Professional Documents
Culture Documents
Failure To Thrive
Failure To Thrive
Uploaded by
ibbs91Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Failure To Thrive
Failure To Thrive
Uploaded by
ibbs91Copyright:
Available Formats
Failure to Thrive Defined as suboptimal growth and weight gain seen on a growth chart.
Fall across 2 centile lines on growth chart = mild Fall across 3 centile lines on growth chart = severe
Repeat observations are essential and FTT is difficult to assess off one reading However a reading below 0.4th centile should always prompt investigation. Mostly due to inadequate food intake. NB it is normal for an infant to lose 10% of birth weight in first few days of life Causes: Inadequate intake Inadequate retention Malabsorption Failure to utilise nutrients Increased requirements Inadequate intake Organic causes Impaired suck/swallow o Cleft lip/palate, neurological disorders Anorexia o Chronic illness leading to anorexia Crohns, renal disease, cystic fibrosis etc Non-organic causes Inadequate availability of food o Poor feeding techniques o Socioeconomic status Pyschosocial deprivation o Poor maternal bonding o Poor maternal education Neglect/abuse o Including factitious illness to cause deliberate FTT Inadequate retention Severe gastro-oesophageal reflux disease Malabsorption Coeliac disease Cystic Fibrosis Cows milk protein intolerance Cholestatic liver disease Short bowel syndrome Post-Necrotising enterocolitis Failure to utilise nutrients
Chromosomal abnormalities IUGR or extreme prematurity Metabolic disturbance
Increase requirements Hyperthyroidism Cystic fibrosis Malignancy Infection (HIV, immunodeficiency) Congenital heart disease Chronic renal failure Investigations: Detailed history including: Food diary PMH Familial growth patterns Family history Developmental history Social history Examination should focus on eliciting signs of organic disease Further information may be needed from health visitors, GP or other professionals involved in the family care Investigations for organic disease: FBC o Anaemia, neutropenia, lymphopenia (immune deficiency) U+E o Renal disease LFT o Liver disease TFT o Thyroid disease C-reactive protein o Inflammation Iron studies o Iron deficiency anaemia IgA tissue transglutaminase antibodies o Coeliac disease Urine dipstick, microscopy and culture o Urine infection, renal disease Genetic testing o Chromosomal abnormalities CXR and sweat test o Cystic fibrosis
Management: Mostly managed in primary care with an MDT approach: Health visitor Paediatric dietician Speech and language therapist (if feeding disorder) Social services (may be appropriate) Hospital admission only needed for children <6months with severe FTT needing active refeeding References Tom Lissauer, Graham Clayden, Illustrated Textbook of Paediatrics. Fourth Edition, 2012
You might also like
- BRS PediatricsDocument825 pagesBRS PediatricsJsph Ldrn Rly93% (14)
- Case Study Liver CirrhosisDocument64 pagesCase Study Liver CirrhosisJoseph Emmanuel Canda100% (1)
- Pediatri Nutrition Support Handbook PDFDocument153 pagesPediatri Nutrition Support Handbook PDFAhmed M MakhloufNo ratings yet
- Nutrition in Infancy and ChildhoodDocument16 pagesNutrition in Infancy and ChildhoodThịnh Nguyễn PhúcNo ratings yet
