylomicrons leave epithelial cell and enter lacteal Lymph in lacteal transports chylomicrons away from intestine
Mineral ions active transportepicellactive transport to liver Waterosmosis epicellosmosisto liver Polysaccharidesdigestiondisaccharidesdigestionmonosaccharideacti ve transportepicelldiffusionto liver Proteinsdigestionamino acidsactive transportepicelldiffusionto liver (passive transport) Fatsemulsification fat droplets digestionfatty acids, glyceroldiffusionepicellsecretionto lacteal-blood capillary, lymph capillary
Chylomicrons- form fat molecules, cholesterol, and phospholipids coated in protein. Move from epicells and into lacteals. Enter the left subclavian vein with lymph. - Very small fatty acids enter the villi directly without being recombined
Large Intestine Functions: food residue in the large intestine contains, water, minerals, bacteria, undigested and unabsorbed materials. Produces no digestive enzymes. Bacteria decompose non-digested food residues, yield B and K vitamins, produce flatus. Mucosa produces large amounts of mucus for lubrication and protection against abrasion. Just a lil bit of digestion going on here. Main function is absorption of water, minerals, and vitamins. Ileocecal valve- regulates movement of chyme
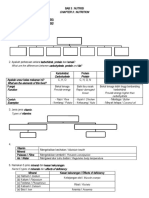
Major Digestive enzymes and their actions:
ENZYME Saliva Amylase
SUBSTRATE
PRODUCT
Starch and glycogen
Maltose
Gastric Juice Pepsin Proteins Peptides
Pancreatic Juice Amylase Lipase Trypsin Starch and glycogen Triglycerides Proteins Maltose monogly + fatty acids Peptides
Intestinal Juice Maltase Sucrase Lactase Lipase Peptidase Maltose Sucrose Lactose Trigylcerides Peptides Glucose Glucose + fructose Glucose + Galactose Monogly+fatty acids Amino Acids
Cecum- first portion of the large intestine, pouch-like, bulges below the ileocecal sphincter Appendix- slender worm-like, extends from the cecum and has no digestive function Colon- forms most of the large intestine, and it is subdivided into four segments. The ascending color extends upward from the cecum along the right side of the abd, as it nears the liver, it turns left to become the transverse colon. Near the spleen, the transverse colon turns downward to become the descending colon along the left side of the abd. Near the pelvis, the descending colon becomes the sigmoid colon, which is characterized by an S-shaped curvature leading to the rectum. Rectum- short, terminal portion of the large intestine. Anal canal- last portion of the rectum and exteriorly opening into the anus. Anus- kept closed except during defecation, involuntarily controlled: internal anal sphincter; voluntarily controlled: external anal sphincter Feces- shit. End product. Large amounts of bacteria, mucus, water, and nondigested food residues. Color is due to bile.
Defecation Reflex: 1. Rectum fills with feces and stretches (which triggers it to contract) 2. Stretching triggers contractions that increase pressure, opens internal sphincter 3. If external anal sphincter is relaxed, shitting occurs. 4. If external anal sphincter stays contracted, holding of the poop occurs.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5824)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Dysrhythmia Recognition Pocket Reference Card PDFDocument14 pagesDysrhythmia Recognition Pocket Reference Card PDFjenn1722100% (2)
- Med Surg Quiz 1 Review.Document3 pagesMed Surg Quiz 1 Review.jenn1722No ratings yet
- Nutrition & You - Chapter 3Document30 pagesNutrition & You - Chapter 3Bridget KathleenNo ratings yet
- P Harm FinalDocument1 pageP Harm Finaljenn1722No ratings yet
- Hemodynamic Management Pocket Card PDFDocument8 pagesHemodynamic Management Pocket Card PDFjenn1722No ratings yet
- Burns Case Study TwoDocument2 pagesBurns Case Study Twojenn1722100% (11)
- Professional and Educational Development in NursingDocument30 pagesProfessional and Educational Development in Nursingjenn1722No ratings yet
- Preceptor Evaluation FormDocument2 pagesPreceptor Evaluation Formjenn1722No ratings yet
- Home Health National Patient Safety GoalsDocument3 pagesHome Health National Patient Safety Goalsjenn1722No ratings yet
- Ethical Concepts in NursingDocument18 pagesEthical Concepts in Nursingjenn1722No ratings yet
- Legal Issues in Nursing - With Class IntroductionDocument37 pagesLegal Issues in Nursing - With Class Introductionjenn1722No ratings yet
- 298 Quiz 2 Study GuideDocument3 pages298 Quiz 2 Study Guidejenn1722No ratings yet
- Quiz 2 Study Guide - SHOCK!!! 25 Questions READ BOOK!!! Know Charts Esp. Stages of Shock ChartDocument1 pageQuiz 2 Study Guide - SHOCK!!! 25 Questions READ BOOK!!! Know Charts Esp. Stages of Shock Chartjenn1722No ratings yet