- Pat 2 Medsurg1Document20 pagesPat 2 Medsurg1api-300849832No ratings yet
- Failure To ThriveDocument11 pagesFailure To ThriveFiraFurqaniNo ratings yet
- Adepoju - Failure To ThriveDocument37 pagesAdepoju - Failure To ThriveAdepoju Victor AbiolaNo ratings yet
- Failure To ThriveDocument15 pagesFailure To ThriveSiti Nursuhada binti Mohd AminNo ratings yet
- Case Presentation CKDDocument35 pagesCase Presentation CKDKojo EgyirNo ratings yet
- Failure To Thrive - AAPDocument11 pagesFailure To Thrive - AAPAlexNo ratings yet
- Case Press FinalDocument32 pagesCase Press FinalmadsoleNo ratings yet
- Failure To ThriveDocument93 pagesFailure To ThriveMuhammad Siddiq100% (1)
- Enteral Nutrition of Preterm BabyDocument54 pagesEnteral Nutrition of Preterm Babylordoftheweb100% (5)
- National TB ControlDocument25 pagesNational TB Controlnirmal2444No ratings yet
- CPG On AID PPT PresentationDocument83 pagesCPG On AID PPT Presentationsharmaine peroNo ratings yet
- Pathological Changes of DM - 2023Document53 pagesPathological Changes of DM - 2023Visura PrabodNo ratings yet
- HISTORY # 1 - PCGH, EchavezDocument11 pagesHISTORY # 1 - PCGH, EchavezHynne Jhea EchavezNo ratings yet
- Failure To ThriveDocument19 pagesFailure To Thriveapi-662340011No ratings yet
- CASE STUDY TablesDocument9 pagesCASE STUDY TablesMicah MagallanoNo ratings yet
- Diabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inDocument28 pagesDiabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inKrissy GaluraNo ratings yet
- Toaz - Info Case Study Pneumonia PRDocument41 pagesToaz - Info Case Study Pneumonia PRTrixNo ratings yet
- Case Presentation: Patient Chart - Mary JohnsonDocument12 pagesCase Presentation: Patient Chart - Mary Johnsonivoneeh_16100% (1)
- Failure To Thrive: Premi Suresh, MD, FAAPDocument57 pagesFailure To Thrive: Premi Suresh, MD, FAAPsiti hazard aldinaNo ratings yet
- Article On DengueDocument6 pagesArticle On Dengueاحمد احمدNo ratings yet
- Coughs and Colds Nurse Management of Upper Respiratory Tract InfectionDocument3 pagesCoughs and Colds Nurse Management of Upper Respiratory Tract InfectionMichael Anthony ErmitaNo ratings yet
- Discharge Plan EndoDocument3 pagesDischarge Plan EndoCharlayne AnneNo ratings yet
- Diabetes Mellitus in ChildrenDocument10 pagesDiabetes Mellitus in Childrenapi-322579342No ratings yet
- Case Study Liver CirrhosisDocument55 pagesCase Study Liver CirrhosisJoseph Emmanuel CandaNo ratings yet
- Case Stude NNJDocument6 pagesCase Stude NNJmuzamirNo ratings yet
- DKA Study GroupDocument24 pagesDKA Study GroupAqila MumtazNo ratings yet
- Kuliah TuberkulosisDocument64 pagesKuliah TuberkulosisLeonardNo ratings yet
- Blighted OvumDocument9 pagesBlighted OvumAdes Desrita CarmeliaNo ratings yet
- Pediatrics: 2 Case ReportDocument50 pagesPediatrics: 2 Case ReportSam Raven AndresNo ratings yet
- Environmental and Nutritional DiseasesDocument44 pagesEnvironmental and Nutritional DiseasesAppas Saha100% (1)
- Paediatric Diabetic KetoacidosisDocument7 pagesPaediatric Diabetic KetoacidosisJuan Carlos BayonaNo ratings yet
- Infant of Diabetic MotherDocument1 pageInfant of Diabetic MotherMithlesh DewanganNo ratings yet
- Clinical Case PresentationDocument44 pagesClinical Case PresentationRUSSELL CILOTNo ratings yet
- HIV AIDS MNT Case StudyDocument22 pagesHIV AIDS MNT Case StudyAlana67% (3)
- Management of Patients With Intestinal and Rectal DisordersDocument33 pagesManagement of Patients With Intestinal and Rectal DisordersDoneva Lyn MedinaNo ratings yet
- Cirrhosis Case For PrintingDocument12 pagesCirrhosis Case For PrintingSean Mercado100% (1)
- Typhoid FeverDocument38 pagesTyphoid FeverRonelenePurisimaNo ratings yet
- Celiac DiseaseDocument2 pagesCeliac DiseaseGiabellNo ratings yet
- Case 10Document7 pagesCase 10Mariel VillamorNo ratings yet
- Adolescents With Tuberculosis-A Review of 145 Cases, 2016Document5 pagesAdolescents With Tuberculosis-A Review of 145 Cases, 2016Yoseph Arif Putra100% (1)
- Cyclic Vomiting SyndromeDocument17 pagesCyclic Vomiting Syndromeminerva_stanciuNo ratings yet
- Complementary FeedingDocument29 pagesComplementary FeedingRebecca BrandonNo ratings yet
- Philippine Urological Association, Inc.: Executive Committee and Board Members 1997Document12 pagesPhilippine Urological Association, Inc.: Executive Committee and Board Members 1997mits98No ratings yet
- Leprosy CHNDocument14 pagesLeprosy CHNPhillip ChingNo ratings yet
- Hiv Case StudyDocument2 pagesHiv Case Studyapi-485814878No ratings yet
- MCN Oral RevalidaDocument11 pagesMCN Oral RevalidaADOLF FRUELAN HIDALGONo ratings yet
- Angelica M.docx LFD 1Document2 pagesAngelica M.docx LFD 1Angelica Malacay RevilNo ratings yet
- Pedia 2017 Case ProtocolDocument14 pagesPedia 2017 Case ProtocolArjay Amba0% (1)
- Renal Tubular AcidosisDocument48 pagesRenal Tubular Acidosissny PNo ratings yet
- Sample Case Presentation - Occult BacteremiaDocument51 pagesSample Case Presentation - Occult BacteremiaPrecious Gutierrez BagazinNo ratings yet
- Kenya ARV Guidelines 2018Document230 pagesKenya ARV Guidelines 2018Felix Wafula MusibiNo ratings yet
- UrosepsisDocument22 pagesUrosepsisWita Ferani KartikaNo ratings yet
- Case Study 11Document3 pagesCase Study 11api-347141638No ratings yet
- Dengue Breakbone Fever Case StudyDocument53 pagesDengue Breakbone Fever Case StudyLeilani Rodriguez AmpoNo ratings yet
- CASE REPORT Hepatitis EditedDocument42 pagesCASE REPORT Hepatitis EditedpernandaselpiaNo ratings yet
- Update On Cancer CachexiaDocument4 pagesUpdate On Cancer CachexiaIyanNo ratings yet
- PPP - Kwashiorkor & MarasmusDocument19 pagesPPP - Kwashiorkor & MarasmusJanine Kristine ManaoisNo ratings yet
- Research PaperDocument28 pagesResearch PapertaniamanansalabautistaNo ratings yet
- What Is DiabetesDocument34 pagesWhat Is DiabetesSunil RawatNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- London GP GroupsDocument13 pagesLondon GP Groupsibbs91No ratings yet
- Appendix 1 - Person Specification Recruitment To One-Year Fixed Term Stand-Alone F2 ProgrammeDocument3 pagesAppendix 1 - Person Specification Recruitment To One-Year Fixed Term Stand-Alone F2 Programmeibbs91No ratings yet
- Peterborough and Stamford Hospitals Nhs Foundation TrustDocument5 pagesPeterborough and Stamford Hospitals Nhs Foundation Trustibbs91No ratings yet
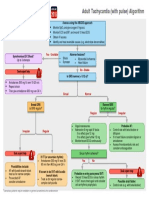
- G2015 Adult Tachycardia PDFDocument1 pageG2015 Adult Tachycardia PDFibbs91No ratings yet
- Case-Based Discussion (CBD) Assessment FormDocument4 pagesCase-Based Discussion (CBD) Assessment Formibbs91No ratings yet
- Tutorials Jan To July 2019Document1 pageTutorials Jan To July 2019ibbs91No ratings yet