- Clinical Worksheet: /var/www/apps/conversion/tmp/scratch - 2/182114054Document20 pagesClinical Worksheet: /var/www/apps/conversion/tmp/scratch - 2/182114054jenn1722No ratings yet
- Crash Cart: Marcha M Phillips Hondros College School of NursingDocument5 pagesCrash Cart: Marcha M Phillips Hondros College School of Nursingjenn1722No ratings yet
- BIO 260 SU 12 Exam 4 Study Tables C & DDocument2 pagesBIO 260 SU 12 Exam 4 Study Tables C & Djenn1722No ratings yet
- IV - Dressing Change and Taping June 2010Document1 pageIV - Dressing Change and Taping June 2010jenn1722No ratings yet
- BIO 260 SU 12 Exam 4 Study Tables A & BDocument3 pagesBIO 260 SU 12 Exam 4 Study Tables A & Bjenn1722No ratings yet
- Chapter 16 ReviewDocument21 pagesChapter 16 Reviewjenn1722No ratings yet
- Study Guide: Chapters 1 - 3 BIO 250Document2 pagesStudy Guide: Chapters 1 - 3 BIO 250jenn1722No ratings yet
- RN and LPN Scope of PracticeDocument6 pagesRN and LPN Scope of Practicejenn1722No ratings yet
- Med-Surg Final Jeopardy Review.Document3 pagesMed-Surg Final Jeopardy Review.jenn1722No ratings yet
- Acid Base Who Is Your DaddyDocument66 pagesAcid Base Who Is Your Daddyjenn1722100% (14)
- Case Study FistulectomyDocument94 pagesCase Study FistulectomynycharlzNo ratings yet
- A - Detailed - Lesson - Plan - in - Science - Grade - Rayge DemoDocument6 pagesA - Detailed - Lesson - Plan - in - Science - Grade - Rayge Demoraygelyn apostolNo ratings yet
- Git NotabeneDocument212 pagesGit NotabeneRoshan VjNo ratings yet
- Gen Bio 2Document35 pagesGen Bio 2acers filedumpNo ratings yet
- Pathophysiology of EsophagusDocument36 pagesPathophysiology of EsophagusShivani Lal0% (1)
- Lesson 4 Digestive SystemDocument10 pagesLesson 4 Digestive SystemJulio De GuzmanNo ratings yet
- Why Is Digestion Important?Document4 pagesWhy Is Digestion Important?Jat GomezNo ratings yet
- Anatomy of The Digestive System-NotesDocument78 pagesAnatomy of The Digestive System-NotesDerrick njugunaNo ratings yet
- Science 8 Fourth 4 DaysDocument4 pagesScience 8 Fourth 4 DaysAshley Lopez100% (5)
- Locomotion & SupportDocument34 pagesLocomotion & SupportIntanNurDaniaNo ratings yet
- Gastrointestinal System 2016Document87 pagesGastrointestinal System 2016nurul dwi ratihNo ratings yet
- Animal Diversity Slides 2023 LWMDocument117 pagesAnimal Diversity Slides 2023 LWMVictoria LowmanNo ratings yet
- Diarrhea CSDocument24 pagesDiarrhea CSMASIINo ratings yet
- Biology - Course - Haidar RahhalDocument36 pagesBiology - Course - Haidar RahhalFatima SlimNo ratings yet
- Gastro 2014 Handout Wo Images PDFDocument188 pagesGastro 2014 Handout Wo Images PDFmike huntNo ratings yet
- Classes of Food Carbohydrate Protein Fat Vitamin Mineral Fibre WaterDocument6 pagesClasses of Food Carbohydrate Protein Fat Vitamin Mineral Fibre WaterNoor FadzleezaNo ratings yet
- Digestive System Processes and Regulation - Anatomy and PhysiologyDocument13 pagesDigestive System Processes and Regulation - Anatomy and PhysiologyFlonie DensingNo ratings yet
- Infusion Pump / Medicpro (KL 8052N)Document2 pagesInfusion Pump / Medicpro (KL 8052N)MEDIC PRO ServiceNo ratings yet
- Physiology A (GLORIANIESCOTO) - Gastrointestinal Tract Physiology Part 1Document7 pagesPhysiology A (GLORIANIESCOTO) - Gastrointestinal Tract Physiology Part 1Raian Isabelo SuyuNo ratings yet
- Diabetic Gastroparesis Principles and Current Trends in ManagementDocument42 pagesDiabetic Gastroparesis Principles and Current Trends in ManagementErika AvilaNo ratings yet
- CH 26 Student DigestiveDocument68 pagesCH 26 Student DigestiveMaski03No ratings yet
- Alimentary Tract-22073Document4 pagesAlimentary Tract-22073daniel balteanNo ratings yet
- (L7) - (NEET 2.0) - Digestion and Absorption - 1st JuneDocument98 pages(L7) - (NEET 2.0) - Digestion and Absorption - 1st JuneUpal Pramanick100% (1)
- PeristalticDocument2 pagesPeristalticAllyzah Faith BernalesNo ratings yet
- Marketing Management Kotler Keller 14th Edition Solutions ManualDocument24 pagesMarketing Management Kotler Keller 14th Edition Solutions ManualStephanieGarciawora100% (46)
- MC Graw Hill Foundation NEET Biology Class 10Document242 pagesMC Graw Hill Foundation NEET Biology Class 10Aquib IrshadNo ratings yet
- GROUP 1 - Digestive SystemDocument76 pagesGROUP 1 - Digestive SystemMa. Therese CampoNo ratings yet
- Q4 Science 8 Week1Document4 pagesQ4 Science 8 Week1Mischelle Pumar DyNo ratings yet
- Nutritional Foundations and Clinical Applications A Nursing Approach 6th Edition Grodner Test BankDocument25 pagesNutritional Foundations and Clinical Applications A Nursing Approach 6th Edition Grodner Test BankNatalieDownsjfai100% (50)