- Failure To ThriveDocument3 pagesFailure To ThrivefernandoNo ratings yet
- Dietetic Intern-No Answers FTT WorksheetDocument2 pagesDietetic Intern-No Answers FTT Worksheetapi-457873289No ratings yet
- Infant Nutrition 101: Amanda Mcmurray Registered Dietitian PediatricsDocument21 pagesInfant Nutrition 101: Amanda Mcmurray Registered Dietitian PediatricsxxpixiexxNo ratings yet
- Weight Faltering - MDIDocument10 pagesWeight Faltering - MDIYurika Elizabeth SusantiNo ratings yet
- CARE PLANS Part 2Document8 pagesCARE PLANS Part 2Mhee FaustinaNo ratings yet
- Case Study 7B For HS 103 Week 8Document7 pagesCase Study 7B For HS 103 Week 8Rijane Tabonoc OmlangNo ratings yet
- SOS Feeding ApproachDocument18 pagesSOS Feeding ApproachJohn Doe100% (1)
- Child Growth. Growth Disorders UpdateDocument57 pagesChild Growth. Growth Disorders UpdateShahpoor Ahmad ShirzadaNo ratings yet
- Help With Infant Failure To Thrive Care Plan: Sign in Sign UpDocument20 pagesHelp With Infant Failure To Thrive Care Plan: Sign in Sign Upapoc lordNo ratings yet
- UntitledDocument386 pagesUntitledLet B100% (1)
- MK Ka Paeds Bazooka-1Document132 pagesMK Ka Paeds Bazooka-1venture kulNo ratings yet
- JCurrMedResPract7117-1973431 052854Document5 pagesJCurrMedResPract7117-1973431 052854maudinaa_lisaNo ratings yet
- Failure To Thrive (FTT) Atau: Gagal TumbuhDocument25 pagesFailure To Thrive (FTT) Atau: Gagal TumbuhSuryani MalikNo ratings yet
- Child Guidance ClinicDocument8 pagesChild Guidance Clinicpurnasha_mitra12100% (6)
- Toronto Notes - PaediatricsDocument100 pagesToronto Notes - Paediatricsmun_chloe100% (7)
- UNICEF-WHO - SimplifiedApproaches - BriefingNote - July 2023Document7 pagesUNICEF-WHO - SimplifiedApproaches - BriefingNote - July 2023Veronica Romero MouthonNo ratings yet
- TRANS - Pediatric Patient ProblemsDocument4 pagesTRANS - Pediatric Patient ProblemsRencel Hope Bañez100% (1)
- Aspen Pediatric Heart Failure NutritionDocument7 pagesAspen Pediatric Heart Failure NutritionkhairachungNo ratings yet
- Nutritional Management of Cystic FibrosisDocument56 pagesNutritional Management of Cystic FibrosisReine Salamoun100% (1)
- FTT Lession PlanDocument10 pagesFTT Lession PlanSAYMABANUNo ratings yet
- High Risk Newborn - Study GuideDocument10 pagesHigh Risk Newborn - Study GuideMalou Yap Buot100% (1)
- Factors Related To Malnutrition Among Children Below Five Years in Rengen Health Center III, Kotido DistrictDocument13 pagesFactors Related To Malnutrition Among Children Below Five Years in Rengen Health Center III, Kotido DistrictKIU PUBLICATION AND EXTENSION100% (1)
- 3-Malnutrition in Children 2022Document27 pages3-Malnutrition in Children 2022Emma GumaNo ratings yet
- Consensus Pediatrics: Growth Assessment and Growth FailureDocument38 pagesConsensus Pediatrics: Growth Assessment and Growth FailurePutri Inda FawziaNo ratings yet
- Hubungan Asupan Protein, Seng, Zat Besi, Dan Riwayat Penyakit Infeksi Dengan Z-Score Tb/U Pada BalitaDocument24 pagesHubungan Asupan Protein, Seng, Zat Besi, Dan Riwayat Penyakit Infeksi Dengan Z-Score Tb/U Pada BalitadaniNo ratings yet
- Nutritional Rehabilitation For Children With Congenital Heart Disease With Left To Right ShuntDocument10 pagesNutritional Rehabilitation For Children With Congenital Heart Disease With Left To Right ShuntJiradett Arm KerdsriNo ratings yet